Abstract
Purpose
In overwhelmed emergency departments (EDs) facing COVID-19 outbreak, a swift diagnosis is imperative. CT role was widely debated for its limited specificity. Here we report the diagnostic role of CT in two EDs in Lombardy, epicenter of Italian outbreak.
Material and methods
Admitting chest CT from 142 consecutive patients with suspected COVID-19 were retrospectively analyzed. CT scans were classified in “highly likely,” “likely,” and “unlikely” COVID-19 pneumonia according to the presence of typical, indeterminate, and atypical findings, or “negative” in the absence of findings, or “alternative diagnosis” when a different diagnosis was found. Nasopharyngeal swab results, turnaround time, and time to positive results were collected. CT diagnostic performances were assessed considering RT-PCR as reference standard.
Results
Most of cases (96/142, 68%) were classified as “highly likely” COVID-19 pneumonia. Ten (7%) and seven (5%) patients were classified as “likely” and “unlikely” COVID-19 pneumonia, respectively. In 21 (15%) patients a differential diagnosis was provided, including typical pneumonia, pulmonary edema, neoplasia, and pulmonary embolism. CT was negative in 8/142 (6%) patients. Mean turnaround time for the first COVID-19 RT-PCR was 30 ± 13 h. CT diagnostic accuracy in respect of the first test swab was 79% and increased to 91.5% after repeated swabs and/or BAL, for 18 false-negative first swab. CT performance was good with 76% specificity, 99% sensitivity, 90% positive predictive value and 97% negative predictive value.
Conclusion
Chest CT was useful to streamline patients’ triage while waiting for RT-PCR in the ED, supporting the clinical suspicion of COVID-19 or providing alternative diagnosis.
Keywords: COVID-19, Diagnosis, Computed tomography, Triage, Emergency
Chest CT in the emergency department for suspected COVID-19 pneumonia
SARS-CoV-2 spread worldwide causing coronavirus disease 2019 (COVID-19) which may overlap seasonal flu and other respiratory diseases. COVID-19 lung involvement progresses toward a severe pneumonia in 15–20% of cases, requiring critical care in 5–10% of them [1]. Thus, expeditious and reliable diagnosis is imperative.
The cornerstone of COVID-19 diagnosis is RT-PCR from oral-nasopharyngeal swab. RT-PCR has near-perfect specificity, but limited sensitivity (30–70%) varying according to viral burden, symptoms severity, and time from symptoms onset [2]. Moreover, the turnaround time for results may be long in overwhelmed laboratories, as during epidemic growth [3]. Chest imaging showed good performance in COVID-19 pneumonia diagnosis [4–6], with chest X-ray representing the first line due to wide availability and portability [6], and CT outperforming RT-PCR sensitivity even in the early stages of the disease [5].
Despite the high sensitivity, the usage of CT to triage symptomatic patients with suspected COVID-19 pneumonia was questioned for a matter of specificity, being CT findings potentially overlapping to other viral pneumonia [7]. The aim of the study was to investigate the value of chest CT in triaging patients with suspected COVID-19 pneumonia in two emergency departments (EDs) in Lombardy, Italy.
We retrospectively analyzed 142 chest CT scans performed from March 8 to 30, 2020, at two tertiary-care University Hospitals in patients referring to the EDs for suspected COVID-19 pneumonia, with inconclusive or possible false-negative X-ray results [8]. Chest CT was performed on a dedicated scanner with a separated access applying standardized protocols for infection control.
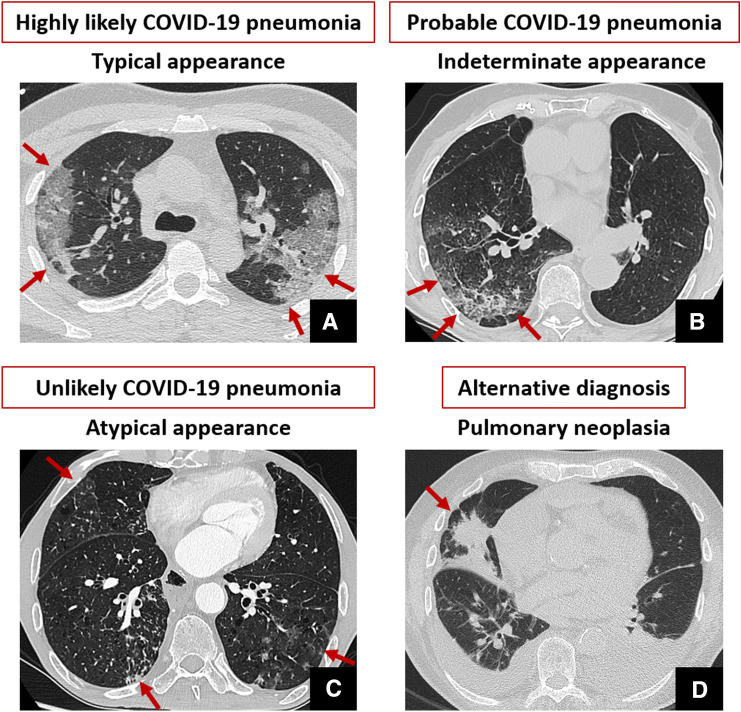
According to RSNA Expert Consensus [9], chest CT scans were classified into: (i) “highly likely COVID-19” in the presence of typical findings, (ii) “likely COVID-19” in the presence of indeterminate findings, (iii) “unlikely COVID-19” in the presence of atypical findings for COVID-19, (iv) “alternative diagnosis” in case of findings indicative for a different causes of symptoms, and (v) “negative” (Fig. 1).
Fig. 1.
Exemplifying CT findings for each class of COVID-19 pneumonia probability based on the presence of typical, indeterminate and atypical finding, or eventual absence of signs of viral pneumonia and alternative CT diagnosis. A is reported unenhanced thin-section axial CT image showing typical peripheral ground-glass opacity with superimposed interlobular septal thickening and intralobular lines visibility (“crazy-paving” pattern), involving both lungs. Unilateral involvement, considered one of the indeterminate features, is reported in B. Atypical findings (C) include bronchiolar wall thickening and tree-in-bud opacities with centrilobular nodules (arrows in C). Finally, alternative diagnosis (D) was reported in the case of chest CT findings not typical for interstitial pneumonia and with clear pulmonary or extra-pulmonary findings explaining symptoms and laboratory test alteration (e.g., pulmonary neoplasia, red arrow in D, associated with bilateral pleural and pericardial effusion)
Nasopharyngeal swabs results were collected, including turnaround time, number of swabs performed, and time-to-positive results.
CT sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were measured, considering results from repeated swabs or bronchoalveolar lavage (BAL) as reference standard.
Statistical analyses were performed using SPSS v.25.0.
All 142 patients (M = 101; median age 61 y.o. [interquartile range (IQR) 50–73]) suffered from fever (≥37.5 °C from a median of 7 days [IQR 3–10]), associated most frequently with cough (75/142, 53%), and dyspnea (45/142, 32%). Acute chest pain and gastrointestinal symptoms were rare (8/142, 6%, in both cases). At arrival, median oxygen saturation (SatO2) was 94% [89–96%].
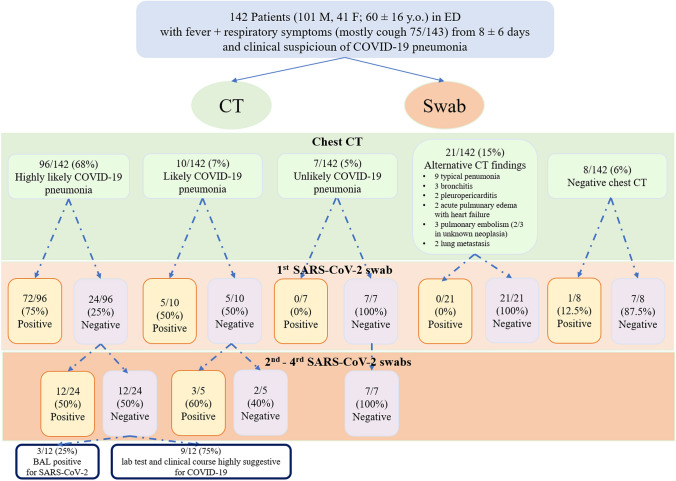
CT and swab results are summarized in Fig. 2.
Fig. 2.
CT and swabs results in triaging patients with suspected COVID-19 pneumonia. Flowchart of CT findings and nasopharyngeal swab results in 142 febrile patients attending the EDs of two hospital in Lombardy with clinical suspicious of SARS-CoV2 infection. The agreement between CT and RT-PCR increased after first swab, for a total of 18 patients initially false negative at RT-PCR on nasopharyngeal swab. Interestingly, CT in addition to the high sensitivity had the advantage to provide differential diagnosis useful for patients’ clinical management
Chest CT was acquired without contrast, except in 8 patients to exclude vascular events.
Chest CT showed typical findings for COVID-19 pneumonia in most of cases (96/142, 68%), while it was classified as “likely COVID-19 pneumonia” in 10/142 (7%), “unlikely” in 7/142 (5%), and “negative” in 8/142 (6%).
In 15% of patients (21/142) CT showed alternative diagnosis including lobar pneumonia, pulmonary edema, and neoplasia.
Turnaround time for first RT-PCR result was 30 ± 13 h (range 2–48 h). A median of 2 swabs was performed per patient.
Swab was negative for SARS-CoV2 infection in all CT scan classified as “unlikely” and “alternative diagnosis,” while was positive in a single case of “negative” CT.
The first swab was positive in 77/106 (73%) and negative in 29/106 (27%) patients classified as “highly likely” and “likely” at CT. In 18/29 (62%) patients, negative swabs turned to positive after repetition or BAL (mean time for positivization: 5 ± 4 days) (Fig. 3). In the remaining 9 patients, laboratory test and clinical course were highly suggestive for COVID-19. In one case classified as “likely COVID-19 pneumonia” H1N1 virus was isolated.
Fig. 3.
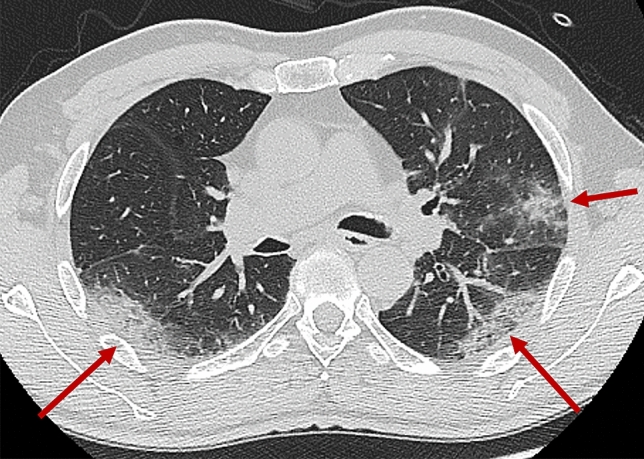
Chest CT typical COVID-19 pneumonia in a patient with initially negative swab. A 61-year-old man suffering from fever (39 °C), cough, and dyspnea from 7 days, presented to the emergency department of San Raffaele Hospital in Milan. Clinical evaluation and laboratory tests resulted highly suspicious for SARS-CoV2-related pneumonia. Nasopharyngeal swab and chest CT were immediately performed. CT showed peripheral opacity with crazy-paving pattern and consolidation (red arrows) mainly involving the upper left lobe and the lower lobes, mainly with posterior distribution. CT findings resulted highly suggestive for SARS-CoV2 pneumonia, but results from the first swab (available only 24 h later) resulted negative. In consideration of high clinical and CT suspicion, another swab was collected after 3 days, and it finally resulted positive
CT diagnostic accuracy was 79% in respect of first swab and raised to 91.5% after repeated swabs and/or BAL.
Chest CT performance in triaging symptomatic patients suspected for COVID-19 was good with 76% specificity, 99% sensitivity, 90% PPV, and 97% NPV.
Our data showed that during the rise of COVID-19 epidemic the integration of chest CT in triaging patients has high PPV and NPV in line with previous results [10, 11], with higher sensitivity than swab [5], which often needed to be repeated and is affected by long turnaround time.
One false negative was observed in a patient with CT performed within 2 days of symptoms onset, probably related to the known lower prevalence of parenchymal involvement in the earliest stages of disease [12, 13]. In our setting, CT specificity and PPV were slightly higher than in most previous reports [5, 10], probably in relation to the better clinical selection of patients and high pretest probability of disease in epidemic territories [8, 11].
Our findings highlight the unique capability of CT to provide alternative diagnoses in a substantial number of cases, which cannot be addressed with chest X-ray. In fact, although COVID-19 pneumonia was the prevalent causes of respiratory dysfunction during the outbreak, it was not the unique.
In agreement with the recent Fleischner Society expert consensus document [14], our data support the integration of CT in triaging suspected patients because it may streamline decision making in overwhelmed EDs, where oral-nasopharyngeal swab may not yet provide trustworthy and fast results, and avoiding exposure in non-COVID-19 patients.
Importantly, one case of H1N1 pneumonia was reported, for the known possibility of overlapping CT findings, highlighting the necessity to provide a microbiological confirmation also in patients with highly suggestive CT findings [8].
Our findings are applicable in a scenario of high prevalence of disease (around 40%), as occurred during the ascending phase of epidemic curve [11]; therefore, they cannot be generalized to low prevalence situation where could be expected a poor PPV [11].
The application of chest CT in triage suspected COVID-19 patients is related to the availability of a dedicated scanner, because long downtime (30–60 min after imaging a suspected patient) for room decontamination and passive air exchange may significantly interfere with routine clinical activity.
In conclusion, in the specific context of the overwhelmed EDs facing COVID-19 outbreak, chest CT may fasten triaging, while waiting for RT-PCR results, by supporting the clinical suspicion of COVID-19 or providing an alternative diagnosis with overlapped clinical presentation.
Acknowledgments
This work was supported by the Italian Ministry of Health with 5 × 1000 funds and by OSR Program COVID-19.
Compliance with Ethical Standards
Conflict of interest
Authors have no conflict of interest to disclose.
Ethical standards
Our research study includes human participants. The study protocol complies with the Declaration of Helsinki and was approved by the local hospital ethics committee (protocol no. 34/int/2020). Patients able to provide a signed informed consent were consented prior to data collection. The ethics committee waived the requirement for obtaining written informed consent for patients who had died or were unreachable after discharge.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 323(11):1061–1069. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed]
- 2.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W (2020) Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 10.1001/jama.2020.3786 [DOI] [PMC free article] [PubMed]
- 3.Reusken C, Broberg EK, Haagmans B, Meijer A, Corman VM, Papa A, Charrel R, Drosten C, Koopmans M, Leitmeyer K, On Behalf Of E-L, Erli N (2020) Laboratory readiness and response for novel coronavirus (2019-nCoV) in expert laboratories in 30 EU/EEA countries, January 2020. Euro Surveill 25(6). 10.2807/1560-7917.ES.2020.25.6.2000082 [DOI] [PMC free article] [PubMed]
- 4.Borghesi A, Zigliani A, Masciullo R, Golemi S, Maculotti P, Farina D, Maroldi R. Radiographic severity index in COVID-19 pneumonia: relationship to age and sex in 783 Italian patients. Radiol Med. 2020;125(5):461–464. doi: 10.1007/s11547-020-01202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L (2020) Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology:200642. 10.1148/radiol.2020200642 [DOI] [PMC free article] [PubMed]
- 6.Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvara S, Lucarini S, Busoni S, Mazzoni LN, Miele V. Chest X-ray in new coronavirus disease 2019 (COVID-19) infection: findings and correlation with clinical outcome. Radiol Med. 2020;125(8):730–737. doi: 10.1007/s11547-020-01232-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. Accessed 14 April 2020
- 8.Neri E, Miele V, Coppola F, Grassi R. Use of CT and artificial intelligence in suspected or COVID-19 positive patients: statement of the Italian Society of Medical and Interventional Radiology. Radiol Med. 2020;125(5):505–508. doi: 10.1007/s11547-020-01197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, Henry TS, Kanne JP, Kligerman S, Ko JP, Litt H (2020) Radiological society of North America expert consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol Cardiothoracic Imaging 2(2):e200152. 10.1148/ryct.2020200152 [DOI] [PMC free article] [PubMed]
- 10.Kim H, Hong H, Yoon SH (2020) Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology:201343. 10.1148/radiol.2020201343 [DOI] [PMC free article] [PubMed]
- 11.Esposito A, Palmisano A, Scotti GM, Morelli MJ, Vignale D, De Cobelli F, Tonon G, Tacchetti C (2020) Why is chest CT important for early diagnosis of COVID-19? Prevalence matters. medRxiv
- 12.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C (2020) Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology:200370. 10.1148/radiol.2020200370 [DOI] [PMC free article] [PubMed]
- 13.Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, Shi H, Zhou M (2020) Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology:200843. 10.1148/radiol.2020200843 [DOI] [PMC free article] [PubMed]
- 14.Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, Schluger NW, Volpi A, Yim JJ, Martin IBK, Anderson DJ, Kong C, Altes T, Bush A, Desai SR, Goldin J, Goo JM, Humbert M, Inoue Y, Kauczor HU, Luo F, Mazzone PJ, Prokop M, Remy-Jardin M, Richeldi L, Schaefer-Prokop CM, Tomiyama N, Wells AU, Leung AN (2020) The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the fleischner society. Chest. 10.1016/j.chest.2020.04.003