Abstract
Context:
Rural residents can be exposed to high levels of agricultural machinery noise and are at risk of hearing loss.
Aims:
This study aimed to determine audiology service use and rates of hearing loss in a regional area of Australia, using both self-report and audiology testing.
Setting and Design:
A survey of randomly selected households was undertaken and 6432 participants were interviewed face to face about their health, hearing, and use of audiology services. A total of 1454 participants were randomly selected to undertake standard audiology testing.
Material and Methods:
Material Hearing was evaluated using conventional audiometry.
Statistical Analysis Used:
Independent t-tests, Chi-squared tests, and logistic regression were used to examine the association amongbetween hearing loss, use of audiology services, and demographic factors.
Results:
Hearing issues were present in 12.5% of the survey participants. The rate of hearing loss increased significantly with age. Males were significantly more likely to have hearing loss than females (9.5% vs. 5.2%, pP << 0.01). The majority of people who reported accessing audiology services in the past 12 months were satisfied with the care they received (85.2%), and experienced short waiting times for these services (68.2% waited ≤≤ 7 days).
Conclusions:
Males had higher rates of hearing issues than females in this rural area. Audiology services in the region were accessible within short waiting times, and clients were satisfied with the service.
Keywords: (3–6): hAudiology, Australia, hearing loss, regional, ruralHearing loss, audiology, rural, regional, Australia
Key messages
Rates of hearing loss in this large, randomly selected, rural population were significantly higher in males than females after controlling for important risk factors.
There was good agreement between self-reported hearing issues and hearing loss detected by audiological testing.
Audiology services were accessible within short waiting times and patients were highly satisfied with the service.
INTRODUCTION
Hearing loss is an important issue in Australia and is estimated to affect 12% of all Australian adults.[1] Hearing loss can lead to reduced quality of life, difficulty communicating, and social isolation.[2] Hearing loss commonly occurs with a range of other comorbid chronic health conditions.[3]
The issue of hearing loss is particularly important in regional, rural, and remote Australia, where there are increased risks from exposure to farm machinery and firearm use.[4] The issue is further compounded by patchy access to audiology services and specialists.[1]
Adult hearing screening has not been systematically implemented across Australia, and for this reason, epidemiological studies are important in understanding the issue.[5] Previous epidemiological studies of hearing loss using audiological testing in Australia have typically focused on older populations and have found high prevalence of hearing loss (Blue Mountains study, population aged 55–99 years, prevalence of hearing loss of 56%,[6] the Busselton study of baby boomers, age range 45–65 years, prevalence of hearing loss of approximately 27%,[7] and the DYNOTPA study, age range 50–103 years, prevalence hearing loss of 51%).[8] The South Australian Hearing study[9] included participants as young as 15 years of age and found that the prevalence of any level of hearing impairment was 22%.
This study aimed to determine population-based rates of hearing loss using self-report and audiometry in the Goulburn Valley region of Victoria, Australia, an area with substantial agricultural and food processing industries. This study also examined patterns of audiology service use in the region.
SUBJECTS AND METHODS
Household survey component
The Crossroads Household survey was a cross-sectional study undertaken in the Goulburn Valley region of Victoria between September 2000 and March 2003. This region encompasses the regional center of Shepparton-Mooroopna (population 35,828) and six “shire capitals” ranging in population size from 2094 to 10,955 at the time of the study, as previously described.[10] The survey focused on access to health care and experience of a range of health conditions, including hearing loss. General demographic questions were included (including age, gender, occupation, income, education, health insurance, English language). Residential address lists from local government offices were used to generate a list of randomly selected households. A stratified random sampling approach was used to yield half of the households in the regional center and 1/12 of the households in the six “shire capitals.” Surveys were completed face to face wherever possible, though participants occasionally self-completed the survey if they preferred.
Participants were asked if they had ever suffered from, or were currently treated for hearing loss, and were asked to specify the nature of their hearing loss. Comprehensive coding was undertaken to identify the most common hearing issues reported by a minimum of five female or five male participants in response to an open question. When a participant reported more than one issue, each issue was recorded separately. Participants were asked if they had accessed an audiologist or audiometrist in the past 12 months, how often they had done so, waiting time, location of the service and were asked to rate their satisfaction with the service. This contributed to the wider aims of the study to assess access to a range of health services.
Clinic component
A random sample of the participants from the survey component of the study aged 25 years or older and who had resided in the region for at least 6 months were invited to attend a “clinic.” A range of measurements were taken and a variety of tests were performed, including standard air conduction audiometric testing. Pure tone audiometry (PTA) was conducted using standard ME70 earphones (GN Otometrics, Schaumburg, Illinois, USA) and aBeltone308 audiometer (Beltone Electronics, Chicago, Illinois, USA), which were calibrated as per manufacturer’s guidelines. Audiometric thresholds for air conduction were established for threshold frequencies of 1000, 2000, and 4000 Hz at hearing levels of 25 and 40 dB. Normal hearing was defined by PTA 1 to 4 kHz at <25 dB, mild hearing loss: PTA 1 to 4 kHz at >25 dB, <40 dB and moderate-to-severe hearing loss: PTA 1 to 4 kHz at >40 dB. Hearing loss in the right, left, and the “better ear” were determined.
Participants were also asked a series of questions about their hearing (“Would you say you have any difficulty hearing?,” “Have you ever been told by a doctor that you have a hearing problem?,” “Have you ever had surgery or any other procedure on your ears?,” “Do you get tinnitus or ringing in your ears?,” and “Have you ever needed a hearing aid?”).
Statistical analysis
Data were imported into SPSS, version 22 (SPSS Inc., Chicago, Illinois, USA). Continuous data are summarized as mean and standard deviation, and categorical data as frequencies and percentages. Independent groups were compared using Student’s t-test. Dichotomous variables were compared using Chi-squared test. Z-test for proportions was used to compare percentages between two groups. Logistic regression was used to examine the association between gender and a range of hearing issues, controlling for age, smoking status, education, and income. Results are reported as unadjusted and adjusted odds ratios (ORs) with 95% confidence intervals (CIs).
The study was approved by the Goulburn Valley Ethics Committee, and signed consent was obtained from each participant.
RESULTS
Participation rates
The response rate for the survey component of this study was 70.3%. The participation rate for the clinic component of this study was 61.3%. The stratification resulted in the regional center yielding 50.2% of the responses for the survey component and 47.9% for the clinic component of the study, with the remainder from the “shire capitals.” Tables 1 and 2 show the characteristics of the participants from the household survey and clinic, respectively.
Table 1.
Demographic characteristics of the survey participants and self-reported nature of hearing loss
| Males | Females | P | |
|---|---|---|---|
| N | 2806 (43.6%) | 3626 (56.4%) | |
| Age (mean ± standard deviation) | 45.6 ± 17.2 | 44.9 ± 17.3 | 0.11 |
| English speaking % | 95.0 | 97.3 | 0.64 |
| Private health insurance % | 45.0 | 42.9 | 0.24 |
| Farmers, n (%) | 111 (4.0%) | 54 (1.5%) | <0.001 |
| Nature of hearing loss | |||
| Partial hearing loss, n (%) | 154 (5.5) | 116 (3.2) | 0.008 |
| Wears/has worn hearing aids, n (%) | 71 (2.5) | 47 (1.3) | 0.001 |
| Industrial hearing loss, n (%) | 88 (3.1) | 16 (0.4) | <0.001 |
| Hearing loss (undefined), n (%) | 43 (1.5) | 29 (0.8) | 0.018 |
| Advanced age, n (%) | 25 (0.9) | 33 (0.9) | 0.882 |
| Infection/damage to ear drum, n (%) | 10 (0.4) | 25 (0.7) | 0.182 |
| Tinnitus, n (%) | 20 (0.7) | 14 (0.4) | 0.186 |
| Nerve damage, n (%) | 5 (0.2) | 10 (0.3) | 0.001 |
Table 2.
Demographic characteristics of the “clinic” participants
| Males | Females | P | |
|---|---|---|---|
| N | 635 (43.7%) | 819 (56.3%) | |
| Age (mean ± standard deviation) | 53.7 ± 15.7 | 52.3 ± 15.6 | 0.501 |
| English speaking % | 97.9 | 98.5 | 0.524 |
| Private health insurance % | 50.4 | 46.9 | 0.101 |
| Farmers % | 9.0 | 3.1 | <0.001 |
| Hearing in better ear % | |||
| Normal hearing | 90.5 | 94.9 | 0.008 |
| Mild hearing loss | 8.3 | 4.4 | |
| Moderate–severe hearing loss | 1.2 | 0.8 | |
| Hearing in left ear % | |||
| Normal hearing | 82.4 | 90.3 | <0.001 |
| Mild hearing loss | 13.3 | 7.2 | |
| Moderate–severe hearing loss | 4.3 | 2.6 | |
| Hearing in right ear % | |||
| Normal hearing | 86.8 | 91.7 | 0.013 |
| Mild hearing loss | 9.9 | 7.1 | |
| Moderate–severe hearing loss | 3.3 | 4.3 | |
Hearing difficulties
Past or present hearing loss or issues were present in 801 (12.5%) of the participants of the household survey [Table 1]. Males were significantly more likely to report hearing loss than females (P < 0.001) [Table 1].
Logistic regression was used to determine whether the higher prevalence of hearing issues reported by males remained after controlling for age, income, education, location of residence, and smoking status. This analysis showed that even after controlling for the strongly influential variable of age, the predominance of hearing issues in males remained, as shown in Table 3.
Table 3.
Gender differences in a range of hearing issues (clinic participants)
| Ratemales (%) | Rate females (%) | Crude OR(95% CI) | # Adjusted OR (95% CI) | |
|---|---|---|---|---|
| Hearing difficulty | 43.95 | 35.22 | 1.49 (1.19–1.87)* | 1.48 (1.17–1.88)* |
| Doctor identified hearing problem | 20.86 | 10.33 | 2.51 (1.82–3.47)** | 2.56 (1.84–3.57)** |
| Tinnitus or ringing in ears | 35.52 | 29.86 | 1.31 (1.03–1.66)* | 1.34 (1.05–1.71)* |
| Surgery or procedure on ears | 11.84 | 7.64 | 1.66 (1.13–2.42)* | 1.59 (1.09–2.33)* |
| Hearing aid(s) | 9.97 | 4.78 | 2.43 (1.56–3.80)** | 2.44 (1.54–3.89)** |
# Adjusted OR: Location of residence (regional center or Shire Capital), smoking status, Income (≤$999 or ≥$1000 per week), education (≤secondary education, or postsecondary education), age (≤50 years of age or ≥51 years of age). * P < 0.05; ** P < 0.001.
Logistic regression also demonstrated that age was a strong predictor in each of the hearing issues, whereby people over the age of 50 were significantly more likely to have a hearing aid [OR 19.58 (95% CI 6.07–63.18)], have difficulty hearing [OR 2.19 (95% CI 1.69–2.82)], having had a doctor tell them they had a hearing problem [OR 3.16 (95% CI 2.11–4.73)], and have tinnitus [OR 1.35 (95% CI 1.04–1.76)]. Similarly, income was another strong predictor, whereby people earning less than $1000 per week were significantly more likely to have a hearing aid [OR 3.43 (95% CI 1.33–8.87)], have difficulty hearing [OR 1.39 (95% CI 1.03–1.88)], and having had a doctor tell them they had a hearing problem [OR 1.75 (95% CI 1.08–2.83)].
Table 4 shows the use, satisfaction with, and waiting time for audiology services. Audiology services were accessed predominantly within the region, with most respondents waiting 7 days or less for an appointment. The majority of respondents were satisfied or highly satisfied with the service they received. There were no significant differences in the use of audiology services between males and females, or between residents of the regional center compared with shire capitals.
Table 4.
Use of audiology services in the Goulburn Valley
| Cohort | |
|---|---|
| “Has accessed an audiologist/audiometrist in the past 12 months?,” n (%) | 239 (3.7) |
| “Frequency of visits to an audiologist/audiometrist in the past 12 months” (mean ± SD) | 1.53 ± 1.13 |
| Waited ≤7 days for an appointment, n (%) | 163 (68.2) |
| Satisfied/highly satisfied with the audiology service, n (%) | 201 (85.2) |
| Accessed audiology services in local area, n (%) | 214 (92.6) |
Note: No significant differences in use of audiology services were observed between males and females, or between residents of the regional center and Shire Capitals.
Audiology (left, right, and better ear)
Respondents who did not wear hearing aids undertook an audiology test (n = 1368). Normal hearing was more common in the right ear than the left ear, as shown in Table 2. Mild hearing loss and moderate-to-severe hearing loss were more common in the left ear (9.8% and 3.3%, respectively) than the right ear, as shown in Table 2. A total of 93% of respondents had normal hearing in their better ear, and 7% showed some degree of hearing loss. Males showed significantly higher rates of hearing loss than females (left, right, and better ear) and respondents aged ≥50 years showed higher rates than respondents aged less than 50 years (left, right, and better ear). Farmers showed a higher rate of hearing loss in their better ear (18.3%) than nonfarmers (6.2%) (P < 0.001). Male farmers and female farmers did not show significantly different rates of hearing loss (Chi-squared 2.549, df = 1, P = 0.11).
The percentage of participants demonstrating some degree of hearing loss (mild, moderate, severe) increased significantly with increasing age in both males and females (P < 0.001). There were no significant differences in rates of hearing loss between males and females at each age group (P = 0.152) [Figure 1].
Figure 1.
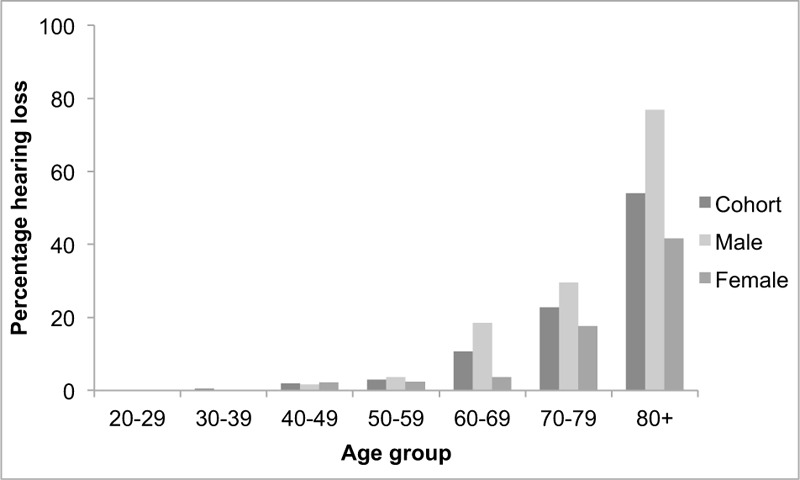
Hearing loss of males and females according to age group. Hearing loss increases with each increasing age group (P < 0.001 for cohort, males, and females)
The majority of respondents self-reported normal hearing which was verified on audiology testing, as shown in Table 5. Unrecognized hearing loss occurred in 4.1%. The Kappa score between audiometry and self-report showed that there was significant agreement (P < 0.001).
Table 5.
Comparison of self-reported hearing loss with hearing loss determined by audiology testing
| Hearing loss by audiology | |||
|---|---|---|---|
|
|
|||
| Hearing loss, n (%) | Normal hearing, n (%) | ||
| Self-reported hearing loss | Hearing loss, n (%) | 39 (2.9%) | 128 (9.5%) |
| Normal hearing, n (%) | 54 (4.1%) | 1124 (83.6%) | |
Chi-squared: P < 0.001; Kappa correlation: P < 0.001.
DISCUSSION
Male excess of hearing issues
In this study, the males showed significantly higher rates of a range of hearing issues (self-reported hearing difficulty, hearing aids, tinnitus, having had a doctor identify a hearing issue, and ear surgery or procedure). Previous research has shown similar results, with males more likely to have hearing difficulties than females due in part to increased exposure to noisy workplaces,[11] military service,[12] and firearm use.[13] As expected, males in this study showed higher rates of asymmetric hearing loss, typically in their left ear (usually reflecting noise-induced hearing loss) than females. Hearing loss in a person’s left ear is often due to the person turning to monitor equipment being towed behind a truck or tractor, and thus being exposed to the engine and exhaust noise, or the use of firearms.[13] A similar study described male excess hearing loss that persisted after controlling for age, education, noise exposure, and occupation, and an association with risk factors including smoking or atherosclerosis was proposed.[14]
Reluctance to seek assistance for hearing loss
Despite the male excess in hearing issues, this study showed that males accessed audiology services at a similar rate to females. Benova et al. [15] suggested that females were less likely than males to acknowledge their hearing difficulties to a health professional, but more likely than males to use hearing aids if they were recommended. Reluctance to access audiology services, and in particular to consider hearing aids, is a common issue, and stigma, expense, and trust contribute to this reluctance (reviewed by McMahon et al. [5].
Hearing aids
The percentage of people in this study with hearing aids (10.0% of males and 4.8% of females) was lower than the study by Kiely et al. [8] (11.4% in people aged ≥50 years), which is likely to be due to the younger age of the participants in this study (mean of 45 years). It is estimated that 80% of people aged 55 to 74 years who would benefit from hearing aids do not use them.[16] Even if a person has had hearing aids fitted, a proportion of aids are not used regularly, referred to as “hearing aids in drawer.”[2] Appropriate fitting of hearing aids is associated with decreased depression, increased life expectancy, and improved retention in the workforce.[5]
Farming and hearing loss
This study showed that farmers were significantly more likely to have hearing loss in their better ear than nonfarmers, and most of the respondents who identified as farmers were male. There is likely to be an underestimation of the prevalence of hearing issues across the region, as the recruitment for this study was limited to people residing in towns, rather than on farms. The prevalence of hearing loss in Australian farmers exceeds 50%, and the risk increases with age and remoteness.[1] Reports suggest that only 18% of farmers use hearing protection.[1] Agricultural field days present an opportunity to screen and educate farmers in a way that overcomes issues associated with distance and time away from farming duties.[17]
Industrial deafness/exposure to firearms
Industrial hearing loss is a common cause of hearing loss and can be short or long term, and is more likely with prolonged exposure. In this study, males were significantly more likely to report industrial or work-related hearing loss than females. This pattern has been reported previously, where men were more likely than women to report industrial or work-related hearing loss.[18] Although only small numbers of responses were recorded, 10 male participants in this study attributed their hearing loss to their use of firearms, or time in the military, whereas no women made this comment. Hearing loss due to use of firearms is more common in males than females and is thought to be due to males using more powerful firearms and using firearms more regularly than females.[19] These results suggest that targeted screening or intervention may be required to address the increased risk of hearing damage for men.
Older people with hearing loss
As expected, this study demonstrated significantly higher rates of hearing loss among older age groups, in both males and females. Prevalence of hearing loss increases in line with increasing age.[20] The rates of hearing loss found in this study were lower than rates reported in similar studies. This may be explained by the use of an audiology screening test that included only mid-range frequencies (1, 2, 4 kHz) and did not test lower or higher frequencies.
Audiology service use
Access to audiology service in rural, regional, and remote Australia can be patchy, and in general, numbers of audiology and speech therapy services decline from major cities to regional areas to remote areas.[1] The average waiting time for audiology services can be difficult to ascertain across rural Australia. Australian guidelines for the management of otitis media in Aboriginal children propose that an acceptable waiting time for audiology services is 3 months or less and 6 months or less for ear, nose, and throat specialist appointments.[21] Telemedicine has been found to be a well-accepted method to reduce waiting times and cost of audiology services.[22] In this study, most people waited less than 7 days for an audiology appointment, suggesting good service accessibility. Furthermore, participants in this study were highly satisfied with the service they received and accessed the services locally. However, it must be recognized that there is likely to be a proportion of people, particularly males, who would benefit from audiology review and advice but have not accessed these services. These findings suggest that improvements can be made in service accessibility and acceptability. Trust in audiology services or providers of hearing aids may be an issue, which can be overcome by improving communication, sharing decision-making, demonstrating technical competence, avoiding pressuring hearing aid sales tactics, and offering comprehensive rehabilitation.[23]
Screening
This study suggests that screening of people for hearing issues may be warranted, especially in males, farmers, and in older people. Screening may need to be opportunistic to target these groups of people, perhaps in a general practice (GP) setting. Implementation of GP-based hearing screening program for adults over 50 years of age has been proposed to identify hearing issues at a sufficiently early stage.[5] However, one study reported that a half of all patients with hearing loss were not referred by GPs, which may suggest perceived financial barriers, time constraints, or inadequate education around the benefits of hearing assessment/rehabilitation.[24] Screening protocols particularly suited to rural areas such as internet or telephone-based testing may be beneficial.
CONCLUSION
Males in the Goulburn Valley showed a greater prevalence of hearing issues than females, by both self-report and audiology testing, which persisted after controlling for confounding factors. Audiology services in the region were reported to be highly satisfactory and were locally accessible within short waiting times. Despite this, a proportion of people with self-identified hearing concerns or hearing loss (by audiological testing) had not accessed audiology services and may benefit from doing so. There were also a group of people who had not recognized a hearing issue that was evident upon audiology testing. This study provides evidence for a need for targeted, opportunistic screening of men and older people in the region.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.National Rural Health Alliance. 2014 [Google Scholar]
- 2.Ciorba A, Bianchini C, Pelucchi S, Pastore A. The impact of hearing loss on the quality of life of elderly adults. Clin Intervent Aging. 2012;7:159–63. doi: 10.2147/CIA.S26059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stam M, Kostense PJ, Lemke U, Merkus P, Smit JH, Festen JM, et al. Comorbidity in adults with hearing difficulties: which Which chronic medical conditions are related to hearing impairment? Int J Audiol. 2014;53((6)):392–401. doi: 10.3109/14992027.2013.879340. [DOI] [PubMed] [Google Scholar]
- 4.Williams W, Brumby S, Calvano A, Hatherell T, Mason H, Mercer-Grant C, et al. Farmers’ work-day noise exposure. Aust J Rural Health. 2015;23((2)):67–73. doi: 10.1111/ajr.12153. [DOI] [PubMed] [Google Scholar]
- 5.McMahon CM, Gopinath B, Schneider J, Reath J, Hickson L, Leeder SR, et al. The need for improved detection and management of adult-onset hearing loss in Australia. Int J Otolaryngol. 2013;2013:7. doi: 10.1155/2013/308509. doi: 10.1155/2013/308509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sindhusake D, Mitchell P, Smith W, Golding M, Newall P, Hartley D, et al. Validation of self-reported hearing loss. The Blue Mountains Hearing Study. Int J Epidemiol. 2001;30((6)):1371–8. doi: 10.1093/ije/30.6.1371. [DOI] [PubMed] [Google Scholar]
- 7.Swanepoel de W, Eikelboom RH, Hunter ML, Friedland PL, Atlas MD. Self-reported hearing loss in baby boomers from the Busselton Healthy Ageing Study: audiometric Audiometric correspondence and predictive value. J Am Acad Audiol. 2013;24((6)):514–21. doi: 10.3766/jaaa.24.6.7. [DOI] [PubMed] [Google Scholar]
- 8.Kiely KM, Gopinath B, Mitchell P, Luszcz M, Anstey KJ. Cognitive, health, and sociodemographic predictors of longitudinal decline in hearing acuity among older adults. J Gerontol A Biol Sci Med Sci. 2012;67((9)):997–1003. doi: 10.1093/gerona/gls066. [DOI] [PubMed] [Google Scholar]
- 9.Wilson DH, Walsh PG, Sanchez L, Davis AC, Taylor AW, Tucker G, et al. The epidemiology of hearing impairment in an Australian adult population. Int J Epidemiol. 1999;28((2)):247–52. doi: 10.1093/ije/28.2.247. [DOI] [PubMed] [Google Scholar]
- 10.Devers MC, Campbell S, Shaw J, Zimmet P, Simmons D. Should liver function tests be included in definitions of metabolic syndrome? Evidence from the association between liver function tests, components of metabolic syndrome and prevalent cardiovascular disease. Diabet Med. 2008;25((5)):523–9. doi: 10.1111/j.1464-5491.2008.02408.x. doi: 10.1111/j. 1464-5491. 2008.02408.x. [DOI] [PubMed] [Google Scholar]
- 11.Moore DR, Edmondson-Jones M, Dawes P, Fortnum H, McCormack A, Pierzycki RH, et al. Relation between speech-in-noise threshold, hearing loss and cognition from 40–69 years of age. PLoS ONE. 2014;9((9)):e107720. doi: 10.1371/journal.pone.0107720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pelausa EO, Abel SM, Simard J, Dempsey I. Prevention of noise-induced hearing loss in the Canadian military. J Otolaryngol. 1995;24((5)):271–80. [PubMed] [Google Scholar]
- 13.Berg RL, Pickett W, Linneman JG, Wood DJ, Marlenga B. Asymmetry in noise-induced hearing loss: evaluation Evaluation of two competing theories. Noise Health. 2014;16((69)):102–7. doi: 10.4103/1463-1741.132092. [DOI] [PubMed] [Google Scholar]
- 14.Cruickshanks KJ, Wiley TL, Tweed TS, Klein BE, Klein R, Mares-Perlman JA, et al. Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin. The Epidemiology of Hearing Loss Study. Am J Epidemiol. 1998;148((9)):879–86. doi: 10.1093/oxfordjournals.aje.a009713. [DOI] [PubMed] [Google Scholar]
- 15.Benova L, Grundy E, Ploubidis GB. Socioeconomic position and health-seeking behavior for hearing loss among older adults in England. J Gerontol B Psychol Sci Soc Sci. 2019;70:443–52. doi: 10.1093/geronb/gbu024. 10.1093/geronb/gbu024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCormack A, Fortnum H. Why do people fitted with hearing aids not wear them? Int J Audiol. 2013;52((5)):360–8. doi: 10.3109/14992027.2013.769066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lower T, Fragar L, Depcynzksi J, Challinor K, Mills J, Williams W. Improving hearing health for farming families. Rural Remote Health. 2010;10((1)):1350. [PubMed] [Google Scholar]
- 18.Jirojwong S, Joubert D, Anastasi S. Perceived industrial deafness and hearing loss among people in a small Queensland rural community. Southeast Asian J Trop Med Public Health. 2005;36((4)):1048–56. [PubMed] [Google Scholar]
- 19.Stewart M, Pankiw R, Lehman ME, Simpson TH. Hearing loss and hearing handicap in users of recreational firearms. J Am Acad Audiol. 2002;13((3)):160–8. [PubMed] [Google Scholar]
- 20.Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. Arch Neurol. 2011;68((2)):214–20. doi: 10.1001/archneurol.2010.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morris P, Ballinger D, Leach A. Recommendations for clinical care guidelines on the management of otitis media in Aboriginal and Torres strait islander populations. Canberra: Office for Aboriginal and Torres Strait Islander Health, Commonwealth Department of Health and Aged Care; 2001. [Google Scholar]
- 22.Eikelboom RH, Atlas MD. Attitude to telemedicine, and willingness to use it, in audiology patients. J Telemed Telecare. 2005;11(2):S22–5. doi: 10.1258/135763305775124920. [DOI] [PubMed] [Google Scholar]
- 23.Preminger JE, Oxenboll M, Barnett MB, Jensen LD, Laplante-Levesque A. Perceptions of adults with hearing impairment regarding the promotion of trust in hearing healthcare service delivery. Int J Audiol. 2015;54((1)):20–8. doi: 10.3109/14992027.2014.939776. [DOI] [PubMed] [Google Scholar]
- 24.Schneider JM, Gopinath B, McMahon CM, Britt HC, Harrison CM, Usherwood T, et al. Role of general practitioners in managing age-related hearing loss. Med J Aust. 2010;192((1)):20–3. doi: 10.5694/j.1326-5377.2010.tb03395.x. [DOI] [PubMed] [Google Scholar]


