Abstract
Despite renewed national interest in mental health care reform, little is known about treatment patterns among youth in the general population. Using longitudinal data from the Medical Expenditure Panel Survey, we examined both initiation and continuity of mental health treatment among 2,576 youth aged 5 to 17 with possible mental health treatment need (defined as a high score on a parent-assessed psychological impairment scale, fair/poor mental health status, or perceived need for counseling). Over a 2-year period, fewer than half of sampled youth initiated new mental health treatment. Minority, female, uninsured, and lower-income youth were significantly less likely to initiate care. Only one third of treatment episodes met criteria for minimal adequacy (≥4 provider visits with psychotropic medication treatment or ≥8 visits without medication). Episodes were significantly shorter for Latino youth. Efforts to strengthen mental health treatment for youth should be broadly focused, emphasizing not only screening and access but also treatment continuity.
Keywords: mental health treatment, episodes of care, quality, access, children, adolescents
Introduction
Developmental, emotional, and behavioral conditions are now the leading causes of disability among youth in the United States (Halfon, Houtrow, Larson, & Newacheck, 2012). These problems have been linked to negative social and physical health outcomes in adulthood (Shonkoff et al., 2012; Smith & Smith, 2010).
Although advocates have long called for improved screening and access to care for youth with mental health problems, recent events, including the fatal shooting of 20 children and 6 adults at an elementary school by an emotionally troubled young man in 2012, have cast renewed attention on the critical lack of supports for high-risk youth (Begley, 2012). These events have spurred bipartisan support for expanded community mental health treatment (Peters, 2013). The White House 2014 budget included a $130 million initiative that would increase funding for counseling and training of youth mental health professionals and expand teacher training to screen youth with mental health problems (Office of Management and Budget, 2014).
As policymakers continue to debate how to improve mental health treatment for youth, they will need accurate data on the quality of this care. As a first step toward quality assessment, it is important to characterize patterns of treatment among youth in the general population, including the duration and intensity of care being provided. Unfortunately, there is a dearth of evidence to inform policy proposals. Recent initiatives, including the Children’s Health Program Reauthorization Act of 2009, have identified a critical lack of data on patterns of mental health service use as a barrier to monitoring treatment and improving treatment quality for publicly insured youth (Dougherty, Schiff, & Mangione-Smith, 2011; Zima et al., 2013).
New Contribution
Our study uses longitudinal data from the Medical Expenditure Panel Survey (MEPS), a nationally representative survey of noninstitutionalized individuals in the United States. Relatively little literature has examined mental health treatment patterns over time, and these studies have either focused on youth with specific diagnoses (Olfson, Gameroff, Marcus, & Waslick, 2003; Stein et al., 2013; Zima et al., 2010) or within specific geographic areas (Costello, Copeland, Cowell, & Keeler, 2007; Garland et al., 2005).
Other studies that have examined youth in the general population with possible mental health problems use data from a single cross-sectional survey and focus on service utilization over a prior period (typically 12 months). Such studies have found that 20% to 50% of all youth with possible mental health problems used mental health treatment in a prior period, and rates were lowest for minority and low-income youth (Jensen et al., 2011; Kataoka, Zhang, & Wells, 2002; Merikangas et al., 2010; Merikangas et al., 2011). These studies do not, however, permit researchers to assess the temporal sequence of treatment. In our study, we separately assess factors that predict initiation of new versus ongoing treatment and examine predictors of treatment intensity once contact has been made with the treatment system.
Conceptual Framework
An episode of care is “a series of temporally contiguous health care services related to treatment of a given spell of illness” (Hornbrook, Hurtado, & Johnson, 1985, p. 171). A typical episode of mental health care consists of an initial evaluation followed by a trial of medication or psychotherapy, after which the course of treatment may be maintained, modified, or discontinued. Examining the linked process of initiating and maintaining treatment provides a better representation of a patient’s experience in treatment than considering each use of services or medication as a discrete event.
In particular, an episodes framework provides insight into the rate of discontinuation after an initial visit, the frequency of contact with a provider, and the median length of time in treatment. These measures do not, by themselves, establish the quality or appropriateness of care rendered for a particular patient, but they do provide an indication of whether care is likely to be fragmented or particularly low intensity for particular populations.
Figure 1 provides a graphical representation of the variety of different types of episodes. Longer duration treatment often persists for more than 1 year (Child 1) and can consist of a mix of outpatient mental health visits and psychotropic medication use. By contrast, an episode could be as short as an isolated 30-day fill of a medication or a provider visit on a single day (as represented by Child 2’s first episode). Although most courses of psychotropic treatment are initiated with a provider office visit, it is possible that an episode of medication treatment may involve little or no proximal contact with a physician (as represented by Child 2’s second episode).
Figure 1.
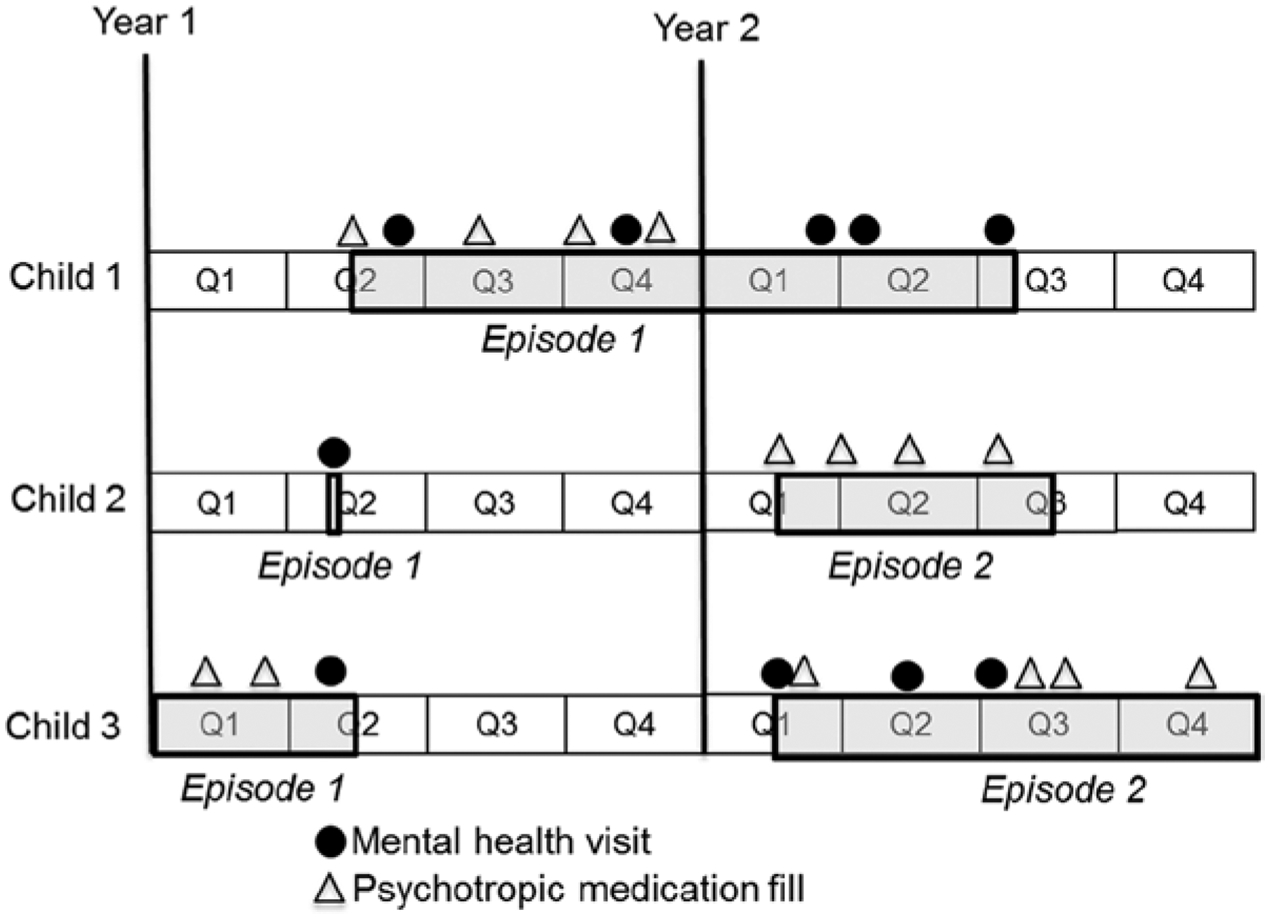
Representation of treatment episodes among three hypothetical children.
There are several challenges associated with measuring episodes, which we address in more detail below. Episodes do not always have sharp boundaries, particularly for individuals with intermittent patterns of utilization. Following other studies in the episodes literature, we define a new episode as treatment initiated after at least 12 weeks without any mental health treatment. While new episodes may continue care for an already-diagnosed condition, they are likely to require new evaluation and intake. Another methodological problem pertains to episodes beginning before, or terminating after, the observation window (Child 3). These episodes are considered to be left-censored and right-censored, respectively, and we account for the censoring process in our regression models.
Method
Study Sample
The MEPS is a nationally representative survey of noninstitutionalized households in the United States (Ezzati-Rice, Rohde, & Greenblatt, 2008). An adult member of the household, usually a parent, provided information about youth under age 18. Households in the MEPS are followed for 2-year periods, and records of treatment utilization were collected five times over a 2-year period. We focus on panels 9 to 13 of the MEPS (calendar years 2004–2009). The full-year response rate for these years was between 57.2% and 63.1%. We adjust for attrition and nonresponse using the longitudinal survey weights.
The MEPS includes several measures to assess mental health functioning in youth. We defined our study sample using three measures collected during the first two interviews. Specifically, we included youth aged 5 to 17 if they met at least one of the following binary criteria: (a) composite score on the Columbia Impairment Scale (CIS) >15, (b) adult respondent rated the youth’s mental health as fair or poor, (c) the adult indicated that the youth had “an emotional, developmental, or behavioral problem for which he or she needs or gets treatment or counseling” (hereafter referred to as “needs counseling”). The pairwise correlations coefficients between these three constructs in the study sample were 0.37 (fair/poor mental health and “needs counseling”), 0.38 (CIS scale and fair/poor mental health), and 0.48 (CIS scale and “needs counseling”).
The CIS is a 13-item scale measuring psychological functioning and impairment in youth (items are displayed in Table 1). Scores can range from 0 to 52 points, with higher scores indicating greater impairment. The parent-administered CIS has been validated in multiethnic community samples, where it demonstrated high test–retest reliability (Bird et al., 1996). The cut-point of >15 was derived using discriminant function analysis and is predictive of other measures of psychological dysfunction and clinician-rated global impairment (Bird et al., 1996). Our final sample consisted of 2,576 youth, or 13.8% of the weighted youth population (by comparison, recent data suggest that the population prevalence of mental disorders among youth is 13% to 20%; Perou et al., 2013).
Table 1.
Columbia Impairment Scale.
| Probe: Please rate on a scale of 0 to 4, where 0 indicates no problem and 4 indicates a very big problem, how much of a problem you think [the child] has with … |
| Getting along with (his/her) mother? |
| Getting along with (his/her) father? |
| Feeling unhappy or sad? |
| (His/her) behavior at school? |
| Having fun? |
| Getting along with other adults? |
| Feeling nervous or afraid? |
| Getting along with brothers and sisters? |
| Getting along with other kids? |
| Getting involved in activities like sports or hobbies? |
| (His/her) schoolwork? |
| (His/her) behavior at home? |
| Staying out of trouble? |
Source. Columbia Impairment Scale. Reproduced from the Child Preventive Health Supplement Section of the Medical Expenditure Panel Survey. Available at http://meps.ahrq.gov/survey_comp/hc_survey/2011/CS110311.htm
Defining Treatment Episodes
New episodes were defined as mental health treatment preceded by at least 12 weeks without treatment (Keeler, Manning, & Wells, 1988; Tansella, Micciolo, Biggeri, Bisoffi, & Balestrieri, 1995; Teh et al., 2010). Information about provider visits, including dates and diagnoses, were collected for each member of the household in each of the five survey rounds. Mental health treatment was considered to be any of the following: (a) a provider visit associated with a mental health diagnosis (ICD-9 codes 291, 292, or 295–314), (b) filled prescriptions for a mental health diagnosis; and/or (c) filled prescriptions specifically for psychotropic medications according to the Multum classification system (Multum, n.d.). MEPS respondents report mental health diagnoses with high accuracy (Machlin, Cohen, Elixhauser, Beauregard, & Steiner, 2009). Additionally, information reported by MEPS respondents is routinely verified using follow-back surveys with the physicians, hospitals, and pharmacies (Agency for Healthcare Research and Quality, 2008).
Timing of prescription fills, with the exception of the start date, is not available by date, only by survey round. To impute fill dates, we incorporated the date the respondent started the prescription and the total number of prescription fills during the round (if one fill, we impute the day in the middle of the round, for two fills we impute two dates 1/3 and 2/3 of the way through the round, etc.). This method is described elsewhere (Selden, 2009).
Outcome Measures
We identified, first, whether the youth received any treatment, and second, where we observed new treatment, whether it was initiated with a specialist (psychiatrist, psychologist, counselor, or social worker) rather than a primary care provider. After treatment was initiated, we considered outcomes related to duration. We measured the length of episodes in days and the total number of outpatient visits to providers. To assess the rates of follow-up after an initial visit, we measured the proportion of youth with more than one visit in an episode. We also constructed a measure of “minimally adequate care,” defined as eight or more mental health visits, or four or more mental health visits with receipt of a psychotropic medication. These definitions are consistent with treatment guidelines for depression and attention-deficit/hyperactivity disorder (Center for Medicaid and CHIP Services, 2012; Harman, Edlund, & Fortney, 2004), two of the most common diagnoses in youth. Similar definitions have been applied in other studies of youth treatment (Carson, Stewart, Lin, & Alegria, 2011; Christakis & Lozano, 2003; Katon, Richardson, Russo, Lozano, & McCauley, 2006).
Predictor Variables
We included predictors based on prior studies of youth mental health treatment: indicators of need (mental and physical health status, age, and sex; Cunningham & Freiman, 1996), insurance status (Stevens, Harman, & Kelleher, 2005), sociodemographic factors (race/ethnicity, household income, parent marital status; Cook, Barry, & Busch, 2013), parental mental health status (Olfson, Marcus, Druss, Alan Pincus, & Weissman, 2003), region (Kataoka et al., 2002), and year. Age was categorized in two groups (5–12, 13–17 years) to separate children and adolescents; household income was classified in groups in relation to the federal poverty level (FPL); parental marital status included married, divorced, or single. Race/ethnicity was identified using census-based measures. Hispanic youth were identified using an ethnicity question. All other youth were classified as Black, White, or “other race.” Measures of mental health status were parent-reported, including the CIS score, 5-point mental health status, and the indicator for whether the youth needed treatment for a mental health condition. Physical health variables included a 5-point physical health status score and indicators that the youth was assessed to be “less healthy than other children”; had any activity-limiting condition; and had ever been diagnosed with asthma, a chronic condition highly comorbid with mental health problems among youth (McQuaid, Kopel, & Nassau, 2001).
Except for asthma diagnosis (which was not collected in earlier panels and therefore missing for 38% of the sample), the percent missing was less than 15% for all predictors. We used multiple imputation to create five completed data sets, analyzed each set, and used standard rules to combine estimates and adjust standard errors for the uncertainty due to imputation (Rubin, 1998).
Statistical Analysis
We calculated descriptive statistics for the sample, applying MEPS survey weights. Because treatment patterns may differ by developmental stage, we stratified our sample by age in unadjusted analysis. We calculated the percentage in each group that had any episodes of care, including youth with episodes already underway at baseline. We calculated the percentage of new episodes (those that did not begin in the first 12 weeks), the percentage that began with specialists, the percentage of episodes that were minimally adequate, and those that consisted of more than one visit. We also calculated the mean number of days and visits per episode.
All of our regression analyses accounted for left- and right-censoring using censored normal regression. This method is equivalent to standard survival analysis techniques using a normal distribution for the dependent variable. The model identifies a cumulative density function that best fits the fully observed portion of the data under the assumption of normal distribution. Left-censored values (i.e., those related to episodes initiated before the observation period) and right-censored values (episodes concluding after the observation period) are predicted by applying the same density function to those portions of the data. Model parameters are estimated by combining estimates from the observed and censored portions of the data (Schnedler, 2005).
For binary dependent variables (i.e., adequate care), the coefficients can be interpreted as the effect, in percentage points, of a one unit change in the predictor variables. Regression models included the predictors described above. Continuous predictors were mean-standardized, so regression coefficients can be interpreted as the marginal effect of a one standard deviation change in the predictor. Regressions were survey-weighted and standard errors and confidence intervals accounted for the complex sampling design.
Results
Sample statistics are displayed in Table 2 for the full sample as well as for the subsamples that were racial/ethnic minorities and met the criterion for high CIS score (33.7% and 65.4% of the full sample, respectively). In the full sample, 51.2% of the sample was in the younger age group (5–12 years old), 45.3% of the sample had managed care, 36.9% were enrolled in public insurance, 22.6% had family incomes below 125% FPL, and 57.5% lived with married parents. The minority subsample had greater use of public insurance and higher family poverty rates, whereas the CIS sample was similar to the full sample in most demographic categories.
Table 2.
Descriptive Statistics for Sample Population.
| Full sample | Minority subsample | High CIS score subsample | ||||
|---|---|---|---|---|---|---|
| Variable name | Est. | SE | Est. | SE | Est. | SE |
| Sample characteristics (survey-weighted) | ||||||
| Female | 41.7% | 1.37 | 43.1% | 1.86 | 40.8% | 1.86 |
| Age 5–12 | 51.2% | 1.39 | 50.9% | 2.05 | 55.5% | 1.84 |
| Race/ethnicity | ||||||
| White | 63.3% | 1.54 | — | — | 67.6% | 1.90 |
| Black | 15.2% | 1.10 | 41.4% | 2.26 | 14.4% | 1.34 |
| Hispanic | 15.2% | 0.95 | 41.4% | 2.00 | 12.3% | 1.12 |
| Other race | 6.3% | 0.82 | 17.2% | 1.56 | 5.7% | 0.98 |
| Health insurance coverage | ||||||
| Any managed care | 45.3% | 1.69 | 55.0% | 2.49 | 44.9% | 2.07 |
| Private health insurance | 56.4% | 1.62 | 39.9% | 2.44 | 57.2% | 2.08 |
| Public insurance | 36.9% | 1.43 | 52.9% | 2.55 | 35.7% | 1.81 |
| Uninsured | 6.7% | 0.86 | 7.2% | 1.10 | 7.0% | 1.10 |
| Income as % of federal poverty line (FPL) | ||||||
| >125% FPL | 22.6% | 1.24 | 35.1% | 1.05 | 22.9% | 1.59 |
| 125–200% FPL | 6.8% | 0.88 | 7.5% | 1.82 | 5.8% | 1.00 |
| 201–300% FPL | 17.6% | 1.15 | 20.8% | 2.14 | 17.6% | 1.47 |
| 301–400% FPL | 32.1% | 1.53 | 24.2% | 1.58 | 33.7% | 1.98 |
| <400% FPL | 20.9% | 1.52 | 12.3% | 4.31 | 20.0% | 1.85 |
| Mental health | ||||||
| CIS score (0–52) | 17.8 | 0.28 | 16.6 | 0.43 | 22.5 | 0.24 |
| Child needs counseling | 52.4% | 1.6 | 52.8% | 2.60 | 42.3% | 1.98 |
| Mental health status (1–5 scale, 5 = poor) | 2.4 | 0.03 | 2.5 | 0.05 | 2.4 | 0.04 |
| Physical health | ||||||
| Physical health status (1–5 scale, 5 = poor) | 2.10 | 0.03 | 2.2 | 0.05 | 2.10 | 0.04 |
| Asthma | 17.3% | 1.25 | 21.6% | 1.76 | 16.9% | 1.50 |
| Child is less healthy | 16.7% | 0.96 | 18.6% | 1.66 | 17.3% | 1.32 |
| Activity limitation | 3.3% | 0.51 | 3.5% | 0.57 | 3.0% | 0.53 |
| Parental characteristics | ||||||
| Divorced parent | 28.4% | 1.38 | 30.1% | 2.17 | 28.5% | 1.73 |
| Single parent | 14.1% | 0.94 | 27.3% | 1.91 | 14.2% | 1.23 |
| Married parents | 57.5% | 1.54 | 42.6% | 2.21 | 57.2% | 2.05 |
| Parent mental health status (1–5 scale, 5 = poor) | 2.34 | 0.04 | 2.41 | 5.36 | 2.30 | 0.05 |
| Region | ||||||
| South | 35.1% | 1.74 | 38.1% | 2.45 | 34.7% | 2.00 |
| West | 23.9% | 1.39 | 29.7% | 2.05 | 24.7% | 1.80 |
| Midwest | 23.2% | 1.53 | 16.9% | 1.47 | 24.2% | 1.89 |
| Northeast | 17.7% | 1.3 | 15.4% | 1.41 | 16.4% | 1.65 |
Note. CIS = Columbia Impairment Scale. Mental/physical health status and CIS score variables expressed in original scales. Minority subsample consists of all children not classified as non-Hispanic white.
Mean CIS scores were 17.8 for the full sample, 16.6 for the minority sample, and 22.5 for the sample with elevated CIS scores (a group that by construction had a CIS > 15). More than half of the overall sample had an indicated need for counseling, and 42.3% of the high CIS sample met this condition. About one third of the three groups had mental health status rated as “fair or poor.”
Treatment Access and Specialist Initiation
In unadjusted analysis (Table 3), we found that 43.9% of the younger sample had any episode of care (95% confidence interval [CI] = 39.6%, 48.3%). Just under half (46.1%) of all episodes were initiated with a mental health specialist (95% CI = 40.3%, 51.8%) versus a primary care provider (such as a pediatrician). Almost three quarters of episodes included medication treatment (72.5%, 95% CI = 66.1%, 79.0%). Older youth had similar initiation rates and use of medications. They were less likely to initiate with a specialist (38.2%, 95% CI = 30.0%, 46.9%).
Table 3.
Unadjusted Percentage of Youth With Episodes Overall, Episodes With Medication, and Initiation of Episodes With Mental Health Specialists.
| Age 5–12 | Age 13–17 | |||
|---|---|---|---|---|
| Estimate | 95% CI | Estimate | 95% CI | |
| Percentage of youth initiating any episode | 43.9% | (39.6%, 48.3%) | 43.9% | (40.1%, 47.7%) |
| Percentage of episodes that include medication treatment | 72.5% | (66.1%, 79.0%) | 71.2% | (64.2%, 78.2%) |
| Percentage of episodes initiated with mental health specialists | 46.1% | (40.3%, 51.8%) | 38.2% | (30.0%, 46.9%) |
Note. CI = confidence interval. An episode of care was defined as mental health treatment preceded by at least 12 weeks without treatment. Estimates are survey-weighted.
In regression analysis (Table 4), several variables were found to significantly decrease the probability of initiating treatment: female gender (−.06, 95% CI = −0.11, −0.01) compared to male; Black race (−0.12, 95% CI = −0.19, −0.05) or Hispanic ethnicity (−0.07, 95% CI = −0.14, −0.01) compared to Whites; uninsured (−0.16, 95% CI = −0.26, −0.05) compared to privately insured; income <125% FPL (−0.12, 95% CI = −0.19, −0.04) and income 201% to 300% FPL (−0.09, 95% CI = −0.15, −0.12) compared to income 301% to 400% FPL; and worse physical health status (−0.06, 95% CI = −0.1, −0.03). Conversely, youth perceived to need counseling (0.40, 95% CI = 0.34, 0.45), with higher CIS scores (0.04, 95% CI = 0.01, 0.06), and worse mental health status (0.1, 95% CI = 0.07, 0.13) had increased probability of treatment episodes. Living with a single parent (0.07, 95% CI = 0.00, 0.14) compared to married parents, also increased the probability of initiating treatment.
Table 4.
Predictors of Initiating Episode of Care and Initiating Episode With Specialist.
| Initiate episode | Initiate with specialist | |||
|---|---|---|---|---|
| Predictor variables | Coefficient | 95% CI | Coefficient | 95% CI |
| Female | −0.06* | (−0.11, −0.01) | 0.12* | (0.02, 0.22) |
| Age 5–12 | 0.02 | (−0.02, 0.07) | 0.03 | (−0.08, 0.14) |
| Race/ethnicity | ||||
| Black | −0.12* | (−0.19, −0.05) | 0.08 | (−0.04, 0.21) |
| Hispanic | −0.07* | (−0.14, −0.01) | 0.01 | (−0.14, 0.16) |
| Other race | −0.05 | (−0.16, 0.05) | 0.01 | (−0.22, 0.25) |
| Insurance coverage | ||||
| Any managed care | 0.00 | (−0.05, 0.06) | 0.00 | (−0.11, 0.12) |
| Public insurance | 0.00 | (−0.07, 0.08) | −0.01 | (−0.16, 0.15) |
| Uninsured | −0.16* | (−0.26, −0.05) | −0.12 | (−0.43, 0.19) |
| Income as % of federal poverty line (FPL) | ||||
| <125% FPL | −0.12* | (−0.19, −0.04) | 0.04 | (−0.14, 0.23) |
| 125–200% FPL | −0.05 | (−0.17, 0.08) | −0.05 | (−0.22, 0.12) |
| 201–300% FPL | −0.09* | (−0.15, −0.02) | −0.05 | (−0.20, 0.11) |
| >400% FPL | 0.01 | (−0.07, 0.08) | 0.06 | (−0.11, 0.23) |
| Mental health | ||||
| CIS score | 0.04* | (0.01, 0.06) | 0.03 | (−0.02, 0.09) |
| Youth needs counseling | 0.40*** | (0.34, 0.45) | 0.11 | (0.00, 0.21) |
| Mental health status | 0.10*** | (0.07, 0.13) | 0.02 | (−0.04, 0.09) |
| Physical health | ||||
| Asthma | 0.05 | (−0.04, 0.13) | −0.02 | (−0.14, 0.10) |
| Physical health status | −0.06*** | (−0.10, −0.03) | −0.03 | (−0.09, 0.03) |
| “Child is less healthy” | −0.02 | (−0.09, 0.05) | −0.04 | (−0.17, 0.09) |
| Activity limitation | 0.08 | (−0.08, 0.25) | −0.24* | (−0.47, −0.02) |
| Parental characteristics | ||||
| Divorced parent | 0.06 | (−0.01, 0.12) | 0.01 | (−0.11, 0.13) |
| Single parent | 0.07* | (0.00, 0.14) | 0.01 | (−0.16, 0.17) |
| Parent mental health | 0.00 | (−0.03, 0.03) | 0.03 | (−0.03, 0.08) |
| Region | ||||
| South | 0.07 | (−0.01, 0.15) | −0.07 | (−0.22, 0.08) |
| West | −0.01 | (−0.09, 0.08) | 0.05 | (−0.14, 0.25) |
| Midwest | 0.04 | (−0.04, 0.12) | −0.04 | (−0.20, 0.13) |
| Panel | 0.00 | (−0.01, 0.02) | 0.00 | (−0.04, 0.03) |
| Intercept | 0.16 | (−0.03, 0.36) | 0.41 | (−0.04, 0.85) |
Note. CI = confidence interval; CIS = Columbia Impairment Scale. Model for initiating care include all samples without episodes at baseline, models for initiation of specialist care only include sample with treatment episodes. Reference categories: Age is 13–17 years old; race/ethnicity is White; income is 301% to 400% FPL; Parental marital status is married; region is Northeast. Child and parental mental health status, CIS score, and child physical health status have been mean-standardized.
p < .05.
p < .001.
p < .0001.
Females had increased probability of initiating with a specialist (0.12, 95% CI = 0.02, 0.22), while having an activity limitation decreased the probability (−0.24, 95% CI = −0.47, −0.02).
Treatment Duration and Quality
Table 5 illustrates that among younger youth with care, 33.3% received minimally adequate care (95% CI = 28.1%, 38.6%). Minimally adequate care was defined as having either four or more visits with medication therapy or eight or more visits without medication. Almost half of all younger youth with medication-based episodes did not have more than two visits, and half of those without medication did not have more than five visits. Overall among those younger youth with episodes, only 60.9% (95% CI = 54.0%, 67.9%) had more than one visit.
Table 5.
Characteristics of Episodes: Average Length and Percentage That Are Minimally Adequate.
| Age 5–12 | Age 13–17 | |||
|---|---|---|---|---|
| Estimate | 95% CI | Estimate | 95% CI | |
| Minimally adequate overall (%) | 33.3% | (28.1%, 38.6%) | 32.3% | (25.7%, 38.9%) |
| Types of episodes not meeting minimal adequacy | ||||
| Medication episodes with 0–1 visits (%) | 47.6% | (41.2%, 54.0%) | 52.3% | (45.5%, 59.2%) |
| Medication episodes with 2–3 visits (%) | 16.8% | (10.7%, 22.9%) | 16.3% | (10.4%, 22.1%) |
| Nonmedication episodes with 1–4 visits (%) | 50.9% | (39.2%, 62.8%) | 46.5% | (36.8%, 56.2%) |
| Nonmedication episodes with 5–7 visits (%) | 16.5% | (6.1%, 26.9%) | 10.3% | (4.9%, 14.6%) |
| >1 visit (%) | 60.9% | (54.0%, 67.9%) | 60.0% | (50.1%, 69.9%) |
| Number of visits (mean) | 7.27 | (5.67, 8.88) | 8.20 | (6.19, 10.22) |
| Number of days (mean) | 160.36 | (131.41, 189.32) | 176.59 | (144.02, 209.16) |
Note. CI = confidence interval. An episode of care was defined as mental health treatment preceded by at least 12 weeks without treatment. Estimates are survey-weighted.
The mean number of visits per episode was 7.27 (95% CI = 5.67, 8.88), and the mean number of days was 160.36 (95% CI = 131.41, 189.32). Patterns in terms of minimal adequacy and episode length were similar for older youth.
In regression analysis (Table 6), higher CIS scores (0.06, 95% CI = 0.01, 0.11) and needing counseling (0.11, 95% CI = 0.02, 0.20) increased the probability of receiving minimally adequate care, while residence in the South decreased the probability (−0.16, 95% CI = −0.27, −0.04). Higher CIS score also increased the probability of having more than one visit (0.06, 95% CI = 0.00, 0.12), while being “other” race decreased the probability (−0.24, 95% CI = −0.45, −0.04). Residence in the South, compared to the Northeast, significantly decreased the number of visits (−4.5 visits, 95% CI = −8.69, −0.30). Hispanic youth had significantly shorter episodes (−50.7 days, 95% CI = −91.36, −9.94), as did residence in the South (−48.0 days, 95% CI = −93.18, −2.78). Youth needing counseling had significantly longer episodes (47.8 days, 95% CI = 14.04, 81.56).
Table 6.
Predictors of Episode Quality and Duration.
| Minimally adequate | More than 1 visit | Total number of visits | Length of episode (days) | |||||
|---|---|---|---|---|---|---|---|---|
| Predictor variables | Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI |
| Female | 0.05 | (−0.04, 0.14) | 0.04 | (−0.09, 0.17) | 2.26 | (−1.38, 5.89) | −5.38 | (−38.39, 27.63) |
| Age 5–12 | −0.01 | (−0.10, 0.08) | −0.03 | (−0.14, 0.08) | −1.00 | (−4.46, 2.40) | −18.10 | (−50.22, 14.12) |
| Race/ethnicity | ||||||||
| Black | −0.03 | (−0.16, 0.09) | −0.06 | (−0.22, 0.11) | −0.10 | (−4.31, 4.13) | −40.8 | (−82.73, 1.09) |
| Hispanic | −0.09 | (−0.22, 0.03) | −0.10 | (−0.26, 0.05) | −1.70 | (−6.73, 3.32) | −50.70* | (−91.36, −9.94) |
| Other race | −0.13 | (−0.29, 0.02) | −0.24* | (−0.45, −0.04) | −2.10 | (−10.60, 6.32) | −56.20 | (−114.25, 1.90) |
| Insurance coverage | ||||||||
| Any managed care | −0.02 | (−0.12, 0.07) | 0.00 | (−0.11, 0.11) | −2.30 | (−5.41, 0.76) | 4.92 | (−30.65, 40.48) |
| Public insurance | 0.03 | (−0.10, 0.15) | −0.02 | (−0.2, 0.15) | −1.10 | (−6.10, 3.88) | 28.89 | (−12.09, 69.88) |
| Uninsured | −0.13 | (−0.33, 0.06) | −0.21 | (−0.62, 0.19) | −3.60 | (−12.84, 5.63) | −22.80 | (−89.97, 44.42) |
| Income as % of federal poverty line (FPL) | ||||||||
| <125% FPL | 0.04 | (−0.14, 0.23) | 0.00 | (−0.21, 0.22) | 2.64 | (−4.09, 9.36) | −12.80 | (−61.93, 36.38) |
| 125–200% FPL | 0.07 | (−0.11, 0.25) | 0.08 | (−0.16, 0.33) | 5.57 | (−1.17, 12.3) | 2.44 | (−61.43, 56.56) |
| 201–300% FPL | 0.04 | (−0.09, 0.17) | −0.01 | (−0.19, 0.17) | 1.45 | (−3.76, 6.65) | 2.09 | (−40.96, 45.14) |
| >400% FPL | 0.07 | (−0.07, 0.21) | 0.04 | (−0.12, 0.21) | 2.20 | (−3.53, 7.92) | 5.60 | (−41.40, 52.59) |
| Mental health | ||||||||
| CIS score | 0.06* | (0.01, 0.11) | 0.06* | (0.00, 0.12) | 1.25 | (−0.23, 2.73) | 16.55 | (1.41, 31.69) |
| Youth needs counseling | 0.11* | (0.02, 0.20) | 0.07 | (−0.08, 0.22) | 1.23 | (−3.00, 5.46) | 47.80* | (14.04, 81.56) |
| Mental health status | 0.00 | (−0.05, 0.05) | −0.01 | (−0.08, 0.06) | −1.10 | (−2.74, 0.63) | −4.070 | (−21.71, 13.57) |
| Physical health | ||||||||
| Asthma | 0.02 | (−0.09, 0.14) | 0.00 | (−0.17, 0.18) | 0.04 | (−4.86, 4.94) | 2.43 | (−50.51, 55.38) |
| Physical health status | −0.02 | (−0.07, 0.04) | 0.00 | (−0.08, 0.07) | −0.20 | (−2.08, 1.70) | −0.12 | (−18.60, 18.36) |
| “Child is less healthy” | −0.03 | (−0.16, 0.09) | −0.02 | (−0.18, 0.13) | 2.85 | (−5.69, 11.39) | 15.30 | (−31.87, 62.47) |
| Activity limitation | −0.11 | (−0.29, 0.07) | −0.23 | (−0.52, 0.06) | 0.00 | (−7.81, 7.80) | −7.25 | (−59.95, 45.44) |
| Parental characteristics | ||||||||
| Divorced parent | 0.01 | (−0.09, 0.11) | 0.02 | (−0.11, 0.15) | 0.09 | (−3.73, 3.90) | −13.40 | (−45.95, 19.25) |
| Single parent | 0.02 | (−0.12, 0.15) | −0.03 | (−0.21, 0.16) | −1.00 | (−5.36, 3.38) | −18.90 | (−65.07, 27.36) |
| Parent mental health | 0.00 | (−0.05, 0.05) | −0.01 | (−0.06, 0.05) | −0.20 | (−1.65, 1.33) | −11.00 | (−27.68, 5.73) |
| Region | ||||||||
| South | −0.16* | (−0.27, −0.04) | −0.06 | (−0.21, 0.10) | −4.50* | (−8.69, −0.30) | −48.00* | (−93.18, −2.78) |
| West | 0.04 | (−0.14, 0.22) | 0.10 | (−0.08, 0.29) | 1.11 | (−7.87, 10.09) | −4.15 | (−59.07, 50.76) |
| Midwest | −0.07 | (−0.19, 0.06) | 0.03 | (−0.14, 0.20) | −3.00 | (−7.4, 1.47) | −21.4 | (−74.99, 32.16) |
| Panel | 0.02 | (−0.01, 0.05) | 0.00 | (−0.04, 0.04) | −0.30 | (−1.25, 0.70) | 1.93 | (−7.32, 11.19) |
| Intercept | 0.11 | (−0.27, 0.50) | 0.71* | (0.25, 1.17) | 12.7 | (−2.61, 28.02) | 151.8* | (29.48, 274.16) |
Note. Cl = confidence interval; CIS = Columbia Impairment Scale. Models include all samples with treatment episodes. Reference categories: age is 13 to 17 years old; race/ethnicity is White; income is 301% to 400% FPL; Parental marital status is married; region is Northeast. Child and parental mental health status, CIS score, and child physical health status have been mean-standardized.
p < .05.
p < .001
p < .0001.
Discussion
Using an episodes of care methodology, our study finds that most youth with possible mental health problems do not initiate any mental health treatment over a 2-year period and that continuity of care is very low on average among those initiating care. Our findings update prior literature on access and provide new information about care patterns once contact is made with the service system.
Our study confirms predictors of initiation identified in other population samples. For example, our study confirms that poverty and lack of health insurance were associated with lower probability of initiating care, likely reflecting complex barriers to care including costs for treatment, transportation difficulties, and financial burden (Bringewatt & Gershoff, 2010). Other studies also find that females are significantly less likely to initiate care (Merikangas et al., 2010). Females may have more internalizing disorders, which may be detected less readily by clinicians (Wren, Scholle, Heo, & Comer, 2003). Black and Hispanic youth were also less likely to initiate care. Some prior studies have identified lower use among this population (Cook et al., 2013), while others have found no differences (Merikangas et al., 2010). These differences persisted after adjusting for socioeconomic factors, possibly reflecting cultural preferences and norms regarding how to cope with mental health difficulties (Yeh, McCabe, Hough, Dupuis, & Hazen, 2003).
Our study is one of the first to quantify problems with continuity and adequacy of care for children. Early mental health treatment termination was also found in a prior analysis of a database of privately insured youth (Harpaz-Rotem, Leslie, & Rosenheck, 2004) and among a community-based sample of Haitian American, African American, and non-Hispanic White youth (Carson et al., 2011). Potential mechanisms identified by prior literature include family preferences (e.g., reluctance to use medications; Berger-Jenkins, McKay, Newcorn, Bannon, & Laraque, 2012), patient–provider interactions (particularly for minority families; Coker, Rodriguez, & Flores, 2010), language barriers (Aratani & Cooper, 2012), or health system–level variables (e.g., poor coordination of care). Youth residing in the South had a lower probability of receiving minimally adequate care. There are fewer pediatric mental health providers in the South, a potential barrier to receiving ongoing office-based visits (Stevens, Harman, & Kelleher, 2004). Minority and uninsured youth were substantially less likely to receive adequate care and also to have shorter episodes of care, but differences were not statistically significant. Future work, with larger sample sizes, should consider these differences in access to adequate care.
Although our study has notable strengths, including the use of detailed, nationally representative treatment data over a 2-year period, there are several limitations. First, our small sample of episodes limited statistical power to detect some clinically significant predictors of treatment continuity and adequate care. Second, we could not follow longer-term treatment beyond the 2-year observation period in the MEPS. Approximately half of the treatment episodes in the data were either left-censored, right-censored, or both. We accounted for this censoring process in statistical analysis using censored normal regression, but this model may not adequately fit the distribution of visits and measures of treatment duration that are highly skewed. We reclassified these outcomes in binary categories (e.g., less than 5 visits, less than 15 visits) and examined logistic regression models for those data that were not censored (i.e., fully observed) and found that the general pattern of results was similar. We also reestimated our linear probability models with logistic regression models, focusing only on the sample with fully observed data, and obtained qualitatively similar results. Third, our measure of minimally adequate care provides only one benchmark of treatment quality. We could not assess clinical competence of providers, comprehensiveness of care provided, or appropriateness of different medication therapies.
Finally, our sample inclusion criteria rely on parental reports of child symptoms and needs, which may not accurately define the subgroup of youth requiring treatment. For example, we included youth perceived by their parents to have fair or poor mental health status. Although a single-item global measure of mental health status predicts future functional status in older adults (Lee, 2000), its reliability and validity is unknown for parental reports of children. We also included youth who met the “needed counseling” criterion, which may be more sensitive to current service use than to actual mental health impairment. In sensitivity analysis, we reestimated our regression models using only the sample with high CIS scores and obtained very similar results, however (available from authors on request).
Conclusion
Efforts to strengthen mental health treatment and improve care for vulnerable youth should be broadly focused, emphasizing not only recognition and access but also continuity of care. Several promising initiatives could accelerate this process. National efforts to reduce stigma could improve awareness of mental health problems in youth, where there remain important gaps in knowledge among the general public. For example, many adults do not recognize that depression and attention-deficit/hyperactivity disorder in youth can be serious problems requiring treatment (Pescosolido, Jensen, Martin, Olafsdottir, & Fettes, 2008). In terms of improving access, the Affordable Care Act will expand coverage to currently uninsured (or underinsured) youth through the new health insurance exchanges. The Paul Wellstone Domenici Mental Health Parity Act, passed in 2008, is a national mental health parity law that applies to many private insurance plans. Final rules setting forth the requirements for insurers under the parity law were finalized in November 2013 (U.S. Department of Health and Human Services, 2013). This law could increase access to services for families, although the effect of parity provisions is still uncertain, and prior experience has been mixed (Barry & Busch, 2008). Within health insurance programs, efforts to monitor services and design payment models that reimburse for integrated care could also improve outcomes. The Children’s Health Insurance Program Reauthorization Act introduced new quality measures, which align with the measure of minimally adequate care that we considered (Dougherty et al., 2011). Monitoring the provision of such care in private and public insurance plans, and designing incentives to increase minimally adequate care, could be important steps toward improving treatment for youth with mental health difficulties.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Drs. Cook and Carson were supported by the United States National Institutes of Health NIMH Grant R01 MH091042. Dr. Saloner received financial support from the Robert Wood Johnson Foundation Health and Society Scholars Program.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Agency for Healthcare Research and Quality. (2008). Design, methods, and field results of the Medical Expenditure Panel Survey Medical Provider Component (MEPS MPC)—2006 calendar year data. Rockville, MD: Author. [Google Scholar]
- Aratani Y, & Cooper JL (2012). Racial and ethnic disparities in the continuation of community-based children’s mental health services. Journal of Behavioral Health Services & Research, 39, 116–129. [DOI] [PubMed] [Google Scholar]
- Barry CL, & Busch SH (2008). Caring for children with mental disorders: Do state parity laws increase access to treatment? Journal of Mental Health Policy and Economics, 11(2), 57–66. [PubMed] [Google Scholar]
- Begley S (2012, December 29). U.S. mentally ill and their families face barriers to care. Reuters. Retrieved from http://www.reuters.com/article/2012/12/29/us-usa-shooting-men-talyill-idUSBRE8BS07020121229 [Google Scholar]
- Berger-Jenkins E, McKay M, Newcorn J, Bannon W, & Laraque D (2012). Parent medication concerns predict underutilization of mental health services for minority children with ADHD. Clinical Pediatrics, 51, 65–76. [DOI] [PubMed] [Google Scholar]
- Bird HR, Andrews H, Schwab-Stone M, Goodman S, Dulcan M, Richters J, … Gould MS (1996). Global measures of impairment for epidemiologic and clinical use with children and adolescents. International Journal of Methods in Psychiatric Research, 6, 295–307. [Google Scholar]
- Bringewatt EH, & Gershoff ET (2010). Falling through the cracks: Gaps and barriers in the mental health system for America’s disadvantaged children. Children and Youth Services Review, 32, 1291–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson NJ, Stewart M, Lin JY, & Alegria M (2011). Use and quality of mental health services for Haitian youth. Ethnicity & Health, 16, 567–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Medicaid and CHIP Services. (2012). Initial core set of children’s health care quality measures: Technical specifications and resource manual for federal fiscal year 2012 reporting. Woodlawn, MD: Centers for Medicare & Medicaid Services. [Google Scholar]
- Christakis D, & Lozano P (2003). Continuity of care is associated with early and consistent treatment of attention-deficit/hyperactivity disorder during a single school year. Journal of Science Communication, 10, 372–375. [Google Scholar]
- Coker TR, Rodriguez MA, & Flores G (2010). Family-centered care for US children with special health care needs: Who gets it and why? Pediatrics, 125, 1159–1167. [DOI] [PubMed] [Google Scholar]
- Cook BL, Barry CL, & Busch SH (2013). Racial/ethnic disparity trends in children’s mental health care access and expenditures from 2002 to 2007. Health Services Research, 48, 129–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Copeland W, Cowell A, & Keeler G (2007). Service costs of caring for adolescents with mental illness in a rural community, 1993–2000. American Journal of Psychiatry, 164, 36–42. [DOI] [PubMed] [Google Scholar]
- Cunningham PJ, & Freiman MP (1996). Determinants of ambulatory mental health services use for school-age children and adolescents. Health Services Research, 31, 409–427. [PMC free article] [PubMed] [Google Scholar]
- Dougherty D, Schiff J, & Mangione-Smith R (2011). The Children’s Health Insurance Program Reauthorization Act quality measures initiatives: Moving forward to improve measurement, care, and child and adolescent outcomes. Academic Pediatrics, 11(3 Suppl.), S1–S10. [DOI] [PubMed] [Google Scholar]
- Ezzati-Rice TM, Rohde F, & Greenblatt J (2008). Sample design of the Medical Expenditure Panel Survey Household Component, 1998–2007 (Methodology Report No. 22). Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. [Google Scholar]
- Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, & Landsverk JA (2005). Racial and ethnic differences in utilization of mental health services among high-risk youths. American Journal of Psychiatry, 162, 1336–1343. [DOI] [PubMed] [Google Scholar]
- Halfon N, Houtrow A, Larson K, & Newacheck PW (2012). The changing landscape of disability in childhood. Future of Children, 22(1), 13–42. [DOI] [PubMed] [Google Scholar]
- Harman JS, Edlund MJ, & Fortney JC (2004). Disparities in the adequacy of depression treatment in the United States. Psychiatric Services, 55, 1379–1385. [DOI] [PubMed] [Google Scholar]
- Harpaz-Rotem I, Leslie D, & Rosenheck RA (2004). Treatment retention among children entering a new episode of mental health care. Psychiatric Services, 55, 1022–1028. [DOI] [PubMed] [Google Scholar]
- Hornbrook MC, Hurtado AV, & Johnson RE (1985). Health care episodes: Definition, measurement and use. Medical Care Research and Review, 42, 163–218. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Goldman E, Offord D, Costello EJ, Friedman R, Huff B, … Roberts R (2011). Overlooked and underserved: “Action signs” for identifying children with unmet mental health needs. Pediatrics, 128, 970–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kataoka SH, Zhang L, & Wells KB (2002). Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry, 159, 1548–1555. [DOI] [PubMed] [Google Scholar]
- Katon WJ, Richardson L, Russo J, Lozano P, & McCauley E (2006). Quality of mental health care for youth with asthma and comorbid anxiety and depression. Medical Care, 44, 1064–1072. [DOI] [PubMed] [Google Scholar]
- Keeler EB, Manning WG, & Wells KB (1988). The demand for episodes of mental health services. Journal of Health Economics, 7, 369–392. [DOI] [PubMed] [Google Scholar]
- Lee Y (2000). The predictive value of self assessed general, physical, and mental health on functional decline and mortality in older adults. Journal of Epidemiology and Community Health, 54, 123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machlin S, Cohen J, Elixhauser A, Beauregard K, & Steiner C (2009). Sensitivity of household reported medical conditions in the medical expenditure panel survey. Medical Care, 47, 618–625. [DOI] [PubMed] [Google Scholar]
- McQuaid EL, Kopel SJ, & Nassau JH (2001). Behavioral adjustment in children with asthma: A meta-analysis. Journal of Developmental and Behavioral Pediatrics, 22, 430–439. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Brody D, Fisher PW, Bourdon K, & Koretz DS (2010). Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics, 125, 75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swendsen J, Avenevoli S, Case B, … Olfson M (2011). Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 50(1), 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Multum. (n.d.). Multum classification system. Retrieved from http://www.multum.com/Lexicon.html
- Office of Management and Budget. (2014). The president’s budget for fiscal year 2014. Retrieved from http://www.whitehouse.gov/omb/budget
- Olfson M, Gameroff MJ, Marcus SC, & Waslick BD (2003). Outpatient treatment of child and adolescent depression in the United States. Archives of General Psychiatry, 60, 1236–1242. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, Druss B, Alan Pincus H, & Weissman MM (2003). Parental depression, child mental health problems, and health care utilization. Medical Care, 41, 716–721. [DOI] [PubMed] [Google Scholar]
- Perou R, Bitsko R, Blumberg S, Pastor P, Ghandour R, Gfroerer J, … Crosby A (2013). Mental health surveillance among children—United States, 2005–2011. Atlanta, GA: Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- Pescosolido B, Jensen PS, Martin JK, Olafsdottir S, & Fettes D (2008). Public knowledge and assessment of child mental health problems: Findings from the national stigma study-children. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 339–349. [DOI] [PubMed] [Google Scholar]
- Peters JW (2013, April 12). In gun debate, no rift on better care for mentally ill. The New York Times. Retrieved from http://www.nytimes.com/2013/04/13/us/politics/senators-make-bipartisan-push-for-mental-health-care.html?_r=0 [Google Scholar]
- Rubin DB (1998). Multiple imputation for nonresponse in surveys. New York, NY: John Wiley. [Google Scholar]
- Schnedler W (2005). Likelihood estimation for censored random vectors. Econometric Reviews, 24, 195–217. [Google Scholar]
- Selden TM (2009). The within-year concentration of medical care: Implications for family out-of-pocket expenditure burdens. Health Services Research, 44, 1029–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129, e232–e246. [DOI] [PubMed] [Google Scholar]
- Smith JP, & Smith GC (2010). Long-term economic costs of psychological problems during childhood. Social Science & Medicine, 71, 110–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein BD, Sorbero MJ, Dalton E, Ayers AM, Farmer C, Kogan JN, & Goswami U (2013). Predictors of adequate depression treatment among Medicaid-enrolled youth. Social Psychiatry and Psychiatric Epidemiology, 48, 757–765. [DOI] [PubMed] [Google Scholar]
- Stevens J, Harman JS, & Kelleher KJ (2004). Ethnic and regional differences in primary care visits for attention-deficit hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics, 25, 318–325. [DOI] [PubMed] [Google Scholar]
- Stevens J, Harman JS, & Kelleher KJ (2005). Race/ethnicity and insurance status as factors associated with ADHD treatment patterns. Journal of Child and Adolescent Psychopharmacology, 15(1), 88–96. [DOI] [PubMed] [Google Scholar]
- Tansella M, Micciolo R, Biggeri A, Bisoffi G, & Balestrieri M (1995). Episodes of care for first-ever psychiatric patients. A long-term case-register evaluation in a mainly urban area. British Journal of Psychiatry, 167, 220–227. [DOI] [PubMed] [Google Scholar]
- Teh CF, Sorbero MJ, Mihalyo MJ, Kogan JN, Schuster J, Reynolds CF III, & Stein BD (2010). Predictors of adequate depression treatment among Medicaid-enrolled adults. Health Services Research, 45, 302–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2013). Final rules under the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (Rule No. 2013–27086). Washington, DC: U.S. Department of Health and Human Services. [Google Scholar]
- Wren FJ, Scholle SH, Heo J, & Comer DM (2003). Pediatric mood and anxiety syndromes in primary care: Who gets identified? International Journal of Psychiatry in Medicine, 33(1), 1–16. [DOI] [PubMed] [Google Scholar]
- Yeh M, McCabe K, Hough RL, Dupuis D, & Hazen A (2003). Racial/ethnic differences in parental endorsement of barriers to mental health services for youth. Mental Health Services Research, 5(2), 65–77. [DOI] [PubMed] [Google Scholar]
- Zima BT, Bussing R, Tang L, Zhang L, Ettner S, Belin TR, & Wells KB (2010). Quality of care for childhood attention-deficit/hyperactivity disorder in a managed care Medicaid program. Journal of the American Academy of Child and Adolescent Psychiatry, 49, 1225–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zima BT, Murphy JM, Scholle SH, Hoagwood KE, Sachdeva RC, Mangione-Smith R, … Jellinek M (2013). National quality measures for child mental health care: Background, progress, and next steps. Pediatrics, 131(Suppl.), S38–S49. [DOI] [PMC free article] [PubMed] [Google Scholar]


