Abstract
Objective: Monitoring the supervision of residents can be a challenging task. We describe our experience with the implementation of a templated note system for documenting procedures with the aim of enabling automated, discrete, and standardized capture of documentation of supervision of residents performing floor-based procedures, with minimal extra effort from the residents.
Materials and methods: Procedural note templates were designed using the standard existing template within a commercial electronic health record software. Templates for common procedures were created such that residents could document every procedure performed outside of the formal procedural areas. Automated reports were generated and letters were sent to noncompliers.
Results: A total of 27 045 inpatient non–formal procedural area procedures were recorded from August 2012 to June 2014. Compliance with NoteWriter template usage averaged 86% in the first year and increased to 94.6% in the second year (P = .0055).
Initially, only 12.5% of residents documented supervision of any form. By the end of the first year, this was above 80%, with the gains maintained into the second year and beyond. Direct supervision was documented to have occurred where required in 62.8% in the first year and increased to 99.8% in the second year (P = .0001) after the addition of hard stops. Notification of attendings prior to procedures was documented 100% of the time by September 2013. Letters sent to errant residents decreased from 3.6 to 0.83 per 100 residents per week.
Conclusion: The templated procedure note system with hard stops and integrated reporting can successfully be used to improve monitoring of resident supervision. This has potential impact on resident education and patient safety.
Keywords: electronic health record, templated notes, resident education, resident supervision, graduate medical education
BACKGROUND AND SIGNIFICANCE
The Accreditation Council for Graduate Medical Education (ACGME) Common Program Requirements mandate the provision of supervision for residents.1 Program directors are required to “monitor resident supervision at all participating sites.” At the same time, residents “must be able to competently perform all medical, diagnostic, and surgical procedures considered essential for the area of practice.” Demonstrating these requirements for both parties may present challenges. Currently, one may try to meet these requirements by doing manual abstraction of medical records,2,3 conducting interviews4 or surveys,5,6 and keeping personal procedural logs.7–9 However, these would require additional time and energy, and may be associated with less than precise results.10
OBJECTIVE
We set out to create and implement a semi-automated system of addressing these requirements in a discrete, standardized, and comprehensive manner that requires minimal extra effort on the residents’ part. Our vision was to have a system for discretely capturing and reporting on procedures performed across the institution. With this, we can ensure that appropriate levels of supervision are being documented, captured, and processed in real time to allow for institution-wide monitoring, reporting, and action based upon the data, where indicated. This potentially enhances resident education and affords the opportunity to impact patient safety by ensuring oversight.
MATERIALS AND METHODS
NoteWriter procedural note templates
Procedural note templates were designed using the standard existing electronic health record (EHR) template (known as NoteWriter) within the EHR software EpicCare Inpatient (Epic Systems Corp., WI, USA). This template allows users to document procedure notes by clicking buttons that cascade to other button choices as they move through the essential fields of procedural note documentation. A group of templates for common specific procedures was created along with a generic template, such that residents could document, in a standardized format, every procedure performed outside of formal procedural areas (FPAs), eg, operating rooms, pulmonary labs, interventional radiology suites (Figure 1). We felt that the area with the greatest need to ensure appropriate oversight would be inpatient procedures performed outside the FPAs, where the “Swiss cheese model” of accident causation is more likely to occur due to a reduction in the number of safety layers.11,12 Indirect supervision13 is also more often utilized in the nonoperative setting, hence posing increased concerns regarding oversight. Likewise, the FPAs all have formalized and standardized processes for oversight of resident supervision. For this reason, as our initial endeavor we mandated compliance with use of the NoteWriter template when documenting procedures in the non-FPAs of the primary teaching hospital (Parkland Memorial Hospital) at our institution.
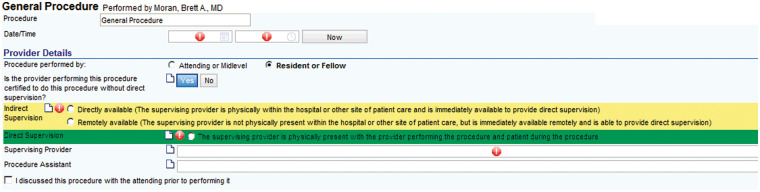
Figure 1.
Screenshot of NoteWriter procedural note template © 2015 Epic Systems Corporation. Used with permission.
In fulfilling our objectives, care was taken to minimize any adverse impact on the residents by implementing our intervention through a pre-existing system in use, and in the context of performing an activity they would already have to perform (documenting a procedure note). Each field within the NoteWriter template captured metadata that enabled discrete, automated reporting.
A total of 17 NoteWriter procedure note templates were launched in July 2012, with broad communication mandating their use to residents and all other providers at Parkland Memorial Hospital. Within every procedure template was a standard module containing a cascading question functionality to prompt for and mandate capture of documentation of oversight by learners, including whether they were privileged to perform without direct supervision, the level of supervision under which the procedure was performed, the supervising provider, and whether prior discussion of the procedure with an attending occurred (Figure 1). A procedural note would then be generated automatically, taking the place of a standard free-text chart entry, which might otherwise contain only limited relevant information that is typically not discrete, consistent, or auditable by system reports.
After an initial review of compliance with this new system at 3 months post implementation, in November 2012 a second memo by the chief medical information officer and the graduate medical education (GME) designated institutional official (DIO) was sent out to re-educate and encourage compliance with this process. From March 2013, the process was further enhanced whereby residents who did not abide by this standard process were sent letters directly from the DIO, directing their attention to the deficiency and reminding them to utilize the standardized templates. Finally, hard stops to encourage users to complete several mandatory fields, including the supervision portion of the template, were added in May 2013. A summary of the timeline with the introduction of interventions is shown in Figure 2.
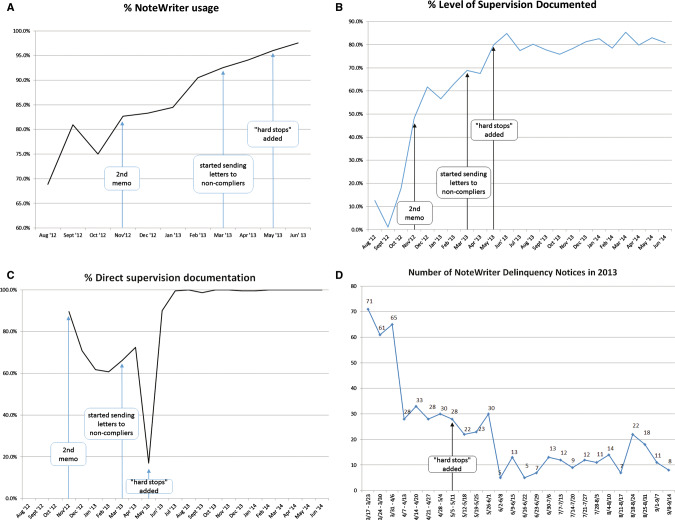
Figure 2.
(A) Proportion of non–formal procedural area (FPA) procedures in the inpatient setting documented using the NoteWriter procedure note template since implementation in July 2012. (B) Proportion of non–FPA procedures documented using the NoteWriter procedure note template that included the level of supervision provided to residents. (C) Proportion of non–FPA procedures in the inpatient setting documenting direct supervision when it was required. (D) Number of letters sent per week to noncompliers in the first 6 months since the initiative started in March 2013. Data from July 2012 were omitted due to the introductory period and the changeover period of the academic year. For the months of August, September, and October 2012, no procedures reported the need for direct supervision.
Automated reports were generated from the EHR on a regular basis to monitor compliance. Our reporting allowed us to capture all procedure note note types. The use of nontemplated versions was detected by the absence of the structured elements that had metadata tags associated with them. Based on these reports, letters were sent out to noncompliers through the office of GME.
All procedure notes (whether using the template or not) were coded to require mandatory co-signature by the designated attending physician. This enabled verification of the accuracy of the designated supervising physician, the level of supervision documented and required, and other pertinent details of the procedure, minimizing the possibility of misattribution.
Parkland Memorial Hospital
Parkland Memorial Hospital is an 860-bed level 1 trauma center located in Dallas, Texas, serving as the primary teaching hospital for the University of Texas Southwestern Medical Center. In fiscal year 2014, Parkland saw 47 863 total discharges, 1 005 663 total outpatient visits, and 265 955 total emergency room visits. Eighty ACGME programs and all levels of residency, from interns to fellows, are represented. Documentation of medical care is performed electronically with EpicCare. Institutional Review Board exemption was granted for publication of these data.
Statistical analysis
The data from the generated reports were summarized and presented with descriptive statistics. Continuous data were subjected to the Student’s t test. The α level was set at 0.05. All P-values reported were based on 2-sided tests. Statistical analyses were performed in GraphPad QuickCalcs (GraphPad Software Inc., La Jolla, CA, USA).
RESULTS
A total of 27 045 inpatient procedures by 1075 residents were recorded from non–formal procedure areas between August 2012 and June 2014 (Tables 1–3). Compliance with use of this discrete documentation averaged 74.8% in the first 3 months.
Table 1.
Breakdown of the number of inpatient and outpatient procedure notes by level of residency
| PGY Level | Inpatient | Outpatient | Unknown |
|---|---|---|---|
| 1 | 6601 | 4032 | |
| 2 | 10 885 | 5574 | 10 |
| 3 | 5423 | 4431 | 16 |
| 4 | 557 | 4641 | 18 |
| 5 | 50 | 77 | 1 |
| 6 | 38 | 3 | |
| 7 | 4 | 1 | |
| 8 | 1 | 4 | |
| Fellow | 2395 | 1280 | 5 |
| Total | 25 954 | 20 043 | 50 |
PGY: Postgraduate year
A small number of procedure locations were not documented
Table 2.
Breakdown of the number of inpatient and outpatient procedure notes by specialty of provider
| Specialty | IP/ED | OP | Unknown | Total |
|---|---|---|---|---|
| Emergency Medicine | 8280 | 6 | 8286 | |
| Dermatology | 259 | 4459 | 2 | 4720 |
| Orthopedic Surgery | 3913 | 563 | 4476 | |
| Ophthalmology | 87 | 4023 | 4 | 4114 |
| Internal Medicine | 3338 | 423 | 3761 | |
| General Surgery | 2498 | 1018 | 3516 | |
| Obstetrics and Gynecology | 1553 | 1487 | 3040 | |
| Oral and Maxillofacial Surgery | 597 | 2220 | 2817 | |
| Physical Medicine and Rehabilitation | 23 | 1884 | 1907 | |
| Urology | 164 | 1437 | 1 | 1602 |
| Plastic Surgery | 1189 | 138 | 1327 | |
| Family Medicine | 250 | 841 | 1091 | |
| Otorhinolaryngology | 338 | 471 | 3 | 812 |
| Pediatrics | 678 | 4 | 682 | |
| Hematology and Oncology | 364 | 237 | 601 | |
| Nephrology | 483 | 2 | 485 | |
| Pathology | 76 | 340 | 416 | |
| Neurology | 327 | 78 | 405 | |
| Cardiology | 327 | 8 | 1 | 336 |
| Neurological Surgery | 318 | 2 | 320 | |
| Pulmonary Diseases | 223 | 1 | 224 | |
| Anesthesiology | 174 | 12 | 38 | 224 |
| Rheumatology | 51 | 90 | 141 | |
| Podiatry | 105 | 16 | 121 | |
| Gastroenterology | 74 | 14 | 1 | 89 |
| Critical Care Surgery | 56 | 56 | ||
| Clinical Neurophysiology | 35 | 15 | 50 | |
| Hematology | 13 | 28 | 41 | |
| Neurocritical Care | 31 | 31 | ||
| Oncology Surgery | 5 | 23 | 28 | |
| Vascular Surgery | 1 | 10 | 11 | 22 |
| Psychiatry | 15 | 2 | 17 | |
| Endocrinology | 11 | 11 | ||
| Clinical Cardiac Electrophysiology | 9 | 9 | ||
| Allergy and Immunology | 1 | 5 | 6 | |
| Hospice and Palliative Medicine | 1 | 1 | ||
| Totals | 25 866 | 19 858 | 50 | 45 774 |
The total number of procedures on this table is less than the total number of procedures in Table 1 due to a tiny proportion of incorrectly documented specialties.
Table 3.
List of the top 20 most performed procedures in the non–formal procedural area inpatient setting from August 2012 to June 2014
| Top 20 most performed procedures | IP/ED |
|---|---|
| Laceration repair | 3868 |
| Splint | 3005 |
| Vascular access | 2896 |
| Incision and drainage | 2782 |
| Lumbar puncture | 1770 |
| General procedure | 1763 |
| Paracentesis | 1200 |
| Arterial line | 1091 |
| Airway access | 1029 |
| Endometrial biopsy | 738 |
| Arthrocentesis | 673 |
| Thoracentesis | 443 |
| Chest tube | 417 |
| Reduction | 304 |
| Intubation | 207 |
| Bone marrow biopsy | 148 |
| Umbilical catheter | 140 |
| Nail removal | 126 |
| Echocardiogram | 93 |
| Intrauterine device removal | 78 |
Further initiatives, including the second memo in November 2012, the individual letters from the DIO for noncompliers in March 2013, and the introduction of hard stops in May 2013, led to a steady improvement in compliance with NoteWriter usage (Figure 2A). This averaged 86% in the first year, increased to 94.6% in the second year (t = 3.10, 20 df, n = 25891, P = .0055), and stabilized in that range thereafter.
Level of supervision
By creating a templated note, we were also able to discretely capture other metrics of importance. When the project began, only 12.5% of residents documented supervision of any form (Figure 2B). By the end of the first year, over 80% of residents were documenting the level of supervision for procedures, with the gains maintained into the second year and beyond. Prior Notification of attendings for certain procedures (eg, thoracentesis or pericardiocentesis) was a requirement for residents, and these were also recorded and captured. This number began at 0%, but with feedback letters from the GME rose to be documented consistently at 100% by September 2013.
Direct supervision
As discussed in the Materials and Methods section, we felt that the highest risk of adverse events might occur in procedures performed in the non-FPA locations of the hospital. Likewise, residents performing procedures for which they had not met the criteria to perform without direct supervision were felt to be the most at-risk group. From the NoteWriter templated procedural notes, direct supervision was documented to have occurred in instances where it was required 62.8% in the first year (Figure 2C). This increased to an average of 99.8% in the second year (t = 4.96, 17 df, n = 3130, P = .0001) after the addition of hard stops in the template to ensure completion of the form. The specific name of the supervising physician was also discretely documented.
Letters to noncompliers
In March 2013, the GME office began to send letters to errant providers detailing their omissions and highlighting the new standard practice for documenting procedures and supervision. While the initial burden of work was high (averaging 52 letters per week over the first 5 weeks, or an average of 3.6 letters per 100 residents per week), the residents modified their behavior, and fewer letters were required each week until they plateaued at an average of 12 per week for this institution of 1452 residents (0.83 letters per 100 residents per week) (Figure 2D).
DISCUSSION
Over the past decade, the spotlight on resident education has been focused on the 80-hour-per-week duty restrictions and the 16-hour shift limit for interns.14–25 Resident supervision has not received as much attention, and this has been reflected in the literature. To the best of our knowledge, our study represents the first attempt at addressing the ACGME’s requirement of provision of supervision to residents at an institutional level and in a semi-automated manner. Our results demonstrate the successful implementation of a simple and effective system that enables the monitoring of resident supervision to be objectively quantified.
At a large institution such as ours, ensuring compliance with a newly implemented policy requires the efforts of multiple parties. The initial memorandum informing the residents of the new policy was sent out by the chief medical informatics officer, along with e-learning modules to help the residents through the process. Individual residency program directors at the institution were also engaged in and informed of this new policy, and were encouraged to brief their residents on the subject. With this minimal effort, we were able to document capture of oversight 75% of the time. A second memorandum was sent out by the associate dean for GME, reminding residents to adhere to use of the templates. Along the way, the design of the templates was optimized to improve workflow based on feedback from the residents, and hard stops were introduced to maximize compliance. Individual letters sent out through the GME office to noncompliant providers also led to a positive response. As a result of all these efforts, compliance with the NoteWriter templated note system improved to the mid to upper 90% range and maintained a high level over the following 2 years. At this time, we are able to document oversight of our residents for non–formal procedural areas an average of 95% of the time via automated reports available to the GME and operational leadership.
The GME team is able to access this report and use it for a variety of purposes, including meeting the ACGME mandate, and also to report on procedures performed by residents, the types of procedures residents are performing, indications for procedures, complications, and specific names of supervising physicians.
The supervision of residents has often been left in the hands of the residency program director. Methods of ensuring adequate and appropriate supervision include surveying of residents and program directors,26–29 direct observation of a select cohort of attending-resident interactions, retrospective audit of patient encounter documentation,30 and use of personal procedural logs.7–9
The discordant expectations of supervising attendings and residents on appropriate levels of supervision have previously been reported.6 Farnan et al. reported that attending physicians often thought they were not given the opportunity to be more involved in resident supervision, while residents felt that their attendings’ micromanagement reduced their autonomy in clinical decision-making. Parkland practices escalated levels of responsibility based on the achievement of competencies under supervision. It is expected that the level of supervision will often decrease as the resident achieves additional competencies and progresses through residency. An objective measure to chart a resident’s progress would facilitate discussions on the appropriate levels of supervision between a resident and a supervising attending. While this could be achieved by keeping a personal log of procedures performed, the NoteWriter templated note system enables generation of resident-specific reports without additional effort on top of standard patient care.
The use of a templated note system is not new. It has been shown previously to improve documentation of patient comorbidities and complications, before the era of EHRs.31 With EHRs, templated notes have been shown to increase completion of advance directive discussion notes.32
With the previous system of documenting procedures in free text, consistency was lacking in the documentation of items such as the level of supervision, privilege to perform, etc. These procedural notes were also not easily auditable due to their free-text nature vs the coded system with templates and hard stops.
The feedback letters to the residents from the office of the GME were also useful, as they often led to discussions of opportunities for improvement in the process as well as feedback to the GME membership on standard practices. We experienced the greatest improvement in compliance after initiating this action. Residents seemed to appreciate the communication and took the opportunity to respond to the emailed letters frequently. It was this engagement that helped fine-tune the template. Not only was this benefit of great value, it had minimal impact on resources within the institution, averaging 0.83 letters per 100 residents weekly, using a templated letter. This was felt to be very tolerable by the GME staff.
Lastly, the use of templated notes along with our process of monitoring and providing feedback on compliance can allow for standardization of many other aspects of patient care that may be important to an organization, including regulatory items, graduate medical education, quality, or performance improvement. This system lends itself to all. The system we have described here can be easily implemented at any institution that utilizes an EHR platform with templated notes functionality. Keys to our success included extensive planning involving the various stakeholders, the availability of timely and comprehensive reports, and understanding the strengths and limitations of the EHR.
Limitations
This study was limited by the quality of data entered by resident physicians. While prompts and hard stops were put in place to ensure completion of the procedure note, there was nothing stopping residents from not documenting procedures at all. If a procedure was incorrectly documented as a note type other than “procedure” (eg, “progress note”), this would not be identified by the reporting system as an error. However, if the procedure was incorrectly documented in the traditional manner as a nontemplated, non–NoteWriter procedure note, the system would pick this up and flag the procedure as having been documented without using the template. This was the method used to calculate compliance with NoteWriter template usage (Figure 2A), which might be an underestimation of the true compliance.
Another limitation is that this system relies on the resident’s account of the procedure and the level of supervision required and received, thus reporting bias may occur. We feel that the residents are, by and large, honest in their documentation. Parkland uses a third-party product to capture resident procedure logs. Access to reports of residents’ proficiency in procedures is maintained outside the EMR via an intranet hyperlink from the hospital portal page. If a nurse or physician is unfamiliar with a particular resident’s qualifications, a quick online check will provide the necessary information. Likewise, the co-signing supervising physician would be able to identify any discrepancies between the level of supervision received and the level of supervision deemed necessary. There was also the possibility of errors in the assignment of the supervising physician by the resident. A countermeasure of these is that all procedure notes were sent to supervising attendings for co-signature. If misattributions were made, the co-signing attending would be made aware. While not foolproof, we believe that the additional layer of checks by forced co-signature would minimize errors and misattributions.
One may also find limit in that we implemented this templated standardized note in just one institution, and enforced it only in the inpatient aspect of patient care. While it was implemented in an enterprise fashion at our hospital, thus exposing a large variety of resident specialties to the experience, one cannot guarantee the same success when doing this at another institution. It should be mentioned, however, that we have begun to deploy this solution at our sister institution, the University of Texas Southwestern Medical Center, with similar initial success.
Future research directions
We have already begun to mandate compliance with this template for non–formal procedural area procedures in the ambulatory setting. This includes our standard process of working with the DIO to send letters to errant residents. The benefits of including this system in the formal procedural areas are being considered.
Finally, this templated procedural note system can also be implemented at other institutions with ease, especially if EpicCare is in use. Collaborating with other academic partners will provide external validity and may allow larger power for analysis of more subtle questions about supervision.
We hope to aim our future direction toward looking for hard outcomes in the use of this process.2 Specifically, we may look to see if there are any differences in patient outcomes, safety, quality, and overall patient satisfaction based on documented supervision by residents. The impact of this system on patient safety will need to be evaluated in a prospective manner.
ACKNOWLEDGMENTS
We would like to acknowledge and thank Corey Parker, Melissa Perry, and Julie Lively for their assistance through their roles in the Office of Graduate Medical Education, and Suzanne Truex for assistance with the figures.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sector.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
Study design: all authors
Data acquisition, interpretation, and analysis: V.S.B., C.M., B.M.
Drafting manuscript: V.S.B., B.M.
Critically revising manuscript: all authors
Approval of final manuscript for submission: all authors
Study supervision: B.M.
REFERENCES
- 1. Education ACfGM. Accreditation Council for Graduate Medical Education Common Program Requirements, 2013. https://www.acgme.org/acgmeweb/tabid/429/ProgramandInstitutionalAccreditation/CommonProgramRequirements.aspx. Accessed May 20, 2015. [Google Scholar]
- 2. Roth CP, Lim YW, Pevnick JM et al. . The challenge of measuring quality of care from the electronic health record. Am J Med Qual. 2009;245:385–394. [DOI] [PubMed] [Google Scholar]
- 3. Houston TK, Wall TC, Willet LL et al. . Can residents accurately abstract their own charts? Acad Med. 2009;843:391–395. [DOI] [PubMed] [Google Scholar]
- 4. Kennedy TJ, Regehr G, Baker GR et al. . Point-of-care assessment of medical trainee competence for independent clinical work. Acad Med. 2008;83(10 Suppl):S89–S92. [DOI] [PubMed] [Google Scholar]
- 5. Baldwin DC Jr, Daugherty SR, Ryan PM. How residents view their clinical supervision: a reanalysis of classic national survey data. J Graduate Med Educ. 2010;21:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Farnan JM, Johnson JK, Meltzer DO et al. . On-call supervision and resident autonomy: from micromanager to absentee attending. The Am J Med. 2009;1228:784–788. [DOI] [PubMed] [Google Scholar]
- 7. Durning SJ, Cation LJ, Jackson JL. Are commonly used resident measurements associated with procedural skills in internal medicine residency training? J Gen Intern Med. 2007;223:357–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patel MB, Guillamondegui OD, Ott MM et al. . O surgery case log data, where art thou? J Am College Surgeons. 2012;2153:427–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Salazar D, Schiff A, Mitchell E et al. . Variability in Accreditation Council for Graduate Medical Education Resident Case Log System practices among orthopaedic surgery residents. J Bone Joint Surgery Am vol. 2014;963:e22. [DOI] [PubMed] [Google Scholar]
- 10. Hanauer DA, Englesbe MJ, Cowan JA Jr et al. . Informatics and the American College of Surgeons National Surgical Quality Improvement Program: automated processes could replace manual record review. J Am College Surgeons. 2009;2081:37–41. [DOI] [PubMed] [Google Scholar]
- 11. Reason J. The contribution of latent human failures to the breakdown of complex systems. Philos Trans Royal Soc Lond, Biol Sci 1990;3271241:475–484. [DOI] [PubMed] [Google Scholar]
- 12. Reason J. Managing the Risks of Organizational Accidents. 1st ed. Ashgate Publishing Company, Farnham, Surrey, UK; 1997. [Google Scholar]
- 13. Whalen T, Wendel G.. Chapter 6—New Supervision Standards: Discussion and Justification. https://www.acgme.org/acgmeweb/Portals/0/PDFs/jgme-11-00-39-45[1].pdf. 2011. Accessed June 7, 2015. [Google Scholar]
- 14. Drolet BC, Soh IY, Shultz PA et al. . A thematic review of resident commentary on duty hours and supervision regulations. J Grad Med Educ. 2012;44:454–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jagannathan J, Vates GE, Pouratian N et al. . Impact of the Accreditation Council for Graduate Medical Education work-hour regulations on neurosurgical resident education and productivity. J Neurosurgery. 2009;1105:820–827. [DOI] [PubMed] [Google Scholar]
- 16. Blum AB, Shea S, Czeisler CA et al. . Implementing the 2009 Institute of Medicine recommendations on resident physician work hours, supervision, and safety. Nat Sci Sleep. 2011;3:47–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Borman KR, Fuhrman GM, Association Program Directors in Surgery. “Resident Duty Hours: Enhancing Sleep, Supervision, and Safety": response of the Association of Program Directors in Surgery to the December 2008 Report of the Institute of Medicine. Surgery. 2009;1463:420–427. [DOI] [PubMed] [Google Scholar]
- 18. Britt LD, Sachdeva AK, Healy GB et al. . Resident duty hours in surgery for ensuring patient safety, providing optimum resident education and training, and promoting resident well-being: a response from the American College of Surgeons to the Report of the Institute of Medicine, “Resident Duty Hours: Enhancing Sleep, Supervision, and Safety.” Surgery. 2009;1463:398–409. [DOI] [PubMed] [Google Scholar]
- 19. Lewis FR. Comment of the American Board of Surgery on the recommendations of the Institute of Medicine Report, “Resident Duty Hours: Enhancing Sleep, Supervision, and Safety." Surgery. 2009;1463:410–419. [DOI] [PubMed] [Google Scholar]
- 20. Ulmer C, Miller Wolman D, Johns MME, eds. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. National Academies Press: Washington, DC; 2009. [PubMed] [Google Scholar]
- 21. Simien C, Holt KD, Richter TH. The impact of ACGME work-hour reforms on the operative experience of fellows in surgical subspecialty programs. J Graduate Med Educ. 2011;31:111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Choma NN, Vasilevskis EE, Sponsler KC et al. . Effect of the ACGME 16-hour rule on efficiency and quality of care: duty hours 2.0. JAMA Int Med. 2013;1739:819–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ahmed N, Devitt KS, Keshet I et al. . A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;2596:1041–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vucicevic D, Mookadam F, Webb BJ et al. . The impact of 2011 ACGME duty hour restrictions on internal medicine resident workload and education. Adv Health Sci Educ Theory Practice. 2015;201:193–203. [DOI] [PubMed] [Google Scholar]
- 25. Levine WN, Spang RC 3rd. ACGME duty hour requirements: perceptions and impact on resident training and patient care. J Am Acad Orthopaedic Surgeons. 2014;229:535–544. [DOI] [PubMed] [Google Scholar]
- 26. De Oliveira GS Jr, Dexter F, Bialek JM et al. . Reliability and validity of assessing subspecialty level of faculty anesthesiologists' supervision of anesthesiology residents. Anesthesia Analgesia. 2015;1201:209–213. [DOI] [PubMed] [Google Scholar]
- 27. Haber LA, Lau CY, Sharpe BA et al. . Effects of increased overnight supervision on resident education, decision-making, and autonomy. J Hosp Med. 2012;78:606–610. [DOI] [PubMed] [Google Scholar]
- 28. Byrne JM, Kashner M, Gilman SC et al. . Measuring the intensity of resident supervision in the Department of Veterans Affairs: the resident supervision index. Acad Med. 2010;857:1171–1181. [DOI] [PubMed] [Google Scholar]
- 29. Reardon C, May M, Williams K. Psychiatry resident outpatient clinic supervision: how training directors are balancing patient care, education, and reimbursement. Acad Psychiatry. 2014;384:476–480. [DOI] [PubMed] [Google Scholar]
- 30. Brickner L, Clement M, Patton M. Resident supervision and the electronic medical record. Arch Intern Med. 2008;16810:1117–1118; author reply 8. [DOI] [PubMed] [Google Scholar]
- 31. Grogan EL, Speroff T, Deppen SA et al. . Improving documentation of patient acuity level using a progress note template. J Am College Surgeons. 2004;1993:468–475. [DOI] [PubMed] [Google Scholar]
- 32. Lindner SA, Davoren JB, Vollmer A et al. . An electronic medical record intervention increased nursing home advance directive orders and documentation. J Am Geriatrics Soc. 2007;557:1001–1006. [DOI] [PubMed] [Google Scholar]