Abstract
Objective:
To investigate the effect of small needle-knife therapy in people with painful knee osteoarthritis.
Design:
Pilot randomised, controlled trial.
Setting:
Rehabilitation hospital.
Subjects:
In-patients with osteo-arthritis of the knee.
Interventions:
Either 1 to 3 small needle-knife treatments over seven days or oral Celecoxib. All patients stayed in hospital three weeks, receiving the same mobility-focused rehabilitation.
Measures:
Oxford Knee Score (OKS), gait speed and kinematics were recorded at baseline, at three weeks (discharge) and at three-months (OKS only). Withdrawal from the study, and adverse events associated with the small needle knife therapy were recorded.
Results:
83 patients were randomized: 44 into the control group, of whom 10 were lost by three weeks and 12 at 3 months; 39 into the experimental group of whom eight were lost at three weeks and three months. The mean (SE) OKS scores at baseline were Control 35.86 (1.05), Exp 38.38 (0.99); at three weeks 26.64 (0.97) and 21.94 (1.23); and at three months 25.83 (0.91) and 20.48 (1.14) The mean (SE) gait speed at baseline was 1.07 (0.03) m/sec (Control) and 0.98 (0.03), and at three weeks was 1.14 (0.03) and 1.12 (0.03) (P < 0.05). Linear mixed model statistical analysis showed that the improvements in the experimental group were statistically significant for total OKS score at discharge and three months
Conclusions:
Small needle-knife therapy added to standard therapy for patients with knee osteoarthritis, was acceptable, safe and reduced pain and improved global function on the Oxford Knee Score. Further research is warranted.
Keywords: Small needle-knife therapy, knee osteoarthritis, gait performance
Introduction
Osteoarthritis of the knee may cause pain and may reduce mobility, and the current main treatments include anti-inflammatory analgesics, exercise and arthroplasty but many patients continue to have problems and other treatments are of uncertain benefit.
In China, small needle-knife therapy has been used to treat knee osteoarthritis; it is a technique that combines both acupuncture and micro-invasive surgery. It was introduced in China from 1976, and it uses a new-style bladed needle that has a flat head and a cylindrical body, primarily used to treat soft tissue injuries and bone hyperplasia. Other names include acupotomy, needle scalpel, mini-scalpel acupuncture and mini-needle-knife, and mini-scalpel needle.1
A systematic review of the effects of small needle-knife therapy compared to acupuncture suggested some short-term benefit (eight trials, 654 patients) but trials were of low quality and adverse effects were not recorded.1 A systematic review of acupuncture found some benefits on function, both short-term and long-term but only a short-term effect on pain (10 trials, 2007 patients).2
In this context, a further randomized, controlled trial investigating its benefits and harms seemed justified. This is an external (i.e. not part of an ongoing trial) pilot study to determine if a larger, definitive study of its effectiveness and risks would be justified. Its aims are limited by the limited resources available, and the main questions were:
is the treatment as acceptable as non-steroidal anti-inflammatory drugs?
is there any evidence of significant harm?
what is the potential size of any benefit, to allow calculation of a sample size?
is telephone follow-up three months after discharge feasible?
Method
The study uses a parallel-group, randomised to alternative treatments on a 1:1 ratio, and observer-blinded design. It was approved by China Registered Clinical Trial Ethics Review Committee (ChiECRCT-20160017) and registered at Chinese Clinical Trial Registry (ChiCTR1800015248). Data were collected and managed between November 2016 and December 2017. The study was carried out at the Department of Orthopaedics, The Second Affiliated Hospital of Anhui University of Chinese Medicine, under the support by the Centre for Movement and Occupational Rehabilitation Sciences, Oxford Brookes University who were responsible for conduct and integrity of the study. There were no changes to the design after trial registration.
In China patients with osteo-arthritis may be admitted for three weeks of inpatient rehabilitation and the study recruited from these patients. For the study, patients had to have knee osteoarthritis as diagnosed using the criteria of the American College of Rheumatologists.3 Severity was classified using X-rays of the knees as defined by Kellgren and Lawrence.4
Patients were excluded if they:
had co-morbidities affecting the joints, such as psoriasis, syphilitic neuropathy, metabolic bone disease, and acute trauma;
were a woman who was pregnant or preparing for pregnancy;
had an allergy to Celecoxib;
had other cardiovascular, cerebrovascular, hepatic, renal, hematopoietic, or endocrine conditions that affected mobility or knee function
After initial recruitment and selection, which also included gaining informed consent, patients were randomly allocated into one of two treatment groups: experimental, treated with small needle-knife therapy, or control, treated with Celecoxib. Allocation was achieved using sealed, numbered envelopes which were filled, by an independent person, using a list of random numbers and that indicated whether the patient should have control or experimental treatment. The research administrator was given the patient’s details to register the patient, and then opened the envelope to tell the clinician the patient’s group. The treating physician knew which group a patient was in, as did the patient.
During the three weeks in the ward both groups of patients had routine treatment including massage therapy, acupuncture, exercises and walking. This was local best practice rehabilitation.
The patients in the small needle-knife therapy group were treated using the type I, No. 4 Hanzhang needle-knives (Hanzhang Acupotome; Beijing Huaxia Acupotome Medical Equipment Factory, Beijing, China). The procedure of small needle knife therapy is shown in Supplemental Figure S1. The size of the needles are 0.6 mm × 50 mm with a sharp blade at the top of the needle (Supplemental Figure S1(A)).
The patient lay in supine position with the knee flexed at 60° by placing a bolster under the knee. Tender points (trigger points) at the knee quadriceps tendon, the capsules, tendon and ligaments surrounding patella, the tibia and fibula collateral ligaments, and the lateral and medial heads of the gastrocnemius muscle, the biceps femoris attachment points were carefully identified (Supplemental Figure S1(B)) and labeled using a marker pen (Supplemental Figure S1(C)). Depending on the patient’s condition, usually no more than 10 tender points were selected at a time. After the tender points were selected, the skin was disinfected using Povidone-iodine.
The small needle knife blade was rapidly pushed perpendicularly to the labelled tender points through the skin. It may reach the surface of bone or joint space (Supplemental Figure S1(D)) and (E)). The manipulation of the needles consists of four steps: incision, stripping, releasing and cutting. It is crucial that the direction of the cutting edge of the blades are in parallel with the muscle fibers, nerves and blood vessels to avoid injury.
During the procedures described below, attention was paid to the anatomic structure of the knee, to avoid any potential injury of nerves such as nervus tibialis, nervus peroneus communis, or blood vessels such as popliteal artery or vein.
There are two types of tender points, small circular points, or long strap-like points. At the small round tender points the needle is pushed perpendicularly into the points to reach the surface of bone; then is moved up and down 2 to 3 times to cut the tender points, felt as a loosening of the tissue. For the long strap-like points, the needle is firstly pushed in with the blade in parallel with the muscle or tendon fibres (crucial to avoid injury), then the blade is used to strip the strap-like tender points longitudinally, or to separate transversely the adhesive/scarred tissue so as to feel decompression or loosening of the tender points/tissue. After this, the needle was withdrawn from the skin, the skin was compressed briefly to stop bleeding, and the same procedure was performed to the next tender point. When all labelled tender points were treated the wounds on skin were dressed using sterile tape (Supplemental Figure S1(F)).
Treatments were repeated, according to clinical judgement. The same tender points were treated again in seven days or different tender points were treated the following day. Each patient had between one and three treatments within 10 days. In the treatment group, patients were assessed after all treatment was completed.
The patients in the control group were treated by daily 200 mg oral Celecoxib for three weeks.
The following data were collected.
Any adverse events were recorded. When patients dropped out or were lost, the reason was established by the surgeons who performed the clinical trial.
The primary outcome measure was the Chinese version of Oxford Knee Score which was completed at baseline, at three weeks (usually the time of discharge from the ward) and by telephone at three months after the patients were discharged (follow-up).5,6 The person collecting the data did not know which group a patient was in.
The only other measure was a detailed in-depth gait analysis was performed using a single sensor inertial measurement unit (IMU) during a standard 10-m walk at baseline, after treatment in the experimental group only, and at discharge.7 An IMU was attached to the lower back, sampling triaxial accelerometer, gyroscope and magnetometer data at a frequency of 100 Hz. Spatiotemporal parameters derived were step time (ms), cadence (steps/min), stride length (m), walking speed (m/s) and Froude. More advanced parameters related to symmetry (Beta), variability (SDA, SDB, Ratio)8 and motor control (Walking Ratio (mm/steps/min)) were also derived. An illustration of the output from the analysis and its components is shown in Supplemental Figure S2.
All data collected were given to research officers in the hospital. Anonymised and encrypted digital data-files were sent over the internet to Oxford Brookes University, Statistics Department.
Analysis was undertaken by researchers unaware of which group had what treatment, using IBM-SPSS version 23. The data were analysed using a linear mixed model. All analyses were by allocated group. No power calculation was undertaken, but we aimed to recruit more than 50 participants to allow a reasonable estimate of benefits and serious harms.
Results
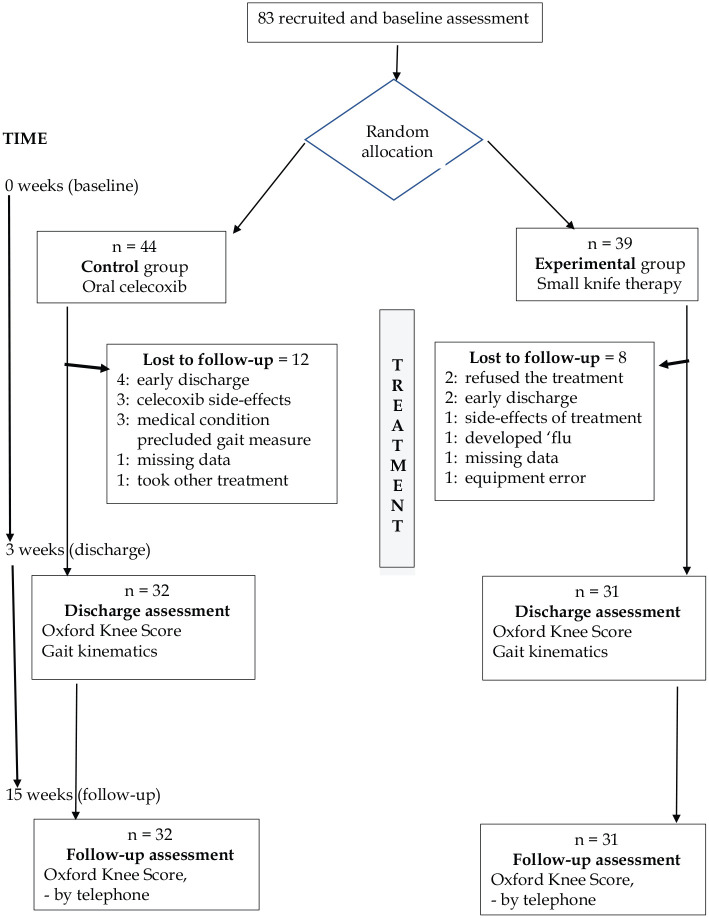
A total of 83 patients were recruited. The baseline demographic data are shown in Table 1, and the flow of patients is shown in Figure 1. No significant harm was recorded for any patient in either group.
Table 1.
Demographic characteristics of participants.
| SNK (n = 39) | Control (n = 44) | |
|---|---|---|
| Age (years)a | 61.90 ± 0.93 | 61.55 ± 1.08 |
| Gender (male/female)b | 3/36 | 10/34 |
| Height (cm)a | 160.18 ± 0.78 | 162.48 ± 0.88 |
| Weight (kg)a | 64.08 ± 1.07 | 65.28 ± 1.05 |
| Kellgren and Lawrence grade (II/III)b | 29/10 | 33/11 |
| Affected side (left/right/both)b | 10/20/9 | 13/16/15 |
SNK: Small needle knife therapy.
Values are mean ± SE.
Values are frequency.
Figure 1.
Study flow chart.
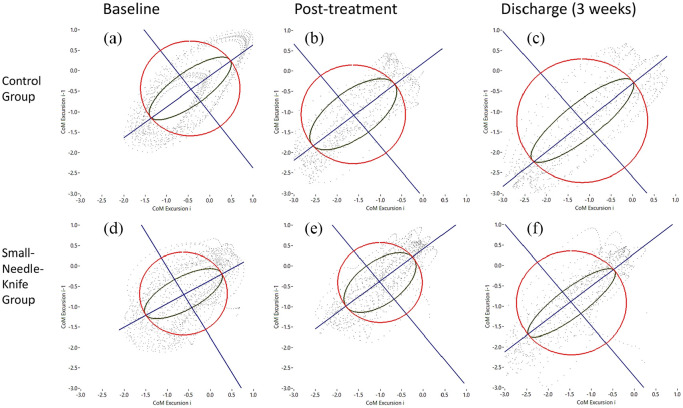
The effect of small needle-knife therapy on Oxford Knee Score and gait kinematics (at discharge only) is shown in Table 2. The Oxford Knee Score decreased (i.e. patients improved) in both groups. Analysis using linear mixed methods showed that the decrease was greater in the group treated with small-knife-therapy, and was particularly evident for the pain sub-score. Both groups showed changes indicating more normal gait kinematics (Figure 2); there was a trend towards greater change in the small needle-knife therapy group in all parameters (Table 3), but only the change in cadence reached the statistical significance of P < 0.05.
Table 2.
Unadjusted Oxford Knee Score (OKS), pre intervention, at the time of discharge (three weeks) and follow-up (three months), mean ± SE.
| OKS-Pre | OKS-discharge | OKS-follow up | Repeated Measure; linear mixed model | ||||
|---|---|---|---|---|---|---|---|
| Time × Group | Time | Group | |||||
| Total score | Control | 35.86 ± 0.74 | 26.64 ± 0.97 | 25.83 ± 0.91 | <0.001 | <0.001 | 0.019 |
| SNK | 38.38 ± 0.70 | 21.94 ± 1.23 | 20.48 ± 1.14 | ||||
| Functional score | Control | 14.66 ± 0.35 | 11.17 ± 0.41 | 10.61 ± 0.39 | <0.001 | <0.001 | 0.066 |
| SNK | 16.13 ± 0.32 | 9.33 ± 0.53 | 8.67 ± 0.49 | ||||
| Pain score | Control | 21.20 ± 0.44 | 15.47 ± 0.59 | 15.22 ± 0.57 | <0.001 | <0.001 | 0.012 |
| SNK | 22.26 ± 0.42 | 12.61 ± 0.72 | 11.82 ± 0.67 | ||||
OKS: Oxford Knee score; SNK: Small needle-knife therapy.
Figure 2.
The phase plots of gait analysis for the control group (a–c) and Small Needle Knife Group (d–f) whereby a visual representation of variability and symmetry parameters can be compared between three representable participants from each group.
Table 3.
Unadjusted gait performance pre-intervention and at the time of discharge (three weeks), mean ± SE.
| Pre | Discharge | ||
|---|---|---|---|
| Speed (m/sec) | Control group | 1.07 ± 0.03 | 1.14 ± 0.03 |
| SNK group | 0.98 ± 0.03 | 1.12 ± 0.03 | |
| Cadence (step/min) | Control group | 108.56 ± 3.71 | 109.55 ± 2.23 |
| SNK group | 98.52 ± 2.04 | 109.34 ± 1.58* | |
| Step time (sec) | Control group | 0.59 ± 0.02 | 0.56 ± 0.01 |
| SNK group | 0.62 ± 0.01 | 0.56 ± 0.01 | |
| Step time Left (sec) | Control group | 0.59 ± 0.02 | 0.56 ± 0.02 |
| SNK group | 0.62 ± 0.01 | 0.55 ± 0.01 | |
| Step time Right (sec) | Control group | 0.59 ± 0.02 | 0.56 ± 0.01 |
| SNK group | 0.62 ± 0.01 | 0.56 ± 0.01 | |
| Step Length Left (m) | Control group | 0.60 ± 0.01 | 0.63 ± 0.01 |
| SNK group | 0.59 ± 0.01 | 0.61 ± 0.01 | |
| Step Length Right (m) | Control group | 0.59 ± 0.01 | 0.63 ± 0.01 |
| SNK group | 0.59 ± 0.01 | 0.60 ± 0.01 | |
| Stride length (m) | Control group | 1.18 ± 0.03 | 1.25 ± 0.02 |
| SNK group | 1.18 ± 0.02 | 1.21 ± 0.02 |
SNK: Small needle knife therapy.
P < 0.05 for intergroup group differences.
Discussion
This study found that small needle-knife therapy resulted in significantly greater improvements of Oxford Knee Score and in gait cadence at three weeks post treatment amongst patients with knee arthritis, in comparison with oral Celecoxib. At three months, the Oxford knee score was still better in the small needle-knife therapy group. Harm was equal in both groups, but one person out of 39 in the surgical treatment group had bleeding. Withdrawal from treatment was no greater than in the group taking Celecoxib.
We considered that this should be considered a pilot trial because:
the numbers are too small to be certain about any differences identified
it depended upon a single expert surgeon
it was carried out in only one centre
the follow-up was limited to three months after treatment
These factors make it unwise to draw definite conclusions or to change clinical practice until further research has been undertaken.
Although small needle-knife therapy is widely used to treat knee osteoarthritis in China, the evidence concerning its effectiveness and the risks of harm is limited.1 Studies of acupuncture, which could be considered similar in some ways, but does not involve any cutting of or damage to tissues, have shown a probable beneficial effect upon function,2 though this also needs further study before being certain. Our findings are consistent with current published research.
Small needle-knife therapy seems similar to micro-fracture treatment which is used in some countries as a medical treatment for the same problem.9,10 However, although it may be referred to as the ‘gold standard’ treatment by some protagonists, there is little evidence of its efficacy.11
One reason for doubt about the effect of small needle-knife therapy is the lack of any good biological explanation for benefit. The nature of tender spots is unknown, and assessment is variable and only moderately repeatable.12 There is obviously likely to be a strong ‘placebo’ (expectation) response. The process is visible and surrounded with some drama and undertaken by a senior clinician. It is also culturally appropriate. Nonetheless the effect lasted 12 more weeks, which is unusual for an expectation response.
There was a low but definite rate of harm; two patients (of 39) did not want the treatment, and one had bleeding. The rate of harm and withdrawal was similar in the control group taking celecoxib.
This study has some limitations. The control intervention was not as likely to generate a high expectation. The research occurred in a single centre, and the operator (an orthopaedic surgeon) is very experienced, and an enthusiast, and the patients were not blinded. The change in the functional sub-score was not statistically significant at the set level (P < 0.05) but was consistent with benefit. Last, the number of patients is relatively low, leaving some uncertainty.
On the other hand, the assessors and the data analyst were independent and blinded, and the outcome measure is widely used and validated. The follow-up was reasonable in the context of an early trial. The changes seen were all consistent, including the short-term changes in gait kinematics
This evidence does suggest that small needle knife therapy may reduce pain and may be associated with improved gait function in patients with knee osteoarthritis. It is certainly enough evidence to justify further research. This research should take various forms. Perhaps the first should be to replicate this study, with other trained or experienced operators. Ideally this would be in another hospital.
At the same time, research into how and why this treatment might be effective should start. For example, would an equal number of randomly located small-knife insertions around the knee be equally effective, or are the tender points important. There is low agreement on the localization of tender points in most conditions.12 Is the improvement due to a reduction in pain, or is there some direct effect on knee function?
At present the evidence is insufficient to warrant widespread use, and the rate of adverse effects will need close monitoring if or when it is introduced more widely.
In conclusion, this randomized clinical trial has provided evidence that small needle knife therapy can improve symptoms of pain and function and possibly gait kinematics in patients with knee osteoarthritis patients, when compared with the control treatment of an oral NSAID Celecoxib. Further studies are warranted to refine the trial study and to reproduce a large scaled controlled trial, to establish tools that can visualize/identify the tender points in knee osteoarthritis, and to develop a method that can guide the microsurgery to be a well-controlled and more precise procedure.
Clinical messages.
Small needle-knife therapy (acupotomy) given to patients with osteoarthritis of the knee was associated with reduced pain and improved function.
The data suggest the treatment and the trial design are sufficiently feasible and safe to warrant further research.
Supplemental Material
Supplemental material, 20-06-06_Figure_1 for The effects of small-needle-knife therapy on pain and mobility from knee osteoarthritis: a pilot randomized-controlled study by Junchen Zhu, Zhiwen Zheng, Yaomeng Liu, Sophie Lawrie, Patrick Esser, Hooshang Izadi, Helen Dawes, Zhidao Xia, Chao Wang, Yingzong Xiong, Xingfu Ma and Derick T Wade in Clinical Rehabilitation
Supplemental material, 20-06-06_Figure_2 for The effects of small-needle-knife therapy on pain and mobility from knee osteoarthritis: a pilot randomized-controlled study by Junchen Zhu, Zhiwen Zheng, Yaomeng Liu, Sophie Lawrie, Patrick Esser, Hooshang Izadi, Helen Dawes, Zhidao Xia, Chao Wang, Yingzong Xiong, Xingfu Ma and Derick T Wade in Clinical Rehabilitation
Acknowledgments
Professor Helen Dawes is supported by the Elizabeth Casson Trust and the NIHR Oxford Health Biomedical Research Centre.
Footnotes
Author contributions: Junchen Zhu: original question, design, patient intervention, aiding reporting, final agreement
Zhiwen Zheng: original question, design, patient evaluation, aiding reporting, final agreement
Yaomeng Liu: data handling; data analysis/presentation, final agreement
Sophie Lawrie: data handling; data analysis/presentation, final agreement
Patrick Esser: detailed gait recording and analysis, data presentation, final agreement
Hooshang Izadi: design & randomization, data analysis and interpretation, final agreement
Helen Dawes: design/practical application, data handling/analysis, revision and approval
Zhidao Xia: design/adaptation to context, two-way communication, writing and approval
Chao Wang: data collection, checking and approving paper
Yingzong Xiong: application of design, data collection, checking and approving paper
Xingfu Ma: data collection, checking and approving paper
Derick T Wade: design, data to be collected, data presentation, writing the paper, approval
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors would like to thank Anhui Province Think Tank Consultant Ltd and Oxford International Rehabilitation Foundation for giving funds to this project. This project is also funded by the Key Research and Development Project of Anhui Province (1704a0802168). The funders had no influence over data collection, analysis or writing up and interpretation.
ORCID iD: Derick T Wade  https://orcid.org/0000-0002-1188-8442
https://orcid.org/0000-0002-1188-8442
Supplemental material: Supplemental material for this article is available online.
References
- 1. Lin X, Huang K, Zhu G, et al. The effects of acupuncture on chronic knee pain due to osteoarthritis: a meta-analysis. J Bone Joint Surg Am 2016; 98(18):1578–1585. [DOI] [PubMed] [Google Scholar]
- 2. Liu FS, Jin DZ, Wu X. Acupotomy versus acupuncture for knee osteoarthritis: a Meta-analysis of randomized controlled trials. Chinese J Tissue Eng Res 2012; 16(44): 8235–8239 DOI: 10.3969/j.issn.2095-4344.2012.44.013. 翔刘福水,金德忠,吴, Liu Fu-shui JD. 针刀与针灸治疗膝骨关节炎疗效比较的Meta分析. 中国组织工程研究. 2012; 16(44):8235–8239. [DOI] [Google Scholar]
- 3. Wu CW, Morrell MR, Heinze E, et al. Validation of American college of Rheumatology classification criteria for knee osteoarthritis using arthroscopically defined cartilage damage scores. Semin Arthritis and Rheum 2005; 35(3):197–201. [DOI] [PubMed] [Google Scholar]
- 4. Kellgren JH, Lawrence JS. Radiological assessment of osteoarthritis Ann Rheum Dis 1957; 16(4): 494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Harris KK, Dawson J, Jones LD, et al. Extending the use of PROMs in the NHS—using the Oxford knee score in patients undergoing non-operative management for knee osteoarthritis: a validation study. BMJ Open 2013; 3(8): e003365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lin K, Bao L, Wang J, et al. Validation of the Chinese (Mandarin) version of the Oxford knee score in patients with knee osteoarthritis. Clin Orthop Relat Res 2017; 475(12): 2992–3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Esser P, Dawes H, Collett J, et al. Assessment of spatio-temporal gait parameters using inertial measurement units in neurological populations. Gait Posture 2011; 34(4): 558–560. [DOI] [PubMed] [Google Scholar]
- 8. Esser P, Dawes H, Collett J, et al. Insights into gait disorders: walking variability using phase plot analysis, Parkinson’s disease. Gait Posture 2013; 38(4): 648–652. [DOI] [PubMed] [Google Scholar]
- 9. Yen Y-M, Cascio B, O’Brien L, et al. Treatment of osteoarthritis of the knee with microfracture and rehabilitation. Med Sci Sports Exer 2008; 40(2): 200–205. [DOI] [PubMed] [Google Scholar]
- 10. Shive MS, Stanish WD, McCormack R, et al. BST-CarGel® treatment maintains cartilage repair superiority over microfracture at 5 years in a multicenter randomized controlled trial. Cartilage 2015; 6(2): 62–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Erggelet C, Vavken P. Microfracture for the treatment of cartilage defects in the knee joint – a golden standard? J Clin Orthop Trauma 2016; 7(3): 145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rozenfeld E, Finestone AS, Moran U, et al. Test-retest reliability of myofascial trigger point detection in hip and thigh areas. J Bodyw Mov Ther 2017; 21(4): 914–919. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 20-06-06_Figure_1 for The effects of small-needle-knife therapy on pain and mobility from knee osteoarthritis: a pilot randomized-controlled study by Junchen Zhu, Zhiwen Zheng, Yaomeng Liu, Sophie Lawrie, Patrick Esser, Hooshang Izadi, Helen Dawes, Zhidao Xia, Chao Wang, Yingzong Xiong, Xingfu Ma and Derick T Wade in Clinical Rehabilitation
Supplemental material, 20-06-06_Figure_2 for The effects of small-needle-knife therapy on pain and mobility from knee osteoarthritis: a pilot randomized-controlled study by Junchen Zhu, Zhiwen Zheng, Yaomeng Liu, Sophie Lawrie, Patrick Esser, Hooshang Izadi, Helen Dawes, Zhidao Xia, Chao Wang, Yingzong Xiong, Xingfu Ma and Derick T Wade in Clinical Rehabilitation