Abstract
Objective
We designed this systematic review of the available literature to measure the pooled prevalence of periodontal disease among Indian adults.
Methods
An electronic search was conducted for studies assessing the prevalence of periodontal disease (gingivitis and periodontitis) in India. The search yielded forty studies, of which thirty eligible cross-sectional studies assessing the prevalence among those 18 years and above were included. The methodological quality of the included studies was assessed. Meta-analyses were conducted for periodontitis outcomes, stratified for different covariates like age groups, gender, geographic region, population group, type of index and study quality. Pooled prevalence was used to estimate overall effect, with 95% confidence intervals (CI).
Results
A total of 92,219 adults participated in 30 studies included for qualitative analysis. Studies utilizing convenience sampling were excluded from quantitative analysis. Pooled prevalence estimates of periodontitis and gingivitis were assessed on from 24 to 21 studies respectively. We found that overall prevalence of periodontal disease was 51% (CI: 41.9-60.1) and gingivitis was 46.6% (CI: 37.8-55.5). Prevalence of mild to moderate periodontitis was 26.2% (CI: 21.1-31.6), while for severe periodontitis it was 19% (CI: 14.3-24.2). Participants 65 years or above had highest proportion of severe periodontitis (32.7%, CI: 23.7-42.5). Urban population showed the highest prevalence of mild to moderate periodontitis 22.7% (CI: 17.3-28.5). Females had lower prevalence (34.4%) of the periodontitis than males (42.2%). The methodological heterogeneity of included studies was low.
Conclusion
Half of Indian adults suffer from some form of periodontal disease. There is need to adopt uniform and accurate measurement tools for recording periodontal condition.
Keywords: Pooled prevalence, Periodontitis, Gingivitis, India
Abbreviations: CPI, Community Periodontal Index; CPITN, Community Periodontal Index of Treatment Needs; LOA, Loss of Attachment; SMD, Standard Mean Deviations; MD, Mean Deviation; AM, Abhishek Mehta; RV, Ramanarayanan Venkitachalam; CJ, Chandrashekar Janakiram
1. Introduction
Chronic diseases globally have exhibited a steady rise, sparing no region or socioeconomic class. Periodontal disease, a component of this rising global burden essentially shares similar risk factors with other chronic diseases.1 However, unlike these, periodontal health seldom garners any attention. Quantifying periodontal disease in a meaningful manner, hence, is critical to its prioritization.
The National Oral Health Survey of India (2002), provides a comprehensive national data on periodontal disease prevalence.2 However, India has not seen an annual or five-yearly conduct of oral health survey for active monitoring of the disease burden. Additionally, unlike dental caries, periodontal epidemiological methods have been inconsistent.3 This inconsistency stems from changing case definitions and variations in measurement tools, probing locations, extent of oral cavity examined, and type of probes used by oral epidemiologists.4 So also, the surveillance of periodontal disease on regular intervals is not feasible due to chronic nature of disease and high cost of survey. The aggregate of these factors is responsible for the lack of adequate data and thereby lack of priority for oral health action.5
Several prevalence studies6, 7, 8, 9, 10, 11 undertaken in India have estimated region wise specific burden of periodontal disease, however, none of them individually account for nationally representative sample. Previously published systematic reviews3,12,13 have failed to report the pooled estimates of the periodontal diseases prevalence. Hence, this systematic review was designed to generate nationally representative data on the burden of periodontal disease among the adult population in India from previously published point prevalence studies.
2. Materials and methods
This systematic review was conducted adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)14 statement. Search method to identify relevant studies using focus question is as follows:
Population: Adults > 18 years.
Intervention = Not applicable.
Determinant: Prevalence.
Outcomes: Periodontal disease.
2.1. Focused question
What is prevalence of periodontal diseases (gingivitis and periodontitis) among the adult population of India?
2.2. Eligibility criteria
This systematic review was limited to cross-sectional studies. Included studies assessed the prevalence and severity of periodontal disease among participants aged over 18 years using the Community Periodontal Index of Treatment Needs (CPITN) or Community Periodontal Index (CPI).
2.3. Definition of disease
In this systematic review, the term “periodontal diseases” includes both gingivitis (gingival inflammation) as well as periodontitis (loss of periodontal attachment). For assessing prevalence of gingivitis we considered CPI/CPITN code of 1 and 2 and for periodontitis it was code 3 and 4. Periodontitis were further classified into mild to moderate (CPI code 3) and severe category (CPI code 4 or presence of loss of attachment). This classification of severe periodontal disease was used previously by Kassebaum et al.1
2.4. Information sources and search
An electronic search was performed with the databases PubMed/MedLine, PubMed Central, Scopus, Complimentary index, Ebscohost, SciELO, Open DOAR, TRIP, Science Citation Index,and Web of Science. We employed a platform-specific search strategy consisting of combinations of controlled terms (MeSH) and text words. The following search strategy was used; MeSH terms: “periodont∗"[All Fields] AND “prevalence"[All Fields] AND “India"[All Fields] and key words such as Community Periodontal Index of Treatment Needs (CPITN) or Community Periodontal Index (CPI) with no language restrictions. Additionally, the bibliographies of retrieved articles were reviewed. The studies published from January 1, 1982 to December 2018 among adult populations were selected. We limited our search from 1982 onwards because that year WHO adopted CPITN index with minor modifications. This final index was then used for recording periodontitis in human populations worldwide. Two authors (AM and CJ) independently eliminated any duplicate from the gathered results and examined the remaining articles by title and abstract. Any disagreement was adjudicated with a third reviewer (RV). Subsequently, the full texts were obtained and analysed for further inclusion/exclusion. Studies that did not meet the inclusion criteria were excluded. Full-text of articles identified from title and abstract screenings were reviewed thereafter.
The review protocol was registered in PROSPERO data with reference number CRD42018098531.
2.5. Data collection process and data items
A Microsoft Excel spreadsheet was used to classify included studies based on year of publication, language, demographic characteristics of participants, authors, place of the study, sample size and sampling technique used, sample size in terms of gender, age range of the studied population, overall age and gender wise prevalence and severity of periodontitis by two reviewers (AM and CJ). The weighted proportion difference was calculated for the outcomes (measured by different scales/indices) of each study. Based on the level of heterogeneity, fixed or random-effects model were used to calculate a pooled estimate of periodontitis and its 95% confidence intervals (CIs).
2.6. Quality assessment
All included studies were assessed independently and in duplicate by two review authors (AM and CJ) for study design characteristics and features of internal validity. A quality assessment instrument was developed to assess the quality of the eligible studies. Each study was assessed in the following domains; study settings, sampling strategy, measurement tools, analysis method and generalizability of findings. The sum of the points awarded to each question was divided by the highest possible score (8) to generate a fraction (between 0 and 1). The overall quality of each study was then assessed by ranking the studies. A score of 0–0.3, 0.4–0.6, and 0.7–1.0 was considered as low, moderate, and high quality respectively (Table 1). Review authors were not blinded to author information and source institution. Any disagreement was resolved by discussion or by third party adjudication.
Table 1.
Characteristics of Included studies.
| First Author | Place of study | Division | Year | Target population | Total Sample size | Index used to measure Periodontal Disease | Age group (years) | QA score |
|---|---|---|---|---|---|---|---|---|
| Mehta K8 | Uttar Pradesh | North | 1987 | Unspecified | 885 | CPITN | 30–35 | 0.6 |
| Anil S15 | Kerala | South | 1990 | Unspecified | 1942 | CPITN | 25–44 | 0.7 |
| Rao S16 | Uttar Pradesh | North | 1993 | Rural | 273 | CPITN | 35-44 &65-74 | 0.8 |
| Jagadeeshan17 | Pondicherry | South | 2000 | Rural | 736 | CPITN | 20 > | 0.7 |
| Madden IM18 | AndhraPradesh | South | 2000 | Unspecified | 133 | CPITN | 25 > | 0.5 |
| Singh GP19 | Punjab | North | 2005 | Unspecified | 1000 | CPITN | 18 > | 0.7 |
| Kumar TS20 | Rajasthan | West | 2009 | Tribal | 1590 | CPITN | 18–54 | 0.8 |
| Singh T21 | Karnataka | South | 2009 | Unspecified | 1564 | CPITN | 20–29 | 0.5 |
| Mehta R22 | West Bengal | East | 2010 | Unspecified | 18594 | CPITN | 20 > | 0.5 |
| Kumar A23 | Haryana | North | 2010 | Rural | 1152 | CPITN | 20–74 | 1 |
| Kundu D9 | West Bengal | East | 2011 | Unspecified | 18418 | CPITN | 20 > | 0.7 |
| Singh A24 | Uttar Pradesh | North | 2012 | Rural | 1026 | CPITN | 35 > | 0.6 |
| Grewal Y25 | Punjab | North | 2014 | Rural | 340 | CPITN | 18–74 | 0.6 |
| Goswami D10 | Assam | East | 2014 | Rural | 372 | CPITN | 20 > | 0.8 |
| Jaykrishnan R26 | Kerala | South | 2005 | Unspecified | 504 | CPITN | 30–50 | 1 |
| Nethravathi N6 | Karnataka | South | 2015 | Unspecified | 1500 | CPITN | 15–74 | 0.5 |
| Kumar V27 | Uttar Pradesh | North | 2015 | Unspecified | 1280 | CPITN | 20 > | 0.8 |
| Maurya R28 | Jammu & Kashmir | North | 2015 | Unspecified | 810 | CPITN | 18–50 | 0.5 |
| Sekhon T29 | Karnataka | South | 2015 | Rural | 1564 | CPITN | 20 > | 0.8 |
| Khiste S30 | Maharashtra | Central | 2017 | Rural | 384 | CPITN | 18 > | 0.8 |
| Bali RK2 | India | North, South, East, West, Central | 2002 | Unspecified | 33296 | CPI | 35-44 &65-74 | 1 |
| Kadanakuppe S31 | Karnataka | South | 2013 | Tribal | 1886 | CPI | 18–74 | 0.8 |
| Philips B32 | Tamil Nadu | South | 2013 | Tribal | 303 | CPI | 35–44 | 0.7 |
| Srivastava R33 | Delhi | North | 2013 | Unspecified | 448 | CPI | 60 & above | 1 |
| Batra M7 | Uttar Pradesh | North | 2014 | Unspecified | 550 | CPI | 20–49 | 0.8 |
| Handa S34 | Haryana | North | 2016 | Urban | 324 | CPI | 35-44 &65-74 | 1 |
| Ramojirao MV35 | Andhra Pradesh | South | 2016 | Rural | 231 | CPI | 35 > | 0.7 |
| Shah N36 | Haryana | North | 2017 | Rural | 408 | CPI | 35-44 &65-74 | 1 |
| Valsan I37 | Kerala | South | 2016 | Tribal | 420 | CPI | 35-44 &65-74 | 1 |
| Shrivastav38 | Madhya Pradesh | Central | 2018 | Tribal | 286 | CPI | 25 > | 1 |
2.7. Synthesis of findings
The decision to pool studies was based on the absence of significant methodological heterogeneity in terms of patient demographic characteristics, measures used to assess periodontal disease and the quality of the studies.We performed an evaluation of the heterogeneity of the data using the Q statistic, a chi-square test, at a threshold p-value of less than 0.10.39 The consistency was assessed visually using by the I2 statistic.40 An I2 value above 75% was indicative of high heterogeneity. The I2 statistic describes the proportion of variation in point estimates attributable to heterogeneity rather than sampling error. Subgroup analyses were performed for age, gender, place of the study and quality of the studies variables.
Meta-analysis was performed using Meta XL software developed for use with Microsoft Excel. Meta-analysis was undertaken using a random-effects model. Pooled prevalence was calculated with 95% Confidence Interval (CI) based on the total sample size and number affected. Subgroup analysis was done with respect to gender (males and females), age group (<35 years, 35–65 years, > 65 years), population sub-group (tribal, rural, urban and general), study quality (moderate and high), region (North, East, West, South and Central India) and the index used (CPI and CPITN). The chi-square test (using OpenEpi software) was applied to assess the relationship between gender and prevalence of periodontal disease.
3. Results
3.1. Study selection
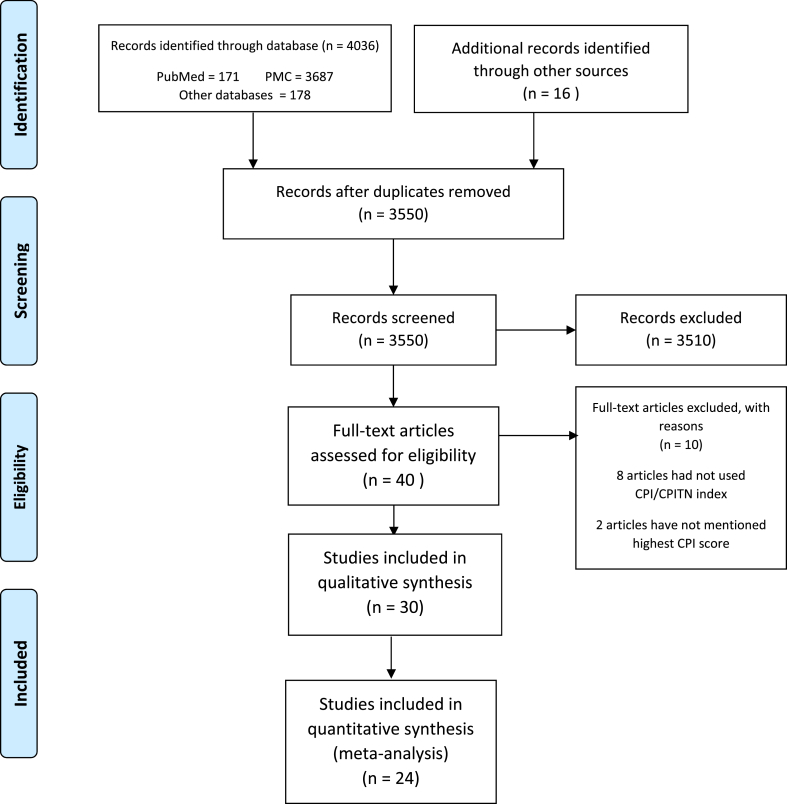
Electronic searches from all sources retrieved 4052 citations (Fig. 1). After removal of duplicates, 3550 records were left for screening. Title and abstracts were screened to yield 40 studies (3510 citations were excluded). Of these 40 studies, 10 did not meet the inclusion criteria [missing values of outcome (CPI scores) (2), variation in index used periodontal assessment viz.did not use either CPI or CPITN (8)].
Fig. 1.
Search strategy.
3.2. Study description
Selected characteristics of the included studies are summarized in Table 1. Thirty studies were included for the systematic review, of which 24 studies comprising 68,140 adults were included for the meta-analysis. Six studies8,21, 22, 25, 28, 31 were excluded from meta-analysis for having used convenience sampling for selection of study participants. The pooled estimate of gingivitis, and periodontal disease was estimated from 21 studies (66,368 participants), and 24 studies (68,140 participants) respectively (Table 2). Ten studies assessed periodontal disease using CPI index, while 20 studies by CPITN. Only three studies were conducted before the year 2000. The target population was unspecified in 14 studies which may be tribal, urban or rural areas of the settings, while 10 studies assessed the prevalence from rural population. Nearly 74% (n = 22) of studies scored high for methodological parameters based on quality assessment.
Table 2.
Pooled Prevalence of periodontal diseases.
| Events | Variables | No. of studies | Total Sample (N) | No. participants with events (n) | Pooled Prevalence (%) | 95% Confidence Intervals |
||
|---|---|---|---|---|---|---|---|---|
| Lower limit | Upper Limit | |||||||
| Gingivitis | Male | 8 | 30858 | 23003 | 75.0 | 74.6 | 75.5 | |
| Female | 8 | 27861 | 21289 | 77.3 | 76.8 | 77.7 | ||
| <35 years | 13 | 18364 | 13860 | 52.9 | 36.4 | 69.1 | ||
| 35–65 years | 19 | 28971 | 18161 | 39.4 | 29.0 | 50.4 | ||
| >65 years | 14 | 16705 | 7390 | 32.9 | 24.6 | 41.9 | ||
| Tribal | 4 | 2599 | 1268 | 46.5 | 26.0 | 67.6 | ||
| Rural | 11 | 6387 | 2539 | 44.6 | 28.6 | 61.1 | ||
| Urban | 1 | 216 | 138 | 63.9 | 57.4 | 70.2 | ||
| Unspecified | 7 | 57490 | 37103 | 51.9 | 38.9 | 64.8 | ||
| Total | 21 | 66368 | 40843 | 46.6 | 37.8 | 55.5 | ||
| Periodontal disease | Male | 9 | 31030 | 13202 | 42.2 | 20.3 | 65.8 | |
| Female | 9 | 28045 | 11586 | 34.4 | 12.4 | 60.2 | ||
| <35 years | 13 | 18364 | 3600 | 34.5 | 21.4 | 48.8 | ||
| 35–65 years | 19 | 28971 | 11319 | 57.4 | 47.3 | 67.2 | ||
| >65 years | 15 | 17153 | 9047 | 63.6 | 51.3 | 75.1 | ||
| Tribal | 4 | 2599 | 1115 | 47.2 | 29.0 | 65.7 | ||
| Rural | 11 | 6387 | 3361 | 48.9 | 32.9 | 65.1 | ||
| Urban | 1 | 216 | 113 | 36.2 | 9.4 | 67.8 | ||
| Unspecified | 9 | 58938 | 20831 | 44.8 | 33.6 | 56.2 | ||
| Total | 24 | 68140 | 25539 | 51.0 | 41.9 | 60.1 | ||
3.3. Synthesis of results
Overall, the prevalence of periodontal disease was 51.0% (CI: 41.9–60.1, 24 studies, 68,140 participants). The pooled prevalence of gingivitis was 46.6% (CI: 37.8–55.5, 21 studies, 66,368 participants) and periodontitis was 51% (Table 2). Males had a higher proportion (42.2%) of periodontitis than females (34.4%). Compared to other age groups, participants aged 65 years and above had higher prevalence (63.6%, CI: 51.3–75.1, 15 studies) of periodontitis, while participants age below 35 years had higher proportion of gingivitis (52.9%, CI: 36.4–69.1, 13 studies). Urban population had higher burden of the gingivitis (63.9%, CI: 57.4–70.2), while periodontal disease was more common among rural participants (48.9%, CI: 32.9–65.1, 19 studies).
3.4. Subgroup analysis
The subgroup analysis of the pooled estimate of prevalence of periodontitis according to its severity is described in Table 3. Nearly 25% of the sample size had prevalence of mild to moderate periodontitis (26.2%, CI: 21.1–31.6, 24 studies), while severe type was only 19.0% (CI: 14.3–24.2, 24 studies). When severity of periodontitis was stratified by age, sex and type of population, males had higher proportion of (19.3%, CI: 11.3–28.8, 9 studies) severe periodontitis than females (14.4%). Persons aged between 35 and 65 years had high proportion (30.0%, CI: 24.7–35.5, 19 studies) of mild to moderate type of periodontitis compared to other age groups, while 65 and above years showed high prevalence of 32.7% (CI: 23.7–42.5, 15 studies) in the severe periodontitis category. Urban population showed higher prevalence estimates for severe periodontitis compared to rural population (Table 2).
Table 3.
Subgroup analysis - Pooled prevalence of periodontal diseases.
| Events | No. of studies | Total Sample (N) | No. participants with events (n) | Pooled Prevalence (%) | 95% Confidence Intervals |
|||
|---|---|---|---|---|---|---|---|---|
| Lower limit | Upper Limit | |||||||
| Severity of Periodontitis | ||||||||
| Mild to Moderate periodontitis | Female | 9 | 28045 | 8111 | 16.7 | 4.2 | 34.4 | |
| Male | 9 | 31030 | 9192 | 17.8 | 5.8 | 33.8 | ||
| <35 years | 13 | 18364 | 2511 | 23.3 | 15.5 | 32.2 | ||
| 35–65 years | 19 | 28971 | 7787 | 30.0 | 24.7 | 35.5 | ||
| >65 years | 15 | 17153 | 5435 | 24.5 | 18.5 | 31.0 | ||
| Tribal | 4 | 2599 | 722 | 20.9 | 10.5 | 33.5 | ||
| Rural | 11 | 6387 | 1952 | 27.8 | 19.7 | 36.7 | ||
| Urban | 1 | 216 | 49 | 22.7 | 17.3 | 28.5 | ||
| Unspecified | 9 | 58938 | 13832 | 26.6 | 18.2 | 36.0 | ||
| Total | 24 | 68140 | 16557 | 26.2 | 21.1 | 31.6 | ||
| Severe periodontitis | Female | 9 | 28045 | 3475 | 14.4 | 7.1 | 23.6 | |
| Male | 9 | 31030 | 4011 | 19.3 | 11.3 | 28.8 | ||
| <35 years | 13 | 18364 | 1090 | 8.5 | 3.8 | 14.8 | ||
| 35–65 years | 19 | 28971 | 3532 | 21.4 | 14.5 | 29.2 | ||
| >65 years | 15 | 17153 | 3612 | 32.7 | 23.7 | 42.5 | ||
| Tribal | 4 | 2599 | 393 | 21.9 | 0 | 58.3 | ||
| Rural | 11 | 6387 | 1410 | 17.4 | 7.6 | 29.9 | ||
| Urban | 1 | 216 | 64 | 29.6 | 23.7 | 35.9 | ||
| Unspecified | 9 | 58938 | 6999 | 20.0 | 13.9 | 26.8 | ||
| Total | 24 | 68140 | 8867 | 19.0 | 14.3 | 24.2 | ||
| Quality of studies | ||||||||
| Gingivitis | High | 18 | 63709 | 39919 | 48.3 | 39.4 | 57.3 | |
| Moderate | 3 | 2659 | 925 | 35 | 3.9 | 74.1 | ||
| Mild to Moderate periodontitis | High | 21 | 65481 | 15860 | 26.4 | 20.9 | 32.3 | |
| Moderate | 3 | 2659 | 697 | 2.2 | 0 | 4.1 | ||
| Severe periodontitis | High | 21 | 65481 | 7859 | 17 | 12.7 | 21.8 | |
| Moderate | 3 | 2659 | 1008 | 1.6 | 0 | 5.3 | ||
| Measures of periodontal disease | ||||||||
| Gingivitis | CPI | 7 | 35494 | 20344 | 47.1 | 33.7 | 60.7 | |
| CPITN | 14 | 30874 | 20499 | 46.3 | 31.4 | 61.5 | ||
| Mild to Moderate periodontitis | CPI | 9 | 36266 | 10620 | 26.9 | 21.7 | 32.4 | |
| CPITN | 15 | 31874 | 5935 | 25.6 | 18.2 | 33.7 | ||
| Severe periodontitis | CPI | 9 | 36266 | 5257 | 24.2 | 12.5 | 38.1 | |
| CPITN | 15 | 31874 | 3609 | 15.7 | 9.1 | 23.5 | ||
Among the studies assessing periodontitis by CPI and CPITN, the prevalence of the mild to moderate periodontitis was very close to overall pooled estimate (Table 3). However, studies that used CPI only, overestimated pooled proportion by 5.2% compared to overall estimate of severe periodontitis. In contrast, the studies that used CPITN, underestimated the prevalence by 3.3% from overall estimate.
Table 4 describes the prevalence of the periodontitis according the region of the studies in India. Except for studies conducted in Eastern India, other regions of India do not show substantial variation in the severe or mild to moderate type of periodontitis.
Table 4.
Pooled estimates of periodontal disease according to various geographic divisions of India.
| Events | Region | No. of studies | Total Sample (N) | No. participants with events (n) | Pooled Prevalence (%) | 95% Confidence Intervals |
|
|---|---|---|---|---|---|---|---|
| Lower limit | Upper Limit | ||||||
| Gingivitis | North | 8 | 13780 | 6199 | 42.7 | 28.5 | 57.5 |
| East | 3 | 22947 | 18446 | 74.3 | 68.2 | 80.0 | |
| West | 2 | 5225 | 2241 | 44.7 | 35.0 | 54.6 | |
| South | 10 | 19130 | 10907 | 49.6 | 38.1 | 61.0 | |
| Central | 3 | 5610 | 3225 | 38.0 | 11.9 | 67.9 | |
| Moderate periodontitis | North | 10 | 15228 | 3536 | 22.7 | 22.1 | 23.4 |
| East | 3 | 22947 | 3433 | 24.8 | 8.9 | 44.8 | |
| West | 2 | 5225 | 1482 | 28.3 | 27.1 | 29.5 | |
| South | 10 | 19130 | 5935 | 28.3 | 22.9 | 34.1 | |
| Central | 3 | 5610 | 2170 | 29.0 | 16.9 | 42.8 | |
| Severe periodontitis | North | 10 | 15228 | 2607 | 15.6 | 15.0 | 16.2 |
| East | 3 | 22947 | 1310 | 5.5 | 03.2 | 8.3 | |
| West | 2 | 5225 | 206 | 4.0 | 3.4 | 4.5 | |
| South | 10 | 19130 | 3525 | 18.6 | 12.9 | 25.2 | |
| Central | 3 | 5610 | 1219 | 26.7 | 8.5 | 49.7 | |
4. Discussion
Periodontal disease is one of the two most important oral diseases contributing to the global burden of chronic disease, thereby qualifying as a major global public health problem. Estimation of the burden of periodontal disease in India has been challenging due to lack of technical expertise, low priority for oral health care, and high economic cost.5 The assumption that periodontal disease is an age-related condition compounded by a poor understanding of its natural history and wide variations in its measurement especially in community settings explains the limited number of studies undertaken to estimate prevalence of periodontal diseases. The National Oral Health Survey 2002, remains India’s solitary National Survey using the WHO methodology,2 estimating the burden of periodontal disease. For reasons unknown, there has been no further nationally representative data on periodontal disease in India. Nevertheless, coinciding with growth of large number of dental teaching institutions in 1990s, an increasing number of point prevalence studies estimating the periodontal disease in India have been reported in literature. A systematic review of these studies is essential in estimating the burden of periodontal disease in India. Previous reviews have had methodological issues like being narrative12 or performing qualitative analysis only,13 and none attempted to provide the estimate of the prevalence of periodontal disease in India. This systematic review provides pooled estimate of periodontal diseases (gingivitis, types of periodontitis) by metanalysis technique.
The overall prevalence of the periodontal disease in India from the included 24 studies involving 68,140 adults was 51.0% (95% CI:41.9–60.1). These figures translate into the estimate that nearly one in two Indian adults or 320 million people have some form of periodontal disease. This estimate is similar to the prevalence of periodontal disease (47.2%) in American adults.41 However, methodological quality is rather different among prevalence estimates of American and Indian studies. The methodological assessment of periodontal disease estimates is superior among American studies that have used regular NHANES data as opposed to Indian estimates from heterogenous studies.
The changes in measurement methodologies has enhanced the understanding of the relationship between plaque, gingivitis and periodontitis. The CPITN index was developed to facilitate performance of population-based surveys under a variety of conditions. The CPITN index was endorsed by WHO42 and has been adopted in many epidemiological studies. We used the CPI score of 3 as mild to moderate periodontitis which corresponds to 4–5 mm clinical loss of attachment. CPI score of 4, CPITN score of 2 and 3,4 of loss attachment index were grouped to be classified as severe type of periodontitis which signifies loss of attachment of more than 5 mm. This variation in indices may have overestimated the severe type of periodontitis in this review which could be considered as a potential limitation of this review.
The included studies in this review used either CPI or CPITN indices, so estimates of periodontal disease by either of the indices were different from when the indices were pooled together thereby suggesting variations in interval estimates. Even though the included studies scored high for quality assessment, but due to random effect variations, the present estimate may not be precise. When compared with this review findings, studies in other countries43 showed wide variation in estimates while employing CPI scores of 3 or 4. The proportion of CPI score of 3 ranged from 57% (Hong Kong) to 8% (Saudi Arabia). For a CPI score of 4, the percentages ranged from 28% (Nepal) to more than 5% (Sri Lanka, Syria and New Zealand). Similar results were obtained in Africa, a CPI score of 3 was frequent and a CPI score of 4 was more infrequent.44 The prevalence of a CPI score of 3 was reported to be more than 50% in studies originating from Kenya, Morocco, South Africa and Tanzania, and <5% in studies from Zimbabwe and Zaire. The prevalence of a CPI score of 4 was reported to be >30% in studies from Libya, Mauritius, Nigeria, Sierra Leone and South Africa.44
Nearly 25% participants had prevalence of periodontitis of mild to moderate type (26.2%, CI: 21.1-31.6), while severe type was only 19% (CI: 14.3-24.2). The current estimate of severe type of periodontitis is higher than recent Global Burden of Disease Study (GBD, 1990–2010)1 of severe periodontitis with prevalence of 11.2% and around 743 million people affected worldwide. The global prevalence of generalized, severe periodontitis among adults, ranged from 5 to 15% regardless of geographical and measuring tool considerations.
The overall prevalence of periodontitis was highest in older age group adults. Such burden of periodontitis will continue to increase with the growing ageing population of India, associated with increased tooth retention and possible lack of importance afforded to geriatric dental care; a common phenomenon globally.1,45,46 Gingival bleeding is an early sign of periodontitis and a leading risk marker for existing periodontal inflammation that accounts for the onset and progression of periodontitis. This review reports the prevalence of gingivitis to be around 47%. This figure is indicative of the population being at risk for periodontal disease and its burden may be more than 51% of the Indian population. The prevalence of periodontal disease derived in this review can be regarded as valid representation of the Indian population. However, due to lack of prevalence studies prior to 2000 in literature, a trend analysis could not be performed. Future prevalence studies in India should be based on full mouth measurement of pocket depth and attachment loss rather than being index based.
4.1. Strengths and limitations
There has been a reduction in the use of CPITN ⁄ CPI in epidemiological studies47 in other parts world, a gradual increase in use of standard measurements of pocket depth and attachment loss have been employed. This has necessitated changes in instrumentation, i.e. the type of probe used and accompanying measurement procedures. These modifications have also promoted changes in the definition of periodontitis for population-based studies. The measurement of pocket depth and attachment loss is now considered as appropriate scoring system rather than index based.4 The magnitude of under-estimation of prevalence may depend on variation in partial mouth scoring system and the type of measure being assessed, which is affected by the true population prevalence. Predominantly the studies in India have either used CPI or CPITN, so estimates may not be true population prevalence as compared to measurement of pocket depth and attachment loss scoring system. In its recent modifications in Oral Health Survey Basic methods (2013), WHO also recommends full mouth CPI and Loss of Attachment index rather index tooth or partial mouth recording system. Also, further variations of periodontal diseases like aggressive periodontitis were not considered for this review due to lack of epidemiological studies assessing the same.
Our estimates are reasonable to assume representativeness for two reasons, one the included studies were from 13 (geographical) out of 30 Indian states and one nationally representative data and second, the number of participants included in this review is large which reflects the precise estimate of prevalence of periodontal disease. From the available literature, this review estimate is the only available data for prevalence of the periodontal disease in India.
5. Conclusion
Periodontal diseases encompass both reversible (gingivitis) as well as irreversible (periodontitis) changes in soft tissues surrounding and supporting the tooth. These diseases are pandemic and are considered a major public health problem. As India lacks continuous surveillance of oral diseases, pooling data from various prevalence studiesis the only option to assess the burden of oral diseases in our population. Evidence from the current pooled analysis of prevalence studies shows a very high burden of periodontal diseases among Indian adults. Oral health policy makers and public health personnel can utilize data from this review to draft measures required for reducing the burden of periodontal disease in Indian population.
Ethics statement
The current study was determined exempt from review by the Faculty of Dentistry, Jamia Millia Islamia Institutional Review Board. The authors do not have any financial or other competing interests to declare.
Author contribution
A Mehta contributed to the design of the review, data acquisition, data interpretation and analysis and drafted the manuscript. C Janakiram contributed to the design of the review, data interpretation and analysis and drafted the manuscript; R Venkitachalam contributed to the statistical analysis anddrafted the manuscript. All authors gave final approval and agree to be accountable to all aspects of the work.
Acknowledgements
The authors wish to thank Dr. Vinita Sanjeevan (Department of Public Health Dentistry, Government Dental College, Goa) for her valuable inputs in preparation of this article.
Contributor Information
Chandrashekar Janakiram, Email: sekarcandra@gmail.com.
Abhishek Mehta, Email: amehta@jmi.ac.in.
Ramanarayanan Venkitachalam, Email: venkitr2006@gmail.com.
References
- 1.Kassebaum N.J., Bernabé E., Dahiya M., Bhandari B., Murray C.J.L., Marcenes W. Global burden of severe periodontitis in 1990-2010: a systematic review and meta-regression. J Dent Res. 2014;93(11):1045–1053. doi: 10.1177/0022034514552491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bali R.K., Mathur V.B., Talwar P.P., Channa H.B. Dental Council of India; New Delhi: 2002. National Oral Health Survey & Fluoride Mapping. [Google Scholar]
- 3.Irfan U.M., Dawson D.V., Bissada N.F. Epidemiology of periodontal disease: a review and clinical perspectives. J Int Acad Periodontol. 2001;3(1):14–21. [PubMed] [Google Scholar]
- 4.Dye B.A. Global periodontal disease epidemiology. Periodontol. 2000;58(1):10–25. doi: 10.1111/j.1600-0757.2011.00413.x. 2012. [DOI] [PubMed] [Google Scholar]
- 5.Janakiram C., Sanjeevan V., Rajeev B.R., Joseph J., Stauf N., Benzian H. Political priority of oral health in India: analysis of the reasons for neglect. J Publ Health Dent. 2018;78(2):144–153. doi: 10.1111/jphd.12254. [DOI] [PubMed] [Google Scholar]
- 6.Nethravathi T.D., Joshipura V., Venugopal S., Subbaiah S.K., Jagadeesh K.N., Apparaju V. A comparative assessment of periodontal status and treatment needs among population in Tumkur district using CPITN: an epidemiological study. J Adv Clin Res Insights. 2015;2:120–123. [Google Scholar]
- 7.Batra M., Gupta D., Tangade P. Assessment of periodontal health among the rural population of Moradabad, India. J Indian Assoc Public Health Dent. 2014;12(1):28–32. [Google Scholar]
- 8.Mehta K., Tewari A., Chawla H.S. Assessment of treatment needs of periodontal disease using CPITN in Uttar Pradesh population. J Indian Soc Pedod Prev Dent. 1987;5(1):1–9. [PubMed] [Google Scholar]
- 9.Kundu D., Mehta R., Rozra S. Periodontal status of a given population of West Bengal: an epidemiological study. J Indian Soc Periodontol. 2011;15(2):126–129. doi: 10.4103/0972-124X.84380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goswami D. Periodontal treatment needs of a rural population of North East India. Clarion. 2014;3(1):8–12. [Google Scholar]
- 11.Agarwal V., Tuli A., Khattak B., Singh A. Prevalence of chronic periodontitis in Meerut: a cross-sectional survey. J Indian Soc Periodontol. 2012;16(4):529–532. doi: 10.4103/0972-124X.106895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chandra A., Yadav O.P., Narula S., Dutta A. Epidemiology of periodontal diseases in Indian population since last decade. J Int Soc Prev Community Dent. 2016;6(2):91–96. doi: 10.4103/2231-0762.178741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shewale A.H. Prevalence of periodontal disease in the general population of India-A systematic review. J Clin Diagn Res. 2016;10(6):ZE04–ZE09. doi: 10.7860/JCDR/2016/17958.7962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7) doi: 10.1371/journal.pmed.1000097. Epub 2009 Jul 21. PMID: 19621072; PMCID: PMC2707599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anil S., Hari S., Vijayakumar T. Periodontal conditions of a selected population in Trivandrum district, Kerala, India. Community Dent Oral Epidemiol. 1990;18(6):325. doi: 10.1111/j.1600-0528.1990.tb00092.x. [DOI] [PubMed] [Google Scholar]
- 16.Rao S., Homagain S., Singh B.P. Periodontal status and treatment needs of an adult rural community. J Pierre Fauchard Acad (India) 1993;7(2):72–78. [PubMed] [Google Scholar]
- 17.Jagadessan M., Rotti S.B., Danabalan M. Oral health status and risk factors for dental and periodontal diseases among rural women in Pondicherry. Indian J Community Med. 2000;25(1):31–38. [Google Scholar]
- 18.Madden I.M., Stock C.A., Holt R.D., Bidinger P.D., Newman H.N. Oral health status and access to care in a rural area of India. J Int Acad Periodontol. 2000;2(4):110–114. [PubMed] [Google Scholar]
- 19.Singh G.P.I., Bindra J., Soni R.K., Sood M. Prevalence of periodontal diseases in urban and rural areas of Ludhiana, Punjab. Indian J Community Med. 2005;30(4):128–129. [Google Scholar]
- 20.Kumar T.S., Dagli J.R., Mathur A. Oral health status and practices of dentate Bhil adult tribes of southern Rajasthan, India. Int Dent J. 2009;59:133–140. [PubMed] [Google Scholar]
- 21.Singh T., Kothiwale S. Assessment of periodontal status and treatment needs in Karnataka, India. Internet J Epidemiol. 2009;9(1):9–12. [Google Scholar]
- 22.Mehta R., Kundu D., Chakrabarty S., Bharati P. Periodontal conditions and treatment in urban and rural population of West Bengal, India. Asian Pac J Trop Med. 2010;3(2):152–157. [Google Scholar]
- 23.Kumar A., Virdi M., Veeresha K., Bansal V. Oral health status & treatment needs of rural population of Ambala, Haryana, India. Internet J Epidemiol. 2010;8(2):1–7. [Google Scholar]
- 24.Singh A, Agarwal V, Tuli A, Khattak B., P Prevalence of chronic periodontitis in Meerut: a cross-sectional survey. J Indian Soc Periodontol. 2012;16(4):529–532. doi: 10.4103/0972-124X.106895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grewal Y., Datta R., Singh K., Singh G., Singh S., Kaur P. Prevalence of periodontal disease in the rural population of Punjab, India. J Pharmaceut Biomed Sci. 2014;4(6):532–535. [Google Scholar]
- 26.Jayakrishnan R., Sharma P.S., Thankappan K.R. Prevalence of periodontal disease among adults in Trivandrum district, Kerala, India. Malyasian Dent J. 2005;26(2):97–104. [Google Scholar]
- 27.Kumar V., Agarwal V., Khatri M., Singh G. Prevalence of periodontitis in rural and urban population. Indian J Community Health. 2015;27(3):366–371. [Google Scholar]
- 28.Maurya R., Kundu D., Singh H., Mishra H. Oral health status, dental caries experience & treatment needs of population of Jammu city. Int J Oral Health Dent. 2015;1(4):164–167. [Google Scholar]
- 29.Sekhon T.S., Grewal S., Gambhir R.S. Periodontal health status and treatment needs of the rural population of India: a cross-sectional study. J Nat Sci Biol Med. 2015;6(1):111–115. doi: 10.4103/0976-9668.149102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khiste S., Gupta B., Ramachandran N., Ranade N., Patrawala A., Shaikh S. Prevalence of periodontal disease in rural population of Raigad district of Maharashtra : a cross-sectional study. J Dent Specialities. 2017;224:119–121. [Google Scholar]
- 31.Kadanakuppe S., Bhat P.K. Oral health status and treatment needs of Iruligas at Ramanagara District, Karnataka, India. W Indian Med J. 2013;62(1):73–80. [PubMed] [Google Scholar]
- 32.Philip B., Chithresan K., Subramanian Vijayaragavan V., Maradi A. Prevalence of periodontal diseases among the adult tribal population in Nilgiris-an epidemiological study. Int J Public Health Dent. 2013;84(1):8–12. [Google Scholar]
- 33.Srivastava R., Gupta S.K., Mathur V.P., Goswami A., Nongkynrih B. Prevalence of dental caries and periodontal diseases, and their association with socio-demographic risk factors among older persons in Delhi, India: a community-based study. Southeast Asian J Trop Med Publ Health. 2013;44(3):523–533. [PubMed] [Google Scholar]
- 34.Handa S., Prasad S., Rajashekharappa C.B., Garg A., Ryana H.K., Khurana C. Oral health status of rural and urban population of Gurgaon block, Gurgaon district, using WHO assessment form through multistage sampling technique. J Clin Diagn Res. 2016;10:ZC43–ZC51. doi: 10.7860/JCDR/2016/19048.7756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramoji Rao M.V., Kumar Katari P., Vegi L., Teja Bypureddy T., Samyuktha Prabhakara Rao K., Siva Tejaswi K. Prevalence of periodontal diseases among rural population of Mustabad, Krishna District. J Int Soc Prev Community Dent. 2016;6(Suppl 1):S59–S63. doi: 10.4103/2231-0762.181169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shah N., Pandey R.M., Duggal R., Mathur V.P., Rajan K. Ministry of Health and Family Welfare, Govt. of India; New Delhi: 2007. Oral Health in India: A Report of the Multi Site Oral Health Survey to Directorate General of Health Services. [Google Scholar]
- 37.Valsan I., Joseph J., Janakiram C., Mohamed S. Oral health status and treatment needs of Paniya tribes in Kerala. J Clin Diagn Res. 2016;10(10):12–15. doi: 10.7860/JCDR/2016/21535.8631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shrivastav A., Maurya R., Shukla C. Oral hygiene and periodontal status in the primitive hidden tribe of Patalkot, a tribal area in Central India. J Indian Soc Periodontol. 2018;22(1):55–59. doi: 10.4103/jisp.jisp_153_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huedo-Medina T., Sanchez-Meca J., Marin-Martinez F., Botella J. 2006. Assessing Heterogeneity in Meta-Analysis: Q Statistic or I2 Index? CHIP Doc June.https://opencommons.uconn.edu/chip_docs/19 [DOI] [PubMed] [Google Scholar]
- 40.Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 41.Eke P.I., Dye B.A., Wei L., Thornton-Evans G.O., Genco R.J. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91(10):914–920. doi: 10.1177/0022034512457373. [DOI] [PubMed] [Google Scholar]
- 42.World Health Organization . third ed. World Health Organization; Geneva ;Albany NY: 1987. Oral Health Surveys : Basic Methods.http://www.worldcat.org/title/oral-health-surveys-basic-methods/oclc/17159438 [Google Scholar]
- 43.Corbet E.F., Zee K.-Y., Lo E.C.M. Periodontal diseases in Asia and Oceania. Periodontol. 2000;29:122–152. doi: 10.1034/j.1600-0757.2002.290107.x. 2002. [DOI] [PubMed] [Google Scholar]
- 44.Corbet E.F., Leung W.K. Epidemiology of periodontitis in the Asia and Oceania regions. Periodontol. 2000;56(1):25–64. doi: 10.1111/j.1600-0757.2010.00362.x. 2011. [DOI] [PubMed] [Google Scholar]
- 45.Tonetti M S, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: a call for global action. J Clin Periodontol. 2017;44(5):456–462. doi: 10.1111/jcpe.12732. [DOI] [PubMed] [Google Scholar]
- 46.Vos T., Alemu Abajobir A., Hassen Abate K. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990 - 2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baelum V., Papapanou P.N. CPITN and the epidemiology of periodontal disease. Community Dent Oral Epidemiol. 1996;24(6):367–368. doi: 10.1111/j.1600-0528.1996.tb00880.x. [DOI] [PubMed] [Google Scholar]