Abstract
Background. The ability to accurately predict hospital length of stay (LOS) or time to discharge could aid in resource planning, stimulate quality improvement activities, and provide evidence for future research and medical practice. This study aimed to determine the predictive factors of time to discharge among patients admitted to the neonatal intensive care unit (NICU) and pediatric ward in Goba referral hospital, Ethiopia. Methods. A facility-based prospective follow up study was conducted for 8 months among 438 patients. Survival analyses were carried out using the Kaplan Meier statistics and Cox regression model. Results. The median length of hospital stay was 7 days (95% confidence interval (CI): 6.45-7.54) and 6 days (95% CI: 5.21-6.78) for patients admitted to NICU and pediatric ward, respectively. In the multivariable Cox regression, the hazard of neonatal patients with less than 37 weeks of gestational age, low birth weight, and those who develop hospital-acquired infection (HAI) after admission had prolonged time to discharge by 54% [adjusted hazard ratio (AHR): 0.46, (95% CI: 0.31-0.66)], 40% [AHR: 0.60, (95% CI: 0.40-0.90)], and 56% [AHR: 0.44, (95% CI: 0.26-0.74)], respectively. The rate of time to discharge among patients who were admitted to the pediatric ward and had HAI delayed discharge time by 49% [AHR: 0.51, (95% CI: 0.30-0.85)] compared to their counterparts. Conclusion. Hospital-acquired infections prolonged hospital stay among neonates and children admitted to the pediatric ward. On a similar note, low gestational age and low birth weight were found to be the independent predictor of longer hospital stay among neonates.
Keywords: predictors of hospital stay, hospital-acquired infections, hospital length of stay, neonates, children, Ethiopia
Introduction
Prolonged hospital length of stay (LOS) remains one of the most important challenges facing hospitals in many countries and has important implications for quality of care, patient safety, and health outcomes.1,2 Delayed hospital discharge can lead to increased costs, an increased risk of complications, and decreased patient satisfaction.3 Particularly in the pediatric population, prolonged hospitalization is costly and poses a significant risk.1,4 In this regard, an appropriate hospital stay is considered to be; efficient, effective, up to standard and tailored to the patients’ actual needs.2
Previous studies have estimated about 22.1 to 48% of days of hospital stay were unnecessary.1,5,6 A study from Iran showed that more than 20% of the hospital stay was inappropriate and 45.1% of this inappropriate stay was due to internal hospital procedures such as delay in discharge or delay in therapy and diagnostics.2 Further previous studies have identified factors associated with length of stay for admitted neonates and pediatrics; among identified factors being ventilator-dependent,7 general medical co-morbidities and severe morbidity,8 age,9 illness severity, obesity, winter and weekend admissions,9 sex,9,10 birth weight,8 admission reason,11 preoperative factors like higher hemoglobin and lower oxygen saturation,4 surgical duration longer than 30 minutes,12 and surgery while in hospital13 were the commonly identified factors. A study by Conner et al also reported that the median length of hospital stay for malnourished pediatric patients was 15 days, which corresponded with a 50% relative increase in the length of stay compared with patients who were not malnourished.14 Besides other factors, such as hospital size, delay in performing diagnostic or therapeutic procedures and delay in medical decision-making were important factors that correlate with the length of stay.1,15,16
The ability to accurately predict hospital length of stay (LOS) and modeling to predict time to hospital discharge could aid in resource planning and administration, stimulate hospital-based quality improvement activities, and support physicians in their counseling of parents and families of neonates admitted to the intensive care unit (NICU).17-19 For the first time, a recent review by Seaton et al identified only 9 studies on prediction of LOS in the neonatal unit and almost all are from Europe and the United States.20 In resource-limiting settings, there is still inadequate information about the predictive factors of LOS, especially among hospitalized children.1,14
In Ethiopia, although efforts over the past few years have been targeted toward improving the quality of neonatal ICU and child survival in hospitals, it remains unknown whether pediatric in-hospital survival has improved with these efforts. Also, the independent predictors of time to hospital discharge among pediatric population remain poorly characterized. Hence, there is a need to assess the possible factors that contributed to pediatric LOS or time to discharge to provide evidence for future research and medical practice. Furthermore, the finding would help pediatricians caring for patients in the country. For this reason, this prospective study intends to investigate the predictors of time to hospital discharge among patients in the neonatal intensive care unit (NICU) and pediatric ward in Goba referral hospital, Ethiopia.
Methods
Setting
The study was conducted at Madda Walabu University Goba Referral Hospital in southeast Ethiopia. It is the only referral hospital in the Bale zone serving over 1.5 million people. It has 20 inpatient units with a total capacity of 127 beds and is also the referral center for advance diagnostic procedures and management of pediatrics. The annual average admission of the hospital is over 8000 patients, of which 869 were in the pediatrics and NICU wards. And the average annual outpatient patient flow is over 110 661 patients. The average bed occupancy rate of the hospital was 66.2% and the average length of stay (ALOS) was 3.6 days. The present study was conducted at the department of pediatric taking care of pediatric and neonatal patients.
Study Design and Participants
A prospective follow up study was conducted among pediatric patients who were admitted to the NICU and pediatric ward from November 2018, to June 2019. Accordingly, all children admitted to the NICU and pediatric ward during the specified period were eligible for the study and followed from the time of admission until discharge.
Study Population
All patients who are admitted to the NICU and pediatric ward in Goba referral hospital were the source and study population. A total of 438 admitted neonates and pediatrics were included in the current study after consent was obtained.
Eligibility
All patients (age less than 18 years) admitted to the pediatric ward, neonatal intensive care unit (NICU) and those transferred from outside hospitals were enrolled. All patients whose parent/guardian consented for the study were eligible. Patients were excluded if they: (1) died prior to NICU and pediatric ward admission; (2) had a major congenital anomaly.
Data Collection Procedures
Data were collected prospectively after consent was sought from all pediatric parents or legal guardians. Socio-demographic and clinical data were collected by the structured questioner. First, all admitted patients were followed for the first 48 hours and patients who have developed any form of hospital-acquired infection (HAIs) after 48 hours of admission were recorded following the Center for Disease Prevention and Control (CDC) guideline.21 Afterwards, all pediatric patients were followed until for outcomes such as hospital discharge, improvement at the time of discharge, death, referral, longer duration of follow up and discharge without medical advice was recorded.
Study Variables
The event of interest was time to discharge or hospital length of stay of children admitted to the NICU and pediatric ward. The length of stay was measured using days from the time of admission until the time of death, transfer, left against medical advice or the end of the study period. Survival times of children who died during their hospital stay, those transferred to other healthcare facilities, or left against medical advice were considered censored times. Days after the transfer to a pediatric ward or another center were not included.
The independent variables were divided into 2 categories. The first category consisted of socio-demographic characteristics; age (months), gestational age, birth weight, gender, place of residence, history of the previous hospitalization. The second category consisted of clinically related factors: patients put on mechanical ventilation, presence of peripheral intravenous (IV) catheter, presence of central venous catheter (CVC), McCabe score, surgery after admission (surgery while in hospital), severe anemia status, presence of underlying diseases, HIV status, and presence of HAIs.
Operational Definitions
Healthcare acquired infections (HAIs): HAIs can be defined as those occurring within 48 hours of hospital admission or 30 days of an operation. Newborns who had an infection in the first 48 hrs of life should be considered to have Early-Onset Sepsis (EOS) and not HAIs; because we just enrolled neonates presenting with no new signs or symptoms of infection after the first 48 hours of admission. In addition, EOS reflects transplacental or, more frequently, ascending infections from the maternal genital tract, whereas Late-Onset Sepsis (LOS) is associated with the postnatal nosocomial or community environment.
Low birth weight: any neonate weighting less than 2500 g at birth irrespective of gestational age.
Presence of underling disease: indicates patients with the following underlying conditions severe acute malnutrition (SAM), diabetes mellitus, chronic renal failure, and cardiac disorder.
Presence of invasive device: references to intubation, presence of urinary catheter, peripheral vascular catheter or central vascular catheter.
Central venous catheter (CVC): is a catheter placed into a large vein/ inserted in a central vein/.
Peripheral intravenous (IV) catheter: A peripheral intravenous (IV) catheter is inserted into small peripheral veins to provide access to administer IV fluids and medications.
Data Management and Analysis
The collected data were checked for completeness and then entered into EpiData version 3.1 and exported to SPSS version 20. The survival data can summarize through life tables, Kaplan-Meier Survival functions, and median time. Accordingly, data for NICU and the pediatrics were analyzed separately. Descriptive analyses were carried out to present the given data. Kaplan-Meier survival curves were generated and the log-rank analysis was used to compare hospital length of stays between subcategories. Cox regression analysis was performed to assess the predictive factors for hospital discharge status. Crude hazard ratios (CHR) and adjusted hazard ratios (AHR), with 95% confidence intervals (CIs) were used to assess the strength of association. To select the potential variables for the multivariable Cox regression model, variables associated with P-value ≤ .25 at bivariate regression were considered. Backward stepwise procedures were employed (these procedures deleting one variable at a time as the regression model progresses). The Log-likelihood (LL) value was used to remove factors from the model in a backward fashion. The model with the highest value of LL was considered to be the best fit model.
Finally, model adequacy was assessed for the variables remained in the multivariate model using Schoenfeld residuals plots and tests of proportional hazard. Statistically significant variables (P-values < .05) in the multivariate analysis of Cox-regression were considered predictors of LOS among the study participants.
Ethics Approval and Informed Consent
Ethical clearance was obtained from the Ethical Review Committee of Madda Walabu University (Ref. No.: RMW 14/66/64) and a formal letter from Madda Walabu University Research Community Engagement and Technology Transfer Vice President Office was obtained. Written informed consent from the parents/legal guardians was obtained after explaining the objectives of the study. Throughout the data collection period, confidentiality and privacy of the patients were observed, and a unique identification code rather than their names were substituted.
Results
Four hundred thirty-eight study participants (median age: 8.5 months (IQR, 2-36 months)) were followed for a total of 3128 person-days. Of these, 191 (43.6%) and 247 (56.4%) patients were from the NICU and pediatric ward, respectively. The median stay for patients admitted to NICU was 7 days (95% confidence interval (CI): 6.45-7.54). While the median hospital stay for patients admitted to pediatric ward was 6 days (95% CI: 5.21-6.78).
Socio-Demographic and Clinical Characteristics of Patients Admitted at NICU
The median (IQR) age of the neonates was 2 days (IQR: 1-6 days). Among 191 neonates, 50.8% of neonates were males, 56.5% were ≥37 weeks of gestational age and 24.1% were low birth weight (LBW). One hundred twenty four (64.9%) were stay in a median of ≤7 days. The top 3 reasons for admissions of the neonates in this study were distributed as follows: late preterm and early neonatal sepsis 13.1%, early neonatal sepsis 11.0%, low birth weight (LBW) 11.0%, and late preterm 8.9% (Table 1). Of the study participants, 26.2% (50/191) were censored [24 (48.0%) were died, 19 (38.0% transferred to another hospital, and 7 (14.0%) were left against medical advice] (Figure 1).
Table 1.
Socio-Demographic and Clinical Characteristics of Neonates Admitted at Goba Referral Hospital, Southeast Ethiopia, 2019 (n = 191).
| Covariates | Category | Frequency | Percent |
|---|---|---|---|
| Age (days) | 1 | 89 | 46.6 |
| 2-4 | 48 | 25.1 | |
| ≥5 | 54 | 28.3 | |
| Sex | Male | 97 | 50.8 |
| Female | 94 | 49.2 | |
| Gestational age | Less than 37 weeks | 83 | 43.5 |
| ≥37 weeks | 108 | 56.5 | |
| Place of residence | Urban | 78 | 40.8 |
| Rural | 113 | 59.2 | |
| Previous hospitalization | Yes | 11 | 5.8 |
| No | 180 | 94.2 | |
| Patients put on mechanical ventilation | Yes | 61 | 31.9 |
| No | 130 | 68.1 | |
| Peripheral intravenous (IV) catheter | Yes | 180 | 95.8 |
| No | 8 | 4.2 | |
| Central venous catheter (CVC) | Yes | 2 | 1.0 |
| No | 189 | 99.0 | |
| Presence of invasive medical device | Yes | 114 | 59.7 |
| No | 77 | 40.3 | |
| Presence of underlying diseasesa | Yes | 6 | 3.1 |
| No | 185 | 96.9 | |
| Surgery after admission | Yes | 1 | 0.5 |
| No | 190 | 99.5 | |
| Antibiotic prophylaxis was given (n = 139) | Yes | 7 | 5.0 |
| No | 132 | 95.0 | |
| Sever anemiab | Yes | 11 | 5.8 |
| No | 176 | 92.1 | |
| Not tested | 4 | 2.1 | |
| McCabe score (n = 114) | Nonfatal diseases | 47 | 41.2 |
| Ultimately fatal diseases | 17 | 14.9 | |
| Rapidly fatal diseases | 47 | 41.2 | |
| Unknown | 3 | 2.6 | |
| HAIs | Yes | 25 | 13.1 |
| No | 166 | 86.9 | |
| HIV status | Reactive | 2 | 1.0 |
| Non-reactive | 167 | 87.4 | |
| Unknown/not tested | 22 | 11.5 | |
| Birth weightc | <2500 g | 46 | 24.1 |
| ≥2500 g | 145 | 75.9 | |
| Reasons for admission in NICU | Late preterm + early neonatal sepsis (ENOS) | 25 | 13.1 |
| ENOS | 21 | 11.0 | |
| Low birth weight (LBW) | 21 | 11.0 | |
| Late preterm | 17 | 8.9 | |
| Moderate hypothermia | 16 | 8.4 | |
| Late preterm + LBW + Mild hypothermia + pneumonia | 14 | 7.3 | |
| Sepsis | 12 | 6.3 | |
| Prematurity + LBW | 11 | 5.8 | |
| Sepsis + PNA | 10 | 5.2 | |
| Prematurity + LBW + sepsis | 8 | 4.2 | |
| Late preterm + LBW + moderate hypoteremia | 8 | 4.2 | |
| LBW + sepsis | 8 | 4.2 | |
| Respiratory distress syndrome (SDS) | 5 | 2.6 | |
| Moderate hypothermia + ENOS | 3 | 1.6 | |
| Pathological jaundice + early preterm | 3 | 1.6 | |
| Staphylococcal scalded skin syndrome | 2 | 1 | |
| Meningitis | 2 | 1 | |
| Prenatal asphyxia (PNA) | 2 | 1 | |
| Macrophage activation syndrome (MAS) + moderate hypothermia | 1 | 0.5 | |
| Bilateral nonpalpable testes | 1 | 0.5 | |
| Spinal bifida | 1 | 0.5 |
Cardiac disorder.
Severe anemia—hemoglobin <50 g/L (for patients older than 28 days) or hemoglobin <90 g/L (for neonates).
Any neonate weighting less than 2500 g at birth irrespective of gestational age was considered low birth weight (LBW).
Figure 1.
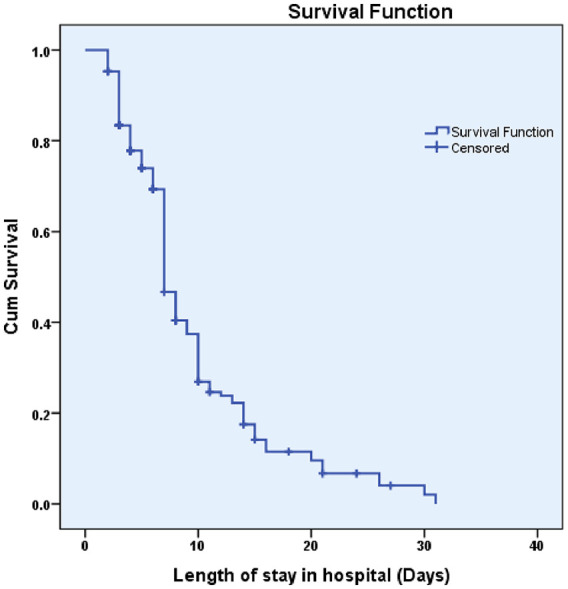
Kaplan Meier survival estimate of hospital length of stay among neonates admitted in NICU in Goba referral hospital, southeast Ethiopia, 2019.
Socio-Demographic and Clinical Characteristics of Patients Admitted at Pediatric Ward
The median ages of the patients were 12 months (IQR, 8-84 months). The majority of patients (41.3%) were female; 75 (30.4%) were in the age category of ≥59 months, 201 (81.4%) were a rural residence, and 30 (12.1%) were diagnosed with at least one type of hospital-acquired infection after 48 hours of admission (Table 2). The overall socio-demographic and clinical characteristics of the study participants admitted at pediatric ward are given in Table 2. Of the 247 pediatric study participants, 28 (11.3%) were censored, including 8 (28.6%) who were dead, and 11 (39.3%) who transferred to another hospital. The remaining 9 (32.1%) left against medical advice (Figure 2).
Table 2.
Socio-Demographic and Clinical Characteristics of Pediatrics Admitted to Pediatric Ward at Goba Referral Hospital, Southeast Ethiopia, 2019 (n = 247).
| Covariates | Category | Frequency | Percent |
|---|---|---|---|
| Age (months) | ≤1 | 11 | 4.5 |
| 2-6 | 30 | 12.1 | |
| 7-11 | 35 | 14.2 | |
| 12-23 | 34 | 13.8 | |
| 24-35 | 28 | 11.3 | |
| 36-59 | 34 | 13.8 | |
| ≥59 | 75 | 30.4 | |
| Gender | Male | 145 | 58.7 |
| Female | 102 | 41.3 | |
| Place of residence | Urban | 46 | 18.6 |
| Rural | 201 | 81.4 | |
| Previous hospitalization | Yes | 35 | 14.2 |
| No | 212 | 85.8 | |
| Patients put on mechanical ventilation | Yes | 12 | 4.9 |
| No | 235 | 95.1 | |
| Peripheral intravenous (IV) catheter | Yes | 238 | 96.4 |
| No | 9 | 3.6 | |
| Central venous catheter (CVC) | Yes | 7 | 2.8 |
| No | 240 | 97.2 | |
| Presence of invasive medical device | Yes | 145 | 58.7 |
| No | 102 | 41.3 | |
| Presence of underlying diseasesa | Yes | 46 | 18.6 |
| No | 201 | 81.4 | |
| Surgery after admissionb | Yes | 46 | 18.6 |
| No | 201 | 81.4 | |
| Antibiotic prophylaxis was given | Yes | 162 | 65.6 |
| No | 85 | 34.4 | |
| Sever anemiac | Yes | 28 | 11.3 |
| No | 192 | 77.7 | |
| Not tested | 27 | 10.9 | |
| McCabe score | Nonfatal diseases | 102 | 41.3 |
| Ultimately fatal diseases | 95 | 38.5 | |
| Rapidly fatal diseases | 48 | 19.4 | |
| Unknown | 2 | 0.8 | |
| HAIs | Yes | 30 | 12.1 |
| No | 217 | 87.9 | |
| HIV status | Reactive | 0 | 0 |
| Non-reactive | 218 | 88.3 | |
| Unknown/not tested | 29 | 11.7 | |
| Reasons for admission in pediatric wards | Measles | 35 | 14.1 |
| Complication of measles + syringocystadenoma papilliferum (SCAP) | 27 | 10.8 | |
| Complication of measles + severe acute malnutrition (SAM) | 24 | 9.6 | |
| Severe community-acquired pneumonia | 23 | 9.2 | |
| Complicated meningitis + SAM | 18 | 7.2 | |
| Severe acute malnutrition (SAM) | 15 | 6 | |
| Pyogenic meningitis | 14 | 5.6 | |
| Complication of measles + syringocystadenoma papilliferum (scap) | 14 | 5.6 | |
| Scabies + cardiogenic pulmonary edema (CPE) | 12 | 4.8 | |
| Chronic diarrhea | 11 | 4.4 | |
| Sepsis | 12 | 4.8 | |
| Pulumonary TB | 7 | 2.8 | |
| Gluteal abscess | 6 | 2.4 | |
| Pathological jaundice | 3 | 1.2 | |
| Acalculous cholecystitis + urinary tract infection (UTI) | 3 | 1.2 | |
| Hepatic failure | 2 | 0.8 | |
| Measles + intestinal parasite | 2 | 0.8 | |
| Fracture | 2 | 0.8 | |
| Foreign body | 2 | 0.8 | |
| Cardiac cachexia + drug-induced dysphagia | 2 | 0.8 | |
| Appendicitis | 2 | 0.8 | |
| Second degree burn | 2 | 0.8 | |
| Scrotal swelling | 1 | 0.4 | |
| Scabies + tinea capitis | 1 | 0.4 | |
| Posterior neck abscess | 1 | 0.4 | |
| Left gluteal abscess | 1 | 0.4 | |
| Infected scale wound | 1 | 0.4 | |
| Horse bite | 1 | 0.4 | |
| Dog bit | 1 | 0.4 | |
| Epilepsy + meningitis | 1 | 0.4 | |
| Coginital infected cyst | 1 | 0.4 | |
| Bladder stone | 1 | 0.4 | |
| Acute tonsillopharyngitis | 1 | 0.4 |
Severe acute malnutrition (SAM), diabetes mellitus, chronic renal failure, cardiac disorder.
Majority of the patients undergo elective surgery while in hospital.
Severe anemia—hemoglobin <50 g/L (for patients older than 28 days) or hemoglobin <90 g/L (for neonates).
Figure 2.
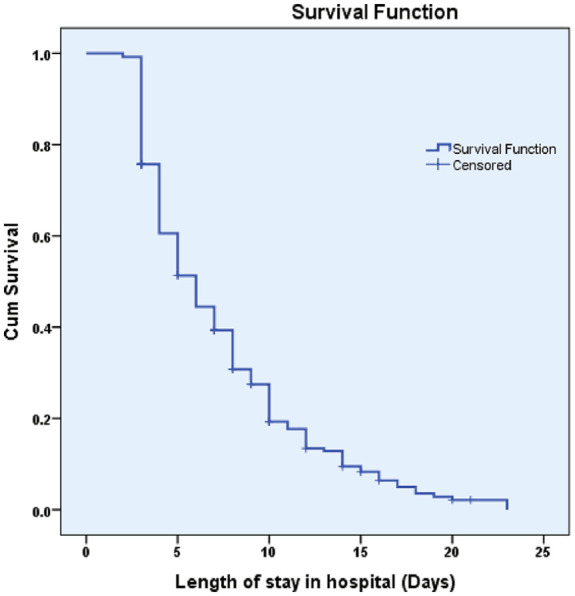
Kaplan Meier survival estimate of hospital length of stay among pediatrics admitted in the pediatric ward in Goba referral hospital, southeast Ethiopia, 2019.
Survival Probability of Time to Hospital Discharge
The log-rank test was conducted to test out for the existence of any significant differences for the time to discharge among various levels of variables. Accordingly, the Kaplan-Meier analysis indicated significant evidence on differences for time to discharge in categories of age, gestational age, HIV status, birth weight, presence of peripheral vascular catheters and presence of HAIs (Tables 3 and 4).
Table 3.
The Log-Rank Test of Predictors for Time to Hospital Discharge of Patients Admitted to NICU in Goba Referral Hospital, Ethiopia (n = 191).
| Covariates | Category | Status of the patient |
Median days (IQR) |
Log rank test | ||
|---|---|---|---|---|---|---|
| Event (n = 141) | Censored (n = 50) | Chi-square | P-value | |||
| Age (days) | 1 | 68 | 21 | 7 (10-5) | 2.90 | .234 |
| 2-4 | 33 | 15 | 10 (15-7) | |||
| ≥5 | 40 | 14 | 7 (13-4) | |||
| Gestational age | <37 weeks | 83 | 18 | 10 (15-7) | 30.37 | <.001* |
| ≥37 weeks | 108 | 32 | 7 (7-4) | |||
| Gender | Male | 73 | 24 | 7 (11-4) | 1.42 | .232 |
| Female | 68 | 26 | 7 (13-6) | |||
| Place of residence | Urban | 60 | 18 | 7(14-5) | 0.03 | .847 |
| Rural | 81 | 32 | 7 (11-5) | |||
| Previous hospitalization | Yes | 5 | 6 | 10 (15-7) | 1.68 | 1.194 |
| No | 136 | 44 | 7 (11-5) | |||
| Patient put on mechanical ventilation | Yes | 40 | 21 | 9 (15-7) | 4.08 | .043* |
| No | 101 | 29 | 7 (10-4) | |||
| Peripheral intravenous (IV) catheter | Yes | 136 | 47 | 7 (11-5) | 0.49 | .484 |
| No | 5 | 3 | 7 (9-3) | |||
| Presence of underlying diseases | Yes | 2 | 4 | 4 (4-4) | 1.22 | .265 |
| No | 139 | 46 | 7 (11-5) | |||
| Surgery after admission | Yes | 1 | 0 | 7 (7-7) | 0.19 | .662 |
| No | 140 | 50 | 7 (11-5) | |||
| Antibiotic prophylaxis was given | Yes | 5 | 2 | 4 (7-4) | 1.30 | .253 |
| No | 96 | 36 | 7 (10-6) | |||
| Severe anemia | Yes | 7 | 4 | 14 (15-10) | 3.35 | .187 |
| No | 133 | 43 | 7 (10-5) | |||
| Not tested | 1 | 3 | — | |||
| McCabe score | Nonfatal diseases | 39 | 8 | 7 (10-5) | 10.47 | .015* |
| Ultimately fatal diseases | 12 | 5 | 4 (7-3) | |||
| Rapidly fatal diseases | 32 | 15 | 12 (15-7) | |||
| Unknown | 1 | 2 | — | |||
| HAIs | Yes | 20 | 5 | 15 (21-10) | 17.42 | <.001* |
| No | 121 | 45 | 7 (10-5) | |||
| HIV status | Reactive | 1 | 1 | 4 (4-4) | 24.80 | <.001* |
| Non-reactive | 125 | 42 | 8 (13-7) | |||
| Unknown/not tested | 15 | 7 | 4 (4-3) | |||
| Birth weight | <2500 g | 37 | 9 | 10 (16-8) | 15.83 | <.001* |
| ≥2500 g | 104 | 41 | 7 (10-4) | |||
P-value < .05.
Table 4.
The Log-Rank Test of Predictors for Time to Hospital Discharge of Patients Admitted to Pediatric Ward in Goba Referral Hospital, Ethiopia (n = 247).
| Covariates | Category | Status of the patient |
Median days (IQR) | Log rank test |
||
|---|---|---|---|---|---|---|
| Event (n = 219) | Censored (n = 28) | Chi-square | P-value | |||
| Age (months) | ≤1 | 11 | 0 | 3 (6-3) | 11.85 | .008* |
| 2-5 | 20 | 2 | 7 (12-5) | |||
| 6-12 | 64 | 9 | 5 (9-3) | |||
| >12 | 124 | 17 | 6 (10-4) | |||
| Gender | Male | 128 | 17 | 5 (10-4) | 0.00 | .976 |
| Female | 91 | 11 | 6 (10-3) | |||
| Place of residence | Urban | 43 | 3 | 4 (7-3) | 4.39 | .036 |
| Rural | 176 | 25 | 6 (10-4) | |||
| Previous hospitalization | Yes | 30 | 5 | 6 (10-4) | 0.03 | .843 |
| No | 189 | 23 | 6 (10-3) | |||
| Patients put on mechanical ventilation | Yes | 10 | 2 | 5 (9-3) | 0.31 | .576 |
| No | 209 | 26 | 6 (10-4) | |||
| Peripheral intravenous (IV) catheter | Yes | 211 | 27 | 6 (10-4) | 2.49 | .114 |
| No | 8 | 1 | 4 (5-3) | |||
| Central venous catheter (CVC) | Yes | 5 | 2 | 16 (20-3) | 4.35 | .037* |
| No | 214 | 26 | 6 (10-4) | |||
| Presence of underlying diseases | Yes | 37 | 9 | 6 (10-4) | 0.26 | .606 |
| No | 182 | 19 | 5 (10-3) | |||
| Surgery after admission | Yes | 41 | 5 | 5 (10-3) | 1.59 | .207 |
| No | 178 | 23 | 6 (10-4) | |||
| Antibiotic prophylaxis was given | Yes | 145 | 17 | 6 (10-4) | 1.81 | .178 |
| No | 74 | 11 | 5 (10-3) | |||
| Severe anemia | Yes | 23 | 5 | 5 (12-4) | 1.17 | .555 |
| No | 173 | 19 | 5 (10-3) | |||
| Not tested | 23 | 4 | 7 (8-4) | |||
| McCabe score | Nonfatal diseases | 93 | 9 | 5 (10-3) | 3.54 | .315 |
| Ultimately fatal diseases | 83 | 12 | 6 (10-4) | |||
| Rapidly fatal diseases | 41 | 7 | 7 (9-3) | |||
| Unknown | 2 | 0 | 3 (8-3) | |||
| HAIs | Yes | 195 | 22 | 10 (16-6) | 10.22 | <.001* |
| No | 24 | 6 | 5 (9-3) | |||
| HIV status | Non-reactive | 194 | 24 | 5 (10-4) | 0.20 | .650 |
| Not-tested | 25 | 4 | 7 (10-3) | |||
P-value < .05.
The Log-Rank Test of Predictors for Time to Hospital Discharge among Patients Admitted to NICU
Table 3 presents the Log-rank test of predictors for time to hospital discharge among neonates. Neonates with hospital-acquired infection after admission have a longer hospital stay than those without hospital-acquired infection (14 days vs 7 days). This visually observed difference was also statistically significant (Log-rank, P-value < .001) (Figure 3). Neonates with <37 weeks of gestational age have a longer hospital stay than neonates ≥37 weeks gestational age (10 days vs 7 days; P < .001) (Figure 4). Neonates with low birth weight (P < .001) (Figure 5), and put on mechanical ventilation (P = .043) had significantly longer hospital stay.
Figure 3.
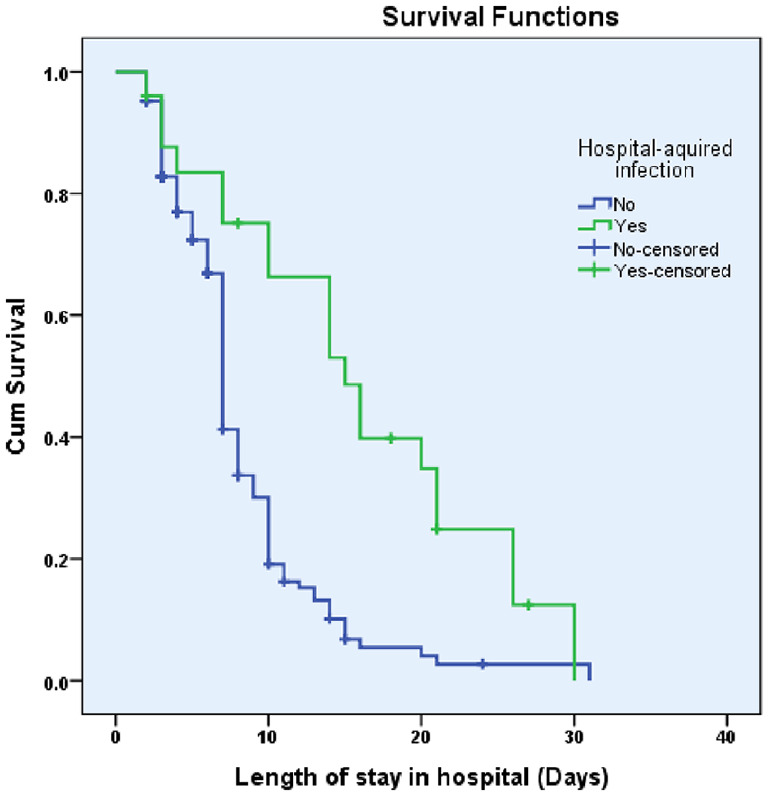
Difference in hazard of the length of stay between patients with healthcare-acquired infection (HAIs) and without HAIs among neonates in NICU.
Figure 4.
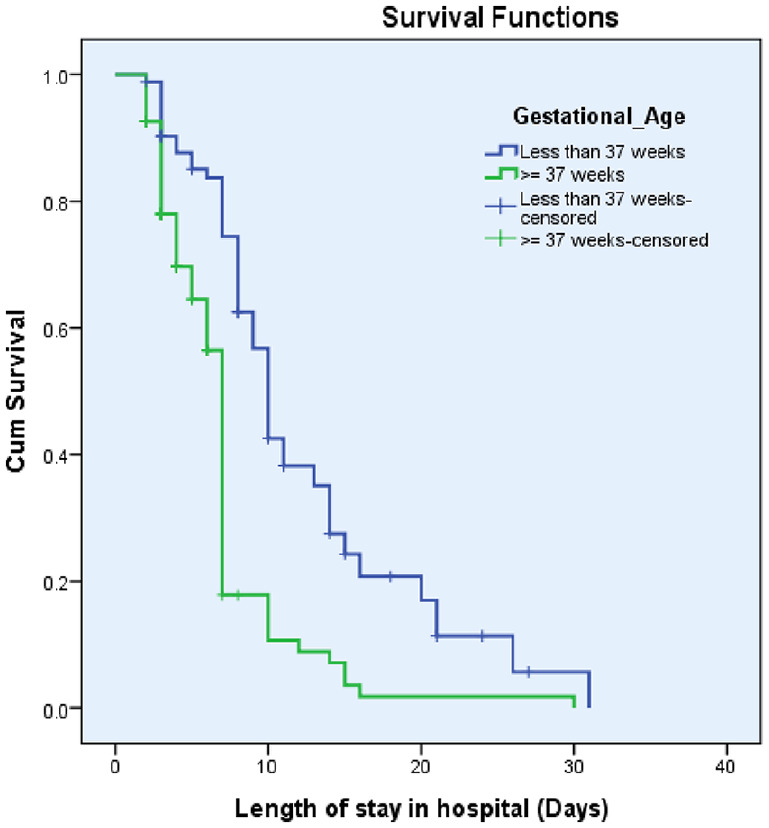
Difference in hazard of the length of stay between patients by gestational age among neonates in NICU.
Figure 5.
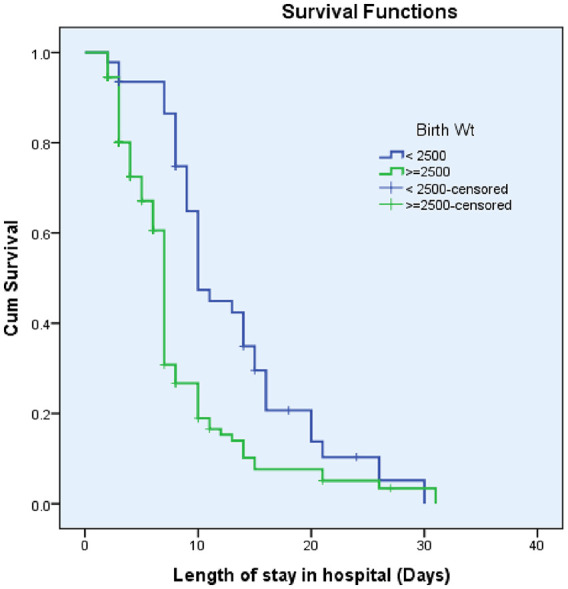
Difference in hazard of the length of stay between patients by birth weight among neonates in NICU.
The Log-Rank Test of Predictors for Time to Hospital Discharge among Patients Admitted to Pediatric Ward
The time to discharge for those children who had HAIs after pediatric ward admission was 10 days, whereas those who did not have HAIs had a median discharge time of 5 days and the difference was still significant (P value < .001) (Figure 6). And patients with the presence of central venous catheter (CVC) had a median discharge time of 16 days as compared to 6 days of patients without (P-value = .037) (Table 4).
Figure 6.
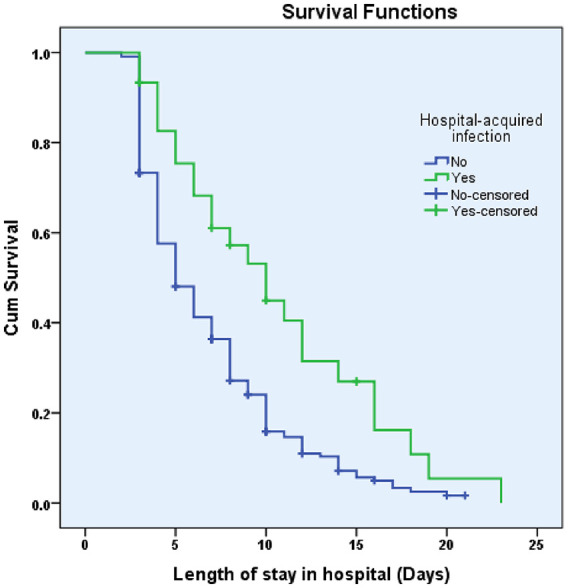
Difference in hazard of the length of stay between patients with healthcare-acquired infection (HAIs) and without HAIs among children admitted in the pediatric ward.
Predictors of Time to Discharge Among Neonates Admitted to NICU
In the bivariate analysis gestational age, birth weight, patient condition based on McCabe score, and presence of HAIs were significantly associated with hospital length of stay. However, in the multivariable Cox regression model the presence of HAIs after admission, gestational age of the neonates, and birth weight remained statistically significant. In the multivariable Cox regression, the hazard of neonates with less than 37 weeks of gestational age, low birth weight, and those who develop HAI after admission had prolonged time to discharge by 54% [adjusted hazard ratio (AHR): 0.46 (95% CI: 0.31-0.66)], 40% [AHR: 0.60, (95% CI: 0.40-0.90)], and 56% [AHR: 0.44, (95% CI: 0.26-0.74)], respectively (Table 5).
Table 5.
Multivariable Analysis (Cox Regression) of Factors Associated With Time to Hospital Discharge of Patients Admitted to NICU in Goba Referral Hospital, Ethiopia (n = 191).
| Predictors | Category | Bivariate HR (95% CI) | P-value (crude) | Multivariable HR (95% CI) | P-value (adjusted) |
|---|---|---|---|---|---|
| Age (days) | 1 | 1 | |||
| 2-4 | 0.73 (0.47-1.11) | .135 | |||
| ≥5 | 0.97 (0.65-1.43) | .875 | |||
| Gestational age | <37 weeks | 0.41 (0.29-0.59)* | <.001 | 0.46 (0.31-0.66)** | <.001 |
| ≥37 weeks | 1 | ||||
| Gender | Male | 1 | |||
| Female | 0.83 (0.59-1.16) | .276 | |||
| Previous hospitalization | Yes | 0.58 (0.24-1.43) | .243 | ||
| No | 1 | ||||
| Patients put on mechanical ventilation | Yes | 0.70 (0.48-1.02) | .067 | ||
| No | 1 | ||||
| Presence of underlying diseases | Yes | 2.11 (0.50-8.81) | .303 | ||
| No | 1 | ||||
| Antibiotic prophylaxis given | Yes | 1.60 (0.65-3.96) | .304 | ||
| No | 1 | ||||
| Sever anemia | Yes | 0.66 (0.08-5.44) | .703 | ||
| No | 1.25 (0.17-8.99) | .824 | |||
| Not tested | 1 | ||||
| McCabe score | Nonfatal diseases | 1 | |||
| Ultimately fatal diseases | 1.42 (0.77-2.62) | .250 | |||
| Rapidly fatal diseases | 0.61 (0.40-0.91)* | .017 | |||
| Unknown | 1.34 (0.18-9.79) | .769 | |||
| HAIs | Yes | 0.38 (0.23-0.63)* | <.001 | 0.44(0.26-0.74)** | .002 |
| No | 1 | 1 | |||
| HIV status | Reactive | 1 | |||
| Non-reactive | 0.31 (0.04-2.33) | .260 | |||
| Unknown/not tested | 1.14 (0.15-8.71) | .894 | |||
| Birth weight | <2500 g | 0.49 (0.34-0.73)* | <.001 | 0.60 (0.40-0.90)** | .014 |
| ≥2500 g | 1 | 1 |
Abbreviation: HR, hazard ratio.
Significant association (P-value < .05) crude.
Significant association (P-value < .05) adjusted.
Predictors of Time to Discharge Among Children Admitted to the Pediatric Ward
After adjusting other covariates, the presence of HAIs was found to be the independent predictor of LOS in children admitted to the pediatric ward. The hazard of time to discharge among patients who had HAIs after admission had delayed discharge time by 49% [AHR: 0.51, (95% CI: 0.33-0.79)] compared to patients without HAIs (Table 6).
Table 6.
Multivariable Analysis (Cox Regression) of Factors Associated With Time to Hospital Discharge of Patients Admitted to Pediatric Ward in Goba Referral Hospital, Ethiopia (n = 247).
| Predictors | Category | Bivariate HR (95% CI) | P-value (crude) | Multivariable HR (95% CI) | P-value (adjusted) |
|---|---|---|---|---|---|
| Age (months) | ≤1 | 2.43 (1.30-4.54)* | .005 | ||
| 2-5 | 0.92 (0.57-1.48) | .743 | |||
| 6-12 | 1.22 (0.90-1.65) | .196 | |||
| >12 | 1 | ||||
| Gender | Male | 1.00 (0.76-1.31) | .978 | ||
| Female | 1 | ||||
| Place of residence | Urban | 1.38 (0.98-1.93) | .060 | 1.39 (0.99-1.95) | .060 |
| Rural | 1 | 1 | |||
| Previous hospitalization | Yes | 0.96 (0.65-1.42) | .859 | ||
| No | 1 | ||||
| Patients put on mechanical ventilation | Yes | 0.84 (0.44-1.60) | .613 | ||
| No | 1 | ||||
| Peripheral intravenous (IV) catheter | Yes | 0.60 (0.29-1.22) | .162 | ||
| No | 1 | ||||
| Central venous catheter (CVC) | Yes | 0.42 (0.17-1.05) | .065 | 0.44 (0.17-1.10) | .080 |
| No | 1 | 1 | |||
| Presence of underlying diseases | Yes | 0.91 (0.64-1.31) | .643 | ||
| No | 1 | ||||
| Surgery after admission | Yes | 0.81 (0.57-1.15) | .256 | ||
| No | 1 | ||||
| Antibiotic prophylaxis given | Yes | 0.84 (0.63-1.11) | .226 | ||
| No | 1 | ||||
| Sever anemia | Yes | 0.76 (0.42-1.38) | .380 | ||
| No | 0.94 (0.60-1.46) | .789 | |||
| Not tested | 1 | ||||
| McCabe score | Nonfatal diseases | 1 | |||
| Ultimately fatal diseases | 0.78 (0.58-1.06) | .120 | |||
| Rapidly fatal diseases | 0.85 (0.59-1.23) | .394 | |||
| Unknown | 1.35 (0.33-5.51) | .671 | |||
| HAIs | Yes | 0.53 (0.34-0.82)* | .004 | 0.51 (0.33-0.79)** | .003 |
| No | 1 | 1 | |||
| HIV status | Non-reactive | 1 | |||
| Not tested | 1.09 (0.71-1.66) | .683 |
Abbreviation: HR, hazard ratio.
−2 Log likelihood: 2053.708.
Significant association (P-value < .05) crude.
Significant association (P-value < .05) adjusted.
Discussion
Accurate information on factors associated with hospital length of stay (LOS) in the neonatal and pediatric units, and what factors are important to aid the prediction of time to discharge has become increasingly essential, and facilitate the improvement of good clinical outcomes.20 This prospective follow up study assessed the predictors of time to hospital discharge among children admitted to the NICU and pediatric ward at Goba referral hospital. In this study, the independent predictors of prolonged hospital LOS among neonates in the NICU were the presence of HAIs, gestational age, and birth weight. Similarly, the presence of HAIs was found to be the independent predictor LOS in children admitted to the pediatric ward.
The median hospital stay reported in our study finding was ≤7 days and ≤6 days for children’s admitted to NICU and pediatric ward, respectively. The overall median LOS reported in this study was 7 days, which is similar to a nationwide study conducted elsewhere.22 However, higher LOS (14 days) has also been reported among patients who presented undernutrition risk on hospital admission in the United States.23 This might be because the study population dissimilarity and also may be associated with the type of study design.
The Kaplan-Meier analysis indicated significant differences in hospital LOS in the categories of patients with HAIs. The median LOS for patients who developed HAIs after 48hours of hospital admission in the NICU and the pediatric ward was significantly higher compared with those without HAIs. This was not a surprising finding in our analysis; it is already known that HAI increases LOS among hospitalized patients. A recent report by Ali et al in Ethiopia also revealed that HAIs were associated with prolonged hospital stay by 6 and more days. In the multivariable analysis, the hazard of patients with HAI after admission in the NICU and pediatric ward had prolonged time to discharge by 56% and 49% compared to patients without HAIs, respectively. Again, this finding is almost similar with the study conducted in Ethiopia which indicates that the mean duration of hospital stay for HAI patients was 13.95 days while that of patients without HAI was 7.63 days and there is a significant mean difference of 6.32 days (P-value < .001) between the 2 groups. Other studies from Kenya reported Nosocomial bacteremia lengthened hospital stay by 10.1 days.24 The present prolonged LOS associated with HAI has several implications in terms of quality of care, the financial burden for health systems, patient satisfaction, and health outcome.25-28
In this study, the overall incidence density rate of admitted pediatrics mortality was 10.2 per 1000 pediatrics days of follow up. In contrast, a study conducted in Arba Minch General hospital (South Ethiopia) reported a 3 times lower incidence density rate of neonatal mortality was reported, 31.6 per 1000 neonate days.29 This might be because the study includes neonates who were admitted to NICU and uses a retrospective cohort method. The finding implies that neonatal mortality is still a significant problem in Ethiopia at 29/1000 live births as reported by the 2016 National study.30
In the present study, inherent factors particularly low birth weight and lower gestational were important variables associated with longer LOS among neonates. This finding was supported by previous studies.8,13,19,20,31,32
Limitation of the Study
We acknowledge that there are several limitations to this study. First, the criteria for admission and discharges may have been variable among different physicians taking care of pediatric patients and could interfere with the results of our findings. Second, the study is limited to one university hospital and the findings may not be generalizable. Third, data did not span up to a year to capture all seasonal variations in hospitalization and length of stay of pediatric patients. Fourth, despite we gathered data for 8 of 12 months of the year, almost less than the excepted average population was included. The possible responses were due to the establishment of NICU service in other hospitals of the Bale zone, and the other was due to consenting issues (as all admitted children were not involved in the present study), which possibly affected our results. The fifth limitation relates to the fact that there we did not include children who would be admitted to the pediatric emergency room during the study period. As a result, the reader should consider the necessary precautionary measures while interpreting the current findings. Since the study was conducted in a governmental referral hospital, the generalization of the study findings is limited to such facilities in low-income settings.
Conclusion
Developing hospital-acquired infection (HAIs) after 48 hours of hospital admission, neonates with <37 weeks of gestational age, and low birth weight were found to be the independent predictor of longer hospital stay for neonates admitted to NICU. On a similar note, the presence of HAIs was associated with prolonged hospital stay among patients admitted to the pediatric ward. The study findings have important implications for quality of care and patient safety in the country.
Footnotes
Author Contributions: BS: Conceptualized, designed the study, data curation, and designed the manuscript; supervised, analyzed, and interpreted data; drafted the initial manuscript; reviewed and revised the manuscript; and approved the final manuscript as submitted.
YT, DZ, DW and ZT: Contributed to the analysis, critically reviewed the manuscript, and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Biniyam Sahiledengle  https://orcid.org/0000-0002-1114-4849
https://orcid.org/0000-0002-1114-4849
Availability of Data and Materials: Data will be available upon request from the corresponding authors.
References
- 1. Asghar Ghods A, Khabiri R, Raeisdana N, et al. Predictors of inappropriate hospital stay: experience from Iran. Glob J Health Sci. 2015;7:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Panis LJ, Gooskens M, Verheggen FW, Pop P, Prins MH. Predictors of inappropriate hospital stay: a clinical case study. Int J Qual Health Care. 2003;15:57-66. [DOI] [PubMed] [Google Scholar]
- 3. Khechen B, Haws BE, Patel DV, et al. Risk factors for a long hospital stay following minimally invasive lumbar discectomy. Clin Spine Surg. 2019;32:56-59. [DOI] [PubMed] [Google Scholar]
- 4. Sasaki J, Dykes JC, Sosa LJ, et al. Risk factors for longer hospital stay following the Fontan operation. Pediatr Crit Care Med. 2016;17:411-419. [DOI] [PubMed] [Google Scholar]
- 5. Barisonzo R, Wiedermann W, Unterhuber M, Wiedermann CJ. Length of stay as risk factor for inappropriate hospital days: interaction with patient age and co-morbidity. J Eval Clin Pract. 2013;19:80-85. [DOI] [PubMed] [Google Scholar]
- 6. Vieira NB, Rodríguez-Vera J, Ferrão E, et al. Appropriateness of hospitalization in a ward of internal medicine—using the Appropriateness Evaluation Protocol. Acta Med Port. 2006;19:67-70. [PubMed] [Google Scholar]
- 7. O’Brien JE, Dumas HM. Hospital length of stay, discharge disposition, and reimbursement by clinical program group in pediatric post-acute rehabilitation. J Pediatr Rehabil Med. 2013;6:29-34. [DOI] [PubMed] [Google Scholar]
- 8. Altman M, Vanpée M, Cnattingius S, Norman M. Moderately preterm infants and determinants of length of hospital stay. Arch Dis Child Fetal Neonatal Ed. 2009; 94:414-418. [DOI] [PubMed] [Google Scholar]
- 9. Shanley LA, Lin H, Flores G. Factors associated with length of stay for pediatric asthma hospitalizations. J Asthma. 2015;52:471-477. [DOI] [PubMed] [Google Scholar]
- 10. Bender GJ, Koestler D, Ombao H, et al. Neonatal intensive care unit: predictive models for length of stay. J Perinatol. 2013;33:147-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Manktelow B, Draper ES, Field C, Field D. Estimates of length of neonatal stay for very premature babies in the UK. Arch Dis Child Fetal Neonatal Ed. 2010;95:288-292. [DOI] [PubMed] [Google Scholar]
- 12. Albergotti WG, Sturm JJ, Stapleton AS, Simons JP, Mehta DK, Chi DH. Predictors of intensive care unit stay after pediatric supraglottoplasty. JAMA Otolaryngol Head Neck Surg. 2015;141:704-709. [DOI] [PubMed] [Google Scholar]
- 13. Berry MA, Shah PS, Brouillette RT, Hellmann J. Predictors of mortality and length of stay for neonates admitted to children’s hospital neonatal intensive care units. J Perinatol. 2008;28:297-302. [DOI] [PubMed] [Google Scholar]
- 14. Conner JM, Aviles-Robles MJ, Asdahl PH, Zhang FF, Ojha RP. Malnourishment and length of hospital stay among paediatric cancer patients with febrile neutropaenia: a developing country perspective. BMJ Support Palliat Care. 2016;6:338-343. [DOI] [PubMed] [Google Scholar]
- 15. Huet B, Cauterman M. Real association of factors with inappropriate hospital days. Stud Health Technol Inform. 2005;116:1021-1026. [PubMed] [Google Scholar]
- 16. Smith JL, De Nadai AS, Petrila J, Storch EA. Factors associated with length of stay in emergency departments for pediatric patients with psychiatric problems. Pediatr Emerg Care. 2019;35:716-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bender GJ, Koestler D, Ombao H, et al. Neonatal intensive care unit: predictive models for length of stay. J Perinatol. 2013;33:147-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Profit J, McCormick MC, Escobar GJ, et al. Neonatal intensive care unit census influences discharge of moderately preterm infants. Pediatrics. 2007;119:314-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hintz SR, Bann CM, Ambalavanan N, Cotten CM, Das A, Higgins RD. Predicting time to hospital discharge for extremely preterm infants. Pediatrics. 2010;125:146-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Seaton SE, Barker L, Jenkins D, Draper ES, Abrams KR, Manktelow BN. What factors predict length of stay in a neonatal unit: a systematic review. BMJ Open. 2016;6:e010466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309-332. [DOI] [PubMed] [Google Scholar]
- 22. Bessaha ML, Shumway M, Smith ME, Bright CL, Unick GJ. Predictors of hospital length and cost of stay in a national sample of adult patients with psychotic disorders. Psychiatr Serv. 2017;68:559-565. [DOI] [PubMed] [Google Scholar]
- 23. Maia I, Xará S, Vaz D, Shiang T, Amaral TF. Undernutrition risk at hospital admission and length of stay among pulmonology inpatients. Pulmonology. 2018; 24:330-336. [DOI] [PubMed] [Google Scholar]
- 24. Aiken AM, Mturi N, Njuguna P, et al. Risk and causes of paediatric hospital-acquired bacteraemia in Kilifi District Hospital, Kenya: a prospective cohort study. Lancet. 2011;378:2021-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Uwaezuoke SN, Obu HA. Nosocomial infections in neonatal intensive care units: cost-effective control strategies in resource-limited countries. Niger J Paediatr. 2013;40: 125-132. [Google Scholar]
- 26. Allegranzi B, Nejad SB, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377:228-241. [DOI] [PubMed] [Google Scholar]
- 27. Magill SS, Hellinger W, Cohen J, et al. Prevalence of healthcare-associated infections in acute care hospitals in Jacksonville, Florida. Infect Control Hosp Epidemiol. 2012;33:283-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zernikow B, Holtmannspötter K, Michel E, et al. Predicting length-of-stay in preterm neonates. Eur J Pediatr. 1999;158:59-62. [DOI] [PubMed] [Google Scholar]
- 29. Dessu S, Kote M, Gebremeskel F, Girum T. Predictors of neonatal mortality among neonates who admitted in Neonatal Intensive Care Unit at Arba Minch General Hospital. Ethiop J Health Dev. 2019;33:46-52. [Google Scholar]
- 30. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. CSA and ICF; 2016. [Google Scholar]
- 31. Maier R, Blondel B, Piedvache A, et al. Duration and time trends in hospital stay for very preterm infants differ across European regions. Pediatr Crit Care Med. 2018; 19:1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mahovo R, Velaphi S. Duration of hospital stay and factors assocaited with prolonged hospital stay in very low birth weight infants surviving to hospital discharge. J Pediatr Perinatol Child Health. 2019;3:208-220. [Google Scholar]


