Abstract
Background and significance. It is increasingly recognized that some patients self-manage in the context of social networks rather than alone. Consumer health information technology (IT) designed to support socially embedded self-management must be responsive to patients’ everyday communication practices. There is an opportunity to improve consumer health IT design by explicating how patients currently leverage social media to support health information communication.
Objective. The objective of this study was to determine types of health information communication patterns that typify Facebook users with chronic health conditions to guide consumer health IT design.
Materials and methods. Seven hundred participants with type 2 diabetes were recruited through a commercial survey access panel. Cluster analysis was used to identify distinct approaches to health information communication both on and off Facebook. Analysis of variance (ANOVA) methods were used to identify demographic and behavioral differences among profiles. Secondary analysis of qualitative interviews (n = 25) and analysis of open-ended survey questions were conducted to understand participant rationales for each profile.
Results. Our analysis yielded 7 distinct health information communication profiles. Five of 7 profiles had consistent patterns both on and off Facebook, while the remaining 2 demonstrated distinct practices, with no health information communication on Facebook but some off Facebook. One profile was distinct from all others in both health information communication practices and demographic composition. Rationales for following specific health information communication practices were categorized under 6 themes: altruism, instrumental support, social support, privacy and stigma, convenience, and Facebook knowledge.
Conclusion. Facebook has been widely adopted for health information communication; This study demonstrates that Facebook has been widely adopted for health information communication. It also shows that the ways in which patients communicate health information on and off Facebook are diverse.
BACKGROUND AND SIGNIFICANCE
Patient-centeredness and patient and family engagement have been recognized by multiple organizations, including the Institute of Medicine, Centers for Medicare and Medicaid Services, and National eHealth Collaborative, as key to improving health care.1,2 Patients’ capacity to engage in their care is shaped by multiple factors, including knowledge, skills, and confidence (ie, activation) and external contexts (ie, physical, social, organizational).3,4 Engaged patients are more likely to seek preventive and routine chronic care, follow through on healthy behaviors, adhere to treatment, and avoid health-damaging behaviors.5 Preliminary studies also suggest that they incur lower health care costs.6 For many, however, engagement is not an individual process, but a collective one that draws upon the instrumental and emotional support of a social network.7–11 This support may take the form of a primary informal caregiver or care partner7 or an extended social network, including multiple family members, friends, community members, and others with similar conditions.
Consumer health information technology (IT), electronic technology used by laypeople to support health and health care management,12–14 has been developed to support the roles of 2 types of social networks. The first type, the personal social network, consists of people with whom an individual has an affect-based relationship or interacts in everyday life. The personal social network may include family members, friends, colleagues, neighbors, and acquaintances, among others.7–9,15–17 Although some of these social network members may serve as primary informal caregivers or care partners, providing emotional and instrumental (eg, transportation, treatment management, and household management) support for health and health care management,8,9,16 others may be less intensely or less regularly involved. Epic’s MyChart, Microsoft’s HealthVault, and CaringBridge are among the few commercially available consumer health IT solutions designed to support the roles of these social network members by enabling communication of health information. Each, however, is limited in terms of how, what, and to whom health information may be communicated.9,18 Better facilitation of communication between patients and their personal social networks requires consumer health IT that integrates existing functionality and better responds to users’ needs and preferences, including those related to privacy, initiation of support requests, mode of communication, and scope of sharing.7–9,15–17,19
The second type of social network engaged in health and health care management consists of individuals who share a common diagnosis, the shared-condition social network. Although this may include those in an individual’s personal social network,9 it may also include others with whom an individual has no other connection. This network can also provide emotional support in addition to serving as a resource for information about alternative means of managing a given condition.10,11 Numerous consumer health IT solutions have been developed to support communication of health information with this type of social network.20,21 These include health communities on multifunction sites such as WebMD22 and Yahoo,23 as well as sites that serve as dedicated health communities such as PatientsLikeMe24 and QuitNet.25 Previous studies have shown that participation in an online health community provides direct benefits in the form of information utility and social support.10,21 Despite the plethora of solutions and demonstration of value, opportunities exist to better support communication with a shared-condition social networks by embedding quality assessments of shared information,22 enhancing the ability for collective sensemaking,26 and translating group experiences into personalized information.27
Broadening and improving consumer health IT requires understanding the needs and preferences of target users,28–30 in part by understanding existing practices.4 A foundational step, therefore, is to draw design insight from how patients not only use available consumer health IT to support health information communication with their social networks, but also how they use general communication technologies for this purpose. Previous studies have documented that patients use a wide range of general communication mechanisms for health information communication, including in-person, phone, e-mail, and social networking sites (SNSs).18,19,31–37 However, these general communication mechanisms are not uniformly used19,37; instead, different patients adopt them to different degrees and perceive unequal costs and benefits associated with them.18,19 This lack of uniformity suggests that patients have a range of motivations for health information communication, each of which is best suited to a certain type of mechanism.
SNSs, in particular, can be differentiated from other general communication mechanisms. In contrast with other mechanisms, SNSs enable unique forms of informational and emotional presentation38–41 and provide chronic illness patients with an immense network of social support, the size and diversity of which far exceed those of other communication settings.42 Similarly, SNSs provide patients with a relatively less personal outlet for emotional expression, resulting in a higher likelihood of sharing socially undesirable information, such as sensitive aspects of illness management.42 Moreover, individuals are less likely to be inhibited by the desire for direct reciprocation for the information they share.43 Thus, an opportunity exists to improve the design of consumer health IT by explicating the ways in which patients leverage social network sites and other communication mechanisms for health information communication.
Although previous studies have defined specific design directions to improve consumer health IT supporting health information communication with social networks, these studies have either drawn on relatively small samples8–10,15–17,19 or focused on analyzing text generated within online health communities.6,44 Moreover, each of these studies predominantly focused on only 1 of the 2 types of social networks (personal or shared-condition) and on either SNS or non-SNS–based health information communication. An opportunity exists to augment our understanding of how to support patients in communicating health information with their social network members by drawing on a large sample survey and simultaneously focusing on personal and shared-condition social networks and SNS and non-SNS–based communication.
This study focuses on Facebook as an example of an SNS platform used for health information communication with social networks. Facebook remains the most visited social networking site in the United States, claiming 72% of online adults as users.45 Its range of communication mechanisms support communication with personal social networks (eg, timeline postings, private messages) and shared-condition social networks (eg, groups).46 In the context of health and health care management, patients engage with Facebook social networks to obtain relevant health information36,47–50 and social support.36,47,49,50 Previous studies have presented evidence suggesting that the vast majority of patients prefer to use Facebook to communicate with shared-condition social networks through moderated groups48,49,51 rather than with their personal social networks.32,48 Patients who use Facebook for health and health care management receive multiple benefits, including increased emotional support, self-esteem, accountability, self-efficacy, and motivation.32,47,49–51
OBJECTIVE
The objective of this exploratory study is to determine types of health information communication patterns (profiles) that typify Facebook users with chronic health conditions, based on data from a detailed sample survey. A further objective is to assess demographic differences among profiles and participant rationales for adhering to a specific profile. The profiles were developed in the context of approaches to communicating health information on and off Facebook through pathways including in person and by telephone, email, text, or videoconference. By developing a small number of distinct but typical profiles, we seek to provide insight into the diversity of patient approaches to health information communication with social networks that must be supported through consumer health IT.
MATERIALS AND METHODS
Study overview
The larger mixed-methods study from which this analysis draws consisted of qualitative interviews and a large sample survey. Individuals who participated in the qualitative interviews were ineligible for the survey. Twenty-five participants were interviewed in depth about their approaches to health information communication on and off Facebook. The qualitative analysis results were used to develop a survey instrument, which was piloted prior to deployment. Seven hundred participants were surveyed online using the final survey instrument. The findings presented here primarily focus on data obtained from the survey; a secondary analysis of the qualitative interviews is also presented to provide further insight into the quantitative results.
Setting
Survey data were collected online through Qualtrics52 from a nationwide sample of adult Facebook users with type 2 diabetes.
Sample
This study focused on individuals with type 2 diabetes. This chronic condition was selected because it may be considered prototypical in that it is growing in prevalence, requires ongoing interaction with health care providers, and involves significant self-management.53,54 Moreover, it disproportionately affects racial and ethnic minorities,53,54 enabling the study of demographically diverse individuals’ health information communication practices. Participants were recruited through a commercial survey access panel provided by Survey Sampling International. Purposive sampling was used to oversample racial and ethnic minorities. Eligible individuals were over 18 years of age, had been diagnosed with type 2 diabetes, were Facebook users, and resided in or were citizens of the United States. The final sample was broadly representative of the population of Facebook users with type 2 diabetes, as illustrated in the Supplementary Appendix (Table A). Our purposive sampling of racial and ethnic minorities yielded a sample that was 21.3% African American, 21.3% Hispanic, and 12.3% Asian.
We received a total of 814 cases from Survey Sampling International, of which 700 were eligible. To eliminate respondents who sped through the survey, broke off partway through the survey, or skipped entire sections of the survey, we removed cases in which respondents failed to answer at least 1 question in each of the 8 survey sections. This eliminated 50 cases, resulting in a total of 650 cases available for analysis.
Data collection
The survey instrument contained questions focusing on: (1) eligibility criteria, (2) general Facebook use, (3) health information communication on Facebook, (4) health information communication off Facebook, (5) privacy, and (6) demographics. Questions relevant to the analysis presented here can be found at the end of the Supplementary Appendix.
Data analysis
Development of global measures
We began by exploring ways to segment the sample using factor and cluster analyses applied to the dimensions of who is in the network, what communication mechanisms are used, and what information is communicated. These analyses were also used to segment the sample based on how, what, and with whom health information was communicated both on and off Facebook. Although responses varied across these variables, no clear segments emerged. As an alternative, we created global measures (described below), which yielded meaningful and distinct clusters.
A global measure was created for each of 3 general behaviors: Facebook use, health information communication on Facebook, and health information communication off Facebook. The global Facebook usage measure was created by summing the z-scores of 3 variables: frequency of Facebook use, a count variable of different types of people in the participant’s Facebook network, and a summation variable of the frequency of use of different features to communicate on Facebook. The global measure of health information communication behavior on Facebook was created by summing the z-scores of 3 composite variables: a count variable of the different types of people with whom the participant communicates health information on Facebook, a summation variable of the frequency with which different features are used to communicate health information on Facebook, and a summation variable of the frequency of different types of health information the participant communicates on Facebook. Finally, the global measure of health information communication behavior off Facebook was created by summing the z-scores of 3 composite variables: a count variable of the different types of people in the participant’s Facebook network with whom he or she communicates health information off Facebook, a summation variable of the frequency of different types of health information the participant communicates off Facebook with people in the Facebook network, and a summation variable of the frequency with which different off-Facebook mechanisms are used to communicate health information with people in the Facebook network.
Development of health information communication profiles
After filtering out approximately 200 participants who never communicated health information on Facebook, k-means cluster analysis55 was used to analyze the intersection of the global measures of Facebook use and health information communication on Facebook. In the emergent clusters, participants were distinguished by level of health information communication, high or some, and level of Facebook use, high or low. The cut-point differentiating high and low Facebook use among participants who communicated health information was then applied to the participants who never communicated health information on Facebook, thus bringing back those 200 participants into the subsequent analysis. A variable was created to capture the resulting groupings. A similar process was used to analyze the intersection of Facebook use with health information communication off Facebook. A bivariate cross-tabulation was used to examine the extent of overlap and pattern between the resulting 2 cluster solutions. Final health information communication profiles were created based on the pattern of the most populated cells within the cross-tabulation.
We assessed the goodness of fit of the 7 profiles by conducting a discriminant function analysis using 5 variables to predict cluster membership: the global measure of Facebook usage, the global measure of health communication on Facebook, the global measure of off-Facebook health communication, a flag for those who never post health information on Facebook, and a flag for those who never share health information off Facebook. These variables correctly classified 87% of the cases.
Composition and comparison of profiles
To compare profiles across general Facebook use behaviors, health status, and demographic variables, one-way ANOVA with post hoc pairwise comparisons were run, using Tukey’s HSD method to test for significant differences between profiles at an alpha level of 0.05. To include nominal dependent variables in this analysis, dummy variables were created and used in place of the categorical variables in the pairwise comparisons.
To further distinguish profiles in terms of their health information communication practices, one-way ANOVA with Tukey’s HSD post hoc analysis was run to compare profiles across what, how, and to whom health information is communicated on and off Facebook. Significance level was set at an alpha of 0.05.
Secondary analysis of interview data and analysis of open-ended survey data
A secondary analysis of interview data was conducted to gain insight into participant rationales for following each approach to health information communication (ie, profile). Interviews were obtained through phone and Skype conversations with Facebook users who were over the age of 18 years, had a diagnosis of type 2 diabetes, and lived in or were citizens of the United States. Recruitment methods have been previously described56 and involved using maximum variance sampling based on a preinterview survey of individuals recruited through Facebook, consisting of 23 questions regarding Facebook use and demographic characteristics. Interview sampling based on survey responses enabled us to recruit individuals with diverse behaviors and demographic characteristics. This preinterview survey was distinct from the main survey, which consisted of 75–80 questions (depending on skip logic and survey version). Some questions included multiple sub-items, presented in grid format. The main survey was created based upon the responses we received during the interviews and a round of pilot testing.
Interview participants were predominantly female (56%) and between the ages of 30 and 64 (84%), and had received education at the level of an associate’s degree or higher (68%). Over one-third identified as a racial or ethnic minority. The secondary analysis included 2 researchers independently categorizing the interview participants into health information communication profiles and collaboratively identifying rationales related to each profile. Preinterview survey responses were used to determine general Facebook use and health information communication practices on Facebook for all interview participants. When interview responses indicated behaviors (ie, general Facebook use and health information communication practices on Facebook) inconsistent with those reported in the preinterview survey, we used the behavior reported in the interview. For example, if a participant indicated that he or she had never communicated health information on Facebook on the preinterview survey but discussed some health information communication practices on Facebook during the interview, we coded the participant as engaging in some health information communication on Facebook. Because we did not ask about off-Facebook health information communication in the preinterview survey, interview transcripts were used to determine health information communication practices off Facebook. Transcripts were then reviewed to select illustrative examples of rationales relevant to each profile.
To further understand the rationales for following specific health information communication approaches, we similarly analyzed participant responses to 2 open-ended questions in the main survey: “It seems that you do not communicate any health information through Facebook. What are your main reasons for that?” and “It seems that you do not communicate any health information off Facebook. What are your main reasons for that?” These survey questions were only presented to individuals who did not communicate any health information on or off Facebook, respectively. This analysis enabled us to gain further insight into the rationales of individuals in profiles that had limited health information communication on and off Facebook.
RESULTS
Sample description
A final sample of 650 Internet survey participants remained after applying data integrity measures. The sample was approximately one-third male and two-thirds female. The median age of participants was 54 years. Most had some college education, with approximately half having completed a 4-year college degree or above. Over one-half were racial or ethnic minorities. All 4 US regions were represented, with the greatest number of participants living in the South. Detailed demographics are represented in Table 1. We also assessed sample representativeness of the estimated population of patients with type 2 diabetes on Facebook, as illustrated in Table A of the Supplementary Appendix. The sample was representative across age, race/ethnicity, and geographic region. It was overrepresentative of women and people with higher levels of education.
Table 1.
Participant demographic characteristics
| Demographic characteristic | n (%) |
|---|---|
| Gender | |
| Male | 246 (37.8) |
| Female | 404 (62.2) |
| Age | |
| 20–44 | 213 (32.8) |
| 45–64 | 286 (44.0) |
| 65+ | 140 (21.5) |
| Education | |
| Less than high school diploma | 9 (1.4) |
| High school graduate or GED | 102 (15.8) |
| Some college but no degree | 138 (21.3) |
| 2-year college degree/AA/AS | 92 (14.2) |
| 4-year college degree/BS/BA | 169 (26.1) |
| Some graduate work | 33 (5.1) |
| Master’s degree | 71 (11.0) |
| Professional degree | 18 (2.8) |
| Doctoral degree | 15 (2.3) |
| Race | |
| White | 391 (61.8) |
| Black/African American | 135 (21.3) |
| Asian | 78 (12.3) |
| American Indian/Alaska Native | 7 (1.1) |
| Native Hawaiian or Other Pacific Islander | 0 (0.0) |
| Two or more races | 22 (3.5) |
| Ethnicity | |
| Hispanic/Latino | 137 (21.3) |
| Non-Hispanic/Latino | 508 (78.7) |
| Region | |
| Northeast | 136 (21.1) |
| Midwest | 83 (12.9) |
| South | 277 (43.0) |
| West | 148 (23.0) |
Profile types
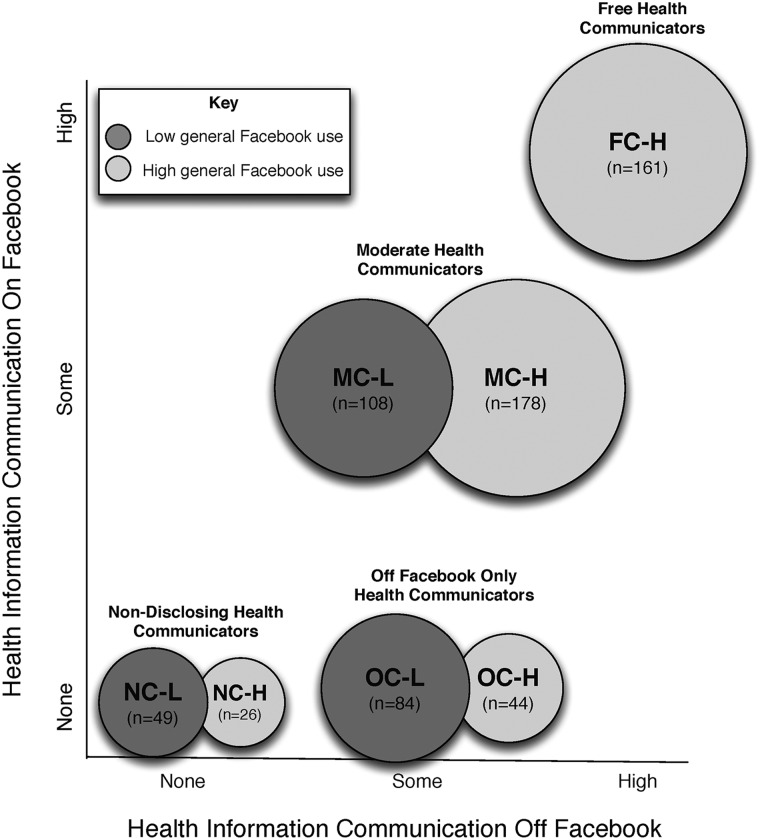
Our analysis yielded 7 distinct health information communication profiles differentiated by degree of general Facebook use, degree of health information communication on Facebook, and degree of health information communication off Facebook. Five of the profiles represented participants with consistent communication patterns both on and off Facebook. In other words, these participants either have high health information communication on and off Facebook (free health communicators, FCs), some health information communication on and off Facebook (moderate health communicators, MCs), or no health information communication on or off Facebook (nondisclosing health communicators, NCs). In the remaining 2 profiles, participants demonstrated distinct communication practices on and off Facebook, with no communication on Facebook but some off Facebook (off Facebook–only health communicators, OCs). Participants also differed in terms of degree of general Facebook use, indicated by H or L (high or low) following the approach to health information communication. In other words, moderate health communicators who had a high level of general Facebook use are indicated by the abbreviation MC-H. A visual schematic representation of these profiles and participant distributions across profiles can be found in Figure 1.
Figure 1.
Seven health information communication profiles.
Profile composition
Key differences among profiles across Facebook use behaviors, health status, and demographics can be found in Table 2. A superscript indicates a significant difference (P < .05) between 2 profiles. A superscript is provided next to the significantly higher value, with the profile number inside the superscript holding the significantly lower value. Table B in the Supplementary Appendix compares profiles across all variables.
Table 2.
Comparison of profiles across general Facebook use, health status, and demographics
| Characteristics | FC-H (1) |
MC-H (2) |
MC-L (3) |
OC-H (4) |
OC-L (5) |
NC-H (6) |
NC-L (7) |
Total |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean/% | N | Mean/% | N | Mean/% | N | Mean/% | N | Mean/% | N | Mean/% | N | Mean/% | N | Mean/% | N | |
| Number of Facebook accounts | 1.36(2) (3) (4) (5) (7) | 161 | 1.14 | 178 | 1.11 | 108 | 1.06 | 44 | 1.02 | 83 | 1.23 | 26 | 1.00 | 49 | 1.17 | 649 |
| Number of devices used to access FB | 2.77 (2) (3) (4) (5) (6) (7) | 161 | 2.16(3) (5) (7) | 178 | 1.53 | 108 | 2.09 (3) (5) | 44 | 1.36 | 84 | 1.69 | 26 | 1.57 | 49 | 2.03 | 650 |
| Did change privacy settings | 60% (3) (5) (7) | 161 | 48%(3) (7) | 178 | 26% | 108 | 36% | 44 | 30% | 84 | 31% | 26 | 22% | 49 | 42% | 650 |
| Health | ||||||||||||||||
| General health | 3.62 (2) (3) (4) (5) (6) (7) | 161 | 2.79 | 178 | 2.67 | 108 | 3.02 | 44 | 2.72 | 83 | 2.73 | 26 | 3.06 | 49 | 3.00 | 649 |
| Years diagnosed with diabetes | 3.13 | 160 | 3.57 (1) | 176 | 3.85 (1) | 107 | 3.74 | 43 | 4.06 (1) | 82 | 3.46 | 26 | 4.08 (1) | 45 | 3.62 | 639 |
| Demographics | ||||||||||||||||
| Age | 40.97 | 158 | 50.52 (1) | 178 | 57.44 (1) (2) | 104 | 56.72 (1) | 44 | 62.01 (1) (2) | 81 | 54.84 (1) | 25 | 58.28 (1) (2) | 49 | 51.94 | 639 |
| People in household | 3.21(2) (3) (4) (5) (6) (7) | 157 | 2.68 (3) (5) | 169 | 2.28 | 106 | 2.15 | 44 | 2.10 | 82 | 2.07 | 26 | 2.29 | 48 | 2.58 | 632 |
| Household income | 3.26 (2) (3) (5) (6) (7) | 160 | 2.58 | 171 | 2.54 | 103 | 2.65 | 43 | 2.50 | 77 | 2.30 | 26 | 2.22 | 45 | 2.71 | 625 |
| Employed full time | 73% (2) (3) (4) (5) (6) (7) | 161 | 41% (3) (5) | 178 | 24% | 108 | 32% | 44 | 23% | 84 | 35% | 26 | 29% | 49 | 42% | 650 |
| Married | 74% (3) (5) | 161 | 59% | 178 | 49% | 108 | 68% | 44 | 48% | 84 | 54% | 26 | 51% | 49 | 59% | 650 |
| Hispanic/Latino | 37% (2) (3) (5) (7) | 161 | 18% | 178 | 15% | 108 | 23% | 44 | 13% | 84 | 19% | 26 | 10% | 49 | 21% | 650 |
| Black/African American | 27% | 161 | 21% | 178 | 23% | 108 | 7% | 44 | 23% | 84 | 19% | 26 | 33% (4) | 49 | 23% | 650 |
| Urban community | 50% (2) (3) (5) | 161 | 28% | 178 | 30% | 108 | 27% | 44 | 31% | 82 | 31% | 26 | 33% | 49 | 35% | 650 |
Facebook access
Although the majority of participants in each profile had only 1 Facebook account, each profile contained participants with multiple accounts. Pairwise comparisons showed that participants were significantly more likely to have multiple accounts in FC-H than in most other profiles. Across profiles, a greater percentage accessed Facebook using a desktop or laptop than a cellphone or tablet. There were no significant differences in percentage of participants in each profile using a desktop, while participants in FC-H were significantly more likely than the majority of other profiles to use a laptop. The percentage using a tablet or cellphone for access ranged from over 60% in FC-H to around 20% in NC-H, MC-L, OC-L, and NC-L.
Facebook privacy
Approximately one-third to one-half of participants across profiles did not change their Facebook privacy settings, with no significant differences among profiles. After accounting for those who did not know if they had changed their settings (n = 111), significant differences among profiles emerged for the percentage who had changed them. Participants in FC-H and MC-H were significantly more likely to have altered their settings than those in MC-L, OC-L, and NC-L. Of those who modified their settings, participants in MC-H, NC-H, OC-L, and NC-L made significantly more changes than those in FC-H. Participants in the former profiles made an average of 5.15 privacy changes compared to 4.40 changes in the latter. There were no significant differences among profiles in the number of reasons participants gave for their current settings or for the number of privacy measures they took apart from changing their settings.
Health status and insurance
Across all profiles, the weighted average of self-rated general health was 3.0 (good) on a 5-point scale. The average self-rated general health of participants in FC-H was significantly higher than in all other profiles. Participants in FC-H, on average, had been diagnosed with diabetes more recently than those in MC-H, MC-L, OC-L, and NC-L. Significant differences existed among profiles in the percentage receiving health coverage through employment, government marketplace, and Medicare. Participants in FC-H were significantly more likely to be covered through employment than those in MC-L and OC-L. Similarly, they were more likely to be covered through a government marketplace than those in OC-L. They were also significantly less likely to be covered through Medicare than participants in other profiles, except NC-H. No significant differences existed among profiles in terms of coverage through Medicaid, Tricare/Veterans Administration, or third-party entities not associated with a government marketplace. Moreover, there were no differences in the percentage of uninsured across profiles.
Demographics
There were no significant differences in gender among the 7 profiles. Participants in FC-H were significantly younger than participants in all other profiles. Participants in MC-H were also significantly younger than participants in MC-L, OC-L, and NC-L. There were no significant differences in education levels across profiles. Participants in FC-H were significantly more likely to be employed than those in all other profiles and least likely to be retired than those in all other profiles except NC-H. Participants in MC-H were significantly more likely to be employed and significantly less likely to be retired than those in MC-L and OC-L. With respect to race and ethnicity, participants in FC-H were significantly more likely to be Hispanic or Latino than those in MC-H, MC-L, OC-L, and NC-L, and participants in NC-L were significantly more likely to be black or African American than those in OC-H. The average self-rated political views were significantly different for participants in FC-H, indicating more liberal ideology than the average, and for participants in MC-L and NC-L, who had slightly more conservative ideology.
Participants in FC-H were more likely to be married than in MC-L and OC-L and less likely to be widowed than those in OC-L. Household size was significantly larger for participants in FC-H compared to all other profiles and for participants in MC-H compared to MC-L and OC-L. There were no significant differences in region of residence, with the exception of participants in MC-L, who were more likely to live in the West than participants in FC-H, MC-H, and OC-L. Regarding community types, those in FC-H were more likely to live in urban communities than those in MC-H, MC-L, and OC-L. Moreover, they were less likely to live in rural communities than those in MC-H and MC-L. Participants in FC-H had significantly higher household income than those in other profiles except OC-H. On average, they also had a significantly higher self-rated financial situation than all other profiles.
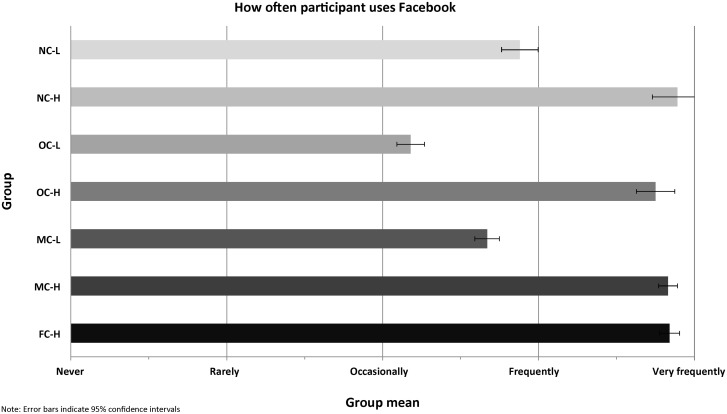
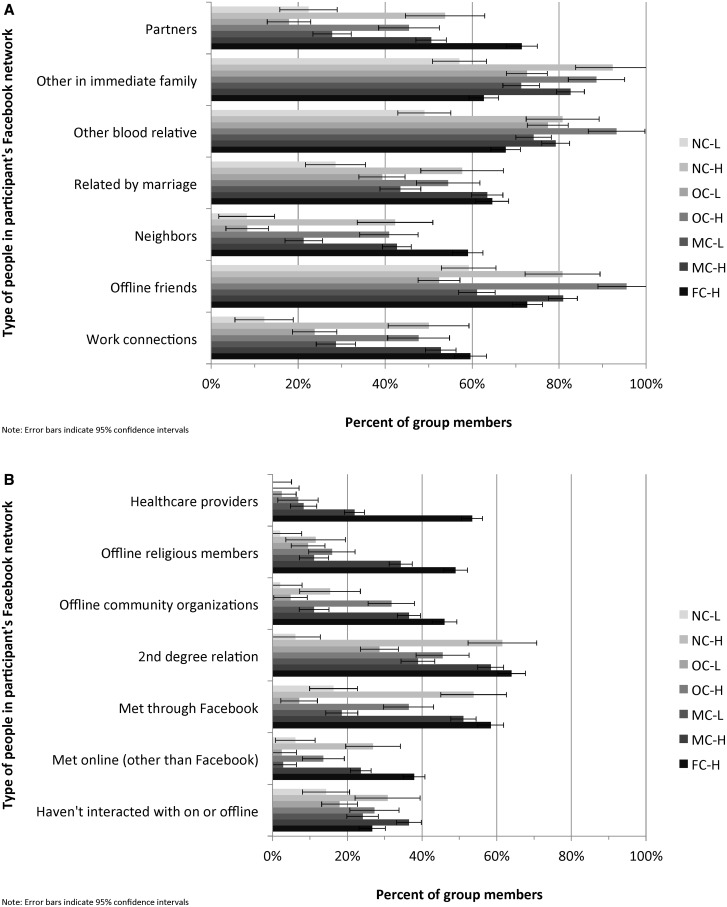
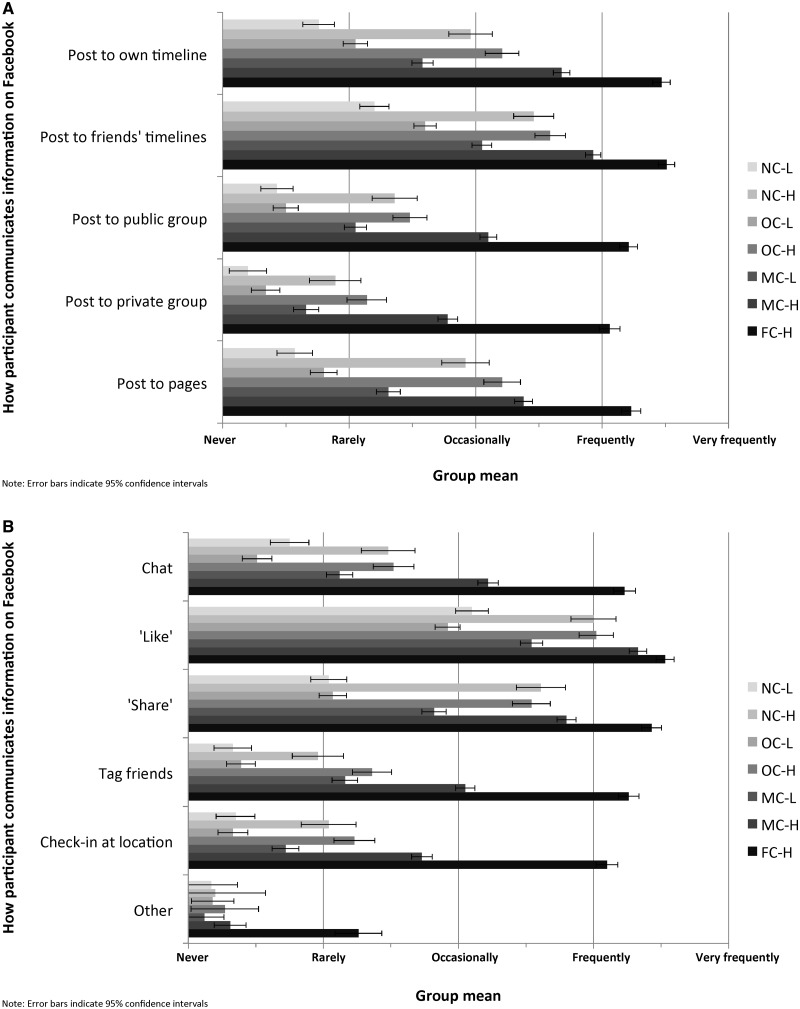
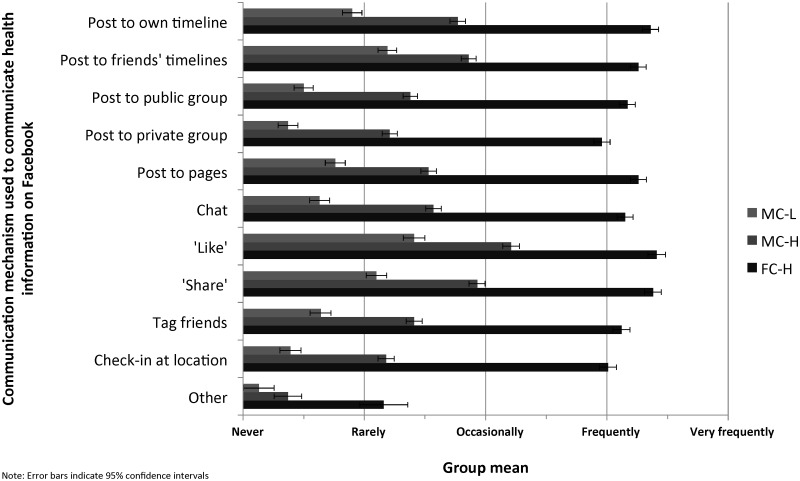
General Facebook use
The profiles differed significantly in terms of general use of Facebook. Participants in FC-H, MC-H, OC-H, and NC-H used Facebook more often than those in MC-L, OC-L, and NC-L (Figure 2). Furthermore, participants in FC-H were more likely than those in most of the other profiles to have partners, health care providers, offline religious community members, and individuals they met online but not through Facebook in their Facebook social network (Figure 3). Participants in FC-H and MC-H were also more likely to include a range of social network member types (eg, relatives by marriage, work connections, second-degree relationships) than participants in MC-L, OC-L, and NC-L. Participants in OC-H were most likely to have offline friends and those in NC-H were most likely to have individuals they met through Facebook in their Facebook social network. There was a fairly consistent pattern across profiles in terms of how participants communicated on Facebook (Figure 4). Participants in FC-H were most likely to use each communication mechanism, followed by those in MC-H and OC-H. Moreover, participants in MC-L and NC-H were more likely to use several communication mechanisms (eg, their own timeline, friends’ timelines, public groups, pages, share) than participants in OC-L and NC-L. All figures in this and the following section include 95% confidence intervals. The confidence interval minimum is cut off at zero when applicable. Table C in the Supplementary Appendix contains details about profiles differences in terms of general Facebook use.
Figure 2.
Frequency of participant Facebook use by profile.
Figure 3.
Types of people in participants' Facebook networks by profile.
Figure 4.
Participants’ use of Facebook communication mechanisms by profile.
Health information communication practices
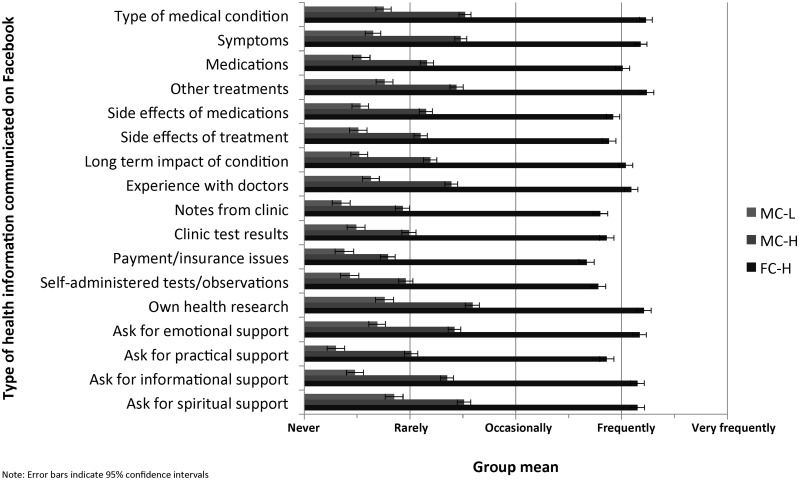
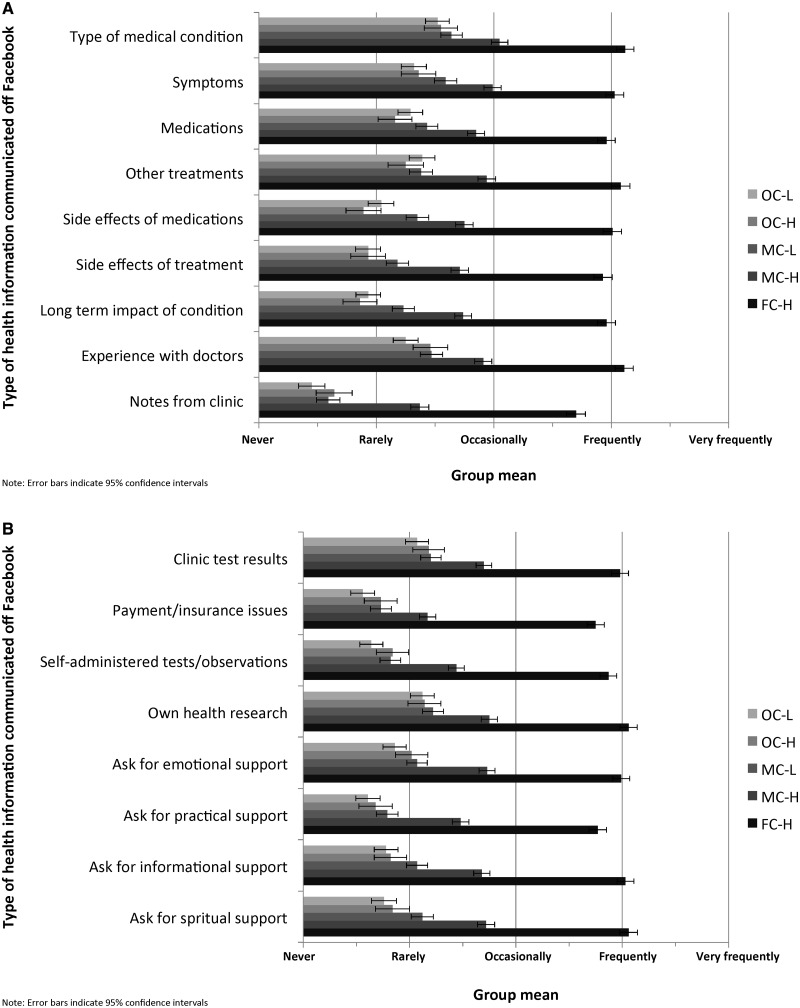
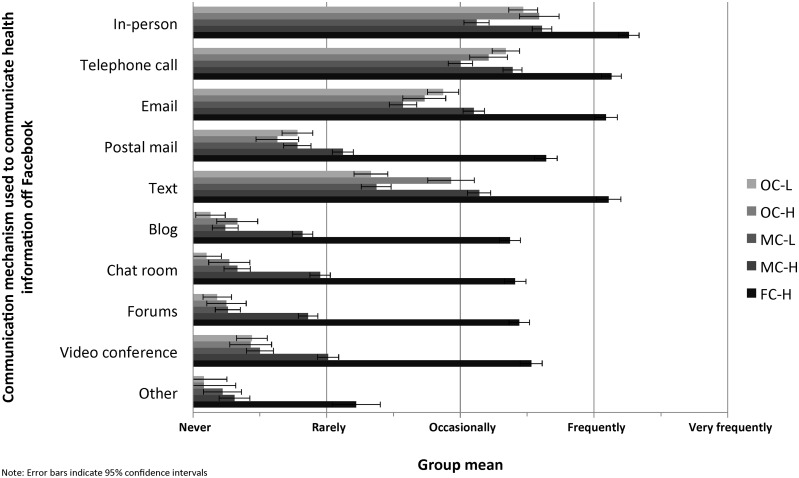
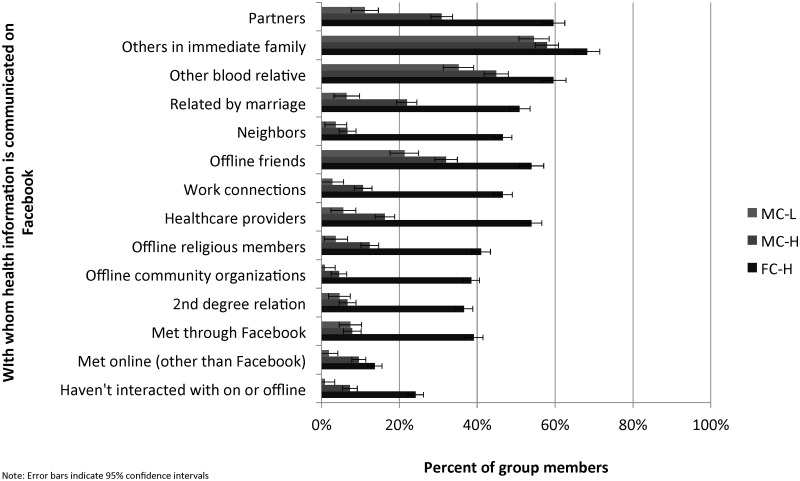
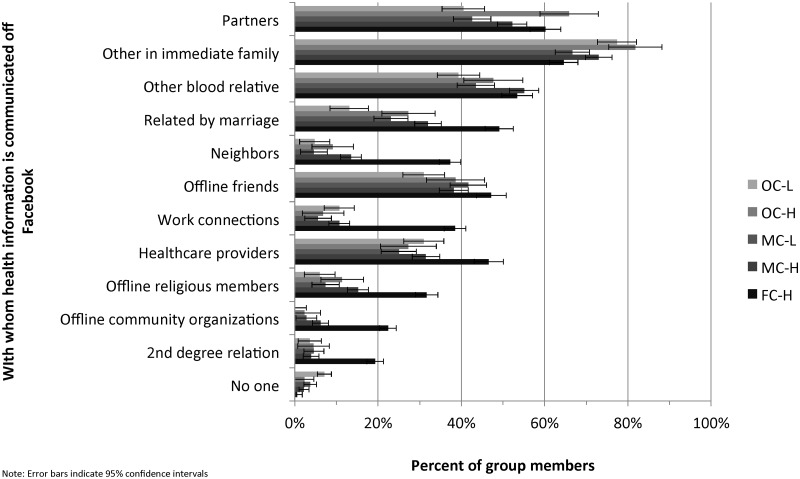
There were statistically significant differences among profiles in terms of what, how, and to whom health information was communicated on and off Facebook. For types of health information communicated on (Figure 5) and off (Figure 6) Facebook, there was a consistent pattern across variables. Participants in FC-H communicated each type of health information most frequently, followed by participants in MC-H. There were also consistent statistically significant differences between participants in MC-H vs MC-L (on Facebook) and vs MC-L, OC-H, and OC-L (off Facebook). A similar pattern was seen for the use of communication mechanisms on (Figure 7) and off (Figure 8) Facebook. However, there was greater variability both on (Figure 9) and off (Figure 10) Facebook in terms of with whom health information was communicated. Although participants in FC-H generally communicated more frequently to each type of social network member, statistically significant differences were not present for all types of social network members. Particularly, off Facebook there were no statistically significant differences in communication practices among participants in FC-H compared to those in MC-H, MC-L, OC-H, and OC-L with individuals who may be considered closer in terms of affect (eg, partners, immediate family members, offline friends). Tables D and E in the Supplementary Appendix contain details about health information communication practices on and off Facebook.
Figure 5.
Types of health information communicated on Facebook by profile.
Figure 6.
Types of health information communicated off Facebook by profile.
Figure 7.
Communication mechanisms used to communicate health information on Facebook.
Figure 8.
Communication mechanisms used to communicate health information off Facebook by profile.
Figure 9.
Whom health information is communicated with on Facebook by profile.
Figure 10.
Whom health information is communicated with off Facebook by profile.
Participant rationales for profiles
Secondary analysis of interview data yielded 4 participants categorized as FC-H, 12 as MC-H, 7 as MC-L, and 2 as OC-H. No interview participants were categorized as OC-L, NC-L, or NC-H. This may have been because our recruitment strategy56 did not adequately reach individuals who have limited health information communication on Facebook. However, 199 survey respondents provided rationales for why they do not communicate any health information on and/or off Facebook. Of these, 44 were classified as OC-H, 82 as OC-L, 26 as NC-H, and 47 as NC-L. Rationales focused on 6 themes: altruism, instrumental support, social support, privacy and stigma, convenience, and Facebook knowledge. Examples of direct quotes from participants can be found in Table 3. For simplicity, quotes are grouped by approach to health information communication and not divided by general Facebook use.
Table 3.
Participant rationales for health information communication approaches
| Health information communication approach | Verbatim quotes from interview participants |
|---|---|
| Free health communicators (FCs) | Altruism: It’s because I believe that we should be – we live in a world where we need to be purposeful and helpful, that I’m able to communicate. Facebook provides such a vast area of people who can benefit from it that I think it’s the perfect tool to use. |
| Instrumental support: Well, I want to keep everybody up-to-date on what’s going on with me, but then somebody else might have some idea or know another way to treat it, or know a good doctor. [I]t's good information for me. That way everybody's informed of it. | |
| Social support: Like with diabetes, it helps when you're trying to keep your blood sugar within check, it helps to have other people kind of rooting you on, giving you their experiences, telling you things that they've done to get their blood sugar down. Mainly, I guess, support. | |
| Privacy and stigma: Why I communicate health information? Believe it or not, I think it's easier sometimes to ask a whole group of people kind of anonymously on Facebook than it is to ask a doctor face-to-face.… I think, when you're on Facebook, you're kind of anonymous. | |
| Convenience: Well, the private messages just seem to be more convenient, and it’s – well, it’s not any more instant than e-mail, it just kind of happened that way. I just, I'm in Facebook, and I can private message somebody right there instead of going back into my e-mail. | |
| Moderate health communicators (MCs) | Altruism: I would post, “Hey, I have some kind of issue with my kidneys.” All that’s gonna do is open up, “What kind of issue? Oh my gosh, are you okay? What are they gonna do?” I have no room to answer a million questions. If I were to post about it, which unless they tell me it was something relative to diabetes, and the information can help someone else, that’s the only way I would post it. If not, I mean it’s my personal information. |
| Instrumental support: I belong to a diabetes care group that I get diabetes information on, although I don’t always find it to be real useful to me, I am controlling my diabetes with diet and exercise and it will only be one year since my diagnosis on September 25th. I'm fairly new to this, so I don’t find a lot of the information about meds and that kind of thing to be very helpful. I tend to look at more of their information on diet. | |
| Social support: I had a post this morning, I had a hypoglycemia issue about 4:30 this morning and I just, I was feeling poorly. I got something and I was kind of recovering, and I just posted an, “Argh, blood sugar dropping” on that, and that’s about it, really. I haven’t really posted anything related to health. The only thing I've done with the alternative diabetes is post my blood sugars in the morning, and I've just been on, associated with that group for just a few days, but I haven’t gotten very far with that. I may open up more, given that it’s a focus group on diabetes control. | |
| Privacy and stigma: In some ways, I’m embarrassed or ashamed to have it, but at the same time on the ADA board, or the forum, or even things from your site, like knowin’ your Facebook page.… As long as it’s just not—I guess my big thing is, is that as long as it’s not used against me in terms of employment, being rejected for something, that’s all. | |
| Convenience: I think [Facebook is] far more accessible, because I can go to it whenever I want to, rather than having to wait on somebody else’s schedule. To me, that is an important factor, and I have learned to appreciate it more as I've been involved with Facebook. | |
| Off-Facebook-only health communicators (OCs) | Instrumental support: I belong to an online community where I share information about one of my conditions and also take surveys about conditions as well as occasionally participate in in-person focus groups regarding a medical condition so I don't feel a need to do this on [F]a[c]ebook. |
| Social support: No. I mean the diabetes [group], but I don’t really post anything. I just see if anybody has any recommendations for anything or links to where, you know, make it, help with prescriptions and what not. | |
| Privacy and stigma: Well, because even though I have a lot of family and friends on [Facebook] – I mean I don’t really know how to describe this. It’s not really everybody’s business of what’s going on with my health. Just immediate family. | |
| Convenience: Just the typing. I type all day at work, so it’s a pain in the butt to have to do it when I’m not there. It’s much easier to pick up the phone and call. | |
| Facebook knowledge: I really don't know how exactly Facebook works other than reading comments from family members, friends etc who's comments I occasionally comment on. | |
| Nondisclosing health communicators (NCs) | Instrumental support: Same as regarding Facebook: health information is for the use of healthcare professionals and myself. Communicating with others has shown to be of little value (to me) in handling my diabetes or other health issues. |
| Social support: Who cares about me? | |
| Privacy and stigma: I refuse to be the typical senior who whines about health problems all the time. I manage my health problems and keep most of it to myself. | |
| Convenience: I don't have access to a computer 2 hrs. a day at the public library. Most of my time is taken up dealing with emails. |
Some themes were present in a subset of profiles, whereas others were present across all profiles but discussed in different ways. For example, participants in FC and MC stated rationales related to altruism; participants in OC or NC did not mention this theme. Similarly, only participants in OC discussed the impact of their knowledge of Facebook on their health information communication practices. In contrast, participants in all 4 themes mentioned rationales related to instrumental support, social support, privacy and stigma, and convenience. However, whereas participants in FC framed these themes positively, participants in MC or OC expressed reservations, and participants in NC framed these themes negatively.
DISCUSSION
Using a large sample survey and cluster analysis techniques, this study identified 7 approaches to communicating health information with social networks on and off Facebook. In contrast to studies limited to activity within Facebook groups defined by a shared health condition,33,36,47 ours also focused on other communication mechanisms within Facebook.46 Moreover, the social networks on which our participants reported were not defined solely by a shared medical condition, but also by personal relationships. This study also extended previous research by simultaneously examining how participants communicated with their Facebook social networks both on and off Facebook. The emergence of 7 clusters demonstrates variability in how individuals living with type 2 diabetes talk to friends, family members, and others about their health, revealing a need for consumer health IT designers to create tailored or customizable solutions supporting the diversity of communication needs and practices.
While the results of our study contradict previous findings related to health information communication on Facebook, they support previous findings related to such communication off Facebook. Unlike previous studies concluding that Facebook is not an established space for communicating health information,19,32,49 ours demonstrates wide adoption for this purpose. Over two-thirds of participants (ie, participants in FC-H, MC-H, and MC-L) stated that they used Facebook to communicate health information, and for participants in FC-H, health information communication was more frequent on than off Facebook. Secondary analysis of interview data suggests that these individuals were motivated by the ability to obtain both instrumental and social support as well as the convenience of using Facebook. Research has shown that people are willing to communicate health information in the context of Facebook groups to individuals with a shared condition.36,47 Our study supports this finding but also suggests that for participants in FC-H, MC-H, and MC-L, Facebook is used at least as often to communicate health information with personal social networks through timelines and other mechanisms. In contrast, our results align with previous studies18,19,37 demonstrating the adoption of multiple off-Facebook communication mechanisms for health information communication. With a larger sample size, our study supports prior conclusions37 that individuals most frequently engage in off-Facebook health information communication in person and via telephone and e-mail.
The adoption of Facebook for health information communication demonstrated in our study is significantly greater within the United States57 than the adoption rates of traditional consumer health IT, such as text message reminders and mobile health applications, many forms of which have limited functionality and do not support health information communication.58 This differential adoption rate may be due to the fact that Facebook better integrates multiple aspects of health management, including the types of support sought and people engaged.8–10,17,21 Moreover, Facebook may integrate more seamlessly with participants’ everyday communication practices. Data from this study demonstrate that individuals who more frequently communicate health information on Facebook are also generally more active on the platform (ie, FC-H and MC-H). Specifically, these individuals engage more frequently with the majority of Facebook communication mechanisms and have built social networks encompassing the widest range of people. Moreover, participants in these profiles mentioned the benefit of being able to use Facebook on their own terms and not having to engage in the extra effort of switching communication platforms. These results suggest that when designing for the FC-H and MC-H profiles, consumer health IT solutions should not be stand-alone solutions. Instead, for these profiles, they should ideally be integrated into broader communication platforms, or at the very least support communication about health in ways that do not segment health from other communication practices of daily life.4
Moreover, profiles were primarily distinguished by quantitative differences in health information communication activity across mechanisms on and off Facebook (the degree to which each mechanism is used) rather than within mechanisms (which mechanism is used). Thus, individuals engaging in health information communication (all profiles except NC-H and NC-L) would benefit from consumer health IT that integrates or interfaces with a wide range of off-Facebook communication mechanisms. Currently, consumer health IT supporting health information communication is severely limited in functionality with regard to the many mechanisms that participants use, such as texts, blogs, and videoconferences.18,19 However, such integration is feasible. For example, CaringBridge59 currently integrates the functionality of a blog, which was used for health information communication by participants in 5 of the 7 profiles. An alternative solution would be to create consumer health IT that enables posting of an internal journal or other information directly to an external blog. Similarly, there is an opportunity to integrate or interface with the range of communication mechanisms currently available on Facebook46 to better support the FC-H, MC-H, and MC-L profiles. It is important to note that these functionalities would likely be used to varying degrees across profiles.
Previous studies have indicated that privacy concerns are a barrier to communicating about health on Facebook,60,61 and this concern was primarily expressed by individuals in the OC and NC profiles. Stigma associated with type 2 diabetes62,63 may have also played a role not only for profiles that did not communicate health information on Facebook, but also for the MC-H and MC-L profiles, as mentioned by interview participants. It is unclear if different design features would encourage greater communication by individuals by addressing concerns related to privacy and stigma. For example, consumer health IT could allow anonymous posting, which some participants in FC-H identified as a potential benefit of using Facebook for health information communication. One’s network could be alerted that someone had posted, while the poster remained unidentifiable. This would allow individuals to obtain instrumental and emotional support without sacrificing privacy or being personally stigmatized. Another option would be for software to recognize keywords in a draft message as the user is preparing it for posting, to then trigger reminders to change the recipients of that post and also make it easy to do so in the moment.15,64
Our study demonstrated few, if any, significant differences in health information communication profile compositions across race/ethnicity, gender, and education. One notable exception was a difference observed for individuals identifying as Hispanic; they were more likely to identify as FC-H than 4 other profiles. A likely reason for this is that the Hispanic sample in our study was significantly younger than participants identifying as non-Hispanic (44.6 vs 54.0, P < .05), and younger individuals were more likely to identify with the FC-H profile. This age difference is consistent with general demographic trends, which show that the median age of the Hispanic population is approximately one decade younger than the general US population.65
Across studies of consumer health IT use, there is no consensus on whether race/ethnicity, gender, and education are associated with significantly different practices. Results of studies of personal health record use vary, although the majority report significant differences based on race and education.66–73 In contrast, studies of Web-based consumer health IT unrelated to use of personal health records primarily show disparities across race/ethnicity, gender, and education.74–80 The impact of these demographic characteristics on consumer health IT use remains inconclusive, but demonstrative of differences. Although our findings demonstrate a general lack of difference in terms of approaches to health information communication, this finding primarily has implications for the design of functionality. Across race/ethnicity, gender, and education, individuals may still have different needs for consumer health IT supporting health information communication with regard to other design dimensions, such as the user interface.81 Consequently, designers should continue to engage with individuals identifying across race/ethnicity, gender, and education to determine the presence or absence of unique needs.82
Compared to all other profiles, FC-H differed significantly across multiple demographic characteristics: age, general health status, years diagnosed with diabetes, number of people in the household, household income, financial situation, employment status, insurance status, and technology access. Overall, individuals within FC-H are younger and healthier than in other profiles, and more likely to have higher household income, more people living in the household, employment, and Facebook access through multiple platforms. They are also less likely to have Medicare. Because the demographic composition of this profile is distinct from the others, a clear persona (ie, a fictitious, specific, concrete representation of target users)83 emerges to guide designers in creating consumer health IT that meets the needs of FC-H. Personas for the remaining profiles are less clear, since fewer significant demographic differences are evident. For these profiles, personas would need to be behaviorally distinguished,84 with less emphasis on demographic characteristics.
The strengths of this study stem from its patient-oriented survey instrument; large, nationwide, racially and ethnically stratified sample; and use of a commercial access panel (allowing the survey to be administered over a few days, eliminating historical effects). However, several limitations exist. First, the sample clustered into unequal profiles. Consequently, failure to demonstrate a significant difference between 2 profiles does not conclusively indicate that 1 would not be obtained with larger numbers of individuals in the smaller profiles. Second, we used type 2 diabetes as a case study. Whether the profiles would be similarly distinct for individuals with a different condition is unknown. Third, given the study’s purpose of drawing design guidance for consumer health IT, it is important to note that it only focused on Facebook users, which constitute only 72% of adults online.45 While profiles NC-L, NC-H, OC-L, and OC-H were smaller than the others, their relevance (no health information communication on Facebook) is likely greater in the larger population. Fourth, focusing solely on Facebook networks means we cannot draw conclusions regarding how participants communicate health information to people outside these networks. Fifth, this study relies on self-report, and future work might seek validation by comparing these findings with observed communication practices on and off Facebook.
CONCLUSION
Individuals with type 2 diabetes have differentially adopted and adapted Facebook to meet their health information communication needs. Some, such as the loquacious individuals in profile FC-H, freely engage social network members in health information communication both on and off Facebook; others, such as the reticent individuals in NC-L and NC-H, do not communicate about health matters with members of their Facebook network through any mechanism. Still others (OC-H and OC-L) choose to discuss health with others in their Facebook networks only through offline mechanisms. By showing the existence of 7 distinct but fairly prevalent profiles among Facebook users who have type 2 diabetes and describing their characteristics and concerns, we have sought to demonstrate the diversity of patient approaches that may need to be supported by consumer health IT.
Moreover, the evolution of these profiles should be studied over time to see how age, cohort, and period effects may impact their prevalence and demographic composition. For example, individuals in profile FC-H may be considered closer to digital natives85 in terms of age and behavior. Further research is needed to determine if more individuals will segment into this profile over time and if individuals in this profile will retain their open health information communication practices or transition to other profiles as they age and their disease progresses. Such changes may cause the composition of each profile to drift. Consumer health IT design must not only be responsive to the needs of all profiles, from loquacious to reticent, but also iterative, adapting to the changing demographics of these key patient groups.
FUNDING
This work was supported by Agency for Healthcare Research and Quality grant number R03 HS22930-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
RSV contributed to study design, data collection, and analysis, and took primary responsibility for drafting the manuscript. TMG contributed to study design, data collection, and analysis, and drafted portions of the methods section. KF contributed to data analysis and drafted portions of the methods section. ICW contributed to study design and data collection and analysis. CAW and JEB contributed to data analysis. HKM contributed to data collection. All authors critically revised the manuscript for important intellectual content, approved the final version to be published, and agreed to be accountable for all aspects of the work.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank the administrators of the Facebook groups and pages who supported our study and all of our participants. We would also like to thank the anonymous reviewers whose thoughtful comments strengthened this manuscript.
REFERENCES
- 1. Batalden M, Batalden P, Margolis P et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;257:509–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thompson MJ, Valdez RS. Online Filipino-Americans' perspectives on informatics-enabled health management. Health Policy and Technol. 2015;44. [Google Scholar]
- 3. Carman KL, Dardess P, Maurer M et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). 2013;322:223–31. [DOI] [PubMed] [Google Scholar]
- 4. Valdez RS, Holden RJ, Novak LL et al. Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Inform Assoc. 2015;221:2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;322:207–14. [DOI] [PubMed] [Google Scholar]
- 6. Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients' ‘scores.' Health Aff (Millwood). 2013;322:216–22. [DOI] [PubMed] [Google Scholar]
- 7. Sarkar U, Bates DW. Care partners and online patient portals. JAMA. 2014;3114:357–58. [DOI] [PubMed] [Google Scholar]
- 8. Skeels MM, Unruh KT, Powell C et al. Catalyzing social support for breast cancer patients. CHI Conf Proc. 2010:173–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Valdez RS, Brennan PF. Exploring patients' health information communication practices with social network members as a foundation for consumer health IT design. Int J Med Inform. 2015;845:363–74. [DOI] [PubMed] [Google Scholar]
- 10. Zhou X, Sun S, Yang J. Sweet home: understanding diabetes management via a Chinese online community. Proceedings of the 32nd Annual ACM Conference on Human Factors in Computing Systems. 2014;3997–4006. [Google Scholar]
- 11. Nambisan P. Information seeking and social support in online health communities: impact on patients' perceived empathy. J Am Med Inform Assoc. 2011;183:298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Flaherty D, Hoffman-Goetz L, Arocha JF. What is consumer health informatics? a systematic review of published definitions. Inform Health Soc Care. 2015;402:91–112. [DOI] [PubMed] [Google Scholar]
- 13. Gibbons MC, Wilson RF, Samal L et al. Impact of consumer health informatics applications. Evid Rep Technol Assess (Full Rep). 2009;188:1–546. [PMC free article] [PubMed] [Google Scholar]
- 14. Or CK, Ben-Tzion. A systematic review of patient acceptance of consumer health information technology. J Am Med Inform Assoc. 2009;164:550–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hartzler A, Skeels MM, Mukai M et al. Sharing is caring, but not error free: Transparency of granular controls for sharing personal health information in social networks. AMIA Annu Symp Proc. 2011;2011:559. [PMC free article] [PubMed] [Google Scholar]
- 16. Weiss JB, Lorenzi NM. Online communication and support for cancer patients: a relationship-centric design framework. AMIA Annu Symp Proc. 2005:799–803. [PMC free article] [PubMed] [Google Scholar]
- 17. Pratt W, Unruh KT, Civan A et al. Personal health information management. Commun ACM. 2006;49:51–55. [Google Scholar]
- 18. Valdez RS. Creating a Foundation for the Design of Culturally Informed Consumer Health IT. Industrial and Systems Engineering: University of Wisconsin-Madison; 2012. [Google Scholar]
- 19. Pang C, Neustaedter C, Riecke BE et al. Technology preferences and routines for sharing health information during the treatment of a chronic illness. SIGHI Conference on Human Factors in Computing Systems. Paris, France: ACM; 2013: 1759–68. [Google Scholar]
- 20. Carron-Arthur B, Ali K, Cunningham JA et al. From help-seekers to influential users: a systematic review of participation styles in online health communities. J Med Internet Res. 2015;17:e271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Johnston AC, Worrell JL, Di Gangi PM et al. Online health communities: an assessment of the influence of participation on patient empowerment outcomes. Inform Technol People. 2013;26:213–35. [Google Scholar]
- 22. Nath C, Huh J, Adupa AK et al. Website sharing in online health communities: a descriptive analysis. J Med Internet Res. 2016;18:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Buis LR. Emotional and informational support messages in an online hospice support community. Comput Inform Nurs. 2008;26:358–67. [DOI] [PubMed] [Google Scholar]
- 24. Wicks P, Keininger DL, Massagli MP et al. Perceived benefits of sharing health data between people with epilepsy on an online platform. Epilepsy Behav. 2012;231:16–23. [DOI] [PubMed] [Google Scholar]
- 25. Myneni S, Cobb NK, Cohen T. Finding meaning in social media: content-based social network analysis of QuitNet to identify new opportunities for health promotion. Stud Health Technol Inform. 2013;192:807–11. [PubMed] [Google Scholar]
- 26. Mamykina L, Nakikj D, Elhadad N. Collective sensemaking in online health forums. Proceedings ACM Conference on Human-Factors in Computing Systems. 2015:3217–26. [Google Scholar]
- 27. Huh J, Ackerman MS. Collaborative help in chronic disease management: supporting individualized problems. CSCW. 2012:853–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wiederhold G, Shortliffe E. System design and engineering in health care. In: Shortliffe E, Cimino JJ, eds. Biomedical Informatics: Computer Applications in Health Care and Biomedicine. 3rd ed.New York: Springer Science+Business Media; 2006:233–64. [Google Scholar]
- 29. Samaras GM, Horst RL. A systems engineering perspective on the human-centered design of health information systems. J Biomed Inform. 2005;38:61–74. [DOI] [PubMed] [Google Scholar]
- 30. Dym CL, Little P. Engineering Design: a Project Based Introduction. 2nd ed.Charlottesville, VA: John Wiley and Sons; 2003. [Google Scholar]
- 31. Ploderer B, Reitberger W, Oinas-Kukkonen H et al. Social interaction and reflection for behaviour change. Personal Ubiquitous Comput. 2014;18:1667–76. [Google Scholar]
- 32. Newman MW, Lauterbach D, Munson SA et al. It's not that I don't have problems, I'm just not putting them on Facebook. Comput Support Coop Work. 2011:341–50. [Google Scholar]
- 33. Bender JB, Jiminez-Marroquin M, Jadad AR. Seeking support on Facebook: a content analysis of breast cancer groups. J Med Internet Res. 2011;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fox S. The Social Life of Health Information. Washington, D.C.: Pew Research Center's Internet and American Life Project; 2011. http://www.pewinternet.org/2011/05/12/the-social-life-of-health-information-2011/ (Accessed December 8, 2015). [Google Scholar]
- 35. Moreno MA, Jelenchick LA, Egan KG et al. Feeling bad on Facebook: depression disclosures by college students on a social networking site. Depress Anxiety. 2011;28:447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhang Y, He D, Sang YM. Facebook as a platform for health information and communication: a case study of a diabetes group. J Med Syst. 2013;37:9942. [DOI] [PubMed] [Google Scholar]
- 37. Skeels MM. Sharing by Design: Understanding and Supporting Personal Health Information Sharing and Collaboration Within Social Networks. Seattle: University of Washington; 2010. [Google Scholar]
- 38. Subrahmanyam K, Reich SM, Waechter N et al. Online and offline social networks: use of social networking sites by emerging adults. J Appl Dev Psychol. 2008;29:420–33. [Google Scholar]
- 39. Marwick AE, Boyd D. I tweet honestly, I tweet passionately: Twitter users, context collapse, and the imagined audience. New Media Soc. 2010;13:114–33. [Google Scholar]
- 40. Kim Y, Sohn D, Choi SM. Cultural difference in motivations for using social network sites: A comparative study of American and Korean college students. Comput Hum Behav. 2011;27:365–72. [Google Scholar]
- 41. Baek YM, Wojcieszak M, Delli Carpini MX. Online versus face-to-face deliberation: Who? Why? What? With what effects? New Media Soc. 2011;14:363–83. [Google Scholar]
- 42. Greene JA, Choudhry NK, Kilabuk E et al. Online social networking by patients with diabetes: a qualitative evaluation of communication with Facebook. J Gen Intern Med. 2011;26:287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wasko ML, Faraj S. Why should I share? examining social capital and knowledge contribution in electronic networks of practice. MIS Quarterly. 2005;29:35–57. [Google Scholar]
- 44. Myneni S, Cobb N, Cohen T. In pursuit of theoretical ground in behavior change support systems: analysis of peer-to-peer communication in a health-related online community. J Med Internet Res. 2016;18:e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Duggan M. Mobile Messaging and Social Media 2015. Pew Research Center, 2015. http://www.pewinternet.org/2015/08/19/mobile-messaging-and-social-media-2015/ (Accessed December 8, 2015). [Google Scholar]
- 46. Menefee HK, Thompson MJ, Guterbock TM et al. Mechanisms of communicating health information through Facebook: implications for consumer health IT design. J Med Internet Res (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Greene JA, Choudhry NK, Kilabuk E et al. Online social networking by patients with diabetes: a qualitative evaluation of communication with Facebook. J Gen Intern Med. 2011;26(3):287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Adzharuddin NA, Ramly NM. Nourishing healthcare information over Facebook. Procedia - Soc Behav Sci. 2015;172:383–89. [Google Scholar]
- 49. Gimenez-Perez G, Recasens A, Simo O et al. Use of communication technologies by people with type 1 diabetes in the social networking era. A chance for improvement. Prim Care Diabetes. 2016;102:121–28. [DOI] [PubMed] [Google Scholar]
- 50. Oh HJ, Lauckner C, Boehmer J et al. Facebooking for health: an examination into the solicitation and effects of health-related social support on social networking sites. Comput Human Behav. 2013;29:2072–80. [Google Scholar]
- 51. Petrovski G, Zivkovic M, Stratrova SS. Social media and diabetes: can Facebook and Skype improve glucose control in patients with type 1 diabetes on pump therapy? One-year experience. Diabetes Care. 2015;38:e51–52. [DOI] [PubMed] [Google Scholar]
- 52. Qualtrics. Provo, UT; 2015. [Google Scholar]
- 53. Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA; 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf (Accessed December 8, 2015). [Google Scholar]
- 54. Centers for Disease Control and Prevention. Diabetes Report Card 2014. Atlanta, GA; 2015. http://www.cdc.gov/diabetes/pdfs/library/diabetesreportcard2014.pdf (Accessed December 8, 2015). [Google Scholar]
- 55. Lloyd SP. Least-Squares Quantization in PCM. IEEE Trans Inf Theory. 1982;28:129–37. [Google Scholar]
- 56. Valdez RS, Guterbock TM, Thompson MJ et al. Beyond traditional advertisements: Leveraging Facebook's social structures for research recruitment. J Med Internet Res. 2014;1610:e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Fox S, Duggan M. Mobile Health 2012. Pew Internet and American Life Project. Washington, DC; 2012. http://www.pewinternet.org/2012/11/08/mobile-health-2012/ (Accessed December 8, 2015). [Google Scholar]
- 58. IMS Institute for Healthcare Informatics. Patient Apps for Improved Healthcare: From Novelty to Mainstream. 2013. Danbury, CT. [Google Scholar]
- 59. CaringBridge. Eagan, MN; 2016. [Google Scholar]
- 60. Moorehead S, Hazlett D, Harrison L et al. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15:e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Antheunis M, Tates K, Nieboer T. Patients' and health professionals' use of social media in health care: motives, barriers and expectations. Patient Educ Counseling. 2013;92:e426. [DOI] [PubMed] [Google Scholar]
- 62. Della LJ, Ashlock MZ, Basta TB. Social constructions of stigmatizing discourse around type 2 diabetes diagnoses in Appalachian Kentucky. Health Commun. 2016;31:806–14. [DOI] [PubMed] [Google Scholar]
- 63. Potter L, Wallston K, Trief P et al. Attributing discrimination to weight: associations with well-being, self-care, and disease status in patients with type 2 diabetes mellitus. J Behav Med. 2015;38:863–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Dourish P, Anderson K. Collective information pracitce: exploring privacy and security as social and cultural phenomena. Human-Computer Interaction. 2006;21:319–42. [Google Scholar]
- 65. Pew Research Center. Median Age for Hispanics Is Lower Than Median Age for Total U.S. Population. 2012. Washington, D.C. [Google Scholar]
- 66. Sarkar U, Karter AJ, Liu JY et al. Social disparities in internet patient portal use in diabetes: evidence that that digital divide extends beyond access. J Am Med Inform Assoc. 2011;183:318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Jhamb M, Cavanaugh KL, Bian A et al. Disparities in electronic health record patient portal use in nephrology clinics. Clin J Am Soc Nephrol. 2015;10:2013–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Goel MS, Brown TL, Williams A et al. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med. 2011;26:1112–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Smith SG, O'Conor R, Aitken W et al. Disparities in registration and use of an online patient portal among older adults: findings from the LitCog cohort. J Am Med Inform Assoc. 2015;224:888–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ancker JS, Barron Y, Rockoff ML et al. Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med. 2011;26(10):1117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Riippa I, Linna M, Ronkko I et al. Use of an electronic patient portal among the chronically ill: an observational study. J Med Internet Res 2014;1612:e275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Osborn CY, Mayberry LS, Wallston KA et al. Understanding patient portal use: Implications for medication management. J Med Internet Res. 2013;157:e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Yamin CK, Emani S, Williams DH et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;1716:568–74. [DOI] [PubMed] [Google Scholar]
- 74. Kontos E, Blake KD, Chou WY et al. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res. 2014;167:e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Tennant B, Stellefson M, Dodd V et al. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J Med Internet Res. 2015;173:e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Eddens KS, Kreuter MW, Morgan JC et al. Disparities by race and ethnicity in cancer survivor stories available on the web. J Med Internet Res. 2009;114:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Glasgow RE, Christiansen SM, Kurz D et al. Engagement in a diabetes self-management website: usage patterns and generalizability of program use. J Med Internet Res. 2011;131:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bidmon S, Terlutter R. Gender differences in searching for health information on the internet and the virtual patient-physician relationship in Germany: exploratory results on how men and women differ and why. J Med Internet Res. 2015;176:e156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Diviani N, van den Putte B, Giani S et al. Low health literacy and evaluation of online health information: a systematic review of the literature. J Med Internet Res. 2015;175:e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Duplaga M. A cross-sectional study assessing determinants of the attitude to the introduction of eHealth services among patients suffering from chronic conditions. BMC Med Inform Decis Mak. 2015;15:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Valdez RS, Gibbons MC, Siegel ER et al. Designing consumer health to enhance usability among different racial and ethnic groups within the United States. Health Technol. 2012;2:225–33. [Google Scholar]
- 82. Brennan PF, Valdez R, Alexander G et al. Patient-centered care, collaboration, communication and coordination: a report from AMIA’s 2013 policy meeting. J Am Med Inform Assoc. 2015;22(e1):e2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Pruitt J, Adlin T. The Persona Lifecycle: Keeping People in Mind Throughout Product Design. San Francisco, CA: Morgan Kauffmann Publishers; 2006:11. [Google Scholar]
- 84. Vosbergen S, Mulder-Wiggers JM, Lacroix JP et al. Using personas to tailor educational messages to the preferences of coronary heart disease patients. J Biomed Inform. 2015;53:100–12. [DOI] [PubMed] [Google Scholar]
- 85. Prensky M. Digital natives, digital immigrants. In: Prensky M, ed. On the Horizon. Bingley, UK: MCB University Press; 2001:9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.