Abstract
Communication in acute care settings is fragmented and occurs asynchronously via a variety of electronic modalities. Providers are often not on the same page with regard to the plan of care. We designed and developed a secure, patient-centered “microblog” messaging platform that identifies care team members by synchronizing with the electronic health record, and directs providers to a single forum where they can communicate about the plan of care. The system was used for 35% of patients admitted to a medical intensive care unit over a 6-month period. Major themes in messages included care coordination (49%), clinical summarization (29%), and care team collaboration (27%). Message transparency and persistence were seen as useful features by 83% and 62% of respondents, respectively. Availability of alternative messaging tools and variable use by non-unit providers were seen as main barriers to adoption by 83% and 62% of respondents, respectively. This approach has much potential to improve communication across settings once barriers are addressed.
Keywords: care team communication, care coordination, innovation, quality improvement, secure messaging
INTRODUCTION
Communication in acute care settings is fragmented and inefficient.1–3 Care team members share impressions, opinions, and knowledge informally, often via alphanumeric pagers, email, and text messaging, to coordinate the plan of care. However, providers frequently disagree about basic components of the plan of care.4,5 Catalyzed by the surge in use of mobile devices, providers are increasingly using email and text messaging apps to communicate informally. Understanding how best to use secure messaging tools to manage the complex acute care communication space is a growing area of interest.6–10 Coherent management of the electronic dialogue is clearly necessary to coordinate the plan of care more effectively.11
Efforts at improving communication among providers using 2-way alphanumeric pagers have demonstrated increased efficiencies, reduced call-backs, and fewer interruptions.12 For more complex exchanges that require input from multiple providers, group emails and text messaging can be helpful.13 Still, key providers involved in developing and executing the plan of care are often left out of these group exchanges; the members of a patient’s care team change frequently and those who simply “reply all” may inadvertently leave out key clinicians or route the message incorrectly (eg, to a nurse, intern, or hospitalist who left the care team after the end of a shift). In short, individual providers are limited to snippets of the electronic dialogue sent via pager, email, or text messaging. The result is siloed, inefficient, and often redundant communication about the plan of care.14,15 In busy care settings, ineffective communication may potentiate the cognitive demands on clinicians and lead to errors.16,17
Social networking applications (eg, Yammer by Microsoft, Inc.) have an appeal as a platform for interprofessional collaboration, but use of these “microblog” technologies for patient-specific clinical communication is nascent and constrained by the requirement to protect personal health information.18 A microblog-type forum is ideal, because all messages about a patient transparently and persistently reside on a virtual “wall” for the entire care team to view; there is no need to forward messages when new providers join the care team or when a patient transfers to a different clinical service or unit.10,11 In theory, this type of approach could enhance information sharing, minimize conversation silos, and mitigate cognitive burden, thereby improving care coordination efficiency and reducing errors related to miscommunication or unnecessary interruptions.
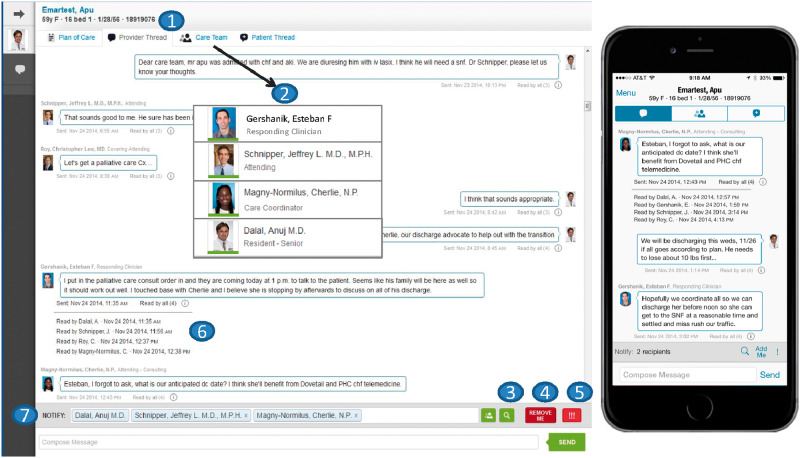
We engaged key stakeholders to design, develop, and iteratively refine a social media–inspired, patient-centered “microblog” messaging platform for use in acute care.15 We configured secure, HIPAA-compliant web-based and mobile messaging applications (Figure 1) to facilitate seamless, patient-specific communication by directing providers to a single forum where they could view and contribute to plan of care discussions. In comparison to other secure messaging and social networking applications, a key feature of our platform is real-time care team synchronization with the electronic health record (EHR); when the care team is accurately and reliably maintained in the EHR, messages are reliably delivered to those who are currently caring for the patient.19,20 In this way, our platform ensures that all messages are viewable by current and future members of the care team; conversations are continually available, as opposed to being siloed within an individual provider’s inbox. In this study we evaluated use of the web-based and mobile applications by providers caring for patients admitted to the acute care setting, performed content analyses of messages, and identified barriers to adoption.
Figure 1.
Patient-centered “microblog” messaging platform: web-based and mobile applications Core functionality includes: (1) a provider thread not viewable by patients; (2) identification of inpatient and ambulatory care team members from Partners Enterprise Patient Lists (PEPL); (3) the ability to search the online provider paging directory to invite other members to the care team; (4) a “Remove Me” button that allows providers to stop receiving active message notifications on patients they are following (providers could still access and view the entire conversation thread); (5) message prioritization (normal and high-priority); (6) read receipts with date and time stamp for each message notification recipient; and (7) automatic updating of notification recipients when care team members change in PEPL (eg, when a nurse or intern comes on shift). A separate patient thread with the same functionality was integrated into an acute care patient portal to facilitate patient-provider messaging, as previously reported.21
METHODS
Setting and participants
This institutional review board–approved study was conducted at a large academic medical center in Boston, Massachusetts. The web-based and mobile (iOS and Android) applications were developed in collaboration with and supported by a secure messaging vendor (CareThread, Inc.). The platform was available for use in a medical intensive care unit (MICU) and 2 noncritical care units as part of 2 institutional initiatives: Promoting Respect and Ongoing Safety through Communication, Patient-Centeredness, Engagement, Communication, and Technology (PROSPECT), funded by the Gordon and Betty Moore Foundation, and the Partners PCORI Transitions study, funded by the Patient-Centered Outcomes Research Institution. The application leveraged institutional single sign-on infrastructure and was quickly accessible from routinely used inpatient clinical applications and encrypted hyperlinks embedded in notification emails (Microsoft Outlook).
As this was a quality improvement study, we were granted a waiver of patient consent. Patients admitted to the MICU for >24 hours from January through May 2015 were included, and any provider (unit- and non-unit-based) involved with the care of a patient admitted to the MICU during this time frame could participate.
Overview of the system: unique features and core functionality
The iterative, participatory design and development process was previously reported.15 The web-based and mobile applications (Figure 1) included unique features similar to microblogs used in social media. First, we obtained the patient’s current providers (names, roles, pictures) from the Partners Enterprise Patient Lists (PEPL) application that was accessible from our EHR and maintained as part of a concurrent quality improvement initiative.20 PEPL is a web-based application routinely used by hospital-based providers to manage role assignments, create unit- and team-based patient lists, and transfer responsibility of care. Role assignments in PEPL were designated manually (eg, by an intern coming on shift), or automatically via other clinical systems (eg, medication administration application used by the bedside nurse), default functionality, and/or administrative schedules (eg, attending). Thus, by leveraging PEPL to provide care team mapping functionality for the patient-centered “microblog” messaging platform, providers could follow the dialogues of specific patients for whom they had an assigned role on the care team. Second, messages were persistently available so that any provider could view conversations at any time (eg, after transfer, during subsequent admissions, etc.). Third, if not previously assigned a role via PEPL, providers were prompted to designate their role on the care team in CareThread's application when adding a patient to their patient list or responding to a message.
Notifications
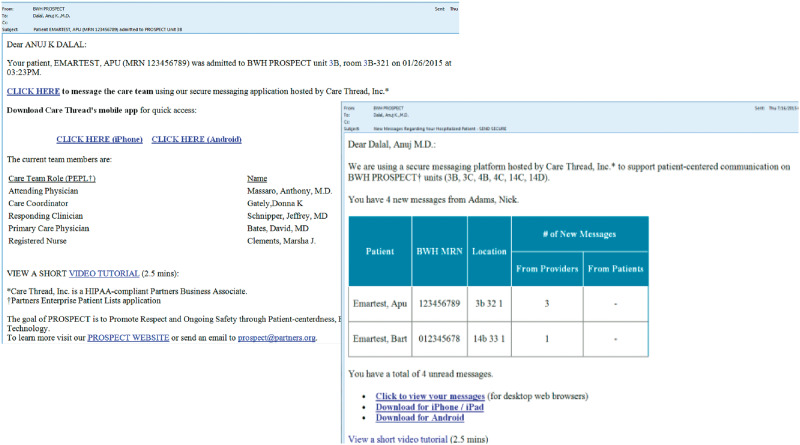
Providers received automated email notifications upon patient arrival to the intervention unit and when new messages were sent via the system (Figure 2). All notification emails contained hyperlinks directing providers to the application. Mobile app users received push notifications (similar to notifications of text messages) unless manually disabled. Providers received no more than 1 email notification per hour unless a message was designated high priority. Email notifications were suppressed altogether if the provider was prompted to view the message via a mobile push notification. Importantly, when new providers assumed responsibility from a previous provider (eg, nurse coming on shift), the message recipient list was automatically updated such that notifications were routed to the provider currently assigned in that role.19
Figure 2.
Notification emails Automated admission notifications emails (left) display patient name and identifying information, as well as current care team members and roles. Message notification emails (right) display number of unread messages. All notification emails contain links to download mobile applications (iOS, Android), and to a short video tutorial.
Implementation and training
We conducted brief training presentations to all dedicated MICU staff (physicians, nurses, etc.) at the beginning of the study and/or their rotation, and identified clinical champions. We educated users that messages sent via web-based and mobile applications would be treated similarly to messages sent via institutional email or alphanumeric pagers (ie, informally), and stored on secure, HIPAA-compliant servers. All notification emails (Figure 2) included a hyperlink to a web-based video tutorial that provided an overview of core functionality as well as hyperlinks to download the mobile app. Research assistants were available for on-site coaching and troubleshooting during normal business hours.
Measurements and data collection
Usage and messaging activity
We tracked access to web-based and mobile applications by providers as well as messaging activity on all patients, including message volume and priority, roles of senders and receivers, message notifications, read receipts, and content of messages.
Survey instrument
We developed a survey instrument to assess use of web-based and mobile applications, frequency of use (semiquantitative), and utility for improving plan of care concordance (5-point Likert scale). We assessed utility of core functionality (5-point Likert scale) and main barriers to use that were previously identified during design and development.15 Finally, we assessed likelihood of use if barriers were addressed (5-point Likert scale) and provided space for comments. The survey questions were vetted by a small group of practicing clinicians to ensure appropriate context and consistent understanding.
Statistical and qualitative analyses
Descriptive statistics were used to report patient demographics, messaging activity, and survey data. Survey questions were divided among participants who agreed vs those who did not agree. The proportion of providers who agreed that the application was useful for improving plan of care concordance was compared among high- vs low-frequency users using Fisher’s Exact test (2-sided, P < .05). The content of messages sent by providers was analyzed and grouped by themes using a 2-person consensus approach.
RESULTS
For 497 patients admitted to the MICU during the study period (60.5 ± 16.0 years of age, 49% male, 68% Caucasian; average unit length of stay 5.0 days; 42 (8.5%) admitted 2 or more times), messages were sent via the system on 175 of them (35.2%; 63.3 ± 14.3 years of age, 51% male, 84% Caucasian; average unit length of stay 7.6 days; 29 (16.6%) admitted 2 or more times). See Table 1 for complete messaging analysis. A total of 928 messages were sent by 180 providers in various roles. The percentages of provider log-ins via web-based and mobile applications were 68% and 32%, respectively. The median messages per patient was 3 (interquartile range [IQR] 1–5), with a maximum of 112 on 1 patient. A majority of messages (76%) were viewed by all notified recipients. Eight themes (Table 2) were identified in a cohort of 46 patients (26.3%) with 5 or more messages (∼1.69 themes per message). Messaging activity on 5 patients (2.9%) continued after transfer to a noncritical care unit.
Table 1.
Patient-centered “microblog” messaging analysis
| Metric | N | Statistics and Comments |
|---|---|---|
| Patients | 175 | Median 3 (IQR 1–5) messages per patient |
| Min, max (1–112) | ||
| Messages | 928 | Mean (std dev) notified recipients per message: 13.2 ± 5.2 |
| High priority: 4; normal priority: 924 | ||
| Message senders | 180 | Relative frequency of use by inpatient provider type: resident/intern > medical director > fellow > attending > consulting attending > care coordinator > nurse |
| Relative frequency of use by ambulatory provider type: specialist > care coordinator > primary care physician | ||
| Median 2 (IQR 1–4) messages per sender | ||
| Message recipients | 574 | Median 5 (IQR 2–18) messages per recipient |
| Message notifications | Total: 12 275 | No. read: 9322 (75.9%) |
| High priority: 57 | No. read: 46 (80.7%) | |
| Normal priority: 12 218 | No. read: 9276 (75.9%) | |
| Time elapsed until message read by notification recipient | – | Median 3 h 1 m (IQR 0–18 h 1 m) |
| Min, Max (1 m, 57 d 1 h 2 m) | ||
| Provider logins (web, mobile) | 8185 by 180 senders | Median 26 (IQR 10–54.5) per sender |
| Provider logins (web) | 5600 by 176 senders | Median 16.5 (IQR 6–44.5) per sender |
| Provider logins (mobile) | 2585 by 76 senders | Median 16.5 (IQR 7.75–29.25) per sender |
| 74 iOS, 2 Android users |
Table 2.
Major themes identified in the cohort of patients with 5 or more messagesa
| Category | N (%) | Examples |
|---|---|---|
| Themes | ||
| Care coordination | 334 (49.4) | Scheduling, coordinating transfer to facilities, discharge planning: “We could arrange home with services, freestanding inpt hospice closer to home, possibly [inpatient palliative care unit] …” |
| Clinical summarization | 197 (29.1) | Admission, status change, transfer updates: “Mrs. [patient] is a 32 year old female with Hodgkins lymphoma s/p allo-SCT with [previous] hospitalization for IPS (s/p prednisone and enbrel), recently treated as an outpatient for pneumonia, and asthma here with mixed hypoxic/hypercarbic respiratory failure” |
| Care team collaboration | 184 (27.2) | Request input from other members of the care team (eg, off-site providers such as primary care physicians, subspecialists): “Thanks for the update. Since he may go to the floor here I am going to give [the hospitalist] a heads up about this case …” |
| Medications, tests, studies, procedures, results, trials | 156 (23.1) | “He was noted to have stones in his gallbladder on RUQ ultrasound, pending final read we will plan to consult surgery for recommendations …” |
| “Today was day 5 of campath. We are planning to slowly taper his steroids” | ||
| Acknowledgment | 105 (15.5) | Praise, feedback, agreement: “Thanks. That seems like the best plan.” |
| Relay patient/ caregiver input | 84 (12.4) | Needs, concerns, wishes: “I spoke with [the patient] yesterday. She would like to go to [rehab] in Cambridge.” |
| Goals of care | 68 (10.1) | End-of-life care, palliation, ethics/legal: “We just wanted to clarify a few things in terms of his Goals of Care. There was mention of a will that states that he would not want to be a Full Code in his current state, however …” |
| Other | 15 (2.2) | “Hi guys, out of the country until 4/27” |
aTotal number of patients with 5 or more messages: n = 46 (676 messages in total). Median messages per patient in cohort: 8.5 (IQR 6–16).
Survey results
Of 43 survey participants (30 physicians, 11 nurses, 1 care coordinator, 1 social worker; 41.2 ± 10.6 years of age, 39.5% male, 78.6% Caucasian), 29 (67.4%) responded (21 physicians, 7 nurses, 1 care coordinator; 41.8 ± 11.1 years of age, 41.4% male, 86.2% Caucasian). Of the 29 respondents, 26 (89.7%) stated that they accessed the application from a desktop computer via a web browser, and 16 (55.2%) stated that they accessed the application from a mobile device via a native app or mobile web browser. Fifteen (51.7%) stated that they sometimes, often, or regularly (ie, for >3 patients per week) used the application to message other providers. Nineteen (65.5%) stated that the application was useful for improving plan of care concordance; this finding tended to be more common among respondents reporting frequent vs nonfrequent use (80% vs 50%; P = .13). Twenty-six respondents (89.7%) stated that they would use the application if all the barriers were addressed; this finding tended to be more common among respondents reporting frequent vs nonfrequent use (100% vs 78.5%; P = .10). Useful features and main barriers are listed in Table 3.
Table 3.
Useful features and main barriers to use
| Useful Features | N (%) Agree, n = 29 |
| A transparent conversation that all care team members can view | 24 (82.8) |
| Persistence of clinical messages on the thread that I can view when necessary (eg, “on-demand”). | 18 (62.1) |
| A “Remove Me” button to suppress notifications when I no longer need to participate in the conversation | 18 (62.1) |
| Ability to search the Partners online paging directory (accessible from “magnifying glass” icon) to invite other members to the care team | 17 (59.6) |
| Quick and reliable identification of the patient's providers via the “Care Team” tab | 17 (58.6) |
| Read-receipt functionality so I can see when my message was viewed and by whom | 15 (51.7) |
| Main Barriers to Use | N (%) Selected, n = 29 |
| Alternative asynchronous messaging modalities (eg, pagers, email, texting) used by other providers with whom I communicate | 24 (82.8) |
| Poor awareness and/or use by providers not working on an intervention unit | 22 (75.9) |
| Inability to communicate with out-of-network providers who do not have a Partners network email address, and therefore cannot receive my message | 15 (51.7) |
| It is an additional step to access (eg, clicking on email hyperlink, downloading mobile app) | 14 (48.3) |
| Poor awareness and/or use by providers working on an intervention unit | 12 (41.4) |
| Other | 3 (10.3) |
| Security and HIPAA concerns | 1 (3.5) |
DISCUSSION
We implemented a patient-centered “microblog” messaging platform in an acute care setting and observed modest usage by providers, most often via the web application. The system was used by key members of the unit-based team to communicate with non-unit-based team members regarding routine matters (few messages were flagged high priority). The system was typically used for patients admitted 2 or more times and with longer lengths of stay. Care coordination and clinical summarization (eg, nonurgent status updates and communication across care settings) were common themes identified in messages; providers less frequently sent messages to relay patient input and discuss goals of care. The main barrier limiting adoption was use of alternative messaging modalities (eg, email, pagers) by non-unit-based providers who were often unaware of and/or unfamiliar with the system. From analysis of feedback from surveys and stakeholders, we identified strategies to overcome barriers and promote adoption (Table 4).
Table 4.
Strategies for overcoming key barriers and to promote adoption
| Key barriers | Strategies to promote adoption |
|---|---|
| Multiple alternative communication modalities, including pagers, email, text messaging, internal EHR messaging | Align with institutional initiatives to adopt newer secure messaging tools while transitioning away from older modalities (eg, alphanumeric pagers). |
| Ensure that messages and notifications are seamlessly integrated into clinical workflow (eg, internal EHR messaging, institutional email). | |
| Provide users with functionality to self-configure notifications sent to mobile devices, email, and/or pagers (if still in use) in order to mitigate alert fatigue/dual alerting. | |
| Poor awareness and/or use by providers | Engage institutional stakeholders including medical/nursing unit directors; inpatient, primary care, and subspecialty leaders; nursing staff; care coordinators; social workers; residency program staff; informatics and information systems leaders. |
| Engage unit and non-unit-based providers early during implementation. | |
| Provide quick access to frequently asked questions, and short online video tutorials embedded into notification emails. | |
| Identification of providers | Leverage EHR web services to identify patient’s care team and provider role assignments. |
| Conduct concurrent quality improvement initiative to improve accuracy of care team role assignments in the EHR.20 | |
| Integrate with institutional and external online directories to identify network and non-network provider profiles (names, pictures). | |
| Additional system to access | Leverage institutional single sign-on infrastructure for all access points (eg, hyperlinks within notification emails, mobile app, EHR). |
| Provide web-based access from within the EHR. | |
| Integrate institutional online directories to access providers’ contact information (eg, email, phone number, pager). | |
| Use enterprise HL7 feed to obtain patient context and admission, transfer, discharge events. | |
| Security, HIPAA, legal concerns, other | Educate users that messages sent via web-based and mobile applications are stored on secure, HIPAA-compliant servers, and include this information in all notification emails. |
| Communicate that messages are not part of the legal record (similar to messages sent via institutional email or alphanumeric pagers). | |
| Ensure that the reply address for notification emails is not rejected as spam and provide a “From” address familiar to institutional users. | |
| Ensure that email connection between third-party vendor and institution is secure in order to incorporate patient context into notification emails. |
We attribute modest adoption to strong sponsorship by clinical champions. The core functionality – message transparency and persistence, mechanisms to mitigate notification fatigue, real-time care team synchronization with the EHR – was perceived favorably by providers, likely due to our efforts at engaging stakeholders during design and development.15 We attribute the high use of the web application to tight integration with commonly used inpatient clinical applications, quick access via hyperlinks in notification emails, and streamlined sign-on procedures (ie, by leveraging institutional log-on infrastructure). Because the mobile application required initial download and account authentication, it was most often used by unit-based providers (who sent the majority of messages). Many non-unit providers (eg, ambulatory specialists) suggested that the initial barriers to setting up the mobile application to respond to just a few messages on study patients outweighed the potential advantages because messages on nonstudy patients were typically sent via network email.
Although we have not found other studies that evaluate the use of microblogs to support clinical communication, a few studies have examined the impact of group messaging tools; most were favorably rated by users with regard to perceived impact on efficiency.13,21,22 Similar to these studies, our results provide preliminary evidence supporting the feasibility of using this type of approach to improve shared understanding of the plan of care throughout hospitalization. To illustrate the potential value for coordinating care, consider the dialogue that transpired on a chronically critically ill patient hospitalized for respiratory failure over a 2-month period: a total of 112 messages were sent by 21 providers in 13 roles and received by 69 different providers in 15 roles; many were clinicians assuming care as the patient transferred to a general medicine unit, as well as individuals in nontraditional disciplines (eg, ethics/legal representatives). In this case, transparency and persistence of the dialogue that transpired while the patient was in the MICU were crucial to ensure consistent understanding of the complex plan of care among a multidisciplinary team of providers after transfer to a noncritical care unit. The alternative, multiple emails often routed incorrectly or leaving out key providers, is typically less efficient and could lead to miscommunication. Lastly, our study underscores the importance of addressing barriers to implementing secure messaging tools (Table 4), namely the availability of competing systems (eg, email, pagers, EHR messaging) and engagement of non-unit-based providers (eg, primary care physicians), who often have key information to share with the inpatient team. Most users suggested that they would use our application once these barriers were addressed.
Our study has several limitations. First, it was conducted at a single institution with a proprietary EHR; however, we have integrated this platform with our recently implemented vendor EHR (Epic Systems Corp., Verona, Wisc.) by leveraging Epic’s web services (eg, for the treatment team) and an HL7 feed (eg, for admission, discharge, transfer events). Second, we did not measure plan of care concordance; however, assessing user perceptions is an important first step for future adoption. Third, we underestimated the effort required to encourage non-unit-based providers to use the system, a key benefit that we regularly conveyed to the unit-based care team. Despite our staff engagement efforts, reaching out to all potential users was impractical given the limited scope of the pilot. When ambulatory providers did participate, the feedback that we received reinforced the potential value of improving communication across settings (Box 1). Finally, we could not use this platform to communicate with providers who were not affiliated with our health care network. Engaging non-network providers during hospitalization is critical given the potential “voltage drop” of information that occurs during transitions.23,24 Institutions and secure messaging companies could explore how to leverage online directories to communicate with non-network providers.
Box 1. Feedback and comments from survey respondents
“It is a useful idea, but will always suffer from the fact that there is no way that EVERYONE is using this for communication → it doesn’t replace conventional means of communication → it becomes redundant → ie, it’s extra work.”
“Great work! I would encourage this for outpatient and complex medical problems.”
“I have had great difficulty getting outpatient providers to respond to messages especially the specialists. This often leads to having to send an email with the same message a day or 2 later.”
“The biggest issue is that people on other services do not use it.”
“This has to be a hospital-wide initiative to inform/educate people before its use can be reliably/routinely adopted.”
CONCLUSION
Our preliminary evaluation suggests tremendous potential for using this type of approach to improve care team communication in acute care. As institutions adopt secure messaging vendors and/or enterprise social networking applications, they should consider how to integrate these tools with the EHR to pull patient context and synchronize with the EHR-designated care team to facilitate patient-centered messaging similar to what we have described. In the future, these technologies could be expanded to the post–acute care setting and used to coordinate care for at-risk patients enrolled in accountable care organizations.11 Furthermore, it could be integrated into patient portals to facilitate patient-provider communication, as we have previously reported.25 We do not believe the challenges experienced during implementation are insurmountable, but they do underscore the importance of developing a strategy to consolidate various communication technologies. Future studies should examine the impact on key outcomes, including plan of care concordance, costs, and adverse events.
FUNDING
This work was supported by a grant from the Gordon and Betty Moore Foundation (GBMF) and the Patient-Centered Outcomes Research Institute (PCORI). GBMF and PCORI had no role in the design or conduct of the study; collection, analysis, or interpretation of data or preparation or review of the manuscript. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of GBMF or PCORI.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
All authors contributed sufficiently and meaningfully to the conception, design, and conduct of the study; data acquisition, analysis, and interpretation; and/or drafting, editing, and revising of the manuscript. The web-based and mobile applications that comprised the messaging platform used in this study was supported by CareThread, Inc.
REFERENCES
- 1. Coiera E. When conversation is better than computation. J Am Med Inform Assoc. 2000;73:277–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coiera E. Communication systems in healthcare. Clin Biochem Rev. 2006;272:89–98. [PMC free article] [PubMed] [Google Scholar]
- 3. Dayton E, Henriksen K. Communication failure: Basic components, contributing factors, and the call for structure. Jt Comm J Qual Patient Saf. 2007;331:34–47. [DOI] [PubMed] [Google Scholar]
- 4. O'Leary KJ, Thompson JA, Landler MP, et al. Patterns of nurse-physician communication and agreement on the plan of care. Qual Saf Health Care. 2010;193:195–199. [DOI] [PubMed] [Google Scholar]
- 5. Figueroa JF, Schnipper JL, McNally K, Stade D, Lipsitz SR, Dalal AK. How often are hospitalized patients and providers on the same page with regard to the patient's primary recovery goal for hospitalization? J Hosp Med. 2016 doi: 10.1002/jhm.2569. doi: 10.1002/jhm.2569. [DOI] [PubMed] [Google Scholar]
- 6. Collins SA, Bakken S, Vawdrey DK, Coiera E, Currie L. Model development for EHR interdisciplinary information exchange of ICU common goals. Int J Med Inform. 2011;808:e141–e149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wu RC, Tran K, Lo V, et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;8111:723–732. [DOI] [PubMed] [Google Scholar]
- 8. Goyder C, Atherton H, Car M, Heneghan CJ, Car J. Email for clinical communication between healthcare professionals. Cochrane Database Syst Rev. 2015;2:CD007979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Manojlovich M, Adler-Milstein J, Harrod M, et al. The effect of health information technology on health care provider communication: A mixed-method protocol. JMIR Res Protoc. 2015;42:e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Khanna RR, Wachter RM, Blum M. Reimagining electronic clinical communication in the post-pager, smartphone era. JAMA. 2016;3151:21–22. [DOI] [PubMed] [Google Scholar]
- 11. Bates DW. Health information technology and care coordination: the next big opportunity for informatics? Yearb Med Inform. 2015;101:11–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ighani F, Kapoor KG, Gibran SK, et al. A comparison of two-way text versus conventional paging systems in an academic ophthalmology department. J Med Syst. 2010;344:677–684. [DOI] [PubMed] [Google Scholar]
- 13. Przybylo JA, Wang A, Loftus P, Evans KH, Chu I, Shieh L. Smarter hospital communication: Secure smartphone text messaging improves provider satisfaction and perception of efficacy, workflow. J Hosp Med. 2014;99:573–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dalal AK, Dykes P, Schnipper J, Bates D. Transforming the acute care environment: A web-based patient-centered toolkit [abstract]. J Hospital Med. 2014;9 (Suppl 2):694. [Google Scholar]
- 15. Dalal AK, Dykes P, McNally K, et al. Engaging patients, providers, and institutional stakeholders in developing a patient-centered microblog. Proc Am Med Inform Assoc Ann Fall Symp. November 16–19, 2014, Washington DC. [Google Scholar]
- 16. Laxmisan A, Hakimzada F, Sayan OR, Green RA, Zhang J, Patel VL. The multitasking clinician: Decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2007;76(11-12):801–811. [DOI] [PubMed] [Google Scholar]
- 17. Edwards A, Fitzpatrick LA, Augustine S, et al. Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform. 2009;789:629–637. [DOI] [PubMed] [Google Scholar]
- 18. Bornkessel A, Furberg R, Lefebvre RC. Social media: opportunities for quality improvement and lessons for providers: a networked model for patient-centered care through digital engagement. Curr Cardiol Rep. 2014;167:504. [DOI] [PubMed] [Google Scholar]
- 19. Dalal AK, Schnipper JL, Massaro A, McNally K, Dykes P, Bates DW. Improving care team communication: Early experience at implementing a patient-centered microblog. Proc Am Med Inform Assoc Ann Fall Symp. 2015 November 14–18, San Francisco, Calif. [Google Scholar]
- 20. Dalal AK, Schnipper JL. Care team identification in the electronic health record: a critical first step for patient-centered communication. J Hosp Med. 2016;115:381–385. [DOI] [PubMed] [Google Scholar]
- 21. Wells S, Rozenblum R, Park A, Dunn M, Bates DW. Organizational strategies for promoting patient and provider uptake of personal health records. J Am Med Inform Assoc. 2015;221:213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wu R, Lo V, Morra D, et al. A smartphone-enabled communication system to improve hospital communication: Usage and perceptions of medical trainees and nurses on general internal medicine wards. J Hosp Med. 2015;102:83–89. [DOI] [PubMed] [Google Scholar]
- 23. Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;2978:831–841. [DOI] [PubMed] [Google Scholar]
- 24. Tang N. A primary care physician's ideal transitions of care? Where's the evidence? J Hospital Med. 2013;88:472–477. [DOI] [PubMed] [Google Scholar]
- 25. Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluation. J Am Med Inform Assoc. 2016;231:80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]