Abstract
Objective: To describe current practices and stakeholder perspectives of patient portals in the acute care setting. We aimed to: (1) identify key features, (2) recognize challenges, (3) understand current practices for design, configuration, and use, and (4) propose new directions for investigation and innovation.
Materials and Methods: Mixed methods including surveys, interviews, focus groups, and site visits with stakeholders at leading academic medical centers. Thematic analyses to inform development of an explanatory model and recommendations.
Results: Site surveys were administered to 5 institutions. Thirty interviews/focus groups were conducted at 4 site visits that included a total of 84 participants. Ten themes regarding content and functionality, engagement and culture, and access and security were identified, from which an explanatory model of current practices was developed. Key features included clinical data, messaging, glossary, patient education, patient personalization and family engagement tools, and tiered displays. Four actionable recommendations were identified by group consensus.
Discussion: Design, development, and implementation of acute care patient portals should consider: (1) providing a single integrated experience across care settings, (2) humanizing the patient-clinician relationship via personalization tools, (3) providing equitable access, and (4) creating a clear organizational mission and strategy to achieve outcomes of interest.
Conclusion: Portals should provide a single integrated experience across the inpatient and ambulatory settings. Core functionality includes tools that facilitate communication, personalize the patient, and deliver education to advance safe, coordinated, and dignified patient-centered care. Our findings can be used to inform a “road map” for future work related to acute care patient portals.
Keywords: patient portal, patient-centered care, acute care, patient engagement
INTRODUCTION
Over the past 5 years, patient portals have been increasingly adopted by health care systems throughout the United States. The trend toward accelerated adoption of these patient engagement technologies is driven by a focus on safety and quality of care through patient-centered care, the “quantified-self” movement and consumer-health technologies, accountable care, online hospital and provider ratings, and online patient communities.1,2 Concurrently, Meaningful Use regulations have also motivated adoption of patient portals.3–5 To date, adoption and use of patient portals has largely been limited to the ambulatory setting: patients use these tools at home to review their health data (lab results, medications, etc.), schedule appointments, request prescription refills, pay bills, and communicate with providers.6 Increasingly, patients and caregivers are interested in accessing health information and communicating with providers during a hospital stay.7–9 However, current patient portals are not appropriately configured for use in the inpatient setting to support the dynamic and complex nature of hospital-based care.
BACKGROUND AND SIGNIFICANCE
Despite mixed results, emerging data support the use of patient-facing health information technology tools to deliver patient-centered care, foster health services efficiency, and improve clinical outcomes.10,11 Although hospitalized and ambulatory patients have some overlapping information and communication needs,9,12 the evidence regarding optimal use of inpatient engagement technologies is scarce.1 In a recent and comprehensive review, Prey et al.1 identified considerable gaps in knowledge and called for future research that focuses on defining optimal strategies for patient engagement using health information technology in the inpatient setting and rigorously evaluating the impact on health outcomes and cost-effectiveness.
Preliminary work suggests that hospitalized patients and/or designated caregivers can use acute care patient portals to seek educational content about medications and test results, and to communicate health concerns, needs, preferences, and questions directly to providers.9 However, a multitude of content and functionality design considerations and implementation challenges persist.9 Key considerations include clinician and administrator stakeholder engagement during design and implementation, use by health care proxies when patients are incapacitated, secure access, seamless data flow during care transitions (ie, to, from, and within the hospital), sustainability, and policies regarding access to mainstream social media tools and web browsing.13–15
Objective
Given the dearth of published findings, we sought to describe current practices and stakeholder perspectives to identify requirements for patient portals in the acute care setting. Specifically, we aimed to: (1) identify key features in common and different across sites, (2) recognize operational and implementation challenges, (3) understand current practices for design, configuration, and use, and (4) propose new directions for investigation and innovation specific to the acute care setting.
MATERIALS AND METHODS
Study design
We employed mixed methods consisting of an electronic survey administered at baseline, and semistructured interviews and focus groups conducted at site visits. Using purposeful sampling, we identified 5 academic medical centers (AMCs) in the United States that were actively designing, developing, implementing, and evaluating patient portals in the acute care setting. Four were identified through the Libretto Consortium, a collaboration of AMCs established by the Gordon and Betty Moore Foundation with a goal of reengineering the critical care setting to facilitate patient engagement, reduce preventable harm, and ensure dignity and respect for patients and family members. The fifth site was identified through a published systematic review.1 Organizations that were implementing existing patient portal technology in the acute care setting without evaluating design, development, or implementation were excluded. Institutional Review Board approval was received from Partners Healthcare Systems, the primary research site, and from each institution that participated in on-site visits. Informed by prior work,1,9 we defined an acute care patient portal as follows: “a patient-facing technology that provides hospitalized patients and care partners secure, online access to personalized health information in order to engage in their care.”
DATA COLLECTION
To assess the current state of acute care patient portals, we used an iterative process to modify a semistructured survey capturing key features, policies, and usage statistics that was previously used for ambulatory patient portals.12,16 The survey topics included use, leadership, access, features and functionalities, educational content, messaging, patient/caregiver input, data access, policies, challenges, and visions and goals. The survey was administered using REDCap.17 A link to the confidential survey was emailed to an identified stakeholder and expert leader for the acute care patient portal at each site. The site representatives volunteered to complete the survey for topics on which they were the site expert, and to seek survey responses from other experts at their site for remaining topics. Site stakeholders included patient and family advisory council (PFAC) members (including actual patient portal users), clinician leaders, policymakers and administrators, information system (IS) leaders, and researchers. Variation in the PFAC member experience of portals was desired in order to better understand the breadth of patient and family perspectives and needs.
We used results from this survey to inform development of semistructured interview/focus group guides and to identify targeted stakeholder groups to participate in interviews and focus groups. The final semistructured guides included questions about clinical content and functionality, personalization and social media tools, messaging tools, patient and caregiver access, “bring your own device” (BYOD) options, policies and decision-making, security and technical architecture, infection control, enrollment procedures for patients and health care proxies, engagement and use, and barriers to and facilitators of implementation (see Online Appendix 1). Data was collected in person during site visits or remotely via video/conference calls when site visits were not feasible; these sessions included a demonstration of the acute care patient portal. Whenever possible, focus groups were conducted with all identified representatives from each stakeholder group. Interviews were conducted when there was only 1 representative from the stakeholder group or when group schedules could not be coordinated. Member checks were performed and recorded throughout the interviews/focus groups to confirm that interpretation of statements and results was consistent with participants’ intended meaning.
Quantitative and qualitative analysis
Surveys: Data from surveys were analyzed using Microsoft Excel and presented quantitatively and descriptively.
Identification of Themes: Focus groups and interviews were recorded and transcribed verbatim. Content was imported into NVivo (version 10) for thematic analysis.18–20 The thematic coding process involved 3 steps: (1) coding of individual transcripts by 2 research team members, emphasizing the focus areas identified from the survey results; (2) team meetings to review coding, arrive at a consensus for major codes, and group major codes into themes by stakeholder group and focus area; and (3) team meetings to identify and reach consensus on thematic variation across sites and stakeholder groups, as well as the main themes from the data.20 Themes that emerged from 2 or more stakeholder groups were identified as being common across stakeholder groups (see Tables 2 and 3).
Table 2.
Themes derived from stakeholder interviews and focus groups; perspectives by common category across stakeholder groups
| Category | Theme |
|---|---|
| Access and Security | 1. Access should be seamless across ambulatory and inpatient settings. |
| 2. Most policies and strategies are borrowed from ambulatory portals. | |
| 3. Security concerns exist for health proxy access, access outside of hospital, and “bring your own device” solutions. | |
| Content and Functionality | 4. Look and feel of content and functionality should be seamless across settings. |
| 5. Multimedia personalization tools may humanize the patient and enhance patient and family connection with the care team. | |
| 6. Educational content should be tailored to the patient’s clinical state. | |
| 7. Displays should be simple and intuitive, with tiered options available for more detailed clinical information as desired. | |
| Engagement and Culture | 8. Stakeholder buy-in is needed during design/development and for setting end-user expectations. |
| 9. Dedicated teams are needed for patient/family enrollment and coaching to increase awareness, facilitate software development and vendor collaboration, and involve clinical governance and leadership. | |
| 10. Clinicians should be actively engaged in using the portal with patients. | |
| 11. A hospital culture of patient-centered innovations may facilitate adoption among providers. |
Table 3.
Themes derived from stakeholder interviews and focus groups; perspectives by stakeholder group
| Stakeholder group | Theme |
|---|---|
| Patients and Families | 1. Access to clinical information, personal notepad, and educational materials is highly valued. |
| 2. Portal should enhance, not replace, in-person communication with the care team. | |
| Clinician Leaders | 3. Appropriate timing for staff to introduce the portal to patients and providing flexible access are critical, because ICU patients are sick and families may be in a state of crisis. |
| 4. Increased documentation requirements, staffing demands, and training resources need to be resolved to support effective adoption by clinicians. | |
| 5. Nursing staff caring for vulnerable populations may have concerns about identifying information being shared on the portal, requiring collaborative agreements such as only first name and photo will be used. | |
| Policymakers and Administrators | 6. Need to promote equitable access to address the “digital divide." |
| Information Systems Leaders | 7. Web-based mobile platforms are ideal with a database architecture that can support real-time data display. |
| 8. Use of standards facilitates integration with the EHR, but read-only access from the EHR is limiting. | |
| Researchers | 9. Pilot testing to refine communication technologies, such as messaging workflows and video-conferencing, is needed. |
| 10. Demonstration of impact on clinical outcomes is essential to sustain clinical staff engagement during and after pilot stages of investigation. |
Development of explanatory model and actionable recommendations
Emergent themes were incorporated into an explanatory model of current practices and experiences that focused on concepts and processes for development and implementation of acute care patient portals. Group sessions were held to refine the model, reach consensus on the final versions, and identify actionable recommendations based upon a synthesis of themes and the explanatory model.
Validation of findings
Identified themes, the explanatory model, and actionable recommendations were presented at an annual meeting to PFAC, clinical, policy/administrative, IS, and research stakeholders representing Libretto sites to confirm that interpretation of results was consistent with participants’ intended meaning. Uncertainties or disagreements were resolved by consensus discussion among the key stakeholders.
RESULTS
Data from surveys, interviews, and focus groups
Five AMCs participated in the survey (Table 1). A single survey was completed by the primary site representative and up to 5 additional experts at each of the 5 sites (response rate 100%). From surveys, 5 groups were identified as key operational leaders and/or stakeholders of the patient portal: PFAC members, clinician leaders, policymakers and administrators, IS leaders, and researchers. Clinician leaders included clinical directors as well as staff nurses and physicians who actively provided patient care; they were identified from existing shared governance infrastructure, including clinical practice councils and leadership groups at each site.
Table 1.
Baseline Survey: Overview of Participating Sites
| Site A | Site B | Site C | Site D | Site E | |
|---|---|---|---|---|---|
| Total number of beds | 793 | 650 | 720 | 1031 | 2478 |
| Geographic location | Northeast | Northeast | West Coast | Mid-Atlantic | Northeast |
| Logistics and Accessibility of Institutional Patient Portal(s) | |||||
| Currently has ambulatory patient portal? | ✓ | ✓ | ✓ | ✓ | ✓ |
| Status of acute care patient portal | Implemented | In development | Implemented | Implemented | Implemented |
| Is acute care patient portal integrated with ambulatory patient portal? | X | X | X | X | ✓ |
| Acute Care Patient Portal Functionality (see above for status of Implemented or In development) | |||||
| Available in 1 or more inpatient units/populations | ✓ | N/A | ✓ | ✓ | ✓ |
| Access to clinical data | ✓ | X | ✓ | X | ✓ |
| Access outside of hospital | X | ✓ | X | X | X |
| Multiple stakeholders responsible for different aspects of portal (eg, content, security, policies) | ✓ | ✓ | ✓ | X | ✓ |
| Access in critical care setting | ✓ | ✓ | ✓ | ✓ | ✓ |
| Access in noncritical care setting | ✓ | X | ✓ | X | ✓ |
Key: ✓ = yes; X = no; N/A = not applicable since the system is still in development.
Four of the 5 sites that participated in the survey also participated in focus groups and interviews. A total of 84 individuals participated in 12 interviews and 18 focus groups (ranging from 3 to 11 participants) that were conducted across these 4 sites. On average, 3.3 ± 2.6 PFAC members, 4.5 ± 3.7 researchers, 3.8 ± 1.9 IS leaders, 6.0 ± 3.6 clinical leaders, and 3.5 ± 1.3 policymakers/administrators participated in interviews or focus groups across the 4 organizations. Approximately half of the PFAC participants were current or past users of patient portals. Thirty transcripts were transcribed from a total 21 hours (1245 minutes) of audio recording. On average, 5 hours (311 minutes) of audio was transcribed per site. The fifth site (Site E) did not participate in focus groups or interviews due to study time constraints.
Themes, facilitators, and barriers identified from stakeholders’ perspective
We identified a total of 21 themes (see Tables 2 and 3) from stakeholder interviews and focus groups: 11 themes in 3 categories common across 2 or more stakeholder groups (Table 2), and 10 themes by 5 stakeholder groups (Table 3). We identified 10 main facilitators and 7 major barriers (Table 4) for the design, configuration, implementation, adoption, and use of acute care patient portals.
Table 4.
Key facilitators of and barriers to design, configuration, implementation, adoption, and use of acute care patient portals identified from stakeholders’ perspective
| Facilitators |
| 1. Patient-centric paradigm shift |
| 2. Human factors engineering design processes with end users |
| 3. Demonstration of improved clinical outcomes |
| 4. Dedicated clinical task force |
| 5. Coaching and awareness efforts |
| 6. Setting end-user expectations |
| 7. Prior sociotechnical innovations |
| 8. An existing ambulatory portal |
| 9. Hybrid device management approach (hospital-issued devices and BYOD) |
| 10. Funding for research |
| Barriers |
| 1. Cultural shift required for use of messaging and personalization tools |
| 2. Clinician effort required to collect new types of data |
| 3. Lack of resources and time for training |
| 4. Care team identification resistance from nurses |
| 5. Environmental constraints on BYOD devices |
| 6. Security concerns for family access and access outside hospital |
| 7. EHR and technical architecture constraints |
Highlighted Themes by Common Category across Stakeholder Group Perspectives
Representative themes from each category are presented here. These themes were used to inform development of the explanatory model of current practices and experiences (described below).
Access and Security
One of the most common perspectives identified across stakeholder groups was that a patient portal should be easily accessible across the inpatient and ambulatory settings (Theme 1, Table 2). Several sites discussed the need for a road map for an integrated network patient portal that would provide seamless access across settings. With regard to policies for health care proxy access, most sites borrowed policies from ambulatory portals (Theme 2, Table 2; Figure 2). Furthermore, participants identified provision of ubiquitous access for designated family caregivers from any location and a BYOD strategy as critical factors for adoption and use (Figure 1). Nonetheless, they suggested that patient portals configured for a BYOD strategy and flexible access must still consider all health data security requirements and environmental constraints (Figure 2), such as wireless guest network access, account setup, and authentication procedures (Theme 3, Table 2). Navigating episodic health care proxy access was thought to be complex and would require more advanced security and policy considerations than those typically required in the ambulatory setting.
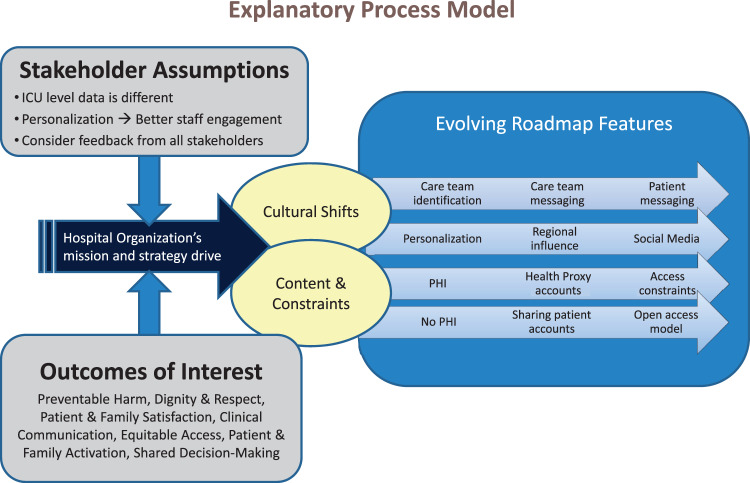
Figure 2.
Process model: development and implementation of acute care patient portals.
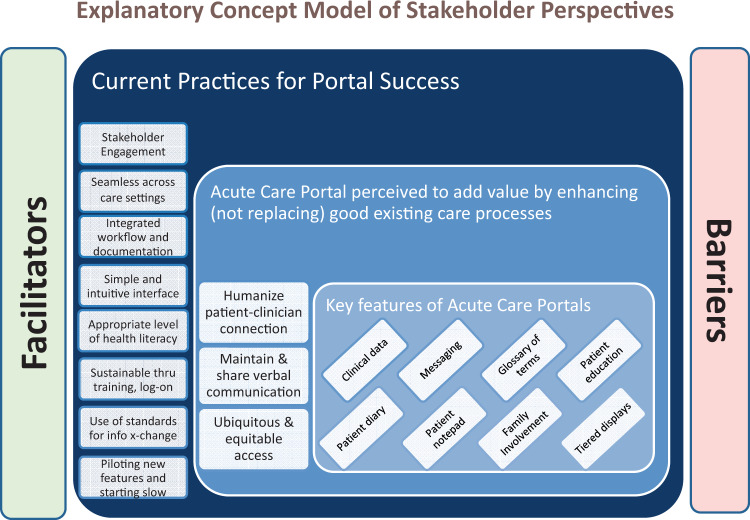
Figure 1.
Concept model: current practices of acute care patient portals.
Content and Functionality
Aligned with the theme of integrated access, the look and feel of the portal’s content and functionality should be consistent across all care settings (Theme 4, Table 2): “Anything done inpatient [on the portal] shouldn’t be any different than what you see in an outpatient [portal].” Participants identified personalization tools, such as functionality to identify hobbies, post photographs, and link to social media accounts, as an important way to humanize the patient-clinician connection in the acute care setting (Theme 5, Table 2; Figure 1). Concerns regarding the use and security of social media were common across stakeholder groups and sites, but were not adequately addressed. Specifically, perspectives regarding the appropriateness and security risks of providing social media access on hospital-issued devices varied widely across sites (Figure 2). Our data indicated that access to social media accounts was favored on the West Coast, in line with patient expectations. Finally, the construction and layout of patient rooms also influenced the appropriateness of types of content that were displayed (Barrier 5, Table 4). For example, single rooms afford more privacy, and thus would be more amenable to the display of personal information, digital photo sharing, and video-conferencing, particularly if a television in the room was used for portal access.
Other important functionality included tailored educational content based on health literacy levels and tiered information display options for patients and family caregivers who desire access to richer clinical data (Themes 6 and 7, Table 2; Figure 1). While content across study sites was provided at a 4th-to-8th-grade reading level, none of the portals included tools that screened for health literacy to enable tailored comprehension of content. Simple, intuitive, and tiered information displays and barcoding technology to facilitate ease of account setup and login were thought to enhance comprehension and usability while minimizing required training (Theme 4, Table 3; Figure 1).
Engagement and Culture
Participants generally felt that a dedicated clinical task force to facilitate key aspects of design and implementation would serve as a form of governance to actively engage clinical staff in using the portal with patients and families (Themes 8–11, Table 2). Aligning with a cultural shift from a traditional clinician-centric to a patient-centric view of hospitalized care, the clinical task force would help prepare the acute care setting for integration of the patient portal into clinical practice (Theme 9, Table 2; Figure 2).
Highlighted Themes by Stakeholder Group Perspective
Patients and Families
Patients and family stakeholders emphasized the critical value of access to clinical information, a personal notepad, and educational materials (Theme 1, Table 3; Figure 1). Furthermore, while they believed that the intent was not to replace in-person communication between patients, family members, and care team members (Theme 2, Table 3), they suggested that the patient portal could add value by facilitating verbal communication (see Figure 1), for example about patient goals, preferences, expectations, and priorities for care.
Clinician Leaders
Because hospitalized patients, particularly those in critical care settings, tend to be sick and family members are often in a state of crisis, clinical leaders suggested that patients and family caregivers would need time to acclimate before accessing tools and resources in the portal (Theme 3 and Table 3). They highlighted the need to balance expected benefits to patients and family caregivers with the increased workload placed upon clinical staff; the patient portal “needs to be built into what we (clinicians) do 100% of the time” (Facilitators 2, 3, and 6, Table 4; Figure 1). For example, additional clinician effort would be required to collect and review new types of data (eg, daily goals) that previously may not have been part of the formal patient record (Barrier 2, Table 4). Finally, they suggested that documentation must be streamlined and integrated with the EHR, because clinicians would “refuse to double document” (Theme 4, Table 3; Figure 1).
Several nursing stakeholders expressed concern about displaying nurses’ names and pictures on the patient portal. For example, at 1 site trauma nurses felt vulnerable, given that their patient population included many victims of violent crimes (Barrier 4, Table 4). To address these concerns while maintaining functionality to identify clinicians for messaging and personalization tools, clinical leaders established a policy that would allow nurses’ first names and photographs on the portal, but not their last names (Theme 5, Table 3; Figure 2).
Policymakers and Administrators
Administrators and policymakers suggested that, given the potential benefits for patients and families/care partners, institutions would have a moral responsibility to promote equitable access to all patients and address the digital divide (Theme 6, Table 3; Figure 1). For example, one administrator commented that “there’s just no one size fits all. I think we have to build our strategies based on certain patient characteristics.” Most agreed that a hybrid device management approach that enables patients to use their own device whenever possible (BYOD strategy) and offers hospital-provisioned devices to patients without a personal device would be ideal (Facilitator 9, Table 4).
Information Systems Leaders
A thorough analysis of requirements to inform the best technical approaches for design and development was thought to be essential. Typically, this analysis would consider the use of third-party vendors, interoperability standards, web-based and mobile platforms, and database architecture approaches that support real-time display (Themes 7 and 8, Table 3; Figure 1). Use of open application programming interfaces for integration and innovative development was a key consideration, but there was concern that some EHRs prevent the storage of data from external applications (Barrier 7, Table 4; Figure 2).
Researchers
Use of patient-clinician messaging and personalization tools was considered potentially disruptive in the hospital environment and represented a cultural shift for clinical staff. Participants voiced the importance of delineating clear expectations for use and evaluating smoother workflows (Theme 9, Table 3 and Barrier 1, Table 4; Figure 2). Funding to enable robust investigation of patient portals by using prospective data-collection techniques, leveraging human factors engineering methods, pilot testing novel features, and linking to outcomes data was also considered important (Theme 10, Table 3 and Facilitators 3 and 10, Table 4; Figure 1).
Explanatory Model
Acute care patient portal explanatory model: concepts of current practices and process of development and implementation experiences
Based on the themes, facilitators, and barriers identified above, we constructed an explanatory model for acute care patient portals. The overall structure and linkages between concepts were informed by the key thematic categories. The specific concepts in the model correspond to individual themes. The explanatory model comprises 2 components: (1) a conceptual model that identifies key and value-added features and synthesizes current practices for successful design, implementation, adoption, and use from the stakeholder perspective (Figure 1); and (2) a process model that explains how stakeholder assumptions and outcomes of interest may influence the hospital mission and strategy for acute care patient portals, drive cultural shift and content, and ultimately impact the evolution of key and value-added features (Figure 2).
As depicted in the concept model (Figure 1, middle box), acute care patient portals can enhance existing care processes by humanizing the clinician-patient connection, maintaining and sharing verbal communication, and providing ubiquitous and equitable access. The 8 key features of an acute care patient portal (Figure 1, smallest box) that are perceived to add value to existing care processes to enable success are: (1) access to clinical data, (2) messaging, (3) glossary of terms, (4) patient education, (5) patient diary, (6) patient notepad, (7) tools to encourage family involvement in care, and (8) tiered displays (Figure 1).
As depicted in the process model (Figure 2) for development and implementation, we identified 3 untested assumptions that appeared to have influenced the acute care patient portal mission and strategy at each hospital: (1) ICU-level data are different, requiring filtered data displays (ie, ICU data vs non-ICU data), (2) personalization tools will increase staff engagement, and (3) design and implementation efforts should consider and incorporate feedback from all stakeholders (Figure 2). Although there was substantial overlap in the outcomes of interest across sites, we observed variation in the preferred primary outcome that drove evolution of key features at individual sites. For example, an emphasis on patient dignity and respect at one site, per stakeholder perspective, influenced the development of personalization tools and a decision to exclude protected health information (PHI); exclusion of PHI was thought to enable sharing of accounts among family members. An emphasis on improving clinical communication and care plan concordance at another site, per stakeholder perspective, led to more robust implementation of care team identification functionality to support patient-centered messaging and the inclusion of PHI to enable display of the plan of care for patients and family caregivers. Because the inclusion of PHI required separate health care proxy accounts, patients and caregivers at this site were perceived to have encountered greater barriers to access the portal than at sites that did not provide access to PHI.
DISCUSSION
Our aim was to describe stakeholder perspectives and current practices for acute care patient portals at early-adopter institutions. The most important theme that emerged was that patients want a unified and seamless experience across care settings, acknowledging that content, data, and specific features will differ from the ambulatory setting. We analyzed major themes, facilitators, and barriers, and developed an explanatory model from which we offer an initial set of actionable recommendations to guide future design, development, implementation, and research efforts related to acute care patient portals. Providing a single integrated experience across settings was the most important actionable recommendation. Other actionable recommendations were: (1) incorporating personalization tools to humanize the patient experience, (2) minimizing health care disparities by ensuring equitable access, and (3) strategically aligning the acute care patient portal with the overall mission of the hospital while continuing to test stakeholders’ assumptions for design, development, and implementation. We anticipate that these early recommendations will evolve as the field matures.
Our results represent an early consensus perspective of a diverse group of patient advocates, health care professionals, policymakers and administrators, information system personnel, and researchers affiliated with leading academic medical centers engaged in innovation and research to improve delivery of patient-centered care in the hospital setting. As such, they emphasize current features of acute care patient portals and mechanisms by which these features are perceived to add value to existing care processes, helping hospitals achieve desired patient-centered outcomes. Furthermore, the results reflect the fact that acute care patient portals at each institution are in various stages of development, implementation, and evaluation, and that individual stakeholder participants are engaged in a variety of activities directly and/or indirectly related to patient portals. Finally, most participants in this study are members of the Libretto Consortium and actively collaborate with other members as part of consortium activities regarding various aspects of acute care patient portal design, development, and implementation, predominantly in the critical care setting.
The increasingly prevalent requirement that clinicians should have a seamless experience accessing patient data across care settings has motivated health care organizations to make significant investments in system-wide EHRs.21 Similarly, we learned that patients and caregivers desire a seamless experience accessing and interacting with content and features via the patient portal regardless of location: patients should be able to use a single log-on to access clinical information about inpatient and ambulatory encounters, and the “look and feel” of the portal must seem equally familiar. In short, acute care patient portals should not become “information islands,” as has been reported for ambulatory patient portals.22 Many participants expressed concern regarding the level to which an acutely ill patient or a preoccupied caregiver would engage in using the patient portal when attempting to access and navigate an unfamiliar online environment. These concerns align with the ambulatory literature indicating that personal factors (eg, age, ethnicity, education level, health literacy, health status, and role as caregiver), provider endorsement, and usability influence engagement with patient portals.22–24
Enhancing the patient-clinician relationship and the concept of “knowing the patient” has been well studied in the nursing literature as an essential precursor to the delivery of high-quality patient care.25,26 Patients and their family caregivers are key sources of information that nurses rely on to obtain information, but families are not always present and patients are not always able to communicate.26 Personalization tools offer a unique opportunity to operationalize the concept of knowing the patient. This technology-driven approach is a potentially powerful way for care team members, including non-unit-based clinicians (eg, consultants who are mobile and wish to work remotely), to humanize their connections with patients. Also, the variation in use of multimedia and social media tools for personalization that we observed across sites indicates the need to better understand the role of such tools during hospitalization, and how best to securely integrate external applications with acute care patient portals. Nonetheless, requirements for ubiquitous access and personalization raise novel policy, security, and device concerns that could directly impact patient and health care proxy access, and may be handled differently at various institutions. While these concerns are novel and represent unexplored layers of complexity in the acute care setting, they are an extension of important concerns addressed in the ambulatory literature, including care partner and proxy access and use of electronic signatures.22,27
Patients and their family caregivers are rapidly becoming more technologically savvy. Nonetheless, hospitals are unfamiliar and isolating places, and patients feel disempowered, particularly when access to their information is limited.1 Furthermore, disparities exist among patients who have and do not have access to smart mobile devices, and those who have high versus low levels of eHealth literacy.28 To bridge the digital divide and minimize health care disparities, stakeholder participants unanimously agreed to provide hospital-issued devices to ensure equitable access to the acute care patient portal. Prior work on ambulatory portals also addresses the need to overcome racial, ethnic, and literacy barriers in order to enable broad adoption and equitable access.24,29
Recent studies support the use of patient educational tools within acute care patient portals, and these tools must be configured for a general health literacy level.9,14 Tools to assess eHealth literacy are promising,28,30 but these were notably absent from the portals that we investigated. Our prior review of health literacy screening instruments suggests that a single question may be a reliable, valid, and feasible means of establishing health literacy.28 Such screening and tools could be leveraged to tailor content specific to patients’ eHealth literacy levels within the acute care patient portal.
As Prey et al.’s1 systematic review suggests, hospitals are unfamiliar, isolating places and patients are in disempowering situations, often with limited (if any) access to their information. We found that sites viewed the acute care patient portal as a platform to enable more effective patient and family empowerment and engagement. We learned that an awareness of the need to provide safe, patient-centered care within the hospital influenced how individual institutions identified the types of outcomes that could be positively impacted by acute care patient portals. An outcomes-focused approach is critical to motivating clinical staff to actively engage with patients and families in using the portal, and should advance the evidence base for inpatient engagement technologies, including impact on specific health outcomes and cost-effectiveness.1 For example, in the ambulatory setting, patient portals are associated with improved medication adherence,31,32 and higher overall activation by patients is associated with better clinical indicators, healthy behaviors, and greater use of preventive services.33 These findings support continued development and investigation to address the knowledge gaps regarding the potential impact of ambulatory and acute care patient portals on clinical outcomes.
We learned that the use of human factors engineering methods is essential to test design and implementation assumptions. Novel features (eg, personalization, goal identification, messaging, etc.) implemented with the intent to improve patient safety, satisfaction, care coordination, and decision-making require formal usability and outcomes evaluation, and this remains a need for both ambulatory and acute care patient portals.32 Finally, health care organizations should reflect on their missions and strategies as they implement these portals, and should consider the link between specific features and clinical outcomes to better understand the potential impact of these features across care settings. We identified that conducting pilot studies is perceived as a successful strategy to test new features, evaluate usability, and assess potential financial and organizational impact.22
Limitations
Our sample size is small and limited to academic medical centers that were identified through the Libretto Consortium. As such, our findings are limited to the early work of these and potentially similarly pioneering institutions; they reflect current practices and opinions that are felt to be successful at each site, gathered using a mixed-methods approach. Furthermore, we acknowledge that the academic medical centers included in this study do not represent all types of facilities in which most people are hospitalized. Nevertheless, because few institutions (academic or non-academic) are actively designing, developing, and implementing acute care patient portals, our findings are noteworthy. An additional weakness was that all the organizations were large integrated-delivery systems with complex operations, which would have the resources needed to integrate acute care patient portals. Another weakness is the inability to contrast any of these findings with information from organizations that were unsuccessful or less successful. Therefore, generalizability of our findings may be limited to these types of institutions. Although we do not provide an analysis of how specific patient populations use portals when hospitalized (ie, medical vs surgical patients), our observations are representative of the spectrum of acute care at these hospitals (eg, 3 of the 5 institutions in our study were involved in efforts in both critical and noncritical care settings). Nonetheless, we acknowledge the limited generalizability and early nature of our findings in this rapidly evolving field. Finally, despite our extensive data-collection efforts and rigorous qualitative analyses, our findings are not exhaustive; they more than likely underscore considerable challenges to design and development and barriers to implementation and adoption as perceived by stakeholder participants.
CONCLUSION
Acute care patient portals are in still in their infancy, but a number of lessons emerged; most notably, patients want access to a single patient portal across care settings. We identify a number of emerging features and describe current practices that could inform the design, configuration, and use of patient portals in the inpatient setting. Based on these early findings, our most notable recommendation is that portal design, development, and implementation should focus on creating a single experience that includes a core set of novel features to humanize patient-clinician relationships and advance safe, coordinated, and dignified patient-centered care. Further qualitative and quantitative research should build upon these concepts, enhance the themes we identified, refine the models we proposed, test design assumptions, and measure the impact on outcomes.
ACKNOWLEDGMENTS
We thank many members of the Libretto Consortium who have contributed in various ways to this work. The authors also thank the many people who agreed to participate in this study.
FUNDING
This work was supported by the Libretto Consortium, which is funded by the Gordon and Betty Moore Foundation, grant number 4609.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTOR
All authors have contributed sufficiently and meaningfully to the conception, design, and conduct of the study; data acquisition, analysis, and interpretation; and/or drafting, editing, and revising the manuscript.
REFERENCES
- 1. Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc. 2014;21:742–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rozenblum R, Miller P, Pearson D, et al. Patient-centered healthcare, patient engagement and health information technology: the perfect storm. In: Grando M, Rozenblum R, Bates D, eds. Information Technology for Patient Empowerment in Healthcare. Berlin: Walter de Gruyter Inc.; 2015:3–22. [Google Scholar]
- 3. Bitton A, Poku M, Bates DW. Policy context and considerations for patient engagement with health information technology. In: Grando MA, Rozenblum R, Bates DW, eds. Information Technology for Patient Empowerment in Healthcare. Berlin: Walter de Gruyter Inc.; 2015:75–90. [Google Scholar]
- 4. Wells S, Rozenblum R, Park A, et al. Personal health records for patients with chronic disease: a major opportunity. Appl Clin Inform. 2014;23:416–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wells S, Rozenblum R, Park A, et al. Organizational strategies for promoting patient and provider uptake of personal health records. J Am Med Inform Assoc. 2015;22:213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Collins SA, Vawdrey DK, Kukafka R, et al. Policies for patient access to clinical data via PHRs: current state and recommendations. J Am Med Inform Assoc. 2011;18 (Suppl 1):i2–i7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dykes PC, Carroll DL, Hurley AC, et al. Building and testing a patient-centric electronic bedside communication center. J Gerontol Nurs. 2013;39:15–19. [DOI] [PubMed] [Google Scholar]
- 8. Caligtan C a, Carroll DL, Hurley AC, et al. Bedside information technology to support patient-centered care. IJMI 2012;81:442–451. [DOI] [PubMed] [Google Scholar]
- 9. Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluation. J Am Med Inform Assoc. Published online first: August 2, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood) 2013;32:207–214. [DOI] [PubMed] [Google Scholar]
- 11. Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients’ ‘scores.’ Health Aff (Millwood). 2013;32:216–222. [DOI] [PubMed] [Google Scholar]
- 12. Collins S, Vawdrey DK, Kukafka R, et al. Policies for patient access to clinical data via PHRs: current state and recommendations. J Am Med Inform Assoc. 2011;18:i2–i7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vawdrey DK, Wilcox LG, Collins SA, et al. A tablet computer application for patients to participate in their hospital care. In: AMIA Ann Symp Proc. 2011;1428–1435. [PMC free article] [PubMed] [Google Scholar]
- 14. Collins S, Gazarian P, Stade D, et al. Clinical workflow observations to identify opportunities for nurses, physicians and patients to share a patient-centered plan of care. In: AMIA Ann Symp Proc. 2014;414–423. [PMC free article] [PubMed] [Google Scholar]
- 15. Dykes P, Stade D, Chang F, et al. Participatory design and development of a patient-centered toolkit to engage hospitalized patients and care partners in their plan of care. In: AMIA Ann Symp Proc. 2014;486–495. [PMC free article] [PubMed] [Google Scholar]
- 16. Leung W, Collins S, Dalal A. Developing an electronic survey to capture current state of acute care patient portals to inform best practices and future directions. Poster Presentation at American Medical Informatics Association Annual Fall Symposium; 2015 Nov 15–18; San Francisco, CA.
- 17. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Joffe H, Yardley L. Content and thematic analysis. In: Marks D, Yardley L, eds. Research Methods for Clinical and Health Psychology. London, UK: SAGE Publications; 2004:248. [Google Scholar]
- 19. Welsh E. Dealing with data: using NVivo in the qualitative data analysis process [12 paragraphs]. Forum Qual. Sozialforsch/Forum Qual Soc Res 2002;32 Retrieved May 20, 2016 from http://www.qualitative-research.net/index.php/fqs/article/view/865/1881. Accessed May 20, 2016. [Google Scholar]
- 20. Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2008;5:80–92. [Google Scholar]
- 21. Payne TH, Corley S, Cullen TA, et al. Report of the AMIA EHR-2020 Task Force on the status and future direction of EHRs. J Am Med Inform Assoc. 2015;22:1102–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Otte-Trojel T, de Bont A, Rundall TG, et al. What do we know about developing patient portals? a systematic literature review. J Am Med Inform Assoc. Published online first: September 2, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Irizarry T, DeVito Dabbs A, Curran CR. Patient Portals and Patient Engagement: A State of the Science Review. J Med Internet Res. 2015;17:e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smith SG, O’Conor R, Aitken W, et al. Disparities in registration and use of an online patient portal among older adults: findings from the LitCog cohort. J Am Med Inform Assoc. 2015;22:888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zolnierek CD. An integrative review of knowing the patient. J Nurs Scholarsh. 2014;46:3–10. [DOI] [PubMed] [Google Scholar]
- 26. Kelley T, Docherty S, Brandon D. Information needed to support knowing the patient. ANS Adv Nurs Sci. 2013;36:351–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sarkar U, Bates DW. Care partners and online patient portals. JAMA. 2014;311:357–358. [DOI] [PubMed] [Google Scholar]
- 28. Collins S, Currie L, Bakken S, et al. Health literacy screening instruments for eHealth applications: a systematic review. JBI. 2012;45:598–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159:677–687. [DOI] [PubMed] [Google Scholar]
- 30. Collins SA, Yoon S, Rockoff ML, et al. Digital divide and information needs for improving family support among the poor and underserved. Health Informatics J. Published online first: June 15, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wright E, Darer J, Tang X, et al. Sharing physician notes through an electronic portal is associated with improved medication adherence: quasi-experimental study. J Med Internet Res. 2015;17:e226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17:e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Greene J, Hibbard JH, Sacks R, et al. When patient activation levels change, health outcomes and costs change, too. Health Aff (Millwood). 2015;34:431–437. [DOI] [PubMed] [Google Scholar]