Abstract
Background: Access to online patient portals is key to improving care, but we have limited understanding of patient perceptions of online portals and the characteristics of people who use them.
Methods: Using a national survey of 3677 respondents, we describe perceptions and utilization of online personal health information (PHI) portals.
Results: Most respondents (92%) considered online PHI access important, yet only 34% were offered access to online PHI by a health care provider, and just 28% accessed online PHI in the past year. While there were no differences across race or ethnicity in importance of access, black and Hispanic respondents were significantly less likely to be offered access (P = .006 and <.001, respectively) and less likely to access their online PHI (P = .041 and <.001, respectively) compared to white and non-Hispanic respondents.
Conclusion: Health care providers are crucial to the adoption and use of online patient portals and should be encouraged to offer consistent access regardless of patient race and ethnicity.
Keywords: electronic medical records, personal health information, digital divide, patient-physician communication
INTRODUCTION
Online patient access to personal health records has the potential to improve health and health care outcomes.1–3 When patients read their personal medical records, it can improve patient-provider communication, the patient’s experience of care, diabetes control, smoking cessation, and the patient’s physical function and quality of life.4–9 Studies of OpenNotes, a national initiative that gives patients access to doctors’ clinical visit notes, demonstrate that when they view their notes, they are more informed about their care, remember what to discuss during doctor visits, feel more in control of their medical care, and improve their medication adherence.3,10
Despite major federal investments to improve the infrastructure supporting patient access to online personal health information (PHI), many patients, especially those in lower socioeconomic groups, are not using these services.11–13 Previous research has found sex, race, and age disparities among patients accessing online PHI.14,15 Concern that the “digital divide” is increasing health disparities is understandable, given that Internet access has historically been limited for those with fewer economic and social resources. However, this is rapidly changing. In a 2015 Pew survey of Americans’ Internet adoption, the gaps in Internet use based on education, income, and racial and ethnic differences had all steadily decreased.16 For example, 78% of African Americans routinely used the Internet in 2015, compared with 85% of whites. In 2000, 38% of African Americans routinely used the Internet, compared with 53% of whites. Although Internet use has increased, we have limited evidence of the impact of rapid adoption on access and engagement with PHI by different demographic groups.
Our primary objective was to evaluate perspectives and patterns of technology use by demographic characteristics. We measured the association between patient-level demographic characteristics (education, race/ethnicity, geographic location) and patient interest in, access to, and engagement with online PHI using the Health Information National Trends Survey (HINTS), a US population-based health care use survey.17,18 We describe patient perceptions of online PHI access and characteristics of patients who are offered and who access this information.
METHODS
The HINTS survey, fielded between August and November 2014, is the data source for this study. HINTS is a national survey conducted periodically to identify and track trends in access and sources for health-related information, health-related behaviors, perceptions, and knowledge. Details of the survey methods are available at the HINTS website.19 Briefly, the HINTS survey process involved developing a sampling frame composed of noninstitutionalized people ages 18 years and older in the United States using a stratified sampling method defined by: (1) areas with high concentrations of minorities, (2) areas with low concentrations of minorities, and (3) areas in central Appalachia regardless of minority concentration. Survey invitees received up to 3 questionnaire mailings and a reminder postcard as needed. The questionnaire was available in both English and Spanish.
The survey used probability sampling to improve representation of specific groups, thus our analysis applied weights to calculate US population estimates and standard errors. Weight adjustment accounted for nonresponse and known population totals based on data from the 2013 American Community Survey (US Census Bureau) on age, sex, education, marital status, race, ethnicity, and Census region. Prior to establishing weights, missing data for these variables were replaced using a hot-deck imputation method.20 Replicate weights were computed using the jackknife replication method.21
Survey questions used in this analysis are shown in Appendix A. The survey queried participants about demographic characteristics and their views on the importance of having access to medical records online, whether access had been offered by a health care provider, and whether they accessed their online PHI via a patient portal. For the analysis, we included all respondents who supplied information for the 3 primary study questions (importance of online PHI access, being offered access, and accessing their PHI online). For analysis of the perception of how important it is to have access to one’s own online PHI, the responses “very important” and “somewhat important” were combined and compared to “not at all important.”
We compared respondents across demographic characteristics to identify differences among participants who: (1) thought online PHI access was important or not, (2) were offered access by their health care provider or not, and (3) accessed their online PHI in the past year or not. Weighted percentages are presented. The Wald chi-square test was used to test for significance. Logistic regression was used to determine the strongest demographic predictors. Individual predictors with an association P < .05 were included in the multivariable model with the exception of income, because >10% of respondents had missing data for this item. All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
The August to November 2014 HINTS survey was mailed to 13 996 addresses and had a 34.4% weighted response rate (n = 3677). After adjusting for oversampling of addresses in high-minority areas, the response rate ranged from 25.9% in the high-minority stratum to 37.2% in the low-minority stratum. Five percent of respondents (n = 185) did not answer at least 1 of the primary questions and were not included in the analysis; these respondents were found to be older, retired, and with lower income compared to the respondents included in our analysis.
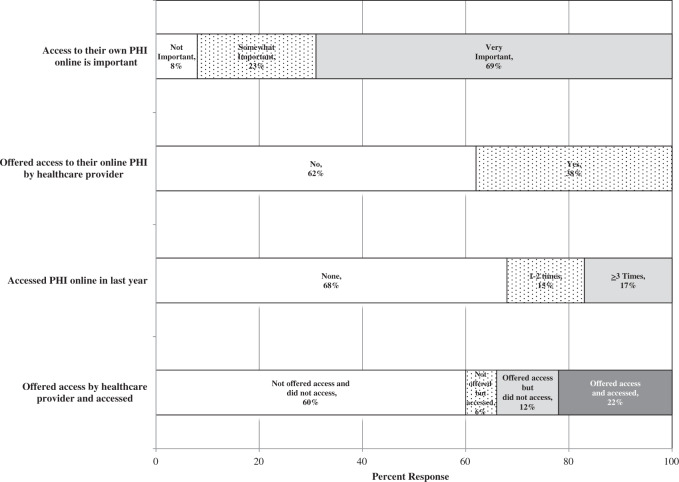
Of the 3492 survey participants responding to the 3 primary online PHI questions, a majority (92%) indicated that they felt access to their PHI online was very or somewhat important; just over a third (34%) reported being offered electronic access to their PHI by their health care provider (Figure 1). Less than a third (28%) reported accessing their own PHI online through a secure website or phone application. Respondents who accessed their own PHI online were significantly more likely to report being offered access by their health care provider (P < .001).
Figure 1.
US adult patient perceptions and access to online personal health information via patient portals.
Demographic characteristics are shown in Table 1 by respondents’ perception of importance of online PHI access, whether they were offered access, and by engagement in patient portal use. Interestingly, while there were no differences across race or ethnicity in reported importance of access (P = .59 and .67, respectively), there were significant differences across race and ethnicity in terms of who was offered access by their health care provider (P = .006 and <.001, respectively) and who accessed their PHI online (P = .041 and <.001, respectively).
Table 1.
Weighted US respondent characteristics by value, health care provider offering, and patient engaging in access of online PHI
| Getting your own medical information electronically is important |
Health care provider offered access to online PHI |
Accessed PHI online in past 12 months |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Respondent Characteristics | Total a | Yes % | No % | P-valueb | Yes % | No % | P-valueb | Yes % | No % | P-valueb |
| 3194 (92) | 298 (8) | 1188 (34) | 2304 (66) | 932 (28) | 2560 (72) | |||||
| Age | ||||||||||
| 18–34 | 31 | 32 | 20 | 32 | 31 | 36 | 30 | |||
| 35–49 | 27 | 27 | 24 | 24 | 28 | 29 | 26 | |||
| 50–64 | 25 | 26 | 18 | 29 | 23 | 23 | 26 | |||
| 65–74 | 10 | 9 | 13 | 9 | 10 | 9 | 10 | |||
| ≥75 | 7 | 6 | 24 | <.001 | 5 | 8 | <.001 | 3 | 9 | <.001 |
| Race | ||||||||||
| White | 78 | 77 | 82 | 78 | 78 | 79 | 77 | |||
| Black | 13 | 13 | 10 | 10 | 15 | 10 | 14 | |||
| Multi | 2 | 2 | 2 | 3 | 2 | 2 | 3 | |||
| Other | 7 | 7 | 5 | 0.59 | 9 | 5 | 0.006 | 9 | 6 | 0.041 |
| Hispanic ethnicity | ||||||||||
| Hispanic | 15 | 15 | 17 | 9 | 18 | 8 | 17 | |||
| Not Hispanic | 85 | 85 | 83 | 0.67 | 91 | 82 | <.001 | 92 | 83 | <.001 |
| Gender | ||||||||||
| Male | 49 | 49 | 45 | 45 | 50 | 48 | 49 | |||
| Female | 51 | 51 | 55 | 0.37 | 55 | 50 | 0.13 | 52 | 51 | 0.97 |
| Marital status | ||||||||||
| Married/living as | 57 | 57 | 53 | 60 | 55 | 59 | 56 | |||
| Other | 43 | 43 | 47 | 0.40 | 40 | 45 | 0.098 | 41 | 44 | 0.33 |
| Education | ||||||||||
| <High school | 11 | 10 | 18 | 6 | 13 | 4 | 14 | |||
| High school graduate | 18 | 17 | 24 | 10 | 22 | 8 | 22 | |||
| Some college | 30 | 30 | 29 | 30 | 30 | 31 | 30 | |||
| College graduate | 41 | 42 | 29 | 0.018 | 53 | 34 | <.001 | 57 | 34 | <.001 |
| Household income | ||||||||||
| <$20k | 19 | 19 | 25 | 12 | 23 | 9 | 23 | |||
| $20k to <$35k | 13 | 12 | 16 | 9 | 14 | 9 | 14 | |||
| $35k to <$50k | 15 | 14 | 17 | 12 | 16 | 12 | 16 | |||
| $50k to <$75k | 18 | 17 | 20 | 19 | 17 | 18 | 17 | |||
| ≥$75k | 36 | 37 | 22 | 0.007 | 48 | 30 | <.001 | 51 | 30 | <.001 |
| Employment | ||||||||||
| Employed/homemaker | 66 | 67 | 58 | 67 | 66 | 70 | 65 | |||
| Retired | 16 | 15 | 29 | 16 | 16 | 12 | 17 | |||
| Unemployed/student/disabled | 18 | 19 | 13 | <.001 | 17 | 18 | 0.90 | 18 | 18 | 0.002 |
| General health | ||||||||||
| Poor | 2 | 2 | 3 | 2 | 2 | 1 | 2 | |||
| Fair | 11 | 10 | 20 | 8 | 12 | 7 | 12 | |||
| Good | 39 | 39 | 35 | 36 | 40 | 36 | 40 | |||
| Very good | 35 | 35 | 35 | 39 | 33 | 40 | 34 | |||
| Excellent | 13 | 14 | 6 | <.001 | 15 | 12 | 0.044 | 15 | 12 | 0.004 |
| Census region | ||||||||||
| Northeast | 18 | 18 | 21 | 16 | 19 | 16 | 19 | |||
| Midwest | 22 | 22 | 19 | 24 | 20 | 22 | 22 | |||
| South | 37 | 37 | 39 | 32 | 40 | 35 | 38 | |||
| West | 23 | 23 | 21 | 0.66 | 27 | 21 | 0.010 | 27 | 21 | 0.16 |
| Urban/rural designation in 2013 | ||||||||||
| Metropolitan | 85 | 86 | 81 | 89 | 83 | 92 | 83 | |||
| Nonmetropolitan | 15 | 14 | 19 | 0.15 | 11 | 17 | 0.004 | 8 | 17 | <.001 |
aReported percentages are rounded to the nearest whole number and may not sum to 100%.
bP-value for Wald chi-square test for independence.
Older, non-white, Hispanic, less educated, lower income respondents with poor self-reported health and living in nonmetropolitan areas and in the Northeast or South reported being offered portal access less often (all P < .05). Similar trends were seen regarding whether respondents accessed their PHI online, although Census region was not significantly associated with online access, and employment status was found to be significant. Sensitivity analysis was performed, restricted to a smaller cohort of respondents who reported seeing a provider in the last year (and thus had a recent opportunity to be offered access and to have new clinical information to access), and the results were the same (data not shown).
Logistic regression results indicate that several demographic characteristics remain significantly associated with patients being offered online access and those accessing their PHI online after adjusting for covariates (Table 2). Individuals 75 years and older were significantly less likely to access online PHI than younger respondents 18 to 34 years of age (odds ratio (OR) = 0.41 75 or older vs 18–34). Black respondents indicated being offered access to their online PHI significantly less often than white respondents (OR = 0.59; 95% confidence interval [CI], 0.42-0.84) and accessing online PHI significantly less often (OR = 0.58; 95% CI, 0.37-0.90). Hispanics reported being offered access and accessing their own PHI online significantly less often (OR = 0.47; 95% CI, 0.32-0.68 and OR = 0.50; 95% CI: 0.29-0.85, respectively) than non-Hispanics. College graduates were significantly more likely to report being offered access and accessing online PHI compared with less educated respondents. Differences were also noted by geographic location. Respondents in the Northeast and South were significantly less likely (OR = 0.60; 95% CI, 0.38-0.94 and OR = 0.67; 95% CI, 0.46-0.98, respectively) to be offered access than respondents in the West. Respondents in metropolitan areas were more likely to access (OR = 1.81; 95% CI: 1.09-3.00).
Table 2.
Respondent characteristics most influential in predicting who is offered access by health care providers and who accesses their online PHI
| Health care provider offered access to online PHI | Accessed PHI online in past 12 months | |
|---|---|---|
| Respondent Characteristics | Adjusted odds ratio (confidence interval)a | Adjusted odds ratio (confidence interval) a |
| Age | ||
| 18–34 | 1 | 1 |
| 35–49 | 0.94 (0.63, 1.42) | 1.03 (0.74, 1.42) |
| 50–64 | 1.42 (0.96, 2.10) | 0.89 (0.63, 1.26) |
| 65–74 | 1.09 (0.66, 1.80) | 0.90 (0.59, 1.37) |
| ≥75 | 0.79 (0.46, 1.37) | 0.41 (0.21, 0.83) |
| Race | ||
| White | 1 | 1 |
| Black | 0.59 (0.42, 0.84) | 0.58 (0.37, 0.90) |
| Multi | 1.49 (0.70, 3.18) | 0.78 (0.40, 1.52) |
| Other | 1.61 (0.83, 3.09) | 1.13 (0.58, 2.21) |
| Hispanic ethnicity | ||
| Hispanic | 0.47 (0.32, 0.68) | 0.50 (0.29, 0.85) |
| Not Hispanic | 1 | 1 |
| Education | ||
| <High school | 0.28 (0.15, 0.55) | 0.21 (0.09, 0.48) |
| High school graduate | 0.33 (0.23, 0.48) | 0.26 (0.17, 0.40) |
| Some college | 0.64 (0.45, 0.89) | 0.61 (0.43, 0.88) |
| College graduate | 1 | 1 |
| Census region | ||
| Northeast | 0.60 (0.38, 0.94) | 0.60 (0.38, 0.96) |
| Midwest | 0.96 (0.66, 1.41) | 0.80 (0.51, 1.25) |
| South | 0.67 (0.46, 0.98) | 0.76 (0.49, 1.17) |
| West | 1 | 1 |
| Urban/rural designation in 2013 | ||
| Metropolitan | 1.54 (0.99, 2.40) | 1.81 (1.09, 3.00) |
| Nonmetropolitan | 1 | 1 |
aAdjusted odds ratios and 95% confidence intervals generated from multivariable logistic models including all characteristics listed in Table 2 as well as employment and general health. Model accounts for replicate weights.
Bold indicates Odds Ratios that are significantly different from the comparison group.
DISCUSSION
This study found that a majority of US adults (92%) consider online access to their own PHI important. No difference in enthusiasm was noted by race or socioeconomic status. Despite the overwhelming perception that online PHI holds value, we also noted concerning differences in who is being offered access by health care providers and who is using these portals; individuals who are older, in poor health, poorly educated, and members of ethnic/racial minority groups were less likely to be offered or to use portal access. Just one third of respondents indicated that their health care provider offered them access to their records. Any benefits associated with access to patient portals will be less likely to accrue if not offered and used. Of concern is our finding that health care providers offered access in an inconsistent manner, significantly less often to black and Hispanic individuals than to white and non-Hispanic individuals.
The discrepancy between those offered access and those who actually engaged appears to fall along the lines typically defined as the digital divide.22,23 Younger, more educated white adults are more frequently offered an invitation to access their PHI online and are therefore more likely to engage in this behavior.
For the analysis, we required respondents to answer the primary survey questions regarding importance of online PHI access, being offered access, and accessing their PHI online. This eliminated 5% of respondents who had missing responses for at least 1 of these survey questions. Respondents who did not answer these questions, compared to those who did, were older, more likely to be retired, and with lower income. Removing these cases from our analysis likely reduced the strength of the differences seen.
Little is known about the effects of the patient-provider relationship on consumer health information technology acceptance and use. These findings are consistent with prior work also noting the important influence of clinicians in patient adoption of online PHI portals.24 Our work includes a broader US population and moves beyond reported intentions to patients’ reports of accessing their PHI. Future work should attempt to measure actual use of portals and varying levels of patient-provider engagement.
This study has several limitations. Although the survey used a national sample and involved stratified selection to improve the responses of population subgroups, the response rate was low and respondents may not be representative of the US population as a whole. Survey question wording could also be interpreted different ways. It is not known if patients sought care at facilities that offer online access to PHI. Facilities offering online PHI may vary in terms of patient demographics compared to facilities that do not offer access. Disparities identified here may result from health care providers working in areas without an online PHI portal, or without an activated portal, as differences were seen across Census regions after adjusting for other significant predictors. The demands of complying with the federal Meaningful Use Incentive Program25 and regulatory demands may play a role, as they require use of many features and creation of reports. Access to more detailed data, including information about the specific patient-physician relationship, may help shed light on the study results presented here.
Our results note overwhelming enthusiasm among this study sample regarding online PHI, yet suggest a concerning variation in who is being offered access and who is accessing their PHI online. Further exploration of the factors limiting patient access to online PHI is an appropriate next step in reaching the goal of engaging all patients in their health care. The health care provider may be a key factor affecting current patient electronic access patterns. Encouraging physicians and other health care providers to openly discuss this technology and promote access is vital to ensuring that patients both use and benefit from accessing their PHI online.26
FUNDING
This work was supported by the Robert Wood Johnson Foundation, Gordon and Betty Moore Foundation, Peterson Center on Healthcare, and Cambia Health Foundation.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
All authors participated in study design, manuscript preparation, and editing. All authors read and approved the final manuscript. All authors agree to be accountable for all aspects of the work. S.P. drafted the manuscript and conducted the data analysis.
REFERENCES
- 1. Ross SE, Lin CT. The effects of promoting patient access to medical records: a review. J Am Med Inform Assoc. 2003;102:129–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Honeyman A, Cox B, Fisher B. Potential impacts of patient access to their electronic care records. Inform Prim Care. 2005;131:55–60. [DOI] [PubMed] [Google Scholar]
- 3. Delbanco T, Walker J, Bell SK, et al. Inviting patients to read their doctors' notes: a quasi-experimental study and a look ahead. Ann Intern Med. 2012;1577:461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bronson DL, O'Meara K. The impact of shared medical records on smoking awareness and behavior in ambulatory care. J Gen Intern Med. 1986;11:34–37. [DOI] [PubMed] [Google Scholar]
- 5. Greenfield S, Kaplan SH, Ware JE, Jr, Yano EM, Frank HJ. Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;35:448–457. [DOI] [PubMed] [Google Scholar]
- 6. Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care. 2009;322:234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bronson DL, Costanza MC, Tufo HM. Using medical records for older patient education in ambulatory practice. Med Care. 1986;244:332–339. [DOI] [PubMed] [Google Scholar]
- 8. Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. 1985;1024:520–528. [DOI] [PubMed] [Google Scholar]
- 9. DesRoches C. Progress and challenges in electronic health record adoption: findings from a national survey of physicians. Ann Intern Med. 2015;1625:396. [DOI] [PubMed] [Google Scholar]
- 10. OpenNotes. http://www.myopennotes.org/what-is-opennotes-2/why-open-visit-notes/. Accessed December 10, 2015. [Google Scholar]
- 11. Steinbrook R. Health care and the American Recovery and Reinvestment Act. N Engl J Med. 2009;36011:1057–1060. [DOI] [PubMed] [Google Scholar]
- 12. Blumenthal D, Dixon J. Health-care reforms in the USA and England: areas for useful learning. Lancet. 2012;3809850:1352–1357. [DOI] [PubMed] [Google Scholar]
- 13. US Status Law. Health Insurance Portability and Accountability Act of 1996. Public Law 104-191. United States; 1996:1936–2103. [PubMed] [Google Scholar]
- 14. Chang BL, Bakken S, Brown SS, et al. Bridging the digital divide: reaching vulnerable populations. J Am Med Inform Assoc. 2004;116:448–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yamin CK, Emani S, Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171 6:568–574. [DOI] [PubMed] [Google Scholar]
- 16. Perrin A DM. Americans' Internet Access: 2000-2015. Pew Res Cent Internet Sci Tech. Pew Research Center; 2015. www.perinternet.org. Accessed May 10, 2015. [Google Scholar]
- 17. Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;95:443–460; discussion 81-84. [DOI] [PubMed] [Google Scholar]
- 18. Hesse BW, Moser RP, Rutten LJ, Kreps GL. The Health Information National Trends Survey: research from the baseline. J Health Commun. 2006;11 (Suppl 1):vii–xvi. [DOI] [PubMed] [Google Scholar]
- 19. National Cancer Institute. National Cancer Institute's Health Information National Trends Survey (HINTS). http://hints.cancer.gov/default.aspx. Accessed December 4, 2015. [Google Scholar]
- 20. Andridge RR, Little RJ. A Review of Hot Deck Imputation for Survey Non-response. Int Stat Rev. 2010;781:40–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Krewski D, Rao JNK. Inference from Stratified Samples: Properties of the Linearization, Jackknife and Balanced Repeated Replication Methods. Ann Stat. 1981;95:1010–1019. [Google Scholar]
- 22. Brodie M, Flournoy RE, Altman DE, Blendon RJ, Benson JM, Rosenbaum MD. Health information, the Internet, and the digital divide. Health Aff (Millwood). 2000;196:255–265. [DOI] [PubMed] [Google Scholar]
- 23. Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res. 2014;167:e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nazi KM. The personal health record paradox: health care professionals' perspectives and the information ecology of personal health record systems in organizational and clinical settings. J Med Internet Res. 2013;154:e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Blumenthal D. Launching HITECH. N Engl J Med. 2010;3625:382–385. [DOI] [PubMed] [Google Scholar]
- 26. Gillum RF. From Papyrus to the electronic tablet: a brief history of the clinical medical record with lessons for the digital age. Am J Med. 2013;12610:853–857. [DOI] [PubMed] [Google Scholar]