Abstract
Objective: To understand the different types and causes of prescribing errors associated with computerized provider order entry (CPOE) systems, and recommend improvements in these systems.
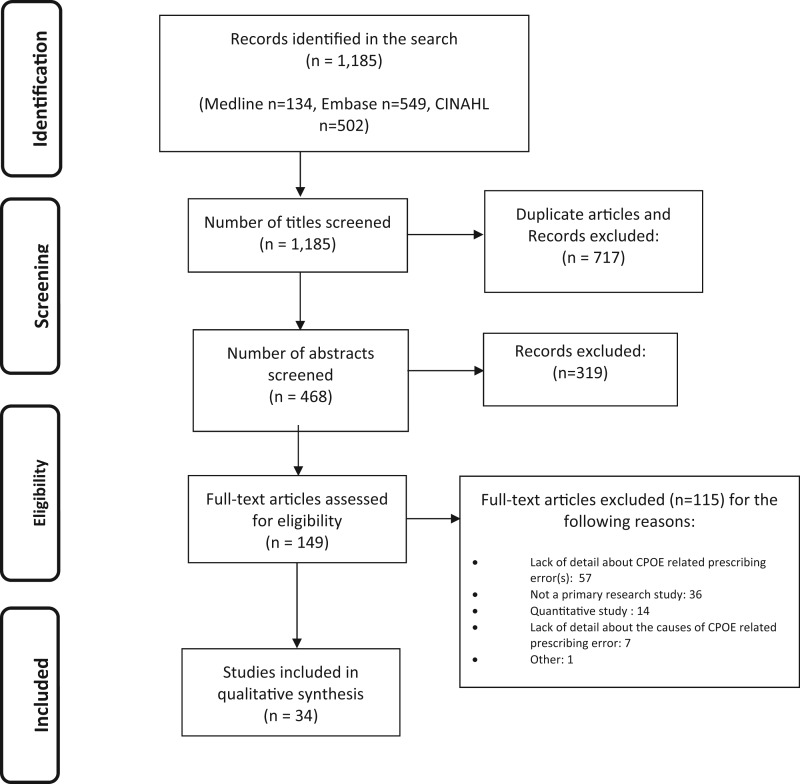
Materials and Methods: We conducted a systematic review of the literature published between January 2004 and June 2015 using three large databases: the Cumulative Index to Nursing and Allied Health Literature, Embase, and Medline. Studies that reported qualitative data about the types and causes of these errors were included. A narrative synthesis of all eligible studies was undertaken.
Results: A total of 1185 publications were identified, of which 34 were included in the review. We identified 8 key themes associated with CPOE-related prescribing errors: computer screen display, drop-down menus and auto-population, wording, default settings, nonintuitive or inflexible ordering, repeat prescriptions and automated processes, users’ work processes, and clinical decision support systems. Displaying an incomplete list of a patient’s medications on the computer screen often contributed to prescribing errors. Lack of system flexibility resulted in users employing error-prone workarounds, such as the addition of contradictory free-text comments. Users’ misinterpretations of how text was presented in CPOE systems were also linked with the occurrence of prescribing errors.
Discussion and Conclusions: Human factors design is important to reduce error rates. Drop-down menus should be designed with safeguards to decrease the likelihood of selection errors. Development of more sophisticated clinical decision support, which can perform checks on free-text, may also prevent errors. Further research is needed to ensure that systems minimize error likelihood and meet users’ workflow expectations.
Keywords: computerized provider order entry, clinical decision support, alerts, medication errors, patient safety, decision-making
BACKGROUND AND SIGNIFICANCE
The Institute of Medicine reported that adverse events are responsible for as many as 98 000 deaths in the United States each year.1 More recent evidence suggests that as many as 400 000 premature deaths occur each year in the United States due to preventable harm.2 Errors in the prescribing and administration of medicines, increasingly complex medical practice (e.g., an aging population), and the increased use of technology have all been quoted as possible reasons for this increase.1–3
Adoption rates of electronic health records have increased in the United States following the meaningful use program.4 Computerized provider order entry (CPOE) systems with clinical decision support (CDS) functionality have been shown to reduce the occurrence of prescribing errors.5–9 These systems can “facilitate and enhance the communication of a prescription, aiding the choice, administration or supply of a medicine through decision support and provide a robust audit trail for the entire medicines use process.”10 However, reports have also emerged that these CPOE systems (with or without CDS) have contributed to new types of errors in both primary and secondary care,3,11,12 some of which are potentially serious in nature, such as a prescription for 70 times over the correct dose of diamorphine that occurred due to misselection of a dose from a drop-down menu.13 These errors have been frequently referred to as the ‘unintended adverse consequences’ of technology,11,14 a term that describes both the unexpected and undesirable nature of these events.15
Due to the relative newness of CPOE systems in many health care organizations, developers and users may be unaware of the generation or causes of these “new” errors. A lack of consideration of human factor principles during the design stage has contributed to the emergence of these issues.16,17 Despite certification requirements from the Office of the National Coordinator for Health Information Technology that require vendors to employ a user-centered design process, a recent study reported that just over half of vendors actually employed usability staff, and that use of this approach was variable at best.18
A 2005 study by Koppel et al. sought to identify and quantify the role of CPOE in facilitating prescribing errors. Since then, many more studies have used qualitative techniques to provide a rich understanding of the types and causes of these errors.19 However, to the best of our knowledge, there has been no published systematic literature review specifically looking at CPOE-related prescribing errors. To address this gap, we conducted a systematic review to understand the different types and causes of errors that occur during the prescribing process when using CPOE systems, and to make recommendations about how these systems could be improved.
METHODS AND MATERIALS
Our review was conducted according to PRISMA guidelines20; each step is summarized below.
Eligibility criteria
Primary research studies that focused on prescribing errors associated with CPOE systems were eligible for inclusion. We were interested in studies that included qualitative data about the types and causes of these errors. Our search strategy covered the use of any type of CPOE system (e.g., self-developed or commercial) in any clinical setting (e.g., hospitals, outpatients, and primary care). Quantitative data were not included because this review was aimed at describing the types and causes of CPOE-related errors and not the frequency of errors. Studies published in peer-reviewed journals or conference proceedings between January 1, 2004 and June 22, 2015 were eligible for inclusion. This allowed us to focus on articles published since the seminal paper by Koppel et al., thus focusing on the current and pertinent issues that have since emerged. The search was restricted to English language publications. Editorials, commentaries, letters, and opinion articles were excluded.
Information sources and search
Three large databases were searched: the Cumulative Index to Nursing and Allied Health Literature, Embase (via OVID), and Medline (via OVID). Appropriate search terms were developed and grouped into “sets,” specifically relating to “computerized provider order entry,” “clinical decision support,” “electronic health records,” and “errors.” In each set, terms were combined with the “OR” operator and all sets were then combined with the “AND” operator. These sets are available via the online supplementary material. Database functionality was used (where possible) to restrict the search to qualitative studies. This search was conducted on the June 22, 2015.
Study selection
After duplicate articles were removed, 3 independent reviewers (CB, HM, and KT) screened the remaining titles to determine whether the articles met the inclusion criteria. Two authors (CB and HM, or CB and KT) then independently reviewed all abstracts and full texts, with one author (CB) acting as a constant across all publications. Disagreements were resolved by discussion, with arbitration by a fourth additional reviewer (SPS), if necessary. The reason a publication was rejected was also documented.
Data collection and analysis
A customized data extraction sheet was used by each of the 3 independent reviewers (CB, HM, and KT) to extract specific details about each study’s location, objectives, methods, and key findings. A narrative synthesis of all eligible studies was undertaken. Papers were read and re-read by 3 authors (CB, KT, and HT), and key recurring themes and sub-themes were identified iteratively from the data.
Bias assessment
We accept that bias may occur due to the subjective nature of qualitative research. A critical analysis of included studies was performed using the CASP (Critical Appraisal Skills Program) tool for qualitative research.21 Mays and Pope have advocated the use of methodological triangulation (use of 2 or more methods) as a way of strengthening the research design and safeguarding the “validity” of qualitative studies.22 We also assessed the included studies for the use of methodological triangulation.
RESULTS
A total of 1185 publications was identified through the database search, with 1036 excluded after removing duplicates and screening the titles and abstracts. On reviewing 149 full-text articles, 115 were excluded; a total of 34 was therefore included in the final review. These were comprised of 31 full text articles and 3 conference abstracts. Studies were conducted in the United States (n = 19), United States and Canada (n = 4), Canada (n = 1), UK (n = 4), Australia (n = 2), Spain (n = 1), Sweden (n = 1), Netherlands (n = 1), and Denmark (n = 1). Our bias assessment revealed 3 articles that did not use more than one method of data collection.23–25 All articles were included as they provided valuable insights. A table summarizing the key findings of the articles has been provided (see Appendix 1).
A descriptive and narrative synthesis of the data was undertaken to understand the different types and causes of prescribing errors associated with CPOE systems, and 8 key themes were identified and are discussed in detail below.
Computer screen display
The layout of the computer screen display affected how users viewed patient information. Displaying an incomplete list of a patient’s medications on the computer screen was found by Horsky et al.26 to have contributed to an incident where a patient was prescribed an overdose of potassium chloride and subsequently developed severe hyperkalemia. Analysis of the same incident also revealed that intravenous (IV) medications were not displayed in same the area of the screen as the patient’s other medications. This was likely to result in users missing or not considering these medicines when prescribing.26 Similar issues have been raised in other studies by Wetterneck et al. and Koppel et al., who suggested that a failure to display all orders, including active, recently administered, PRN (Pro re nata) (when required), and STAT (statim) (immediate), may inhibit the user from reviewing the entirety of a patient’s medications and result in duplicate doses being prescribed.3,27 The use of multiple screens, which require users to click through various parts of the CPOE system in order to access the necessary information, have been found to disrupt workflow and also lead to users incorrectly entering information ‘where it might fit’ rather than in the appropriate section of the record. The danger is that such information might not then be visible to other users and clinical safety checks may be bypassed.11 Horsky et al.26 also found that similarly designed screens in one system had important functional differences; e.g., the parameter for limiting the amount of medication delivered was time dependent for drip (IV infusion) administration yet dose dependent for IV bolus administration, and subsequently could be easily confused by prescribers. The ease of moving between different patients on an electronic system was also felt by Adelman et al.28 to have contributed to the placement of incorrect patient orders, particularly if the prescriber’s workflow had been interrupted.
Drop-down menus and auto-population
It is no surprise that selection errors associated with different drop-down lists (e.g., patient names, medication names, drug dosages, etc.) have been frequently reported.3,28–31 Westbrook et al. examined the system related errors that occurred across 2 commercial CPOE systems and found numerous examples of selection errors. These included specific cases where the wrong administration route of a medication; e.g., sodium chloride 0.9% infusion via the epidural route instead of the IV route, were selected.32 Juxtaposition errors, whereby a medication listed before or after the desired medication was erroneously chosen, also resulted in orders being placed for drugs with an entirely different indication than what was intended.11 One example included users’ misselection of ethamsylate (a hemostatic agent) instead of ethambutol (an antibiotic) from a drug list.29 Delays in system response time resulted in prescribers using “multiple clicks” to select a drug item, which increased the risk of misselection.30 Odukoya et al.33 noted that inadvertent “mouse wheeling” (selecting an incorrect item by unknowingly scrolling past the correct item) could also have contributed to incorrect orders being placed. A range of prescribing errors have been attributed to the presence of auto-population functionality, whereby on entering the first few letters (or numbers) of a drug name (or dose), the system “suggests” information that could be easily selected in error.33,34 Snyder et al.35 encountered a wrong drug order when “vir” was typed for the intended drug “Viread,” and “efavirenz,” an alternative antiretroviral, was suggested as a prescribing option by the system autofill functionality and was therefore erroneously selected.
Wording
The wording of the text used within CPOE systems has also been shown to contribute to prescribing errors. For example, in one study users misinterpreted the data label “total volume,” which they thought meant the total volume of dose that should be administered, rather than the system “meaning” (i.e., the total volume of an individual bag of fluid). Horsky et al.26 described these misinterpretations as a “user-design mismatch.” Another example included a dose of 20 mg written as 0020.000 mg, which could be misinterpreted due to the additional zeros presented.36 One study that explored CPOE-related prescribing errors in a general practice setting found that users had difficulty finding items or knowing the specific wording that would allow them to select certain drugs; e.g., a particular type of insulin from a pick-list.30
Default settings
Overly restrictive default settings have been associated with a number of CPOE-related prescribing errors. Prescribers may simply fail to change a default order sentence containing drug name, form, and dosage, or a default time presented by the system, thus resulting in a patient receiving the wrong dose, missing a dose, or receiving it at an unintended time.3,29,32 Koppel et al.3 found that some ‘late in the day orders,” where the prescriber intended the patient to receive the drug on the same day, were delayed until the next day, with potential consequences for the patient. If the drug combination carbidopa/levodopa (Sinemet®), for example, is not administered at the appropriate time, a patient with Parkinson’s disease can experience increased motor symptoms. Similarly, duplicate dose errors have been reported, with a patient being administered a night-time dose of the antiviral efavirenz (Sustiva®) and an inappropriate second dose the following morning because the system automatically defaulted to a 09:00am daily dose.35 Lack of knowledge about the default stop dates and times of certain medications can also lead to errors.26 Some systems combine default order sentences as part of an order set to make it easier to prescribe a group of medicines; e.g., medications for post-surgical analgesia. Doctors interviewed in one study described an instance where a nonsteroidal anti-inflammatory drug was “hidden” in an order set and inappropriately prescribed to an asthmatic patient.29 Default settings for some medicines used in certain clinical specialities therefore may not be appropriate due to the range of prescribing options that are dependent on patient specific factors. For example, the dose of azathioprine (an immunosuppressant) is often dependent on the patient’s weight, indication, laboratory results, and thiopurine S-methyltransferase activity; thus a list of suggested doses may be confusing unless the system is able to guide the user by taking these other patient factors into consideration.
Non-intuitive ordering or information transmission
Inflexible or complex ordering processes made entering some orders particularly difficult and resulted in users employing workarounds. These included selecting a default drug order sentence (e.g., give twice daily) and adding a contradictory free-text comment that advises the nurse to administer different instructions (e.g., give three times daily). Unfamiliar abbreviations were also entered in free-text boxes, which in turn were open to misinterpretation by different users.36 Zhan et al.37 found that a CPOE system failed to recognize the abbreviation “TID” (take three times a day) and therefore did not record this order. Odukoya et al.38 described an example of confusing directions written in free-text: “take a half tablet and there will be a period and then it will say take two tablets…” Users employed workarounds to prescribe complex prescriptions, which are generally very difficult to write electronically, such as tapering courses of prednisolone.39 “Copy and paste” functionality, which is designed to save users time, was also found to unintentionally give rise to the generation of incorrect orders.23 Wentzer et al.40 also observed instances where medications that had been previously prescribed on a prior hospital admission and stopped were transferred to the new admission as an “active” medication and inappropriately continued.
Interoperability issues
One study described the compatibility issues between a prescribing system and a community pharmacy system, which related to a failure of one system to correctly interpret the terminology, possibly due to a lack of standardized codes in requests; e.g., “magnesium citrate” or “mag. citrate.” Certain requests (e.g., mag. citrate) were translated incorrectly by the community pharmacy system once received, and led to prescriptions being generated for the inappropriate drug name, quantity package size, and patient name.33 Similarly, Nanji et al.41 identified important information that was omitted from prescriptions electronically ordered from either inpatient or outpatient prescribing systems and received by a community pharmacy system. The study suggested that this was related to a mismatch between the text-box size in the prescribing system (on which the order was originally placed) and the pharmacy system (on which the order was received), thus leading to certain information being missed or not communicated.41
Repeat prescriptions and automated processes
An important difference between handwritten and electronic prescriptions is the ease with which a repeat electronic prescription can be generated with a few simple clicks.31 This is clearly more efficient for users, but there is a downside. There have been cases where pharmacists have picked up prescription errors in the past but the original prescriptions (which contained the error) were not updated in the system and subsequently repeated.33,41 These erroneous electronic prescriptions may be harder to detect, as one study participant describes: “But if there's a black and white typed document that includes nonsense, it is harder to recognize it and it's more easily overlooked or assumed to be correct…”31
Users work processes
Inappropriate work processes, for example entering all of a patient’s medicines in batches at the end of a ward round on the CPOE system, pose safety risks.42 Issues can arise around whether a prescriber can correctly recall potentially large lists of medications.40 Delays in entering information can result in clinicians who were not present on the ward round being unable to immediately utilize such information for their own decision making.42 Similarly, an inconvenient log-in process can give rise to users working under other colleagues’ log-ins, which has both legal and professional implications.43 Wentzer et al.40 found that some doctors would login to the CPOE system and allow a nurse to work under their account; thus the person whose ID the system recognized as making an order was not actually the true prescriber of that order.
CDS systems
The consequences of over-alerting and alert fatigue are well described in the literature.34,44 However, a lack of appropriate safeguards may also prevent prescribing errors from being detected, particularly if users have wrongly assumed that their orders are being checked. For example, Schiff et al.39 identified one hospital site that was unaware that their CDS alerts had been switched off following a system update. This study also identified many CDS systems that did not offer sufficient protection againist many common errors.39 Wetterneck et al.27 found that orders for different forms of the same medication; e.g., metoprolol 25 mg tablets (oral) and metoprolol 5 mg IV, were not identified as potential duplicates when prescribed together, and therefore did not generate an alert. Underutilization of CDS functionality was reported by Khajouei et al.,43 who found that a button prescribers needed to click to perform a dosage calculation was not clearly displayed, and therefore prescribers continued to manually calculate doses, which increased the risk of potental human errors. CDS systems have also provided users with erroneous information, such as inappropriate dosages that do not take into account patient specific factors (e.g., reduced renal function)34 or orders based on outdated drug information.39
DISCUSSION
In this evaluation, we have described the types and causes of prescribing errors associated with CPOE systems, specifically identifying themes from qualitative studies. The eight key areas were computer screen display, drop-down menus and autopopulation, wording, default settings, nonintuitive ordering or information transmission, repeat prescriptions and automated processes, users’ work processes, and CDS alerting. All of these relate closely to human factors and user-centered design. Table 1 provides a summary of the key themes, associated issues, and recommendations, and whether the error could be classified (predominantly) as system related, user related, or both.
Table 1.
Key themes, associated issues and recommendations
| Main error facilitator | Key themes | Specific issues | Recommendations |
|---|---|---|---|
| System related | Computer screen display |
|
|
| System related | Drop-down menus and auto-population |
|
|
| System related | Wording |
|
|
| System related and user related | Default settings |
|
|
| System related | Non-intuitive ordering or information transmission |
|
|
| System related | Repeat prescriptions and automated processes |
|
|
| User related | User’s work processes | User education and training about the risks of using workarounds | |
| System related and user related | CDS systems |
|
Abbreviations: CDS: Clinical Decision Support.
This systematic review described errors relating to the way information was displayed on the computer screens.26,42 One simple solution might be to organize the screen layout such that all medications (including both oral and IV) are listed in one area, with minimal navigation required. Additionally, data labels should be clear to the user and guide them to separate areas where further specific information can be obtained.17,45 System developers and implementers should consider the potential for a “user-design mismatch” and the importance of designing the system according to the users’ workflow and the terminology that they use.26 Indeed, as many issues may not be identified until after system implementation, there is a clear need for post-implementation testing to ensure that these systems are working as intended.42 Chan et al.,46 found that a well-designed CPOE system could also possibly reduce the need for training, with no participants requesting assistance when ordering using the user-centered design format compared to over one-third of participants requesting assistance on a “standard” CPOE test system. Horsky et al.26 demonstrated the potential for confusion amongst users who used functions that were visually very similar on the order screen, but behaved differently, e.g., the function to calculate total dose for drip (infusion) or IV (bolus) orders. Design tools such as color and language should be applied consistently throughout a system (and possibly all systems) to prevent users misinterpreting information during the prescribing process.17
The design of CPOE systems is a critical consideration. Drop-down menus can provide a list of drug dosing options in ascending or descending order, so as to make it easier for prescribers to find exactly what they are looking for. However, long lists of medications, particularly those listed alphabetically, with names which look-alike or sound-alike are prone to selection errors. Westbrook et al.32 found that 43% of system-related errors were due to selection errors, which led the authors to conclude that reducing the opportunities for users to “select” items from lists during the course of prescribing may reduce CPOE-related errors. This should be weighed against the potential consequences of prescribers entering erroneous doses in free-text, and the additional time this manual entry of information may take.17 Tall man lettering has been used to help users distinguish between similar drug names such as hydrOXYzine and hydrALAzine.47 There is some limited evidence from experimental studies to support its use more generally48; however, there is currently a lack of robust studies relating specifically to CPOE systems.47 Galanter et al.49 showed that indication-based alerts can help intercept wrong drug and wrong patient orders (commonly encountered with selection and autofill entry errors), by halting the prescriber’s workflow and allowing them to self-correct the order. Due to the potential burden of excessive CDS alerting, the limited use of indication alerts for high-risk, look-alike/sound-alike drug pairs should be considered.50
The issues identified in this review pertaining to default doses have been supported in the quantitative literature. Eslami et al.51 found that 86% (n = 113) of orders placed for 2 aminoglycoside antibiotics (gentamycin and tobramycin) using the suggested default dose were associated with an overdose, compared to only 53% (n = 66) cases when the default dose was not selected. This default dose was based on an average sized adult with normal renal function, and thus poses the question about whether such default doses are well placed in certain clinical specialties where patients are more likely to have parameters that frequently fluctuate outside of normal limits (e.g., ICU or a nephrology ward).51 Order sets can standardize prescribing and improve adherence to guidelines. However, we found that certain items were inadvertently prescribed for some patients (via an order set) as they were “hidden” among a list of medications, which included both suitable and unsuitable items. Bobb et al.52 suggested that order sets should be more patient specific, presenting only relevant recommendations, e.g., a non-penicillin drug for a penicillin allergic patient as first-line treatment. They also recommended that individual items within an order are linked, so that they updated in unison. For instance, if an order set contains supportive therapy (e.g., a proton pump inhibitor) for an indicated medication (e.g., steroid), the supportive therapy should be ceased when the indicated medicine is discontinued.52
We found that free-text orders are commonly used as a method of bypassing system requirements or CDS alerts. A quantitative study conducted by Palchuk et al.53 found discrepancies between the information contained in the structured and free-text fields in 16% (n = 470) of electronic prescriptions. System developers should consider the development of more sophisticated CDS which can perform checks on free-text orders.53 Furthermore, the frequent use of free-text options by users may suggest a lack of suitable structured functions. Dhavle et al.54 found that many free-text comments encountered in their study, could be avoided by using an updated version of the electronic prescribing system, which incorporated additional structured fields. Developers should address this need by providing prescribing options, such as a tapering course of steroids or alternate day dosing, as part of ongoing system optimization and development55; in addition to accelerating the rate at which new functionality reaches users.54 Certain CPOE systems are unable to accommodate prescriptions for drugs given via multiple routes (oral and rectal); this suggests a possible lack of understanding and consideration of actual prescribing and administration practices that would need to be addressed. Ongoing testing and evaluation of systems (and any customizations made) is needed in order to optimize and enhance CPOE systems following initial implementation.56
CDS has undoubtedly contributed to a reduction in errors and has huge potential to further improve safety in the future.57 However, as this review has found, there is still much to be done to improve the safety of these systems. Schiff et al. discovered that only 26.6% (n = 95) of a sample of erroneous test-orders generated warnings thus allowing many potentially harmful orders to be placed.39 Additionally, there was considerable variability in the way organizations implemented CDS functionality and the ability of different systems to warn clinicians about errors,39 which may confuse users who work across multiple sites. Wright et al.58 also found examples of malfunctioning CDS, resulting in a failure to generate warnings when needed or the production of unnecessary alerts. Such malfunctions were due to software upgrades, code changes, accidental alteration of CDS rules, and faults with external systems.58 Customization is crucial for organizations striving to achieve safer patient care following CPOE implementation. One study found that even a small 5% increase in the Leapfrog score (an evaluation tool, which tests CPOE systems ability to safeguard against erroneous test order) was associated with a significant reduction in preventable adverse drug events.59 Thus, organizations should be reassured of the benefits of customizing their system to include a range of CDS checks. Perhaps one of the most crucial developments will be the production of more patient specific and better worded alerts to reduce the impact of alert fatigue and erroneous suggestions.60 A recently published study by Slight et al.50 found that some alerts (e.g., duplicate drug alerts) contained confusing wording and did not explicitly describe the error present, (e.g., “(the drug) already exists… under the selected assessment,” highlighting the need to improve system usability.
Human factors and user-centered design is key across all of these 8 areas and should be prioritized when developing these systems. There is a need to thoroughly evaluate CPOE related incidents so as to better understand system failings, using various (or a combination of different) approaches61 such as failure mode and effect analysis,62 visual and cognitive walkthrough evaluation,26 and usability evaluation techniques (including semi-structured interviews and observations).63 Phansalkar et al.64 created a list of such principles specific to the design of CDS alerts to prevent confusion and maximize their impact. Russ et al.65 saw a significant reduction in prescribing errors when they redesigned CDS alerts according to human factors principles; this was attributed to improved visibility of text, more logical organization of information and more informative alerts.
This systematic review has provided strong insights into the key structural design elements associated with CPOE related prescribing errors. However, we have only reported what has been published in the literature and there may be unpublished work that could also provide valuable insights. Another possible limitation is that our review spans over ten years and it is possible that some system vendors may be currently working on or have already addressed some of the issues highlighted.3 For instance, all 6 EHRs evaluated in one study displayed patient identifiers on the top of the computer screen throughout the prescribing process, thus helping to reduce wrong patient errors.36 We also acknowledge that we did not register our review with a prospective register for systematic reviews. Finally, there may also have been a publication bias towards studies that reported more positive findings and consequently the number of different types of CPOE related prescribing errors may be much higher. However, the findings of this review highlight the need for further research into uncovering these specific types of errors and for the establishment of a national reporting database where these types of errors should be logged and addressed (both by vendors and by local customization teams.19,66
CONCLUSION
We identified 8 key areas that have been associated with CPOE related prescribing errors – all relate closely to human factors and user-centered design. The design and layout of the computer screen display should be carefully considered. Drop-down menus should be designed with safeguards to prevent the occurrence of selection errors. Local customization and development of more sophisticated CDS, which is able to perform checks on free-text and provide users with adequate prescribing functions, is clearly needed. Developers must aim to improve the specificity, sensitivity, and usability of these systems in light of the recent research in this area.
CONTRIBUTIONS
SPS, CB, and KR conceived this review. CB, KLT, and HLM conducted the literature search and extracted the data. CB and SPS led the writing of this manuscript with all other coauthors (HLM, KLT, DFS, JA, KR, AKH, DWB) commenting on subsequent drafts. All authors gave their approval for the final version to be published.
Figure 1.
Diagrammatic representation of the steps involved in the literature search.
Supplementary Material
ACKNOWLEDGMENTS
We gratefully acknowledge Health Education Kent, Surrey, and Sussex for partial funding of this evaluation. We also acknowledge the additional assistance received from Mr Neil Watson, Newcastle-upon-Tyne NHS Foundation Trust, in supporting this work.
SUPPLEMENTARY MATERIAL
Supplementary material are available at Journal of the American Medical Informatics Association online.
REFERENCES
- 1. Kohn LT, Corrigan J, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, D.C: National Academy Press; 2000. [PubMed] [Google Scholar]
- 2. James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf 2013;9(3):122–8. [DOI] [PubMed] [Google Scholar]
- 3. Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005;293(10):1197–203. [DOI] [PubMed] [Google Scholar]
- 4. Slight SP, Berner ES, Galanter W, et al. Meaningful use of electronic health records: experiences from the field and future opportunities. JMIR Med Inform 2015;3(3):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 1998;21;280(15):1311–6. [DOI] [PubMed] [Google Scholar]
- 6. Nuckols TK, Smith-Spangler C, Morton SC, et al. The effectiveness of computerized order entry at reducing preventable adverse drug events and medication errors in hospital settings: a systematic review and meta-analysis. Syst Rev 2014;3:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bates DW, Teich JM, Lee J, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc 1999;6(4):313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Garg A, Adhikari N, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes. A systematic review. JAMA 2005;293:1223–38. [DOI] [PubMed] [Google Scholar]
- 9. Kaushal R, Jha AK, Franz C, et al. Return on investment for a computerized physician order entry system. J Am Med Inform Assoc 2006;13(3):261–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. NHS Connecting for Health. ePrescribing Functional Specification for NHS Trusts 2007. See www.connectingforhealth.nhs.uk/systemsandservices/eprescribing/baselinefunctspec.pdf. Accessed August 10, 2016. [Google Scholar]
- 11. Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 2006;13(5):547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gandhi TK, Weingart SN, Seger AC, et al. Outpatient prescribing errors and the impact of computerized prescribing. J Gen Intern Med 2005;20(9):837–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shulman R, Singer M, Goldstone J, Bellingan G. Medication errors: a prospective cohort study of hand-written and computerised physician order entry in the intensive care unit. Crit Care 2005;9(5):R516–R21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ash JS, Sittig DF, Dykstra R, Campbell E, Guappone K. Exploring the unintended consequences of computerized physician order entry. Stud Health Technol Inform 2007;12(Pt 1):198–202. [PubMed] [Google Scholar]
- 15. Ash JS, Sittig DF, Poon EG, Guappone K, Campbell E, Dykstra RH. The extent and importance of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 2007;14(4):415–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Russ AL, Zillich AJ, McManus MS, Doebbeling BN, Saleem JJ. A human factors investigation of medication alerts: barriers to prescriber decision-making and clinical workflow. AMIA Annu Symp Proc 2009;2009:548–52. [PMC free article] [PubMed] [Google Scholar]
- 17. Khajouei R, Jaspers MW. The impact of CPOE medication systems' design aspects on usability, workflow and medication orders: a systematic review. Methods Inf Med 2010;49(1):3–19. [DOI] [PubMed] [Google Scholar]
- 18. Ratwani RM, Fairbanks RJ, Hettinger AZ, Benda NC. Electronic health record usability: analysis of the user-centered design processes of eleven electronic health record vendors. J Am Med Inform Assoc 2015;ocv050;doi: 10.1093/jamia/ocv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. US Food and Drug Administration. Computerized Prescriber Order Entry Medication Safety (CPOEMS): Uncovering and Learning From Issues and Errors. 2015. http://www.fda.gov/downloads/Drugs/DrugSafety/MedicationErrors/UCM477419.pdf. Accessed August 10, 2016. [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;21;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Critical Appraisal Skills Programme (CASP). CASP Checklist 2014. http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf. Accessed August 10, 2016. [Google Scholar]
- 22. Mays N, Pope C. Qualitative Research: Rigour and qualitative research. BMJ (Clinical research ed) 1995;311(6997):109–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Caudill-Slosberg M, Weeks WB. Case study: identifying potential problems at the human/technical interface in complex clinical systems. Am J Med Qual 2005;20(6):353–7. [DOI] [PubMed] [Google Scholar]
- 24. Chan J, Shojania KG, Easty AC, Etchells EE. Usability evaluation of order sets in a computerised provider order entry system. BMJ Qual Saf 2011;20(11):932–40. [DOI] [PubMed] [Google Scholar]
- 25. Baysari MT, Reckmann MH, Li L, Day RO, Westbrook JI. Failure to utilize functions of an electronic prescribing system and the subsequent generation of ‘technically preventable' computerized alerts. J Am Med Inform Assoc 2012;19(6):1003–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Horsky J, Kuperman GJ, Patel VL. Comprehensive analysis of a medication dosing error related to CPOE. J Am Med Inform Assoc 2005;12(4):377–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wetterneck TB, Walker JM, Blosky MA, et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc 2011;18(6):774–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Adelman JS, Kalkut GE, Schechter CB, et al. Understanding and preventing wrong-patient electronic orders: a randomized controlled trial. J Am Med Inform Assoc 2013;20(2):305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Savage I, Cornford T, Klecun E, Barber N, Clifford S, Franklin BD. Medication errors with electronic prescribing (eP): two views of the same picture. BMC Health Serv Res 2010;10:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Slight SP, Howard R, Ghaleb M, Barber N, Franklin BD, Avery AJ. The causes of prescribing errors in English general practices: a qualitative study. Br J Gen Pract 2013;63(615):e713–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Goldman RE, Dube C, Lapane KL. Beyond the basics: Refills by electronic prescribing. Int J Med Inform 2010;79(7):507–14. [DOI] [PubMed] [Google Scholar]
- 32. Westbrook JI, Baysari MT, Li L, Burke R, Richardson KL, Day RO. The safety of electronic prescribing: manifestations, mechanisms, and rates of system-related errors associated with two commercial systems in hospitals. J Am Med Inform Assoc 2013;20(6):1159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Odukoya OK, Stone JA, Chui MA. E-prescribing errors in community pharmacies: exploring consequences and contributing factors. Int J Med Inform 2014;83(6):427–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ash JS, Sittig DF, Campbell EM, Guappone KP, Dykstra RH. Some unintended consequences of clinical decision support systems. AMIA Annu Symp Proc 2007;2007:26–30. [PMC free article] [PubMed] [Google Scholar]
- 35. Snyder AM, Klinker K, Orrick JJ, Janelle J, Winterstein AG. An in-depth analysis of medication errors in hospitalized patients with HIV. Ann Pharmacother 2011;45(4):459–68. [DOI] [PubMed] [Google Scholar]
- 36. Jäderlund Hagstedt L, Edvard Rudebeck C, Petersson G. Usability of computerised physician order entry in primary care: assessing ePrescribing with a new evaluation model. Inform Prim Care 2011;19(3):161–8. [DOI] [PubMed] [Google Scholar]
- 37. Zhan C, Hicks RW, Blanchette CM, Keyes MA, Cousins DD. Potential benefits and problems with computerized prescriber order entry: analysis of a voluntary medication error-reporting database. Am J Health Syst Pharm 2006;63(4):353–8. [DOI] [PubMed] [Google Scholar]
- 38. Odukoya OK, Chui MA. Relationship between e-prescriptions and community pharmacy workflow. J Am Pharm Assoc 2012;52(6):e168–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Schiff G, Amato MG, Eguale T, et al. Computerised physician order entry-related medication errors: analysis of reported errors and vulnerability testing of current systems. BMJ Qual Saf 2015;24(4):264–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wentzer HS, Bottger U, Boye N. Unintended transformations of clinical relations with a computerized physician order entry system. Int J Med Inform 2007;76 (Suppl 3):S456–61. [DOI] [PubMed] [Google Scholar]
- 41. Nanji KC, Rothschild JM, Boehne JJ, Keohane CA, Ash JS, Poon EG. Unrealized potential and residual consequences of electronic prescribing on pharmacy workflow in the outpatient pharmacy. J Am Med Inform Assoc 2014;21(3):481–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cresswell KM, Bates DW, Williams R, et al. Evaluation of medium-term consequences of implementing commercial computerized physician order entry and clinical decision support prescribing systems in two ‘early adopter' hospitals. J Am Med Inform Assoc 2014;21(e2):e194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Khajouei R, Wierenga PC, Hasman A, Jaspers MW. Clinicians satisfaction with CPOE ease of use and effect on clinicians' workflow, efficiency and medication safety. Int J Med Inform 2011;80(5):297–309. [DOI] [PubMed] [Google Scholar]
- 44. van der Sijs H, Aarts J, Vulto A, Berg M. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc 2006;13(2):138–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Odukoya O, Chui M. Examining the impact of e-prescribing use on community pharmacy workflow. J Am Pharm Assoc 2012;52(2):262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chan J, Shojania KG, Easty AC, Etchells EE. Does user-centred design affect the efficiency, usability and safety of CPOE order sets? J Am Pharm Assoc 2011;18(3):276–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lambert BL, Schroeder SR, Galanter WL. Does Tall Man lettering prevent drug name confusion errors? Incomplete and conflicting evidence suggest need for definitive study . BMJ Qual Saf 2015, Published Online First: 23 December 2015, doi:10.1136/bmjqs-2015-004929. [DOI] [PubMed] [Google Scholar]
- 48. David Gerrett AGG, Darker IT, Ruth Filik, Purdy KJ. Tall Man Lettering: Final Report of The Use of Tall Man Lettering to Minimise Selection Errors of Medicine Names in Computer Prescribing and Dispensing Systems ITQ Invitation Reference ed. 2009. http://webarchive.nationalarchives.gov.uk/20130502102046/http://www.connectingforhealth.nhs.uk/systemsandservices/eprescribing/refdocs/tallman.pdf. Accessed 10, August 2016. [Google Scholar]
- 49. Galanter WL, Bryson ML, Falck S, et al. Indication alerts intercept drug name confusion errors during computerized entry of medication orders. PLoS One 2014;9(7). e101977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Slight SP, Eguale T, Amato MG, et al. The vulnerabilities of computerized physician order entry systems: a qualitative study. J Am Med Inform Assoc 2015; doi: 10.1093/jamia/ocv135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Eslami S, Abu-Hanna A, De Keizer NF, De Jonge E. Errors associated with applying decision support by suggesting default doses for aminoglycosides. Drug Saf 2006;29(9):803–9. [DOI] [PubMed] [Google Scholar]
- 52. Bobb AM, Payne TH, Gross PA. Viewpoint: controversies surrounding use of order sets for clinical decision support in computerized provider order entry. J Am Med Inform Assoc 2007;14(1):41–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Palchuk MB, Fang EA, Cygielnik JM, et al. An unintended consequence of electronic prescriptions: prevalence and impact of internal discrepancies. J Am Med Inform Assoc 2010;17(4):472–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Dhavle AA, Yang Y, Rupp MT, Singh H, Ward-Charlerie S, Ruiz J. Analysis of prescribers' notes in electronic prescriptions in ambulatory practice. JAMA Intern Med 2016;176(4):463–70. [DOI] [PubMed] [Google Scholar]
- 55. Walsh KE, Adams WG, Bauchner H, et al. Medication errors related to computerized order entry for children. Pediatrics 2006;118(5):1872–9. [DOI] [PubMed] [Google Scholar]
- 56. Cresswell KM, Bates DW, Sheikh A. Ten key considerations for the successful optimization of large-scale health information technology. J Am Med Inform Assoc 2016 doi: 10.1093/jamia/ocw037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bright TJ, Wong A, Dhurjati R, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med 2012;157(1):29–43. [DOI] [PubMed] [Google Scholar]
- 58. Wright A, Hickman T-TT, McEvoy D, et al. Analysis of clinical decision support system malfunctions: a case series and survey. J Am Med Inform Assoc 2016;doi: 10.1093/jamia/ocw005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Leung AA, Keohane C, Lipsitz S, et al. Relationship between medication event rates and the Leapfrog computerized physician order entry evaluation tool. J Am Med Inform Assoc 2013;20(e1):e85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Coleman JJ, van der Sijs H, Haefeli WE, et al. On the alert: future priorities for alerts in clinical decision support for computerized physician order entry identified from a European workshop. BMC Med Inform Decis Mak 2013;13:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Jaspers MWM. A comparison of usability methods for testing interactive health technologies: methodological aspects and empirical evidence. Int J Med Inform 2009;78(5):340–53. [DOI] [PubMed] [Google Scholar]
- 62. Vélez-Díaz-Pallarés M, Delgado-Silveira E, Carretero-Accame ME, Bermejo-Vicedo T. Using healthcare failure mode and effect analysis to reduce medication errors in the process of drug prescription, validation and dispensing in hospitalised patients. BMJ Qual Saf 2013;22(1):42–52. [DOI] [PubMed] [Google Scholar]
- 63. Friedman M, Wyatt J. Evaluation Methods in Biomedical Informatics (Health Informtics). 2nd ed.Springer; 2005. New York [Google Scholar]
- 64. Phansalkar S, Edworthy J, Hellier E, et al. A review of human factors principles for the design and implementation of medication safety alerts in clinical information systems. J Am Med Inform Assoc 2010;17(5):493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Russ AL, Zillich AJ, Melton BL, et al. Applying human factors principles to alert design increases efficiency and reduces prescribing errors in a scenario-based simulation. J Am Med Inform Assoc 2014;21(e2):e287–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. National Institute for Clinical Excellence. Medicines Optimisation: the Safe and Effective Use of Medicines to Enable the Best Possible Outcomes. 2015. Available at: https://www.nice.org.uk/guidance/ng5. Accessed August 10, 2016. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.