Abstract
Objectives: Readmission following colorectal surgery, typically due to surgery-related complications, is common. Patient-centered discharge warnings may guide recognition of early complication signs after colorectal surgery.
Materials and Methods: User-centered design of a discharge warnings tool consisted of iterative health literacy review and a heuristic evaluation with human factors and clinical experts as well as patient end users to establish content validity and usability.
Results: Literacy evaluation of the prototype suggested >12th-grade reading level. Subsequent revisions reduced reading level to 8th grade or below. Contents were formatted during heuristic evaluation into 3 action-oriented zones (green, yellow, and red) with relevant warning lexicons. Usability testing demonstrated comprehension of this 3-level lexicon and recognition of appropriate patient actions to take for each level.
Discussion: We developed a discharge warnings tool for colorectal surgery using staged user-centered design. The lexicon of surgical discharge warnings could structure communication among patients, caregivers, and clinicians to improve post-discharge care.
Keywords: readmissions, colorectal surgery, usability testing, health literacy, discharge instructions
INTRODUCTION
Hospitals face increased financial responsibility for 30-day readmissions. Published interventions focus largely on reducing readmissions for medical patients.1,2 The discharge needs of surgical patients are often distinct, requiring specific engagement. The majority of surgical patients are readmitted for common complications related to the surgical procedure itself.3–7 This predictability offers the opportunity to provide postoperative patients with targeted discharge warnings aimed at recognizing common post-discharge complications.8,9
Among surgical procedures, colorectal surgery has one of the highest unplanned 30-day readmission rates.4,6 Common causes of readmission include ileus or bowel obstruction, surgical site infection, and dehydration.4,6 Prompt attention to warning signs for these common complications is critical for health care systems to have the opportunity to intervene early to avoid readmission.9 Patients play a critical role by identifying and communicating early problems. As recommended by the Institute of Medicine, patients need discharge instructions with tailored information that empowers them to participate in their post-discharge care.8,10
We previously developed discharge instructions to address the specific needs of colorectal surgery patients following discharge.6,9 In the prototype, the discharge instructions included a set of specific, actionable warnings, consisting of a lexicon for complications following colorectal surgery that activates patients to communicate with their health care providers. This discharge warnings lexicon was developed through a systematic review of the literature6 and a Delphi expert consensus panel with a national sample of colorectal surgeons.9
The current study presents our effort to transform physician-centered discharge warnings into an understandable, usable warnings lexicon for patients using health literacy and usability heuristics standards and cognitive interviews with patients during the postoperative period. Finally, we provide a discussion of how these discharge warnings can be effectively integrated within a clinical team structure that includes patients and their caregivers.
METHODS
A multiphase, user-centered design process was used to design and test the discharge warnings prototype.11 A design thinking approach11 was used to synthesize → ideate → prototype and then iteratively revise the warning signs and symptoms tool for colorectal surgery patients. The synthesis process included a previously conducted meta-analysis of conditions associated with readmission following colorectal surgery.6 Data synthesis moved to concept ideation using a Delphi expert panel of surgical experts, who developed an initial prototype with a physician-centric lexicon for discharge warnings.9 The current study begins from this initial prototype and moves through testing and prototype revisions.
Procedures
Phase 1: Health literacy review
We conducted a literacy evaluation of the discharge warnings prototype,9 led by a health literacy expert (MPO), using the Flesch-Kincaid Readability Test, the revised Dale-Chall method, and the Lexile Framework to make substantial revisions to our patient-facing content.12 The goal of the literacy evaluation was to reduce the required reading level to that of an 8th-grade education or below in order to be consistent with the average reading level of the local patient population we were interested in observing.13
Phase 2: Heuristics evaluation with experts and end users
To ensure that the discharge warnings lexicon was presented succinctly and uniformly, we conducted a series of heuristic evaluations. First, a human factors psychologist (BC) conducted an initial heuristics review using a subset of nationally recognized usability heuristics published by the National Institutes of Health and available at: http://www.usability.gov.14 The goal of the heuristics evaluations was to ensure that the discharge warnings conformed to known human limitations and research-based guidelines for page layout; headings, titles, and labels; text and color appearance; lists; content organization; and usability.14 Second, 2 additional investigators, a clinician (AN) and a non-clinician (LH), reviewed the preliminary list of findings and identified additional concerns. The human factors expert then compiled these findings into an adapted prototype for usability testing by patient end users.
Patients were recruited for cognitive interviews to determine usability during their first postoperative clinic appointment following colorectal surgery at the surgical oncology clinic of the Michael E. DeBakey VA Medical Center. The first postoperative clinic appointment was typically within 2 weeks of hospital discharge. Patients who underwent elective colon or rectal surgery and had a scheduled appointment were eligible to participate. Eligible patients were identified and approached by members of the surgical care team during their clinic appointment. Patients interested in participating gave informed consent at the appointment and were provided with a color copy of the colorectal discharge warnings and everyday care instructions. A 30-min telephone interview was scheduled with each patient for the following week. Patients were asked to read over and review the warning signs and symptoms at home during the intervening time between their postoperative clinic visit and the scheduled interview. Interviews continued until thematic saturation was achieved regarding usability guidelines, defined as no new themes being uncovered in 2 subsequent interviews.
All interviews were audio recorded and transcribed verbatim. Interviews were conducted by research staff who had no role in the care of the patients. Interviews followed a semistructured interview guide (see Table 1 for questions). Six multidisciplinary research personnel (surgery, gerontology, hospital medicine, human factors psychology, and organizational psychology) then performed a thematic analysis of interview transcripts using a card-sorting procedure to identify content that patients found most salient.15,16 A single-linkage cluster analysis of the card-sorting data was performed using the Jaccard index as a metric of distance. Patient response themes were derived from the “clusters” of patient responses (using a 0.33 distance threshold).
Table 1.
Thematic analysis of phase 2 qualitative responses
| Page | Question | Response Theme(s) |
|---|---|---|
| Warning Signs | When looking at this page, what is the first thing that stands out to you? |
|
| Warning Signs | What is the green zone telling you? |
|
| Warning Signs | What is the yellow zone telling you? |
|
| Warning Signs | What is the red zone telling you? |
|
| Everyday Care | When looking at this page, what is the first thing that stands out to you? |
|
| Everyday Care | In your own words, can you describe the information on this page? |
|
| Both Pages | Do you have any other suggestions for how we could improve the usefulness of these instructions? |
|
Note: Phrases in quotation marks are representative quotes from that theme.
RESULTS
Phase 1
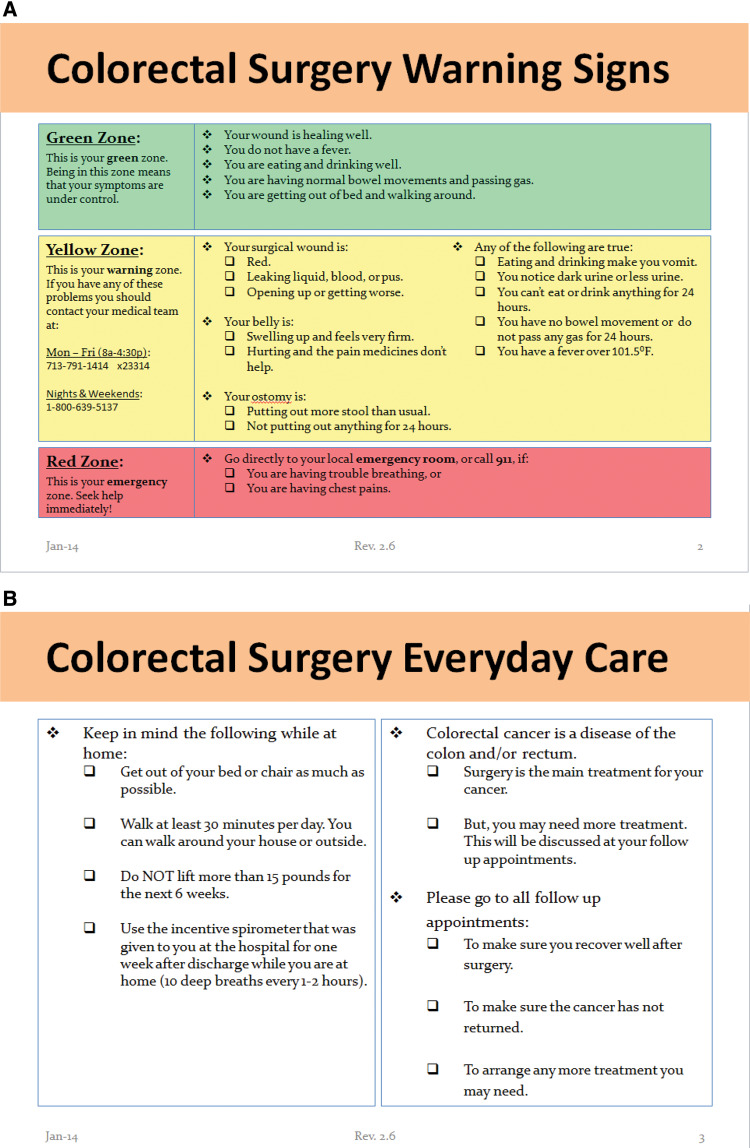
Results of the iterative design process and literacy evaluation revealed that the initial discharge warnings, using language adopted directly from the expert panel, required a literacy level consistent with >12th-grade education (Figure 1 ). Subsequent revisions to the content of the discharge warnings, in consultation with our health literacy expert, reduced the required reading level to ≤8th grade (Figure 2 ).
Figure 1.
Initial version of the warning signs page developed for discharge instructions incorporating the 12 warning signs identified by the Delphi panel.
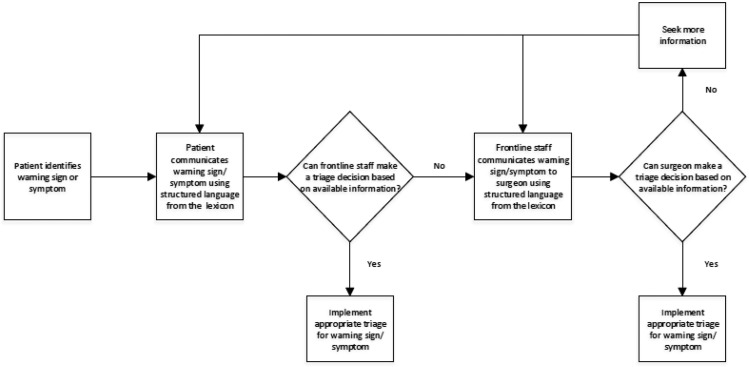
Figure 2.
Second major iteration of the warning signs tool developed for the discharge instructions.
Phase 2
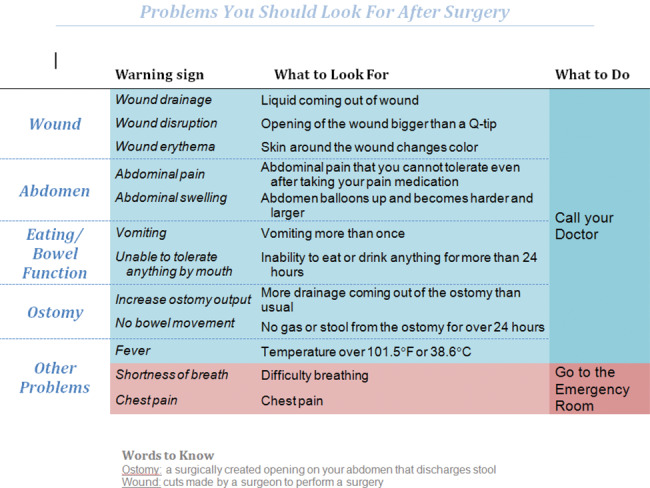
A comprehensive heuristics evaluation revealed several inconsistencies regarding the presentation and readability of the information provided by the discharge warnings. As shown in Figure 2, the discharge warnings had low-contrast colorized text, an inconsistent grouping scheme, inconsistent use of bold text, unclear calls to action, and a mix of passive and active voice. The human factors expert integrated the consensus findings of the heuristics evaluation into a revised version of the discharge warnings lexicon page using a simpler language base and a more consistent design (Figure 3 ).
Figure 3.
Final iteration of the (A) discharge warning signs and (B) everyday care pages developed for patients receiving colorectal surgery as part of cancer therapy.
Patient interviews
Thematic saturation for usability was achieved after 7 post-colorectal surgery patients completed cognitive interviews. All the participants were male, ranging in age from 49 to 73 years. One completed only primary school, 2 had high school diplomas, and the rest had at least some college. The patient interviews and thematic analysis indicated that these patients understood the information provided and approved of the manner in which warning signs and symptoms were presented (Table 1). Patients demonstrated comprehension of the 3-level heuristic for warnings (ie, the green, yellow, and red zones) and recognized appropriate patient actions. Patients further suggested edits to the design, readability, and formatting of certain pages.
Discharge warnings
Patients first noticed the colors, discharge warnings, and heading. Patients understood that the green zone indicated that “everything is going well,” the yellow zone indicated “things you need to look out for,” and the red zone indicated that the patient needed to see a doctor right away. Patients rated the clarity of information on this page from 1 (lower) to 5 (higher), for an average of 4.7 (standard deviation = 0.5).
Everyday care instructions
The thematic analysis of responses to our open-ended questions about the everyday care instructions revealed that patients first noticed the instructions and heading. Patients understood that the information indicated that they needed to “get moving” and to “keep up with it.” Patients rated the clarity of the information on this page from 1 (lower) to 5 (higher), for an average of 5.0.
DISCUSSION
We describe a user-centered “design thinking” process culminating in a set of discharge warnings that are usable and understandable for patients who have recently undergone colorectal surgery.17,18 The current study began from a prototype consisting of a surgeon-defined lexicon of signs and symptoms for common complications of colorectal surgery that most often result in hospital readmission.6,9 Two consecutive adaptations of the instructions arose from structured revisions drawn from the health literacy (Figure 2) and human factors (Figure 3) literature and under the supervision of experts. The structure and content of this patient-centered version was then evaluated for usability by patients who recently underwent elective colorectal surgery. Cognitive interviews demonstrated that our discharge instructions were clear and usable for patients during the critical first month following surgery. The usefulness of these discharge instructions lies in their potential to trigger awareness and facilitate communication between patients and their clinicians to potentially mitigate common post-surgical complications.
Theoretical foundation
Our discharge instructions rely on a lexicon (ie, simple terms used to communicate complex phenomena) to inform communication between patients and their clinical teams. The findings of this study suggest that patients and caregivers can make sense of the meaning and clinical usefulness of simple terms that describe warning signs and symptoms signaling a potential postoperative complication.19 Furthermore, patients grasped that different terms signified different levels of urgency for action (ie, an urgency heuristic using commonly understood green, yellow, and red signals). This sense-making lexicon was easily understood as a “warning signs” framework that provides clear instructions to patients on when to act.19 Breakdowns in communication between patients and providers are commonly associated with preventable readmissions.20 In qualitative studies, patients and caregivers often express frustration with their attempts to obtain appropriate medical triage for post-discharge problems;21,22 however, the available literature has not addressed ways to improve communication between patients and the health care system after discharge.8 The lexicon developed in this study offers an important step forward by providing patients with an understandable list of clinical prompts that are patient-centered and actionable, and clearly communicate medical problems that have meaning for patients and clinicians that can potentially extend beyond colorectal surgery.19
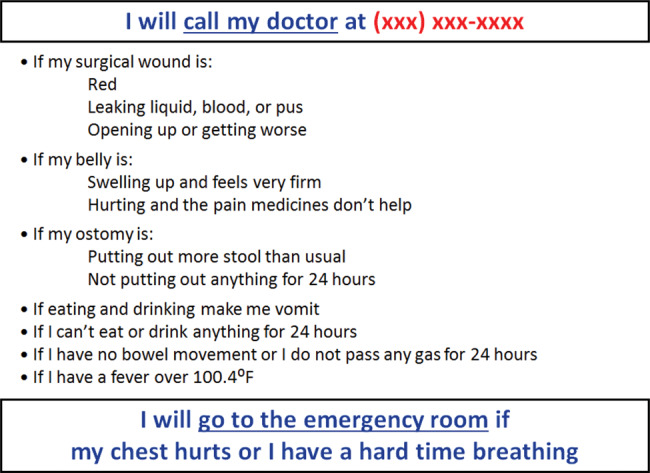
The design of these warning signs is grounded in the naturalistic decision-making processes of experts.23 This literature finds that experts (eg, surgical nurse practitioners) often act intuitively using a recognition model that takes into account the specific environment (follow-up after colorectal surgery), relevant cues (wound is red and patient has a fever), expectations about what those cues mean (likely surgical site infection), and a course of action to address the issue (schedule immediate appointment). To make appropriate postoperative triage decisions, front-line clinicians (eg, nurses working at a 24 h nursing help line) and surgical experts must first obtain information from patients to identify the environment and relevant cues (Figure 4 ). Insufficient information transfer between patients and providers may lead to significant delays in medical care as additional information is sought. Delays impact the health care system’s ability to intervene in postoperative problems in the outpatient setting. Patients and their caregivers can be activated regarding the concerns that expert surgeons use to triage postoperative care with only modest training at the time of discharge, using tools integrated into patient health portals, such as our discharge warnings, to reinforce this training. Clear communication is an important skill for effective teams, and improving team communication features prominently in successful training programs in health care.24,25
Figure 4.
Postoperative triage using the colorectal surgery warning signs lexicon.
The current study has limitations. Usability testing was performed with a small number of veteran patients drawn from a single health system whose perspectives may not apply to other settings. While this important subpopulation (older, comorbid men) is often linked to readmission following colorectal surgery,6 additional validation studies with a broader sample (gender, race, socioeconomic and insurance status, etc.) are needed to confirm the usability of this warning signs lexicon and its effectiveness in reducing readmissions.
Clinical implications
The findings of this study suggest that patient-centered discharge instructions can be easily understood and integrated into a warning signs lexicon for patients following elective colorectal surgery. The structure and content of discharge warnings are critical in activating patients to monitor their health and communicate with clinicians whenever warning signs of complications are present. Patients can be given these warning signs as part of discharge instructions generated from electronic medical records and trained on how to report them to their clinicians. Future studies should measure differences in patient understanding, frequency of communication using the specific language of the discharge warnings, and ultimately changes in emergency room or hospital admissions among those receiving instructions with and without this specific warning signs lexicon.
Funding
This research was supported by a Health Services Research and Development Quality Enhancement Research Initiative grant (RRP 12‐532) awarded to ADN and DHB, and in part by resources at the Veterans Affairs HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13‐413) at the Michael E. DeBakey VA Medical Center and Baylor College of Medicine.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the United States government, or other affiliated institutions.
Competing Interest
The authors have no competing interests to declare.
Contributions
ADN: obtaining funding; data acquisition, analysis, interpretation; drafting work; final approval; agreement to be accountable for all aspects of the work. MJH: data analysis and interpretation, drafting work, final approval, and agreement to be accountable for the work. LTL: data analysis and interpretation, revising work for important intellectual content, final approval, and agreement to be accountable for the work. MKP-O: data analysis and interpretation, revising work for important intellectual content, final approval, and agreement to be accountable for the work. BC: data acquisition, analysis and interpretation; revising work for important intellectual content; final approval; and agreement to be accountable for the work. WLM: data analysis and interpretation, revising work for important intellectual content, final approval, and agreement to be accountable for the work. LIH: data acquisition, analysis and interpretation; revising work for important intellectual content; final approval; and agreement to be accountable for the work. DAA: data interpretation, revising work for important intellectual content, final approval, agreement to be accountable for the work. BWT: data analysis and interpretation, revising work for important intellectual content, final approval, and agreement to be accountable for the work. DHB: obtaining funding, data interpretation, revising work for important intellectual content, final approval, and agreement to be accountable for the work.
References
- 1. Jack BW, Chetty VK, Anthony D et al. . A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Int Med. 2009;1503:178–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;16617:1822–8. [DOI] [PubMed] [Google Scholar]
- 3. Dharmarajan K, Hsieh AF, Lin Z et al. . Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;3094:355–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Merkow RP, Ju MH, Chung JW et al. . Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;3135:483–95. [DOI] [PubMed] [Google Scholar]
- 5. Hinami K, Bilimoria KY, Kallas PG, Simons YM, Christensen NP, Williams MV. Patient experiences after hospitalizations for elective surgery. Am J Surg. 2014;2076:855–62. [DOI] [PubMed] [Google Scholar]
- 6. Li LT, Mills WL, White DL et al. . Causes and prevalence of unplanned readmissions after colorectal surgery: a systematic review and meta-analysis. J Am Geriatr Soc. 2013;617:1175–81. [DOI] [PubMed] [Google Scholar]
- 7. Kable A, Gibberd R, Spigelman A. Complications after discharge for surgical patients. ANZ J Surg. 2004;743:92–97. [DOI] [PubMed] [Google Scholar]
- 8. Horstman MJ, Stewart DE, Naik AD. Improving patients’ post-discharge communication: making every word count. Circulation. 2014;13013:1091–94. [DOI] [PubMed] [Google Scholar]
- 9. Li LT, Mills WL, Gutierrez AM, Herman LI, Berger DH, Naik AD. A patient-centered early warning system to prevent readmission after colorectal surgery: a national consensus using the Delphi method. J Am College Surgeons. 2013;2162:210–16. [DOI] [PubMed] [Google Scholar]
- 10. Roundtable on Health Literacy. Facilitating Patient Understanding of Discharge Instructions: Workshop Summary. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 11. Brown T. Design thinking. Harv Bus Rev. 2008;866:84–92, 141. [PubMed] [Google Scholar]
- 12. Paasche-Orlow MK, Taylor HA, Brancati FL. Readability standards for informed-consent forms as compared with actual readability. New Engl J Med. 2003;3488:721–26. [DOI] [PubMed] [Google Scholar]
- 13. Kelly PA, Haidet P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. 2007;661:119–22. [DOI] [PubMed] [Google Scholar]
- 14. US Department of Health and Human Services. Research-Based Web Design & Usability Guidelines, enlarged/expanded edition. Washington, DC: US Government Printing Office; 2006. [Google Scholar]
- 15. Spencer D. Card Sorting: Designing Usable Categories. Brooklyn, NY: Rosenfield Media; 2009. [Google Scholar]
- 16. Wood J, Wood L. Card sorting: current practices and beyond. J Usability Stud. 2008;41:1–6. [Google Scholar]
- 17. Gosbee JW, Gosbee LL. Using human factors engineering to improve patient safety. Oakbrook Terrace, IL: Joint Commission Resources; 2005. [Google Scholar]
- 18. Corry MD, Frick TW, Hansen L. User-centered design and usability testing of a web site: An illustrative case study. Educ Technol Res Dev. 1997;454:65–76. [Google Scholar]
- 19. Klein G, Moon B, Hoffman RR. Making sense of sense-making 2: a macrocognitive model. IEEE Intell Syst. 2006;215:88–92. [Google Scholar]
- 20. Auerbach AD, Kripalani S, Vasilevskis EE et al. . Preventability and Causes of Readmissions in a National Cohort of General Medicine Patients. JAMA Intern Med. 2016;1764:484–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cain CH, Neuwirth E, Bellows J, Zuber C, Green J. Patient experiences of transitioning from hospital to home: an ethnographic quality improvement project. J Hosp Med. 2012;75:382–87. [DOI] [PubMed] [Google Scholar]
- 22. Kangovi S, Barg FK, Carter T et al. . Challenges faced by patients with low socioeconomic status during the post-hospital transition. J Gen Intern Med. 2014;292:283–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Klein G. Naturalistic decision making. Hum Factors. 2008;503:456–60. [DOI] [PubMed] [Google Scholar]
- 24. Baker DP, Salas E, King H, Battles J, Barach P. The role of teamwork in the professional education of physicians: current status and assessment recommendations. Jt Comm J Qual Patient Saf. 2005;314:185–202. [DOI] [PubMed] [Google Scholar]
- 25. Weaver SJ, Dy SM, Rosen MA. Team-training in healthcare: a narrative synthesis of the literature. BMJ Qual Saf. 2014;235:359–72. [DOI] [PMC free article] [PubMed] [Google Scholar]