Abstract
Introduction
Microprocessor knee analyses to date have been primarily limited to microprocessor knees as a category rather than comparisons across different models. The purpose of the current analysis was to compare outcomes from four common knee models.
Methods
A retrospective analysis of clinical outcomes was performed. Outcomes for functional mobility, quality of life, satisfaction with amputee status, and injurious falls were compared. Specific knee types represented were C-Leg (Ottobock), Orion (Blatchford), Plié (Freedom Innovations), and Rheo (Össur).
Results
Outcomes from 602 individuals were included. No significant differences were noted for functional mobility (H = 2.91, p = 0.406) or satisfaction (H = 4.43, p = 0.219). For quality of life, differences existed for C-Leg versus Plié (p = 0.010). For injurious falls, C-Leg (χ2(1,137) = 10.99, p < 0.001) and Orion (χ2(1,119) = 4.34, p = 0.037) resulted in significantly reduced injurious falls compared to non-microprocessor knee users. C-Leg (H = 19.63, p < 0.001) and Plié (H = 14.04, p = 0.003) users saw declines with advanced aging.
Conclusions
Our data indicate relative parity among the 4 microprocessor knees with regard to functional mobility and satisfaction. In contrast to mobility, neither satisfaction nor quality of life values reflected declines with aging. Finally, when compared to non-microprocessor knees, significant differences were observed across the microprocessor knee types in relation to the reduction of injurious falls.
Keywords: MPK, mobility, quality of life, falls, amputee, outcomes
Introduction
Having been the subject of numerous systematic reviews and practice guidelines, microprocessor knees (MPKs) are among the most studied components in prosthetic rehabilitation.1–8 This scrutiny has coalesced into a set of reasonably expected benefits associated with the use of MPKs included as part of a clinical practice guideline.1 These include reductions in self-reported stumbles, falls and associated frustrations, reductions in the reported cognitive demands associated with prosthetic ambulation, increases in self-reported confidence while walking, mobility, satisfaction, well-being and quality of life and increases in self-selected walking speeds on both level and uneven terrain.1 Unfortunately, the available data is unable to provide guidance as to prescription basis for differing MPK types.
Lack of understanding across different knees
The majority of the studies from which both systematic reviews and practice guidelines have been produced have reported upon the impacts of the C-Leg (Ottobock, Dudderstadt, Germany), and to a limited extent the Rheo (Össur, Reykjavík, Iceland), in comparison to non-microprocessor knees (nMPK). Providing clinical guidance is challenging given the different models of MPKs available, as well as the different target demographics for MPKs versus nMPKs. For example, Medicare does not cover MPK use for individuals classified as K2, subsequently leading to many patients at K2 and K1 ambulatory level being prescribed nMPK. Such payor guidelines however do not extend into specific knee types.
There are a number of MPKs that utilize one or more microprocessors to dynamically adapt their functionality during gait with substantial differences in their underlying algorithms and physical response mechanisms.9,10 For example, the C-Leg (Ottobock, Dudderstadt, Germany) relies entirely on hydraulic pistons to control knee flexion and extension,9,11 while the Orion (Blatchford Group, Basingstoke, Hampshire, United Kingdom) and Plié (Freedom Innovations, Irvine, California, United States) utilize varying combinations of hydraulics and pneumatics to achieve controlled knee flexion and extension.9,11 The Rheo (Össur, Reykjavík, Iceland), on the other hand, relies on an entirely different mechanical control system incorporating a magnetorheological fluid chamber to control knee flexion and extension.9
The ability of MPKs beyond the C-Leg to help patients realize the anticipated benefits associated with an MPK has been comparatively understudied.12–16 Recently published evidence has suggested that some MPK alternatives to the C-Leg have failed to consistently provide the benefits frequently associated with MPKs such as reduced stumbles and falls, reduced mental exertion during ambulation, and increased self-reported mobility and physical function.14,15 Other frequently utilized MPKs, such as the Plié (Freedom Innovations, Irvine, California, United States) and the Orion (Blatchford Group, Basingstoke, Hampshire, United Kingdom) received limited consideration in recent literature.9,11,17 Analyses comparing different MPKs are infrequent, and when they have occurred, they are generally short-term observations on small study cohorts that carry a risk of actual or perceived bias due to direct manufacturer funding and publication.9,10,12
Lack of understanding across varying ages
In additions to variations in MPK type, the available evidence suggests that some constructs of interest among MPK users appear to be more resilient to aging than others. Values for prosthetic mobility, for example, may decline slightly with aging.14,18–22 However, these trends may be confounded by MPK type in the various clinical studies. By contrast, satisfaction and quality of life among MPK users may be more stable across population ages.14,16,18,23,24 It is unclear however whether the available data is confounded by different MPK types. Indeed, there is a lack of understanding how the effect of aging on various prosthetic outcomes is mitigated by MPK models.
Thus, the purpose of the current analysis was to analyze prosthetic mobility, satisfaction with amputee status, quality of life, and injurious falls among large cohorts using different types of MPKs without any potential bias or influence from manufacturer funding or publication input. Focus was placed on the four most frequently utilized MPKs in the United States through a retrospective analysis of real-world patient outcomes. In addition to differences across MPKs, differences were examined across multiple age groups to identify any aging related trends in outcomes by MPK type. It was first hypothesized that differences in prosthetic outcomes would be seen across the specific MPK models. Although it is believe that the different underlying mechanical function (i.e. different control algorithms, sensors, actuators, fluid mediums, processor speeds, etc.) may contribute to any differences, there is insufficient understanding of how the nervous system interacts with different mechanically imposed prosthetic interactions, subsequently limiting hypothesis specificity at this stage. But, it would be expected that the results from this study may direct future work to discern the link between mechanisms and outcomes. Second, while differences in prosthetic outcomes were expected across MPK types, it was hypothesized that similar age-related changes would be seen in the specific MPK models.
Methods
Study design
A retrospective analysis of outcomes collected in clinic was performed. Outcomes are being collected as part of routine care within multiple clinics across continental United States. The current analysis utilized the unilateral AKA outcomes database with data collected from April 2016 through April 2020. The current analysis was approved and deemed exempt from patient consent by Western Investigational Review Board (Protocol #20170059). This study conforms to all STROBE guidelines.
Microprocessor knees
The current analysis focused on four different knee units. Within the continental United States, there are four primary MPKs that are provided. Users wearing the C-Leg (Ottobock, Dudderstadt, Germany), the Orion (Blatchford Group, Basingstoke, Hampshire, United Kingdom), Plié (Freedom Innovations, Irvine, California, United States), or the Rheo (Össur, Reykjavik, Iceland) were considered for the current analysis.
Participants
For an individual to be included in the analysis, they needed to be age 18 or older, currently using a prosthesis, and able to read, write, and understand English or Spanish. These inclusion criteria were consistent with at least one endpoint outcome measure.25 Additionally, individuals must have received one of the noted MPK models prior to the outcomes assessment, and the outcomes assessment must have been within the warranty period for the MPK knees to ensure highest likelihood individuals were still on that specific knee unit. For falls analysis, for reasons noted below, the additional restriction on inclusion was placed such that individuals must have received the noted MPK model 6 months or more prior to the outcomes assessment. Individuals were excluded if they were considered either K1 or K2 ambulator status and therefore noted as K3 or above functional ambulator.26
Procedure
As part of their routine prosthetic care, patients were asked to complete a self-report survey outcomes packet. Within the outcomes survey packet, there are questions comprising the 12-item Prosthetic Limb Users Survey of Mobility (PLUS-M).25,27 The 12-item PLUS-M survey asks patients 12 questions surrounding the construct of functional mobility with 5 response options including: 1) Unable to do, 2) With much difficulty, 3) With some difficulty, 4) With a little difficulty, and 5) Without any difficulty. The responses to the 12-items are then summed and this raw score is converted to a T-score.
In addition to functional mobility, individuals are also asked the Prosthesis Evaluation Questionnaire (PEQ) Well-being survey. The survey comprises questions to give information on outcomes of health state satisfaction and quality of life. Although originally administered as a continuous visual analog scale, the instrument has subsequently been administered as a discrete scale to ease clinical use with regards to patient administration and survey scoring.18,28 The current assessments implement questions on a discrete scale of 1–10, with a value of 1 being “worst possible life” (quality of life) or “extremely dissatisfied” (health state satisfaction), and a value of 10 being “best possible life” (quality of life) or “extremely satisfied” (health state satisfaction).
Finally, the outcomes assessment includes a question to record history of falls. At the initiation of routine outcomes collection within the clinics, it was decided to anchor the fall question to a traumatic event as opposed to inquiring only about general falls. The question, “Have you had a fall in the previous 6 months that resulted in a hospital or physician visit?” allows for a single binary response. By anchoring the fall recall to a traumatic event there is enhanced patient recall.29 This is believed to reduce recall bias and the associated error but comes with the limitation that it undervalues the impact of falls that do not necessarily elevate to the level of seeking medical attention. The 6-month window associated with the fall question necessitated further inclusion restriction on the injurious falls analysis as noted above.
In order to further understand the differences in the MPK types with regards to falls, the percentage of fallers within each category of MPK was compared to a benchmark population percentage drawn from the literature. Previous literature has reported injurious falls among community dwelling lower limb prosthesis users to range between 19% and 27% over time frames of 18 and 12 months respectively.30,31 More recent work on a larger cohort of patients with transfemoral amputation due to diabetes or vascular disease reported similar percentage at 16.3% over a shorter time window of only 6 months.32 Due to the consistent methodology and time window of 6 months among a nMPK only cohort, 16.3% was chosen as the population benchmark for comparison of MPK performance in the current analysis.
It was understood a priori that the Rheo knee unit would have the least number of patients. As such, while the Rheo knee users would be included in analysis, the decision was made to instead match group sizes based on the lowest number of units of either the C-Leg, Orion, or Plie. Once this group was identified, an equivalent number of users from the remaining 2 groups would be randomly selected. Random selection was done through the randperm random number generator function within Matlab® (v2019b). This then created the 3 groups from the C-Leg, Orion, and Plie which would then be combined with Rheo. In this manner, it provided a random sample of all individuals using the knee units. This process was repeated 9 more times to confirm consistent findings across randomly chosen groups. Within MPK groups, individuals were subsequently broken down into age groupings based on those previously published by PLUS-M33 (i.e. under 35, 35-49, 50-64, 65 and older) to allow secondary analysis of age.
Demographic data was compiled for all four knee units to understand potential differences in prescribing patterns based on patient phenotypes. Based on non-normality of the data, interval data (i.e. PLUS-M, satisfaction and quality of life) was compared using Kruskal-Wallis H tests. Categorical data (i.e. injurious fall status) was compared using a Chi-Square test. In the event of any factor level significant differences, a Bonferroni correction was applied for post-hoc pairwise comparisons with adjusted p-values subsequently presented.
Results
There were a total of 602 participants that were ultimately included for analysis. This included 68 Rheo users, and then 178 each of C-Leg, Orion, and Plié users (Table 1). Among users of the C-leg, Plie and Rheo, vascular disease/diabetes was the most common amputation etiology specified. Individuals with C-Leg were of the oldest median age. Height stature was fairly consistent across the Orion, Plié, and Rheo, while C-Leg users were slightly shorter. The heaviest median weight group was the Plié. Plié users also comprised of the highest percentage of females. C-Leg followed by Rheo had the highest percentage of users that reported no assistive devices. Rheo users comprised the highest percentage of employed individuals.
Table 1.
Descriptive data for individuals using different microprocessor knees.
| Microprocessor Knee | C-Leg | Orion | Plie | Rheo |
|---|---|---|---|---|
| Age, median (y) [IQR] | 61.23 [48.78,68.11] | 57.97 [46.15,67.74] | 56.95 [46.76,65.27] | 58.63 [44.67,66.22] |
| Height, median (cm) [IQR] | 172.72 [165.10,180.34] | 175.26 [170.18,182.88] | 175.26 [167.64,182.88] | 175.26 [167.64,180.34] |
| Weight, median (kg) [IQR] | 80.79 [68.48,92.97] | 81.63 [69.95,93.76] | 83.90 [72.56,99.55] | 81.63 [70.86,95.01] |
| Female (%) | 44 (24.72%) | 37 (20.79%) | 56 (31.46%) | 17 (25.00%) |
| Assistive device | ||||
| None | 83 (46.63%) | 59 (33.15%) | 67 (37.64%) | 30 (44.12%) |
| Cane | 44 (24.72%) | 44 (24.72%) | 37 (20.79%) | 18 (26.47%) |
| Crutches | 25 (14.04%) | 34 (19.10%) | 45 (25.28%) | 11 (16.18%) |
| Walker | 19 (10.67%) | 19 (10.67%) | 19 (10.67%) | 4 (5.88%) |
| Forearm crutches | 6 (3.37%) | 13 (7.30%) | 9 (5.06%) | 4 (5.88%) |
| Unspecified | 1 (0.56%) | 9 (5.06%) | 1 (0.56%) | 1 (1.47%) |
| Cause of amputation | ||||
| Vascular/diabetes | 53 (29.78%) | 45 (25.28%) | 57 (32.02%) | 22 (32.35%) |
| Non-vascular/diabetes | 46 (25.84%) | 47 (26.40%) | 37 (20.79%) | 16 (23.53%) |
| Unspecified | 79 (44.38%) | 86 (48.31%) | 84 (47.19%) | 30 (44.12%) |
| Employed (%) | 43 (24.16%) | 50 (28.09%) | 55 (30.90%) | 22 (32.35%) |
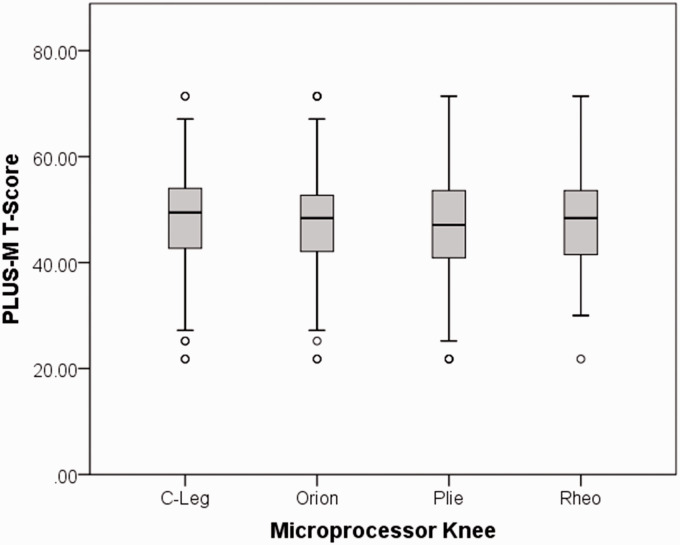
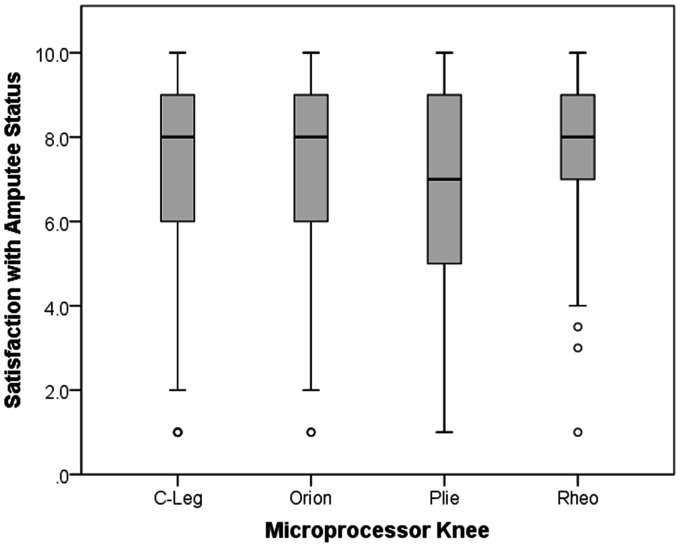
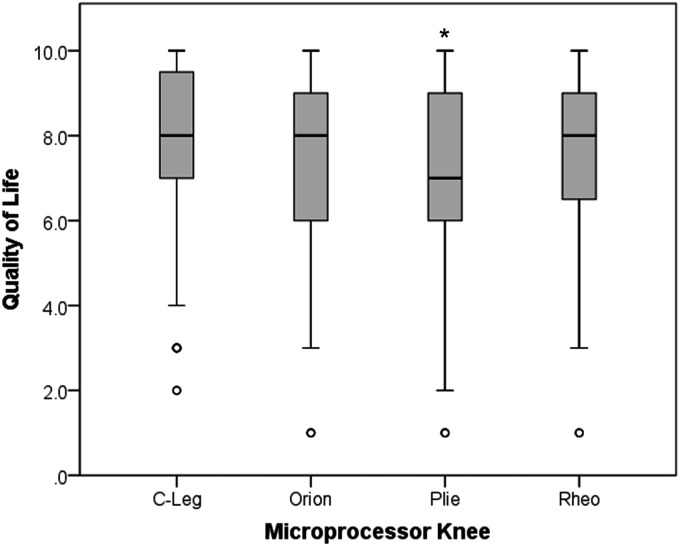
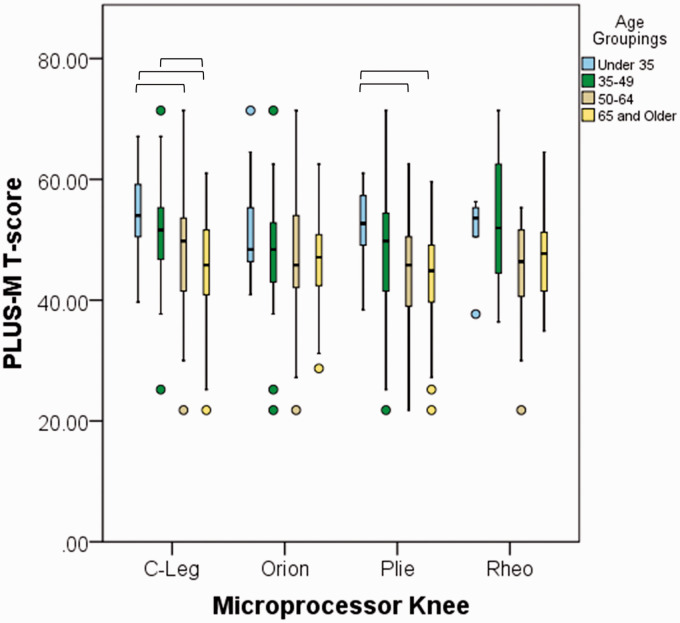
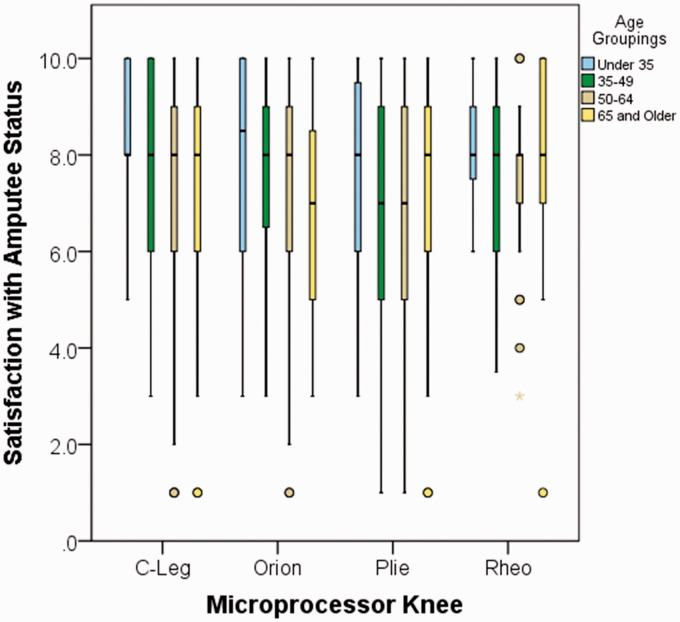
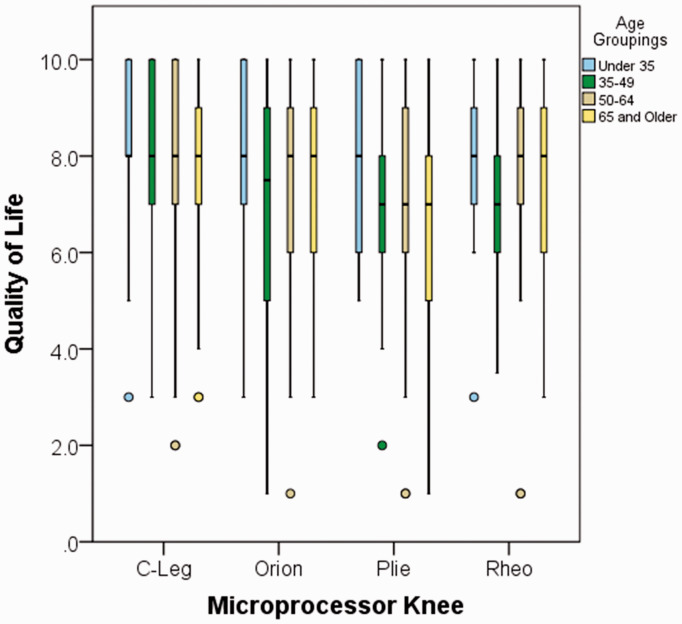
C-Leg users reported the greatest median mobility (Figure 1), however there were no statistical differences between any of the four user groups (H = 2.91, p = 0.406). Satisfaction with amputee status, derived from the Prosthesis Evaluation Questionnaire – Well Being subsection, showed C-Leg and Orion users reported highest median satisfaction. However, there were no statistical differences between the four groups (H = 4.43, p = 0.219; Figure 2). For quality of life, factor level differences were noted between the four knee categories (H = 10.15, p = 0.017; Figure 3). Post-hoc analysis revealed significant C-Leg users reported greater quality of life versus Plié (p = 0.010). No other pairwise comparisons reached statistical significance.
Figure 1.
Median mobility for users of different microprocessor knee models. The highest mobility was reported in C-Leg users, followed by Orion, Rheo, and Plié. PLUS-M: Prosthetic Limb Users Survey of Mobility.
Figure 2.
Satisfaction with amputee status based on Prosthesis Evaluation Questionnaire – Well Being subsection. C-Leg and Orion users reported highest median satisfaction, while Plié users reported the lowest.
Figure 3.
Quality of life based on Prosthesis Evaluation Questionnaire – Well Being subsection. Individuals using C-Leg reported highest quality of life, followed by Orion, Rheo, and last Plié. *Sig. vs. C-Leg at p < 0.05.
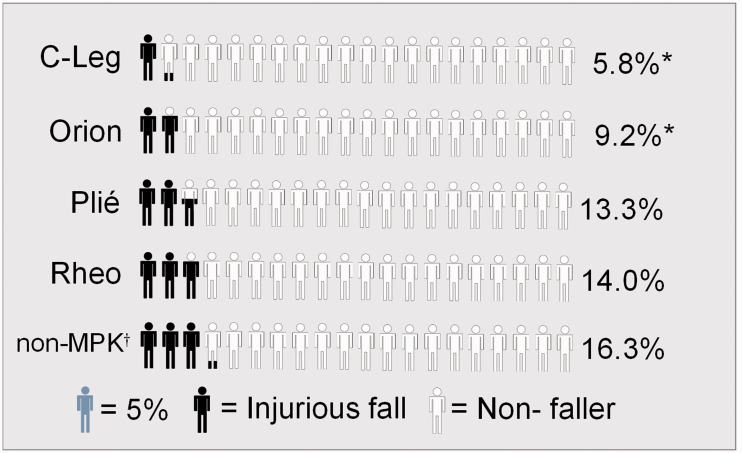
Next, injurious falls were examined. Due to the associated 6-month window on the fall question, outcomes assessed on individuals within the first 6 months were excluded, resulting in 419 MPK users available for fall analysis inclusive of 43 Rheo users, 137 C-Leg users, 119 Orion users, and 120 Plié users. Overall, among the 419 MPK users, 10.0% of individuals reported an injurious fall over the prior 6 months. The lowest percentage of individuals to report an injurious fall for which the individuals sought medical attention were the C-Leg and Orion users (Figure 4). No statistical differences were noted between the four groups (χ2(3,419) = 5.01, p = 0.171). However, when comparing against previous benchmark levels for injurious falls over the prior 6 month period among nMPK users,32 C-Leg (χ2(1,137) = 10.99, p < 0.001) and Orion (χ2(1,119) = 4.34, p = 0.037) resulted in significantly reduced injurious falls compared to nMPK.
Figure 4.
Inspecting injurious falls over previous 6 months revealed lowest percentage of falls among those with the C-Leg followed by Orion. Rheo knee users reported the highest percentage of injurious falls. Orion and C-Leg effectively reduced the number of injurious falls incurred over a 6-month period compared to non-microprocessor knees (non-MPK). *Sig. vs. non-MPK at p < 0.05, †Population benchmark for 6-month injurious fall rate from Wurdeman et al.32
Finally, when investigating MPK outcomes across different age groups, we noted a consistent pattern of modest declines in mobility with aging across all MPKs. The Orion appeared to be the most resilient to the effect of age on mobility, as no differences were noted across age subgroups (H = 2.56, p = 0.464; Figure 5). However, this may also be a reflection of qualitatively observed lower mobility of younger Orion users. Rheo also had no significant differences across age (H = 4.61, p = 0.202), although differences may be due to limited sample size when splitting the Rheo sample into 4 sub-groups by age. C-Leg (H = 19.63, p < 0.001; Under 35 vs 50-64: p = 0.028, Under 35 vs 65 and Older: p < 0.001, 35-49 vs 65 and Older: p = 0.025) and Plié (H = 14.04, p = 0.003; Under 35 vs 50-64: p = 0.005, Under 35 vs 65 and Older: p = 0.009) users saw declines with advanced aging.
Figure 5.
Median mobility for users of different microprocessor knee models broken down into age subgroups. Age impacts Plié users the most. – Sig. at p < 0.05, PLUS-M: Prosthetic Limb Users Survey of Mobility.
By contrast, both of the constructs assessed with the PEQ-Well Being survey appeared to be resilient to the impacts of advancing age noting lack of statistically significant differences for both satisfaction (C-Leg: (H = 4.76, p = 0.191); Orion: (H = 4.38, p = 0.223); Plié: (H = 0.96, p = 0.810); Rheo: (H = 1.88, p = 0.598)) and quality of life (C-Leg: (H = 3.18, p = 0.365); Orion: (H = 3.45, p = 0.327); Plié: (H = 4.57, p = 0.206); Rheo: (H = 1.11, p = 0.774)). Qualitatively, the oldest Orion users report lowest satisfaction with amputee status (Figure 6). Qualitatively, individuals age 35-49 and 50-64 reported lowest quality of life among Plié users (Figure 7).
Figure 6.
Median satisfaction with amputee status for age subgroups. C-Leg and Orion showed differences between youngest users and oldest users.
Figure 7.
Median quality of life for age subgroups. Quality of life followed similar trends as mobility, showing age impacts Plié users the most.
Discussion
The current study had individuals stratified into four different groups based on the type of MPK they utilized. There were minimal differences in group demographics, but there were differences in performance with current study hypotheses partly supported. It was first hypothesized that differences would be noted across MPKs in the measured outcomes. Overall results noted areas of parity, but also certain measures that would indicate differences in performance. It was also hypothesized that similar age-related changes would be observed across the MPK designs. This was partially supported, with significant age differences noted for two of the four groups.
Our data indicate relative parity among users of the 4 most commonly used MPKs with regard to prosthetic mobility as measured by the PLUS-M. Differences in average mobility scores within the four groups were small and failed to reach statistical significance. With respect to clinical significance, although the minimal detectable change is more pertinent in repeated measures analyses, it is worth noting that observed group differences did not exceed the minimal detectable change of 4.5 points that has been identified with the PLUS-M patient report outcomes instrument.34,35 The relative parity among the MPKs in the current analysis would suggest that when improved mobility is considered a primary aim for MPK prescription, all models would be indicated.
Our data indicate a pattern of progressive decline in prosthetic mobility with advancing age which is consistent with the original PLUS-M development sample,36 although the degree of decline was less within our sample and slightly varied across knee types. This may be reflective of MPK benefits to mobility in our sample of all MPK users versus the mixed pool of individuals within the PLUS-M development sample. Future work should determine the magnitude of decline in mobility with aging that could be expected in the absence of technology such as MPKs. Importantly, the noted mobility levels for aging individuals with MPKs reinforces the collective observation from prior publications that older adults are frequently capable of meaningful prosthetic mobility with the use of MPKs.20,22,37
Improvements in both satisfaction and quality of life have generally been reported with the use of MPKs. This has been measured using the Well-Being subscale of the PEQ in which subjects are asked to rate their satisfaction with “how things have worked out since [their] amputation” over the past four weeks and their quality of life over the last four weeks.14,16,18–20,23,24 Improvements within the broader construct of quality of life associated with the use of an MPK have also been reported using the EuroQol Five Dimensions Questionnaire (EuroQol EQ-5D) assessing the dimensions of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.38,39
Our data demonstrates relative parity in the satisfaction and quality of life reported by the users of all 4 analyzed MPKs. While the median satisfaction value reported with the Plié was slightly lower than the other MPKs, this failed to reach statistical significance and was also associated with the greatest interquartile range, suggesting a broader range of satisfaction values associated with the knee. A similar pattern was observed within the construct of quality of life, with slightly lower quality of life values associated with the Plié.
In contrast to mobility, neither satisfaction nor quality of life values were associated with notable declines with aging for users of any of the four MPKs. This contrast could be interpreted as counter to previous work showing a strong relationship between mobility and both constructs of satisfaction and quality of life,28 however it more likely serves to underscore the multiple factors associated with satisfaction and quality of life. For example, previous work did not layer aging on top of the analysis and it would seem reasonable that factors involved with satisfaction and quality of life vary across the life spectrum and possibly different amputation levels.
The percentage of community dwelling lower limb prosthesis users that incur an injurious fall has been reported between 19% and 27% over time frames of 18 and 12 months respectively.30,31 This percentage is consistent with the slightly lower value of 16.3% reported more recently over a shorter time window of only 6 months.32 Users of transfemoral prostheses have been reported to be 2.8 times more likely to sustain an injurious fall.31 The current analysis found that across all subjects the percentage of individuals with injurious fall in the previous 6 months was only 10%, although some specific knee designs seem to be more suited for fall deterrence. This is consistent with previously published literature reporting that the transition from nMPKs to MPKs has generally been associated with decreases in reported stumbles and falls using both the PEQ-Addendum18,19 and raw stumble and fall counts.20,22,40,41
Our data demonstrated a non-significant increase in the number of injurious falls associated with both the Plié and the Rheo relative to the C-leg and the Orion. This is consistent with previously published observations of increased stumbles14 and falls15 with the transition from nMPKs to the Rheo MPK. The ability for the C-Leg and Orion to significantly reduce injurious falls compared to nMPKs would suggest that when stability and falls reduction is considered a primary aim for MPK prescription, these models may be more indicated.
An additional consideration to this work is that the examined populations included a range of amputation etiologies (Table 1). By contrast, the benchmark data for injurious falls used for comparison was taken from a cohort of individuals with amputation secondary to diabetes or vascular disease.32 The relationship between amputation etiology and injurious fall rates among users of transfemoral prostheses remains unclear. Wong has reported a paradoxical relationship in which patients with better balance demonstrate higher odds of falling. This may reflect a tendency among those with poor balance to avoid activities in which falls might be experienced.30 Thus, the fall rates observed in the MPK cohorts of this publication may reflect higher activity levels and fall rates associated with a more diverse range of amputation etiology than that observed in the benchmark data. However, given the identical means of data collection and the associated recall period, this benchmark data represented the best available comparison group for injurious fall rates in the absence of MPKs.
The current study carries the advantage of being completed and disseminated absent of potential bias due to manufacturer funding or publication. This allows rehabilitation specialists to care for patients with confidence when selecting various manufacturer components. Additionally, an analysis on more than 600 MPK users adds increased benefit as it provides ability for greater generalizability compared to previous literature that may have been limited with sample size.16,19,30,40,41 Analyses lacking manufacturer bias on large samples of patients is warranted for further refinement of clearer prescription guidelines. However, the current analysis also has limitations with its findings. First, the current study was retrospective observation analysis of patient outcomes. This allows for understanding of clinical effectiveness as opposed to efficacy, whereby effectiveness is defined as “performance [of the intervention] under ‘real-world’ conditions”.42 This subjects the current analysis to potential selection bias. An additional limitation is the unequal sample size of Rheo users which is directly related to the aforementioned selection bias whereby there are not many Rheo knees fitted in the participating clinics. Third, the current analysis database was not able to identify experience on an MPK and some individuals may have transitioned recently from nMPK to MPK. Also, the current analysis looked across different MPK type users with population specific instruments. Future work should consider non-population specific measures to allow comparison to individuals without amputation. Additionally, the current study chose to investigate mobility, quality of life, satisfaction with amputee status, and falls. There may be other constructs and outcome measures for considering differences in MPKs that are better suited. Finally, the current study was an analysis of the end outcomes experienced by patients without attempt to determine underlying mechanistic cause. It is recommended for next steps to include a mechanistic approach to understand how the various mechanical differences of the knee designs contribute to different end outcomes in light of modern motor control theory.
Conclusions
The purpose of the current analysis was to analyze prosthetic mobility, satisfaction with amputee status, quality of life, and injurious falls among large cohorts of different types of MPKs. We would recommend that future products begin to include data on these and similar domains/constructs as they are introduced to the market to better inform clinical decisions. The availability of such data, combined with additional analyses such as the current study, can lend itself towards clearer prescription guidelines which currently become less specific when differentiating between manufacturers of similar categories of devices. Our data indicate relative parity among users of the 4 most commonly used MPKs with regard to prosthetic mobility as measured by the PLUS-M. Our data demonstrates relative parity with high satisfaction and quality of life reported by the users of all 4 analyzed MPKs. In contrast to mobility, neither satisfaction nor quality of life values reflected declines with aging. Finally, when compared to nMPKs, significant differences were observed across the MPK types in relation to the reduction of injurious falls.
Acknowledgments
Thank you to Dwiesha England, MS, Mandi Laurie, MS, and Taavy Miller, MSPO, for assistance with data collection and reduction.
Contributorship
JC conceived the study. PS researched literature. SW sought ethical approval and conducted data analysis. JC, PS, and SW JC, PS, and SW were involved in protocol development, data interpretation, writing the first draft of the manuscript, and critical revisions.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Hanger Clinic is a provider of prosthetic rehabilitation services operating independently of any manufacturer. As such, the authors declare no conflict of interest with this comparative analysis of different manufacturer knee types.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: JC.
ORCID iDs
Phillip M Stevens https://orcid.org/0000-0003-3488-0707
Shane R Wurdeman https://orcid.org/0000-0002-9526-9760
References
- 1.Stevens PM, Wurdeman SR. Prosthetic knee selection for individuals with unilateral transfemoral amputation: a clinical practice guideline. J Prosthet Orthot 2019; 31: 2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sedki I, Fisher K. Developing prescribing guidelines for microprocessor-controlled prosthetic knees in the South East England. Prosthet Orthot Int 2015; 39: 250–254. [DOI] [PubMed] [Google Scholar]
- 3.Kannenberg A, Zacharias B, Probsting E. Benefits of microprocessor-controlled prosthetic knees to limited community ambulators: systematic review. J Rehabil Res Dev 2014; 51: 1469–1496. [DOI] [PubMed] [Google Scholar]
- 4.Sawers AB, Hafner BJ. Outcomes associated with the use of microprocessor-controlled prosthetic knees among individuals with unilateral transfemoral limb loss: a systematic review. J Rehabil Res Dev 2013; 50: 273–314. [DOI] [PubMed] [Google Scholar]
- 5.Theeven PJ, Hemmen B, Brink PR, et al. Measures and procedures utilized to determine the added value of microprocessor-controlled prosthetic knee joints: a systematic review. BMC Musculoskelet Disord 2013; 14: 333–2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Samuelsson KA, Toytari O, Salminen AL, et al. Effects of lower limb prosthesis on activity, participation, and quality of life: a systematic review. Prosthet Orthot Int 2012; 36: 145–158. [DOI] [PubMed] [Google Scholar]
- 7.Highsmith MJ, Kahle JT, Bongiorni DR, et al. Safety, energy efficiency, and cost efficacy of the C-Leg for transfemoral amputees: a review of the literature. Prosthet Orthot Int 2010; 34: 362–377. [DOI] [PubMed] [Google Scholar]
- 8.van der Linde H, Hofstad CJ, Geurts AC, et al. A systematic literature review of the effect of different prosthetic components on human functioning with a lower-limb prosthesis. J Rehabil Res Dev 2004; 41: 555–570. [DOI] [PubMed] [Google Scholar]
- 9.Thiele J, Schollig C, Bellmann M, et al. Designs and performance of three new microprocessor-controlled knee joints. Biomed Tech (Berl) 2019; 64: 119–126. [DOI] [PubMed] [Google Scholar]
- 10.Bellmann M, Kohler TM, Schmalz T. Comparative biomechanical evaluation of two technologically different microprocessor-controlled prosthetic knee joints in safety-relevant daily-life situations. Biomed Tech (Berl) 2019; 64: 407–420. [DOI] [PubMed] [Google Scholar]
- 11.Thiele J, Westebbe B, Bellmann M, et al. Designs and performance of microprocessor-controlled knee joints. Biomed Tech (Berl) 2014; 59: 65–77. [DOI] [PubMed] [Google Scholar]
- 12.Li S, Cao W, Yu H, et al. Physiological parameters analysis of transfemoral amputees with different prosthetic knees. Acta Bioeng Biomech 2019; 21: 135–142. [PubMed] [Google Scholar]
- 13.Prinsen EC, Nederhand MJ, Sveinsdottir HS, et al. The influence of a user-adaptive prosthetic knee across varying walking speeds: a randomized cross-over trial. Gait Posture 2017; 51: 254–260. [DOI] [PubMed] [Google Scholar]
- 14.Prinsen EC, Nederhand MJ, Olsman J, et al. Influence of a user-adaptive prosthetic knee on quality of life, balance confidence, and measures of mobility: a randomised cross-over trial. Clin Rehabil 2015; 29: 581–591. [DOI] [PubMed] [Google Scholar]
- 15.Hafner BJ, Askew RL. Physical performance and self-report outcomes associated with use of passive, adaptive, and active prosthetic knees in persons with unilateral, transfemoral amputation: Randomized crossover trial. J Rehabil Res Dev 2015; 52: 677–700. [DOI] [PubMed] [Google Scholar]
- 16.Howard CL, Wallace C, Perry B, et al. Comparison of mobility and user satisfaction between a microprocessor knee and a standard prosthetic knee: a summary of seven single-subject trials. Int J Rehabil Res 2018; 41: 63–73. [DOI] [PubMed] [Google Scholar]
- 17.McGrath M, Laszczak P, Zahedi S, et al. Microprocessor knees with 'standing support' and articulating, hydraulic ankles improve balance control and inter-limb loading during quiet standing. J Rehabil Assist Technol Eng 2018; 5: 20556683187953962055668318795396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hafner BJ, Willingham LL, Buell NC, et al. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil 2007; 88: 207–217. [DOI] [PubMed] [Google Scholar]
- 19.Hafner BJ, Smith DG. Differences in function and safety between Medicare functional classification level-2 and -3 transfemoral amputees and influence of prosthetic knee joint control. JRRD 2009; 46: 417–433. [PubMed] [Google Scholar]
- 20.Kaufman KR, Bernhardt KA, Symms K. Functional assessment and satisfaction of transfemoral amputees with low mobility (FASTK2): a clinical trial of microprocessor-controlled vs. non-microprocessor-controlled knees. Clin Biomech (Bristol, Avon) 2018; 58: 116–122. [DOI] [PubMed] [Google Scholar]
- 21.Seelen H, Hemmen B, Schmeets A, et al. Cost and consequences of a prosthesis with an electronically stance and swing phase controlled knee joint. TAD 2009; 21: 25–34. [Google Scholar]
- 22.Lansade C, Vicaut E, Paysant J, et al. Mobility and satisfaction with a microprocessor-controlled knee in moderately active amputees: a multi-centric randomized crossover trial. Ann Phys Rehabil Med 2018; 61: 278–285. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman KR, Levine JA, Brey RH, et al. Energy expenditure and activity of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Arch Phys Med Rehab 2008; 89: 1380–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Theeven PJ, Hemmen B, Geers RP, et al. Influence of advanced prosthetic knee joints on perceived performance and everyday life activity level of low-functional persons with a transfemoral amputation or knee disarticulation. J Rehabil Med 2012; 44: 454–461. [DOI] [PubMed] [Google Scholar]
- 25.Hafner BJ, Gaunaurd IA, Morgan SJ, et al. Construct validity of the prosthetic limb users survey of mobility (plus-M) in adults with lower limb amputation. Arch Phys Med Rehab 2017; 98: 277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.LCD: Lower limb prostheses, https://med.noridianmedicare.com/documents/2230703/7218263/Lower+Limb+Prostheses+LCD+and+PA/d3244c51-74d3-4214-a789-7481bc2e03d5 (2019, accessed 21 June 2019).
- 27.Hafner BJ, Morgan SJ, Abrahamson DC, et al. Mobility from the prosthetic limb user's perspective: Use of focus groups to guide development of the prosthetic limb users survey of mobility. Prosthet Orthot Int 2016; 40: 582–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wurdeman SR, Stevens PM, Campbell JH. Mobility analysis of AmpuTees (MAAT 1): quality of life and satisfaction are strongly related to mobility for patients with a lower limb prosthesis. Prosthet Orthot Int 2018; 42: 461–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strange D, Takarangi MK. Memory distortion for traumatic events: the role of mental imagery. Front Psychiatry 2015; 6: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong CK, Chihuri ST, Li G. Risk of fall-related injury in people with lower limb amputations: a prospective cohort study. J Rehabil Med 2016; 48: 80–85. Jan [DOI] [PubMed] [Google Scholar]
- 31.Miller WC, Speechley M, Deathe B. The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Arch Phys Med Rehabil 2001; 82: 1031–1037. [DOI] [PubMed] [Google Scholar]
- 32.Wurdeman SR, Miller TA, Stevens PM, et al. Microprocessor knee technology reduces odds of incurring an injurious fall for individuals with diabetic/dysvascular amputation. JPO 2020; 32: 64–69. [DOI] [PubMed] [Google Scholar]
- 33.UWCORR. Prosthetic limb users survey of mobility (PLUS-M™) Version 1.2 Short Forms Users Guide, www.plus-m.org (2013, accessed 4 January 2020).
- 34.Wurdeman SR, Stevens PM, Campbell JH. Mobility analysis of amputees (MAAT 3): matching individuals based on comorbid health reveals improved function for above-knee prosthesis users with microprocessor knee technology. Assist Technol 2018; 28: 1–7. [DOI] [PubMed] [Google Scholar]
- 35.Hafner BJ, Morgan SJ, Askew RL, et al. Psychometric evaluation of self-report outcome measures for prosthetic applications. J Rehabil Res Dev 2016; 53: 797–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.UWCORRProsthetic Limb User Survey, www.plus-m.org (2013, accessed 5 December 2016).
- 37.Burnfield JM, Eberly VJ, Gronely JK, et al. Impact of stance phase microprocessor-controlled knee prosthesis on ramp negotiation and community walking function in K2 level transfemoral amputees. Prosthet Orthot Int 2012; 36: 95–104. [DOI] [PubMed] [Google Scholar]
- 38.Gerzeli S, Torbica A, Fattore G. Cost utility analysis of knee prosthesis with complete microprocessor control (C-Leg) compared with mechanical technology in transfemoral amputees. Eur J Health Econ 2009; 10: 47–55. [DOI] [PubMed] [Google Scholar]
- 39.Cutti AG, Lettieri E, Del Maestro M, et al. Stratified cost-utility analysis of C-Leg versus mechanical knees: findings from an Italian sample of transfemoral amputees. Prosthet Orthot Int 2017; 41: 227–236. [DOI] [PubMed] [Google Scholar]
- 40.Kahle JT, Highsmith MJ, Hubbard SL. Comparison of nonmicroprocessor knee mechanism versus C-Leg on prosthesis evaluation questionnaire, stumbles, falls, walking tests, stair descent, and knee preference. JRRD 2008; 45: 1–14. [DOI] [PubMed] [Google Scholar]
- 41.Wong CK, Rheinstein J, Stern MA. Benefits for adults with transfemoral amputations and peripheral artery disease using microprocessor compared with nonmicroprocessor knees. Am J Phys Med Rehab 2015; 94: 804–810. [DOI] [PubMed] [Google Scholar]
- 42.Singal AG, Higgins PD, Waljee AK. A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol 2014. Jan 2; 5: e45. [DOI] [PMC free article] [PubMed] [Google Scholar]