Abstract
Although pediatricians in Germany work as general practitioners for children, they are planned and trained as medical specialists. In consequence, distances between practices and residences of patients can be very large. The implementation of task-sharing models is a promising option to sustain pediatric outpatient care in rural regions. In this study we assessed the need for and acceptance of delegation of tasks in outpatient pediatric healthcare to non-physician healthcare professionals and developed a task-sharing concept. A standardized questionnaire was developed and addressed a wide range of healthcare professionals. On the basis of the results of the questionnaire and a subsequent workshop involving representatives of the various fields of pediatric care a delegation-concept was developed. A total of 206 questionnaires were answered (response rate: 17%). About 70% of the respondents (n = 145) agreed with the delegation of counseling on prevention, 66% (n = 135) with the delegation of tasks in the transition process into adult medicine. All proposed tasks were conceivable for at least a third of the respondents. Mostly, pediatricians could envision delegation more than the non-physician health care professionals. A three-dimension-delegation-concept was developed: which tasks can be delegated to whom in which setting. Basically, if nurses or medical practice assistants are adequately qualified, all tasks can be delegated to both. The delegation was approved by most of the respondents. Implementation of task-sharing provides a new option to support pediatricians and create better access to outpatient pediatric health care in rural regions. The next step should be the implementation of the delegation concept in pilot projects.
Keywords: task-sharing, pediatrics, concept development, Germany, interprofessional cooperation
What do we already know about this topic?
There is good international experience with interprofessional cooperation.
How does your research contribute to the field?
It is good to carry out research projects on interprofessional collaboration in order to find out if and how it leads to an improvement of health care systems.
What are your research’s implications towards theory, practice, or policy?
It will help to know about the need and acceptance among service providers and to have a concept for interprofessional collaboration when pilot projects are requested and conducted.
Background
The German healthcare system applies separate planning schemes to the different medical specialists in outpatient care. Supply in outpatient healthcare is planned on the basis of ratios of physicians to residents in defined planning regions. These ratios vary for the different medical specializations and also depend on the degree of rurality of the respective region. The planning schemes have 2 main objectives: (1) to provide a sufficient level of outpatient healthcare supply for all residents and (2) to ensure the economic sustainability of the physicians’ practices.1 Pediatricians in outpatient practices have a special position in the healthcare system. Although their main clinical focus is the provision of primary and preventative healthcare for children and adolescents (“general practitioners for children”) they are trained and planned as medical specialists.2 As a result the pediatrician-to-resident ratio is different to the general practitioners (GPs)-to-resident ratio. Since the last revision in 2019, the ratio for larger cities is 2043 under-18-year-olds per pediatrician, as the cities sometimes provide considerable services for the surrounding regions. For other regions, the ratio amounts 2862 under-18-year-olds per pediatrician (a GP is in all regions responsible for approximately 1609 persons all ages).1 This means that in regions with a generally lower population density, more children have to be registered than in the cities so that a pediatrician can settle down.
The Federal State of Mecklenburg-Western Pomerania (M-WP) in the northeast of Germany has large rural areas and the lowest population density in Germany (in average 69 people per km2 (2018)).3 Consequently, in some rural regions in M-WP, both general GPs and pediatricians in outpatient practices are challenged to operate economically and, in these regions, it has become increasingly difficult to recruit young pediatricians to fill pediatric practice vacancies.
In order to develop a sustainable model of outpatient pediatric care and to secure high quality medical care in rural regions, innovative healthcare models have to be developed. One viable option is to integrate cooperation-concepts between physicians and non-physician healthcare professionals in the healthcare system. In several countries, task-sharing between healthcare professionals has long been established practice. An OECD Health Working Paper describes experiences from 12 different OECD-countries (Australia, Belgium, Canada, Cyprus, Czech Republic, Finland, France, Ireland, Japan, Poland, United Kingdom, and United States). Although the development of new nursing roles varies greatly, in these systems nurses often act as the first health care provider, especially in rural areas. Tasks for nurses can include amongst other things assessing, diagnosing, treating and monitoring a variety of health problems; initiating, ordering and interpreting pathology and radiology results; organizing out-of-area transfers for patients requiring complex acute care and providing preventative healthcare and education.4 A Review showed that care delivered by nurses might generate similar or better health outcomes for a broad range of patient conditions compared to care by doctors.5 However, delegation in pediatric care is far more common outside of Germany where it is often adapted or modified for special needs, which may have cultural reasons or may be rooted in the healthcare system.
In Germany, task-sharing between healthcare professionals has been the subject of discussion over the past 2 decades. In the German healthcare system, GPs are responsible for all health care services provided in their practices, even if practice staff with other healthcare professions perform certain tasks.6 GPs can delegate tasks to their staff. Delegation means “assigning specific tasks to qualified health care personnel but remaining responsible and legally accountable for the health care of a patient.”6 In 2008 it became legally possible (with reimbursement since 2009) to delegate medical tasks to qualified non-physician healthcare professionals outside the GP practices (outside of the immediate “communication distance”) in Germany.8 As a result, the delegation of medical tasks to non-physician professionals has become an integrated part of GP outpatient care. Non-physician professionals (mostly medical practice assistants (MPAs) or nurses) conduct home visits to patients with limited mobility, sometimes supported by telemedicine.9-11 The change in law was triggered by the AGnES projects of the University Medicine Greifswald.7-12 After the change in law, several qualifications and curricula emerged to enable the implementation of delegation in outpatient GP practices in routine healthcare.7,13
It is different in outpatient pediatric care. Since 2007, a certified qualification “prevention assistant for medical practice assistants,” qualifies pediatric nurses or comparable health care professionals to carry out prevention services, for example vaccination and counseling, in pediatric outpatient practices within the communication distance. In order to be admitted to the examination, a person must have completed professional training as MPA or nurse with relevant work experience in a GPs or pediatrician’s practice.14 The evaluation of this qualification revealed that delegation of prevention services to “prevention assistants” reduced the pediatricians’ workload.15 Since 2019 the curriculum has been expanded to include the “social pediatric assistant.”14 To ensure the provision of pediatric care in rural regions, delegation in pediatric outpatient health care should be further developed, including outside the communication distance with the physician.
In this study we assessed the need for and acceptance of the delegation of defined tasks in outpatient pediatric healthcare to non-physician healthcare professionals. On the basis of the results, a delegation concept was developed.
Methods
A standardized questionnaire was developed to assess the need for and acceptance of the delegation in outpatient pediatric healthcare to different non-physician healthcare professionals. Three dimensions of delegation were addressed in the questionnaire (see Figure 1):
Figure 1.
Part of the questionnaire, questions about the delegation of pediatricians’ tasks.
- Which tasks (6 specific tasks were included) can be delegated?
- For which degree of clinical acuity (acutely ill, chronically ill, healthy) tasks can be delegated?
- Which health care professions (nurses, midwifes, medical practice assistants, occupational therapists, physiotherapists, other) can overtake delegated tasks?
We addressed a wide range of healthcare professionals working both in in- and outpatient pediatric care facilities: pediatricians, nurses, midwifes, occupational therapists, and physiotherapists, as well as medical practice assistants and other professionals working in pediatric care management, for example, social workers. To evaluate the need for delegation, participants were asked to provide their personal perspective concerning the existence and nature of challenges in the provision of medical care for children and adolescents in their own region. The core of the survey included questions regarding the delegation of 6 defined medical tasks in pediatric care to non-physician health professionals with special training: counseling on health promotion and prevention, supporting the transition-process of chronically ill adolescents, carrying out vaccinations, carrying out parts of regular screenings, case management for children with special needs and triage of acutely ill patients. Three of these tasks (counseling on health promotion and prevention, carrying out vaccinations and case management for children with special needs) were differentiated for 4 age groups (0-to-2-year-olds, 3-to-6-year-olds, 7-to-14-year-olds, and over 14-year-olds). The tasks were chosen on the basis of the results of a prior qualitative analysis of expert interviews.16
The questionnaire also included questions about demographics (age, sex), education, professional, and working context (in- or outpatient, years of experience, team composition, number and age distribution of treated children). The questionnaire was prepared with the software “EvaSys—Electric Paper Evaluationssysteme GmbH Lüneburg, Version 7.0.”
Sets of identical questionnaires were mailed to all outpatient pediatric practices (n = 484: we sent 4 copies to 121 practices), GPs with an additional qualification in pediatrics (n = 112: we sent 4 copies to 28 practices), hospitals with inpatient pediatric departments (n = 300: we sent 20 copies to 15 departments), inpatient rehabilitation clinics offering pediatric care (n = 55: we sent 5 copies to 11 clinics), and intensive care nursing teams (n = 100: we sent 10 copies to 10 teams) in the Federal State of Mecklenburg-Western Pomerania (M-WP). Additionally, we addressed other health professionals working in M-WP: family nurses and midwifes working in families with social or financial problems (Early Aids, “Frühe Hilfen”) (n = 60), nurses working as consultants with families with preterm babies17 (n = 61), a team for pediatric palliative care (n = 6), the medical directors of municipal public health departments (n = 8) and social pediatric centers (n = 3). Furthermore we invited 1 member respectively of: the Association of Statutory Health Insurance Physicians in M-WP (“Kassenärztliche Vereinigung”), the Board of Physicians in M-WP (“Ärztekammer”), the Association of Pediatricians in M-WP (“Berufsverband der Kinder- und Jugendärzte”), the Association of General Practitioners in M-WP (“Hausärzteverband”), the Association of Hospitals in M-WP (“Krankenhausgesellschaft”), the Association for Pediatric Nursing in Germany (“Berufsverband Kinderkrankenpflege in Deutschland”) and a scientist in the field of pediatric nursing to participate in the survey (n = 7).
The data was analyzed using Stata® version 14.2 (Copyright 1985-2015 StataCorp LP, StataCorp 4905 Lakeway Drive College Station, Texas 77845 USA 2015). The responses given as full text entites in the write-in blanks of the standardized questionnaire were categorized by 3 researchers using the software MAXQDA 12 (MAXQDA, VERBI Software—Consult—Sozialforschung GmbH, Berlin) and discussed in the project team.
The results of the standardized survey were used to develop a first draft for the concept for the delegation of tasks in outpatient pediatric healthcare to non-physician healthcare professionals. After conceptualizing the first draft, a workshop was organized where the results of the questionnaire were reported and the first draft of the concept was discussed and developed further in a consensus process.
The study was approved by the ethics committee of the University Medicine Greifswald (Germany) (BB 133/16).
Results
In total, 1196 questionnaires were dispatched. Thereof, 206 (17.2%) were filled out and returned. Four of them had a missing in profession, so we included in this analysis n = 202 questionnaires. On average, the participants were 45 years old (SD 11.2 years). 11,9 % (n = 24) were male. About 30.2% (n = 61) of the participants were pediatricians, and 30.2% (n = 61) of the participants were nurses, thereof n = 52 pediatric nurses and n = 9 general nurses. Other professionals who answered the questionnaire were medical practice assistants (n = 43), midwifes (n = 17) and “other professions” (including eg, social workers, administrative staff, physiotherapists, n = 20). About 55.7% of the nurses, 65.1% of the medical practice assistants, and 76.5% of the midwifes had more than 10 years prior working experience. The demographic and professional-specific characteristics of all participants are given in Table 1.
Table 1.
Characteristics of Participating Healthcare Professionals.
| Pediatricians | Midwifes | Nurses | MPAsa | Other | Total | |
|---|---|---|---|---|---|---|
| Respondents, n (%) | 61 (30.2) | 17 (8.4) | 61 (30.2) | 43, (21.3) | 20 (9.9) | 202 (100) |
| Age (years) | ||||||
| Average (SD) | 48.7 (11.2) | 47.7 (10.5) | 45.4 (9.4) | 40.5 (12.1) | 41.4 (11.5) | 45.1 (11.2) |
| Min/max | 29/76 | 29/66 | 19/62 | 16/62 | 24/62 | 16/76 |
| Missings | 3 | 0 | 1 | 0 | 1 | 5 |
| Gender | ||||||
| Female n (%) | 39 (63.9) | 17 (100) | 56 (91.8) | 39 (90.7) | 15 (75) | 166 (82) |
| Male n (%) | 18 (29.5) | 0 | 1 | 1 | 4 | 24 |
| Missings | 4 | 0 | 4 | 3 | 1 | 12 |
| Level of schooling | ||||||
| 10 years, n (%) | Not askedb | 9 (52.9) | 40 (65.6) | 29 (67.4) | 12 (60) | |
| >10 years, n (%) | 7 (41.2) | 15 (24.6) | 11 (25.6) | 8 (40) | ||
| Missings | 1 | 6 | 3 | 0 | ||
| Work experience (years) | ||||||
| <5 years, n (%) | Not askedc | 1 (6.7) | 17 (27.9) | 11 (25.6) | 9 (45.0) | |
| >5 years, n (%) | 15 (88.3) | 41 (67.2) | 31 (72.1) | 11(55.0) | ||
| Missings | 1 | 3 | 1 | 9 | ||
Medical practice assistants.
Level of schooling of pediatricians always >10 years.
After basic training, the specialist training is at least 6 years.
Some 58% of the participants (n = 117) mentioned problems in the provision of medical care for children and adolescents in M-WP. Problems were perceived by 84% of the pediatricians (n = 51), 65% of midwifes (n = 11), 48% of nurses (n = 29), 39% of medical practice assistants (n = 17), and 45% of the members of “other professions” (n = 9). Mentioned healthcare problems (n = 306) included themes referring to pediatricians like absence of pediatricians (n = 52), absence of pediatric specialists (n = 38), long distances (n = 36), too few pediatricians in rural areas (n = 20), overworked pediatricians (n = 18), recruitment problems for successors in the outpatient praxis (n = 15), long waiting times (n = 14), absence of time/information/consulting (n = 13), and children visiting GPs also in cases they should go to pediatricians (n = 8). Participants also declared problems related to inpatient care (n = 32 entries), the absence of non-physician health professionals like absence of nursing care (n = 11), midwifery (n = 5), and physical therapists (n = 4). As further problems respondents stated a lack of cooperation between healthcare professionals (n = 14), problems with health insurances (n = 9) and problems in non-classical medical ways like problems in social and/or societal field (n = 13) or problems caused by parents (n = 4).
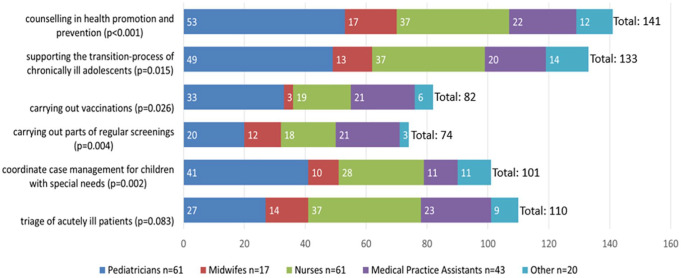
Some 70% (n = 141) of the participants approve of the delegation of counseling on health promotion and prevention to non-physician health professionals. Sixty-six percent of the participants (n = 133) indicated that tasks in the transition process of chronically ill adolescents could be delegated. Fifty-four percent (n = 110) supported the delegation of triage of acutely ill patients, 50% (n = 101) approved case management for children with special needs, 41% (n = 82) carrying out vaccinations, and 37% (n = 74) carrying out parts of regular screenings. Figure 1 shows the approval of different healthcare professionals regarding the delegation of the various tasks by physicians. The proportion of approval of task-delegation among the respondents depended largely on their professions. Pediatricians were more likely to approve of task-delegation than non-physician health professionals (see Figure 2).
Figure 2.
Approval of the delegation of tasks for different healthcare professionals (n = 202), absolute numbers of answers, P-values show significant differences in the response behavior of the different health care professions.
The delegation of counseling on health promotion and prevention, carrying out vaccination, and case management for children with special needs was assessed for different age groups of patients. The pediatricians represented the opinion for all 3 tasks “the older the child, the sooner delegation is imaginable.” Midwifes and nurses could imagine more delegation of counseling on health promotion and prevention if the children are younger. They have rarely confirmed to overtake carrying out vaccination as a delegated task without differences in the age of patients. Like the pediatricians, MPAs could imagine more often carrying out vaccinations the older the children are. Regardless of age midwifes and nurses could imagine themselves delegating the task case management for children with special needs which MPAs were rarely able to imagine. The results are shown in Table 2.
Table 2.
Approval of Different Health Professionals of Delegation to Non-Physician Health Care Professionals by Age Group of Pediatric Patients.
| Task | Age group of pediatric patients (years) | Pediatricians n (%) | Midwifes n (%) | Nurses n (%) | MPAsa n (%) | Other n (%) | Total n (%) |
|---|---|---|---|---|---|---|---|
| Respondents n (%) | 61 (30.2) | 17 (8.4) | 61 (30.2) | 43 (21.3) | 20 (9,9) | 202 (100) | |
| Counseling on health promotion and prevention | 0-2 | 38 (62) | 17 (100) | 31 (51) | 12 (28) | 11 (55) | 109 (54) |
| 3-6 | 43 (70) | 12 (71) | 24 (39) | 17 (40) | 10 (50) | 106 (52) | |
| 7-14 | 44 (72) | 10 (59) | 21 (34) | 17 (40) | 11 (55) | 103 (51) | |
| ≥15 | 45 (74) | 11 (65) | 22 (36) | 15 (35) | 10 (50) | 103 (51) | |
| Carrying out vaccinations | 0-2 | 12 (20) | 3 (18) | 13 (21) | 5 (12) | 1 (5) | 34 (17) |
| 3-6 | 14 (23) | 3 (18) | 14 (23) | 11 (26) | 0 (0) | 42 (21) | |
| 7-14 | 22 (36) | 3 (18) | 14 (23) | 14 (32) | 3 (15) | 56 (28) | |
| ≥15 | 31 (51) | 3 (18) | 14 (23) | 19 (44) | 5 (25) | 72 (36) | |
| Case management for children with special needs | 0-2 | 33 (54) | 9 (53) | 23 (38) | 5 (12) | 7 (35) | 77 (38) |
| 3-6 | 33 (54) | 9 (53) | 20 (33) | 4 (9) | 10 (50) | 76 (38) | |
| 7-14 | 39 (64) | 7 (41) | 22 (36) | 7 (16) | 12 (60) | 87 (43) | |
| ≥15 | 38 (62) | 9 (53) | 20 (33) | 5 (12) | 10 (50) | 82 (41) |
Medical practice assistants.
Those who could imagine the delegation of the defined task were asked about the appropriate health care professions (with appropriate qualification). Nearly 10% of the respondents were not consequent in their answering and crossed in the first step no or no position but chose at least 1 health care profession who could overtake the task. About the delegating group (the pediatricians) we found: more than a half of all participating pediatricians selected for the tasks “counseling on health promotion and prevention,” “supporting the transition-process of chronically ill adolescents,” and “coordinate case management for children with special needs” nurses and midwifes as suitable for task-overtaking. More than a third of all participating pediatricians selected nurses and MPAs for the task “carrying out vaccinations.” For the task “carrying out parts of regular screening” 46.6% of the pediatricians who could imagine these tasks as delegated (n = 21) chose nurses and 85.7% of them chose MPAs as the suitable health care profession. For the task “triage of acutely ill patients” 69.0% of the pediatricians who could imagine these tasks as delegated (n = 29) considered nurses and 62.1% of them considered MPAs as the suitable health care profession. About the task-overtaking professionals we found: midwifes selected for nearly all tasks (except for “carrying out vaccinations”) nearly all proposed health care professions, most frequently themselves. Nurses and MPAs chose for all of the tasks most frequently their own profession as suitable. The results are shown in Table 3.
Table 3.
Profession-Specific Approval of Delegation to Different Non-Physician Health Care Professions
| Task: counseling on health promotion and prevention (only respondents, who chose at least 1 non-physician health care profession, n = 159) | ||||||
|---|---|---|---|---|---|---|
| Pediatricians. . . |
Midwifes. . . |
Nurses. . . |
MPAa. . . |
Other. . . |
||
| n = 55 | n = 17 | n = 39 | n = 32 | n = 16 | ||
| . . .approve delegation to | Midwifes n (%) | 29 (52.7) | 15 (88.2) | 18 (46.2) | 11 (34.4) | 7 (43.8) |
| Nurses n (%) | 38 (69.1) | 7 (41.2) | 35 (89.7) | 12 (37.5) | 8 (50.0) | |
| MPAa n (%) | 42 (76.4) | 10 (58.8) | 16 (41.0) | 19 (59.4) | 6 (37.5) | |
| Ergotherapists n (%) | 17 (30.9) | 10 (58.8) | 12 (30.8) | 3 (9.4) | 6 (37.5) | |
| Physiotherapists n (%) | 15 (27.3) | 9 (52.9) | 12 (30.8) | 2 (6.0) | 7 (43.8) | |
| Other n (%) | 9 (16.4) | 1 (5.9) | 3 (7.7) | 0 | 4 (25.0) | |
| Task: supporting the transition-process of chronically ill adolescents (answered this question and chose at least 1 non-physician health care profession, n = 155) | ||||||
| Pediatricians. . . | Midwifes. . . | Nurses. . . | MPAa. . . | Other. . . | ||
| n = 54 | n = 15 | n = 39 | n = 31 | n = 16 | ||
| . . .approve delegation to | Midwifes n (%) | 9 (16.7) | 10 (66.7) | 9 (23.1) | 1 (3.2) | 3 (18.8) |
| Nurses n (%) | 39 (72.2) | 12 (80.0) | 36 (92.3) | 11 (35.5) | 11 (68.8) | |
| MPAa n (%) | 42 (77.8) | 11 (73.3) | 16 (41.0) | 16 (51.6) | 6 (37.5) | |
| Ergotherapists n (%) | 14 (25.9) | 10 (66.7) | 11 (28.2) | 4 (12.9) | 6 (37.5) | |
| Physiotherapists n (%) | 16 (29.6) | 10 (66.7) | 12 (30.8) | 2 (6.4) | 6 (37.5) | |
| Other n (%) | 3 (5.6) | 1 (6.7) | 4 (10.2) | 1 (3.2) | 4 (25.0) | |
| Task: carrying out vaccinations (answered this question and chose at least 1 non-physician health care profession, n = 102) | ||||||
| Pediatricians. . . | Midwifes. . . | Nurses. . . | MPAa. . . | Other. . . | ||
| n = 35 | n = 3 | n = 22 | n = 32 | n = 10 | ||
| . . .approve delegation to | Midwifes n (%) | 4 (11.4) | 2 | 2 (9.1) | 1 (3.1) | 0 |
| Nurses n (%) | 22 (62.9) | 3 | 18 (81.8) | 9 (28.1) | 3 (30.0) | |
| MPAa n (%) | 23 (65.7) | 2 | 7 (31.8) | 20 (62.5) | 3 (30.0) | |
| Other n (%) | 1 (2.9) | 3 | 1 | 0 | 1 (10.0) | |
| Task: carrying out parts of regular screenings (answered this question and chose at least 1 non-physician health care profession, n = 93) | ||||||
| Pediatricians. . . | Midwifes. . . | Nurses. . . | MPAa. . . | Other. . . | ||
| n = 21 | n = 13 | n = 21 | n = 31 | n = 7 | ||
| . . .approve delegation to | Midwifes n (%) | 6 (28.6) | 11 (84.6) | 8 (38.1) | 5 (16.1) | 0 |
| Nurses n (%) | 10 (47.6) | 3 (23.1) | 16 (76.2) | 8 (25.8) | 2 | |
| MPAa n (%) | 18 (85.7) | 5 (38.5) | 8 (38.1) | 20 (64.5) | 2 | |
| Ergotherapists n (%) | 7 (33.3) | 6 (46.1) | 5 (23.8) | 3 (9.7) | 1 | |
| Physiotherapists n (%) | 6 (28.6) | 6 (46.1) | 6 (28.6) | 1 (3.2) | 2 | |
| Other n (%) | 1 (4.8) | 0 | 2 | 0 | 0 | |
| Task: coordinate case management for children with special needs (answered this question and chose at least 1 non-physician health care profession, n = 127) | ||||||
| Pediatricians. . . | Midwifes. . . | Nurses. . . | MPAa. . . | Other. . . | ||
| n = 45 | n = 11 | n = 31 | n = 24 | n = 16 | ||
| . . .approve delegation to | Midwifes n (%) | 9 (20.0) | 7 (63.6) | 7 (22.6) | 3 (12.5) | 3 (18.8) |
| Nurses n (%) | 33 (73.3) | 5 (45.4) | 27 (87.1) | 9 (37.5) | 8 (50.0) | |
| MPAa n (%) | 33 (73.3) | 8 (72.7) | 11 (35.5) | 11 (45.8) | 6 (37.5) | |
| Ergotherapists n (%) | 5 (11.1) | 4 (36.4) | 3 (9.7) | 1 (4.2) | 3 (18.8) | |
| Physiotherapists n (%) | 4 (8.9) | 4 (36.4) | 4 (12.9) | 2 (8.3) | 2 (12.5) | |
| Other n (%) | 4 (8.9) | 0 | 3 (9.7) | 0 | 2 (12.5) | |
| Task: triage of acutely ill patients (answered this question and chose at least 1 non-physician health care profession, n = 133) | ||||||
| Pediatricians. . . | Midwifes. . . | Nurses. . . | MPAa. . . | Other. . . | ||
| n = 29 | n = 14 | n = 41 | n = 35 | n = 14 | ||
| . . .approve delegation to | Midwifes n (%) | 13 (44.8) | 13 (92.9) | 13 | 4 (11.4) | 4 (28.6) |
| Nurses n (%) | 20 (69.0) | 10 (71.4) | 34 | 15 (42.9) | 8 (57.1) | |
| MPAa n (%) | 18 (62.1) | 12 (85.7) | 17 | 21 (60.0) | 5 (35.7) | |
| Other n (%) | 2 (6.9) | 2 | 0 | 0 | ||
Medical practice assistants.
Based on the results of the standardized questionnaire, a first draft of a concept for the delegation of physician tasks in outpatient pediatric healthcare was developed. In this first draft, one dimension was defined. This first dimension “Which physician tasks can be delegated—differentiated by agegroups of patients” based on the answers of the delegating profession, the pediatricians. More than a half could imagine to delegate counseling, supporting the transition process, case-manangement, and carrying out vaccinations. Almost half of the participating doctors could imagine triage, at least a third can also imagine to delegate parts of early detection examinations.
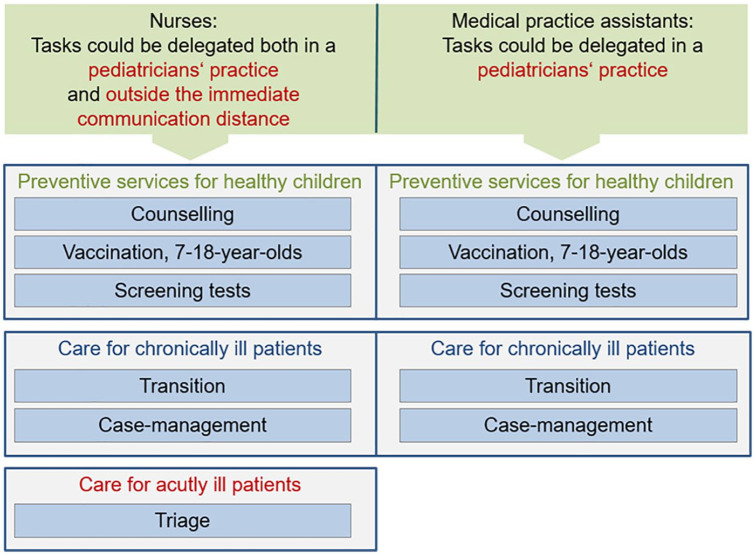
The subsequent workshop was conducted with 9 representatives of various fields of pediatric care (outpatient pediatricians, pediatric nurses, coordinator of midwifes, coordinator of social pediatric care, 2 nurses with different special qualifications as family and pediatric nurse). In the workshop, the results of the questionnaire were reported and the first draft of the delegation concept was discussed and developed further in a consensus process. Further dimensions were added: “To whom tasks can be delegated.” The results of the questionnaire were very heterogeneous, so that only the discussion showed, that the best professions would be nurses and MPAs. The participants in the workshop agreed that the education and training status is decisive for the delegation of tasks. In principle, professional experience of at least 5 years should be required. Nurses and MPAs must be participants in the pediatric training offered by the Medical Association. Contents and further minimum standards in education and training must be specified, if possible using already developed and approved educational modules in this area. A third dimension was called “For which degree of clinical acuity tasks can be delegated.” Therefore, a distinction was made between nurses and MPAs due to different vocational/professional education-contents. The same distinction was made for a new aspect of delegation we added: “Which degree of autonomy can be given to the non-physician healthcare professionals (inside the pediatricians’ practice or outside).”
Figure 3 depicts the resulting delegation concept for outpatient pediatric healthcare. All dimensions were maintained. The first dimension consists of the 6 defined tasks and is grouped in 3 categories of children: healthy children for prevention (relevant for all children), chronically ill children and acutely ill children, sometimes for different age-groups. The second dimension is the adopting profession. As a result of the workshop, midwifes were excluded from the concept as their experience and education is limited to very young children. Basically, all tasks can be delegated both to nurses and to MPAs. The third dimension of the delegation concept is the setting (delegation within or outside the pediatric practice). The biggest impact for delegation in rural regions can be achieved if delegation takes place outside the pediatricians’ practices. Nurses can conduct all delegation tasks outside the pediatricians’ practice, for example, in a branch practice or in a cooperating GP-practice. Due to the lower level of education of medical practice assistants compared to nurses, they should perform delegated tasks predominantly within the pediatricians’ practice.
Figure 3.
Concept of delegation of physician tasks to non-physician healthcare professionals in outpatient pediatric practices for nurses and medical practice assistants.
Discussion
The results of the survey among professionals in pediatric healthcare showed considerable agreement with respect to problems in the assurance of outpatient pediatric care in rural regions and that there is a need for innovative options in pediatric healthcare. Among the possibilities for task-sharing in outpatient pediatric healthcare we found the greatest acceptance for the tasks “counseling on health promotion and prevention” and “supporting the transition-process of chronically ill adolescents.” Both the delegating physicians as well as specific health care professions could imagine task-sharing in form of delegation. More than a half of the pediatricians could imagine triage of acutely ill patients for nurses and MPAs but not for midwifes while non-physicians could imagine mostly for themselves (midwifes, nurses, and MPAs) but not often for other non-physicians. Delegating of the case management for children with special needs could imagine more than a half of the pediatricians, more than a third from them for midwifes and nurses and less than a third for MPAs. Carrying out vaccinations and regular screenings was relatively rarely imaginable for pediatricians, a little more common among the nurses and MPAs.
Although among the responding midwifes delegation was often quite imaginable and they were also relatively often selected as a task-taking group they were excluded from the concept due to the workshop. They have had often positive attitudes in the questionnaire, even without large age group differences. However, the representative of the professional group made the restriction on the limited experience for older children, which was confirmed by the pediatricians in the workshop.
Literature reviews of the roles of healthcare professionals in various countries revealed a large variation in the development of new roles.4 A 1973 study in North California showed that there was a relevant demand for nurse practitioners who could overtake some tasks from the medical doctors.18 Nurse practitioners are academically qualified nurses with broad competences, which do not presently exist in Germany. In the North Carolina study only physicians were asked for their opinion. More openness towards task-sharing was found if physicians have had experience in cooperation with nurse practitioners. Altschuler et al. showed in 2012 in California that more patients can be treated in primary care practices if parts of preventive and chronic care services are delegated to non-physician practice staff.19 Meanwhile sharing some physicians’ tasks with nurse practitioners has been widely adopted in the USA. In the Netherlands a study was conducted to examine the feasibility and impact of task delegation to nurses in pediatric care. This study showed a high approval for the delegation of regular screening examinations.20 In our analysis, this task had the lowest acceptance among all health professionals.
Our analysis revealed a heterogeneity of perceptions of delegating tasks to non-physician healthcare professionals. A majority of the delegating profession, the pediatricians, approves of the delegation of specified tasks and indicated most often nurses and medical practice assistants as suitable professions to overtake these tasks. Nurses and medical practice assistants both assess their own profession often as more suitable than the other ones for most of the evaluated tasks. This may be partly attributable to a lack of awareness of the qualification, experience and daily tasks of the respective other professions. However, the biggest impact for delegation in rural regions will be achieved if delegation takes place outside the pediatricians’ practices.
A particular emphasis should be put on triage. On the one hand, triage is a task that non-physician healthcare professionals can do in delegation as a planned task. On the other hand, if non-physician healthcare professionals work in delegation outside the immediate communication distance of the pediatrician, unexpected situations with respect to the health situation of patients can occur. This makes nurses more appropriate due to their stronger medical training background. Healthcare professionals who take over tasks in delegation always need to have the competence to react appropriately and to manage such situations.
A limitation of this investigation is the low response rate. As a consequence the results may be not fully representative for the whole group of all professionals in pediatrics.
A strength of the study is that all relevant professions (pediatricians, nurses, midwifes, medical practice assistants, occupational therapists, physiotherapists, other) were asked, since children often need interprofessional care. Additionally representatives of the major medical and professional institutions were invited. Another strength is the combination of a standardized assessment with a consecutive expert workshop as the basis for the development of a delegation concept. This 2 step approach makes the concept more suitable for the implementation in a healthcare setting. Additionally to the survey described here, a survey among parents of kindergarten-children was published. This survey showed, that parents in rural regions have a high acceptance of delegation in outpatient pediatric care.21
Conclusion
We developed a comprehensive concept for the delegation of physician tasks to non-physician healthcare professionals in outpatient pediatric practices in rural regions. The implementation of this concept will support pediatricians in outpatient practices and improves patients’ access to outpatient pediatric health care in rural regions. The next step should be the implementation of the delegation concept in pilot projects to explore effects on healthcare providers and patients and to assess barriers and promoting factors for a broader regional implementation.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was financially supported by the Federal Ministry of Economics, Employment and Health Mecklenburg-Vorpommern. The Ministry was not involved in the publication.
ORCID iD: Angelika Beyer  https://orcid.org/0000-0003-4654-4233
https://orcid.org/0000-0003-4654-4233
References
- 1. Kassenärztliche Bundesvereinigung. Die Bedarfsplanung Grundlagen, Instrumente und Umsetzung (Stand Januar 2020). 2019. Homepage der Kassenärztlichen Bundesvereinigung; http://www.kbv.de/html/bedarfsplanung.php Accessed May 15 2020. [Google Scholar]
- 2. Fegeler U, Jäger-Roman E, Martin R, Nentwich HJ. Ambulante allgemeinpädiatrische Grundversorgung. Monatsschr Kin-derheilkd. 2014;162(12):1117-1130. [Google Scholar]
- 3. Statista. Bevölkerungsdichte (Einwohner je km2) in Deutschland nach Bundesländern zum 31. Dezember 2019. https://de.statista.com/statistik/daten/studie/1242/umfrage/bevoelkerungsdichte-in-deutschland-nach-bundeslaendern/ Accessed August 5 2019.
- 4. Delamaire M, Lafortune G. Nurses in Advanced Roles. OECD Publishing; 2010. [Google Scholar]
- 5. Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 2018;2018(7): 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mergenthal K, Beyer M, Gerlach FM, Guethlin C. Sharing responsibilities within the general practice team - a cross-sectional study of task delegation in Germany. PLoS One 2016; 11(6): e0157248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rieser S. Bitte mehr von Eva, Verah, Agnes. Dtsch Arztebl. 2013;110(45):C1818-C1819. [Google Scholar]
- 8. Ruppel T, van den Berg N, Hoffmann W. Legal analysis of the implementation rules of delegation of home visits by family doctors to non-physician health professionals: is the implementation in accordance with the intention of the law? Gesundheitswesen. 2016;78(10):622-627. [DOI] [PubMed] [Google Scholar]
- 9. Schmiedhofer MH, Brandner S, Kuhlmey A. Delegation of medical treatment to non-physician health care professionals: the medical care structure agneszwei in Brandenburg - a qualitative acceptance analysis. Gesundheitswesen. 2015;79(6):453-460. [DOI] [PubMed] [Google Scholar]
- 10. van den Berg N, Fiß T, Meinke C, Heymann R, Scriba S, Hoffmann W. GP-support by means of AGnES-practice assistants and the use of telecare devices in a sparsely populated region in Northern Germany–proof of concept. BMC Fam Pract. 2009;10:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kleinke S, Heymann R, Oppermann RF, Jakobi B, Hoffmann W. Transfer of the AGnES concept to the regular German health-care system: legal evaluation, reimbursement, qualification. Gesundheitswesen. 2010;72(5):285-292. [DOI] [PubMed] [Google Scholar]
- 12. van den Berg N, Meinke C, Matzke M, Heymann R, Fleßa S, Hoffmann W. Delegation of GP-home visits to qualified practice assistants: assessment of economic effects in an ambulatory healthcare centre. BMC Health Serv Res. 2010;10:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Institut für hausärztliche Fortbildung im Deutschen Haus-ärzteverband (IHF) e.V., Fortbildungen MFA. 2020. Hausärz-teverband; https://www.ihf-fobi.de/fortbildungen-mfa/verah/fortbildung.html Accessed August 12 2020. [Google Scholar]
- 14. DAPG e.V. 2020. https://www.dapg.info/ Accessed August 15 2020.
- 15. Schoierer J, Lob-Corzilius T, Wermuth I, Nowak D, Böse-O’Reilly S. Does the prevention act improve prevention in pediatric outpatient settings!? Gesundheitswesen 2017;79(3):174-178. [DOI] [PubMed] [Google Scholar]
- 16. van den Berg N, et al. Kurzbericht: Versorgungsepidemiologische Analyse der medizinischen Kinder- und Jugendversorgung in Deutschland (Expertise im Auftrag des DAKJ e.V. - 2016). 2016. Homepage des Bundesgesundheitsministeriums; https://www.bundesgesundheitsministerium.de/themen/praevention/kindergesundheit/kindergesundheit.html#c3149 Accessed July 27 2020. [Google Scholar]
- 17. GKV-Spitzenverband. Sozialmedizinische Nachsorge. https://www.gkv-spitzenverband.de/krankenversicherung/rehabilitation/sozialmedizinische_nachsorge/sozialmedizinische_nachsorge.jsp Accessed 31 January 2017.
- 18. Lawrence RS, DeFriese GH, Putnam SM, Pickard CG, Cyr AB, Whiteside SW. Physician receptivity to nurse practitioners: a study of the correlates of the delegation of clinical responsibility. Med Care. 1977;15(4):298-310. [DOI] [PubMed] [Google Scholar]
- 19. Altschuler J, Margolius D, Bodenheimer T, Grumbach K. Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. Ann Fam Med. 2012;10(5):396-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Benjamins SJ, Damen ML, Van Stel HF. Feasibility and impact of doctor-nurse task delegation in preventive child health care in the Netherlands, a controlled before-after study. PLoS One. 2015;10(10):e0139187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Beyer A, Stentzel U, Hoffmann W, van den Berg N. Attitude of parents towards pediatric care and interprofessional task-sharing in regions distant versus close to care facilities: results of a standardized survey. Gesundheitswesen. Published online September 4, 2020. doi: 10.1055/a-1192-4840 [DOI] [PubMed] [Google Scholar]