Abstract
Introduction:
The aim of this study was to evaluate conjunctivochalasis (CCH) and its relationship with tear meniscus and tear function in an elderly population.
Materials and methods:
This prospective, observational study included 144 eyes of 144 patients aged >65 years who were referred to our clinic for various reasons. The patients were separated into group 1 including 64 eyes of 64 patients with CCH and group 2 including 80 eyes of 80 patients without CCH. All patients in both groups underwent a full ophthalmological examination, and the presence of CCH, fluorescein tear break-up time (FTBUT) test, Schirmer test, ocular surface staining (Oxford grading score) and OSDI (Ocular Surface Disease Index) test results were recorded. Measurements of the conjunctivochalasis area (CCHA), tear meniscus height (TMH) and tear meniscus area (TMA) were taken using anterior segment optic coherence tomography (AS-OCT).
Results:
Group 1 comprised 34 females and 30 males with a mean age of 71.15 ± 12.34 years. Group 2 comprised 43 females and 37 males with a mean age of 68.16 ± 6.05 years (p = 0.122). The CCH rate was 44.4% in all of the examined patients. The OSDI score and the ocular surface staining test were significantly higher (p < 0.05), and the FTBUT, TMH and TMA were significantly lower (p < 0.05) in group 1 than in group 2. The Schirmer I test results were not significantly different between the two groups.
Conclusion:
The prevalence of CCH is quite high in elderly individuals and may disrupt tear function in these patients.
Keywords: conjunctivochalasis, elderly population, tear meniscus
Introduction
Conjunctivochalasis (CCH) is a common clinical condition characterized by redundant, loose, non-oedematous inferior bulbar conjunctiva interposed between the globe and the lower eyelid causing obliteration of the inferior tear reservoir. It tends to be bilateral and is more prevalent in older populations.1 It can be seen in different areas such as nasal, temporal and central regions of the upper and lower eyelids.2 CCH can cause a number of eye problems ranging from dryness in the early mild stage to disturbance of tear outflow in the moderate stage and exposure problems as it becomes severe.3
Conjunctiva with CCH may cause dry eye, interfering with tear distribution due to the mechanical effect of sliding on the cornea and the disruption of integrity of breakdown of continuity tear meniscus in addition to lacrimal punctum occlusion. Intermittent epiphora, prolongation of tear clearance and an accumulation of inflammatory components on the ocular surface as a consequence of ocular surface disease and conjunctival epithelium changes can be caused by punctum occlusion.4–6 Any inflammation can be improved with the long-term use of protective drops providing symptom relief.4 Long-term changes in the corneal epithelium may cause displacement in the grey line and occlusion of meibomian gland orifices. This process leads to further instability of the tear film, aggravating the symptoms.6
Anterior segment optic coherence tomography (AS-OCT), which provides high-resolution cross-sectional images of anterior segment structures, including the anterior chamber angle, cornea, conjunctiva and tear meniscus, has recently become more widely used.7–9 The uniform distribution of the tear film on the ocular surface is important because the distribution of the tear film in the inferior tear meniscus when blinking ensures good optic quality on the ocular surface.10,11 A reduction in inferior tear meniscus is increasingly prevalent in the diagnosis of dry eye.12 Therefore, the measurement of both tear meniscus height (TMH) and area using AS-OCT is becoming more widespread.13,14 The measurement of tear meniscus area (TMA) is important, as tear distribution may change in CCH. AS-OCT has been reported as an objective means of the measurement of TMA for the diagnosis of CCH.15,16
The aim of this study was to determine TMH, TMA and conjunctivochalasis area (CCHA) values using AS-OCT in an elderly population with CCH and to evaluate the effects on tear function.
Method
The study was conducted in accordance with the principles of the Helsinki Declaration. Approval for the study was granted by the Ethics Committee of Ankara Numune Research and Training Hospital, where the study was carried out (approval number E-18-2097).
This prospective, observational study included 144 eyes of 144 individuals. The patients were divided into two groups according to the presence of CCH. Group 1 included 64 eyes of 64 patients (34 females and 30 males), and group 2 included 80 eyes of 80 patients (43 females and 37 males).
All participants were questioned regarding symptoms of epiphora, pain, burning and itching sensations in the eyes.
The diagnosis of CCH was based on slit lamp examination findings according to the size of the conjunctival folds compared with the height of the normal TMH and number of folds. Grade 0 (no CCH) without persistent fold, grade 1 with a single small fold, grade 2 with two or more folds but not higher than the tear meniscus and grade 3 with multiple folds that are higher than the tear meniscus were evaluated.17
After full ophthalmological examination and OSDI (Ocular Surface Disease Index) test, tear function tests were performed in the following order: the measurement of TMH and TMA, Schirmer I test without anaesthesia, fluorescein tear break-up time (FTBUT) and ocular surface staining. Each evaluation was performed by an experienced and masked physician in the early phase.
The OSDI is a questionnaire of 12 items to evaluate the symptoms of eye-related irritation and the effect on visual acuity. The questionnaire was administered into Turkish by a single doctor (D.O.). The total OSDI score of each patient was calculated as follows: OSDI score = Total score of all answered questions × 100/Total number of questions answered × 4. A total score of ⩾33 was evaluated as severe.18,19
A standard Schirmer’s filter paper strip (Bio Schirmer Strips; Bio-Tech Vision Care Pvt Ltd, Gujarat, India) was applied to the lower third of the lateral bulbar conjunctiva without topical anaesthesia, left for 5 minutes, then the patient was instructed to blink normally. The results were recorded in millimetres (mm).
The FTBUT test was applied with biomicroscope under cobalt blue. Fluorescein was dropped onto the tear film of the patient, who was then told to blink only once. The FTBUT is recorded as the time in seconds from the blink until the appearance of the first break spot in the fluorescein under cobalt blue illumination. The test was repeated for a total of three times, and the average was taken as the result.
The ocular surface staining with fluorescein test was applied to the lower eyelid of the patients. Fluorescein paper diluted with unpreserved artificial tears was placed in the lateral third of the bulbar conjunctiva. Biomicroscopy was evaluated by a single doctor (D.O.) for the fluorescein staining score, and the ocular surface was graded using the Oxford scoring system (grade 0 = absent and grade 5 = the most severe).
Exclusion criteria were any previous ocular surgery, meibomian gland disease which may cause dry eye; inflammatory, autoimmune, haematological or neoplastic disease; diabetes mellitus; or thyroid disease.
Determination of the tear meniscus area and conjunctivochalasis area using anterior segment optic coherence tomography
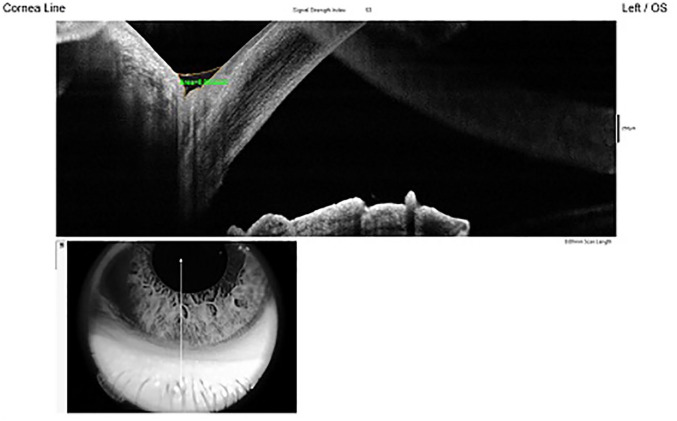
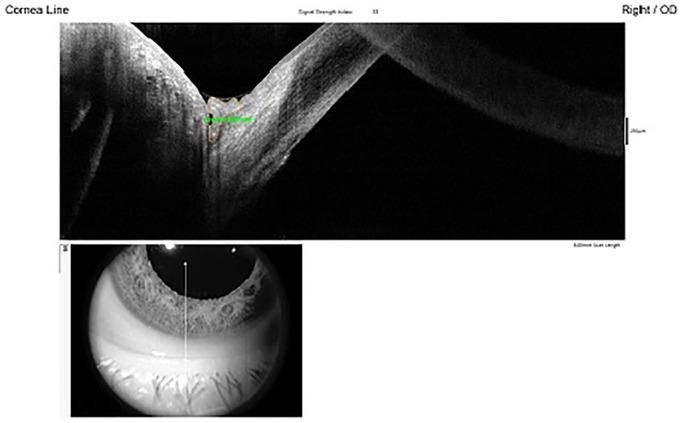
TMA and CCHA measurements were taken using the Fourier-domain OCT (RTVue, software version 2.7; Optovue, Inc., Fremont, CA, USA). This uses a light source with a wavelength of 1310 nm, a high scanning speed of 30 000 A-scans/second and measures 256 B-scans over the cornea, which enables real-time three-dimensional (3D) image acquisition. The Cornea–Anterior Module is additional software on the device, for anterior segment imaging and the measurement of tear meniscus parameters, including TMH, TMA and CCHA. In the current study, the images were taken after connecting the Cornea–Anterior Module lens to the OCT. The lower tear meniscus and conjunctiva in each eye were imaged with vertical scans centred on the inferior cornea and the lower eyelid, and were evaluated each eye with a digital caliper. TMH, TMA and CCHA were defined as the triangular-shaped wedge of tear film between the lower lid margin and ocular surface (cornea/conjunctiva). TMA and CCHA are shown in Figures 1 and 2.
Figure 1.
Tear meniscus area measurement.
Figure 2.
Conjunctivochalasis area measurement.
All measurements of the patients were taken by one individual (D.O.) with three separate evaluations, and the mean of all the measurements was calculated.
Statistical analyses
All data were analysed using Statistical Package for Social Sciences (SPSS, Inc., Chicago, IL, USA) 15.0 program for Windows. Continuous variables were expressed with mean ± standard deviation (SD) and categorical variables with number (n). The independent-samples t test was used in the comparison of the means of the patient and control groups. Pearson correlation analysis was used to determine the relationship between TMA and OSDI, fluorescein tear break-up time (FTBUT), ocular surface staining, Schirmer tests and CCHA parameters. A p value of <0.05 was considered as statistically significant.
Results
In this study, all patients aged >65 years, CCH was determined in 44.4%. Group 1 comprised 34 females and 30 males, and group 2 comprised 43 females and 37 males. Mean age of patients was 71.15 ± 12.34 years in group 1 and 68.16 ± 6.05 years in group 2. There were no significance between two groups in terms of the age distribution (p = 0.122). The mean CCH score was 2.12 ± 0.23 in group 1. Distribution of all the symptoms in both groups is shown in Table 1.
Table 1.
Symptoms of the subjects.
| Group 1 (n = 64) | Group 2 (n = 80) | p | |
|---|---|---|---|
| Epiphora | 16 | 10 | 0.054 |
| Pain | 23 | 17 | 0.103 |
| Burning and itching sensations | 38 | 29 | 0.046* |
| Asymptomatic | 20 | 42 | 0.045* |
Statistically significant, p < 0.05 is recorded as significant.
Group 1 patients were significantly more symptomatic than group 2, and burning and itching sensations were the most frequent symptoms. The results of the tear function tests, nasal temporal, central TMH, TMA and CCHA are shown in Table 2. Significant differences were found between the groups with respect to OSDI, FTBUT, nasal TMH, and central TMA and nasal TMA (p = 0.021, p = 0.041, p = 0.021, p = 0.035 and p = 0.023, respectively; Tables 2 and 3). We selected lowest TMA and highest CCHA for each patient and applied correlation tests. TMA was found to be statistically correlated with age, OSDI score, FTBUT and CCHA (p = 0.046, p = 0.025, p = 0.022 and p = 0.021, respectively). CCHA was found to be statistically correlated with age, OSDI score, FTBUT and TMA (p = 0.031, p = 0.043, p = 0.044 and p = 0.021, respectively; Table 4).
Table 2.
Results of the tear function tests.
| Group 1 | Group 2 | p | |
|---|---|---|---|
| OSDI | 44.13 ± 16.58 | 18.09 ± 9.61 | 0.021* |
| FTBUT | 5.32 ± 4.12 | 12.35 ± 5.16 | 0.041* |
| Ocular surface staining (0–5) | 1.18 ± 0.43 | 0.65 ± 0.32 | 0.185 |
| Schirmer test | 11.25 ± 5.98 | 13.57 ± 2.50 | 0.980 |
OSDI, Ocular Surface Disease Index; FTBUT, fluorescein tear break-up time.
p < 0.05 is recorded as significant.
Table 3.
Measurements of tear meniscus height, tear meniscus area and conjunctivochalasis area.
| Group 1 | Group 2 | p | |
|---|---|---|---|
| TMH (µm) nasal | 221.19 ± 12.41 | 301.26 ± 56.47 | 0.021* |
| TMH (µm) central | 289.19 ± 9.22 | 296.25 ± 15.51 | 0.143 |
| TMH (µm) temporal | 305.28 ± 08.14 | 299.15 ± 18.35 | 0.124 |
| TMA (mm2) nasal | 0.043 ± 0.014 | 0.081 ± 0.026 | 0.023* |
| TMA (mm2) central | 0.051 ± 0.009 | 0.089 ± 0.011 | 0.035* |
| TMA (mm2) temporal | 0.063 ± 0.021 | 0.085 ± 0.038 | 0.121 |
| CCHA (mm2) nasal | 0.28 ± 0.09 | – | |
| CCHA (mm2) central | 0.19 ± 0.10 | – | |
| CCHA (mm2) temporal | 0.17 ± 0.06 | – | |
| LIPCOF grade nasal | 2.12 ± 0.23 | – | |
| LIPCOF grade central | 1.22 ± 0.01 | – | |
| LIPCOF grade temporal | 0.91 ± 0.13 | – |
CCHA, conjunctivochalasis area; TMA, tear meniscus area; TMH, tear meniscus height.
p < 0.05 is recorded as significant.
Table 4.
Correlations of tear meniscus area and conjunctivochalasis area with tear function tests and age in group 1 conjunctivochalasis patients.
| TMA (r) |
CCHA (r) |
|||
|---|---|---|---|---|
| r | p | r | p | |
| Age | −0.610 | 0.046* | 0.678 | 0.031* |
| OSDI score | −0.751 | 0.025* | 0.571 | 0.043* |
| FTBUT (sn) | −0.586 | 0.022* | 0.533 | 0.044* |
| Schirmer I test (mm/5sn) | 0.171 | 0.113 | 0.679 | 0.108 |
| Ocular surface staining | 0.183 | 0.121 | 0.121 | 0.132 |
| CCHA | −0.779 | 0.021* | – | – |
| TMA | – | – | 0.779 | 0.021* |
CCHA, conjunctivochalasis area; FTBUT, fluorescein tear break-up time; OSDI, Ocular Surface Disease Index; TMA, tear meniscus area.
p < 0.05 is recorded as significant.
Discussion
Although CCH is a common condition in clinical practice, particularly in elderly patients, it is usually an overlooked finding. These patients are often treated with artificial tears because they usually present with dry eye symptoms. However, treatment of dry eye is not satisfactory. CCH tends to get ignored, but it should be considered in the differential diagnoses of ocular surface disease and dry eye. In previous studies, CCH frequency has been reported to range between 8.6% and 98.3% in elderly populations.20–22 In the current study of an elderly population, CCH was present in 44.4% of the sample. Diseases such as meibomian gland disease, which are common in the society, and other causes of dry eye were not enrolled in the current study. Thus, our frequency of CCH was lower than previous studies.
It is known that conjunctival flexibility decreases with ageing and this can lead to increased CCH. Ageing is one of the most significant risk factors for the development of CCH.20 In the current study of an elderly population, an increase was determined in the mean CCHA when the TMA was decreased because the protrusion into tear meniscus created by CCH caused blockage and reduced the TMA.
Dry eye symptoms increase with the severity of CCH. Particularly in the middle and nasal regions, the symptoms associated with the punctum occlusion and disruption of tear meniscus are greater in CCH. FTBUT is more important than the Schirmer test in the diagnosis of dry eye in CCH, because the problem is related to the distribution of tears on the ocular surface, and false-positive rates may be high in the Schirmer test because of the prolongation of tear clearance. Dalianis and colleagues23 reported that the mean FTBUT values were 5.5 minutes in all patients and 2.8 minutes in symptomatic ones, and CCH in the temporal region caused symptoms, particularly epiphora. In the current study, FTBUT was significantly decreased in patients with CCH (5.32 ± 4.12 in group 1 and 12.35 ± 5.16 in group 2; p = 0.041). FTBUT decreased when the TMA decreased and the CCHA increased, suggesting that CCH caused a decrease in FTBUT through the disruption of tear distribution and a decrease in the TMA by blocking the tear meniscus.
The TMA and CCHA are distributed variably along the inferior lid margin; thus, TMA and CCHA should be measured in the central nasal and temporal parts of the eyelid. CCH severity can be evaluated using a slit lamp or by AS-OCT. The assessment of the severity of CCH with AS-OCT provides more objective information than biomicroscopic examination.16,20 The measurement of CCHA and TMA with AS-OCT provides more accurate interpretation about the tear function. Measurement of CCHA and TMA with caliper can be reproduced. Thus, these measurements can be taken as an objective criteria for the follow-up and regulation of treatment of patients with CCH.
In the current study, an evaluation was made with the addition of the Cornea–Anterior Module software on the diagnostic device to measure the area of conjunctival protrusion into the TMA in patients. CCH was found at a rate of 44.4% in a sample aged >65 years, and the CCHA was measured as 0.28 ± 0.09 mm2 in the nasal region, 0.15 ± 0.10 mm2 in the central region and 0.17 ± 0.06 mm2 in the temporal region of group 1. The nasal TMA was 0.043 ± 0.014 mm2 in group 1 and 0.081 ± 0.026 mm2 in group 2, and the central TMA was 0.051 ± 0.009 mm2 in group 1 and 0.089 ± 0.011 mm2 in group 2, and the difference was statistically significant (p = 0.023 and p = 0.035, respectively). Previous studies have shown that the TMA is associated with dry eye.10,11 The results of the current study also showed a statistically significant correlation between the TMA and age, OSDI score, and FTBUT (p = 0.046, 0.025 and 0.022, respectively). However, no correlation was found between the TMA and the Schirmer I test and ocular surface staining (p = 0.113 and 0.121, respectively) in group 1. Thus, it was established that CCH disrupted the tear distribution but did not affect the amount of tears.
Limitations
The major limitation of this study was its small sample size. CCH may be treated with surgical procedures when it is refractory to medical treatment. However, none of the patients were examined after surgery. The tear function of the patients after surgery or medical therapy should be evaluated in further studies.
Conclusion
In conclusion, CCH is found at a high rate in the elderly population and it is mostly neglected during ophthalmologic examination. When elderly patients present with complaints such as burning, itching sensations and epiphora, they should be investigated for CCH, and if diagnosed, tear function tests and AS-OCT evaluation of CCH should be performed. CCH evaluation using AS-OCT is a useful method for determining its effect on the TMH and TMA.
Footnotes
Authors’ note: The authors are responsible for the content and writing of the paper.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Dilay Ozek  https://orcid.org/0000-0002-2797-4759
https://orcid.org/0000-0002-2797-4759
Contributor Information
Dilay Ozek, Associate Professor, Department of Ophthalmology, Ankara City Hospital, Dumlupinar Bulvari 364/B D.24 Etimesgut, Ankara, Turkey.
Emine Esra Karaca, Department of Ophthalmology, Ankara City Hospital, Ankara, Turkey.
Ozlem Evren Kemer, Department of Ophthalmology, Ankara City Hospital, Ankara, Turkey.
References
- 1. Hughes WL. Conjunctivochalasis. Am J Ophthalmol 1942; 25: 48–51. [Google Scholar]
- 2. Meller D, Tseng SC. Conjunctivochalasis: literature review and possible pathophysiology. Surv Ophthalmol 1998; 43: 225–232. [DOI] [PubMed] [Google Scholar]
- 3. Di Pascuale M, Espana E, Kawakita T, et al. Clinical characteristics of conjunctivochalasis with or without aqueous tear deficiency. Br J Ophthalmol 2004; 88: 388–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf 2017; 15: 438–510. [DOI] [PubMed] [Google Scholar]
- 5. Huang Y, Sheha H, Tseng SC. Conjunctivochalasis interferes with tear flow from fornix to tear meniscus. Ophthalmology 2013; 120: 1681–1687. [DOI] [PubMed] [Google Scholar]
- 6. Tomlinson A, Bron AJ, Korb DR, et al. The International Workshop on Meibomian Gland Dysfunction: report of the Diagnosis Subcommittee. Invest Ophthalmol Vis Sci 2011; 52: 2006–2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sakata LM, Lavanya R, Friedman DS, et al. Comparison of gonioscopy and anterior segment ocular coherence tomography in detecting angle closure in different quadrants of the anterior chamber angle. Ophthalmology 2008; 115: 769–774. [DOI] [PubMed] [Google Scholar]
- 8. Doors M, Tahzib NG, Eggink FA, et al. Use of anterior segment optical coherence tomography to study corneal changes after collagen cross-linking. Am J Ophthalmol 2009; 148: 844–851. [DOI] [PubMed] [Google Scholar]
- 9. Wang J, Aquavella J, Palakuru J, et al. Repeated measurements of dynamic tear distribution on the ocular surface after instillation of artificial tears. Invest Ophthalmol Vis Sci 2006; 47: 3325–3329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Doane MG. Blinking and the mechanics of the lacrimal drainage system. Ophthalmology 1981; 88: 844–851. [DOI] [PubMed] [Google Scholar]
- 11. Tsubota K, Nakamori K. Effects of ocular surface area and blink rate on tear dynamics. Arch Ophthalmol 1995; 113: 155–158. [DOI] [PubMed] [Google Scholar]
- 12. The definition and classification of dry eye disease: report of the definition and classification subcommittee of the international dry eye workshop. Ocul Surf 2007; 5: 75–92. [DOI] [PubMed] [Google Scholar]
- 13. Ibrahim OM, Dogru M, Takano Y, et al. Application of visante optical coherence tomography tear meniscus height measurement in the diagnosis of dry eye disease. Ophthalmology 2010; 117: 1923–1929. [DOI] [PubMed] [Google Scholar]
- 14. Czajkowski G, Kaluzny BJ, Laudencka A, et al. Tear meniscus measurement by spectral optical coherence tomography. Optom Vis Sci 2012; 89: 336–342. [DOI] [PubMed] [Google Scholar]
- 15. Gumus K, Crockett CH, Pflugfelder SC. Anterior segment optical coherence tomography: a diagnostic instrument for conjunctivochalasis. Am J Ophthalmol 2010; 150: 798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Poh S, Lee R, Gao J, et al. Factors that influence tear meniscus area and conjunctivochalasis: the Singapore Indian eye study. Ophthalmic Epidemiol 2018; 25: 70–78. [DOI] [PubMed] [Google Scholar]
- 17. Höh H, Schirra F, Kienecker C, et al. Lid-parallel conjunctival folds are a sure diagnostic sign of dry eye. Ophthalmologe 1995; 92: 802–808. [PubMed] [Google Scholar]
- 18. Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol 2000; 118: 615–621. [DOI] [PubMed] [Google Scholar]
- 19. Miller KL, Walt JG, Mink DR, et al. Minimal clinically important difference for the Ocular Surface Disease Index. Arch Ophthalmol 2010; 128: 94–101. [DOI] [PubMed] [Google Scholar]
- 20. Mimura T, Yamagami S, Usui T, et al. Changes of conjunctivochalasis with age in a hospital-based study. Am J Ophthalmol 2009; 147: 171–177. [DOI] [PubMed] [Google Scholar]
- 21. Zhang X, Li Q, Zou H, et al. Assessing the severity of conjunctivochalasis in a senile population: a community-based epidemiology study in Shanghai, China. BMC Public Health 2011; 11: 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hashemi H, Rastad H, Emamian MH, et al. Conjunctivochalasis and related factors in an adult population of Iran. Eye Contact Lens 2018; 44(Suppl. 1): S206–S209. [DOI] [PubMed] [Google Scholar]
- 23. Dalianis G, Trivli A, Terzidou C. The location of conjunctivochalasis and its clinical correlation with the severity of dry eye symptoms. Medicines 2018; 5: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]