Abstract
Objective: Follow-up with a primary care provider after hospital discharge has been associated with a reduced likelihood of readmission. However, primary care providers are frequently unaware of their patients’ hospitalizations. Event notification may be an effective tool for reducing readmissions by notifying primary care providers when their patients have been admitted to and discharged from a hospital.
Materials and Methods: We examined the effect of an event notification system on 30-day readmissions in the Bronx, New York. The Bronx has among the highest readmission rates in the country and is a particularly challenging setting to improve care due to the low socioeconomic status of the county and high rates of poor health behaviors among its residents. The study cohort included 2559 Medicare fee-for-service beneficiaries associated with 14 141 hospital admissions over the period January 2010 through June 2014. Linear regression models with beneficiary-level fixed-effects were used to estimate the impact of event notifications on readmissions by comparing the likelihood of rehospitalization for a beneficiary before and after event notifications were active.
Results: The unadjusted 30-day readmission rate when event notifications were not active was 29.5% compared to 26.5% when alerts were active. Regression estimates indicated that active hospitalization alert services were associated with a 2.9 percentage point reduction in the likelihood of readmission (95% confidence interval: −5.5, −0.4).
Conclusions: Alerting providers through event notifications may be an effective tool for improving the quality and efficiency of care among high-risk populations.
Keywords: Medicare, health information exchange, readmissions
INTRODUCTION
Primary care providers in the United States often have little or no information about hospitalizations of their patients.1 These information gaps may reduce providers’ ability to coordinate services for their patients, leading to poorer quality of care, including higher rates of readmission.
Event notifications may help improve care coordination, leading to smoother transitions by increasing primary care providers’ awareness of hospitalizations.2–4 Also referred to as automatic alerts or subscription services, event notification systems automate real-time electronic messaging to subscribed providers. Event notifications can be deployed for a variety of patient services, but a common application is for hospitalizations and emergency department visits. Drawing on a hospital’s admission-discharge-transfer system, an event notification system sends messages to a primary care provider or case manager when a patient has been admitted or discharged from a hospital.5 The notifications also identify the organization treating the patient.3 This provides an opportunity to better coordinate postdischarge care.4,6
Prior studies suggest that health care providers believe that event notifications can improve care.4,6–8 Event notifications for patients with human immunodeficiency virus have been associated with increased re-engagement with care services and improved clinical indicators.9 However, a limited number of quantitative evaluations of event notifications did not find an effect on postdischarge visits to primary care providers, readmissions, or emergency department revisits.10,11
In this study, we sought to evaluate the effect of event notifications on readmissions of Medicare fee-for-service (FFS) beneficiaries in the Bronx, New York. Readmissions of Medicare beneficiaries are common, costly, and may reflect poor quality of care.12 Physician follow-up after hospital discharge may improve the coordination of care for patients and has been linked to lower odds of readmission.13 The Bronx is a particularly challenging setting in which to improve care due to the low socioeconomic status of the county and high rates of poor health behaviors among its residents.14,15 These factors likely contribute to the county’s readmissions rates, which are among the highest in the country.16 It is not known whether an event notification system is an effective intervention to reduce readmissions in this setting.
METHODS
Setting
As part of a Centers for Medicare and Medicaid Services award, the project described was supported by grant number 1C1CMS331065 from the Department of Health and Human Services, Centers for Medicare & Medicaid Services. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented here was conducted by the awardee. Findings might or might not be consistent with or confirmed by the findings of the independent evaluation contractor.
We examined the effect of event notifications provided by the Bronx Regional Health Information Organization (RHIO) on 30-day readmissions of Medicare FFS beneficiaries over the period January 2010 through June 2014. Established in 2005, the Bronx RHIO is a nonprofit organization that facilitates health information exchange (HIE) services for more than 60 inpatient and ambulatory care organizations in New York City.
The Bronx RHIO’s event notification system was launched in December 2011. Subscribing providers and organizations are alerted when their patients have emergency department visits, hospital admissions, or hospital discharges via secure email or HL7 messages. The Bronx RHIO’s event notification system uses the admission-discharge-transfer feeds from participating hospitals to identify events. Each subscribing provider may manage event notification messages differently. The individual messages and actions may be managed by clinicians, case managers, or other staff. During the study period, 11 different organizations in the Bronx subscribed patients to the event notification system. These organizations included an Accountable Care Organization (ACO), ambulatory care practices, home health agencies, and integrated service delivery organizations.
For patients who have actively consented to have their information shared by the Bronx RHIO, providers and health care organizations are able to request event notification services (i.e., the providers “subscribe”). Subscriptions to event notification services are initiated either by the organization identifying specific patients for enrollment or by establishing criteria and rules for the Bronx RHIO to apply to automatically enroll patients. The former subscription method accounts for the majority of all active event notification enrollments (> 75%), and a patient’s inclusion may be active or inactive over time. Among all patients with event notification services, about 55% are subscribed on an ongoing basis. For the remainder, the average time with active event notification enrollment was 3.1 months. Additional details of the Bronx RHIO’s event notification system have previously reported.2
Subjects
All records for Medicare FFS beneficiaries in the Bronx RHIO’s centralized data repository (i.e., beneficiaries who had sought care from a provider participating in the Bronx RHIO) were linked to Medicare claims. Centers for Medicare and Medicaid Services provided synthetic identifiers based on each beneficiary’s social security number, gender, and date of birth supplied by the Bronx RHIO. This initial linkage identified 293 158 claims for inpatient admissions (Supplementary Appendix). From this set of claims, we excluded admissions that could not be linked on all 3 identifiers (5.2% excluded), those for services that took place outside of the study period (7.4% excluded), and any for beneficiaries who never consented to inclusion in the Bronx RHIO (57% excluded). Of the remaining 88 845 admissions, the study cohort was further limited to beneficiaries subscribed to event notifications by a provider participating in the Bronx RHIO. Claims included records of beneficiaries’ use of health care services at both participating and nonparticipating providers in New York and elsewhere. We further excluded hospitalizations with negative lengths of stay (i.e., coding errors), those with a length of stay > 20 days to reduce the influence of outliers, and beneficiaries who died within 30 days of discharge to account for the competing risk of mortality. The study cohort included 14 141 hospital admissions among 2559 beneficiaries. Additional information about the study cohort can be found in the Supplementary Appendix.
Measures
Our outcome measure was an indicator for all-cause 30-day readmission. The unit of analysis was the hospitalization and, therefore, a readmission could serve as an index admission for a subsequent readmission. The determinant of interest was an indicator of a beneficiary’s enrollment in the Bronx RHIO’s event notification system during an inpatient admission. The Bronx RHIO supplied the dates for all beneficiaries for whom event notifications were active.
Patient-level explanatory variables included demographic characteristics (age, gender, race), length of stay,17 and a risk-adjustment index based on Elixhauser comorbidities.18 Hospitals were identified using national provider identifiers.
Analysis
Unadjusted comparisons were made between beneficiaries with event notifications and all other Medicare FFS beneficiaries included in the Bronx RHIO’s centralized data repository without event notifications using means and t-tests. The chi-square test for linear trend was used to measure changes in annual readmission rates.
We also fit linear probability models with beneficiary-level fixed effects to estimate the association between event notifications during hospitalization and subsequent readmissions. This approach compared the likelihood of readmission for a beneficiary when event notifications were not active to the same beneficiary when event notifications were active. Since beneficiaries served as their own controls, the regression models did not include time-invariant characteristics such as gender or race/ethnicity, but did include age and the Elixhauser comorbidity index, which may have been different for each admission. Regression models also included indicators for the year and quarter of admission to control for secular trends, and robust standard errors were adjusted for clustering at the level of the hospital.
Potential cost savings associated with event notifications were also estimated.19 The difference between inpatient utilization rates when event notifications were and were not present was multiplied by the total number of admissions with active event notifications. This provided an estimated number of potentially avoided readmissions attributable to event notifications. Multiplying by the median Medicare reimbursement to hospitals in our sample provided an estimate of cost savings due to potentially avoided readmissions.
Secondary analyses
Eight additional analyses were conducted to explore possible alternative explanations for our primary findings and to assess potential sources of bias. (1) We examined the possibility that our findings were attributable to other internal mechanisms to notify primary care providers of patients’ hospitalizations by excluding admissions where the admitting and the readmitting hospital were part of the same entity.2 (2) Stratified analyses based on subscribers' ACO status were conducted. ACOs may have other ways of actively communicating admission and discharge information to outpatient providers such as dedicated staff or other shared information systems. The impact of our 20-day length of stay exclusion criteria was examined by (3) including admissions with longer stays, up to 30, 40, and 50 days. (4) Beneficiaries who died within 30 days of discharge were included in the sample to examine whether differential mortality rates may have affected our estimates. (5) Observations from 2014 were excluded since we only had 6 months of claims for the year and some claims may not have been adjudicated. (6) We examined a sample limited to Medicare-Medicaid dual-eligibles since this population tends to be affected by fragmentation in care to a greater degree than the broader Medicare population.20–22 (7) Same-day readmissions were treated as a single hospitalization since procedures to respond to alerts were frequently designed to facilitate provider follow-up with patients within 2 to 3 days of discharge and not necessarily on the same day.2,4,23 Lastly, (8) the effects of event notifications were examined using the entire sample of consented Medicare FFS beneficiaries in the Bronx.
RESULTS
Medicare FFS beneficiaries enrolled in event notifications by the Bronx RHIO compared to other Medicare FFS beneficiaries in the Bronx
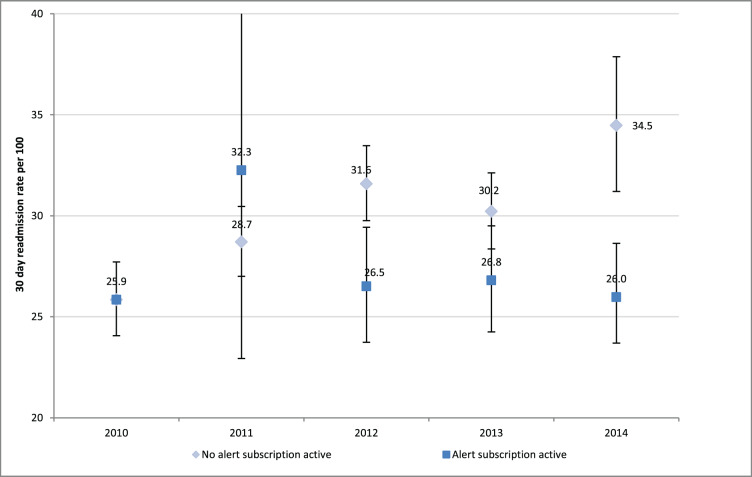
Event notifications were active for 25.4% of admissions. Beneficiaries enrolled in event notifications tended to be older and more racially/ethnically diverse and have higher comorbidity measures compared to other hospitalized beneficiaries in the Bronx who were not enrolled in event notification services (Table 1). Beneficiaries with event notifications were also more likely to be dual-eligibles than beneficiaries who were not enrolled in them. Compared to all Medicare FFS beneficiaries in the Bronx who were not enrolled in event notifications, the annual 30-day readmission rate was higher among the study cohort. A statistically significant upward trend in 30-day readmissions was observed among participants prior to the implementation of event notifications in December of 2011 (χ2 test, P = .02). Medicare FFS beneficiaries in the Bronx who were excluded from the study cohort had higher readmission rates in the last half-year of the study (2014), but the change in trend was not statistically significant (P = .25).
Table 1.
Demographic characteristics of Medicare fee-for-service (FFS) beneficiaries who enrolled in event notifications (study cohort) compared to all other hospitalized FFS beneficiaries in the Bronx (2010–2014)
| Characteristics | Study panel | Other hospitalized FFS beneficiaries in the Bronx |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| (n = 2559) | (n = 75 991) | |
| Age | 72.73 (14.34) | 70.92 (15.11) |
| Sex (male) | 0.31 (0.46) | 0.41 (0.49) |
| Race/ethnicity | ||
| White non-Hispanic | 0.40 (0.49) | 0.54 (0.50) |
| African American non-Hispanic | 0.37 (0.48) | 0.28 (0.45) |
| Other non-Hispanic | 0.05 (0.23) | 0.06 (0.24) |
| Hispanic | 0.17 (0.37) | 0.12 (0.32) |
| Elixhauser score | 2.91 (1.55) | 2.40 (1.53) |
| Length of stay (in days) | 5.23 (3.98) | 4.96 (4.04) |
| Medicaid dual eligible | 0.69 (0.46) | 0.57 (0.49) |
| Annual readmission rates | ||
| 2010 | 25.58 (0.44) | 24.45 (0.43) |
| 2011 | 28.83 (0.45) | 24.39 (0.43) |
| 2012 | 30.17 (0.46) | 24.32 (0.43) |
| 2013 | 29.11 (0.45) | 24.39 (0.43) |
| 2014 | 29.10 (0.45) | 25.06 (0.43) |
Information from the beneficiary’s first admission was used to calculate means and standard deviations. All differences were statistically significant with P < .001 except for “Other non-Hispanic” (P = .076) and 2010 readmission rates (0.064).
Association between event notifications and readmissions
When event notifications were not active during an admission, the unadjusted 30-day readmission rate among the study cohort was 29.5% (95% confidence interval [CI], 28.7–30.4) compared to 26.5% (95% CI: 25.1–28.0) when alerts were active. In our primary regression analysis, the presence of active event notifications was associated with a 2.9 percentage point reduction in the likelihood of readmission (95% CI,−5.5, −0.4, P = .024). This represents a 9.8% decline relative to the unadjusted baseline rate of 29.5%.
Stratified and secondary analyses
The results of secondary analyses were consistent with our primary analysis (Table 2). After (1) excluding hospitalizations at facilities within the same system, active event notifications were associated with a 3.2 percentage point reduction in readmissions (95% CI, −5.3, −0.1, P = .003). (2) Stratification by ACO status was done to test whether the estimated effects of event notifications could be explained by other methods of communication, other information technology (IT) systems, or other formal relationships between providers inherent in ACOs. Event notifications were associated with reductions in readmissions among beneficiaries not subscribed by an ACO, suggesting that other activities associated with an ACO were not driving our results. Among beneficiaries participating in an ACO, the estimated effect of event notifications was not statistically significant, which may have been due to measurement error arising from activities other than event notifications undertaken by the ACO to reduce readmissions. Estimates from analyses that (3) included admissions with stays > 20 days and (4) that did not exclude patients who died within 30 days of discharge were consistent with those from our primary analysis. Larger reductions in readmission rates associated with active event notifications were seen after (5) excluding admissions from 2014 (β = −3.5 percentage points, 95% CI, −5.5, −1.4) and (6) when the analysis was limited to dually eligible beneficiaries (β = −3.2 percentage points, 95% CI, −6.1, −0.3, P = .031). When (7) same-day readmissions were combined with index hospitalizations, the estimate was nearly identical to our primary analysis. Lastly, the association between event notifications and readmissions in our (8) analysis of all Medicare FFS beneficiaries in the Bronx was in the same direction as our primary analysis but did not achieve statistical significance (β = −1.2 percentage-points, 95% CI,−2.7, 0.0, P = .133).
Table 2.
Results of additional analyses of the association between active event notification services and 30-day readmissions
| β (95% CI) | P-value | |
|---|---|---|
| Primary analysis | −0.029 (−0.055, −0.040) | .024 |
| (1) Excluding readmissions to same organization | −0.032 (−0.053, −0.011) | .003 |
| (2) Excluding beneficiaries subscribed by an ACO | −0.041 (−0.060, −0.022) | .001 |
| Limited to beneficiaries subscribed by an ACO | −0.048 (−0.113, 0.018) | .150 |
| (3) Variable lengths of stay | ||
| ≤ 30 days | −0.029 (−0.056, −0.002) | .035 |
| ≤ 40 days | −0.029 (−0.054, −0.004) | .022 |
| ≤ 50 days | −0.028 (−0.052, −0.003) | .027 |
| (4) Sample including patients who died within 30 days | −0.033 (−0.056, −0.010) | .005 |
| (5) Excluding observations from 2014 | −0.035 (−0.055, −0.014) | .001 |
| (6) Limited to beneficiaries who were dually eligible | −0.032 (−0.061, −0.003) | .031 |
| Limited to Medicare beneficiaries who were not dually eligible | −0.022 (−0.049, 0.007) | .118 |
| (7) Same-day readmissions treated as a single hospitalization | −0.030 (−0.056, −0.004) | .024 |
| (8) All Medicare beneficiaries in the Bronx | −0.012 (−0.027, 0.004) | .133 |
Estimated financial savings
The median amount paid by Medicare for a hospitalization among all Bronx Medicare FFS beneficiaries during the study period was $10 800. The predicted mean 30-day readmission rate without event notifications, controlling for beneficiary characteristics and the year/quarter of admission, was 29.4% compared to 26.5% with active event notifications. The estimated costs savings from potentially avoided readmissions attributable to event notifications was $1.25 million among the study participants, or approximately $488 per hospitalized beneficiary.
DISCUSSION
Our results suggest that event notifications reduce the likelihood of readmission. This is an important finding in light of the current policy focus on readmissions and the large investments that have been made in health IT. Policy initiatives have placed significant pressure on hospitals to reduce readmissions.24 For example, Medicare’s Hospital Readmissions Reduction Program penalizes hospitals with excessive readmission rates for certain conditions.25 Additionally, hospital readmission rates are publicly reported26 and are used as performance measures for ACOs27 and Patient Centered Medical Homes.28 Our findings suggest that event notifications could be an effective tool for health care organizations to meet the goals of these programs.29 In a broader context, poor communication between hospitals and outpatient providers during transitions of care is often a substantial obstacle in preventing readmissions.30 Our results suggest that readmissions can be reduced through improved communication achieved by providers’ use of event notifications.3
Prior evidence suggesting that event notifications may help avoid readmissions has been primarily based on qualitative studies.2,7 This is the first quantitative evaluation to identify an association between event notifications and reduced readmissions. An earlier study of e-mail messages sent within 24 hours of an emergency department visit to outpatient physicians found no effect on subsequent utilization.11 Although the study was based on a randomized controlled trial, it focused on a more general sample of adult patients, unlike our sample of Medicare FFS beneficiaries at high risk of readmission. Additionally, the study focused on emergency department visits instead of hospitalizations as the trigger for notifications, and the intervention centered on e-mail sent specifically to physicians rather than a notification delivered to an organization. A more recent randomized controlled trial of hospitalized older adults did not find a statistically significant decline in the risk of readmission associated with the use of a discharge notification system.10 However, the trial was conducted in a single multispecialty group practice, whereas our study included an ACO, ambulatory care practices, home health agencies, and integrated service delivery organizations.
Figure 1.
30-day readmission rates (with 95% confidence intervals) among Medicare fee-for-service (FFS) beneficiaries in the Bronx, New York, stratified by index admissions where event notification services were and were not active.
Note: Event notification services started in 2011.
Our results add to the growing evidence base indicating that HIE may improve the quality and efficiency of care. For example, prior studies have suggested that alerting outpatient providers about pending laboratory results improved follow-up care after hospital discharge,31 and alerts to attending physicians about soon-to-be-discharged patients at risk for thromboembolism increased the use of preventative measures.32
Although event notification systems show promise, they have limitations. Organizations receiving alerts do not always have the staff, procedures, and other resources to act on them.4,6,7,10,33 Providers also vary in the way that they respond4,7,34 and do not always follow up on hospitalization alerts.11,35 Event notifications may be most effective if incorporated into a suite of preventive measures addressing readmissions.36
Importantly, our estimates of savings associated with reductions in readmissions were substantially larger than the cost of installing an event notification system in an outpatient practice.37 However, under fee-for-service payment models, there are not strong incentives for providers to adopt this technology, and the desire for health care organizations to improve quality may not be sufficient to achieve widespread adoption. Newer payment and delivery models such ACOs may help stimulate adoption through incentives to improve quality and reduce costs. Given the resources and organizational commitment necessary to effectively use hospitalization alerts, adoption may be slow until these models become more prevalent or other incentives are created by policymakers.
The reduction in readmissions and associated cost savings seen in our results are noteworthy for policymakers. Importantly, event notifications were associated with lower readmission rates in a population characterized by low socioeconomic status, high morbidity, and high health care utilization. The Bronx ranks last among counties in New York State on a variety of health outcomes and factors contributing to poor health,15 and has among the highest readmission rates in the nation.16 Moreover, our study participants who enrolled in event notifications were older and more medically complex than other Medicare beneficiaries, and were also more likely to be racial and ethnic minorities than other beneficiaries in the Bronx. Event notifications may be a useful tool to improve population health given their success in reducing readmissions among our study participants.
Health IT has been promoted as a means to reduce health care expenditures but, to date, there has been limited evidence of its ability to do so.38–40 This has led to questions as to whether public investments made in health IT, such as those made through the Meaningful Use incentive programs, have been worth the cost.41 In this study, positive effects associated with an HIE intervention came > 5 years after the collaborating partners formed. Not only is it possible that other HIE interventions have not been given sufficient time for growth and development, but shifts in federal policies affecting health IT over the past decade may have hampered HIE efforts.42 The future of innovative HIE applications may again be in jeopardy as the country is poised to change health IT policy yet again.43 In this respect, the country has failed to adequately support HIE. The fact that the Bronx is seeing benefits may be due, in part, to the fact that New York State has made relatively large and sustained investments in this technology.
Limitations
Our study has several limitations to consider. Most importantly, unobserved health care delivery interventions that were undertaken concurrently may have influenced our results. Although we conducted several secondary analyses to account for other potential mechanisms to increase primary care providers’ awareness of hospital admissions and discharges of their patients, this may not have adequately controlled for all of them. While our regression models did account for differences between index hospitals that were independent of time, we were not able to control for potential differences between primary care providers. Providers who adopted event notification systems may have been different than nonadopters. Additionally, the results may not be widely generalizable to other health care organizations. Other HIE organizations offer event notifications,3 but the formatting of information and the technology used may be different. Our findings also may not be generalizable to the broader Medicare population. In the absence of unique identifiers for beneficiaries, we were not able to reliably link some claims to data from the Bronx RHIO, and our sample was limited to beneficiaries who had consented to be included in the RHIO. Lastly, the Bronx is a densely populated county with a disproportionate share of low-income residents and racial and ethnic minorities. Health care providers and Medicare beneficiaries in the county likely differ from those in many other parts of the country.
CONCLUSION
Event notifications were associated with lower readmission rates among Medicare FFS beneficiaries in the Bronx, New York. Our study suggests that event notifications may be an effective approach to improve the quality and efficiency of health care among high-risk populations.
Supplementary Material
ACKNOWLEDGMENTS
This project was made possible with the assistance of the New York eHealth Collaborative, the Bronx Regional Health Information Organization, and programming support from Phyllis Johnson, MBA, of Weill Cornell Medical College. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the US Department of Health and Human Services or any of its agencies. This project was approved by the Weill Cornell Institutional Review Board.
FUNDING
This project was made possible with funding from the New York State Department of Health.
COMPETING INTERESTS
Dr Unruh reports personal fees from naviHealth. No other authors report potential conflicts of interest.
CONTRIBUTORS
MAU designed the work, acquired data, and interpreted results. HYJ designed the work and interpreted results. RK interpreted results. JRV designed the work, analyzed data, acquired data, and interpreted results. All authors contributed to the drafting and revising of the work. All authors had final approval of the published version and agree to be accountable for the work.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
REFERENCES
- 1. Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–41. [DOI] [PubMed] [Google Scholar]
- 2. Vest JR, Ancker JS. Health information exchange in the wild: the association between organizational capability and perceived utility of clinical event notifications in ambulatory and community care. J Am Med Inform Assoc. Published online first: 23 April 2016, doi:10.1093/jamia/ocw040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Office of the National Coordinator for Health Information Technology. Improving Hospital Transitions and Care Coordination Using Automated Admission, Discharge and Transfer Alerts: a Learning Guide. Washington D.C. 2013. [Google Scholar]
- 4. Trudnak T, Mansour M, Mandel K, et al. A case study of pediatric asthma alerts from the Beacon Community Program in Cincinnati: technology is just the first step. EGEMS. 2014;2:1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moore T, Shapiro JS, Doles L, et al. Event detection: a clinical notification service on a health information exchange platform. AMIA Annu Symp Proc. 2012;2012:635–42. [PMC free article] [PubMed] [Google Scholar]
- 6. Gutteridge DL, Genes N, Hwang U, et al. Enhancing a geriatric emergency department care coordination intervention using automated health information exchange-based clinical event notifications. EGEMS. 2014;2:1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Altman R, Shapiro JS, Moore T, et al. Notifications of hospital events to outpatient clinicians using health information exchange: a post-implementation survey. Inform Prim Care. 2012;20:249–55. [DOI] [PubMed] [Google Scholar]
- 8. Afilalo M, Lang E, Léger R, et al. Impact of a standardized communication system on continuity of care between family physicians and the emergency department. CJEM. 2007;9:79–86. [DOI] [PubMed] [Google Scholar]
- 9. Magnus M, Herwehe J, Gruber D, et al. Improved HIV-related outcomes associated with implementation of a novel public health information exchange. Int J Med Inform. 2012;81:e30–8. [DOI] [PubMed] [Google Scholar]
- 10. Gurwitz JH, Field TS, Ogarek J, et al. An electronic health record-based intervention to increase follow-up office visits and decrease rehospitalization in older adults. J Am Geriatr Soc 2014;62:865–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lang E, Afilalo M, Vandal AC, et al. Impact of an electronic link between the emergency department and family physicians: a randomized controlled trial. CMAJ. 2006;174:313–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jencks SF, Williams M V, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009; 360:1418–28. [DOI] [PubMed] [Google Scholar]
- 13. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–22. [DOI] [PubMed] [Google Scholar]
- 14. Centers for Medicare and Medicaid Services. Hospital Compare. 2015. https://www.medicare.gov/hospitalcompare/readmission-reduction-program.html. Accessed December 31, 2015. [Google Scholar]
- 15. Institute University of Wisconsin Population Health. County Health Rankings & Roadmaps. 2015. http://www.countyhealthrankings.org/. Accessed January 1, 2015. [Google Scholar]
- 16. Goodman DC, Fisher ES, Chang C-H. After Hospitalization: A Dartmouth Atlas Report on Post-Acute Care for Medicare Beneficiaries. The Dartmouth Institute for Health Policy & Clinical Practice; Lebanon, NH: 2011. [PubMed] [Google Scholar]
- 17. Unruh MA, Trivedi AN, Grabowski DC, et al. Does reducing length of stay increase rehospitalization of Medicare fee-for-service beneficiaries discharged to skilled nursing facilities?. J Am Geriatr Soc. 2013;61:1443–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 19. Frisse ME, Holmes RL. Estimated financial savings associated with health information exchange and ambulatory care referral. J Biomed Inform. 2007;40:S27–32. [DOI] [PubMed] [Google Scholar]
- 20. Grabowski DC. Medicare and Medicaid: conflicting incentives for long-term care. Milbank. Q 2007;85:579–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Unruh MA, Grabowski DC, Trivedi AN, et al. Medicaid bed-hold policies and hospitalization of long-stay nursing home residents. Health Serv Res 2013;48:1617–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jung H-Y, Trivedi AN, Grabowski DC, et al. Integrated Medicare and Medicaid managed care and rehospitalization of dual eligibles. Am J Manag Care. 2015;21:711–7. [PMC free article] [PubMed] [Google Scholar]
- 23. Herwehe J, Wilbright W, Abrams A, et al. Implementation of an innovative, integrated electronic medical record (EMR) and public health information exchange for HIV/AIDS. J Am Med Inf Assoc. 2012;19:448–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Agency for Healthcare Research & Quality. National Strategy for Quality Improvement in Health Care. Agency-Specific Quality Strategic Plan Table Work Qual. 2015. http://www.ahrq.gov/workingforquality/nqs/nqsplans3.htm. Accessed January 1, 2015. [Google Scholar]
- 25. Centers for Medicare & Medicaid Services. Readmissions Reduction Program. 2015. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed November 20, 2015. [Google Scholar]
- 26. Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305:504–5. [DOI] [PubMed] [Google Scholar]
- 27. Centers for Medicare and Medicaid Services. Shared Savings Program. Quality Measures and Performance Standards. 2015. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Quality_Measures_Standards.html. Accessed January 1, 2015. [Google Scholar]
- 28. Rosenthal MB, Abrams MK, Bitton A, et al. Recommended core measures for evaluating the patient-centered medical home: cost, utilization, and clinical quality. The Commonwealth Fund. 2012;1–12. [Google Scholar]
- 29. Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–8. [DOI] [PubMed] [Google Scholar]
- 30. Burke RE, Guo R, Prochazka AV, et al. Identifying keys to success in reducing readmissions using the ideal transitions in care framework. BMC Health Serv Res. 2014;14:423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. El-Kareh R, Roy C, Williams DH, et al. Impact of automated alerts on follow-up of post-discharge microbiology results: a cluster randomized controlled trial. J Gen Intern Med. 2012;27:1243–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Piazza G, Anderson FA, Ortel TL, et al. Randomized trial of physician alerts for thromboprophylaxis after discharge. Am J Med. 2013;126: 435–42. [DOI] [PubMed] [Google Scholar]
- 33. Moran WP, Davis KS, Moran TJ, et al. Where are my patients? It is time to automate notification of hospital use to primary care practices. South Med J. 2012;105:18–23. [DOI] [PubMed] [Google Scholar]
- 34. Anand V, Sheley ME, Xu S, et al. Real time alert system: a disease management system leveraging health information exchange. Online J Public Health Inform. 2012;4:ojphi.v4i3.4303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Field T, Fouayzi H, Gagne S, et al. PS2‐6: Who opens alerts to physicians? (and who doesn’t?). Clin Med Res. 2013;11:151. [Google Scholar]
- 36. Bradley EH, Curry L, Horwitz LI, et al. Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes. 2013;6:444–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Field TS, Garber L, Gagne SJ, et al. Technological resources and personnel costs required to implement an automated alert system for ambulatory physicians when patients are discharged from hospitals to home. Inf Prim Care. 2012;20:87–93. [DOI] [PubMed] [Google Scholar]
- 38. Agha L. The effects of health information technology on the costs and quality of medical care. J Health Econ. 2014;34:19–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Borzekowski R. Measuring the cost impact of hospital information systems: 1987–1994. J Health Econ. 2009;28:938–49. [DOI] [PubMed] [Google Scholar]
- 40. Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–52. [DOI] [PubMed] [Google Scholar]
- 41. Mennemeyer ST, Menachemi N, Rahurkar S, et al. Impact of the HITECH act on physicians’ adoption of electronic health records. J Am Med Inform Assoc. Published Online First: July 30, 2015, doi:10.1093/jamia/ocv103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lenert L, Sundwall D, Lenert ME. Shifts in the architecture of the Nationwide Health Information Network. J Am Med Informatics Assoc 2012;19: 498–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. AMA Wire. CMS Chief Vows to Replace Meaningful Use with Better Policy. 2016. http://www.ama-assn.org/ama/ama-wire/post/cms-chief-vows-replace-meaningful-use-better-policy. Accessed February 19, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.