Abstract
Few opportunities exist for physician trainees to gain exposure to, and training in, the field of clinical informatics, an Accreditation Council for Graduate Medical Education–accredited, recently board-certified specialty. Currently, 21 approved programs exist nationwide for the formal training of fellows interested in pursuing careers in this discipline. Residents and fellows training in medical and surgical fields, however, have few avenues available to gain experience in clinical informatics. An early introduction to clinical informatics brings an opportunity to generate interest for future career trajectories. At University of California Los Angeles (UCLA) Health, we have developed a novel, successful, and sustainable program, the Resident Informaticist Program, with the goals of exposing physician trainees to the field of clinical informatics and its academic nature and providing opportunities to expand the clinical informatics workforce. Herein, we provide an overview of the development, implementation, and current state of the UCLA Health Resident Informaticist Program, with a blueprint for development of similar programs.
Keywords: informatics, education, mentors, curriculum
BACKGROUND
Health information technology (HIT), the field of information sciences that utilizes technologies to store, share, and analyze health information,1 remains a profession in relative infancy. While the field continues to define itself and evolve, the composition of what will make a mature workforce of HIT professionals remains unclear.2,3 It is clear, however, that including health care professionals in the ultimate HIT workforce framework will be elemental and critical.2–4 According to William Hersh, the health care information technology workforce should include clinicians involved in HIT development, implementation, and management on a full- or part-time basis.5
In 2005, the American Medical Informatics Association (AMIA) recognized this growing demand for physicians with formal HIT training and for a certification process for clinical informatics, the discipline of applying HIT to delivering health care services.4,6 AMIA defines clinical informaticians (or informaticists) as “those who transform health care by analyzing, designing, implementing, and evaluating information and communication systems that enhance individual and population health outcomes, improve patient care, and strengthen the clinician-patient relationship.”6,7 AMIA led the process of defining core content for the subspecialty of clinical informatics, now accredited by the Accreditation Council for Graduate Medical Education (ACGME) and sponsored by the American Board of Preventive Medicine, as well as training requirements for clinical informatics fellowships.6 The clinical informatics subspecialty board exam was first administered in October 2013. Currently, there are 21 accredited clinical informatics fellowship programs in the United States, being held to standard ACGME requirements of providing thorough, organized, and comprehensive training. Each 2-year training program typically enrolls 1 to 2 fellows. In endeavoring to develop programs that provide proper training for physicians entering IT fields, AMIA further recognized the additional potential of strengthening the HIT workforce.3,4,6
Fully trained and practicing clinicians can find education through the AMIA 10 × 10 programs, whose initial goal was to ensure that every hospital had 1 physician and one nurse trained in informatics.8 A number of US medical schools currently offer courses in HIT and clinical informatics, with some offering additional graduate degrees and others incorporating coursework as part of the medical school curriculum.9 Few residency training programs in informatics exist. Stanford and Partners Healthcare, associated with the Harvard School of Medicine, offers 2-week or 1-month elective rotations for residents to be exposed to various topics in the field of biomedical and clinical informatics.10,11 These programs include a requirement to either design or complete a project during the rotation.10,11 At UCLA Health, we have developed a novel program to provide formal training in clinical informatics for residents and fellows in medical and surgical fields on a larger scale than what could otherwise be provided by a shorter elective.
Program overview
The UCLA Health Resident Informaticist (RI) Program is taught by the UCLA Physician Informaticist (PI) Committee, a group of 21 physicians, all of whom have obtained build certification in our electronic health record (EHR); 14 have American Board of Preventive Medicine certification in clinical informatics and 2 have completed an AMIA 10 × 10 course. The PIs receive 20–70% support from the health system to work on clinical informatics. The program includes a structured curriculum (see below). The program has a mandatory monthly 90-min session, which includes didactic lectures on a broad variety of health IT topics taught by PIs or local experts, and a journal club that highlights the field as an academic discipline. In addition, each RI designs an informatics project with the intent to complete it during enrollment in the program. All RIs are provided with an HIT textbook, and assigned readings serve as the basis of monthly didactic topics. RIs can extend their enrollment in the program for a second year. The program started in 2013, and a new cohort starts each academic year.
Program details
Program Acceptance. Trainees at postgraduate year 2 and above are eligible to apply. Interns are ineligible because their participation may not comply with ACGME-mandated duty hours. The application solicits information about the trainee’s interests in informatics, experience, project ideas, and ability to participate in program requirements. Applications are reviewed and ranked by the UCLA PI Committee. The number of positions offered each year varies based on the availability of PI mentors and health IT department/EHR technical team resources.
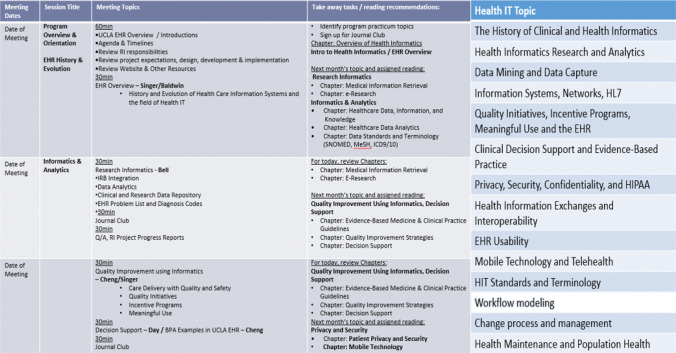
Curriculum. The PI faculty develop the yearlong curriculum, covering major topics in the field of clinical informatics (an excerpt of which can be found in Figure 1) and identifying matching reading materials from an HIT textbook. RIs are invited to participate in EHR build sessions taught by the PIs. All RIs are given access to an EHR practice environment in order to learn, practice, and develop these skills. Further, RIs lead discussions of journal articles about clinical informatics during monthly meetings. Each RI is expected to present one article during the course of enrollment.
Program Practicum. All RIs are mentored by a PI to design, develop, and implement a clinical informatics project with the intent to complete it within the academic year. Each RI is also matched with a health IT department/EHR technical team member, who aids in the technical completion of the project. Through the process, RIs gain an understanding of process and workflow design. Some participate in strategic meetings with key stakeholders and hospital/IT leadership. At the end of each academic year, the RIs present their work at a symposium attended by health system leadership.
Project Stipend. Each RI who successfully completes the program is awarded a $1500 stipend to serve as an academic enrichment fund. RIs are permitted to use these funds for academic travel or for educational supplies, such as laptops, tablets, or textbooks.
Participation in the RI program satisfies the requirement of ACGME milestone competencies in areas related to training in HIT.
Figure 1.
Excerpt from UCLA Resident Informaticist Program monthly curriculum, including covered health IT topics.
RESULTS
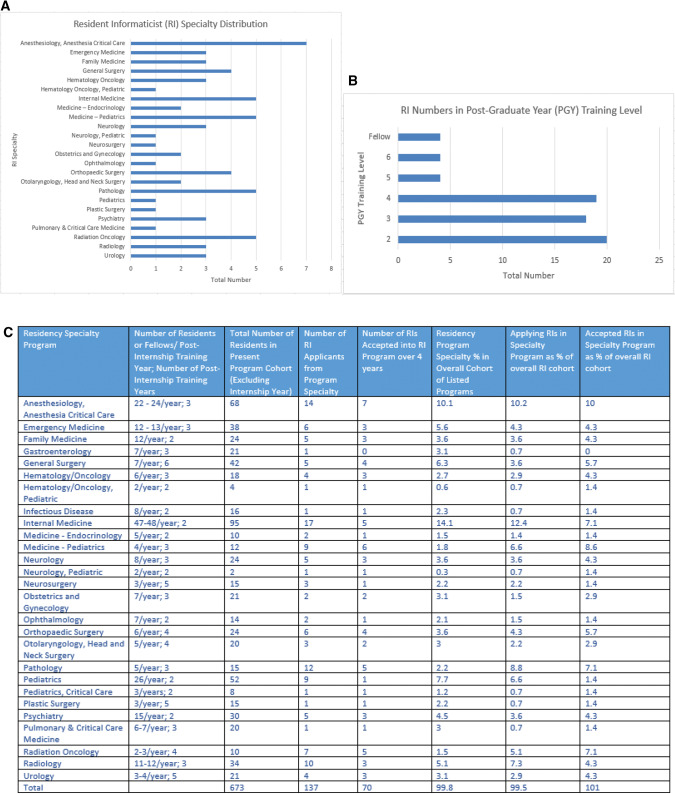
Currently in its fourth year, the RI program has received applications from 137 residents and fellows and has accepted 70 applicants (51% acceptance). Figures 2 A and B show RI distribution according to specialty and postgraduate training level. Figure 2C shows the overall cohort of the training programs from which we have received RI applicants. Further demonstrated are the numbers and percentages of RI applicants and participants as a proportion of the overall residency cohort.
Figure 2.
(A) Distribution of RIs by specialty. (B) Distribution of RIs by postgraduate training level. (C) Overall UCLA residency specialty cohort and overall RI cohort distribution.
Among the first 53 RIs accepted, 50 completed the program. Among their projects, 27 (55%) resulted in positive changes impacting patient care, provider efficiency and workflow, reporting, or end user training. The proportion of projects resulting in enhancements (Table 1) has increased annually: 8/18 (44%) in program year (PY) 1, 9/16 (56%) in PY2, and 11/15 (73%) in PY3. Within the first 3 years of the program, 3 RIs have had abstracts accepted for presentation at our annual national EHR vendors’ user group meetings and/or annual AMIA meetings. Three RIs extended enrollment in the program in PY2 and 3 in PY3. One RI has applied, and been accepted, for matriculation in a Clinical Informatics Fellowship Program. Four of 49 RIs (8%) who completed the program have secured faculty positions that include some component of clinical informatics work. Table 2 shows a breakdown and totals of yearly program expenses.
Table 1.
2013–2016 UCLA resident informaticist participant information and project titles
| Resident Informaticist (RI) Specialty | RI Postgraduate (PG) Training Level | RI Project Title |
|---|---|---|
| Anesthesiology | 2 | Reimagining CareConnect Training for Anesthesia Residents |
| Neurosurgery | 6 | Use of Mobile EHR Computing to Improve Communication Between Physicians and Prevent Signout Errors |
| Internal Medicine | 4 | *Using the EHR to Improve Population Health Performance in Residency Education |
| Psychiatry | 3 | *Electronic Medical Records and Legal Status in Psychiatry |
| Radiology | 2 | Optimizing Computerized Physician Order Entry for Research Scans |
| Pathology | 4 | Department of Pathology: GYN Cytology (Pap Smears) Orders Interface |
| Neurology | 4 | Development of Natural Language Processing Tools for the Identification of Stroke Quality Measures |
| Medicine – Pediatrics | 4 | *Implementation of Best Practice Advisories for the Identification of Chronic Kidney Disease |
| General Surgery | 4 | *Improving SCIP Antibiotic Compliance |
| Radiation Oncology | 4 | Patient Health History Questionnaires and CareConnect |
| Internal Medicine | 3 | Patient Health History Questionnaires and CareConnect |
| Hematology Oncology | 3 | CareConnect and Cancer Registry Data: Meaningful Use and Compatibility with Quality Metrics |
| Obstetrics and Gynecology | 4 | *Labor and Delivery Orders and Documentation Worfklow Optimization |
| Medicine – Endocrinology | 4 | *Building a Preference Med List for Endocrine Clinics |
| Orthopedic Surgery | 3 | *Resident eLearning Modules |
| General Surgery | 4 | *Individualizing Signout Reports for Specific Surgical Services |
| Anesthesiology | 2 | A CareConnect Dashboard for Administrators to Track Anesthesiology Resident Progress Toward ACGME Competencies |
| Emergency Medicine | 3 | *Improving ED Efficiency with a Diagnosis-Driven SmartSet |
| Radiology | 2 | Using the EHR to Facilitate the Protocoling and Ordering of Radiopharmaceuticals Involving Nuclear Medicine Studies |
| Radiology | 2 | Automated Quantification of Radiology Report Discrepancies |
| Radiation Oncology | 5 | Cancer Care Summary |
| Neurology | 3 | *Using e-Calculators to Improve Care in Patients with Atrial Fibrillation |
| Urology | Fellow | *SMS Text Messages Following Discharge from the UCLA Emergency Department |
| Medicine – Endocrinology | Fellow | *Developing a Diabetes Care Health Maintenance Module |
| Orthopedic Surgery | 2 | *e-Prescribing of Controlled Substances |
| Emergency Medicine | 2 | *Design and Implementation of Relevant Data Report Tools |
| Family Medicine | 2 | *How Patients Use MyChart: An Analysis of the Demographics and Usage Patterns for UCLA’s Patient Portal |
| Family Medicine | 3 | Billing Education Initiative. UCLA Family Health Center |
| Urology | 4 | *Introducing Quality Care Indicators for Benign Prostatic Hyperplasia into CareConnect to Improve the Value of Care Delivery |
| Anesthesiology | 3 | Optimization of the PACU Status Board |
| General Surgery | 3 | *iPad Consent – Tablets for Mobile Documentation of Surgical Consent |
| Anesthesiology | 2 | CareConnect Training Tools for Anesthesia Providers |
| Psychiatry | 4 | *e5150 Project |
| Pediatric Hematology Oncology | 6 | *Developing Problem List Quality Metrics for Clinical Care, Research, and Quality Improvement |
| Ophthalmology | 3 | Best Practice Advisories for the Stein Eye Insitute |
| Clinical Pathology | 2 | Integration of Pathology Results in a Disease-Specific Manner |
| Radiation Oncology | 4 | *Utilizing the Electronic Medical Record to Screen for Patients Who Might Benefit from Postoperative Radiotherapy Following Radical Prostatectomy |
| Transfusion Medicine – Pathology | 4 | *Improving Blood Transfusion Safety and Monitoring Through CPOE Assistive Texts and Transfusion Synoptic Dashboard |
| Anesthesiology | 3 | Association Between BMI and Postoperative Oxygen Saturation at Ambulatory Surgery Centers |
| Otolaryngology – Head and Neck Surgery | 2 | *Improving Signout and Rounding Lists in CareConnect |
| Orthopedic Surgery | 3 | *Surgical Case Logging for Residents |
| Orthopedic Surgery | 3 | *Improvement of Procedural Documentation (ProcDoc) |
| Emergency Medicine | 3 | *Relevant Data Support Tools in the Emergency Department: Infections in Immunocompromised Patients |
| Obstetrics and Gynecology | Fellow | *The UCLA Baby-Friendly Health Initiative: Using Patient-Facing EHR Tools for Health Education and Engagement |
| Urology | 4 | *Building an Effective Prostate Cancer Snapshot |
| Child Neurology | 4 | *Improvement of UCLA CareConnect Inbasket Utilization |
| Internal Medicine | 4 | *Incorporating Gender Identity into CareConnect |
| Pulmonary and Critical Care Medicine | 4 | Utilizing MyChart Questionnaires to Improve Care for Patients with COPD |
| Family Medicine | 3 | MyUCLAHealth Usage and Diabetic Control: Analysis of Patient Portal Usage |
| Hematology Oncology | Fellow | *Assessing the Compliance of UCLA’s EHR with FDA21 CFR P11 |
Projects that resulted in system enhancements are marked with an asterisk.
Table 2.
UCLA resident informaticist program expenses
| Itemized expense | PY1 (19 RIs) Expense | PY2 (16 RIs) Expense | PY3 (15 RIs) Expense |
|---|---|---|---|
| RI stipend ($1500/year) | $28 500 | $24 000 | $22 500 |
| Monthly meeting expenses (food, parking) | $70 | $70 | $80 |
| Yearly symposium expenses | $1250 | $2000 | $1500 |
| Academic meeting RI travel expenses | $0 | $3000 | $3000 |
| Overall program expenses | $29 820 | $29 070 | $27 080 |
DISCUSSION
Outcomes and successes
Figures 2A–C show information regarding the overall cohort of residency and fellowship programs at UCLA and their distribution by RI applicant and participant numbers. All levels of training are represented. Further, residents and fellows from a majority of our training programs are represented. As noted in the figure, some program specialties are disproportionately represented by both application number and participating RI number. A greater proportion of pathology, radiation oncology, and medicine-pediatrics residents and fellows have applied and participated, while a far smaller proportion of trainees from subspecialty fellowship programs (gastroenterology, infectious diseases, and pulmonary and critical care medicine) have applied and participated as compared to their distribution in the overall cohort. While these observations have not been formally studied, we have some hypotheses about these findings. First, it seems logical that fields rich in technology, like radiation oncology and pathology, would attract trainees interested in informatics endeavors. As of 2014, the number of pathologists board certified in clinical informatics was 3 times that of other physician specialties.12 For similar reasons, we suspect that the technology-rich fields of radiology and radiation oncology likewise appeal to a disproportionate number of trainees with informatics interests. On the other hand, programs disproportionately less represented are generally fields where RI applicants are fellows rather than residents. These trainees have already chosen career specialties with trajectories into highly specialized medical fields, while others may still be looking for future career interests. Further, fellows in highly specialized fields often pursue their academic interests through projects directly related to their training and perhaps have less time to devote to other interests. Finally, other outside influences such as a highly motivating PI in one field or better advertising of the program in other specialties, for example, could have influences on applicant attraction that have not been evaluated for this study. We suspect that these latter effects may be the basis for the disproportionately higher number of medicine-pediatrics applicants.
We evaluate the success of the RI program by the number of applications being submitted, the number of completed projects that have resulted in system improvement, and anonymous feedback surveys completed by the RIs upon graduation. By these measures, we consider the program to be a success. The number of applicants is consistently greater than the number of available slots. We consider projects to be successful when they result in system enhancements such as improved workflow or processes, streamlined patient care delivery, improved provider care delivery toward higher quality patient care, or technical advancements to our electronic health record or information services system. Some of those projects have included development of dashboards, preventive care trackers, clinical quality improvement projects, patient questionnaires, tools that improve and streamline provider efficiency in managing patient care and end user training, and reporting. Projects completed to date are listed in Table 1. While not all RI projects were considered successful by way of the stated definition of project success, all RIs gained experience in project design and development and the group benefited by learning what types of projects are feasible. Incidental benefits of the program include interdepartmental engagement of residents and fellows, many of whom work collaboratively on projects to achieve institutional project adoption. Objective success by way of qualitative or quantitative research is the basis of further studies of our RI program. Table 3 summarizes the results of RI program satisfaction surveys. Overall, the RIs report that the program is a rewarding experience with educational benefit and value for their training. PYs 2 and 3 brought improved RI satisfaction. With PY3, we added additional survey questions related to RI expectation and satisfaction (Figure 3).
Table 3.
Resident Informatics Program satisfaction survey results (2013–2016)
| UCLA Resident Informaticist (RI) Feedback 2013–2016 | |||||||
|---|---|---|---|---|---|---|---|
| Please rate the following statements about the Resident Informaticist Program | |||||||
| Question | Year |
Never |
Rarely |
Sometimes |
Usually |
Always |
RI comments |
| Number of Respondents | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| I clearly understood the educational goals and objectives of the program | (2013–2014) | 0 | 1 | 3 | 3 | 2 |
|
| (n = 9) | (0) | (11) | (33) | (33) | (22) | ||
| (2014–2015) | 0 | 0 | 0 | 2 | 9 | ||
| (n = 11) | (0) | (0) | (0) | (18) | (82) | ||
| (2015–2016) | 0 | 0 | 0 | 3 | 9 | ||
| (n = 12) | (0) | (0) | (0) | (25) | (75) | ||
| I had sufficient supervision and support from my mentors | (2013–2014) | 0 | 1 | 3 | 2 | 3 | |
| (n = 9) | (0) | (11) | (33) | (22) | (33) | ||
| (2014–2015) | 0 | 0 | 1 | 1 | 9 | ||
| (n = 11) | (0) | (0) | (9) | (9) | (82) | ||
| (2015–2016) | 0 | 0 | 0 | 4 | 8 | ||
| (n = 12) | (0) | (0) | (0) | (33) | (67) | ||
| I received an adequate amount of educational benefit from this program | (2013–2014) | 0 | 1 | 3 | 2 | 3 | |
| (n = 9) | (0) | (11) | (33) | (22) | (33) | ||
| (2014–2015) | 0 | 0 | 0 | 4 | 7 | ||
| (n = 11) | (0) | (0) | (0) | (36) | (64) | ||
| (2015–2016) | 0 | 0 | 0 | 1 | 11 | ||
| (n = 12) | (0) | (0) | (0) | (8) | (92) | ||
| My mentor was available to me and devoted the appropriate amount of time to teaching | (2013–2014) | 0 | 0 | 1 | 3 | 5 | |
| (n = 9) | (0) | (0) | (11) | (33) | (56) | ||
| (2014–2015) | 0 | 0 | 1 | 1 | 9 | ||
| (n = 11) | (0) | (0) | (9) | (9) | (82) | ||
| (2015–2016) | 0 | 0 | 0 | 3 | 9 | ||
| (n = 12) | (0) | (0) | (0) | (25) | (75) | ||
| My mentor communicated effectively | (2013–2014) | 0 | 0 | 0 | 1 | 8 | |
| (n = 9) | (0) | (0) | (0) | (11) | (89) | ||
| (2014–2015) | 0 | 0 | 1 | 1 | 9 | ||
| (n = 11) | (0) | (0) | (9) | (9) | (82) | ||
| (2015–2016) | 0 | 0 | 0 | 2 | 10 | ||
| (n = 12) | (0) | (0) | (0) | (17) | (83) | ||
| My mentor gave appropriate and constructive feedback | (2013–2014) | 0 | 0 | 0 | 1 | 8 | |
| (n = 9) | (0) | (0) | (0) | (11) | (89) | ||
| (2014–2015) | 0 | 0 | 1 | 1 | 9 | ||
| (n = 11) | (0) | (0) | (9) | (9) | (82) | ||
| (2015–2016) | 0 | 0 | 0 | 2 | 10 | ||
| (n = 12) | (0) | 0 | 0 | (17) | (83) | ||
Figure 3.
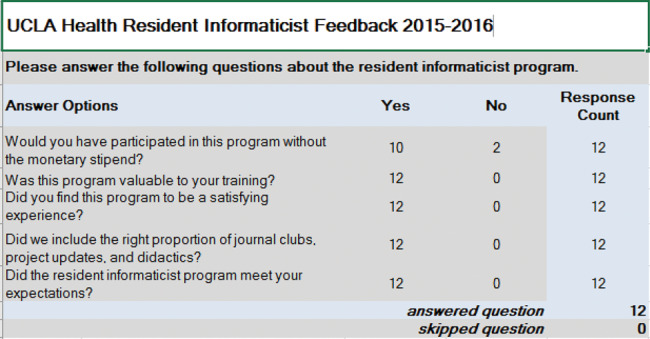
UCLA Health Resident Informaticist Program supplemental expectation and satisfaction survey responses for 2015–2016.
Programmatic challenges
We had to overcome 3 barriers in order to create and sustain the program. In PY1, we faced a number of administrative challenges. In order to achieve programmatic success, hospital and school of medicine support was critical. We met with the medical school dean to ensure that program requirements would not violate ACGME duty-hour regulations. Similar assurances were provided to training program directors, who have strongly endorsed the program to their trainees. Commitment by program directors to provide protected time for RI involvement has been requisite for RI acceptance to the program. Second, we had to determine a mechanism to provide a financial incentive for participation without violating restrictions regarding moonlighting and outside compensation. Including a stipend for RI participation was planned from program inception in order to provide some compensation for time spent in the program and working on informatics projects. While the majority of RIs would participate in the absence of the stipend, 2/10 RI respondents reported that the stipend was an important motivator for project completion and helped to prioritize their participation in the program among other competing responsibilities (Figure 3). While we are unable to distribute stipends directly to RIs, we are able to direct stipends to their respective program finance officers, who then open academic enrichment funds on their behalf. Our third challenge was in securing long-term funding from the health system for support of the program. Costs include the RI stipends, textbooks, expenses related to food budgets for monthly meetings, and end-of-year symposium expenses. Further, the program subsidizes travel-related expenses for RIs who have had projects accepted for presentation at national meetings. The health system has pledged its support by budgeting the program into yearly operating expenses.
In the first 2 years, attaining an adequate time commitment from our health IT department/EHR technical team/PI mentor group was challenging. Each PI mentor has competing time interests. All PIs continue to maintain busy clinical practices, and many have heavy administrative and research-related commitments. For some, carving out dedicated time to mentor RI projects posed a challenge. To address this, some PIs volunteered to mentor more RIs than others, and often 2 PI mentors were assigned to one RI in order to assure that project momentum continued in the event that 1 PI mentor was otherwise committed at critical junctures in project progress. Further, while the PIs are capable EHR-certified builders, many RI project design and build details required technical faculties beyond their scope of training. Technical team resources are limited, and during periods of EHR version upgrades, enhancements, institution of new modules, and build freezes, RI project progress sometimes met delays due to system priorities.
A final obstacle we faced was in balancing RI project interests with organizational priorities and institutional goals. When soliciting RI project plan ideas, we prioritize those that align with system projects already under way or with organizational priorities as defined by our health IT strategic road map in order to prevent significant diversion from organizational and strategic goals and priorities. However, we also endeavor to support RI project ideas that may not necessarily coordinate with priorities currently on our strategic road map, as we have found that many of those ideas often result in unanticipated but profound system benefits that might otherwise not be pursued. Available resources, both financial and workforce, may limit the ability to take on these types of projects; however, institutional leadership prioritization in support of this program has allowed for the dedication of time and resource commitments accordingly. Further, we have tightly refined our project selection process to include only project ideas that we believe have the potential for tangible process, system, and patient care improvements.
CONCLUSIONS
The UCLA RI Program has evolved each year by building on lessons learned from prior cohorts. We have modified the curriculum to cover what we believe are the most foundational topics. We have better aligned proposed RI projects with health system priorities, and the PIs are better able to recognize whether projects can be feasibly completed. As a result, RI satisfaction survey results have improved. Our goal is to provide a background in informatics for all RIs. While we are aware that the majority of those enrolled will not pursue further training or a career in the health informatics field, the program has generated interest for some graduates to pursue Clinical Informatics Fellowships and others to secure faculty positions including informatics work.
Clinical informatics and HIT resources within any health care system are limited; it is imperative to align programmatic goals and projects with the overall HIT strategic road map for such a program to prosper. With this program, we have built a novel pathway for resident and fellow trainees to gain exposure, access, and introduction to the fields of HIT and clinical informatics. While much work is needed to understand the ever-growing demand for a diverse health IT workforce, we believe that impactful programs such as ours are achievable and sustainable and can be additionally beneficial by contributing to a burgeoning need.
ACKNOWLEDGMENTS
We are grateful to the UCLA David Geffen School of Medicine. Without the support of our school of medicine and graduate training programs, this program would not be possible. We would also like to thank all the RIs, whose dedication to the program and enthusiasm for its success has made it a joy for us to teach. We are also grateful to the UCLA Health PIs for their dedication to the mentorship and teaching of our RIs, and to the UCLA Health IT Department technical team members, whose partnership on RI projects was an integral part of project and program success. Finally, we thank the senior leadership of the UCLA Health System and the UCLA Health Information Services and Solutions Health IT Department for support of and funding for the UCLA RI Program. Achieving success in a program such as this is not possible without the commitment and vision of health system leadership, the chief information officer, and the chief medical informatics officer, all of whom acknowledge the potential for profound benefits such as those we have realized. The UCLA Health Physician Informaticist Committee members are all affiliated with the UCLA Health Department of Information Services and Solutions at the David Geffen School of Medicine, with other departmental affiliations as follows:
John D Bartlett, MD, Department of Ophthalmology; Douglas S Bell, MD, PhD, Department of Medicine; Eric M Cheng, MD, MS, Department of Neurology; Annapoorna Chirra, MD, Department of Medicine; Lawrence D Dardick, MD, Department of Family Medicine; Frank C Day, MD, MPH, Department of Emergency Medicine; Christopher Denny, MD, Department of Pediatrics; Darryl T Hiyama, MD, Department of Surgery; Carlos F Lerner, MD, MPhil, Department of Pediatrics; Yu-Hsiang Clara Lin, MD, Department of Medicine; Lynne McCullough, MD, Department of Emergency Medicine; James M Moore, MD, Department of Anesthesiology; Arash Naeim, MD, PhD, Department of Medicine; Tina A Nguyen, MD, Department of Obstetrics and Gynecology; Michael A Pfeffer, MD, Department of Medicine; Mindy Ross, MD, Department of Pediatrics; Ariel Seroussi, MD, Department of Psychiatry; Jennifer S Singer, MD, Department of Urology; Daniel V Vigil, MD, Departments of Family Medicine and Orthopedic Surgery; Hawkin E Woo, MD, Department of Medicine; Allan D Wu, MD, Department of Neurology.
FUNDING Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sector.
COMPETING INTERESTS
The authors have no competing interests to declare.
Contributorship statement
JS, EC, MF, and KB designed, developed, and implemented the UCLA RI Program from conception to inception. The UCLA Physician Informaticist Committee members contributed to the operations and mentorship of the UCLA Health RI Program. JS drafted the manuscript. EC, MF, and KB provided manuscript revisions. All authors approved publication of the final manuscript.
REREFENCES
- 1. HealthIT.gov. https://www.healthit.gov/patients-families/basics-health-it. Accessed October 4, 2016.
- 2. Hersh J, Margolis A, Quiros F et al. Building a health informatics workforce in developing countries. Health Aff. 2010;2:274–77. [DOI] [PubMed] [Google Scholar]
- 3. Detmer DE, Munger BS, Lehmann CU. Clinical informatics board certification: history, current status, and predicted impact on the clinical informatics workforce. Appl Clin Inf. 2009;1:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kulikowski CA, Shortliffe EH, Currie LM et al. AMIA Board white paper: definition of biomedical informatics and specification of core competencies for graduate education in the discipline. J Am Med Inform Assoc. 2012;19:931–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hersh J. Who are the informaticians? What we know and should know. J Am Med Inform Assoc. 2006;13:166–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. AMIA. https://www.amia.org/clinical-informatics-board-review-course/history. Accessed August 2, 2016.
- 7. Safron C, Shabot M, Munger BS et al. Program requirements for fellowship education in the specialty of clinical informatics. J Am Med Inform Assoc. 2009;15:158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. AMIA. https://www.amia.org/education/10x10-courses. Accessed August 2, 2016.
- 9. AMIA. https://www.amia.org/education/programs-and-courses. Accessed August 2, 2016.
- 10. Partners Healthcare. http://informatics.partners.org/elective-rotation/. Accessed August 2, 2016.
- 11. Stanford School of Medicine. http://peds.stanford.edu/Rotations/medical_informatics/documents/medical-informations-rotation-summary.pdf. Accessed August 2, 16.
- 12. AMIA. https://learn.amia.org/topics/4. Accessed August 15, 2016.