Abstract
National Public Health Institutes (NPHIs) are national-level institutions that can lead and coordinate a country’s public health system. The Africa Centres for Disease Control and Prevention (Africa CDC) considers NPHI development critical to strengthening public health systems in Africa. This paper describes how Joint External Evaluation (JEE) reports demonstrate the role NPHIs can play in supporting the goals of IHR compliance and global health security. This study is a secondary document-based qualitative analysis of JEE reports from 11 countries in the WHO AFRO region (Botswana, Ethiopia, Liberia, Mozambique, Namibia, Nigeria, Rwanda, Sierra Leone, South Africa, Uganda, and Zambia). Researchers found three distinct thematic areas: i) core public health functions, ii) governance, and iii) coordination, collaboration, and communication. These themes and their interlinkages, both in pairs and all three, were of importance in displaying the roles that NPHIs could play in the strengthening of health systems. The data suggests that NPHIs, though not always explicitly mentioned in the data, may have a vital role in strengthening health systems across Africa and their governments’ goals of achieving IHR compliance.
Key words: National public health institute, global health security, joint external evaluation
Introduction
The Global Health Security Agenda (GHSA), a collaboration among World Health Organization (WHO) member states, aims to strengthen global capacity to prevent, detect, and respond to public health threats.1-3 GHSA helps countries achieve compliance with the 2005 International Health Regulations (IHR), an agreement between all 196 WHO member states to “a new standard of reciprocal responsibility among nations” with a commitment to the advancement of “core capacities required to detect, assess, report, and respond to any public health event that might cross borders, whether of natural, accidental, or deliberate origin.”4 To assess a country’s status and progress toward meeting the IHR across 19 technical areas, the WHO developed the Joint External Evaluation (JEE). Within each technical area are indicators that measure different aspects of that capacity.5 Evaluators assign each indicator a score on a five-point scale, ranging from “no capacity” to “sustainable capacity” and identify a technical area’s priority actions and its indicators’ strengths and challenges.5 JEEs often link to other GHSA tools, including National Action Plans for Health Security (NAPHS). NAPHS help countries determine actions and resources needed to address gaps identified in JEEs.
Countries have employed different ways to improve the competencies necessary to achieve IHR compliance, including establishing or strengthening National Public Health Institutes (NPHIs). NPHIs are science-based, national-level institutions that provide leadership and coordination for a country’s public health system.6-10 While Ministries of Health are often heavily focused on clinical services, which can result in limited coordination of and focus on public health programs and systems, NPHIs bring together disparate, public health functions to centralize programming and responses. NPHI functions and attributes, shown in Table 1, vary depending on a country’s needs, but generally, NPHIs are responsible for coordinating national laboratory and surveillance activities, outbreak detection and response, workforce development, implementing public health programs, and public health research.7,9-11 These institutes increase efficiency within the public health system through improved coordination and reduce fragmentation, redundancy, and organizational barriers that might exist in a system without such a focal point.9,10 Several countries have long-standing NPHIs (e.g., Colombia, Ethiopia, Finland, United States), while other countries established an NPHI in response to a public health crisis (e.g., Canada, Liberia).9,12-14 NPHIs can be structured as line agencies of the Ministry of Health, semi-autonomous parastatal organizations, or a hybrid of the two (Table 1).9,10 In 2017, the Africa Centres for Disease Control and Prevention (Africa CDC) was launched as a specialized technical institution of the African Union (AU) to help build AU Member States’ capacities for surveillance, response, and prevention of infectious diseases.15 Africa CDC considers NPHI development critical to strengthening public health systems in Africa by supporting the integration and coordination of its strategic pillars.9,15,16 Supporting the establishment and creation of NPHIs in member countries is foundational to Africa CDC’s mandate, and its operational structure includes regional collaborating centers to build cross-border relationships and support regional public health functions among NPHIs. This, along with wide participation in JEEs in Africa, indicates results of JEE reports may be valuable to guide priorities and needs for NPHIs across the continent.
NPHI establishment is neither a requirement of IHR nor a technical area of the JEE. As such, report indicators do not specifically include NPHIs. The paper uses JEE reports to identify direct and indirect references to NPHIs and the roles that NPHIs can play in relevant technical areas. Through themes identified, the paper will describe how JEE reports demonstrate these roles and how NPHIs can support the goals of IHR compliance and global health security.
Materials and Methods
Study Design and Sample
This analysis was a document-based qualitative case study of 11 JEE reports from WHO’s AFRO region. Using purposive sampling, JEE reports were included in the sample based on: i) the availability of a JEE report in English and ii) whether the country had established or was pursuing establishment of an NPHI. Communications between country leadership, IANPHI, and US Centers for Disease Control and Prevention at the time of the study determined the establishment status of the NPHI. The selected countries had JEE reports published prior to June 2018; dates of evaluations can be found in Table 2. The study spanned a seven-month period from February-August 2019.
Data Collection and Analysis
The JEE reports for the 11 selected countries were publicly available through the WHO website.17 Data collection, storage, and analysis occurred in Microsoft Excel. Researchers converted the reports, indicator by indicator, into an Excel spreadsheet to create the data set. The data were secondary, gathered from 13 of 19 technical areas after determining through a review of the content of the reports that six technical areas were not under the direct purview of NPHI functions and attributes, as displayed in Table 1. Included and excluded technical areas are in Table 3.
The data examined were from the “Recommendations for priority actions” sections and “Strengths/best practices” and “Areas that need strengthening and challenges” subsections for indicators within the technical areas. The sections and subsections provided justifications for each indicator that could be converted into separate data entries, which served as the data set. The research team iteratively created and refined the codebook based on deductive coding of two initial JEE reports.18,19 Resulting discussions led to the finalization of the codebook and two researchers coded each report using it. A third researcher, the tie-breaker, reviewed the initial coders’ work, confirming consensus.19 When necessary and appropriate, the tiebreaker resolved disagreements between the two initial coders by making final decisions about which codes correctly applied according to the code definition.19,20
The use of extant text allowed for a contextual thematic analysis of the data for the presence of direct mentions of NPHIs and their functions and attributes in relation to the JEE.18 For analysis, researchers treated data coded with “NPHI” as a separate subset of the full dataset in order to determine how JEE reports mentioned NPHIs. First, researchers identified patterns from the coded data from the NPHI subset and the larger dataset separately. Analysis generated subthemes from the identified patterns, which then translated to three larger thematic areas and their interlinkages. The findings led to the creation of a conceptual map (Figure 1) that presents key results from the larger dataset and the NPHI subset.
Results
The research team identified three main themes from the JEE reports analyzed that demonstrated roles NPHIs can play in supporting the goals of IHR compliance and global health: i) core public health functions; ii) governance; and iii) coordination, collaboration, and communication. Although each theme could appear separately, they were more commonly interdependent or interlinked. The data directly linked NPHIs with these three themes. Data described NPHIs’ potential roles in a country’s public health system, as well as the environment of resources and conditions that enable NPHIs to function (e.g., financing, authorizing legislation).
Table 1.
NPHI Functions and Attributes, as defined in the Framework for Development of National Public Health Institutes in Africa by the Africa Centres for Disease Control and Prevention (Africa CDC) and the Framework for the Creation and Development of National Public Health Institutes by the International Association of National Public Health Institutes (IANPHI).9,10 Both frameworks highlight similar functions and attributes; however, the language used in Table 1 more closely reflects the Africa CDC Framework, except where noted.
| Functions are “external-facing,” focused on impact on entities outside of an NPHI | Attributes are “internal-facing,” such as management and operations |
|---|---|
| Africa CDC and IANPHI | Africa CDC and IANPHI |
| • Population health and health-related indicators | • Science-based |
| • Public health laboratory and surveillance systems, and emergency preparedness and response (Note: IANPHI separates Reduction of the impact of emergencies and disasters on health) | • National scope |
| • Disease prevention and health promotion | • Transparent and accountable |
| • Advocacy, communication and social mobilization | • Strong and continuously improving NPHI workforce |
| • Policies and plans that support individual and community health efforts | • Adequate infrastructure to perform core functions efficiently |
| • Health protection and support for regulation and enforcement | • Clearly defined legal authority for its work |
| • Evaluation and promotion of equitable access to services | • Linkages at international, national, and subnational levels |
| • Public health workforce development | • Plans for sustainability |
| • Evaluation, prevention, and control of public health issues in clinical settings | IANPHI also includes: |
| • Research in public health | • Focus on the major public health problems affecting the country |
| • Limitations on political influence |
Figure 1 shows the progression of analysis from individual themes to a collated concept map that displays the themes that both sets of data had in common. In Figure 1A, the areas with unique colors display how the overlapping subthemes fit into larger thematic areas: core public health functions (orange); governance (purple); and coordination, collaboration, and communication (green). Subthemes found in either the NPHI dataset or the larger dataset, are detailed in Appendix A. The subthemes under “core public health functions” are abstracted from the more granular subthemes within each core public health function. The added slices in Figure 1B depict interlinkages between adjacent thematic areas. Appendix B displays all overlapping subthemes and subthemes that are only present in the larger dataset which are not in Figure 1. Figure 1C represents the completed conceptual map, where the added circle displays the interlinkage of all three thematic areas. All overlapping subthemes and subthemes only present in the larger dataset, not depicted in Figure 1, are in Appendix C. One of the subthemes presented, core functions, is a simplification of the four subthemes presented in the core public health functions thematic area. Notably, if a subtheme appeared in multiple classifications in Appendices A-C, it can be found in the area where it had the most thematic interaction on Figure 1. For example, Integrated Disease Surveillance and Response was a subtheme in both the intersection of core functions and governance and the intersection of all three themes, so it is in the latter section in Figure 1.
Core Public Health Functions
Capacity to perform core public health functions is a key element in public health systems. In both the larger data set and the NPHI-coded data, core public health functions included workforce development, surveillance, laboratory capacity, and emergency preparedness and response activities.
Surveillance uses public health and clinical data to detect disease and report epidemiologic trends. JEE reports recommended implementing Integrated Disease Surveillance and Response (IDSR) 21 or event-based surveillance as methods to improve surveillance capacity, giving examples of NPHI involvement in surveillance and reporting. JEE evaluators lauded Ethiopia’s national surveillance system, housed in the Ethiopia Public Health Institute (EPHI), as a best practice:
“The national surveillance system is accessible to staff in the EPHI. [...] The staff assigned to follow the outbreak situation are responsible for drafting the situation report. Situation reports are shared to decision makers on a daily basis and with partners on a weekly basis.”
Emergency preparedness and response capacity is a country’s ability to prevent, detect, and respond to outbreaks or other public health threats. JEE reports cited the need for the use of tabletop exercises, identification of risks, and creation of Emergency Operating Centers (EOCs) for public health. NPHIs were home to EOCs for several countries in the dataset, including Nigeria:
“[Nigeria Centre for Disease Control (NCDC)] EOC has activated several times and has been an important contributor to the successful control of the several public health emergencies.”
Some NPHIs, such as Mozambique’s, also functioned as homes to national and reference laboratories, bearing responsibility for their responsible for capacity and quality:
“Diagnostic capacity for an increasing number of zoonotic diseases, e.g. trypanosomiasis, Rift Valley Fever, leptospirosis and influenza, is ongoing at the National Institute of Health.”
The larger data set recommended improving training and developmental opportunities, creating career paths for trained public health workforce within all levels of the government, planning for future workforce needs, and ensuring sufficient staffing to strengthening the public health workforce, while NPHI-coded data included the need for trained staff.
Table 2.
Countries and dates of Joint External Evaluations.
| Country | Dates of Joint External Evaluation |
|---|---|
| Botswana | December 2017 |
| Ethiopia | March 2016 |
| Liberia | September 2016 |
| Mozambique | April 2016 |
| Namibia | November-December 2016 |
| Nigeria | June 2017 |
| Rwanda | May 2018 |
| Sierra Leone | October-November 2016 |
| South Africa | November-December 2017 |
| Uganda | June 2017 |
| Zambia | August 2017 |
Table 3.
JEE technical areas included and excluded from the analysis.
| Included in analysis | Excluded from analysis |
|---|---|
| • National legislation, policy and financing | • Antimicrobial resistance |
| • IHR coordination, communication, and advocacy | • Food safety |
| • Zoonotic Disease | • Immunization |
| • Biosafety and biosecurity | • Points of entry |
| • National laboratory system | • Chemical events |
| • Surveillances | • Radiation emergencies |
| • Reporting | |
| • Human resources | |
| • Emergency preparedness | |
| • Emergency response operations | |
| • Linking public health and security authorities | |
| • Medical countermeasures and personnel deployment | |
| • Risk communication |
Governance
National governments, ministries, subnational entities, and NPHIs all had governance responsibilities according to the data. Governments may grant the public health system legal authority by creating, passing, amending, and enforcing policies and legislation that strengthen the public health system. This included policies that bring the country in line with IHR requirements, such as identifying an IHR National Focal Point (NFP) or updating zoonotic disease legislation to align with IHR. A frequently cited priority action or an area that needed strengthening was the creation and passing of legislation relating to NPHIs, either for establishment or providing legal authority to execute key functions, seen in Namibia’s report:
“Plans for a national public health institute need to move forward with a strategy for its organization, finance, and the passage of legislation for its establishment.”
Namibia’s example showed that NPHIs not only relied on the national government to establish the institute, but also had governance responsibilities such as strategizing for operations and financing.
Coordination, Collaboration, and Communication
Discussion of coordination, collaboration, and communication within the public health system without one of the other themes was rare. However, it was still seen individually throughout activities across national ministries and within different levels of government in both the larger data set and NPHI subset. The larger data set also had instances of coordination, collaboration, and communication internationally, regionally, and across different sectors.
Communication with partners, stakeholders, and the public was a key responsibility for actors within the public health system, which included the sharing of information and data. Notably, the data mentioned NFPs and World Organization for Animal Health (OIE) delegates for their role in this and other aspects of coordination, collaboration, and communication. As seen in Nigeria, NFPs are important to the coordination of public health, especially in relation to health securities.
Interlinkages
A critical finding of this analysis was the interdependence of and linkages among the three themes. This was particularly true of the NPHI data subset, where interlinking was seen more frequently than in the larger data set. Data showed overlaps between sets of two themes and all three themes together.
Core Public Health Functions and Governance
Legislative mandates, creating units and teams, deploying and managing resources, and creating standard operating procedures (SOPs) and manuals all existed at the intersection of core functions and governance. A method to operationalize technical capacities in Nigeria was the presence of an NPHI:
“Among the most noteworthy best practices observed in Nigeria is the existence of a national public health institute [Nigeria Centre for Disease Control (NCDC)] that was recently designated as the National IHR Focal Point. This designation further increases the visibility of the IHR, as the NCDC, which currently functions as the centre of Nigeria’s public health infrastructure, is better placed to lead the country’s progress towards full IHR compliance. Additionally, the Integrated Disease Surveillance and Response Guidelines, which were revised in 2013 have been used by the NCDC to conduct surveillance and response activities in the country.”
Figure 1.
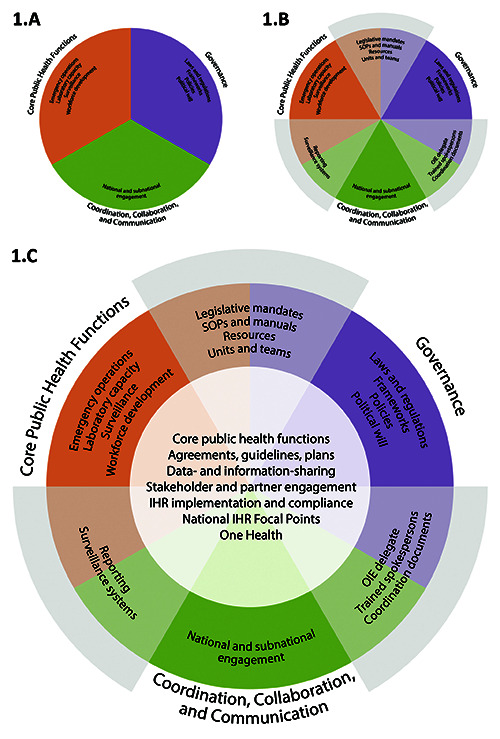
The conceptual map in 1.A-1.C is a stepwise presentation of results, displaying the overlapping subthemes within thematic areas and their interlinkages, as seen in the NPHI subset and larger data set. 1.A presents the three identified thematic areas, 1.B adds the interlinkage of two thematic areas, and 1.C adds the interlinkage of all three thematic areas.
Core Public Health Functions and Coordination, Collaboration, and Communication
Core public health functions featured prominently in the data paired with coordination, collaboration, and communication, such as maintaining surveillance networks and monitoring priority zoonotic diseases. Emergency operations necessitated coordination, collaboration, and communication among stakeholders for risk communications, information-sharing, and responding to events. In addition, the technical areas of deployment of medical countermeasures, biosafety and biosecurity, and reporting relied on coordination, collaboration, and communication amongst various actors and across sectors and core functions. Accordingly, in Ethiopia, they called to:
“Elevate the [Pharmaceuticals Fund and Supply Agency] to the EPHI for nationallevel coordination and mobilization of the medical countermeasures supply chain preand post-public health emergency.”
Coordination, Collaboration, and Communication and Governance
The relationship between governance and coordination, collaboration, and communication was important in establishing agreements (e.g., memoranda of understanding) between stakeholders within a country, between neighboring countries, and across sectors. Data mentioned this in the role that Nigeria CDC plays in response activities. Notably, identified priorities included the existence of guidelines for the roles of IHR NFP in relation to other stakeholders. A lack of standardized documentation for IHR implementation resulted in a call for SOPs.
Core Public Health Functions; Governance; and Coordination, Collaboration, and Communication
Data- and information-sharing, stakeholder and partner engagement, emergency operations, One Health, resource deployment and management, and IDSR depended on all three themes. NPHIs such as the Zambia National Public Health Institute (ZNPHI) exist at this intersection:
“Strengthening of the regional and district laboratories to test for some diseases, involvement of private laboratories in IDSR, increased budget allocation to laboratories by the government and the sustainable commitment of the Government in the establishment and operation of the newly carved out National Public Health Institute.”
The interlinkage of governance; coordination, collaboration, and communication; and core functions were also seen in the production of coordination documents like protocols, SOPs, guidelines, and memoranda of understanding, which provided standards for public health system. These documents regulate the management of resources and relationships as well as ensure the quality of services the public health system provides.
The three themes also intersected in emergency operations, requiring capacity in disease detection, legal authority to begin responses, and the ability to communicate when an emergency is occurring. For example, South Africa’s proposed NPHI will be responsible for the detection and reporting of emergencies:
“[T]here is an urgent need to domesticate the WHO resolutions and hence provide an enabling environment for reporting of potential [public health emergencies of international concern] to WHO. For example, the country has a draft bill on the National Public Health Institute of South Africa (NAPHISA) which addresses reporting to WHO.”
Discussion
NPHIs can serve as a central point in a nation’s public health system by hosting the intersection of the three identified themes, as found in the analysis. Strong, synergistic linkages between core public health functions; governance; and coordination, collaboration, and communication are vital to prevention, detection, and response to public health threats. Establishing an NPHI can improve a country’s ability to respond, increase efficiency, reduce costs, and strengthen core capacities through improved coordination and integration of services.22
Large-scale, international disease outbreaks threatening public health around the world consistently illuminate the need for responsive institutions. Several countries established their NPHIs in just those circumstances, including the Public Health Agency of Canada in 2004 after the SARS outbreak and the National Public Health Institute of Liberia (NPHIL) in 2017 in response to the 2014-2016 Ebola outbreak. 13,14
Many countries have determined NPHIs, or similar institutions, add value even before public health threats occur.12 Colombia’s Instituto Nacional de Salud (INS) has been in operation for over 100 years, with a history of strengthening core functions such as surveillance and emergency preparedness. This allowed the country to quickly respond to the 2016 Zika outbreak and has helped INS become a regional leader in public health.23 The Zambian government realigned some of the core functions of their Ministry of Health to establish ZNPHI, which serves as the country’s center of excellence for public health security. The creation of a public health emergency operations center within ZNPHI allows for greater coordination to respond to public health emergencies and events, including, activating this function to address the cholera outbreak that began in October 2017.24
The presence of NPHIs, such as NPHIL and ZNPHI, throughout Africa supports the five strategic pillars of Africa CDC in its mission to empower its member states to have ownership and responsibility of their populations’ health. The Africa CDC Framework for Development of National Public Health Institutes in Africa serves as a guiding document for the establishment and strengthening of NPHIs throughout the continent and how these institutes can integrate and coordinate the strategic pillars.9 The presence of the core public health functions and key attributes outlined by the Framework (Table 1) became apparent throughout the thematic areas and their interlinkages established during analysis. This underscores the roles that NPHIs can play in strengthening health systems and helping governments achieve IHR compliance.
Core public health functions, as defined by Africa CDC, are “external-facing” NPHI aspects with influences on a country’s population, both individually and societally, and on organizations.9 Seven of the 10 core functions listed in Table 1 were present in the thematic areas and interlinkages of the data, highlighting the roles NPHIs can play in achieving the IHR compliance and global health security. These functions are also present in the themes themselves. Public health laboratory and surveillance systems, and emergency preparedness and response and Public health workforce development are core functions. Meanwhile, Policies and plans that support individual and community health efforts and Health protection and support for regulation and enforcement are roles of governance.9
Key attributes are “internal-facing” and focus on the operationalization of NPHIs.9,10 Similarly, the data had numerous overlaps with seven of the 10 attributes in Table 1. The majority presence of these attributes in the data also suggest that NPHIs, even when not always explicitly mentioned in the data, may have a vital role in the strengthening of the health systems across Africa and their governments’ goal of achieving IHR compliance. Coordination, collaboration, and communication and Linkages at international, national, and subnational levels are analogous concepts while Clearly defined legal authority for its work is akin to the thematic idea of governance and its subtheme of legal mandates.9
Limitations
Utilizing JEE Reports as a data source had limitations. First, the research team was limited to English-language JEEs only as the team did not have translation capacity. Secondly, each JEE represents a specific time in a nation’s public health system, focusing on the time period leading up to and including the conduction of the JEE in a country. Since the conclusion of the JEEs and publication of these reports, some countries have been actively working to address gaps identified during the JEE process (e.g., creating National Action Plan for Health Security). Notably, there are countries included in the study, such as Liberia, that did not have an NPHI at the time of their JEE but have since established one. Thus, the current context and functionalities, such as those of National Public Health Institute of Liberia (NPHIL), are not part of the analysis completed in this study. Lastly, although JEEs do not explicitly address all the functions and attributes of an NPHI identified in the Africa CDC and IANPHI frameworks, such as research in public health, they remain a valuable tool for a majority of those listed.
Conclusions
Individually, each identified theme cannot fulfill all the roles and responsibilities of a national public health system. Merely having technical capacity is insufficient; there is a need to harness these capabilities with governance and coordination, collaboration, communication and channel them toward IHR compliance.9,23 NPHIs, foster linkages and therefore can serve as the focal point for a nation’s public health activities and promote global health security. When these linkages are leveraged effectively, NPHIs have demonstrated success in supporting or leading emergency response activities, including outbreaks of Lassa Fever in Nigeria and cholera in Zambia, and post-cyclone response in Mozambique.24-26
Acknowledgments
The authors would like to thank the NPHI staff from the IANPHI Africa network, who validated the value of this analysis to advancing NPHIs as critical to global health security. These individuals represented the IANPHI member institutes from Ethiopia, Kenya, Mozambique, Nigeria, Sierra Leone, South Africa, Tunisia, and Zambia, as well as the Ministry of Social Services in Namibia. We would also like to show our gratitude to the countries whose reports were used in this study: Botswana, Ethiopia, Liberia, Mozambique, Namibia, Nigeria, Rwanda, Sierra Leone, South Africa, Uganda, and Zambia. This analysis would not have been possible without their contributions. The analysis in this paper was preceded by an effort to utilize JEE report results for discussion about cross-border emergency management capacities in Southern Africa. We thank Julia Klebe and James Banaski for leading that effort.
References
- 1.Flahault A, Wernli D, Zylberman P, Tanner M. From global health security to global health solidarity, security and sustainability. Bull World Health Organ 2016;94:863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Health Security Agenda. About the GHSA, updated 2019. Available from: https://www.ghsagenda.org/about. [Google Scholar]
- 3.The White House Office of the Press Secretary. Fact sheet: the global health security agenda [press release]. July 28, 2015. [Google Scholar]
- 4.Kluge H, Martin-Moreno JM, Emiroglu N, et al. Strengthening global health security by embedding the international health regulations requirements into national health systems. BMJ Glob Health 2018;3:e000656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Joint external evaluation tool: international health regulations (2005), second edition. Geneva: World Health Organization; 2018. [Google Scholar]
- 6.Binder S, Adigun L, Dusenbury C, et al. National public health institutes: contributing to the public good. J Public Health Policy 2008;29:3-21. [DOI] [PubMed] [Google Scholar]
- 7.Koplan JP, Puska P, Jousilahti P, et al. Improving the world's health through national public health institutes. Bull World Health Organ 2005;83:154-7. [PMC free article] [PubMed] [Google Scholar]
- 8.Frieden TR, Koplan JP. Stronger national public health institutes for global health. Lancet 2010;376:1721-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Africa Union. Africa Centres for Disease Control and Prevention. Framework for development of national public health institutes in Africa. Available form: https://africacdc.org/download/framework-for-development-of-national-publichealth-institutes-in-africa/. Accessed: [Google Scholar]
- 10.International Association of National Public Health Institutes. Framework for the creation and development of national public health institutes. International Association of National Public Health Institutes; 2007. [Google Scholar]
- 11.Bloland P, Simone P, Burkholder B, et al. The role of public health institutions in global health system strengthening efforts: the US CDC's perspective. PLoS Med 2012;9:e1001199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heymann DL. NPHIs as focal points for leadership in prevention and control of infectious diseases. J Public Health Policy 2008;29:374-6. [DOI] [PubMed] [Google Scholar]
- 13.International Association of National Public Health Institutes. Public Health Agency of Canada (PHAC); 2007. [Google Scholar]
- 14.International Association of National Public Health Institutes. Liberia's national public health institute is 'now a legal entity' 2016. Available from: http://www.ianphi.org/news/2016/nphil.html. [Google Scholar]
- 15.African Union. Africa Centres for Disease Control and Prevention. Africa Centres for Disease Control and Prevention strategic plan (2017-2021). 2017. [Google Scholar]
- 16.Barzilay EJ, Vandi H, Binder S, et al. Use of the staged development tool for assessing, planning, and measuring progress in the development of national public health institutes. Health Secur 2018;16:S18-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. WHO African region: JEE mission reports Available from: https://www.who.int/ihr/procedures/mission-reports-africa/en/. [Google Scholar]
- 18.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. [Google Scholar]
- 19.Jalma KS. Women’s friendship dissolution: a qualitative study University of Minnesota; 2008. [Google Scholar]
- 20.Syed M, Nelson SC. Guidelines for establishing reliability when coding narrative data. Emerging Adulthood 2015;3.27588221 [Google Scholar]
- 21.Kasolo F, Yoti Z, Bakyaita N, et al. IDSR as a platform for implementing IHR in African countries. Biosecur Bioterror 2013;11:163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nkengasong JN, Maiyegun O, Moeti M. Establishing the Africa Centres for Disease Control and Prevention: responding to Africa's health threats. Lancet Global Health 2017;5. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Colombia’s NPHI keeps the public healthy. Centers for Disease Control and Prevention; 2019. [Google Scholar]
- 24.Mukonka V. Zambia: a regional leader in NPHI development and emergency management. Centers for Disease Control and Prevention; 2018. Available from: https://blogs.cdc.gov/global/2018/08/17/zambia-a-regional-leader-in-nphi/. [Google Scholar]
- 25.Centers for Disease Control and Prevention. National public health institutes: leadership in emergencies. Centers for Disease Control and Prevention; 2018. Available from: https://www.cdc.gov/ globalhealth/stories/nphi-leadership-inemergencies. html. [Google Scholar]
- 26.Centers for Disease Control and Prevention. "A culture of responding:" training course pays off for Mozambique. Centers for Disease Control and Prevention; 2018. Available from: https://www.cdc.gov/globalhealth/healthprotection/nphi/stories/mozambique-training-course.html. [Google Scholar]


