Abstract
Background:
Hospitals provide treatment to improve patient health and well-being but the characteristics of the care environment receive little attention. Excessive noise at night has a negative impact on in-patient health through disturbed sleep. To address this hospital staff must measure night-time environmental noise levels. Therefore, an understanding of environmental noise measurement techniques is required. In this review, we aim to 1) provide a technical overview of factors to consider when measuring environmental noise in hospital settings; 2) conduct a rapid review on the equipment and approaches used to objectively measured noise in hospitals and identify methodological limitations.
Design:
A rapid review of original research articles, from three databases, published since 2008. Studies were included if noise levels were objectively measured in a hospital setting where patients were receiving treatment.
Results:
1429 articles were identified with 76 included in the review. There was significant variability in the approaches used to measure environmental noise in hospitals. Only 14.5% of studies contained sufficient information to support replication of the measurement process. Most studies measured noise levels using a sound level meter positioned closed to a patient’s bed area in an intensive care unit.
Conclusion:
Unwanted environmental noise in hospital setting impacts negatively on patient and staff health and well-being. However, this literature review found that the approaches used to objectively measure noise level in hospital settings have been inconsistent and poorly reported. Recommendations on best-practice methods to measure noise levels in hospital environments are provided.
Keywords: Hospital, indoor environment, measurement technique, noise, sound level
INTRODUCTION
“Noise” is defined as sound that is “unwanted”,[2,3,4] with the environments we encounter every day containing numerous noise sources (i.e. “environmental” noise). Hospitals are noisy environments with sounds produced by equipment, the beeping of pagers, the voices of staff and other patients.[5] The effect that excessive levels of such noise can have on patient care has been the topic of much research. Environmental noise can impact patient safety[6]; an extensive review by Pope reported that environmental noise in hospitals affects the sleep of patients, can increase their blood pressure and diminish their immune responses, as well as a host of other negative side effects.[4]
The World Health Organization (WHO) issued guidelines on the maximum amount of noise that should be present in hospitals. The guidelines suggest that noise on wards should not exceed 30 dB LAeq, whilst noise in treatment rooms should be kept “as low as possible”.[7] However, studies measuring environmental noise in hospitals have identified that such levels are not realistic. It has been noted that the guidelines did not account for the presence of patients, instead referring to buildings that are “empty”.[4] Moreover, noise levels on nursing units “frequently” exceed 100 dB LAeq, this being the equivalent of a car horn and far removed from the WHO guidelines.[4] Numerous other studies have attempted to quantify the levels of noise in hospitals.[5,8,9,10]
There are a number of limitations when measuring noise in hospitals that make a comparison between studies difficult. [9] Noise levels usually vary rapidly with time and so some form of single-figure or average figure is usually reported. There are many factors to consider in noise measurement and not all are appropriate for hospital noise assessment. They include time period, sampling rate, frequency range, frequency weighting, peak, maximum, percentile levels or energy average. Different measuring devices (e.g. sound level meters and dosimeters) and the different ways in which a device can be calibrated yield different results.[4,9] The purpose of this rapid review was to describe the equipment and approaches used in studies that objectively measured noise levels in hospitals and identify any associated methodological limitations. Recommendations will be developed to guide the accurate measurement, documentation and reporting of environmental noise measurements in hospitals.
METHODS
A “rapid review” enables an evaluation of existing literature using systematic review methods, whilst allowing for a reduction in the breadth and depth of a full systematic review.[11] The WHO guidelines for rapid reviews states that the literature search can be limited to two or more databases with additional limits on date, language and study design.[12] Although potentially relevant research studies might not be identified using this approach, there is evidence to show that conclusions determined from rapid reviews are similar to conclusions reached in more comprehensive reviews.[13]
Search strategy
Original research articles were identified from three databases (Scopus, PubMed and Cochrane Library) to enable identification of research studies published in both medical and acoustics journals. Input from an Information Technologist enabled us to develop a robust search strategy (see Appendix A) which was piloted. Boolean operators were used to combine search terms relating to “noise” and “hospitals”. Several search limits were applied to reduce the breadth and depth of the review, as permitted by rapid review guidelines.[11,12] Searches were limited to English Language only and due to technological advances in sound measurement, were restricted to articles published in the last ten years (≥2008).
Article selection process
Following removal of duplicates, all articles identified from the searches were screened firstly by title/abstract before full-text screening by one author (R.W.) who had expertise in acoustics. Research of any design was included into the review. A random sub-sample of 20 articles considered relevant for inclusion into the review were independently checked against the entry criteria by two authors (E.H. and F.A.). Included studies fulfilled the following criteria;
-
(1)
Research studies focusing on environmental noise measurements in hospitals as a primary aim;
-
(2)
Studies conducted in a hospital setting;
-
(3)
Studies that report objectively measured noise levels using a device which gives an output in decibel (dB);
-
(4)
Studies that report indoor levels of noise in areas where patients (adults and children) are being treated (i.e. wards, intensive care units, operating theatres, out-patient clinics);
Studies reported in English language.
Data extraction
Data were extracted from all included studies into a tabular format by one author (R.W.). To reduce reporting bias, data from a random sample of 20 studies was independently extracted by another author (WJD) and compared with the original data extraction table. Information extracted included authors, year of publication, setting, noise level measurement device details, location of device, time period of measurements, amplitude type, weight network, time constant, calibrations made and type of noise parameter recorded.
Quality appraisal
The way in which the technical aspects of the included studies were reported was appraised by one author (R.W.). To reduce reporting bias, a random sample of 20 articles were appraised independently by another author (H.L.). Classification of the reporting quality of the studies were based on inclusion of the following variables; the setting; the measuring device used; the location of the device; the time period for the measurement; the type of amplitude measured; the weighting network used; the time constant; the calibration process; and the type of sound level parameter measured (e.g. Leq, Lmax, etc.). Studies were appraised as “comprehensive” if all of these variables were provided in sufficient detail to enable an accurate reproduction of the measurement process; “average” for studies that included information on most of the aforementioned variables, but not all; and “limited” if either vital information was omitted or ambiguities demonstrated in their measurement process, or both. A variable was considered as being “vital” if significant changes in the measurement data could arise if the parameters were changed (this being judged based specifically on the present context of measurements within hospitals). For example, A-weighting in sound pressure level (SPL) measurement attenuates low frequencies heavily with respect to C-weighting and so it is reasonable to suggest that a 24-hour measurement on an ICU with the respective networks applied would yield different results. Given this, failure to indicate the weighting would mean that assumptions would need to be made about the measurement process and this can affect the validity of the data.
RESULTS
Fig. 1 provides an overview of study selection process; 1429 articles were screened (649 from Scopus, 74 from Cochrane and 706 from PubMed), of which, 111 full-texts were assessed for eligibility against inclusion criteria and 76 articles included in the review. The included studies were conducted across 22 countries; USA (26), UK (6), Turkey (5), Taiwan (4), Australia (4), Brazil (3), Canada (3), China (3), India (3), Iran (3), Portugal (2), Germany (2), Sweden (2), France (2), Spain (1), Greece (1), South Africa (1), Finland (1), Switzerland (1), Argentina (1), Belgium (1) and Italy (1).
Figure 1.
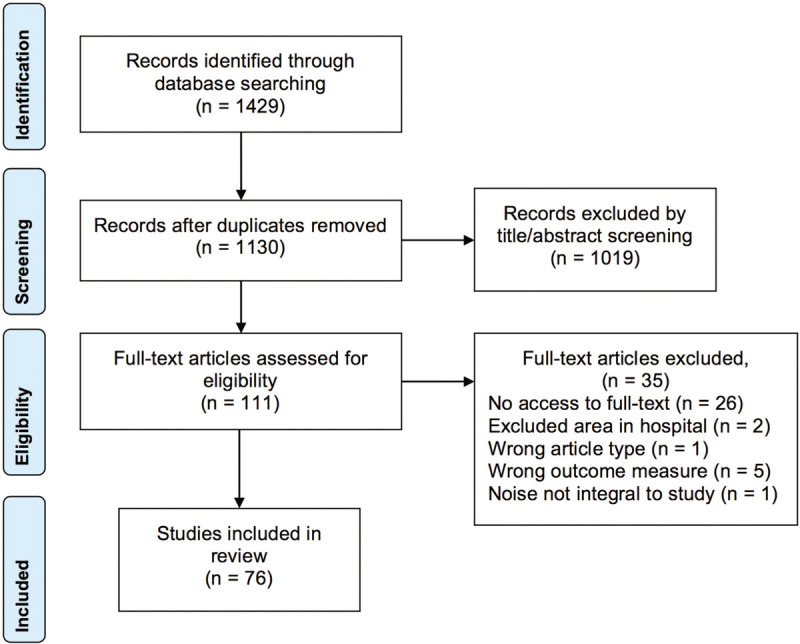
Flow diagram of search strategy and article selection for systematic search and review modified from Moher et al.[14]
Characteristics of the measurement approaches used in studies reporting noise levels in hospitals
Table 1 presents an overview of the study characteristics and measurement approaches used.
Table 1.
Study characteristics and approaches used to measure hospital noise levels from included studies
| Author | Reporting rating | Setting | Device used | Device location | Time period | Type of amplitude measured | Weighting | Time constant | Calibration | Measurements Made |
|---|---|---|---|---|---|---|---|---|---|---|
| Elliott et al.[15] | Comprehensive | ICU (Australia) | Bruel and Kjaer 2250 SLM (class not stated) | Between 0.75 and 1 m above the patient’s head, 1.75 m above the ground, 1 m below the ceiling, 1.5 m from the wall | 24-hours | Pressure | A, C | Fast | Yes | LAeq, LCpeak, LAmax, LAmin, LCeq, LA90 |
| Liu [16] | Comprehensive | NICU (USA) | Larson Davis Spark 706 dosimeter (Type-II) | Bedside (mic 12 inches above the infant’s head), within an incubator (mic halfway between infant’s head and top of incubator), staff work area (suspended from the ceiling, no more than 5 feet above the desk), central entry area (suspended from ceiling, no more than 5 feet above desk) | 24-hours (Leq at 1-s, 1-min, 5-min and hourly intervals, LA10, LA50 and LA90 recorded for 1, 3, 4 and 6-hour intervals) | Pressure | A | Slow | Yes | LAeq, LA10, LA50, LA90 |
| Matook et al.[17] | Comprehensive | NICU (USA) | Quest Sound Pro DL-2 SLM (class not stated) | In a b-ox placed on a shelf in the quadrant of an NICU bay | Two 12-hour recordings (0700-1900 and 1900-0700), 60-s intervals | Pressure | A | Slow | Yes | LAeq, LAmax, LApeak |
| Pope [4] | Comprehensive | Medical/surgical nursing units (USA) | Quest Q300 noise dosimeters (class not stated) | Behind the beds of patients with additional measurements made both at nurse’s station and with microphones attached to nurses | 12-hours (0625-1830) | Pressure | A | Slow | Yes | LAeq, LAmin, LAmax, LApeak |
| Short et al. [18] | Comprehensive | Emergency department (Australia) | Digitech QM 1588 SLM (class not stated) | shelf, 1.4 m above the head of patients’ beds in 6 areas − triage, acute, short stay, resuscitation, paediatrics and cubicles | 24-hours at 15-min intervals | Pressure | A | Fast | Yes | LAeq, LAmax, LAmin |
| Memoli et al.[19] | Comprehensive | ICU (UK) | NPL-Minim with MEMS microphones(conforming to Class-I) | Detailed diagram provided of all microphone locations | 30-min continuous recording, with all measurements taken at intervals of 15-min, 1-min and 1-s | Pressure | A | Fast | Yes | LAeq, LAmax, LAmin, LA0.1, LA5, LA10, LA25, LA50, LA75, LA90, LA95 |
| Carvalhais et al.[20] | Comprehensive | NICU (Portugal) | 01 dB model Solo-Premium Class-I SLM (model not stated) | At least 1 m away from the wall at a height between 1 and 1.65 m | 24-hours | Pressure | A, C | Slow | Yes | LAeq, LCpeak, LA90 |
| Knauert et al.[21] | Comprehensive | ICU (USA) | Extech Instruments HD600 SLM (Type-II) | Central location in patient’s room adjacent to the foot of the patient’s bed | 2000-0800, 2000-2359, 0000-0359 and 0400-0800, 10-s intervals | Pressure | A, C | Fast | Yes | LAeq, LCpeak |
| Luetz et al. [22] | Comprehensive | ICU (Germany) | XL2 SLM with M2233 microphone (class and manufacturer not stated) | 40 cm from patient’s head (additional SLMs placed at windows and doors) | 24-hours, 1-min intervals | Pressure | A | Fast | Yes | LAeq, LAmax |
| Fasih-Ramandi and Nadri [23] | Comprehensive | ICU (Iran) | Cel 450 SLM (class not stated) | Above the beds | 24-hours, 5-min intervals | Pressure | A | Fast | Yes | LAeq, LAmax, LAmin |
| Santos et al.[24] | Comprehensive | NICUs of 3 hospitals (Portugal) | Solo-Premium Class-I SLM (model not stated) | At least 1 m away from walls/equipment at a height of between 1 and 1.65 m and also inside incubators | 24-hours | Pressure | A, C | Slow | Yes | LAeq, LCpeak |
| McLaren and Maxwell-Armstrong [25] | Average | Surgical Wards (UK) | Type 230 Integrating octave band SLM (manufacturer and class not stated) | Entrance to the second bay (consisting of 6 beds), approximately 4 m from the nursing station. | 24-hours (15 minute intervals at 4-hourly time periods), Wednesday-Thursday | Pressure | A | Not stated | Not stated | LAmax, LAeq |
| Nathan et al. [26] | Average | NICU (South Africa) | Type-I SLM (manufacturer and model not stated) | Suspended from the ceiling in each room at a height of 2 m | Two 12-hour intervals in each room (0800 − 2000) on consecutive weekdays | Pressure | A | Not stated | Not stated | LAeq, LAmax, LAmin |
| Chen et al. [27] | Average | NICU (Taiwan) | NL-31 & Rion Co. SLMs (class not stated) | Bedside, away from walls & floor | 24 hours, with hourly data reported | Pressure | A | Slow | Not stated | LAeq, LAmax, LA10, LA90 |
| Lasky and Williams[28] | Average | NICU (USA) | Larson Davis Spark 703+ PND (class not stated) | Inside patients’ beds, within 30 cm of their ears | 1-s intervals | Pressure | A | Not stated | Not stated | LAeq |
| Richardson et al.[29] | Average | Wards (UK) | Norsonic NOR-116 SLM (class not stated) | Corner of a 6-bed bay, 1 m from the ground and 1 m from the wall, on a tripod | 24-hours | Pressure | A | Not stated | Yes | LAeq, LApeak |
| Williams et al.[30] | Average | NICU (USA) | Larson Davis Spark 703+ PND (class not stated) | Inside the upper corner of the incubator, 12 inches from the child’s ear | 2-hours (1-s intervals) in the period between 0800 and 1700, ideally between 1000 and 1200 (Monday-Friday) | Pressure | A | Not stated | Yes | dBA SPL |
| Hsu et al.[31] | Average | ICU (Taiwan) | RION NL-22 Type-II SLM | Bedside, 30 cm from the patients’ heads | 42-hours (1-s intervals), divided into seven 6-hour periods | Pressure | A | Not stated | Not stated | LAeq, LAmax, LAmin |
| Hu et al.[32] | Average | ICU (China) | AWAI AWA5610D SLM (class not stated) | Bedside | 24-hours | Pressure | A | Not stated | Not stated | Mean, peak and minimum LpA |
| Lawson et al.[33] | Average | ICU (both in patient rooms and in rooms adjacent to them) (USA) | Bruel and Kjaer SLM (model and class not stated) | Microphone suspended from ceiling (6 inches above bed pillow) | Ten 24-hour periods with 15-min intervals for the LAeq measurement, 10-s intervals for peak measurements | Pressure | A, C | Not stated | Yes | LCpeak, LAeq |
| Gladd and Saunders[34] | Average | Treatment room of chemotherapy clinic (USA) | Bruel and Kjaer 2250 SLM (class not stated) | Suspended 1 foot from the ceiling in the centre of each room | 11-hours (daytime), 1-s intervals | Pressure | A, C | Not stated | Yes | LCpeak, LAeq |
| Johansson et al.[35] | Average | ICU (Sweden) | Bruel and Kjaer 2260 SLM (class not stated) | Close to patients’ beds | 24-hours | Pressure | A | Fast | Not stated | LAeq24hours, LAFmax |
| Liu[36] | Average | NICU (USA) | Larsen Davis Spark 706 dosimeter (class not stated) | Bedside, 8-12 inches above the infant’s head | 24-hours | Pressure | A | Slow | Not stated | LAmin, LAmax, LA90, LA50, LA10, LAeq |
| Xie and Kang[37] | Average | ICU | Solo Type-I SLM (model and class not stated) | 1.2 m height between the wall and patient’s bed (close to the patient’s head), away from reflecting surfaces | 30-min measurements periods throughout the night, 1-s intervals | Pressure | A | Not stated | Not stated | LAeq, LAmax, LA5, LA10, LA50, LA90 & LA95 |
| Zamberlan-Amorim[38] | Average | NICU & nursing ward (Brazil) | Quest-400 dosimeter (class not stated) | Central area of each room and suspended 70 cm from the ceiling | Fourteen 12-hour recordings (0700-1900 and 1900-0700) | Pressure | A | Not stated | Not stated | LAeq, LAmax, LApeak |
| Cordova et al.[39] | Average | Burn ICU (USA) | A-weighted SLM (manufacturer, model and class not stated) | Centre of the nurses’ station, 6 m from the patients’ rooms on average, additional measurements within random rooms (near patients’ heads) | 24-hour measurements with 5-s intervals over 1 month | Pressure | A | Not stated | Not stated | LAmax, LAmin, LAeq |
| Darbyshire and Young[40] | Average | ICU (UK) | CEL-630 SLM (class not stated) | One SLM central in the room and another near the patients’ heads (patients central to the room were generally chosen) | 24 hours, 1-min intervals | Pressure | A | Not stated | Yes | LApeak, LAeq |
| Ginsberg et al.[41] | Average | Operating theatre (USA) | Thomas Scientific 8331A20 SLM (class not stated) | Flat on the anesthesia machine in the operating room | 2-minute intervals at different points throughout the surgery | Pressure | A | Not stated | Not stated | LAmax |
| Fortes-Garrido et al.[42] | Average | NICU (Spain) | Bruel and Kjaer 2270 & 2250 SLMs (Type-I) | Central in the NICU, 80 cm below the ceiling, 153 cm from the wall in one room & 80/215 in the other | 15 days (1-s intervals) | Pressure | A | Fast | Not stated | LA10, LA50, LA90, LAeq1h |
| Kol et al. [43] | Average | Pediatric ICU (Turkey) | Extech 407780 SLM (class not stated) | At least 1 m away from surfaces and 1-1.5 m away from architectural elements (windows/air vents/ etc.) | 12-hour measurements with 5-s intervals over 1 month | Pressure | A | Not stated | Yes | LAeq, LAmax, LAmin |
| Kol et al.[44] | Average | ICU (Turkey) | Extech 407780 SLM (class not stated) | Between 2 patient’s beds and the nurses’ station, at least 1 m away from surfaces and architectural elements | 24-hours | Pressure | A | Not stated | Yes | LAeq, LAmax, LAmin |
| Hu et al.[45] | Average | ICU (China) | AWAI AWA5610 SLM (class not stated) | Horizontally, 10 cm away from the patient’s auricle | 24-hours, 20-min intervals | Pressure | A | Not stated | Not stated | LAeq |
| Calikusu and Balci[46] | Average | NICU (Turkey) | Geartech DT-8852 SLM (class not stated) | On a table in the noisiest area of the ICU (diagram provided in study) | 24-hours, 1-s intervals | Pressure | A | Not stated | Yes | dBA SPL |
| Giv et al.[47] | Average | Operating theatre (Iran) | Noise level gauge | At the location of staff and surgeons | 5-min periods at the start of, during and after surgery | Pressure | A | Not stated | Yes | LAeq, LAeq10, LAeq50, LAeq90, noise pollution level (NPL) |
| Parra et al.[48] | Average | NICU (France) | ACOEM WED noise dosimeter (class not stated) | One microphone in the centre of the room (50 cm from any surface) and another inside the incubator within 30 cm of the ear of each patient | 24-hours, 1-s intervals | Pressure | A | Not stated | Not stated | LAeq, LAmax, LA10 |
| Voigt et al.[49] | Average | ICU (USA) | IC Sentinel (for simultaneous sound and light measurement) | Placed to the left of the patient’s bed, near the head, directly under the main ceiling lights | 1-hour periods, with different times of day simulated | Pressure | A | Not stated | Yes | dBA SPL |
| Akansel and Kaymakci[50] | Limited | ICU (Turkey) | Bruel Kjaer 2144 Model Deal Channel Frequency Analyser SLM (class not stated) | Patients’ beds (1.5 m above the floor) | 24 hours (15-min intervals), Monday-Friday | Pressure | A | Not stated | Not stated | Average from individual dBA SPL readings |
| Darcy et al.[51] | Limited | NICU (USA) | Sper Scientific Mini Sound Meter 840014C SLM (class not stated) | Central location for each room (within reason to avoid getting in the way) | 12-hours (day & night periods), 5-min intervals | Pressure | A | Slow | Yes | Average from individual dBA SPL readings |
| Dube et al.[9] | Limited | PCU (USA) | Type-II noise dosimeter (Quest Technologies Q-300), Type-II SLM (Quest Technologies 2900) | Central desk | 24-hours | Pressure | A | Not stated | Yes | Average from individual dBA SPL readings |
| Livera et al.[52] | Limited | NICU (India) | Digital SLM (class not stated) | Single measurements in adjoining rooms of NICUs and hourly measurements in the centre of NICU rooms | Single measurements at 3 AM, additional hourly measurements for 15 days | Pressure | Not stated | Not stated | Not stated | Average from individual dB SPL readings |
| Taylor-Ford et al.[53] | Limited | Surgical Wards (USA) | Quest 2900 SLM (class not stated) | Nursing station, suspended from ceiling | 6 days, 10-min intervals | Pressure | Not stated | Not stated | Not stated | Leq, Lmin, Lmax, L10, L90 |
| Tsara et al.[54] | Limited | ICU (Greece) | Cirrus CR: 245/R2 Environmental Noise Analyser (Type-I) | Noise-monitoring stations placed in each department | 24-hours (divided into three 8-hour periods), 1-hour intervals | Pressure | A | Not stated | Not stated | dBA SPL & LAmax |
| Vinodhkumaradithyaa et al.[55] | Limited | Tertiary Care Hospital (India) | Type-I Digital SLM (Manufacturer and model not stated) | At body level in 14 areas of the hospital | 1-hour (morning & evening periods), 3-min intervals | Pressure | A | Fast | Not stated | LAeq, LA10, LA90, LAmax, LAmin |
| Altuncu et al.[56] | Limited | NICU (Turkey) | 2235 Bruel & Kjaer SLM (class not stated) | Near the head of the infant in the NICU | 5-minute period in the morning, 15-s intervals | Pressure | A | Slow | Not stated | Median from individual LpA readings |
| Macedo et al.[57] | Limited | ICU (Brazil) | Minipa MSL-1532C SLM (class not stated) | Not stated | 2-hour periods for morning, afternoon & night | Pressure | A | Not stated | Not stated | Average from individual dBA SPL readings |
| Ramesh et al.[58] | Limited | NICU (India) | Portable digital SLM (manufacturer, model and class not stated) | Centre of each room in the NICU | Hourly noise measurements over 15 days | Pressure | Not stated | Not stated | used “standard sounds” | Geometric mean of individual LpA readings |
| Dennis et al.[59] | Limited | Emergency Department(USA) | Sper Scientific 8400029 SLM (class not stated) | Central nursing station, entrance of patient’s doorway & next to patient’s right ear | 5-s measurements − 30 mins before & after quiet time and one 1h 30m before the end of quiet time | Pressure | Not stated | Not stated | Not stated | Average from individual LpA readings |
| Juang et al.[60] | Limited | Hospital ward (Taiwan) | Lutron 4030 SLM (class not stated) | 1.5 m above the ground | 1-hour recordings over 5 days between 0830-0930, 1130-1230 and 1600-1700 | Pressure | Not stated | Not stated | Yes | Average from individual dB SPL readings |
| Merilainen et al.[61] | Limited | ICU (Finland) | Not stated | Next to patient’s bed | Not stated | Not stated | Not stated | Not stated | Not stated | Average from individual dB SPL readings |
| Khademi et al.[62] | Limited | Wards of ICU, emergency & kidney transplant departments of hospital (Iran) | EXTECH 407727 SLM (class not stated) | Not Stated | 2-min intervals every 30-mins for 5 days | Pressure | Not stated | Not stated | Yes | Leq, Lpeak |
| Kurmann et al.[63] | Limited | Operating theatre (Switzerland) | PCE 353 SLM (Class not stated) | Directly above the operative field | Measurements taken once per second | Intensity? | Not stated | Not stated | Not stated | dB |
| Li et al. [64] | Limited | Surgical ICU(Taiwan) | TES-1352A-RS232 SLM (class not stated) | 30 cm away from the head of the bed with another on the nurses’ station | Nighttime | Pressure | Not stated | Not stated | Not stated | Average from individual dB SPL readings |
| Linder and Christian[65] | Limited | Pediatric oncology unit (USA) | Extech Instruments 407736 digital SLM Type-II (class not stated) | Bedside supply cart for each patient (48 inches from the bed) | 12-hours, 30-s intervals (nighttime) | Pressure | Not stated | Not stated | Yes | dB SPL |
| Olivera et al.[66] | Limited | NICU (Argentina) | Type-II Center 322 Sonometer | In a corner between 2 incubators | 24 hours, 5-s intervals | Pressure | A | Fast | Yes | Average from individual dBA SPL readings |
| Salandin et al.[10] | Limited | ICU (Germany) | Integrated acoustic-level-analyser (DIN EN 60651, Class-I) | “Representative locations of an ICU” | 48-hours | Pressure | A | Fast | Not stated | LAeq, LAmax, LA5, LAmin |
| Van Enk and Steinberg[67] | Limited | NICU (USA) | Extech Instruments 407736 dosimeter (class not stated) | Near the patient’s head | Two 30-s readings taken over a 90-s period | Pressure | A | Slow | Not stated | Median from individual dBA SPL readings |
| Elser et al.[68] | Limited | NICU (USA) | Quest Technologies NoiseProDL dosimeter (class not stated) | Within 6 inches of the child’s head in an incubator | 20-mins | Pressure | Not stated | Not stated | Not stated | Leq, Lpeak |
| Guerin et al.[69] | Limited | Pharmacy department (Canada) | Class-II TES 1353 & Class-II Bruel & Kjaer 2240 SLMs mounted on tripods (1.45 m from floor) | Measurements made in 13 zones in the department, 1-5 measurement points were used based on the surface area of each zone | A series of 3-hour periods for both day and night with LAeq recorded at 5-min intervals | Pressure | A | Slow | Yes | LAeq5min |
| Padmakumar et al.[70] | Limited | ICU (UK) | Tecpel DSL-330 SLM (Type-II) | Adjacent to patient’s bedside, 1 m above and to the right of the patient | 24-hours with 3-s intervals | Pressure | A | Fast | Yes | LAmax, LAmin, ’average’ |
| Tegnestedt et al.[71] | Limited | 3 different rooms within an ICU (Sweden) | Spark 706 Larson Davis dosimeter (class not stated) | Behind the headrest of the ICU bed, 1 m from the patient’s head | Five 24-hour periods | Pressure | A,C | Slow for LAeq, fast for Lpeak | Not stated | LAeq, LAmax, Lpeak |
| Verhaert et al.[72] | Limited | Operating theatre (Belgium) | CR110A doseBadge dosimeter & NOR140 sound analyzer (class not stated) | Dosimeter attached to shoulders of surgeon & surgeon’s assistant | Measurement periods between 1h 47m & 2h 49m depending on surgical procedure being measured | Pressure | A,C | Not stated | Yes | LAeq, LCpeak, LA95 |
| Wang et al.[73] | Limited | ICU (USA) | Bruel and Kjaer 2260 SLM (Class not stated) | Nine locations around the ICU, with an additional six in corridors | Six 90-min periods, 8-min intervals | Pressure | A | Not stated | Not stated | LApeak, mean |
| Bano et al.[74] | Limited | Internal medicine ward (Italy) | PCE-222 phonometer | Placed on a 1.4 m high trolley in the middle of each room | 5-min periods, 1-s intervals, during 0730-0830, 1330-1430, 1830-1930 and 2330-0030 | Pressure | A | Not stated | Not stated | Average |
| Filus et al.[75] | Limited | Emergency ward (Brazil) | Bruel and Kjaer 2230 SLM (class not stated) | Carried by evaluator, measurements made at 10 sites in the ER | 2m 30s periods with three repeats for each site throughout the day | Pressure | A | Not stated | Yes | LAmin, LAmax,LAeq |
| Wang et al.[76] | Limited | NICU (Canada) | SoundEar noise meters (class and model not stated) | Single noisemeters placed in each patient area (pod), with another in a central desk area | 2 months, 5-min intervals | Pressure | Not stated | Not stated | Not stated | Leq |
| Wang et al.[77] | Limited | NICU (Canada) | SoundEar noise meters (class and model not stated) | Noisemeters placed in 4 locations in the ward | 2 months, 5-min intervals | Pressure | Not stated | Not stated | Not stated | Leq |
| Hill and LaVela[78] | Limited | Patient rooms & nursing stations (USA) | Amprobe SM-20A SLM (class not stated) | 3 patient rooms & 3 nursing substations | 24-hours, 8-min intervals | Pressure | A | Slow | Yes | Average, LAmax, LAmin |
| Watson et al.[79] | Limited | NICU, PICU, CICU (USA) | QuestTechnologies dosimeter (class and model not stated) | Attached to the lapels of patients | Six 4-periods over 24-hours | Pressure | A | Not stated | Not stated | Mean dBA |
| Yelden et al.[80] | Limited | Inpatient neurological rehabilitation unit (UK) | Tecpel 331 SLM(Class-I) | Within 1 m of patient’s bedside at head level and at least 2 m from the door | Six 2-hour periods over 12-hours, 30-s intervals | Pressure | Not stated | Not stated | Not stated | Mean from collected SPL readings |
| Chow and Shellhaas[81] | Limited | NICU (USA) | Digital language processor − noise levels extracted using software | On the arm of each infant’s isolette | 16-hour recordings, split into day & night, with 5-min intervals | Not stated | Not stated | Not stated | Not stated | Mean, peak |
| Daraiseh et al.[82] | Limited | Pediatric inpatient units (USA) | QuestTechnologies Noise Pro DL(class not stated) | Dosimeter attached to the shirt collar of nurses (as close to the ear as possible), additional dosimeters attached to the head of patients’ beds | Six 4-hour recordings over a 24-hour period (5-min intervals) | Pressure | A | Not stated | Not stated | Mean from individual readings |
| Kramer et al.[83] | Limited | Pediatric ICU (USA) | QuestTechnologies NoisePRO DLX dosimeter(class not stated) | Microphone 1 m from the patient’s head | 24-hours, 1-min intervals | Pressure | A | Not stated | Yes | Average, LApeak |
| Delaney et al.[84] | Limited | ICU (Australia) | Extech SDL 600 (class not stated) | Nurses’ station & patient’s clinical environment (mounted adjacent to patient’s head, 155 cm away) | 9-hours, 5-s intervals | Pressure | A | Not stated | Not stated | dBA SPL (mean and peak taken from these) |
| Elbaz et al.[85] | Limited | ICU (France) | NoxMedical T3 Microphone (class not stated) | 40 cm from patient’s head | 24-hours, 30-s intervals | Pressure | C | Not stated | Not stated | Took medians from collected SPL data |
| Ramm et al.[86] | Limited | NICU (Australia) | Extech Sound Level Datalogger Dosimeter (class not stated) | Above a sink in a “high traffic area” in each room (0.5 m from the ceiling and 2.16 m from the floor) between 2 bed spaces | 4-weeks, 60-s intervals (day broken down into different periods for analysis) | Pressure | Not stated | Not stated | Not stated | Max, min |
| White and Zomorodi[87] | Limited | Nurses’ stations in critical care units (USA) | Decibel 10th iPhone App (version 3.8.1–iPhone model not stated) | Central nurses’ station and individual nurses’ station | Six 30-s periods both for morning and evening | Pressure | Not stated | Not stated | Not stated | Average from individual LpA readings |
Of the 76 studies that measured environmental noise in hospitals since 2008, noise levels were most commonly measured in an intensive care unit (70% of studies), while the remaining studies reported noise levels in emergency departments, patient wards, operating theatres, a pharmacy department or multiple locations around a hospital. The majority of studies (66%) used some form of Sound Level Meter (SLM), whilst a further 20% used dosimeters to measure noise levels in a hospital setting. There was a large amount of variation in the location of the measuring device between studies, with 47% of studies using the area around the patient’s bed as the location for recording noise measurements. Furthermore, the measurement durations varied widely, with numerous studies recording both day and night noise levels and at different periods of time throughout the day. The majority of studies (96%) explicitly stated that SPLs were measured and 66% of studies used an A-weighting network. The most popular measurement method was the time-average SPL (Leq), being present in 58% of all studies. Lmax (maximum SPL) and Lmin (minimum SPL) were also popular (38% and 28% respectively). The arithmetic “average” of sound levels was calculated in 26% of all studies, but details on this calculation were ambiguous. Each study using this approach was rated as “limited” for reporting quality.
Quality appraisal of measurement approaches
The way in which the technical aspects of the included studies was reported was appraised as “comprehensive” for 11 studies, “average” for 25 studies and “limited” for 40 studies. This means that only 14.5% of the 76 hospital studies included in the review, provided sufficient details to enable the authors to repeat the measurement.
A high proportion of studies were able to provide sufficient information about the measurement process in some areas. With respect to the time periods in which the measurements were conducted, 97% of all studies provided information on both the duration of the measurement process and also the sampling period for measurements. Similarly, most studies (87%) also provided details about the specific location of the measuring instruments.
However, it is important to note that there were a number of key absences across the studies. The time constant, for example, was only discussed in 33% of all studies, whilst only 43% provided information about the calibration process. Moreover, although the details on the frequency weighting function used in the respective studies was generally present, with 78% of studies including this information (65.8% for A-weighting, 10.5% for C-weighting and 1.3% for both), 22% were not explicit as to which network was used.
Recommendations
Based on this review, the following recommendations are provided to guide the accurate measurement and documentation of environmental noise measurements in hospitals.
Purpose. A noise survey may have a variety of different approaches and the specific purpose should be identified. The noise survey may be designed to assess the noise exposure at specific patient bed spaces, noise exposure of staff or measuring the noise climate of specific rooms or types of setting. The measurements may be made to assess compliance with a benchmark (such as WHO) or to compare with environmental noise levels across similar settings or as part of a noise reduction programme.
SLM setting. The purpose of the noise survey will determine the choice of instrumentation. Currently there is no standardised method for measuring hospital noise. Modern sound level meters are often capable of measuring many different acoustic metrics. The accuracy and comparability of all of these metrics is not guaranteed, not least because permitted tolerances of sound level meters are defined for a limited range of metrics.[1] This makes it difficult for the non-specialist to know what to measure and why. Many of the studies included in this review compared their results to the WHO guidelines, which are expressed in LAeq (A-weighted time-average SPL) and LAFmax (A-weighted maximum SPL measured over a given period of time with ‘fast’ time constant (i.e. 125ms)).
For most long-term measurement applications in a hospital environment, A-weighting would be most appropriate since it considers the frequency-dependent loudness perception of the human hearing system (i.e. LAeq). There are large meta-analyses of outdoor environmental noise which indicate that variants of LAeq are an adequate predictor of noise annoyance.[88]
Care should be exercised when attempting to measure the maximum SPL, for three main reasons. Firstly, even if a researcher considers a maximum value to be representative of a distribution of noise levels measured in a location, it is unlikely to be generalisable. For example, if a hospital ward measurement is repeated on the next night, a different maximum value will likely occur. Secondly, there are several different ways of measuring a maximum value. For example, Lpeak means decibel value corresponding to the maximum pressure (positive or negative) arriving at the microphone,[1] while LAFmax means the maximum A-weighted SPL measured with a Fast time constant. Lpeak will typically be many decibels higher than LAFmax. Finally, the evidence relating measured maxima to human responses is not as strong as for average values like LAeq, at least for noise exposures below the range where noise-induced hearing loss is likely. This is reflected in the widespread use of LCpeak in workplace noise exposure legislation, but not in standardised methods intended to predict annoyance or disturbance from noise.
If it is desired to measure the maximum SPL, it is recommended that the device be set to ‘fast’ and A-weighted (i.e. LAFmax). This would allow comparison with WHO guidelines. LA10 (SPL exceeded for 10% of the measurement time period) and LA90 (SPL exceeded for 90% of the measurement time period) would be useful alternative metrics. They are widely used in environmental noise surveys as markers of the near-highest and background sound levels, respectively. Measured over day, night or 24-hour periods, they might also be useful measures of the noise climate on a hospital ward.
Locations. The positioning of the measuring device should be made sufficient for the “point-of-interest” for your study. For example, if a patient’s noise exposure is of interest, then a location close to the patient’s ear will be more appropriate than a central location in the room. The measuring device should be positioned in a location that is not disruptive to the day-to-day clinical activity of the hospital staff. Any contact with the measuring device during measurements should be avoided as this can affect the maximum SPL to be recorded. Compromises may be required to balance preferences for the ideal location for the point-of-interest with practical considerations. It is important to ensure that any measuring devices are at least 1 m (more if possible) away from any large reflecting surfaces (doors, walls, windows, floors, ceilings, etc.) and that they are on a stable surface, such as being mounted on a tripod. Close reflecting surfaces will increase the measured sound level, dependent on several factors which make the result less generalisable, like the size and acoustic absorption coefficient of the surface.
Documentation and reporting. It is essential to be explicit about the procedure that was followed and equipment used. Failure to document this information can cause the measurement data to be uninterpretable and meaningless. The provision of detailed information will avoid any unnecessary confusion and support the perceived accuracy of your results. The essential information to be reported is as follows:
-
(1)
The precise location of the measuring device, using a picture or diagram if necessary.
-
(2)
The time period and sampling intervals for the measurement.
-
(3)
Equipment manufacturer and model.
-
(4)
Equipment calibration process.
-
(5)
Time constant and frequency weighting (e.g. LAeq, LAFmax, LA90, etc.).
Data analysis. Researchers should exercise caution when attempting to manipulate the measurement data and avoid this where possible. Instead, all desired measurements and results should ideally come directly from the measuring instrument, and any supporting software, in order to minimise data errors. To calculate the “average” environmental noise level when this is not achievable with the instrumentation at your disposal, then the calculation of the arithmetic mean is not recommended because this does not produce an Leq. Instead, the Leq should be estimated from the measured data and the process used to do described in detail. To avoid confusion the use of the term “average” in this context should be avoided.
CONCLUSION
This rapid review of 76 studies provides a detailed overview of the equipment and approaches used in studies that have measured noise levels in hospitals. There was significant variability in the approaches used to measure environmental noise in hospitals. Few studies (14.5%) contained sufficient technical information to support the replication of the environmental noise measurement process; descriptions on important parameters such as weighting, time constant and measurement time period were missing. In hospital environments, it is recommended to use LAeq or LAFmax. The measurement equipment setting and process should be fully documented with details on device location and the time period of the recording noted. Attempts to average any measured data should be avoided where possible. In addition, most studies measured noise levels using a SLM positioned closed to a patient’s bed area in an intensive care unit. It is recommended future studies also measure noise levels in other areas of a hospital such as in-patient wards, where the impact of noise can have a negative impact on patients’ health.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This study was supported by a Collaborative Venture Funds Grant between the University of Huddersfield and the Calderdale and Huddersfield NHS Foundation Trust. The authors declare no conflict of interests.
Appendix A—Search terms
Scopus database
#1 “noise” [NDEXTERMS]
#2 “noise, occupational” [NDEXTERMS]
#3 “sound” [NDEXTERMS]
#4 “acoustics” [NDEXTERMS]
#5 “loudness perception” [NDEXTERMS]
#6 “sound intensity” [NDEXTERMS]
#7 “acoustic noise measurement” [NDEXTERMS]
#8 “acoustic measuring instruments” [NDEXTERMS]
#9 “noise measuring” [NDEXTERMS]
#10 “psychoacoustics” [NDEXTERMS]
#11 “noise spectrum” [TITLE-ABS]
#12 reverb* [TITLE-ABS]
#13 “noise level” [TITLE-ABS]
#14 “sound level” [TITLE-ABS]
#15 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14
#16 “intensive care units” [NDEXTERMS]
#17 “neonatal intensive care unit” [INDEXTERMS]
#18 “patients’ rooms” [INDEXTERMS]
#19 “hospitals” [INDEXTERMS]
#20 “critical care” [INDEXTERMS]
#21 “health facilities” [INDEXTERMS]
#22 hospital* [TITLE-ABS]
#23 “patients’ ward” [TITLE-ABS]
#24 “patients’ room” [TITLE-ABS]
#25 “emergency room” [TITLE-ABS]
#26 “emergency ward” [TITLE-ABS]
#27 “intensive care” [TITLE-ABS]
#28 “critical care” [TITLE-ABS]
#29 #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28
#30 #15 and #29
Cochrane library
#1 MeSH descriptor: [Noise] explode all trees
#2 MeSH descriptor: [Noise, Occupational] explode all trees
#3 MeSH descriptor: [Sound] explode all trees
#4 MeSH descriptor: [Acoustics] explode all trees
#5 MeSH descriptor: [Loudness Perception] explode all trees
#6 MeSH descriptor: [Psychoacoustics] explode all trees
#7 “noise spectrum” or reverb* or “noise level” or “sound level”:ti,ab,kw (Word variations have been searched)
#8 MeSH descriptor: [Intensive Care Units, Neonatal] explode all trees
#9 MeSH descriptor: [Intensive Care Units] explode all trees
#10 MeSH descriptor: [Patients’ Rooms] explode all trees
#11 MeSH descriptor: [Hospitals] explode all trees
#12 MeSH descriptor: [Critical Care] explode all trees
#13 MeSH descriptor: [Health Facilities] explode all trees
#14 hospital* or “patients’ ward” or “patients’ room” or “emergency room” or “emergency ward” or “intensive care” or “critical care”:ti,ab,kw (Word variations have been searched)
#15 #1 or #2 or #3 or #4 or #5 or #6 or #7
#16 #8 or #9 or #10 or #11 or #12 or #13 or #14
#17 #15 and #16
Pubmed database
#1 “noise” [MeSH Terms]
#2 “noise, occupational” [MeSH Terms]
#3 “sound” [MeSH Terms]
#4 “acoustics” [MeSH Terms]
#5 “loudness perception” [MeSH Terms]
#6 “psychoacoustics” [MeSH Terms]
#7 “noise spectrum” [Title/Abstract]
#8 reverb* [Title/Abstract]
#9 “noise level” [Title/Abstract]
#10 “sound level” [Title/Abstract]
#11 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10
#12 “intensive care units” [MeSH Terms]
#13 “intensive care units, neonatal” [MeSH Terms]
#14 “patients’ rooms” [MeSH Terms]
#15 “hospitals” [MeSH Terms]
#16 “critical care” [MeSH Terms]
#17 “health facilities” [MeSH Terms]
#18 hospital* [Title/Abstract]
#19 “patients’ ward” [Title/Abstract]
#20 “patients’ room” [Title/Abstract]
#21 “emergency room” [Title/Abstract]
#22 “emergency ward” [Title/Abstract]
#23 “intensive care” [Title/Abstract]
#24 “critical care” [Title/Abstract]
#25 #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24
#26 #11 and #25
REFERENCES
- 1.ISO IEC 61672-1:2013, in Electroacoustics—Sound Level Meters Part 1: Specifications. IEC; 2013. [Google Scholar]
- 2.Muzet A. Environmental noise, sleep and health. Sleep Medicine Reviews. 2007;11:135–42. doi: 10.1016/j.smrv.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Goines LHL. Noise pollution: a modern plague. Southern Medical Journal. 2007;100:287–94. doi: 10.1097/smj.0b013e3180318be5. [DOI] [PubMed] [Google Scholar]
- 4.Pope D. Decibel levels and noise generators on four medical/surgical nursing units. Journal of Clinical Nursing. 2010;19:2463–70. doi: 10.1111/j.1365-2702.2010.03263.x. [DOI] [PubMed] [Google Scholar]
- 5.Wilson CW, Stephens K, Swanson-Biearman B, LaBarba J. Improving the patient’s experience with a multimodal quiet-at-night initiative. Journal of Nursing Care Quality. 2017;32:134–40. doi: 10.1097/NCQ.0000000000000219. [DOI] [PubMed] [Google Scholar]
- 6.Katz JD. Noise in the operating room. Anesthesiology. 2014;121:898. doi: 10.1097/ALN.0000000000000319. [DOI] [PubMed] [Google Scholar]
- 7.Berglund B, et al. Guidelines for Community Noise. World Health Organisation; 1999. [Google Scholar]
- 8.Christensen M. Noise levels in a general surgical ward: a descriptive study. Journal of Clinical Nursing. 2005;14:156–64. doi: 10.1111/j.1365-2702.2004.01040.x. [DOI] [PubMed] [Google Scholar]
- 9.Dube JA, et al. Environmental noise sources and interventions to minimize them: a tale of 2 hospitals. J Nurs Care Qual. 2008;23:216–24. doi: 10.1097/01.NCQ.0000324585.68966.51. [DOI] [PubMed] [Google Scholar]
- 10.Salandin A, Arnold J, Kornadt O. Noise in an intensive care unit. Journal of the Acoustical Society of America. 2011;130:3754–60. doi: 10.1121/1.3655884. [DOI] [PubMed] [Google Scholar]
- 11.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information & Libraries Journal. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 12.Tricco A, et al. Rapid reviews to strengthen health policy and systems: a practical guide. Geneva: World Health Organisation; 2017. [Google Scholar]
- 13.Watt A, et al. Rapid reviews versus full systematic reviews: an inventory of current methods and practice in health technology assessment. Int J Technol Assess Health Care. 2008;24:133–9. doi: 10.1017/S0266462308080185. [DOI] [PubMed] [Google Scholar]
- 14.Moher DL, Tetzlaff AJ, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta Analyses: The PRISMA Statement. Annals of Internal Medicine. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 15.Elliott RM, McKinley SM, Eager D. A pilot study of sound levels in an Australian adult general intensive care unit. Noise and Health. 2010;12:26–36. doi: 10.4103/1463-1741.59997. [DOI] [PubMed] [Google Scholar]
- 16.Liu WF. The impact of a noise reduction quality improvement project upon sound levels in the open-unit-design neonatal intensive care unit. Journal of Perinatology. 2010;30:489–96. doi: 10.1038/jp.2009.188. [DOI] [PubMed] [Google Scholar]
- 17.Matook SA, et al. Variations of NICU sound by location and time of day. Neonatal network: NN. 2010;29:87–95. doi: 10.1891/0730-0832.29.2.87.. [DOI] [PubMed] [Google Scholar]
- 18.Short AE, et al. Noise levels in an Australian emergency department. Australasian Emergency Nursing Journal. 2011;14:26–31. [Google Scholar]
- 19.Memoli G, et al. Towards the acoustical characterisation of an Intensive Care Unit. Applied Acoustics. 2014;79:124–30. [Google Scholar]
- 20.Carvalhais C, et al. Is there sufficient training of health care staff on noise reduction in neonatal intensive care units? A pilot study from neonoise project. Journal of Toxicology and Environmental Health—Part A: Current Issues. 2015;78:897–903. doi: 10.1080/15287394.2015.1051204. [DOI] [PubMed] [Google Scholar]
- 21.Knauert M, et al. Comparing average levels and peak occurrence of overnight sound in the medical intensive care unit on A-weighted and C-weighted decibel scales. Journal of Critical Care. 2016;36:1–7. doi: 10.1016/j.jcrc.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luetz A, et al. Feasibility of noise reduction by a modification in ICU environment. Physiological Measurement. 2016;37:1041–55. doi: 10.1088/0967-3334/37/7/1041. [DOI] [PubMed] [Google Scholar]
- 23.Fasih-Ramandi F, Nadri H. Background noise in Iranian hospital intensive care units. Noise Control Engineering Journal. 2017;65:14–21. [Google Scholar]
- 24.Santos J, et al. Assessment and characterization of sound pressure levels in Portuguese neonatal intensive care units. Archives of Environmental and Occupational Health. 2017:1–7. doi: 10.1080/19338244.2017.1304883. [DOI] [PubMed] [Google Scholar]
- 25.McLaren E, Maxwell-Armstrong C. Noise pollution on an acute surgical ward. Annals of the Royal College of Surgeons of England. 2008;90:136–9. doi: 10.1308/003588408X261582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nathan LM, et al. Noise levels in a neonatal intensive care unit in the Cape metropole. SAJCH South African Journal of Child Health. 2008;2:50–4. [Google Scholar]
- 27.Chen HL, et al. The Influence of Neonatal Intensive Care Unit Design on Sound Level. Pediatrics and Neonatology. 2009;50:270–4. doi: 10.1016/S1875-9572(09)60076-0. [DOI] [PubMed] [Google Scholar]
- 28.Lasky RE, Williams AL. Noise and light exposures for extremely low birth weight newborns during their stay in the neonatal intensive care unit. Pediatrics. 2009;12:540–6. doi: 10.1542/peds.2007-3418. [DOI] [PubMed] [Google Scholar]
- 29.Richardson A, et al. Development and implementation of a noise reduction intervention programme: a pre- and postaudit of three hospital wards. Journal of Clinical Nursing. 2009;18:3316–24. doi: 10.1111/j.1365-2702.2009.02897.x. [DOI] [PubMed] [Google Scholar]
- 30.Williams AL, et al. Intensive care noise and mean arterial blood pressure in extremely low-birth-weight neonates. American Journal of Perinatology. 2009;26:323–9. doi: 10.1055/s-0028-1104741. [DOI] [PubMed] [Google Scholar]
- 31.Hsu SM, et al. Associations of exposure to noise with physiological and psychological outcomes among post-cardiac surgery patients in ICUs. Clinics. 2010;65:985–9. doi: 10.1590/S1807-59322010001000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hu RF, et al. Effects of earplugs and eye masks on nocturnal sleep, melatonin and cortisol in a simulated intensive care unit environment. Crit Care. 2010;14:R66. doi: 10.1186/cc8965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lawson N, et al. Sound intensity and noise evaluation in a critical care unit. American Journal of Critical Care. 2010;19:e88–e98. doi: 10.4037/ajcc2010180. [DOI] [PubMed] [Google Scholar]
- 34.Gladd DK, Saunders GH. Ambient noise levels in the chemotherapy clinic. Noise and Health. 2011;13:444–51. doi: 10.4103/1463-1741.90322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johansson L, et al. The sound environment in an ICU patient room–a content analysis of sound levels and patient experiences. Intensive Crit Care Nurs. 2012;28:269–79. doi: 10.1016/j.iccn.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 36.Liu WF. Comparing sound measurements in the single-family room with open-unit design neonatal intensive care unit: The impact of equipment noise. Journal of Perinatology. 2012;32:368–73. doi: 10.1038/jp.2011.103. [DOI] [PubMed] [Google Scholar]
- 37.Xie H, Kang J. The acoustic environment of intensive care wards based on long period nocturnal measurements. Noise and Health. 2012;14:230–6. doi: 10.4103/1463-1741.102960. [DOI] [PubMed] [Google Scholar]
- 38.Zamberlan-Amorim NE, et al. Impact of a participatory program to reduce noise in a neonatal unit. Revista Latino-Americana de Enfermagem. 2012;20:109–16. doi: 10.1590/s0104-11692012000100015. [DOI] [PubMed] [Google Scholar]
- 39.Cordova AC, et al. Noise levels in a burn intensive care unit. Burns. 2013;39:44–8. doi: 10.1016/j.burns.2012.02.033. [DOI] [PubMed] [Google Scholar]
- 40.Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Critical Care. 2013:17. doi: 10.1186/cc12870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ginsberg SH, et al. Noise levels in modern operating rooms during surgery. Journal of Cardiothoracic and Vascular Anesthesia. 2013;27:528–30. doi: 10.1053/j.jvca.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 42.Fortes-Garrido JC, et al. The characterization of noise levels in a neonatal intensive care unit and the implications for noise management. Journal of Environmental Health Science and Engineering. 2014:12. [Google Scholar]
- 43.Kol E, Aydin P, Dursun O. The effectiveness of environmental strategies on noise reduction in a pediatric intensive care unit: Creation of single-patient bedrooms and reducing noise sources. Journal for Specialists in Pediatric Nursing. 2015;20:210–7. doi: 10.1111/jspn.12116. [DOI] [PubMed] [Google Scholar]
- 44.Kol E, et al. The effectiveness of measures aimed at noise reduction in an intensive care unit. Workplace Health Saf. 2015;63:539–45. doi: 10.1177/2165079915607494. [DOI] [PubMed] [Google Scholar]
- 45.Hu RF, et al. An investigation of light and sound levels on intensive care units in China. Australian Critical Care. 2016;29:62–7. doi: 10.1016/j.aucc.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 46.Calikusu Incekar M, Balci S. The effect of training on noise reduction in neonatal intensive care units. Journal for Specialists in Pediatric Nursing. 2017:22. doi: 10.1111/jspn.12181. [DOI] [PubMed] [Google Scholar]
- 47.Giv MD, et al. Evaluation of noise pollution level in the operating rooms of hospitals: A study in Iran. Interventional Medicine and Applied Science. 2017;9:61–6. doi: 10.1556/1646.9.2017.2.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Parra J, et al. Sound levels in a neonatal intensive care unit significantly exceeded recommendations, especially inside incubators. Acta Paediatrica, International Journal of Paediatrics. 2017;106:1909–14. doi: 10.1111/apa.13906. [DOI] [PubMed] [Google Scholar]
- 49.Voigt LP, et al. Monitoring sound and light continuously in an intensive care unit patient room: A pilot study. Journal of Critical Care. 2017;39:36–9. doi: 10.1016/j.jcrc.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 50.Akansel N, Kaymakçi S. Effects of intensive care unit noise on patients: A study on coronary artery bypass graft surgery patients. Journal of Clinical Nursing. 2008;17:1581–90. doi: 10.1111/j.1365-2702.2007.02144.x. [DOI] [PubMed] [Google Scholar]
- 51.Darcy AE, Hancock LE, Ware EJ. A descriptive study of noise in the neonatal intensive care unit: Ambient levels and perceptions of contributing factors. Advances in Neonatal Care. 2008;8:165–75. doi: 10.1097/01.ANC.0000324341.24841.6e. [DOI] [PubMed] [Google Scholar]
- 52.Livera MD, et al. Spectral analysis of noise in the neonatal intensive care unit. Indian Journal of Pediatrics. 2008;75:217–22. doi: 10.1007/s12098-008-0048-z. [DOI] [PubMed] [Google Scholar]
- 53.Taylor-Ford R, et al. Effect of a noise reduction program on a medical- surgical unit. Clinical Nursing Research. 2008;17:74–88. doi: 10.1177/1054773807312769. [DOI] [PubMed] [Google Scholar]
- 54.Tsara V, et al. Noise levels in Greek hospitals. Noise and Health. 2008;10:110–2. doi: 10.4103/1463-1741.44350. [DOI] [PubMed] [Google Scholar]
- 55.Vinodhkumaradithyaa A, et al. Noise levels in a tertiary care hospital. Noise Health. 2008;10:11–3. doi: 10.4103/1463-1741.39003. [DOI] [PubMed] [Google Scholar]
- 56.Altuncu E, et al. Noise levels in neonatal intensive care unit and use of sound absorbing panel in the isolette. International Journal of Pediatric Otorhinolaryngology. 2009;73:951–3. doi: 10.1016/j.ijporl.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 57.Macedo ISC, et al. Noise assessment in intensive care units. Brazilian Journal of Otorhinolaryngology. 2009:75. doi: 10.1016/S1808-8694(15)30547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ramesh A, et al. Efficacy of a low cost protocol in reducing noise levels in the neonatal intensive care unit. Indian J Pediatr. 2009;76:475–8. doi: 10.1007/s12098-009-0066-5. [DOI] [PubMed] [Google Scholar]
- 59.Dennis CM, et al. Benefits of quiet time for neuro-intensive care patients. J Neurosci Nurs. 2010;42:217–24. doi: 10.1097/jnn.0b013e3181e26c20. [DOI] [PubMed] [Google Scholar]
- 60.Juang DF, et al. Noise pollution and its effects on medical care workers and patients in hospitals. International Journal of Environmental Science and Technology. 2010;7:705–16. [Google Scholar]
- 61.Merilainen M, Kyngas H, Ala-Kokko T. 24-hour intensive care: an observational study of an environment and events. Intensive Crit Care Nurs. 2010;26:246–53. doi: 10.1016/j.iccn.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 62.Khademi G, et al. Noise pollution in intensive care units and emergency wards. Iranian Journal of Otorhinolaryngology. 2011;23:141–8. [PMC free article] [PubMed] [Google Scholar]
- 63.Kurmann A, et al. Adverse effect of noise in the operating theatre on surgical-site infection. Br J Surg. 2011;98:1021–5. doi: 10.1002/bjs.7496. [DOI] [PubMed] [Google Scholar]
- 64.Li SY, et al. Efficacy of controlling night-time noise and activities to improve patients’ sleep quality in a surgical intensive care unit. Journal of Clinical Nursing. 2011;20:396–407. doi: 10.1111/j.1365-2702.2010.03507.x. [DOI] [PubMed] [Google Scholar]
- 65.Linder LA, Christian BJ. Characteristics of the nighttime hospital bedside care environment (sound, light, and temperature) for children with cancer. Cancer Nursing. 2011;34:176–84. doi: 10.1097/NCC.0b013e3181fc52d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Olivera M, et al. Acoustic pollution in hospital environments. Journal of Physics: Conference Series. 2011:332. [Google Scholar]
- 67.Van Enk RA, Steinberg F. Comparison of private room with multiple-bed ward neonatal intensive care unit. HERD. 2011;5:52–63. doi: 10.1177/193758671100500105. [DOI] [PubMed] [Google Scholar]
- 68.Elser HE, et al. The effects of environmental noise and infant position on cerebral oxygenation. Advances in Neonatal Care. 2012;12:S18–S27. doi: 10.1097/ANC.0b013e31826853fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guérin A, Leroux T, Bussières JF. Pre-post pilot study of noise levels at a university hospital center pharmacy department. Journal of Pharmacy Practice. 2013;26:448–53. doi: 10.1177/0897190012468450. [DOI] [PubMed] [Google Scholar]
- 70.Padmakumar AD, et al. Evaluation of noise levels in intensive care units in two large teaching hospitals − A prospective observational study. Journal of the Intensive Care Society. 2013;14:205–10. [Google Scholar]
- 71.Tegnestedt C, et al. Levels and sources of sound in the intensive care unit − An observational study of three room types. Acta Anaesthesiologica Scandinavica. 2013;57:1041–50. doi: 10.1111/aas.12138. [DOI] [PubMed] [Google Scholar]
- 72.Verhaert N, et al. Noise exposure of care providers during otosurgical procedures. B-ent. 2013;9:3–8. [PubMed] [Google Scholar]
- 73.Wang Z, et al. Role of a service corridor in ICU noise control, staff stress, and staff satisfaction: Environmental research of an academic medical center. Health Environments Research and Design Journal. 2013;6:80–94. doi: 10.1177/193758671300600307. [DOI] [PubMed] [Google Scholar]
- 74.Bano M, et al. The influence of environmental factors on sleep quality in hospitalized medical patients. Frontiers in Neurology. 2014:5. doi: 10.3389/fneur.2014.00267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Filus W, De Lacerda ABM, Albizu E. Ambient noise in emergency rooms and its health hazards. International Archives of Otorhinolaryngology. 2014;19:205–9. doi: 10.1055/s-0034-1387165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang D, et al. Examining the effects of a targeted noise reduction program in a neonatal intensive care unit. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2014;99:F203–F208. doi: 10.1136/archdischild-2013-304928. [DOI] [PubMed] [Google Scholar]
- 77.Wang D, et al. Reduction of noise in the neonatal intensive care unit using sound-activated noise meters. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2014;99:F515–F516. doi: 10.1136/archdischild-2014-306490. [DOI] [PubMed] [Google Scholar]
- 78.Hill JN, LaVela SL. Noise levels in patient rooms and at nursing stations at three VA medical centers. Health Environments Research and Design Journal. 2015;9:54–63. doi: 10.1177/1937586715592635. [DOI] [PubMed] [Google Scholar]
- 79.Watson J, et al. Impact of noise on nurses in pediatric intensive care units. American Journal of Critical Care. 2015;24:377–84. doi: 10.4037/ajcc2015260. [DOI] [PubMed] [Google Scholar]
- 80.Yelden K, et al. A rehabilitation unit at night: Environmental characteristics of patient rooms. Disability and Rehabilitation. 2015;37:91–6. doi: 10.3109/09638288.2014.906662. [DOI] [PubMed] [Google Scholar]
- 81.Chow VY, Shellhaas RA. Acoustic environment profile of the neonatal intensive care unit: High ambient noise and limited language exposure. Journal of Neonatal Nursing. 2016;22:159–62. [Google Scholar]
- 82.Daraiseh NM, et al. Noise exposure on pediatric inpatient units. Journal of Nursing Administration. 2016;46:468–76. doi: 10.1097/NNA.0000000000000377. [DOI] [PubMed] [Google Scholar]
- 83.Kramer B, Joshi P, Heard C. Noise pollution levels in the pediatric intensive care unit. Journal of Critical Care. 2016;36:111–5. doi: 10.1016/j.jcrc.2016.06.029. [DOI] [PubMed] [Google Scholar]
- 84.Delaney LJ, et al. The nocturnal acoustical intensity of the intensive care environment: An observational study. Journal of Intensive Care. 2017;5((1)) doi: 10.1186/s40560-017-0237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Elbaz M, et al. Sound level intensity severely disrupts sleep in ventilated ICU patients throughout a 24-h period: a preliminary 24-h study of sleep stages and associated sound levels. Annals of Intensive Care. 2017:7. doi: 10.1186/s13613-017-0248-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ramm K, et al. A comparison of sound levels in open plan versus pods in a neonatal intensive care unit. Health Environments Research and Design Journal. 2017;10:30–9. doi: 10.1177/1937586716668636. [DOI] [PubMed] [Google Scholar]
- 87.White BL, Zomorodi M. Perceived and actual noise levels in critical care units. Intensive and Critical Care Nursing. 2017;38:18–23. doi: 10.1016/j.iccn.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 88.Miedema H, Oudshoorn C. Annoyance from transportation noise: relationships with exposure metrics DNL and DENL and their confidence intervals. Environmental health perspectives. 2001;109:409–16. doi: 10.1289/ehp.01109409. [DOI] [PMC free article] [PubMed] [Google Scholar]


