Abstract
Background
Oncological patients have several additional risk factors for developing a cardiac implantable electronic device (CIED)–related infection. Therefore, we evaluated the clinical impact of our comprehensive bundle approach that includes the novel minocycline and rifampin antimicrobial mesh (TYRX) for the prevention of CIED infections in patients living with cancer.
Methods
We retrospectively reviewed all consecutive patients who had a CIED placement at our institution during 2012–2017 who received preoperative vancomycin, intraoperative pocket irrigation with bacitracin and polymyxin B, plus TYRX antimicrobial mesh, followed by postoperative oral minocycline.
Results
A total of 154 patients had a CIED, with 97 permanent pacemakers (PPMs), 23 implantable cardioverter defibrillators (ICDs), and 34 cardiac resynchronization therapy (CRT) devices. An underlying solid cancer was present in 62% of patients, while 38% had a hematologic malignancy. Apart from a higher proportion of surgical interventions in the PPM group than in the ICD and CRT groups (P = .007), no other oncologic variables were statistically significantly different between groups. Despite an extensive median follow-up period (interquartile range) of 21.9 (6.7–33.8) months, 16 patients (10%) had a mechanical complication, while only 2 patients (1.3%) developed a CIED infection, requiring the device to be explanted.
Conclusions
Our comprehensive prophylactic bundle approach using TYRX antimicrobial mesh in an oncologic population at high risk for infections was revealed upon extensive follow-up to be both safe and effective in maintaining the rate of CIED infection at 1.3%, well within published averages in the broader population of CIED recipients.
Keywords: antimicrobials, bundle, cancer, cardiac implantable electronic devices, envelope, infection, prevention
The indications for cardiac implantable electronic devices (CIEDs) have greatly increased over the past few decades. In the United States, more than 100 000 implantable cardioverter defibrillators (ICDs) and 300 000 permanent pacemakers (PPMs) are implanted every year [1]. The rate of infection of these CIEDs has been estimated at 1% to 4% [2, 3]. Infection complications of these devices are a serious clinical problem associated with increased morbidity and mortality [4]. Furthermore, the Inpatient Prospective Payment System and Fiscal Year 2013 Rates–Final Rule published by the Centers for Medicare and Medicaid Services has established CIED-related infections as a hospital-acquired condition, not eligible for financial reimbursement. Therefore, the need to prevent CIEDs from becoming infected has continued to grow.
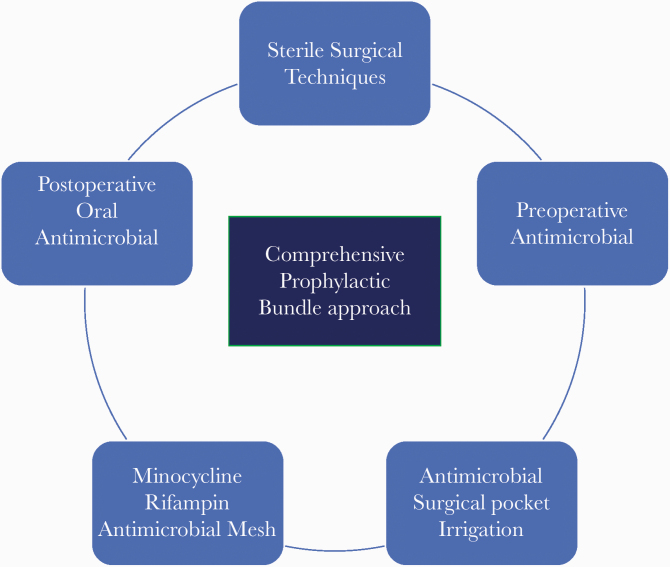
The use of a sterile surgical technique and appropriate timing of perioperative antimicrobials have been the only long-standing interventions that have consistently been demonstrated in randomized controlled studies to reduce the rate of postoperative CIED infections [5–8]. Most recently, the Worldwide Randomized Antibiotic Envelope Infection Prevention Trial (WRAP-IT) has demonstrated the safety and effectiveness of the TYRX minocycline and rifampin multifilament mesh envelope (TYRX; Medtronic, Dublin, Ireland), which elutes antibiotics locally within the generator surgical pocket for a minimum of 7 days as an adjunct intervention to prevent CIED-related infections in high-risk patients [8, 9]. However, no studies have evaluated the effectiveness of the use of prophylactic antimicrobials in solely immunocompromised patients living with cancer, a specific population usually excluded from randomized studies. Cancer patients have several modifiable and nonmodifiable risk factors that place them at a higher risk for developing an implant-related infection. Herein, we evaluated patients’ traditional and cancer-specific risk factors for CIED-related infections, as well as the safety and effectiveness of CIED placement in patients with cancer using our comprehensive prophylactic bundle approach that includes the TYRX antimicrobial mesh (Figure 1).
Figure 1. .
Comprehensive prophylactic bundle approach.
METHODS
Hospital Setting and Study Population
We retrospectively reviewed the charts of all consecutive patients who underwent CIED placement during 2012 through 2017 at the University of Texas MD Anderson Cancer Center (Houston, TX, USA). All patients who received a PPM, an ICD, or a cardiac resynchronization therapy (CRT) device were included, and because each device type carries an incremental risk for infection, the recipient of each device type was analyzed independently. We collected data on patient demographics, baseline comorbidities, medication use, cancer characteristics, cancer treatments, and timing of CIED placement. We also documented the use of our comprehensive antimicrobial bundle approach, which includes preoperative intravenous vancomycin and intraoperative surgical pocket irrigation with polymyxin B and bacitracin, followed by placement of the TYRX antimicrobial mesh and postoperative oral minocycline 100 mg twice daily for 5 days. The use of antimicrobials for all patients was confirmed via electronic chart review as well as inpatient and outpatient pharmacy records. Additionally, we documented the traditional modifiable and nonmodifiable risk factors for CIED infections and the factors unique to patients undergoing active cancer therapy that further increase the risk for infection, including long-term intravenous catheter placement, neutropenia, thrombocytopenia, and non-CIED-related local and systemic infections. Furthermore, we gathered information on noninfectious complications, the time and type of CIED infection, recovered pathogens, and medical and surgical approaches. All patients were followed up until the last visit at our institution or until death. The study was approved by the institutional review board, and written consent was waived due to the retrospective nature of the study.
Definitions
CIED infections were categorized as follows: (a) superficial incisional infection affecting the skin or soft tissue without communication to the pocket; (b) pocket or generator infection with localized swelling, erythema, warmth, pain, purulent discharge, sinus formation, or exposure of hardware components such as the generator or proximal leads [8]; or (c) definite or possible CIED-related infective endocarditis, as established in the Novel 2019 International CIED Infection Criteria [10, 11].
Statistical Analysis
Categorical variables were compared between groups using the chi-square test or Fisher exact test as appropriate. Continuous variables were compared between groups using the Kruskal-Wallis test (for 3-group comparisons) and the Wilcoxon rank sum test (for 2-group comparisons). If a significant result (P < .05) was detected for a test that compared 3 groups, then pairwise comparisons were performed with α levels adjusted using Holm’s sequential Bonferroni adjustment to control for type I error. All tests were 2-sided with a significance level of .05, except for pairwise comparisons with α adjustment. The statistical analyses were performed using SAS, version 9.3 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Patients’ Baseline Characteristics
We included 154 patients who had a CIED placement (Table 1). A total of 97 (63%) patients had a PPM, 23 (15%) had an ICD, and 34 (22%) a CRT. The median age of our studied population (interquartile range [IQR]) was 73 (30–93) years. Approximately two-thirds were White (71%), and 63% were male. The main comorbid conditions were hypertension (73%), hyperlipidemia (56%), coronary artery disease (46%), and myocardial infarction (19%), with a median ejection fraction (IQR) of 55% (33%–61%). Additionally, 30% of patients had diabetes mellitus, 21% were receiving oral diabetic medicines, and 9% required insulin. The median body mass index (IQR) was 27.4 (24.0–31.6). The cardiac surgical history of our population included prior CIED placement (34%), coronary artery bypass graft (16%), and valve replacement (6%). Furthermore, several patients were receiving a medication that placed them at risk for a CIED-related infection, including antiplatelet drugs (53%), anticoagulant drugs (36%), and systemic steroids (10%). As expected because of the indications for CIED placement, in general the ICD and CRT groups had significantly more cardiac comorbidities than the PPM group (Supplementary Table 1).
Table 1. .
Patients’ Baseline Characteristics at Time of CIED Placement
| Variables | Total (n = 154) | PPM (n = 97) | ICD (n = 23) | CRT (n = 34) | P |
|---|---|---|---|---|---|
| Age, median (range), y | 73 (30–93) | 74 (30–93) | 63 (33–88) | 72 (46–84) | .004 |
| Sex, male, No. (%) | 97 (63) | 59 (61) | 14 (61) | 24 (71) | .58 |
| Ethnicity, No. (%) | .029 | ||||
| White | 110 (71) | 72 (74) | 11 (48) | 27 (79) | |
| Black | 28 (18) | 14 (14) | 10 (43) | 4 (12) | |
| Hispanic | 9 (6) | 5 (5) | 1 (4) | 3 (9) | |
| Asian | 7 (5) | 6 (6) | 1 (4) | 0 (0) | |
| Comorbidities | |||||
| Hypertension, No. (%) | 112 (73) | 70 (72) | 17 (74) | 25 (74) | .99 |
| Hyperlipidemia, No. (%) | 86 (56) | 50 (52) | 12 (52) | 24 (71) | .15 |
| Coronary artery disease, No. (%) | 71 (46) | 37 (38) | 14 (61) | 20 (59) | .035 |
| Diabetes, No. (%) | 46 (30) | 23 (24) | 7 (30) | 16 (47) | .038 |
| Myocardial infarction, No. (%) | 29 (19) | 11 (11) | 8 (35) | 10 (29) | .007 |
| COPD, No. (%) | 21 (14) | 10 (10) | 4 (17) | 7 (21) | .26 |
| Ejection fraction, median (IQR), % | 55 (33–61) | 60 (55–65) | 30 (25–40) | 30 (25–35) | <.0001 |
| BMI, median (range), kg/m2 | 27.4 (24.0–31.6) | 26.5 (22.8–31.0) | 26.9 (25.2–32.2) | 28.7 (27.7–32.8) | .042 |
| Active alcohol use, No. (%) | 11 (7) | 8 (8) | 1 (4) | 2 (6) | >.99 |
| Active smoking, No. (%) | 10 (6) | 8 (8) | 0 (0) | 2 (6) | .50 |
| Cardiac surgical history, No. (%) | |||||
| CABG | 24 (16) | 9 (9) | 7 (30) | 8 (24) | .015 |
| Valve replacement | 9 (6) | 4 (4) | 1 (4) | 4 (12) | .28 |
| Biological | 8 (5) | 4 (4) | 1 (4) | 3 (9) | .56 |
| Mechanical | 1 (1) | 0 (0) | 0 (0) | 1 (3) | .37 |
| History of prior CIEDs, No. (%) | 52 (34) | 30 (31) | 6 (26) | 16 (47) | .16 |
| Baseline medications, No. (%) | |||||
| Antiplatelets | 81 (53) | 45 (46) | 13 (57) | 23 (68) | .09 |
| Anticoagulation | 55 (36) | 34 (35) | 8 (35) | 13 (38) | .94 |
| Oral diabetic medicines | 32 (21) | 17 (18) | 5 (22) | 10 (29) | .34 |
| Insulin | 16 (10) | 4 (4) | 3 (13) | 9 (26) | .001 |
| Systemic steroids | 15 (10) | 12 (12) | 2 (9) | 1 (3) | .32 |
| Laboratory values, median (IQR) | |||||
| Absolute neutrophil count, 1000 cells/μL | 4.29 (2.83–5.57) | 4.21 (2.78–5.60) | 3.75 (2.57–4.57) | 4.50 (3.09–6.20) | .46 |
| Absolute lymphocyte count, 1000 cells/μL | 1.18 (0.73–1.75) | 1.16 (0.74–1.53) | 1.00 (0.52–1.63) | 1.51 (0.83–2.26) | .13 |
| Hemoglobin, g/dL | 11.4 (10.2–12.7) | 11.2 (10.1–12.2) | 11.9 (11.0–13.2) | 11.9 (10.4–13.6) | .049 |
| Platelets, cells/μL | 165 (118–224) | 166 (118–219) | 170 (119–227) | 157 (116–220) | .89 |
| Creatinine clearance, mL/min | 70 (55–86) | 70 (55–85) | 71 (66–100) | 65 (48–76) | .06 |
| Total follow-up, median (IQR), mo | 21.9 (6.7–33.8) | 19.6 (6.0–31.0) | 22.6 (6.0–42.3) | 26.8 (12.7–41.9) | .14 |
Abbreviations: BMI, body mass index; CABG, coronary artery bypass graft; CIED, cardiac implantable electronic devices; COPD, chronic obstructive pulmonary disease; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; IQR, interquartile range; PPM, permanent pacemaker.
Of interest, at the time of CIED placement, although many patients were on active oncologic care (64%), as we intentionally did not implant in the higher-risk patients until counts recovered, none were neutropenic or severely thrombocytopenic. Furthermore, during CIED placement and under sterile surgical conditions, all 154 patients received our comprehensive antimicrobial bundle, which includes preoperative systemic antibiotics, intraoperative antimicrobial pocket irrigation, TYRX antimicrobial mesh, and immediate postoperative oral antibiotics. First-generation, nonresorbable TYRX antimicrobial mesh was placed in 15 patients (10%), while second-generation, resorbable TYRX mesh was placed in the remaining 139 patients (90%), with a similar distribution among all 3 CIED groups (P = .22). As patients were either on active oncologic care or cancer survivors, all patients were followed extensively for a median (IQR) of 21.9 (6.7–33.8) months.
Patients’ Oncologic and Treatment Characteristics
All patients included in our study had an underlying cancer diagnosis. A total of 96 patients (62%) had an underlying solid cancer diagnosis, while 58 patients (38%) had a hematologic malignancy (Table 2). Only 9 of the 29 patients in the latter group who were on active oncological therapy, due to the underlying risk for infection, were on prophylactic antimicrobials at the time of CIED placement (5 patients were on levofloxacin, 1 on Bactrim, and 1 on cefpodoxime). Of note, up to 1 year before CIED placement, 48% had received chemotherapy, 54% had received radiation therapy, 12% had received immunotherapy, and 8% had received a hematopoietic stem cell transplant (5% autologous and 3% allogeneic). Up to 1 year after CIED placement, 34% received chemotherapy, 14% received radiation therapy, 9% received surgery, 9% received immunotherapy, and 3% received a hematopoietic stem cell transplant (2% autologous and 1% allogeneic). Furthermore, at the time of CIED placement, 32% had central venous access: 12% had a peripherally inserted central catheter, 10% had a port-a-cath, 8% had a central venous catheter, and 2% had a hemodialysis catheter. Apart from a higher proportion of surgical interventions in the PPM group than in the ICD and CRT groups (P = .007), none of the remaining oncologic variables significantly differed between groups (P > .05).
Table 2. .
Patients’ Oncologic and Treatment Characteristics
| Variables | Total (n = 154) | PPM (n = 97) | ICD (n = 23) | CRT (n = 34) | P |
|---|---|---|---|---|---|
| Cancer type, No. (%) | .67 | ||||
| Solid | 96 (62) | 63 (65) | 13 (57) | 20 (59) | |
| Hematologic | 58 (38) | 34 (35) | 10 (43) | 14 (41) | |
| Cancer on active therapy at time of CIED placement, No. (%) | 99 (64) | 68 (70) | 12 (52) | 19 (56) | .14 |
| Cancer therapy received within 1 y before CIED placement, No. (%) | |||||
| Chemotherapy | 74 (48) | 45 (46) | 13 (57) | 16 (47) | .68 |
| Radiation therapy | 83 (54) | 48 (49) | 15 (65) | 20 (59) | .32 |
| Immunotherapy | 19 (12) | 11 (11) | 4 (17) | 4 (12) | .68 |
| HSCT | 13 (8) | 8 (8) | 1 (4) | 4 (12) | .70 |
| Type of HSCT | .67 | ||||
| Autologous | 8 (5) | 5 (5) | 0 (0) | 3 (9) | |
| Allogeneic | 5 (3) | 3 (3) | 1 (4) | 1 (3) | |
| Cancer therapy received within 1 y after CIED placement, No. (%) | |||||
| Chemotherapy | 52 (34) | 33 (34) | 6 (26) | 13 (38) | .63 |
| Radiation therapy | 21 (14) | 17 (18) | 2 (9) | 2 (6) | .22 |
| Immunotherapy | 14 (9) | 10 (10) | 0 (0) | 4 (12) | .25 |
| Surgery | 14 (9) | 14 (14) | 0 (0) | 0 (0) | .007 |
| HSCT | 5 (3) | 3 (3) | 2 (9) | 0 (0) | .17 |
| Type of HSCT | .052 | ||||
| Autologous | 3 (2) | 3 (3) | 0 (0) | 0 (0) | |
| Allogeneic | 2 (1) | 0 (0) | 2 (9) | 0 (0) | |
| Central IV access, at time of CIED placement, No. (%) | .36 | ||||
| None | 104 (68) | 64 (66) | 16 (70) | 24 (71) | |
| PICC | 18 (12) | 13 (13) | 1 (4) | 4 (12) | |
| Port-a-cath | 16 (10) | 9 (9) | 2 (9) | 5 (15) | |
| CVC | 13 (8) | 9 (9) | 4 (17) | 0 (0) | |
| Hemodialysis catheter | 3 (2) | 2 (2) | 0 (0) | 1 (3) |
Abbreviations: CIED, cardiac implantable electronic devices; CRT, cardiac resynchronization therapy; CVC, central venous catheter; HSCT, hematopoietic stem cell transplantation; ICD, implantable cardioverter defibrillator; IV, intravenous; PICC, peripheral inserted central catheter; PPM, permanent pacemaker.
CIED and TYRX Mechanical Complications
Placement of the CIED plus TYRX mesh had an overall complication rate of 10% (Table 3). The most common complications included small generator pocket hematoma that did not need require any further intervention (6 cases; 4%), lead dislodgement or malfunction (4 cases; 3%), and deep venous thrombosis (3 cases; 2%). The severe complications that occurred were ventricular perforation (2 cases; 1%) and pneumothorax (1 case; 1%). The rates and types of mechanical complications were similar between the 3 CIED groups (P > .86).
Table 3. .
CIED Infections and Mechanical Complications
| Variables | Total (n = 154) | PPM (n = 97) | ICD (n = 23) | CRT (n = 34) | P |
|---|---|---|---|---|---|
| History of CIED infections before index placement, No. (%) | .09 | ||||
| None | 147 (95) | 95 (98) | 22 (96) | 30 (88) | |
| 2 (1) | 1 (1) | 0 (0) | 1 (3) | ||
| Lead | 2 (1) | 0 (0) | 0 (0) | 2 (6) | |
| Endocarditis | 3 (2) | 1 (1) | 1 (4) | 1 (3) | |
| Non-CIED infections within 1 y after CIED placement, No. (%) | 82 (53) | 49 (51) | 14 (61) | 19 (56) | .63 |
| UTI/urosepsis | 46 (30) | 28 (29) | 6 (26) | 12 (35) | .71 |
| Pneumonia | 29 (19) | 17 (18) | 5 (22) | 7 (21) | .86 |
| URI/bronchitis | 14 (9) | 6 (6) | 3 (13) | 5 (15) | .21 |
| SSTI | 13 (8) | 9 (9) | 2 (9) | 2 (6) | .92 |
| Bacteremia | 12 (8) | 6 (6) | 3 (13) | 3 (9) | .46 |
| Dental abscess | 1 (1) | 1 (1) | 0 (0) | 0 (0) | >.99 |
| Septic arthritis | 1 (1) | 0 (0) | 0 (0) | 1 (3) | .37 |
| CIED infection, index placement, No. (%) | .6 | ||||
| Pocket infection | 1 (1) | 0 (0) | 0 (0) | 1 (3) | |
| Lead/endocarditis | 1 (1) | 1 (1) | 0 (0) | 0 (0) | |
| CIED mechanical complications, index placement, No. (%) | .91 | ||||
| Generator pocket hematoma | 6 (4) | 4 (4) | 1 (4) | 1 (3) | |
| Lead dislodgment/malfunction | 4 (3) | 2 (2) | 1 (4) | 1 (3) | |
| Local deep venous thrombosis | 3 (2) | 1 (1) | 1 (4) | 1 (3) | |
| Ventricular perforation | 2 (1) | 2 (2) | 0 (0) | 0 (0) | |
| Pneumothorax | 1 (1) | 1 (1) | 0 (0) | 0 (0) |
Abbreviations: CIED, cardiac implantable electronic devices; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; PPM, permanent pacemaker; SSTI, skin soft tissue infection; URI, upper respiratory tract infection; UTI, urinary tract infection.
CIED and TYRX Infection Complications
Our study population had 7 patients (5%) with a history of a prior CIED-related infection (Table 3). After CIED placement and up to 1 year after the index surgical intervention, our population had several non-CIED-related infections, which increased the risk for transient bacteremia and secondary infection of the newly placed cardiac device. The most common infections encountered were urinary tract infections and urosepsis (46 cases; 30%), pneumonia (29 cases; 19%), upper respiratory tract infection plus bronchitis (14 cases; 9%), skin and soft tissue infection (13 cases; 8%), and bacteremia (12 cases; 8%). Nonetheless, infection of the newly placed CIED occurred in only 2 patients (1.3%); 1 patient developed PPM cardiac lead–related endocarditis, and 1 patient with a CRT developed a local pocket site infection. Both patients had multiple risk factors for infection, including 2 cardiac leads, being on anticoagulants, having a history of a CIED device, and on active oncologic therapy before CIED placement. The first patient with Hodgkin lymphoma was in remission and not receiving oncologic therapy after CIED placement, while the second patient with breast cancer was continued on active oncologic therapy. The underlying demographics and risk factors for CIED infection in these 2 patients can be found in Table 4. Of these 2 patients, the first patient developed septic shock and bacteremia from Streptococcus pneumoniae and had a high likelihood of secondary infection of the CIED, while the source of infection in the other patient remained unknown. Additionally, both patients were treated with an appropriate antimicrobial course and eventually had their CIEDs removed.
Table 4. .
Confirmed Cases of CIED Infection
| Age, Race/Sex | Device | Arrhythmia and EF | Risk Factors | Cancer | Oncologic Therapy (Pre-CIED) | Oncologic Therapy (Post-CIED) | Laboratory Values (ANC/platelets) | IV Access | Antimicrobials to Prevent CIED Infection | Non-CIED Infection | CIED Infection and Management (Time From CIED Placement) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 48 y, WM | PPM | Atrial flutter, third-degree heart block, 50% | 2 leads, oral antiplatelets, anticoagulation, PPM for 5 y prior, and CIED endocarditis | Hodgkin lymphoma | Mantle cell radiation, chemotherapy, splenectomy, and autologous HSCT | None | 5180 cells/μl352 cells/μl | PICC | (a) Preoperative vancomycin, (b) polymyxin B plus bacitracin pocket irrigation, (c) resorbable TYRX, (d) postoperative minocycline | Septic shock, pneumonia, and pneumococcal bacteremia | Lead infection (pneumococcus) status post–PPM exchange and 6 wk of antimicrobials (118 d) |
| 74 y, WF | CRT-D | Atrial fibrillation, 25% (chemotherapy-induced cardiomyopathy) | HTN, CAD, 3 leads, oral anticoagulation, ICD for 2 y prior | Invasive ductal breast carcinoma | Bilateral mastectomy, chest radiation, chemotherapy, and hormonal therapy | Chest radiation and hormonal therapy | 800 cells/μl224 cells/μl | None | (a) Preoperative vancomycin, (b) polymyxin B plus bacitracin pocket irrigation, (c) resorbable TYRX, (d) postoperative minocycline | Recurrent urinary tract infections | Generator infection (culture negative) status post CRT-D exchange and 2 weeks of antimicrobials (1174d) |
Abbreviations: ANC, absolute neutrophil count; CAD, coronary artery disease, CRT-D, cardiac resynchronization therapy defibrillator; EF, ejection fraction; HSCT, hematopoietic stem cell transplantation; HTN, hypertension; ICD, implantable cardio defibrillator; IV, intravenous; PICC, peripherally inserted central catheter; PPM, permanent pacemaker; W, White.
DISCUSSION
To the best of our knowledge, this is the first study with an extended follow-up period that solely included patients with cancer and proceeding with CIED placement, which is a unique population at increased risk for recurrent local and systemic infections. Fortunately, our standard antisepsis bundle and infection control protocols, along with the adjuvant use of the TYRX antimicrobial envelope, were demonstrated to be both safe and effective in maintaining the rate of CIED infection at 1.3%, well within published averages in the broader population of all CIED recipients [12].
Risk factors for CIED infection have been categorized as (a) patient-related, (b) procedure-related, and (c) device-related factors [8]. The patient-related risk factors include renal insufficiency, chronic obstructive pulmonary disease, diabetes mellitus, coronary artery disease, myocardial infarction, congestive heart failure, oral anticoagulant antiplatelets, and corticosteroids, as well as fever and/or leukocytosis before implantation and history of device infection [13]. The procedure-related risk factors include temporary pacing procedure duration, device upgrade, revision and replacement, lead repositioning, postoperative hematoma, and inexperienced operator and/or cardiac center, while the use of perioperative antimicrobials was the only procedure-related protective measure against infection. The device-related risk factors include an abdominal pocket, dual chamber devices, use of ≥2 leads, and use of high-powered devices such as ICD or CRT defibrillator devices over PPMs [8, 13]. Our patient population had multiple of the above risk factors, which placed them at a high risk for developing a CIED infection.
Additionally, our immunocompromised patients with cancer have their own risk factors for infection, including intermittent neutropenia, thrombocytopenia, and a hypercoagulable state, increasing the risk for hematomas and thrombosis. As a general rule at our institution, in order to mitigate the risk for infection, we coordinate the device implantation with the oncology team and perform the procedure between chemotherapeutic cycles, ideally when the patient’s ANC is >1500 cells/μL and platelets are >40 000 cells/μL. These patients also have long-term intravascular devices with frequent access and receive extensive and repetitive surgeries, radiation, and chemotherapeutic regimens. Some cancer patients also proceed with immunotherapy and hematopoietic stem cell transplant. Hence, these patients are exposed to nosocomial pathogens in both the outpatient and inpatient settings. Many are also on long-term corticosteroids or other potent immunosuppressant drugs. Furthermore, patients living with cancer are prone to recurrent local and systemic infections, increasing the probability of secondary CIED infection. Unfortunately, most of these risk factors cannot be modified or eliminated to reduce device infections. Moreover, the risk of an infection in an individual patient is mostly determined by a combination of risk factors rather than an absolute number [12]. Therefore, composite weighted risk scores have been created to identify patients at low, medium, and high risk for developing CIED infection and to identify the potential need for enhanced prophylactic interventions [14].
Multiple procedures to reduce the high rate of CIED-related infections have been used in clinical practice [8]. The PADIT trial, which performed a large cluster randomized crossover bundle approach study of 19 603 patients (including 66% at high risk for infection) revealed a nonsignificant benefit from an “incremental” approach (preoperative intravenous vancomycin or cefazolin, plus intraoperative bacitracin wash and postoperative oral cephalosporin) over the “conventional” approach (single dose of preoperative cefazolin or vancomycin; odds ratio [OR], 0.77; P = .1) [15]. This study led to several nonrandomized retrospective [14, 16–18] and prospective trials [19] using the TYRX antimicrobial envelope, which elutes a high concentration of minocycline and rifampin within the surgical pocket. These studies revealed a significant clinical reduction in CIED infection (pooled OR, 0.29; P < .004), especially in patients at high risk for infection [12]. The follow-up landmark randomized controlled WRAP-IT study, which included 6983 patients at 181 centers in 25 countries, confirmed the success of the antimicrobial envelope. The primary end point of a major CIED infection was encountered in 42 (1.2%) patients in the control group, as opposed to 25 patients (0.7%) in the envelope group (P = .04), with a 40% relative risk reduction for a major CIED infection. The main limitations of these studies varied between (a) a relatively short follow-up period, usually 6–12 months; (b) lack of consecutive patient inclusion; (c) minimal number of included patients who had cancer; and (d) selection of control groups from different locations and time periods (with the exception of the WRAP-IT study), leading to several inherited biases.
In contrast to perioperative antimicrobials, the effectiveness of the TYRX antimicrobial envelope for the reduction of CIED infection must be balanced by the cost of this preventive device [20]. Standardized adjusted incremental costs associated with CIED infection from the published literature range from $14 360 to $16 498 and $28 676 to $53 349 for PPMs and ICDs, respectively, while the price of the TYRX envelope is slightly below $1000 [4, 20]. The WRAP-IT study revealed that the number needed to treat was 200 when the TYRX mesh was used for all CIED placements and decreased to 100 for high-risk patients undergoing ICD/CRT defibrillator replacement or upgrade [21]. Therefore, until the cost-effectiveness ratio improves, use of the antimicrobial envelope should be reserved primarily for those high-risk patients with several risk factors for developing a CIED infection.
Our study has a few limitations. First, our study was retrospective with no control group because once the envelope became available in 2012, all patients in our population had TYRX mesh placement along with CIED placement, owing mainly to the additive risk factors for infection in these cancer patients. Furthermore, a comparative group of patients in the pre-TYRX era may have led to further historical biases. Nonetheless, in comparison with published data on CIED recipients overall, our study revealed a similar CIED infection rate in patients with cancer [9, 14, 16, 18, 19]. Second, all patients were treated with standard-of-care strategies to prevent CIED infection [8], along with the bundle antimicrobial approach (preoperative antimicrobials, pocket irrigation, TYRX mesh, and postoperative oral antibiotics). Therefore, the individual impact of each item in the bundle would be difficult to elucidate. Furthermore, as our patients are exposed to several pathogens, including methicillin-resistant Staphylococcus aureus [22], and a few are allergic to β-lactams [23], and thus this population differed from the populations in the above-mentioned studies, perioperative vancomycin alone and postoperative oral minocycline were used.
CONCLUSIONS
All in all, our prophylactic bundle approach that includes the TYRX antimicrobial mesh supports no increase in CIED-related infections in an oncologic patient population. Therefore, this vulnerable population typically not offered a cardiac device should not be denied a CIED solely because of the risk for infection.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
We thank Sarah Bronson, ELS, from the University of Texas MD Anderson Cancer Center’s Department of Scientific Publications for her editorial assistance.
Financial support. This research was supported by the National Institutes of Health/ National Cancer Institute under award number P30CA016672.
Potential conflicts of interest. All authors have no financial interests to declare in relation to the content of this article. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Buch E, Boyle NG, Belott PH. Pacemaker and defibrillator lead extraction. Circulation 2011; 123:e378–80. [DOI] [PubMed] [Google Scholar]
- 2. Darouiche RO. Treatment of infections associated with surgical implants. N Engl J Med 2004; 350:1422–9. [DOI] [PubMed] [Google Scholar]
- 3. Connolly SJ, Philippon F, Longtin Y, et al. Randomized cluster crossover trials for reliable, efficient, comparative effectiveness testing: design of the Prevention of Arrhythmia Device Infection Trial (PADIT). Can J Cardiol 2013; 29:652–8. [DOI] [PubMed] [Google Scholar]
- 4. Sohail MR, Henrikson CA, Braid-Forbes MJ, et al. Mortality and cost associated with cardiovascular implantable electronic device infections. Arch Intern Med 2011; 171:1821–8. [DOI] [PubMed] [Google Scholar]
- 5. Classen DC, Evans RS, Pestotnik SL, et al. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med 1992; 326:281–6. [DOI] [PubMed] [Google Scholar]
- 6. de Oliveira JC, Martinelli M, Nishioka SA, et al. Efficacy of antibiotic prophylaxis before the implantation of pacemakers and cardioverter-defibrillators: results of a large, prospective, randomized, double-blinded, placebo-controlled trial. Circ Arrhythm Electrophysiol 2009; 2:29–34. [DOI] [PubMed] [Google Scholar]
- 7. Baddour LM, Epstein AE, Erickson CC, et al. ; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee; Council on Cardiovascular Disease in Young; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Nursing; Council on Clinical Cardiology; Interdisciplinary Council on Quality of Care; American Heart Association Update on cardiovascular implantable electronic device infections and their management: a scientific statement from the American Heart Association. Circulation 2010; 121:458–77. [DOI] [PubMed] [Google Scholar]
- 8. Blomström-Lundqvist C, Traykov V, Erba PA, et al. ; ESC Scientific Document Group European Heart Rhythm Association (EHRA) international consensus document on how to prevent, diagnose, and treat cardiac implantable electronic device infections. Eur J Cardiothorac Surg 2020; 57:e1–e31. [DOI] [PubMed] [Google Scholar]
- 9. Tarakji KG, Mittal S, Kennergren C et al. Antibacterial Envelope to Prevent Cardiac Implantable Device Infection. N Engl J Med 2019; 380:1895–905. [DOI] [PubMed] [Google Scholar]
- 10. Habib G, Lancellotti P, Antunes MJ, et al. ; ESC Scientific Document Group 2015 ESC guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015; 36:3075–128. [DOI] [PubMed] [Google Scholar]
- 11. Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000; 30:633–8. [DOI] [PubMed] [Google Scholar]
- 12. Ali S, Kanjwal Y, Bruhl SR, et al. A meta-analysis of antibacterial envelope use in prevention of cardiovascular implantable electronic device infection. Ther Adv Infect Dis 2017; 4:75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Polyzos KA, Konstantelias AA, Falagas ME. Risk factors for cardiac implantable electronic device infection: a systematic review and meta-analysis. Europace 2015; 17:767–77. [DOI] [PubMed] [Google Scholar]
- 14. Mittal S, Shaw RE, Michel K, et al. Cardiac implantable electronic device infections: incidence, risk factors, and the effect of the AigisRx antibacterial envelope. Heart Rhythm 2014; 11:595–601. [DOI] [PubMed] [Google Scholar]
- 15. Krahn AD, Longtin Y, Philippon F, et al. Prevention of arrhythmia device infection trial: the PADIT trial. J Am Coll Cardiol 2018; 72:3098–109. [DOI] [PubMed] [Google Scholar]
- 16. Bloom HL, Constantin L, Dan D, et al. ; COoperative Multicenter study Monitoring a CIED ANtimicrobial Device Investigators Implantation success and infection in cardiovascular implantable electronic device procedures utilizing an antibacterial envelope. Pacing Clin Electrophysiol 2011; 34:133–42. [DOI] [PubMed] [Google Scholar]
- 17. Shariff N, Eby E, Adelstein E, et al. Health and economic outcomes associated with use of an antimicrobial envelope as a standard of care for cardiac implantable electronic device implantation. J Cardiovasc Electrophysiol 2015; 26:783–9. [DOI] [PubMed] [Google Scholar]
- 18. Kolek MJ, Patel NJ, Clair WK, et al. Efficacy of a bio-absorbable antibacterial envelope to prevent cardiac implantable electronic device infections in high-risk subjects. J Cardiovasc Electrophysiol 2015; 26:1111–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Henrikson CA, Sohail MR, Acosta H, et al. Antibacterial envelope is associated with low infection rates after implantable cardioverter-defibrillator and cardiac resynchronization therapy device replacement: results of the citadel and centurion studies. JACC Clin Electrophysiol 2017; 3:1158–67. [DOI] [PubMed] [Google Scholar]
- 20. Kay G, Eby EL, Brown B, et al. Cost-effectiveness of TYRX absorbable antibacterial envelope for prevention of cardiovascular implantable electronic device infection. J Med Econ 2018; 21:294–300. [DOI] [PubMed] [Google Scholar]
- 21. Biffi M. The never-ending story of CIED infection prevention: shall we WRAP-IT and go? J Cardiovasc Electrophysiol 2019; 30:1191–6. [DOI] [PubMed] [Google Scholar]
- 22. Montassier E, Batard E, Gastinne T, et al. Recent changes in bacteremia in patients with cancer: a systematic review of epidemiology and antibiotic resistance. Eur J Clin Microbiol Infect Dis 2013; 32:841–50. [DOI] [PubMed] [Google Scholar]
- 23. Taremi M, Artau A, Foolad F, et al. Safety, efficacy, and clinical impact of penicillin skin testing in immunocompromised cancer patients. J Allergy Clin Immunol Pract 2019; 7:2185–91.e1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.