Abstract
We examined the acceptability and effects of delivering doctors’ visit notes electronically (via OpenNotes) to patients and care partners with authorized access to patients’ electronic medical records. Adult patients and care partners at Geisinger Health System were surveyed at baseline and after 12 months of exposure to OpenNotes. Reporting on care partner access to OpenNotes, patients and care partners stated that they had better agreement about patient treatment plans and more productive discussions about their care. At follow-up, patients were more confident in their ability to manage their health, felt better prepared for office visits, and reported understanding their care better than at baseline. Care partners were more likely to access and use patient portal functionality and reported improved communication with patients’ providers at follow-up. Our findings suggest that offering patients and care partners access to doctors’ notes is acceptable and improves communication and patients’ confidence in managing their care.
Keywords: health information technology, electronic health records, consumer health information, care partner
BACKGROUND AND SIGNIFICANCE
A provider-sponsored patient portal can be instrumental in efforts to engage patients and families in care.1,2 Several studies have examined factors affecting patients’ use of such portals3–5 and patients perspectives regarding privacy and control of their health information.6–8 Family members and friends are frequently involved in the care of patients who are more vulnerable9–11 and may facilitate access and use of a patient portal.12–14 However, the longitudinal experiences of patients and families who share formal access to a patient’s portal account has, to our knowledge, not been examined.
In an initial demonstration and evaluation of OpenNotes,1,15 nearly 9,000 Geisinger Health System (GHS) patients were invited to read doctors’ electronic visit notes through the patient portal. Many reported informally sharing visit notes with family members or friends1 or that they desired family member or friends to have their own access to visit notes.16 However, patients who formally authorized a family member or friend “care partner” to share access to their portal account were excluded from the initial OpenNotes study. Therefore, we undertook this study to examine patients’ and care partners’ perceptions of OpenNotes, confidence in managing aspects of patient care, and online practices after 12 months of exposure to the intervention.
METHODS
GHS, an integrated health system in central Pennsylvania, has offered patients access to a portal, MyGeisinger, since 2001. MyGeisinger has afforded patients the ability to share access to their account with 1 or more care partners since 2003. Authorized care partners are provided their own credentials (login and password), enabling access to patients’ electronic medical records and communication with providers on patients’ behalf.
GHS patients ages 18 and older who had shared access to their patient portal account as of April 2014 were eligible for the study, as were their care partners. Details of participant recruitment have been described elsewhere.14 Upon providing informed consent and completing baseline surveys, participants were invited electronically to view doctors’ visit notes through MyGeisinger. Both patients and care partners were notified electronically when doctors' visit notes were signed and available for viewing. After 12 months, participants who had completed the baseline survey were recontacted.
Information about eligible patients’ health and health services use was extracted from their electronic health records at baseline. At follow-up, participants were asked whether they viewed doctors’ electronic visit notes and reasons they did or did not view them. Participants who viewed doctor visit notes were asked about their use and perceptions of OpenNotes. At baseline and follow-up, participants were asked to assess their confidence in undertaking health management tasks, using questions modified from a prior instrument17,18 as previously described.14 Measures of online practices of patients and care partners were constructed from digital recordings of MyGeisinger interactions for the 12-month periods before (July 19, 2013 to July 18, 2014) and after (July 19, 2014 to July 18, 2105) exposure to OpenNotes.
Characteristics of participants who responded at follow-up were compared with those who did not. Participants’ experiences with OpenNotes were examined from responses to follow-up surveys. Pre-post differences in online practices were evaluated using binary logistic regression models, taking into account within-individual correlation. To examine longitudinal effects of OpenNotes, we examined participants’ online practices and confidence managing aspects of patient health at baseline and follow-up. Differences in confidence managing patient health at follow-up were separately evaluated for patients and care partners using ordinal logistic regression models, taking into account correlations between observations. We used a proportional odds model, in which we modeled the likelihood that patients and care partners moved from a lower to a higher category of confidence. All analyses were performed using SAS version 9.4.19 This study was approved by the GHS Institutional Review Board (2013-0423).
RESULTS
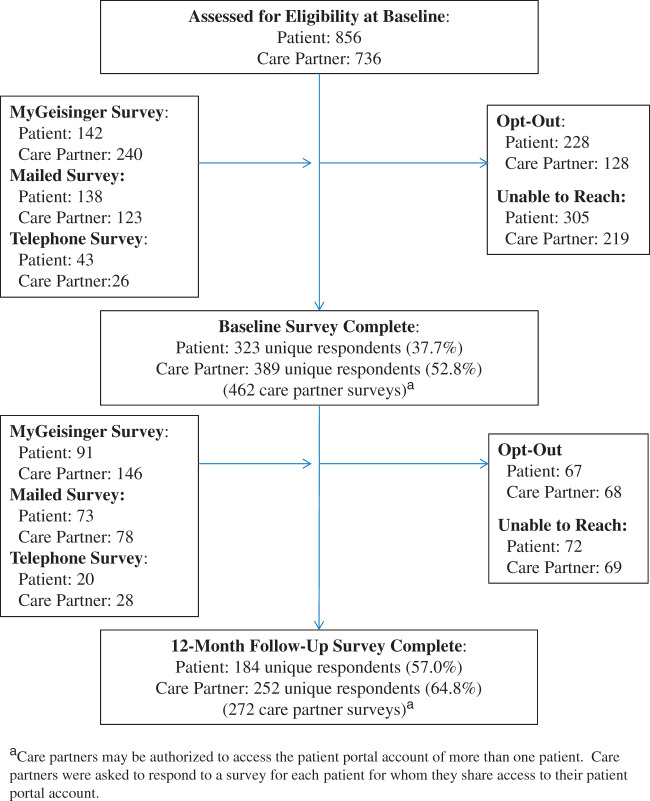
Of 856 patients and 736 care partners eligible for the study, 323 patients and 389 care partners provided informed consent and completed a baseline survey, and 184 patients and 252 care partners responded at follow-up (57.0% and 64.8% response, respectively; Figure 1). Patient respondents were younger (P = .02) and care partner respondents had better self-rated health (P = .01) than nonrespondents, but otherwise did not differ significantly with respect to demographic and health characteristics (electronic Appendix).
Figure 1.
Patient and care partner responses at baseline and 12-month follow-up.
Among participants with available notes, most patients (63.9%) and a large majority of care partners (87.5%) reported viewing 1 or more doctor notes (Table 1). Patients and care partners reported that they did not view doctor notes due to forgetting or not knowing about them (29.6% and 46.7%, respectively). Patients also reported not viewing notes because they relied on their care partners to read them (18.5%), or they did not have access to a computer (16.7%). Patients and care partners viewed doctor notes to learn about the patient’s health, remember or better understand what was said by the provider, or verify the accuracy of the notes. More than 1 in 3 (35.5%) care partners viewed doctor notes because they were unable to attend the visit and wanted to know what was discussed. Approximately half of patients and a quarter of care partners discussed or shared visit notes with others. Patients and care partners most often discussed or shared notes with each other (86.0% and 52.7%, respectively) or another family member/friend (34.0% and 67.3%), and less often with a health care professional (10.0% and 12.7%).
Table 1.
Patient and care partner motivations for viewing and sharing OpenNotes
| Patients | Care Partners | |
|---|---|---|
| One or more doctor’s notes availablea | 90.2% (n = 166) | 91.2% (n = 248) |
| Viewed 1 or more doctor’s notesb | ||
| No | 36.1% (n = 60) | 12.5% (n = 31) |
| Yes | 63.9% (n = 106) | 87.5% (n = 217) |
| Main reason did not view doctor’s notesb,d (%) | ||
| Forgot or did not know about them | 29.6 | 46.7 |
| Care partner reads for me | 18.5 | N/A |
| Do not have access to a computer | 16.7 | 0.0 |
| Could not find them | 7.4 | 16.7 |
| Did not think it would be useful | 3.7 | 20.0 |
| Too busy to read | 9.3 | 0.0 |
| Thought reading notes would make me anxious | 1.9 | 3.3 |
| Other | 13.0 | 13.3 |
| Reasons for viewing doctor’s notesb (%) | ||
| To know about patient’s health | 50.9 | 59.9 |
| To be sure I understood what the doctor said | 51.9 | 49.3 |
| To remember what happened during the visit | 38.7 | 32.3 |
| I was curious | 35.8 | 23.0 |
| Wanted to know what the doctor was thinking | 23.6 | 35.0 |
| To see if the notes were accurate | 21.7 | 18.9 |
| Unable to attend doctor visit and wanted to know what was discussed | Not asked | 35.5 |
| Have a right to see what is in my medical record | 31.1 | Not asked |
| Discussed or shared visit notes with other peoplec | 47.2% (n = 50) | 25.5% (n = 55) |
| Shared notes with:c (%) | ||
| Care partner or patient (respectively) | 86.0 | 52.7 |
| Another family member or friend | 34.0 | 67.3 |
| Another health care professional | 10.0 | 12.7 |
aSample includes responses from n = 184 patient surveys and 272 surveys that were completed by 184 patients and 252 care partners (care partners may have access to patient portal accounts of more than 1 patient).
bResponses refer to patients (n = 60) and care partners (n = 31) who did not view available doctor’s notes, and patients (n = 106) and care partners (n = 217) who did view available doctor’s notes.
cResponses are for patients (n = 50) and care partners (n = 55) who discussed or shared visit notes.
dItem nonresponse <1% for all items except reason did not view doctor notes (patients = 10.0%, care partners = 3.2%).
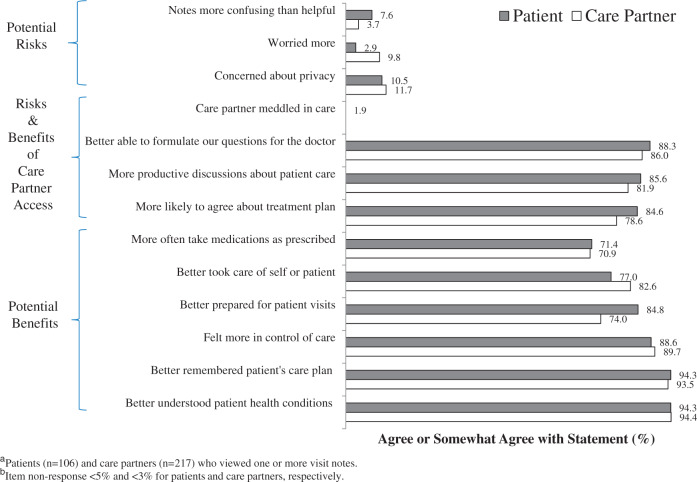
A large majority of patients and care partners reported benefits and few reported downsides of reading doctors’ notes, although about 1 in 10 patients and care partners reported concerns about privacy (Figure 2). The ability of care partners to access doctors’ visit notes was overwhelmingly endorsed as beneficial, with patients and care partners stating they were more likely to agree about the patient’s treatment plan (84.6% and 78.6%, respectively), had more productive discussions about the patient’s care (85.6% and 81.9%), and were better able to formulate questions for the doctor (88.3% and 86.0%). Few patients reported that their care partner meddled in care (1.9%). Patients and care partners reported many benefits of OpenNotes, including better understanding of patient health conditions (94.3% and 94.4%), better ability to remember the patient’s care plan (94.3% and 93.5%), feeling more in control of care (88.6% and 89.7%), and more often taking medications as prescribed (71.4% and 70.9%). At 12 months, most patients stated that they would like continued access to visit notes for themselves (94.3%) and care partners (92.4%); nearly all care partners (98.1%) desired continued access to OpenNotes (data not shown).
Figure 2.
Patient and care partner experiences with OpenNotes.
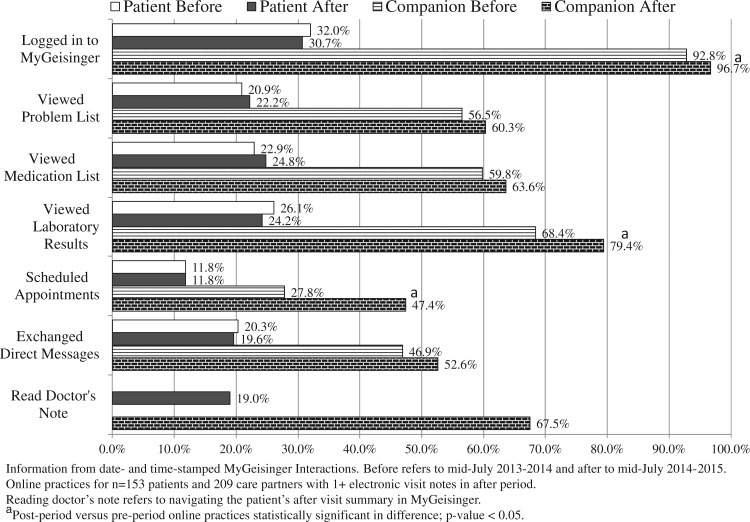
Patients’ use of MyGeisinger was comparable before and after 12 months’ exposure to OpenNotes (Figure 3). After exposure to OpenNotes, care partners were more likely to log in to MyGeisinger (96.7% vs 92.8%; P = .01) and use it to view results of patients’ laboratory tests (79.4% vs 68.4%; P < .001) as well as to schedule appointments (47.4% vs 27.8%; P < .001). Approximately 1 in 5 patients (19.0%) and 2 in 3 care partners (67.5%) used MyGeisinger to access doctor notes and patient after-visit summaries.
Figure 3.
Patient and care partner online practices, before and after exposure to OpenNotes.
Participants’ confidence in managing aspects of patient health was examined at baseline and after 12 months’ exposure to OpenNotes (Table 2). At follow-up, patients were more confident in their ability to manage their health information (Odds Ratio (OR) = 2.14; 95% CI, 1.59-2.89) and care (OR = 1.48; 95% CI, 1.14-1.93), they were better prepared for office visits (OR = 1.40; 95% CI, 1.04-1.90), and better understood their plan of care (OR = 1.39; 95% CI, 1.04-1.85) than at baseline. Care partners were confident in their ability to manage aspects of patients’ health at baseline, and few differences were observed at follow-up, although care partners were more likely to report improved communication with the patients’ health care providers (OR = 1.74; 95% CI, 1.36-2.23).
Table 2.
Patient and care partner perceived ability to manage care and satisfaction with communication
| Confidence managing aspects of patient’s care | Patientsa |
Care Partnersb |
||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | OR (95% CI) | Baseline | Follow-up | OR (95% CI) | |
| Preparedness to manage patient’s health information (%) | 2.14 (1.59−2.89) | 0.85 (0.65−1.11) | ||||
| Not at all or a little bit | 37.8 | 12.2 | 1.5 | 0.7 | ||
| Somewhat | 15.6 | 19.9 | 8.1 | 11.8 | ||
| Quite a bit | 20.6 | 40.3 | 33.0 | 33.5 | ||
| Very | 26.1 | 27.6 | 57.4 | 54.0 | ||
| Preparedness to manage patient’s care (%) | 1.48 (1.14−1.93) | 0.89 (0.71−1.12) | ||||
| Not at all or a little bit | 25.7 | 10.5 | 3.7 | 0.7 | ||
| Somewhat | 20.8 | 21.0 | 5.5 | 14.0 | ||
| Quite a bit | 24.0 | 42.5 | 36.9 | 32.4 | ||
| Very | 29.5 | 26.0 | 53.9 | 52.9 | ||
| Preparedness for office visits (%) | 1.40 (1.04−1.90) | 0.95 (0.74−1.21) | ||||
| Not at all or a little bit | 14.2 | 3.3 | 2.6 | 3.4 | ||
| Somewhat | 18.6 | 13.9 | 9.7 | 9.7 | ||
| Quite a bit | 25.1 | 41.7 | 28.8 | 30.2 | ||
| Very | 42.1 | 41.1 | 58.8 | 56.7 | ||
| Understanding of patient’s plan of care (%) | 1.39 (1.04−1.85) | 0.96 (0.76−1.22) | ||||
| Not at all or a little bit | 1.91 | 7.2 | 3.7 | 1.8 | ||
| Somewhat | 17.5 | 17.1 | 11.5 | 11.0 | ||
| Quite a bit | 26.8 | 39.8 | 30.0 | 35.3 | ||
| Very | 36.6 | 35.9 | 54.8 | 51.8 | ||
| Understanding of patient’s health and medical conditions (%) | 1.27 (0.94−1.71) | 0.87 (0.69−1.11) | ||||
| Not at all or a little bit | 13.7 | 5.5 | 1.8 | 1.1 | ||
| Somewhat | 18.7 | 14.4 | 8.5 | 7.4 | ||
| Quite a bit | 26.4 | 40.9 | 31.0 | 37.5 | ||
| Very | 41.2 | 39.2 | 58.7 | 54.0 | ||
| Communication with patient providers (%) | Not asked | 1.74 (1.36−2.23) | ||||
| Fair or poor | 7.5 | 5.5 | ||||
| Good | 24.5 | 15.1 | ||||
| Very good | 34.0 | 32.1 | ||||
| Excellent | 34.0 | 47.2 | ||||
aPatient (n = 184) and care partner (n = 272) respondents who completed both baseline and follow-up surveys. Care partner responses reflect perspectives with respect to patients with whom they share access to the patient portal.
bPatient nonresponse <2.5%; care partner nonresponse <3.0% for all measures.
DISCUSSION
As in the initial OpenNotes trial, the majority of patients read their doctor visit notes, reported clinically relevant benefits, and wanted to continue to have ready access in the future. This was also true of care partners. Moreover, patients and care partners reported that joint access led to more productive discussions about the patient’s care, better agreement about the patient’s treatment plan, and improved ability to formulate questions for the doctor. After 12 months of exposure to OpenNotes, care partners were more likely to access and use the patient portal and reported better communication with doctors, while patients were more confident in their ability to manage clinically important elements of their care.
Benefits of the patient portal may operate through mechanisms of convenience, continuity, activation, and understanding.5 Our findings suggest that for some patients these mechanisms may be amplified by the active involvement of a care partner. Care partners were more likely than patients to access visit notes, the vast majority of patients who discussed visit notes did so with their care partner, and patients overwhelmingly endorsed the benefits of shared notes for managing and communicating about their care. Overall, it is reasonable to hypothesize that an observed increase in patients’ confidence in managing their care was at least in part due to care partners facilitating information access and a stronger patient–care partner therapeutic alliance involving more productive discussion and greater agreement about care. Such a hypothesis is consistent with recent studies finding clinical benefit from purposefully involving care partners through technology.20–24
Our findings that shared notes increased patients’ confidence in addressing aspects of their health may be important, because self-management affects a range of clinical and health services outcomes.25–27 Strategies that strengthen patients’ capacity to manage their health commonly involve introducing new health professionals, technologies, or processes to care delivery.28–30 In contrast, OpenNotes makes doctors’ visit notes directly available to patients (and, in this study, care partners), without introducing new personnel or technology, or making radical changes to the provider’s practice. Our study contributes to a larger literature suggesting that strategies to actively involve and support patients in their care are more likely to be feasible and effective when they collaboratively involve providers at the point of care.31
It is reassuring that few patients reported drawbacks to extending OpenNotes to care partners. Approximately 1 in 10 patients were concerned about the privacy of their health information, which is lower than reported in the original OpenNotes study.1,32 Relatively low rates of patient concerns and experienced drawbacks may be attributed to study participants being drawn from a selected group of patients who chose to share access to their patient portal account. However, establishing that delivering doctors’ visit notes to care partners was acceptable in this selected population is nevertheless an important prerequisite for broader dissemination of OpenNotes through shared access.
That more than one-third of care partners viewed visit notes because they were unable to attend doctor visits and wanted to know what was discussed speaks directly to how shared notes may improve transparency, communication, and continuity of care.14,33 Accessing patients’ health information34,35 and managing health system demands36–38 are significant challenges for family caregivers. Shared notes may help family caregivers by confirming treatment decisions and reducing uncertainty regarding the recommended plan of care.
Our study results are subject to several limitations. Study participants were limited to patients and care partners in a single health system. Although our response rate is comparable to other surveys of registered patient portal users1,7 and similar patient subgroups,39–41 it is nevertheless low, which limits our ability to generalize findings to the entire population from which the sample was drawn. Our pre-post design precludes our ability to fully attribute observed differences to OpenNotes, as opposed to other innovations or practice changes. Unlike the original OpenNotes study, we did not assess doctor perspectives or experiences. Our results do not provide insight regarding the much larger population of patients who informally share doctor notes with family members or friends,1,32 or whose family members access notes using the patient’s identity credentials.4,14
OpenNotes is a movement that is stimulating transparency and innovative change, with the goals of improving communication and engaging patients more actively in care. This study demonstrates the feasibility of delivering OpenNotes through shared access to electronic medical records. Results suggest that expanding access to shared notes holds promise as a strategy to better support and engage patients and families in care.
FUNDING
This work was supported by a grant from the Robert Wood Johnson Foundation. Its contents are solely the responsibility of the authors and do not represent the official view of the Robert Wood Johnson Foundation.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
Substantial contributions to conception and design: D.C., J.A.G., J.D.D., J.L.W., R.A.S., T.D., J.W.; acquisition of data: A.B., D.C.; analysis and interpretation of data: A.B., D.C., J.A.G., J.D.D., J.L.W., R.A.S., T.D., J.W.; drafting the article: J.L.W.; revising it critically for important intellectual content: D.C., J.A.G., J.D.D., R.A.S., T.D., J.W.; and final approval of the version to be published: A.B., D.C., J.A.G., J.D.D., J.L.W., R.A.S., T.D., J.W. A.B. and D.C. had full access to data in the study, and all authors take responsibility for the integrity of the data and accuracy of the data analysis.
SUPPLEMENTARY MATERIAL
Supplementary material is available online at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We gratefully acknowledge the OpenNotes study team for their support of this work.
REFERENCES
- 1. Delbanco T, Walker J, Bell SK et al. Inviting patients to read their doctors' notes: a quasi-experimental study and a look ahead. Ann Int Med. 2012;157(7):461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ricciardi L, Mostashari F, Murphy J, Daniel JG, Siminerio EP. A national action plan to support consumer engagement via e-health. Health Affairs. 2013;32(2):376–384. [DOI] [PubMed] [Google Scholar]
- 3. de Lusignan S, Mold F, Sheikh A et al. Patients' online access to their electronic health records and linked online services: a systematic interpretative review. BMJ Open. 2014;4(9):e006021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Goldzweig CL, Orshansky G, Paige NM et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Int Med. 2013;159(10):677–687. [DOI] [PubMed] [Google Scholar]
- 5. Otte-Trojel T, de Bont A, Rundall TG, van de Klundert J. How outcomes are achieved through patient portals: a realist review. J Am Med Inform Assoc. 2014;21(4):751–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Caine K, Kohn S, Lawrence C, Hanania R, Meslin EM, Tierney WM. Designing a Patient-Centered User Interface for Access Decisions about EHR Data: Implications from Patient Interviews. J General Int Med. 2015;30 (Suppl 1):7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zulman DM, Nazi KM, Turvey CL, Wagner TH, Woods SS, An LC. Patient interest in sharing personal health record information: a web-based survey. Ann Int Med. 2011;155(12):805–810. [DOI] [PubMed] [Google Scholar]
- 8. Crotty BH, Walker J, Dierks M et al. Information sharing preferences of older patients and their families. JAMA Int Med. 2015;175(9):375–382. [DOI] [PubMed] [Google Scholar]
- 9. Wolff JL, Roter DL. Family presence in routine medical visits: a meta-analytical review. Soc Sci Med. 2011;72(6):823–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Laidsaar-Powell RC, Butow PN, Bu S et al. Physician-patient-companion communication and decision-making: a systematic review of triadic medical consultations. Patient education and counseling. 2013;91(1):3–13. [DOI] [PubMed] [Google Scholar]
- 11. IOM. Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 12. Woods SS, Schwartz E, Tuepker A et al. Patient experiences with full electronic access to health records and clinical notes through the My HealtheVet Personal Health Record Pilot: qualitative study. J Med Internet Res. 2013;15(3):e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mayberry LS, Kripalani S, Rothman RL, Osborn CY. Bridging the digital divide in diabetes: family support and implications for health literacy. Diabetes Technol Ther. 2011;13(10):1005–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wolff JL, Berger A, Clarke D et al. Patients, care partners, and shared access to the patient portal: online practices at an integrated health system. J Am Med Inform Assoc. 2016(in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Walker J, Leveille SG, Ngo L et al. Inviting patients to read their doctors' notes: patients and doctors look ahead: patient and physician surveys. Ann Int Med. 2011;155(12):811–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jackson SL, Mejilla R, Darer JD et al. Patients who share transparent visit notes with others: characteristics, risks, and benefits. J Med Internet Res. 2014;16(11):e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Res Nurs Health. 1990;13(6):375–384. [DOI] [PubMed] [Google Scholar]
- 18. Zwicker D. Preparedness for Caregiving Scale. Best Practices in Nursing Care to Older Adults. New York University: Hartford Institute for Geriatric Nursing; 2010. [Google Scholar]
- 19. SAS Institute I. SAS Software. 8.1 ed. Cary, NC; 2000.
- 20. Piette JD, Marinec N, Janda K et al. Structured caregiver feedback enhances engagement and impact of mobile health support: a randomized trial in a lower-middle-income country. Telemed J E-health. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Piette JD, Striplin D, Marinec N et al. A mobile health intervention supporting heart failure patients and their informal caregivers: a randomized comparative effectiveness trial. J Med Internet Res. 2015;17(6):e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aikens JE, Trivedi R, Heapy A, Pfeiffer PN, Piette JD. Potential Impact of Incorporating a Patient-Selected Support Person into mHealth for Depression. J General Int Med. 2015;30(6):797–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wittenberg-Lyles E, Oliver DP, Kruse RL, Demiris G, Gage LA, Wagner K. Family caregiver participation in hospice interdisciplinary team meetings: how does it affect the nature and content of communication? Health Commun. 2013;28(2):110–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Piette JD, Gregor MA, Share D et al. Improving heart failure self-management support by actively engaging out-of-home caregivers: results of a feasibility study. Congest Heart Fail. 2008;14(1):12–18. [DOI] [PubMed] [Google Scholar]
- 25. Lorig K, Ritter P, Stewart A et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39(11):1217–1223. [DOI] [PubMed] [Google Scholar]
- 26. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Affairs. 2013;32(2):207–214. [DOI] [PubMed] [Google Scholar]
- 27. Kinney RL, Lemon SC, Person SD, Pagoto SL, Saczynski JS. The association between patient activation and medication adherence, hospitalization, and emergency room utilization in patients with chronic illnesses: a systematic review. Patient Educ Counseling. 2015;98(5):545–552. [DOI] [PubMed] [Google Scholar]
- 28. Thom DH, Hessler D, Willard-Grace R et al. Health coaching by medical assistants improves patients' chronic care experience. Am J Managed Care. 2015;21(10):685–691. [PubMed] [Google Scholar]
- 29. Lorig K, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. [DOI] [PubMed] [Google Scholar]
- 30. Pare G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inform Assoc. 2007; 14(3):269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Grande SW, Faber MJ, Durand MA, Thompson R, Elwyn G. A classification model of patient engagement methods and assessment of their feasibility in real-world settings. Patient Educ Counseling. 2014;95(2):281–287. [DOI] [PubMed] [Google Scholar]
- 32. Vodicka E, Mejilla R, Leveille SG et al. Online access to doctors' notes: patient concerns about privacy. J Med Internet Res. 2013;15(9):e208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wolff JL, Darer JD, Larsen KL. Family caregivers and consumer health information technology. J General Int Med. 2016;31(1):117–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zulman DM, Piette JD, Jenchura EC, Asch SM, Rosland AM. Facilitating out-of-home caregiving through health information technology: survey of informal caregivers' current practices, interests, and perceived barriers. J Med Internet Res. 2013;15(7):e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Levine C. HIPAA and talking with family caregivers: what does the law really say? Am J Nursing. 2006;106(8):51–53. [DOI] [PubMed] [Google Scholar]
- 36. Wolff JL, Spillman BC, Freedman VA, Kasper JD. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Int Med. 2016;176(3):372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Giovannetti ER, Wolff JL, Xue QL et al. Difficulty assisting with health care tasks among caregivers of multimorbid older adults. J General Int Med. 2012;27(1):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jennings LA, Reuben DB, Evertson LC et al. Unmet needs of caregivers of individuals referred to a dementia care program. J Am Geriatrics Soc. 2015;63(2):282–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Voils CI, Yancy WS Jr, Weinberger M et al. The trials and tribulations of enrolling couples in a randomized, controlled trial: a self-management program for hyperlipidemia as a model. Patient Educ Counseling. 2011;84(1):33–40. [DOI] [PubMed] [Google Scholar]
- 40. Steinhauser KE, Clipp EC, Hays JC et al. Identifying, recruiting, and retaining seriously-ill patients and their caregivers in longitudinal research. Palliative Med. 2006;20(8):745–754. [DOI] [PubMed] [Google Scholar]
- 41. Trivedi RB, Szarka JG, Beaver K et al. Recruitment and retention rates in behavioral trials involving patients and a support person: a systematic review. Contemp Clin Trials. 2013;36(1):307–318. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.