Abstract
Background
Neuropathic pain seriously affects life quality, and it is urgent to develop novel drugs with high efficacy and few side effects. Sanguinarine (SG) is a natural plant medicine with anti-inflammatory and neuroprotection effects. This study aimed to investigate the effect of SG on chronic constriction injury (CCI)-induced neuropathic pain.
Materials and Methods
CCI rat model was established and rats were randomly divided into sham group, sham + SG group (6.25 mg/kg), CCI group, CCI + SG group (1.00, 2.50 and 6.25 mg/kg). The mechanical sensitivity and heat hypersensitivity of rats were monitored at different time points. Immunohistochemical, PCR, Western blot and ELISA were used to analyze p-p38 MAPK, NF-κB p65, TNF-α, IL-1β, and IL-6 levels.
Results
The mechanical sensitivity and heat hypersensitivity significantly reduced in rats of CCI group, but significantly increased in rats of CCI+SG group. TNF-α, IL-1β, and IL-6 levels significantly increased in the spinal cord of CCI rats, but significantly decreased in rats of CCI+SG group. In addition, p38 MAPK activator antagonized beneficial effects of SG on neuropathic pain. Overexpression of p38 MAPK reduced the mechanical sensitivity and heat hypersensitivity, and enhanced NF-κB activity and the expression of inflammatory factors in CCI rats.
Conclusion
SG alleviates neuropathic pain via suppressing p38MAPK signaling and downregulating the expression of TNF-α, IL-1β, IL-6 and NF-κB activation. SG may be a potential therapeutic agent to treat neuropathic pain.
Keywords: sanguinarine, neuropathic pain, inflammatory cytokines, NF-kB, p38MAPK
Introduction
Neuropathic pain (NP) is characterized by hyperalgesia, spontaneous pain and allodynia, and is usually caused by physical sensory system damage or disease in peripheral or central nervous system.1 NP seriously affects life quality. Increasing lines of evidence have shown that p38 mitogen-activated protein kinase (MAPK) plays an active role in the occurrence and maintenance of hyperalgesia and hyperalgesia.2 Meanwhile, inflammatory factors play an important role in the occurrence and development of pain-related diseases.3 For example, interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), and interleukin-1β (IL-1β) are involved in the occurrence and development of NP.4 In addition, p38 MAPK could mediate the activation of nuclear factor kappa B (NF-κB) and trigger inflammatory response.5
Sanguinarine (SG) (13-methyl (1,3) benzodioxolo [5,6-c]-1,3-dioxolo [4,5-i] phenanthridinium) is an alkaloid extracted from the root of Sanguinaria canadensis and other poppy fumaria species.6,7 Recent evidence suggests that SG inhibits the occurrence and development of inflammation via the inhibition of the phosphorylation of p38 MAPK and the activation of NF-κB.8 However, there are few reports about the effect of SG on NP.
The aim of this study was to establish a rat model with chronic constriction injury (CCI) of the sciatic nerve to investigate whether SG exerts analgesic effects on NP, and to elucidate the underlying mechanism.
Materials and Methods
Animals
This study was carried out in strict accordance with the recommendations in the Guidelines for Shandong University. All experiments were approved by the Animal Ethics Committee of Shandong University following Chinese National Guidelines for Experimental Animal Welfare. Adult male Sprague Dawley rats (weight 180–200 g) were provided by Shandong Animal Experimental Animal Center and placed in a humidity control room at a temperature of 24 ± 1 °C with light/dark cycle for 12 hours. Animals had free access to food and water. All rats were randomly divided into six groups (n = 8): sham group, sham + SG group (6.25 mg/kg), CCI group, CCI + SG group (1.00, 2.50 and 6.25 mg/kg). For CCI model, rats were anesthetized with isoflurane and placed in the lateral position and sciatic nerve was exposed, 4 sites were properly ligated with 3.0 chromic catgut, and the two ligation sites were separated by about 1 mm. In sham group, sciatic nerve was exposed but not ligated. Immediately after surgery, sham + SG group (6.25 mg/kg) and CCI + SG group (1.00, 2.50 and 6.25 mg/kg) were intraperitoneally injected with SG (1.00, 2.50 and 6.25 mg/kg). Sham group and CCI group were injected with the same dose of 0.9% normal saline, once every two days.
For subgroup analysis, the rats were further divided into six groups (n = 8): sham group, intrathecal injection of 10 μL normal saline daily for seven consecutive days; CCI group, intrathecal injection of 10 μL normal saline daily for seven consecutive days; CCI + SB203580 group, intrathecal injection of 10 μL 20 umol/L of SB203580 daily for seven consecutive days; CCI + N.S group, intrathecal injection of 10 μL normal saline daily for seven consecutive days; CCI + SG (6.25 mg/kg) group, intraperitoneal injection of SG (6.25 mg/kg) once every two days; CCI + SG (6.25 mg/kg) + anisomycin group, intraperitoneal injection of SG (6.25 mg/kg) once every two days and intrathecal injection of 10 μL 20 μmol/L of anisomycin daily for seven consecutive days.
Behavioral Assessment of Mechanical Sensitivity and Heat Hypersensitivity
Based on the method of Vivancos et al,9 an electronic von Frey plantar aesthesiometer (Model: 2091, Yuyan Instruments Co., Ltd, Shanghai, China) was used to measure paw withdrawal mechanical threshold (PWT). Rats were placed on an elevated wire mesh, and the hind paw was vertically stimulated by the metal probe, and the stimulation intensity gradually increased, resulting in rapid paw contraction or paw licking within 3 seconds. The minimum stimulation intensity for the rat to produce a contraction response was recorded as PWT.
The heat hypersensitivity was measured using the plantar test.10 Rats were allowed to acclimate for 30 minutes before the test, then each rat was placed on an elevated glass platform and the heat source was located in the middle of the plantar of the left hind paw under the glass plate. The intensity of thermal stimulation was adjusted to reach 50 °C and the cut-off delay was set to 25s in order to prevent tissue injury. The time from the start of stimulation to the time the hind paw is lifted, licked or avoided was recorded as thermal withdrawal latency (TWL). The behavioral tests were carried out before CCI surgery and 1, 3, 7 and 14 days after CCI.
Immunohistochemical Staining
The collected samples were fixed in 10% neutral formaldehyde solution, embedded in paraffin, and cut into sections. After de-paraffinization, gradient alcohol dehydration and antigen repair, the sections were blocked with normal goat serum, and then incubated with p-p38MAPK primary antibody (1:200, k20329-jhs, baileibo, China) overnight at 4°C. After washing with PBS, the sections were incubated with to secondary antibody coupled to peroxidase enzyme and then stained with diaminobenzidine and hematoxylin. Three sections were randomly selected from each tissue sample. Each section was observed with 10×40 optical microscope in five fields. Image Proplus 6.0 image analysis system was used for analysis.
Western Blot Analysis
Spinal cord tissue was collected and then mechanically homogenized, Homogenates were centrifuged at 13,000 rpm for 15 min at 4 °C, and then the supernatant was collected. Protein concentration in the lysate was evaluated using Protein Assay Kit (PC0020, Solanum). Equal amounts of total protein were separated by electrophoresis on sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to polyvinylidene fluoride membrane (Merk Millipore, USA). The membrane was incubated with 5% skim milk for 2 hours at room temperature, then incubated with antibodies for p-p38 MAPK, NF-κB p65 and β-actin (all from Cell Signaling) at 4 °C overnight, and finally incubated with secondary antibodies. ChemiDoc MP imaging system (Bio-Rad) was used to detect protein expression, and IMAGE J software (version 1.47, USA) was used to analyze the gray levels.
RT-PCR
Total RNA was extracted from the spinal cord tissue using the Trizol (Quick-Start Protocol, Cat. Nos.74104), and treated with DNase I and isopropanol. Complementary DNA (cDNA) was synthesized with Oligo(dt) 12-18 using QuantiNovaTM Relieve Transcription kit (Quick-Start Protocol, Cat. Nos.205411). PCR was performed using QuantiNova SYBR® Green PCR kit (Quick-Start Protocol, Cat. Nos.208054). The primers were as follows: NF-κB p65, 5ʹ- GTGCAGAAAGAAGACATTG −3ʹ (forward) and 5ʹ- AGGCTAGGGTCAGCGTATGG −3ʹ (relieve); β-actin, 5ʹ-ACTCTGTGTGGATTG-GTGGC-3ʹ (forward) and 5ʹ-AGAAAGGGTGTAAAACGCAGC-3ʹ (relieve). The results were analyzed by 2-ΔΔCt method.
Enzyme-Linked Immunosorbent Assay (ELISA)
The dorsal horn of the spinal cord was collected and the contents of TNF-α, IL-1β and IL-6 were quantified by rat-specific ELISA kits (ELISA: MultiSciences, China) according to the manufacturer’s instructions.
Statistical Analysis
All data were expressed as mean ± standard error (SD). The data were analyzed by ANOVA followed by post hoc test of LSD (if variance is equal) or Dunnett T3 (if variance is not equal). P < 0.05 was considered statistically significant.
Results
SG Improved PWT and TWL of CCI Rats
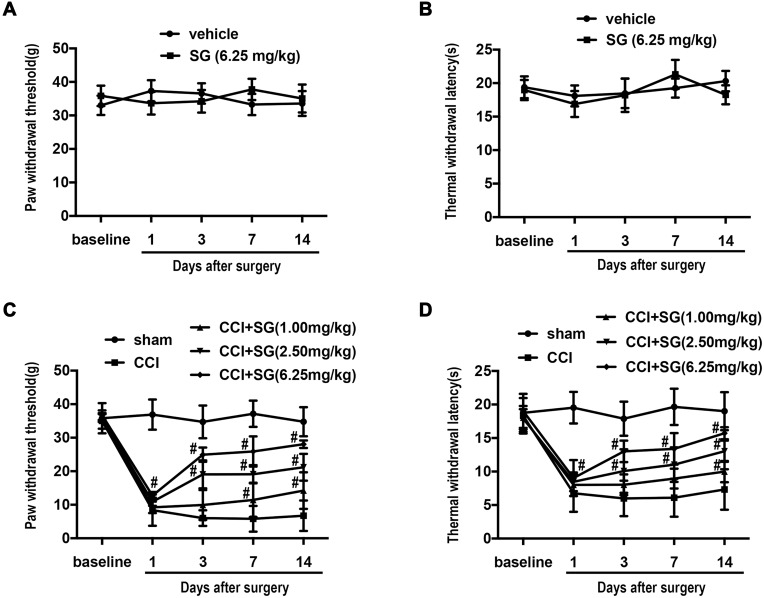
Compared with the sham group (vehicle), the sham+ SG group (6.25 mg/kg) showed no significant changes in PWT and TWL (Figure 1A and B, n=8, P >0.05). As shown in Figure 1C and D, compared with the sham group, PWT and TWL of CCI group significantly reduced after surgery (n=8, * P<0.05), but SG treatment significantly increased PWMT and PWTL in dose-dependent manner (n=8, P <0.05). These results indicate that the mechanical sensitivity and heat hypersensitivity significantly reduced in rats of CCI group, but significantly increased in rats of CCI+SG group.
Figure 1.
The effect of SG on PWT and TWL of CCI Rats. Compared with sham group, PWT and TWL did not change significantly after surgery ((A and B), n = 8, P > 0.05). PWT (C) and TWL (D) in CCI group were significantly lower. PWT and TWL significantly increased in CCI + SG group (1.00, 2.50 and 6.25 mg/kg). #p<0.05 vs CCI group.
Abbreviations: SG, sanguinarine; CCI, chronic constriction injury; PWT, paw withdrawal threshold; TWL, thermal withdrawal latency.
SG Decreased Levels of Pro-Inflammatory Factors in Spinal Dorsal Horn of CCI Rats
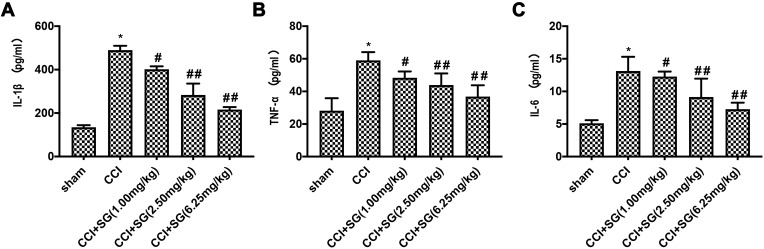
ELISA showed that levels of IL-1β (Figure 2A), TNF-a (Figure 2B), and IL-6 (Figure 2C) in the dorsal horn of the spinal cord of CCI group significantly increased in CCI group compared with sham group (P <0.05). However, intraperitoneal injection of SG (1.00, 2.50, 6.25 mg/kg) reduced the levels of TNF-α, IL-1β, and IL-6 in a dose-dependent manner (P <0.05). These results indicate that SG decreased levels of pro-inflammatory factors in spinal dorsal horn of CCI rats.
Figure 2.
The effects of SG on IL-1β, TNF-a, and IL-6 levels in spinal dorsal horn of CCI Rats. The levels of IL-1β, TNF-a, and IL-6 levels in spinal dorsal horn were detected by ELISA. The levels of IL-1β (A), TNF-a (B), and IL-6 (C) significantly increased in CCI group, but significantly decreased in CCI+SG group. Data are shown as mean ± SD, n = 3. *p<0.05 vs sham group, #p<0.05 and ##p<0.01 vs CCI group.
Abbreviations: SG, sanguinarine; CCI, chronic constriction injury.
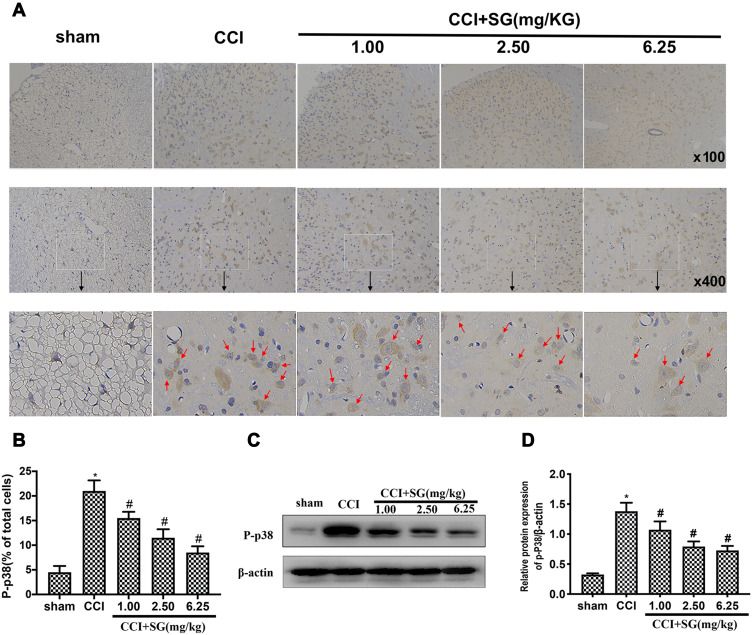
SG Inhibited the Activation of P38 Protein in Spinal Dorsal Horn
Immunohistochemical analysis showed that compared with Sham group, the activation of p38 MAPK (p-p38 MAPK staining) in spinal dorsal horn of rats in CCI group significantly increased. However, SG reduced p-p38 MAPK staining in CCI + SG group (1.00, 2.50 and 6.25 mg/kg) in a dose-dependent manner (Figure 3A and B).
Figure 3.
The effects of SG on the activation of p38 MAPK in spinal dorsal horn of CCI Rats. (A) Immunohistochemical staining of p-p38 protein in spinal dorsal horn. (B) Quantitative analysis of the percentage of positive p-p38 staining in all cells. (C) Western blot analysis of p-p38 protein levels in spinal dorsal horn. (D) Densitometry analysis of relative p-p38 level versus β-actin. Data are shown as mean ± SD, n = 3. Compared with the sham operation group (*P < 0.05), compared with CCI group (#P < 0.05).
Abbreviations: SG, sanguinarine; CCI, chronic constriction injury.
Furthermore, Western blot analysis confirmed that p-p38 MAPK levels in spinal dorsal horn of rats in CCI group significantly increased, while SG significantly decreased p-p38 MAPK levels in CCI + SG group (1.00, 2.50 and 6.25 mg/kg) in a dose-dependent manner (Figure 3C and D).
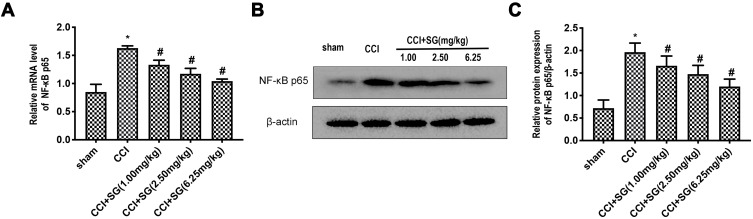
SG Inhibited the Activation of NF-κB in Spinal Dorsal Horn
RT-PCR and Western blot analysis showed that mRNA and protein levels of NF-κB p65 in spinal dorsal horn of rats in CCI group increased significantly (P < 0.05). However, mRNA and protein levels of NF-κB p65 in the spinal dorsal horn of CCI rats decreased significantly after SG treatment in a dose-dependent manner (P < 0.05, Figure 4A–C).
Figure 4.
Effect of SG on NFκB p65 expression in spinal dorsal horn of CCI rats. (A) RT-PCR analysis of NF - κ B p65 mRNA levels in the dorsal horn of the spinal cord. (B) Western blot analysis of NF - κ B p65 protein levels in the dorsal horn of the spinal cord. (C) Densitometry analysis of NF - κ B p65 protein levels in the dorsal horn of the spinal cord. Data are shown as mean ± SD, n = 3. Compared with the sham operation group (*P < 0.05), compared with CCI group (#P < 0.05).
Abbreviations: SG, sanguinarine; CCI, chronic constriction injury.
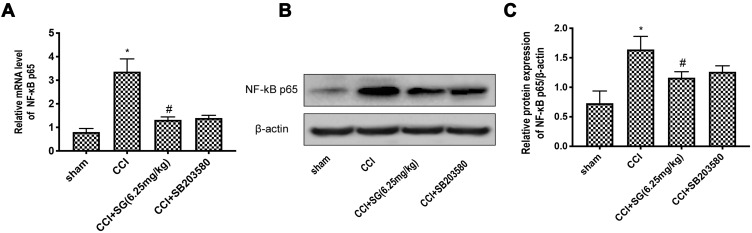
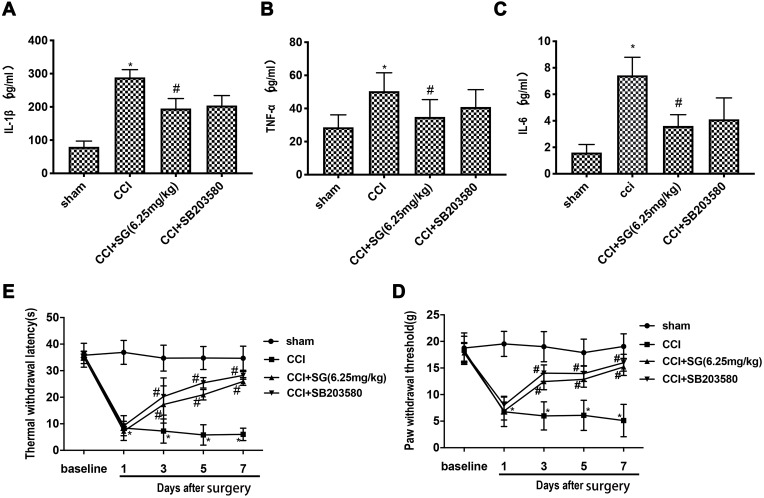
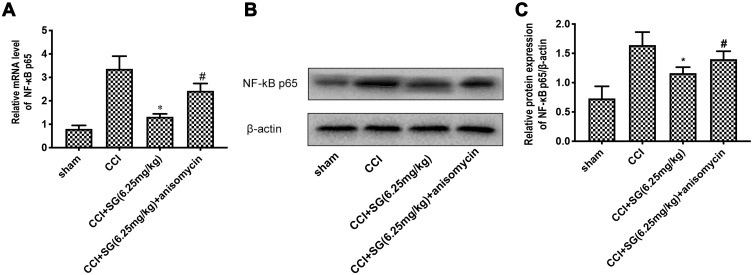
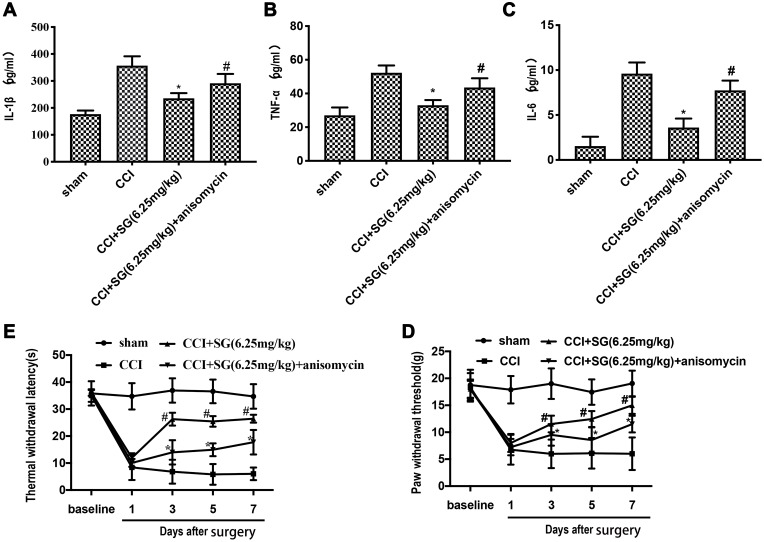
SG Inhibited p38MAPK Activation to Downregulate NF-κB in CCI Rats
To elucidate the mechanism by which SG inhibits the activation of NF-κB in CCI model, we focused on p38 MAPK pathway. Both SG and p38MAPK antagomir significantly inhibited the expression of NF-κB p65 (Figure 5A–C) and inflammatory factors (Figure 6A–C), while improved PWT and TWL significantly (p < 0.05) (Figure 6D–E). Consistently, p38MAPK agonists significantly increased the expression of NF-κB p65 (Figure 7A–C) and inflammatory factors (Figure 8A–C), while reduced PWT and TWL (p < 0.05) (Figure 8D–E). These results indicate that SG can inhibit neuroinflammation and the activation of NF-κB in CCI rats by inhibiting p38MAPK signaling.
Figure 5.
Effect of p38MAPK pathway inhibitor SB203580 on NF-κB in spinal cord of CCI rats. (A) RT-PCR analysis of NF - κ B p65 mRNA levels in the dorsal horn of the spinal cord. (B) Western blot analysis of NF - κ B p65 protein levels in the dorsal horn of the spinal cord. (C) Densitometry analysis of NF - κ B p65 protein levels in the dorsal horn of the spinal cord. Data are shown as mean ± SD, n = 3. Compared with the sham operation group (*P < 0.05), compared with CCI group (#P < 0.05).
Abbreviations: SG, sanguinarine; CCI, chronic constriction injury.
Figure 6.
Effects of p38MAPK inhibitor SB203580 on inflammatory factors, PWT and TWL in CCI rats. (A–C). ELISA of inflammatory factors TNF-a, IL-1B and IL-6. The data are expressed as mean ± SD, n = 3. Compared with the sham group (*P < 0.05), compared with CCI group (#P < 0.05). (D and E) PWT and TWL in each group. The data are expressed as mean ± SD, n = 8. Compared with the sham group (*P < 0.05), compared with CCI group (#P < 0.05).
Abbreviations: SG, sanguinarine; CCI, chronic constriction injury; PWT, paw withdrawal threshold; TWL, thermal withdrawal latency.
Figure 7.
Effect of p38MAPK agonist anisomycin on NF-κB in spinal cord of CCI rats. (A) RT-PCR analysis of NF - κ B p65 mRNA levels in spinal dorsal horn. (B) Western blot analysis of NF - κ B p65 protein levels in spinal dorsal horn. (C) Densitometry analysis of NF - κ B p65 protein levels in spinal dorsal horn. Data are shown as mean ± SD, n = 3. Compared with sham operation group (*P < 0.05), compared with CCI group (#P < 0.05).
Abbreviations: SG, sanguinarine; CCI, chronic constriction injury.
Figure 8.
The effect of p38 MAPK pathway agonist anisomycin on inflammatory factors, PWT and TWL of CCI rats. (A–C). ELISA of inflammatory factors TNF-a, IL-1B and IL-6. The data are expressed as mean ± SD, n = 3. Compared with sham group (*P < 0.05), compared with CCI group (#P < 0.05). (D and E) PWT and TWL in each group. The data are expressed as mean ± SD, n = 8. Compared with CCI group, *P < 0.05, compared with CCI + SG (6.25 mg/kg) group, #P < 0.05.
Abbreviations: SG, sanguinarine; CCI, chronic constriction injury; PWT, paw withdrawal threshold; TWL, thermal withdrawal latency.
Discussion
In this study, we chose CCI model to induce NP and found that PWT and TWL of CCI group were significantly lower than those of sham group. The reduced mechanical sensitivity and heat hypersensitivity in CCI model confirm successful establishment of rat model of NP. Based on this model we showed that SG treatment led to increased PWT and TWL in CCI rat model in a dose-dependent manner, indicating that SG can alleviate hyperalgesia in rats.
As we all know, inflammation is closely related to the occurrence and development of pain diseases, and pro-inflammatory factors play an important role in NP.11 In this study, the expression levels of IL-1β, IL-6 and TNF-α were quantified by ELISA, and the results showed that IL-1β, IL-6 and TNF-α levels in spinal cord tissue increased significantly in CCI model rat. However, after SG treatment, IL-1β, IL-6 and TNF-α levels decreased significantly in CCI model rat. Therefore, these data indicate that SG could alleviate pain in neurogenic rat by reducing the expression of pro-inflammatory factors in spinal cord.
p38MAPK and NF‐κB participate in the development and maintenance of NP.12 In one study, p38MAPK in spinal dorsal horn of CCI group was significantly activated compared to sham group.13 In another study on CCI rat model, NF-κB in spinal dorsal horn was upregulated to promote the expression and release of IL-1β, IL-6, TNF-α, resulting in NP.14 In this study, the results showed that compared with sham group, the expression levels of p38MAPK and NF-κB p65 increased significantly in spinal dorsal horn of CCI group. However, the upregulation of p-p38 and NF-κB p65 in CCI model rat could be significantly inhibited by SG in a dose-dependent manner.
The phosphorylation of p38MAPK can upregulate pro-inflammatory factors IL-1 β, IL-6, TNFα.15–18 In the pathological circumstance, NF-κB can be translocated from the cytoplasm to the nucleus to induces the expression of pro-inflammatory factors in the downstream inflammatory pathway.14 In order to further verify whether SG alleviates neuropathic pain in CCI model rat through p38MAPK signaling, we treated model rat with p38MAPK activator and antagonist. The results showed that the activation of p38 MAPK could reduce PWT and TWL. Nevertheless, silencing p38 MAPK had the opposite effects and remarkably inhibited the activation of NF-κB and the expression of inflammatory factors TNF-a, IL-1B and IL-6, similar to the effects of SG treatment. Furthermore, overactivation of p38 MAPK attenuated the inhibitory effects of SG on the activation of NF-κB and the expression of inflammatory factors TNF-a, IL-1B and IL-6. These results indicate that SG can exhibit anti-inflammation effects through inhibiting p38 MAPK, consistent with previous findings.8
In summary, our study provides strong evidence that SG alleviates NP via suppressing p38MAPK signaling, NF-κB activation and the expression of pro-inflammatory factors. Our new findings suggest that SG may be a potential therapeutic agent to treat NP.
Acknowledgments
The technical assistance of the Key Laboratory of Cerebral Microcirculation in Universities of Shandong (Taishan Medical University) is gratefully acknowledged.
Funding Statement
This work was supported by the Natural Foundation of Shandong Province (no. ZR2017PH010) and Taian Science and Technology Guidance Project (no. 2017NS0143).
Disclosure
The authors have no conflicts of interest.
References
- 1.Jensen TS, Baron R, Haanpää M, et al. A new definition of neuropathic pain. Pain. 2011;152(10):2204–2205. doi: 10.1016/j.pain.2011.06.017 [DOI] [PubMed] [Google Scholar]
- 2.Wang JY, Chen SP, Gao YH, Qiao LN, Zhang JL, Liu JL. Effect of repeated electroacupuncture intervention on hippocampal ERK and p38MAPK signaling in neuropathic pain rats. Evid Based Complement Alternat Med. 2015;2015:641286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munoz EM. Microglia-precursor cell interactions in health and in pathology. Biocell. 2018;42(2):41–45. doi: 10.32604/biocell.2018.07011 [DOI] [Google Scholar]
- 4.Old EA, Clark AK, Malcangio M. The role of glia in the spinal cord in neuropathic and inflammatory pain. Handb Exp Pharmacol. 2015;227:145–170. [DOI] [PubMed] [Google Scholar]
- 5.Cai Y, Li W, Tu H, et al. Curcumolide reduces diabetic retinal vascular leukostasis and leakage partly via inhibition of the p38MAPK/NF-κ B signaling. Bioorg Med Chem Lett. 2017;27(8):1835–1839. doi: 10.1016/j.bmcl.2017.02.045 [DOI] [PubMed] [Google Scholar]
- 6.Montes FQ, Vázquez-Hernández A, Fenton-Navarro B. Active compounds of medicinal plants, mechanism for antioxidant and beneficial effects. Phyton Int J Exp Bot. 2019;88:1–10. [Google Scholar]
- 7.Meng YY, Liu Y, Hu ZF, et al. Sanguinarine attenuates lipopolysaccharide-induced inflammation and apoptosis by inhibiting the TLR4/NF-κB pathway in H9c2 cardiomyocytes. Curr Med Sci. 2018;38(2):204–211. doi: 10.1007/s11596-018-1867-4 [DOI] [PubMed] [Google Scholar]
- 8.Deng W, Fang Y, Liu Y, et al. Sanguinarine protects against pressure overload-induced cardiac remodeling via inhibition of nuclear factor-κB activation. Mol Med Rep. 2014;10(1):211–216. doi: 10.3892/mmr.2014.2206 [DOI] [PubMed] [Google Scholar]
- 9.Vivancos GG, Verri Jr. WA, Cunha TM, et al. An electronic pressure-meter nociception paw test for rats. Braz J Med Biol Res. 2004;37(3):391–399. doi: 10.1590/S0100-879X2004000300017 [DOI] [PubMed] [Google Scholar]
- 10.Hargreaves K, Dubner R, Brown F, Flores C, Joris J. A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain. 1988;32(1):77–88. doi: 10.1016/0304-3959(88)90026-7 [DOI] [PubMed] [Google Scholar]
- 11.Calvo M, Dawes JM, Bennett DL. The role of the immune system in the generation of neuropathic pain. Lancet Neurol. 2012;11(7):629–642. doi: 10.1016/S1474-4422(12)70134-5 [DOI] [PubMed] [Google Scholar]
- 12.Austin PJ, Moalem-Taylor G. The neuro-immune balance in neuropathic pain: involvement of inflammatory immune cells, immune-like glial cells and cytokines. J Neuroimmunol. 2010;229(1–2):26–50. doi: 10.1016/j.jneuroim.2010.08.013 [DOI] [PubMed] [Google Scholar]
- 13.Cao J, Wang JS, Ren XH, Zang WD. Spinal sample showing p-JNK and P38 associated with the pain signaling transduction of glial cell in neuropathic pain. Spinal Cord. 2015;53(2):92–97. doi: 10.1038/sc.2014.188 [DOI] [PubMed] [Google Scholar]
- 14.Sun T, Luo J, Jia M, Li H, Li K, Fu Z. Small interfering RNA-mediated knockdown of NF-κBp65 attenuates neuropathic pain following peripheral nerve injury in rats. Eur J Pharmacol. 2012;682(1–3):79–85. doi: 10.1016/j.ejphar.2012.02.017 [DOI] [PubMed] [Google Scholar]
- 15.Fu ES, Zhang YP, Sagen J, et al. Transgenic inhibition of glial NF-kappa B reduces pain behavior and inflammation after peripheral nerve injury. Pain. 2010;148(3):509–518. doi: 10.1016/j.pain.2010.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saha RN, Jana M, Pahan K. MAPK p38 regulates transcriptional activity of NF-kappaB in primary human astrocytes via acetylation of p65. J Immunol. 2007;179(10):7101–7109. doi: 10.4049/jimmunol.179.10.7101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu Y, Liu Q, Zhang M, Yan Y, Yu H, Ge L. MicroRNA-362-3p attenuates motor deficit following spinal cord injury via targeting paired box gene 2. J Integr Neurosci. 2019;18(1):57–64. [DOI] [PubMed] [Google Scholar]
- 18.Xu L, Huang Y, Yu X, Yue J, Yang N, Zuo P. The influence of p38 mitogen-activated protein kinase inhibitor on synthesis of inflammatory cytokine tumor necrosis factor alpha in spinal cord of rats with chronic constriction injury. Anesth Analg. 2007;105(6):1838–1844. doi: 10.1213/01.ane.0000287660.29297.7b [DOI] [PubMed] [Google Scholar]