Abstract
Coronavirus disease 2019 (COVID-19) causes a spectrum of disease; some patients develop a severe proinflammatory state which can be associated with a unique coagulopathy and procoagulant endothelial phenotype. Initially, COVID-19 infection produces a prominent elevation of fibrinogen and D-dimer/fibrin(ogen) degradation products. This is associated with systemic hypercoagulability and frequent venous thromboembolic events. The degree of D-dimer elevation positively correlates with mortality in COVID-19 patients. COVID-19 also leads to arterial thrombotic events (including strokes and ischemic limbs) as well as microvascular thrombotic disorders (as frequently documented at autopsy in the pulmonary vascular beds). COVID-19 patients often have mild thrombocytopenia and appear to have increased platelet consumption, together with a corresponding increase in platelet production. Disseminated intravascular coagulopathy (DIC) and severe bleeding events are uncommon in COVID-19 patients. Here, we review the current state of knowledge of COVID-19 and hemostasis.
Keywords: COVID-19, Coagulopathy, D-dimer, Thrombocytopenia, Thrombosis
Introduction
The Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) that has swept the globe in 2019 and 2020 causes Coronavirus Disease 2019 (COVID-19), a predominantly respiratory illness with 11.5–13% mortality among hospitalized patients [1, 2, 3]. 80% of patients infected by SARS-CoV-2 may be asymptomatic or only mildly symptomatic, but around 10% develop severe respiratory symptoms that evolve to acute respiratory distress syndrome (ARDS) [4].
SARS-CoV-1 and SARS-CoV-2, the enveloped single-stranded RNA viruses responsible for the 2002–2004 SARS epidemic and the more recent COVID-19 pandemic, respectively, bind angiotensin-converting enzyme 2 (ACE2), an intrinsic membrane protein with enzymatic activity that physiologically counters the activation of the renin-angiotensin-aldosterone system. ACE2 is expressed broadly, including in lung alveolar pneumocytes, as well as endothelial cells, the heart, and the kidneys [5, 6]. SARS-CoV-2 has an at least 10-fold-greater affinity for human ACE2 than SARS-CoV-1 has [7].
SARS-CoV-2 causes lung inflammation which progresses to cytokine storm in the most severe cases. The lungs of patients with COVID-19 show extensive alveolar and interstitial inflammation [8]. COVID-19 causes a spectrum of disease, with frequent involvement of the hemostatic system [9, 10]. Severe pulmonary inflammation causes activation and damage of the pulmonary vasculature and may trigger pulmonary thrombosis early in the disease course [11]. There is a high incidence of venous thromboembolism (VTE) in hospitalized COVID-19 patients, particularly those with severe illness. The incidence of thrombotic complications is 16–69% in patients with COVID-19 admitted to intensive care [3, 10, 12, 13]; the incidence was highest in Llitjos et al. (69%) due to active ultrasound surveillance for deep-vein thrombosis (DVT). The incidence of venous and possibly arterial thrombosis remains high in COVID-19 patients despite administering standard thromboprophylaxis [3]. In one Italian COVID-19 study, the incidence of VTE (despite thromboprophylaxis) was 27.6% in the ICU and 6.6% in the general ward. The rate of ischemic stroke and acute coronary syndrome was 2.5 and 1.1%, respectively [14].
Hypercoagulability due to severe viral pneumonia is not novel. This increased VTE incidence in COVID-19 patients is similar to that seen in patients with other epidemic coronavirus pneumonias, including severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS-CoV) [15, 16]. H1N1 influenza carried an 18-fold increased risk of developing VTE when compared to critically ill patients with ARDS with no H1N1 influenza infection [17].
The SARS-CoV-2 virus does not appear to have intrinsic procoagulant effects itself; rather, the coagulopathy is most likely the result of the profound COVID-19 inflammatory response and endothelial activation/damage [18]. Recent COVID-19 autopsy reports demonstrate pulmonary endothelial viral inclusions and apoptosis, increased angiogenesis, and increased capillary microthrombi [19, 20].
Patients with COVID-19 pneumonia exhibit coagulation abnormalities, most commonly elevated levels of fibrinogen and D-dimer, often with mild thrombocytopenia [18, 21]. Elevated D-dimer has been associated with a higher mortality rate. A subset of COVID-19 patients can have abnormally short PT and aPTT [15]. The shortened aPTT is often related to elevated Factor VIII (FVIII) [22] as an acute-phase response. In more severely affected patients, a disseminated intravascular coagulopathy (DIC)-like state can develop with relatively mild prolongation of the PT and aPTT (while fibrinogen tends to remain normal/elevated) [18]. However, D-dimer levels are elevated far out of proportion to any abnormalities detected in the PT/INR, aPTT, fibrinogen level, or platelet count; these findings are unusual for DIC, as defined by the criteria of the International Society of Thrombosis and Hemostasis (ISTH) [23]. Unlike the pattern seen in classic DIC from bacterial sepsis or trauma, in COVID-19 prolongation of the aPTT and/or PT is minimal [24], thrombocytopenia is mild (a platelet count of 100–150 ×109/L), hypofibrinogenemia is rare, and laboratory results supporting hyperfibrinolysis are uncommon [25]. COVID-19-associated coagulopathy is the term used to describe this spectrum of coagulation changes. Three stages of COVID-19-associated coagulopathy have been proposed: stage 1 showing elevated D-dimer, stage 2 showing elevated D-dimer together with mildly prolonged PT/INR and aPTT and mild thrombocytopenia, and stage 3 with critical illness and laboratory studies progressing towards classic DIC [11].
Here, we will discuss what is known about COVID-19-associated changes in platelet count, activation states, and production; we will review the association of these platelet parameters with COVID-19 outcomes. Additionally, we will review the predominantly procoagulant changes seen in the coagulation system during COVID-19 infection and their association with COVID-19 mortality.
Platelets
Of the patients affected by the 2003 SARS epidemic, 20–55% had thrombocytopenia [26]. Subsequent rebound thrombocytosis was also reported [16, 27]. The patients who developed thrombocytopenia during the epidemic experienced greater morbidity/mortality [28]. MERS was also associated with thrombocytopenia [16].
Thrombocytopenia is detected in 5–41.7% of COVID-19 patients (the incidence varies according to disease severity) [1, 29, 30, 31], and it is typically mild (counts are generally 100–150 ×109/L). Mild thrombocytopenia has been detected in 58–95% of severe cases of COVID-19 [21, 30, 32]; on average, patients with severe disease have a platelet count only 23 ×109/L to 31 ×109/L lower than those with non-severe disease [33, 34]. The fact that such severely ill patients with systemic immune and coagulation activation maintain reasonable platelet counts implies a marked compensatory platelet production response. Severe thrombocytopenia is only rarely reported in COVID-19 patients, for instance, in association with an immune thrombocytopenic purpura-like state [35].
A meta-analysis of 7,613 COVID-19 patients revealed that patients with severe disease had a lower platelet count than those with non-severe disease. Additionally, the non-survivors had a much lower platelet count than the survivors [25, 36]. However, not all studies have found platelet counts to be a predictor of COVID-19 mortality [37]. Compared to patients with severe pneumonia but without COVID-19, those with COVID-19 disease actually had higher platelet counts, according to Yin et al. [38]. The pediatric COVID-19 syndrome of Kawasaki-like illness has been associated with a lower average platelet count than that seen in classical Kawasaki disease, although the platelet counts did not fall below the lower limit of normal [39].
Thrombocytopenia at admission in COVID-19 patients was associated with a 4.24-fold increased risk of inpatient mortality in a study from Wuhan [1]. Patients with thrombocytopenia (median 105 ×109/L) were more likely to be older, male, have a higher APACHE II score, lower absolute neutrophil and lymphocyte counts, higher C-reactive protein (CRP), and a lower PaO2/FiO2 ratio than those without thrombocytopenia (median 186 ×109/L). The hemoglobin and D-dimer levels did not differ in these two groups.
A temporal trend of dropping platelet counts in patients with COVID-19 could suggest a worsening thrombotic state [40]; lower nadir platelet counts are associated with increased mortality. In Yang et al. [31], compared to the reference group (i.e., a platelet count ≥150 ×109/L), nadir platelet counts of 100–150, 50–100, and 0–50 ×109/L had a relative risk for in-hospital mortality of 3.4 (95% confidence interval [CI] 2.4–5.0), 10.0 (95% CI 7.2–14.0), and 13.7 (95% CI 9.9–18.9), respectively. Conversely, improvement of thrombocytopenia in COVID-19 patients can signify imminent clinical improvement [1].
Viral infection can be associated with thrombocytopenia due to a variety of causes [41]. While hypoproliferative thrombocytopenia is observed at later stages of viral infection, the rapid development of thrombocytopenia in response to viral infections is generally mediated via enhanced platelet clearance/destruction [42]. Platelets can be activated by viral antigen-antibody complexes or host inflammatory responses; activated platelets are more readily cleared from the circulation by the reticuloendothelial system [42]. Viruses can also interact with megakaryocytes and reduce platelet synthesis [43].
Platelets play an important role in inflammatory signaling as well as in infectious response [44]. By combining thrombotic and immune recruitment functions, platelets may help focus hemostasis and immune responses against potential infectious agents to prevent microbial invasion [45]. Platelets interact directly with viruses via a variety of receptors [42], including Toll-like receptors [46, 47]. While platelets are capable of engulfing and aggregating pathogens, their microbial killing potential is limited [45]. Platelets and their released products have been variably reported to suppress viral infection and support virus persistence, depending on the particular infection [42]. Platelets also appear to play a role in recruiting and activating circulating leukocytes to the endothelial surface, leading to white blood cell diapedesis [48, 49]. The interactions between endothelial cells, platelets, and leukocytes play a critical role in the procoagulant effect of viral infections [16]. Thrombocytopenia, platelet secretion, and interactions with leukocytes may have either injurious or protective immune consequences in viral infections [47].
While platelets contribute to the basal barrier integrity of the alveolar capillaries, they may also contribute to lung injury in a variety of pulmonary disorders and syndromes [50]. Platelet-leukocyte aggregates [51, 52] and platelet-endothelial interactions [53] appear to play a role in the pathogenesis of acute lung injury in animal models due to physico/chemical damage and influenza infection, respectively. For example, in dengue fever, platelet-derived IL-1β causes increased endothelial permeability [54].
Several mechanisms of COVID-19-associated thrombocytopenia have been posited (Table 1). This could be purely consumptive, particularly related to endothelial damage and platelet aggregate formation in the lung, but marrow suppression and immune clearance are also possible contributors [29]. Thachil [32] suggests that platelets are being consumed to form pulmonary thrombi, with a possible anti-infective effect, to prevent viremic spread via the bloodstream. In preliminary data from our institution, McMullen et al. [American Journal of Clinical Pathology, in press] have shown there are significant intravascular platelet aggregates in COVID-19 autopsy lung specimens, located primarily in the interalveolar capillaries and smaller vessels; the degree of platelet deposition is not more than is seen in other fatal pulmonary infections, however. Of note, none of the COVID-19 patients assessed in their study were thrombocytopenic.
Table 1.
Possible mechanisms of COVID-19-associated thrombocytopenia (modified from [103])
| Platelet activation and subsequent clearance by reticuloendothelial system − Activation by increased thrombin generation and consumptive coagulopathy − Direct viral-platelet interaction activation −associated with formation of platelet-leukocyte aggregates − FcR-mediated interaction with immune complexes |
| Platelet clearance due to increased endothelial damage − Pulmonary vasculature-specific − Widespread damage |
| Platelet autoantibody formation, with subsequent platelet clearance |
| Splenic/hepatic sequestration Marrow/megakaryocyte suppression − Due to inflammatory response − Due to direct viral infection − Due to reduced thrombopoietin |
Liu et al. [1] showed that COVID-19 patients with thrombocytopenia had a statistically significantly larger mean platelet volume (MPV, median 10.3 fL) than COVID-19 patients with retained platelet counts (median 9.9 fL). Outside of congenital platelet disorders, an increased mean platelet volume implies an increase in circulating young platelets and is the body's response to thrombocytopenia [55]. In healthy adults with normal platelet counts, the normal MPV range is 9.0–12.4 fL [56]. Platelet size positively correlates with surface receptor number and platelet ATP content. The number of ribosomes is higher in large platelets and they incorporate more amino acids, suggesting a higher potential for protein synthesis [57]. Larger platelets have increased hemostatic potential, bind more fibrinogen, and have greater levels of phosphorylation after thrombin stimulation than smaller platelets [57].
In preliminary data, COVID-19 patients at our hospital were found to have significantly larger MPVs than critically ill non-COVID-19 patients matched for platelet count (11.6 vs. 10.5 fL) (Table 2). We compared MPV in 10 patient pairs matched for platelet count: 10 adult COVID-19-positive patients admitted to ICU (either the COVID-19 cohort ICU or the cardiac ICU) and 10 adult patients testing negative for SARS-CoV-2 and admitted to the surgical, medical, or neurological ICU.
Table 2.
Platelet parameters in COVID-19 patients
| COVID-19 patients |
Non-COVID-19 ICU patients |
Normal range | |||
|---|---|---|---|---|---|
| mean | SD | mean | SD | ||
| Platelet count, ×109/L |
(n = 10) 234.1 |
(n = 10) 151.1 |
(n = 10) 250.30 |
(n = 10) 152.7 |
150–450 |
| MPV, fL |
(n = 9) 11.58* |
(n = 9) 1.04 |
(n = 9) 10.49 |
(n = 9) 1.00 |
9.0–12.4 |
| median | range | median | range | ||
|---|---|---|---|---|---|
| IPF, ×109/L IPF, % |
(n = 3) 42.57 14.63 |
(n = 3) 12.2–99.5 4.2–25.0 |
(n = 2) 4.25 7.05 |
(n = 2) 3.3–5.2 6.4–7.7 |
1.25–7.02 3.3–8.6 |
N = 20, i.e., 10 pairs of patients matched for platelet count. * p = 0.013, paired Student's t test (compared to non-COVID-19 patients). MPV, mean platelet volume; IPF, immature platelet fraction.
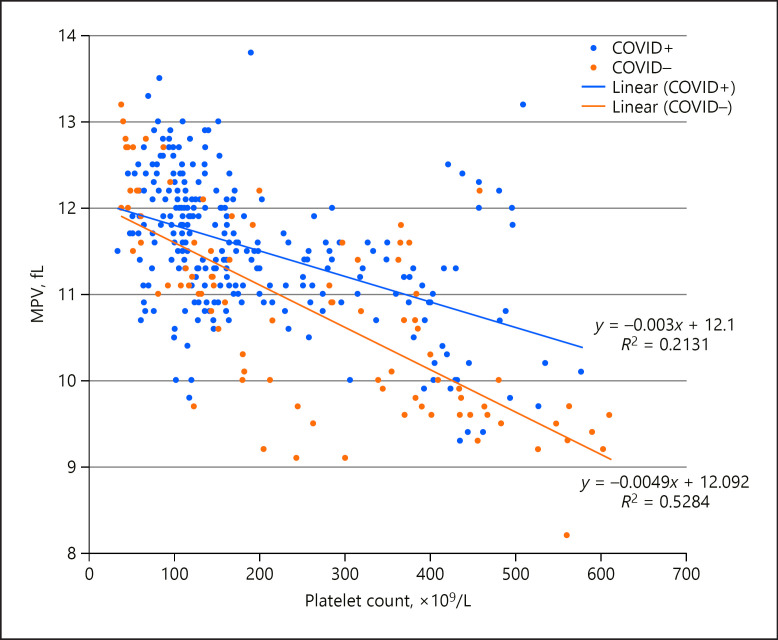
This trend for higher MPV in COVID-19 patients persisted in a larger dataset of hematologic values from the same 20 patients when no longer matched for platelet count (Student's t test p < 5 ×10−7) (Fig. 1). This trend towards greater MPV persists even in COVID-19 patients with normal platelet counts.
Fig. 1.
Relationship between platelet count and mean platelet volume (MPV) in a sample of ICU patients affected by COVID-19 (COVID+; n = 10, with 266 measurements) or not (COVID–; n = 10, with 91 measurements). These populations were significantly different from each other (Student's t test, p < 5 ×10−7).
Reticulated platelets are immature platelets with a high granule content, residual mRNA, and increased mean volume compared with older circulating platelets [58, 59, 60]. In healthy adults with normal platelet counts, the relative immature platelet fraction (IPF, also known as reticulated platelets) ranges from 3.3 to 8.6% [56]. Younger platelets show higher levels of activation in response to agonists (as assessed by P-selectin exposure), and thus more readily promote the formation of platelet aggregates [56]. The reticulated platelet count is positively associated with cardiovascular risk and mortality [58, 61].
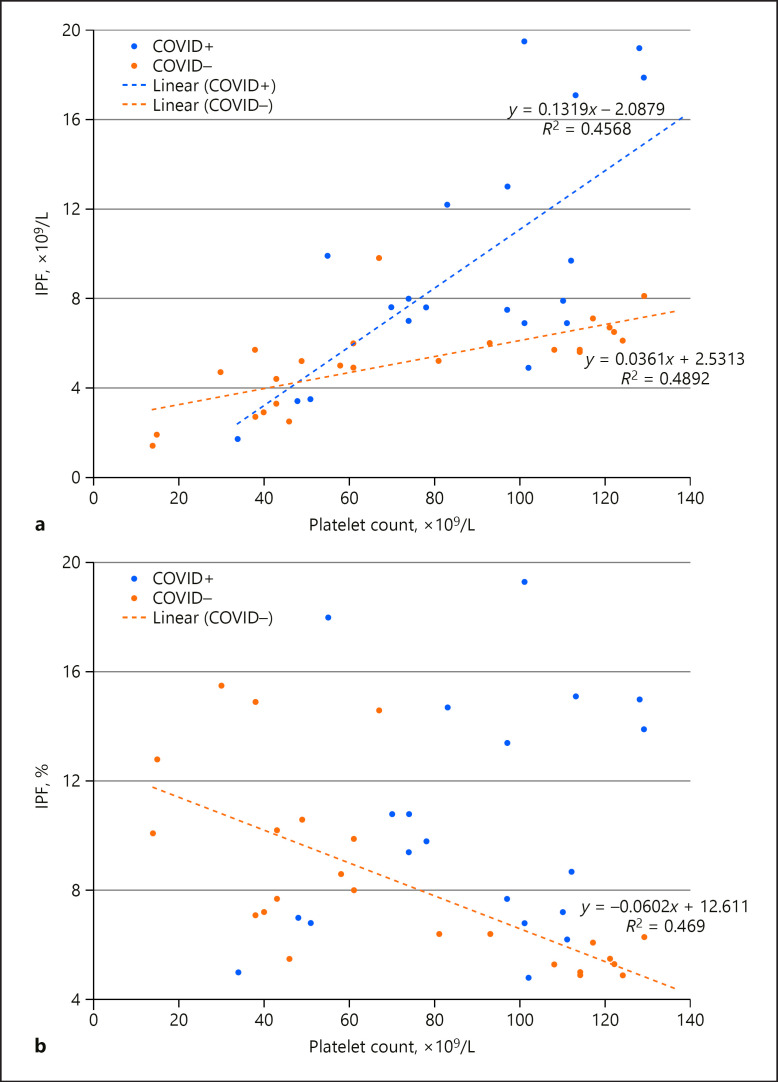
In our hospital, there is a significant trend of elevated IPF in COVID-19 patients (Fig. 2). We investigated four COVID-19-positive and four COVID-19-negative thrombocytopenic patients from our original dataset described above. COVID-19 positivity was highly predictive of an absolute IPF of 7.5 ×109/L or higher (Fig. 2a). In the non-COVID-19 patients, a relative IPF of ≥8% was restricted to those with platelet counts less than 70 ×109/L (Fig. 2b). In contrast, COVID-19-positive patients had relative IPF ≥8% at platelet counts up to 251 ×109/L (data not shown).
Fig. 2.
Relationship between platelet count and immature platelet fraction (IPF) in a sample of thrombocytopenic ICU patients affected by COVID-19 (COVID+; n = 4, with 23 measurements) or not (COVID–; n = 4, with 23 measurements). a Absolute IPF counts. These populations were significantly different from each other (Student's t test, p < 0.005). b Relative IPF counts. Of note, the relative IPF counts for COVID+ patients did not form a strong enough relationship with platelet count to display a relevant trendline. These populations were significantly different from each other (Student's t test, p < 0.05).
These findings suggest that COVID-19 is associated with the increased production of large immature platelets, as megakaryocytes respond to increased platelet consumption. Interestingly, COVID-19 is associated with increased numbers of immature platelets even at normal platelet counts. As immature platelets are known to be more functional [56, 58], this could be another mechanism for increased clotting events in COVID-19.
In keeping with these findings that COVID-19 patients have larger and less mature platelets (parameters associated with increased platelet reactivity), Ranucci et al. [62]showed that, upon admission to the ICU, a group of intubated COVID-19 patients with normal platelet counts had an increased platelet contribution to clot strength according to a viscoelastic analysis.
In addition to having increased numbers of immature platelets, COVID-19 patients may have increased levels of circulating activated platelets. Such activated platelets are normally only a small proportion of the total circulating population. Hille et al. [56] reported that reticulated (younger) and nonreticulated (older) platelets from healthy patients show a low percentage of P-selectin positivity in unstimulated samples (median in all groups <5%). Similarly, Handtke et al. [55] reported that small and large platelets have similar basal surface levels of P-selectin. Manne et al. [63] recently reported that circulating platelets from at least some of the COVID-19 patients they studied had a higher level of P-selectin detectable on their surface membranes than did normal controls. Although there was a considerable overlap of results between patients and normal donors, a statistically higher level of surface P-selectin was found in the patient group following in vitro exposure to low-concentration (2.5 µM) thrombin receptor-activating peptide (TRAP). At the higher stimulus intensity of 25 µM TRAP, a difference in response between patients and normal donors was no longer seen. The enhancement of platelet aggregation in the patients was similarly observed to be greater in response to lower concentrations than higher concentrations of several platelet agonists [63]. Zhang et al. [64] have very recently taken such analysis still further, reporting their detection of ACE2 expression by platelets, the direct stimulatory effects of SARS-CoV-2 or its Spike protein on platelets, and the ability of recombinant human ACE2 protein or anti-Spike monoclonal antibody to inhibit Spike protein-induced platelet activation. Hottz et al. [104]have further recently demonstrated increased platelet-monocyte interaction and associated tissue factor expression by monocytes in severe COVID-19 patients.
Antiplatelet Agents
A role for antiplatelet agents in COVID-19 disease has been considered, but there is no randomized evidence to support this treatment at this time. Particularly for those patients with mild thrombocytopenia, such treatment would carry a greater risk of bleeding [65].
Endothelium, von Willebrand Factor, and ABO Blood Group
COVID-19 pneumonia is associated with endothelial cell disruption, tissue factor expression, and activation of the coagulation cascade. These responses worsen oxygenation, and local hypoxia establishes a deleterious positive thromboinflammatory feedback loop [8]. Direct endothelial damage by the virus and/or endothelial activation by cytokines released during COVID-19 infection are possible mechanisms of thrombosis [66]. Activated or damaged endothelial cells release their Weibel-Palade bodies containing ultra-large molecular-weight multimers of von Willebrand factor (vWF). The ultra-large vWF multimers can spontaneously bind platelets and lead to microthrombosis if not trimmed by ADAMTS13.
vWF has previously been shown to play a role in the development of thrombocytopenia during viral infections. Intravenous administration of adenovirus (as used for gene therapy studies) is associated with platelet activation and acute thrombocytopenia. This cytopenia is not seen in adenovirus-treated vWF knock-out mice, however [67].
COVID-19 patients have significantly elevated vWF levels; mean vWF antigen has been reported to be 455–529% [10, 22]. Escher et al. [66, 68] reported elevated vWF antigen and function, together with increased FVIII clotting activity in COVID-19 patients, likely reflecting the combined effect of the greater release of Weibel-Palade bodies from endothelial cells and the acute-phase reaction that raises the FVIII level. ADAMTS13 activity is mild-to-moderately reduced in COVID-19 patients [68, 69, 70].
In a study from Yale New Haven hospital, markers of the activation of endothelial cells and platelets were significantly elevated in COVID-19 patients in the ICU compared to non-ICU patients (vWF antigen mean 565% [SD 199] vs. 278% [SD 133], p < 0.0001; soluble P-selectin mean 15.9 ng/mL [SD 4.8] vs. 11.2 ng/mL [3.1], p = 0.0014). Mortality was significantly correlated with vWF antigen (r = 0.38; p = 0.0022) and soluble thrombomodulin (r = 0.38; p = 0.0078) [71].
In a study on ABO blood group distribution in 2,173 COVID-19 patients by Zhao et al. [72], group A individuals were more likely to have symptomatic COVID-19 disease, while group O individuals were less likely to have it; this association is not universally identified, however. Latz et al. [73] did not show any correlation between ABO type and COVID-19-related intubation or death, but they did confirm that group O individuals were least likely to test positive for SARS-CoV-2. A genome-wide association study involving 1,980 patients in Europe showed the 9q34.2 locus (including the ABOglycosyltransferase gene) to be associated with severe COVID-19 with respiratory failure. This study also confirmed the higher risk in blood group A than in other blood groups (odds ratio [OR] 1.45; 95% CI 1.20–1.75) and a protective effect in blood group O versus the other blood groups (OR 0.65; 95% CI 0.53–0.79) [74]. These findings could be due to elevated vWF levels in non-group O individuals, which predispose to thromboembolic events, as has been well-described prior to the current pandemic [75].
An alternative explanation for this ABO-differentiated susceptibility could be the isohemagglutinin-mediated neutralization or clearance of the SARS-CoV-2 virus coated with A substance (as would be created by group A or AB individuals) [76]. Enveloped viruses (such as coronaviruses) are glycosylated, meaning that their envelope proteins are post-translationally modified by the addition of glycans. The interaction between SARS-CoV Spike protein and ACE2 can be specifically blocked by anti-A antibodies when the Spike protein is synthesized by cells that express group A substance [77]. Gallian et al. [78]showed a lower seroprevalence of antibodies neutralizing SARS-CoV-2 in group O donors, which they interpret as reflecting a lower rate of infection in these individuals, likely due to the natural protection from anti-A and anti-B isohemagglutinins.
Coagulation
Patients hospitalized for COVID-19 infection typically have elevated fibrinogen and D-dimer levels. On average, fibrinogen is increased to 5.0–7.0 g/dL in COVID-19 ICU patients [10, 24]. CRP is another acute-phase reactant that increases greatly during the acute-phase reaction [79] associated with elevated IL-6 [34, 80, 81].
D-dimers are significantly increased in COVID-19 [10, 24], likely reflecting pulmonary vascular bed thrombosis and fibrinolysis [8]. D-dimers reflect fibrin clot formation, clot crosslinking by FXIIIa, and fibrinolysis. The marked elevation of D-dimers in COVID-19 appears to reflect coagulation activation from viremia and cytokine storm, but superinfection and organ dysfunction are other possible causes. Unfortunately, often the mean D-dimer values cannot be directly compared across publications due to frequent omission of whether D-dimers are reported in D-dimer equivalent units (DDU) or fibrinogen equivalent units (FEU) [82, 83]. A D-dimer cut-off of >1 μg/mL (DDU/FEU units not reported) may stratify COVID-19 patients at a higher risk of poor outcomes [82]. Temporally increasing D-dimer levels indicate the progressive severity of COVID-19 infection and can be used as a predictor that more aggressive critical care will be needed. Of nearly 1,500 COVID-19 hospital admissions, Li et al. [25]found two admission covariates that correlated with an increased risk of death: age (OR 1.18; 95% CI 1.02–1.36) and baseline D-dimer level (OR 3.18; 95% CI 1.48–6.82).
Guan et al. [30]reported a series of 1,099 patients with COVID-19 from China; elevated D-dimer (>0.5 mg/L) (DDU/FEU units not reported) was found in 260/560 (46%) patients. Han et al. [24]reported elevated D-dimer and fibrinogen levels among patients with COVID-19 compared to healthy controls (mean D-dimer 10,400 vs. 260 ng/mL [DDU/FEU units not reported]; mean fibrinogen 500 vs. 290 mg/dL). Fibrinogen degradation products (FDP) were also significantly increased, i.e., 33.8 versus 1.6 mg/L [24]. D-dimers and FDP progressively increased with COVID-19 severity, but the fibrinogen level stayed elevated [24]. This is substantially different from typical DIC [62]. However, Tang et al. [2] did describe 15/21 of the non-survivors (71.4%, vs. 0.6% of the survivors) as meeting the criteria for DIC during hospitalization, with low fibrinogen levels present late in their course. In 183 consecutive COVID-19 patients from Wuhan, D-dimers and FDP levels as well as PT clotting times were significantly increased in non-survivors at admission [2]. At presentation, non-survivors had a mean D-dimer level of 2.12 (range 0.77–5.27) μg/mL, while survivors had a mean of 0.61 (range 0.35–1.29) μg/mL; FEU versus DDU was not specified [2]. Both survivors and non-survivors had elevated fibrinogen upon hospital admission and the levels in these two groups were not statistically different. According to Zhou et al. [84], factors associated with mortality included an elevated D-dimer >1.0 μg/mL (FEU or DDU units not specified) on admission and increased PT. In a multivariate regression, a D-dimer level >1.0 μg/mL at admission was associated with increased mortality with an OR 18.42 (95% CI 2.64–128.55). Huang et al. [85]showed that D-dimer levels on admission were higher in patients needing critical care support (median D-dimer level 2.4 mg/L [0.6–14.4]) than in those not requiring such support (median D-dimer level 0.5 mg/L [0.3–0.8], p = 0.0042) (DDU vs. FEU not specified). These data have prompted the ISTH interim guidelines for COVID-19 coagulopathy to suggest that patients who have a 3–4-fold increase in D-dimers should be considered for hospital admission, even in the absence of other severe symptoms, due to the evidence of increased thrombin generation [40].
In the study by Li et al. [25], fibrinogen was higher at baseline in the subjects who died (median 4.3 [IQR 3.2–5.2] vs. 3.6 [IQR 2.9–4.5] g/L) but also lower at nadir (2.6 [IQR 1.7–3.9] vs. 3.2 [IQR 2.6–3.9] g/L). This implies a greater degree of fibrinogen consumption in the COVID-19 mortalities.
Al-Samkari et al. [23] confirmed excess clotting in 400 COVID-19 inpatients in the USA, all treated with prophylactic anticoagulation. Overall, the thrombotic complication rate was 9.5% (6.8–12.8%) while the overall bleeding rate was 4.8% (2.9–7.3%). D-dimer >2.5 μg/mL at initial presentation was predictive of bleeding, thrombosis, critical illness, and death (DDU vs. FEU not specified). Additional markers at the initial presentation predictive of thrombosis during hospitalization included a platelet count >450 ×109/L (adjusted OR 3.6; 95% CI 1.3–10.0). Forty-one (10.3%) and 10 (2.5%) patients had a platelet count <100 ×109/L or <50 ×109/L during their hospital course, respectively. Patients with more severe thrombocytopenia (<50 ×109/L) had increased bleeding manifestations. They alsofound a very low rate of DIC (2% of critically ill patients) using ISTH criteria.
In a small-scale study by Panigada et al. [22], 55% of the COVID-19 patients had antithrombin levels below the reference range, while protein C was not decreased in any of the patients assessed. Antithrombin is known to be consumed during coagulation, and the mild antithrombin deficiency that they described is consistent with this. The lack of significant protein C deficiency is quite unusual for typical DIC [86], providing further support that the COVID-19-associated coagulopathy may be distinct from DIC.
aPTT waveform analysis was reported in three ICU patients with COVID-19 [87]. These patients had mostly mildly prolonged aPTT clotting times. A biphasic waveform (a marker for DIC) was not present in any of the patients. However, all three showed an increased maximum clot velocity, implying a prothrombotic state.
The finding of small-vessel endothelial damage in COVID-19 patients may help explain the increased incidence of arterial and microvascular thrombotic events [19, 88] in addition to VTE. Severely ill COVID-19 patients can experience arterial thrombosis-related acral ischemia [89]. Among 1,916 adults treated for COVID-19 in 2 New York hospitals, 1.6% experienced an ischemic stroke. In comparison, the stroke rate among influenza patients between 2016 and 2018 was 0.2%. The median time from COVID-19 symptom onset to stroke was 16 days [90].
COVID-19 patients commonly have lupus anticoagulants. Bowles et al. [91]described a 20% incidence of prolonged screening aPTT in 216 COVID-19 patients. Of the patients with prolonged screening aPTT, fully 91% had a detectable lupus anticoagulant. Helms et al. [10]showed 88% lupus anticoagulant positivity in tested COVID-19 ICU patients. Whether these frequent lupus anticoagulants are pathogenic for the increased thrombotic risk in COVID-19 patients, or are epiphenomena, is not known at this time. The markedly elevated CRP levels seen in COVID-19 patients may also be causing false positivity [92].
Viscoelastic Analysis
COVID-19 is associated with a hypercoagulable profile, mostly affecting clot formation kinetics and clot strength. Ranucci et al. [62] showed that, upon admission to the ICU, a group of intubated COVID-19 patients with normal platelet counts, mildly prolonged aPTT, and elevated plasma fibrinogen had a markedly increased fibrinogen contribution to clot strength on Quantra viscoelastic analysis. Similar findings are seen with the TEG 5000 instrument, with an increased α angle and maximum amplitude, using a kaolin activator with native blood in the presence of heparinase [22]. Pavoni et al. [81] showed similar hypercoagulable findings with ROTEM that persisted over the course of COVID-19 illness. In contrast to these findings with clot kinetics and clot strength, clot time (CT and R time) are less commonly hypercoagulable in COVID-19.
ICU patients with COVID-19 commonly show a complete absence of detectable fibrinolysis 30 min after achievement of maximum clot amplitude (LY30 0.0%) [93]. Patients with both 0.0% LY30 and a D-dimer level >2,600 ng/mL (FEU) had a VTE event rate of 50% compared with 0% in patients meeting neither criterion (p = 0.008), and a hemodialysis rate of 80% compared with 14% in patients meeting neither criterion (p = 0.004) [93]. In this way, COVID-19 coagulopathy is somewhat similar to sepsis-induced disseminated intravascular coagulation, which typically presents with suppressed fibrinolysis [94]. However, as compared to sepsis-associated DIC, D-dimer levels are typically more significantly elevated in COVID-19 [94]. While LY30 measurement during COVID-19 can seem to imply fibrinolytic shutdown, the markedly elevated D-dimer level clearly shows continuing fibrinolysis. The very low LY30 TEG values for these patients reveal an absence of elevated in vitrofibrinolysis. The details of in vivofibrinolysis in COVID-19 have not yet been investigated, but fibrinolysis is obviously continuing to some degree.
COVID-19 coagulopathy can often meet criteria for the relatively newly defined entity of sepsis-induced coagulopathy (SIC), which is defined and quantified according to a reduced platelet count, increased INR, and higher organ dysfunction score [95, 96].
Anticoagulation and Anticoagulation Monitoring
Critically ill patients in ICU settings experience VTE rates of 13–30% without chemoprophylaxis, and 5–15% with routine chemoprophylaxis [93]. However, Chinese COVID-19 inpatients were not routinely treated with prophylactic anticoagulation, as is common practice in the USA [12]. Routine thromboprophylaxis is not standard in Chinese hospitals, partly due to the lower rate of VTE detected in Asians [97]. This must be kept in mind when comparing D-dimer levels in COVID-19 studies.
In a retrospective study on 449 patients with severe COVID-19, no difference in 28-day mortality was found between heparin users and nonusers (30.3 vs. 29.7%; p = 0.910). However, the 28-day mortality of heparin users was lower than that of nonusers in patients with an ISTH SIC score ≥4 or a D-dimer level >3.0 μg/mL (FEU vs DDU not specified) [98]. Prophylactic-dose low-molecular-weight heparin is recommended for all hospitalized COVID-19 patients despite abnormal coagulation tests in the absence of active bleeding, and is withheld only if platelet counts are <25 ×109/L, or the fibrinogen level is <0.5 g/L [99].
Some have argued for the use of therapeutic dose anticoagulation in COVID-19 patients without identified thrombosis [100]. However, it must be kept in mind that therapeutic anticoagulation is associated with increased bleeding. In October 2020, the American Society of Hematology published guidelines suggesting using prophylactic-intensity over intermediate-intensity or therapeutic-intensity anticoagulation in patients with COVID-19 related critical illness who do not have suspected or confirmed VTE [105]. VTE rates remain quite high in COVID-19 patients despite therapeutic anticoagulation [13]. The mild prolongation of aPTT in COVID-19 patients may necessitate the monitoring of unfractionated heparin with anti-Xa assays.
Bleeding is rare in the setting of COVID-19. Transfusion therapy should not be instituted on the basis of laboratory results alone, but rather be reserved for those with active bleeding, requiring an invasive procedure, or who are at an otherwise high risk for bleeding complications. If bleeding does develop, patients can be managed with principles similar to those in ISTH guidelines for DIC [101].
Conclusion
The currently available evidence suggests that the COVID-19 coagulopathy represents a combination of localized pulmonary platelet consumption, low-grade DIC (only rarely meeting the ISTH DIC criteria), and variably a thrombotic microangiopathy. Elevated vWF levels and soluble thrombomodulin imply activated or damaged endothelium, as has been seen histologically in autopsy studies. It would be anticipated that damaged endothelium would result in the release of ultra-large vWF multimers capable of interacting with platelets, leading to platelet activation, microthrombi, and platelet consumption. Elevated soluble P-selectin levels and platelet flow cytometric studies suggest increased activation of endothelium and/or circulating platelets in COVID-19 patients [102]. Evidence of a direct stimulatory role of SARS-CoV-2 Spike protein upon platelets has also recently been presented [64]. Severe COVID-19 illness is associated with increased platelet activation as well as platelet-monocyte aggregation [104]. Platelets from severely ill COVID-19 patients can induce monocyte TF expression (in a P-selectin and αIIb/β3 dependent manner) [104], which may amplify inflammation and hypercoagulability in these patients.
The homeostatic response to platelet consumption is increased platelet production with an increase in the IPF. This compensatory response is robust in COVID-19 and can be out of proportion to the degree of thrombocytopenia, with elevated MPV and IPF occurring even in COVID-19 patients with normal platelet counts.
Despite the large number of publications focusing on the hemostatic changes associated with COVID-19, it should be kept in mind that all severe infectious disorders are associated with changes in hemostasis laboratory values as well as thrombotic and bleeding events. Al-Samkari et al. [23] have shown that the VTE rate in critically ill COVID-19 patients receiving thromboprophylaxis is similar to the previously published rates in patients with non-COVID-19 critical illness. They showed similar findings for bleeding events. This raises the question as to whether COVID-19 has a unique effect on the hemostatic system or simply causes the expected activation of the hemostatic system in the setting of severe inflammation [23].
Continued controlled studies are necessary to guide best treatment for COVID-19 patients and better elucidate the role that platelets play in COVID-19 pathophysiology.
Conflict of Interest Statement
G.D.W. is on an advisory committee at Diagnostica Stago and receives honoraria. J.L.M. declares no conflicts of interest.
Acknowledgements
The authors would like to thank Kara Newton and Drs. Megan Parilla and Sandeep Gurbuxani for assistance with patients' identification and data extraction.
References
- 1.Liu Y, Sun W, Guo Y, Chen L, Zhang L, Zhao S, et al. Association between platelet parameters and mortality in coronavirus disease 2019: retrospective cohort study. Platelets. 2020 May;31((4)):490–6. doi: 10.1080/09537104.2020.1754383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020 Apr;18((4)):844–7. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klok FA, Kruip MJ, van der Meer NJ, Arbous MS, Gommers DA, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 Jul;191:145–7. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marietta M, Ageno W, Artoni A, De Candia E, Gresele P, Marchetti M, et al. COVID-19 and haemostasis: a position paper from Italian Society on Thrombosis and Haemostasis (SISET) Blood Transfus. 2020 May;18((3)):167–9. doi: 10.2450/2020.0083-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020 Apr;5((4)):562–9. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaduganathan M, Vardeny O, Michel T, McMurray JJ, Pfeffer MA, Solomon SD. Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19. N Engl J Med. 2020 Apr;382((17)):1653–9. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020 Mar;367((6483)):1260–3. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGonagle D, O'Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020 Jul;2((7)):e437–45. doi: 10.1016/S2665-9913(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020 Jun;75((23)):2950–73. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, et al. CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis) High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020 Jun;46((6)):1089–98. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thachil J, Cushman M, Srivastava A. A Proposal for Staging COVID-19 Coagulopathy. Research and Practice in Thrombosis and Haemotasis. 2020 doi: 10.1002/rth2.12372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Lancet Haematology COVID-19 coagulopathy: an evolving story. Lancet Haematol. 2020 Jun;7((6)):e425. doi: 10.1016/S2352-3026(20)30151-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Llitjos JF, Leclerc M, Chochois C, Monsallier JM, Ramakers M, Auvray M, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020 Jul;18((7)):1743–6. doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Humanitas COVID-19 Task Force Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020 Jul;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spyropoulos AC, Levy JH, Ageno W, Connors JM, Hunt BJ, Iba T, et al. Subcommittee on Perioperative, Critical Care Thrombosis, Haemostasis of the Scientific, Standardization Committee of the International Society on Thrombosis and Haemostasis Scientific and Standardization Committee communication: clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020 Aug;18((8)):1859–65. doi: 10.1111/jth.14929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020 Jun;127:104362. doi: 10.1016/j.jcv.2020.104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Obi AT, Tignanelli CJ, Jacobs BN, Arya S, Park PK, Wakefield TW, et al. Empirical systemic anticoagulation is associated with decreased venous thromboembolism in critically ill influenza A H1N1 acute respiratory distress syndrome patients. J Vasc Surg Venous Lymphat Disord. 2019 May;7((3)):317–24. doi: 10.1016/j.jvsv.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 18.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020 Jun;135((23)):2033–40. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020 Jul;383((2)):120–8. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020 May;395((10234)):1417–8. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020 Jun;7((6)):e438–40. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V, et al. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020 Jul;18((7)):1738–42. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Samkari H, Karp Leaf RS, Dzik WH, Carlson JC, Fogerty AE, Waheed A, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020 Jul;136((4)):489–500. doi: 10.1182/blood.2020006520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Han H, Yang L, Liu R, Liu F, Wu KL, Li J, et al. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 2020 Jun;58((7)):1116–20. doi: 10.1515/cclm-2020-0188. [DOI] [PubMed] [Google Scholar]
- 25.Li Q, Cao Y, Chen L, Wu D, Yu J, Wang H, et al. Hematological features of persons with COVID-19. Leukemia. 2020 Aug;34((8)):2163–72. doi: 10.1038/s41375-020-0910-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang M, Ng MH, Li CK. Thrombocytopenia in patients with severe acute respiratory syndrome (review) Hematology. 2005 Apr;10((2)):101–5. doi: 10.1080/10245330400026170. [DOI] [PubMed] [Google Scholar]
- 27.Wong RS, Wu A, To KF, Lee N, Lam CW, Wong CK, et al. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. BMJ. 2003 Jun;326((7403)):1358–62. doi: 10.1136/bmj.326.7403.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zou Z, Yang Y, Chen J, Xin S, Zhang W, Zhou X, et al. Prognostic factors for severe acute respiratory syndrome: a clinical analysis of 165 cases. Clin Infect Dis. 2004 Feb;38((4)):483–9. doi: 10.1086/380973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang Y, Zeng X, Jiao Y, Li Z, Liu Q, Ye J, et al. Mechanisms involved in the development of thrombocytopenia in patients with COVID-19. Thromb Res. 2020 Sep;193:110–5. doi: 10.1016/j.thromres.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19 Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020 Apr;382((18)):1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang X, Yang Q, Wang Y, Wu Y, Xu J, Yu Y, et al. Thrombocytopenia and its association with mortality in patients with COVID-19. J Thromb Haemost. 2020 Jun;18((6)):1469–72. doi: 10.1111/jth.14848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thachil J. What do monitoring platelet counts in COVID-19 teach us? J Thromb Haemost. 2020 Aug;18((8)):2071–2. doi: 10.1111/jth.14879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta. 2020 Jul;506:145–8. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Henry BM, de Oliveira MH, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020 Jun;58((7)):1021–8. doi: 10.1515/cclm-2020-0369. [DOI] [PubMed] [Google Scholar]
- 35.Bomhof G, Mutsaers PG, Leebeek FW, Te Boekhorst PA, Hofland J, Croles FN, et al. COVID-19-associated immune thrombocytopenia. Br J Haematol. 2020 Jul;190((2)):e61–4. doi: 10.1111/bjh.16850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jiang SQ, Huang QF, Xie WM, Lv C, Quan XQ. The association between severe COVID-19 and low platelet count: evidence from 31 observational studies involving 7613 participants. Br J Haematol. 2020 Jul;190((1)):e29–33. doi: 10.1111/bjh.16817. [DOI] [PubMed] [Google Scholar]
- 37.Amgalan A, Othman M. Hemostatic laboratory derangements in COVID-19 with a focus on platelet count. Platelets. 2020 Aug;31((6)):740–5. doi: 10.1080/09537104.2020.1768523. [DOI] [PubMed] [Google Scholar]
- 38.Yin S, Huang M, Li D, Tang N. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolysis. 2020 Apr; doi: 10.1007/s11239-020-02105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pouletty M, Borocco C, Ouldali N, Caseris M, Basmaci R, Lachaume N, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann Rheum Dis. 2020 Aug;79((8)):999–1006. doi: 10.1136/annrheumdis-2020-217960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020 May;18((5)):1023–6. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chabert A, Hamzeh-Cognasse H, Pozzetto B, Cognasse F, Schattner M, Gomez RM, et al. Human platelets and their capacity of binding viruses: meaning and challenges? BMC Immunol. 2015 Apr;16((1)):26. doi: 10.1186/s12865-015-0092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Assinger A. Platelets and infection - an emerging role of platelets in viral infection. Front Immunol. 2014 Dec;5:649. doi: 10.3389/fimmu.2014.00649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Seyoum M, Enawgaw B, Melku M. Human blood platelets and viruses: defense mechanism and role in the removal of viral pathogens. Thromb J. 2018 Jul;16((1)):16. doi: 10.1186/s12959-018-0170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fitzgerald JR, Foster TJ, Cox D. The interaction of bacterial pathogens with platelets. Nat Rev Microbiol. 2006 Jun;4((6)):445–57. doi: 10.1038/nrmicro1425. [DOI] [PubMed] [Google Scholar]
- 45.Herter JM, Rossaint J, Zarbock A. Platelets in inflammation and immunity. J Thromb Haemost. 2014 Nov;12((11)):1764–75. doi: 10.1111/jth.12730. [DOI] [PubMed] [Google Scholar]
- 46.Estevez B, Du X. New Concepts and Mechanisms of Platelet Activation Signaling. Physiology (Bethesda) 2017 Mar;32((2)):162–77. doi: 10.1152/physiol.00020.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hottz ED, Bozza FA, Bozza PT. Platelets in Immune Response to Virus and Immunopathology of Viral Infections. Front Med (Lausanne) 2018 Apr;5:121. doi: 10.3389/fmed.2018.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ed Rainger G, Chimen M, Harrison MJ, Yates CM, Harrison P, Watson SP, et al. The role of platelets in the recruitment of leukocytes during vascular disease. Platelets. 2015;26((6)):507–20. doi: 10.3109/09537104.2015.1064881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smyth SS, McEver RP, Weyrich AS, Morrell CN, Hoffman MR, Arepally GM, et al. 2009 Platelet Colloquium Participants Platelet functions beyond hemostasis. J Thromb Haemost. 2009 Nov;7((11)):1759–66. doi: 10.1111/j.1538-7836.2009.03586.x. [DOI] [PubMed] [Google Scholar]
- 50.Weyrich AS, Zimmerman GA. Platelets in lung biology. Annu Rev Physiol. 2013;75((1)):569–91. doi: 10.1146/annurev-physiol-030212-183752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zarbock A, Singbartl K, Ley K. Complete reversal of acid-induced acute lung injury by blocking of platelet-neutrophil aggregation. J Clin Invest. 2006 Dec;116((12)):3211–9. doi: 10.1172/JCI29499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nemmar A, Hoet PH, Vandervoort P, Dinsdale D, Nemery B, Hoylaerts MF. Enhanced peripheral thrombogenicity after lung inflammation is mediated by platelet-leukocyte activation: role of P-selectin. J Thromb Haemost. 2007 Jun;5((6)):1217–26. doi: 10.1111/j.1538-7836.2007.02557.x. [DOI] [PubMed] [Google Scholar]
- 53.Sugiyama MG, Gamage A, Zyla R, Armstrong SM, Advani S, Advani A, et al. Influenza Virus Infection Induces Platelet-Endothelial Adhesion Which Contributes to Lung Injury. J Virol. 2015 Dec;90((4)):1812–23. doi: 10.1128/JVI.02599-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morrell CN, Aggrey AA, Chapman LM, Modjeski KL. Emerging roles for platelets as immune and inflammatory cells. Blood. 2014 May;123((18)):2759–67. doi: 10.1182/blood-2013-11-462432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Handtke S, Steil L, Palankar R, Conrad J, Cauhan S, Kraus L, et al. Role of Platelet Size Revisited-Function and Protein Composition of Large and Small Platelets. Thromb Haemost. 2019 Mar;119((3)):407–20. doi: 10.1055/s-0039-1677875. [DOI] [PubMed] [Google Scholar]
- 56.Hille L, Lenz M, Vlachos A, Grüning B, Hein L, Neumann FJ, et al. Ultrastructural, transcriptional, and functional differences between human reticulated and non-reticulated platelets. J Thromb Haemost. 2020 Aug;18((8)):2034–46. doi: 10.1111/jth.14895. [DOI] [PubMed] [Google Scholar]
- 57.Handtke S, Thiele T. Large and small platelets-(When) do they differ? J Thromb Haemost. 2020 Jun;18((6)):1256–67. doi: 10.1111/jth.14788. [DOI] [PubMed] [Google Scholar]
- 58.Lador A, Leshem-Lev D, Spectre G, Abelow A, Kornowski R, Lev EI. Characterization of surface antigens of reticulated immature platelets. J Thromb Thrombolysis. 2017 Oct;44((3)):291–7. doi: 10.1007/s11239-017-1533-x. [DOI] [PubMed] [Google Scholar]
- 59.Psaila B, Bussel JB, Linden MD, Babula B, Li Y, Barnard MR, et al. In vivo effects of eltrombopag on platelet function in immune thrombocytopenia: no evidence of platelet activation. Blood. 2012 Apr;119((17)):4066–72. doi: 10.1182/blood-2011-11-393900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nishimura S, Nagasaki M, Kunishima S, Sawaguchi A, Sakata A, Sakaguchi H, et al. IL-1α induces thrombopoiesis through megakaryocyte rupture in response to acute platelet needs. J Cell Biol. 2015 May;209((3)):453–66. doi: 10.1083/jcb.201410052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Armstrong PC, Hoefer T, Knowles RB, Tucker AT, Hayman MA, Ferreira PM, et al. Newly Formed Reticulated Platelets Undermine Pharmacokinetically Short-Lived Antiplatelet Therapies. Arterioscler Thromb Vasc Biol. 2017 May;37((5)):949–56. doi: 10.1161/ATVBAHA.116.308763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ranucci M, Ballotta A, Di Dedda U, Bayshnikova E, Dei Poli M, Resta M, et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020 Jul;18((7)):1747–51. doi: 10.1111/jth.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Manne BK, Denorme F, Middleton EA, Portier I, Rowley JW, Stubben C, et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020 Sep;136((11)):1317–29. doi: 10.1182/blood.2020007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang S, Liu Y, Wang X, Yang L, Li H, Wang Y, et al. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J Hematol Oncol. 2020 Sep;13((1)):120. doi: 10.1186/s13045-020-00954-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Iba T, Levy JH, Levi M, Connors JM, Thachil J. Coagulopathy of Coronavirus Disease 2019. Crit Care Med. 2020 Sep;48((9)):1358–64. doi: 10.1097/CCM.0000000000004458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res. 2020 Jun;190:62. doi: 10.1016/j.thromres.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Othman M, Labelle A, Mazzetti I, Elbatarny HS, Lillicrap D. Adenovirus-induced thrombocytopenia: the role of von Willebrand factor and P-selectin in mediating accelerated platelet clearance. Blood. 2007 Apr;109((7)):2832–9. doi: 10.1182/blood-2006-06-032524. [DOI] [PubMed] [Google Scholar]
- 68.Escher R, Breakey N, Lämmle B. ADAMTS13 activity, von Willebrand factor, factor VIII and D-dimers in COVID-19 inpatients. Thromb Res. 2020 Aug;192:174–5. doi: 10.1016/j.thromres.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Martinelli N, Montagnana M, Pizzolo F, Friso S, Salvagno GL, Forni GL, et al. A relative ADAMTS13 deficiency supports the presence of a secondary microangiopathy in COVID 19. Thromb Res. 2020 Sep;193:170–2. doi: 10.1016/j.thromres.2020.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Blasi A, von Meijenfeldt FA, Adelmeijer J, Calvo A, Ibañez C, Perdomo J, et al. In vitro hypercoagulability and ongoing in vivo activation of coagulation and fibrinolysis in COVID-19 patients on anticoagulation. J Thromb Haemost. 2020 Aug;18((10)):2646–53. doi: 10.1111/jth.15043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Goshua G, Pine AB, Meizlish ML, Chang CH, Zhang H, Bahel P, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020 Aug;7((8)):e575–82. doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhao J, Yang Y, Huang H, Li D, Gu D, Lu X, et al. Relationship between the ABO Blood Group and the COVID-19 Susceptibility. Clin Infect Dis. 2020 Aug; doi: 10.1093/cid/ciaa1150. ciaa1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Latz CA, DeCarlo C, Boitano L, Png CY, Patell R, Conrad MF, et al. Blood type and outcomes in patients with COVID-19. Ann Hematol. 2020 Sep;99((9)):2113–8. doi: 10.1007/s00277-020-04169-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ellinghaus D, Degenhardt F, Bujanda L, Buti M, Albillos A, Invernizzi P, et al. Severe Covid-19 GWAS Group Genomewide Association Study of Severe Covid-19 with Respiratory Failure. N Engl J Med. 2020 Jun;:NEJMoa2020283. doi: 10.1056/NEJMoa2020283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee-Sundlov MM, Stowell SR, Hoffmeister KM. Multifaceted role of glycosylation in transfusion medicine, platelets, and red blood cells. J Thromb Haemost. 2020 Jul;18((7)):1535–47. doi: 10.1111/jth.14874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gérard C, Maggipinto G, Minon JM. COVID-19 and ABO blood group: another viewpoint. Br J Haematol. 2020 Jul;190((2)):e93–4. doi: 10.1111/bjh.16884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Breiman A, Ruvën-Clouet N, Le Pendu J. Harnessing the natural anti-glycan immune response to limit the transmission of enveloped viruses such as SARS-CoV-2. PLoS Pathog. 2020 May;16((5)):e1008556. doi: 10.1371/journal.ppat.1008556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gallian P, Pastorino B, Morel P, Chiaroni J, Ninove L, de Lamballerie X. Lower prevalence of antibodies neutralizing SARS-CoV-2 in group O French blood donors. Antiviral Res. 2020 Sep;181:104880. doi: 10.1016/j.antiviral.2020.104880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med. 2020 Jun;58((7)):1131–4. doi: 10.1515/cclm-2020-0198. [DOI] [PubMed] [Google Scholar]
- 80.Liu F, Li L, Xu M, Wu J, Luo D, Zhu Y, et al. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol. 2020 Jun;127:104370. doi: 10.1016/j.jcv.2020.104370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pavoni V, Gianesello L, Pazzi M, Stera C, Meconi T, Frigieri FC. Evaluation of coagulation function by rotation thromboelastometry in critically ill patients with severe COVID-19 pneumonia. J Thromb Thrombolysis. 2020 Aug;50((2)):281–6. doi: 10.1007/s11239-020-02130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Reyes Gil M, Lee A, Key N, et al. COVID-19 and D-dimer: Frequently Asked Questions. ASH. https://www.hematology.org/covid-19/covid-19-and-d-dimer. [Google Scholar]
- 83.Lippi G, Favaloro EJ. D-dimer is Associated with Severity of Coronavirus Disease 2019: A Pooled Analysis. Thromb Haemost. 2020 May;120((5)):876–8. doi: 10.1055/s-0040-1709650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar;395((10229)):1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb;395((10223)):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Takahashi H, Takakuwa E, Yoshino N, Hanano M, Shibata A. Protein C levels in disseminated intravascular coagulation and thrombotic thrombocytopenic purpura: its correlation with other coagulation parameters. Thromb Haemost. 1985 Aug;54((2)):445–9. [PubMed] [Google Scholar]
- 87.Tan CW, Low JG, Wong WH, Chua YY, Goh SL, Ng HJ. Critically ill COVID-19 infected patients exhibit increased clot waveform analysis parameters consistent with hypercoagulability. Am J Hematol. 2020 Jul;95((7)):E156–8. doi: 10.1002/ajh.25822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fara MG, Stein LK, Skliut M, Morgello S, Fifi JT, Dhamoon MS. Macrothrombosis and stroke in patients with mild Covid-19 infection. J Thromb Haemost. 2020 Aug;18((8)):2031–3. doi: 10.1111/jth.14938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kolivras A, Dehavay F, Delplace D, Feoli F, Meiers I, Milone L, et al. Coronavirus (COVID-19) infection-induced chilblains: A case report with histopathologic findings. JAAD Case Rep. 2020 Apr;6((6)):489–92. doi: 10.1016/j.jdcr.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, et al. Risk of Ischemic Stroke in Patients With Coronavirus Disease 2019 (COVID-19) vs Patients With Influenza. JAMA Neurol. 2020 Jul; doi: 10.1001/jamaneurol.2020.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bowles L, Platton S, Yartey N, Dave M, Lee K, Hart DP, et al. Lupus Anticoagulant and Abnormal Coagulation Tests in Patients with Covid-19. N Engl J Med. 2020 Jul;383((3)):288–90. doi: 10.1056/NEJMc2013656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Connell NT, Battinelli EM, Connors JM. Coagulopathy of COVID-19 and antiphospholipid antibodies. J Thromb Haemost. 2020 May;:jth.14893. doi: 10.1111/jth.14893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wright FL, Vogler TO, Moore EE, Moore HB, Wohlauer MV, Urban S, et al. Fibrinolysis Shutdown Correlation with Thromboembolic Events in Severe COVID-19 Infection. J Am Coll Surg. 2020 Aug;231((2)):193–203.e1. doi: 10.1016/j.jamcollsurg.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Asakura H. Classifying types of disseminated intravascular coagulation: clinical and animal models. J Intensive Care. 2014 Mar;2((1)):20. doi: 10.1186/2052-0492-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Iba T, Levy JH, Warkentin TE, Thachil J, van der Poll T, Levi M, Scientific and Standardization Committee on DIC, and the Scientific and Standardization Committee on Perioperative and Critical Care of the International Society on Thrombosis and Haemostasis Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost. 2019 Nov;17((11)):1989–94. doi: 10.1111/jth.14578. [DOI] [PubMed] [Google Scholar]
- 96.Iba T, Levy JH, Yamakawa K, Thachil J, Warkentin TE, Levi M, Scientific and Standardization Committee on DIC of the International Society on Thrombosis and Haemostasis Proposal of a two-step process for the diagnosis of sepsis-induced disseminated intravascular coagulation. J Thromb Haemost. 2019 Aug;17((8)):1265–8. doi: 10.1111/jth.14482. [DOI] [PubMed] [Google Scholar]
- 97.White RH, Keenan CR. Effects of race and ethnicity on the incidence of venous thromboembolism. Thromb Res. 2009;123(Suppl 4):S11–7. doi: 10.1016/S0049-3848(09)70136-7. [DOI] [PubMed] [Google Scholar]
- 98.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 May;18((5)):1094–9. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lisa Baumann Kreuziger AL, David Garcia, Adam Cuker, Mary Cushman, Maria DeSancho, and Jean M. Connors COVID-19 and VTE/Anticoagulation: Frequently Asked Questions. ASH. ASH COVID-19 Resources Web site. https://www.hematology.org/covid-19/covid-19-and-vte-anticoagulation. Published 2020. Updated 6/23/2020, 2020. [Google Scholar]
- 100.Barrett CD, Moore HB, Yaffe MB, Moore EE. ISTH interim guidance on recognition and management of coagulopathy in COVID-19: A comment. J Thromb Haemost. 2020 Aug;18((8)):2060–3. doi: 10.1111/jth.14860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wada H, Thachil J, Di Nisio M, Mathew P, Kurosawa S, Gando S, et al. The Scientific Standardization Committee on DIC of the International Society on Thrombosis Haemostasis Guidance for diagnosis and treatment of DIC from harmonization of the recommendations from three guidelines. J Thromb Haemost. 2013 Feb; doi: 10.1111/jth.12155. [DOI] [PubMed] [Google Scholar]
- 102.Fijnheer R, Frijns CJ, Korteweg J, Rommes H, Peters JH, Sixma JJ, et al. The origin of P-selectin as a circulating plasma protein. Thromb Haemost. 1997 Jun;77((6)):1081–5. [PubMed] [Google Scholar]
- 103.Amgalan A, Othman M. Exploring possible mechanisms for COVID-19 induced thrombocytopenia: unanswered questions. J Thromb Haemost. 2020 Jun;18((6)):1514–6. doi: 10.1111/jth.14832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hottz ED, Azevedo-Quintanilha IG, Palhinha L, Teixeira L, Barreto EA, Pão CR, et al. Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020 Sep;136((11)):1330–41. doi: 10.1182/blood.2020007252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.ASH 2020 guidelines on the use of anticoagulation in patients with COVID-19: Draft recommendations. Washington, DC: American Society of Hematology Published October 8, 2020 http://www.hematology.org/COVIDguidelines. [Google Scholar]