Abstract
COVID-19 can evolve to a severe lung compromise with life-threatening hypoxemia. The mechanisms involved are not fully understood. Their understanding is crucial to improve the outcomes. Initially, past-experience lead to the implementation of standardized protocols assuming this disease would be the same as SARS-CoV. Impulsive use of ventilators in extreme cases ended up in up to 88% fatality. We compare medical and physiological high altitude acute and chronic hypoxia experience with COVID-19 hypoxemia. A pathophysiological analysis is performed based on literature review and histopathological findings. Application of the Tolerance to Hypoxia formula = Hemoglobin/PaCO2 + 3.01 to COVID-19, enlightens its critical hypoxemia. Pneumolysis is defined as progressive alveolar-capillary destruction resulting from the CoV-2 attack to pneumocytes. The adequate interpretation of the histopathological lung biopsy photomicrographs reveals these alterations. The three theoretical pathophysiological stages of progressive hypoxemia (silent hypoxemia, gasping, and death zone) are described. At high altitude, normal low oxygen saturation (SpO2) levels (with intact lung tissue and adequate acid–base status) could be considered silent hypoxemia. At sea level, in COVID-19, the silent hypoxemia starting at SpO2 ≤ 90% (comparable to a normal SPO2 {88–92%} at 3500 m) suddenly evolves to critical hypoxemia. This, as a consequence of progressive pneumolysis + inflammation + overexpressed immunity + HAPE-type edema resulting in pulmonary shunting. The proposed treatment is based on the improvement of the Tolerance to Hypoxia (Hemoglobin factor), oxygen therapy, inflammation reduction, antibiotics, antitussives, rehydration & anticoagulation if required. Understanding the pathophysiology of COVID-19 may assist in this disease's management.
Keywords: HAPE, Tolerance to hypoxia, SARS-cov-2, Pneumolysis, EPO, Open circuit earth space suits
Introduction
COVID-19 has been referred to as the most significant public health crisis since World War II [1]. Fifty years of experience treating patients at high altitude are useful in explaining the critical hypoxia encountered in COVID-19, causing countless deaths. With current ineffective viral treatment along with a poor understanding of hypoxia, the devastation continues. COVID-19, a multifaceted disease, was initially considered a SARS (Severe Acute Respiratory Syndrome) “pneumonia” inducing ventilator use. However, up to 88.1% died on ventilators in New York [2]. An initial lower high altitude incidence may be due to extreme ultra-violet radiation [3] and other climatologic conditions. Additionally, high altitude physiological adaptation such as downregulated ACE2 receptor expression [4] and higher tolerance to hypoxia [5] may play a role.
In COVID-19, similarities to High-Altitude Pulmonary Edema (HAPE) were observed. Nevertheless, with adequate treatment, HAPE reverts within a few days, leaving no sequelae. Conversely, unlike pneumonia, CoV-2 induces rapid lung inflammation and alveolar-capillary destruction [6, 7] as described in a recently submitted paper: "COVID-19 simulating extreme high-altitude exposure with altered oxygen transport physiology, multiple diseases, and scarce need of ventilators: Andean Condor' s-eye-view".
We propose that alveolar-capillary destruction should be named pneumolysis (pneumo = lung; lysis = destruction), resulting in progressive hypoxemia, subsequent hypercapnia, and pulmonary shunts [8]. These lead to critical hypoxia, and if the patient survives, he can develop pulmonary fibrosis and sequelae. Furthermore, as hypoxia progresses, simulating a fast Mt. Everest ascent, it could trigger pulmonary hypertension and, consequently, HAPE-type edema in the remaining intact lung tissue, further aggravating the hypoxemia.
Pneumolysis should not be confused with “pneumonolysis”. Pneumonolysis was a term mostly used in the middle of the XXth century. It referred to the surgical separation of the parietal pleura and fascia of the chest wall (extrapleural pneumonolysis), or the separation of the visceral and parietal layers of the pleura (intrapleural pneumonolysis), in pulmonary tuberculosis [9].
Histopathology
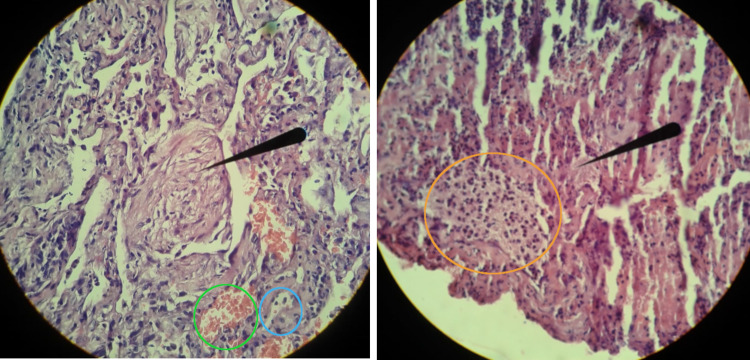
Lung biopsy histopathological findings of a patient suffering from severe COVID-19 are shown in the photomicrographs in Fig. 1. The patient was extubated before the biopsy. The microbial culture revealed Acinetobacter Baumannii, a Gram-negative bacillus that is aerobic, pleomorphic, and non-motile (opportunistic pathogen frequent among immunocompromised individuals). Three days later, his condition deteriorated, so he was intubated once more and passed away 14 days later. The pathological findings were: intra-alveolar Masson Body, which is a histomorphologic hallmark of organizing pneumonia. However, it is also associated with other conditions, such as the proliferative phase of diffuse alveolar damage, which seems to be the case in COVID-19. Pneumocytes nuclear atypia also described, in our criteria, could be due to the alterations resulting from CoV-2 entrance into pneumocytes for self-replication. The presence of RBCs in the alveoli shows the hemorrhage, possibly resulting from capillary stress failure due to pulmonary hypertension secondary to intense hypoxemia. Likewise, it could be due to the Pneumolysis itself, compromising the capillaries, producing capillary fragility. The severe lung pneumocyte damage and secondary superinfection are shown in Fig. 1. These microabscesses could explain the effectiveness of the use of Azithromycin and other antibiotics.
Fig. 1.
Left. Photomicrograph of a lung biopsy from a patient suffering from severe lung compromise (pneumolysis) in COVID-19. The black arrow shows the presence of a Masson Body inside an alveolus. In the green circle, alveoli are filled with red blood cells, possibly resulting from intra-alveolar hemorrhage. In the blue circle, the thickened interstitium resulting from fibrosis is shown. Right. Photomicrograph of a COVID-19 lung biopsy showing pneumolysis. The black arrow points to hyaline type membranes that can result from the fibrinous exudate and necrotic debris of cells. In the orange circle, a microabscess with pneumocystis can be appreciated. Nuclear atypia in the pneumocytes can also be observed. Photo and pathological analyses are courtesy of Dr. Felipe de Jesus Montelongo (Intensivist) and Dr. Manuel Gabriel Romo Sanchez (Pathologist) from the Hospital General de Ecatepec Las Americas, ISEM, México
Pathophysiology
The pneumolysis in incipient disease could give rise to Silent hypoxemia. Cov-2 incubation time takes longer (4–7 days) than other coronavirus or influenza virus. Initially, incipient hypoxia induces gradual pulmonary hypertension and alveolar recruitment. The oxygen dissociation curve fulfills the oxygen demand, with minimal increase in ventilation, adjusting PaCO2 levels (which is 20 times more diffusible than oxygen), maintaining a normal acid–base status. COVID-19 extreme hypoxia is similar to acute exposure to the summit of Mt. Everest, where the PaO2 = 24.6 mmHg [10]. As pneumolysis progresses, hyperventilation increases gradually, possibly reducing the PaCO2; however, once the lung becomes more severely compromised, ventilatory insufficiency gives rise to an increase of the PaCO2, acidosis, and along with a low hemoglobin count [7, 9,11], respiratory distress and "gasping" occurs. Possible ventilation, PaO2, PaCO2, and pH changes in pneumolysis can be divided into three theoretical pathophysiological stages: (1) Silent hypoxemia, (2) Gasping and (3) Death zone (Fig. 2). Superimposed edema, inflammatory, and immune reaction with pulmonary shunts in COVID-19 with a low hemoglobin count [9], can aggravate hypoxemia. Tolerance to hypoxia (depending on high hemoglobin and a low PaCO2) rapidly decreases, thereby ending life (Fig. 3) [5].
Fig. 2.
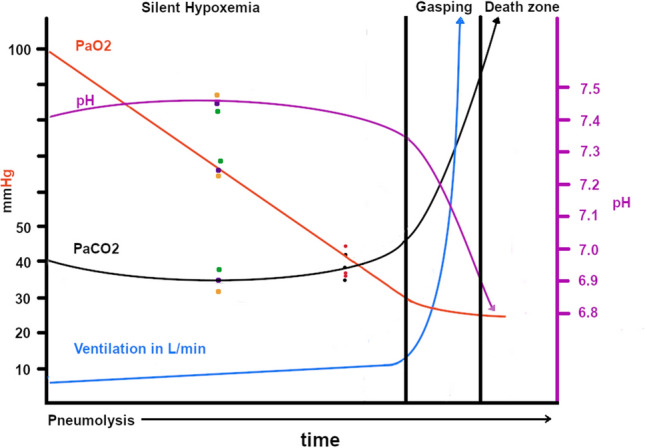
Progressive COVID-19 lung compromise and expected squematic diagram showing the three theoretical pathophysiological stages of pneumolysis: Silent hypoxemia, Gasping and Death zone. Pneumolysis and Acid–Base alterations lead to severe hypoxemia, hypercapnia, acidosis, and the loss of life. The three set of points on the left (orange, purple and green) were obtained from data at https://www.youtube.com/watch?v=_KMLW8eO0q0 by Dr. Shiv Kumar Singh. The 3 (red and black) points on the right were obtained from [12]
Fig. 3.
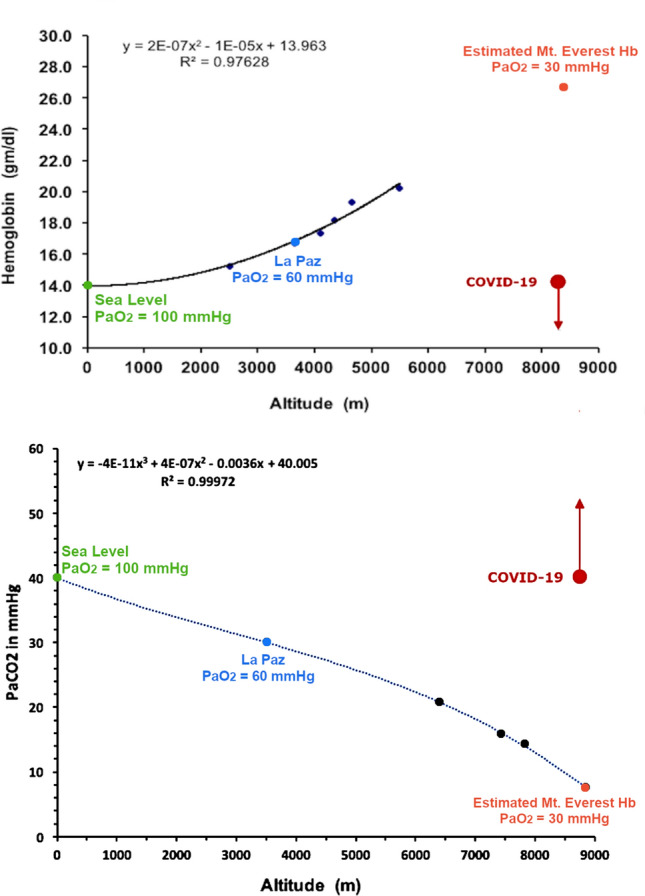
Tolerance to Hypoxia = (Hb/PaCO2) × 3.01. Shown here are the two variables and the probable COVID-19 behavior. A) Hemoglobin-Altitude, B) PaCO2-Altitude. Red arrows: acute hypoxia in COVID-19 pneumolysis, at sea level, simulating Mt. Everest extreme hypoxia, with hemoglobin and PaCO2 values progressing oppositely to expected optimal life-sustaining physiology under chronic hypoxic conditions
At high altitude, we live in permanent “Silent hypoxemia”. We ventilate slightly more than at sea level, but it is unnoticeable. Adequate acid–base balance is crucial [13]. La Paz (3100–4100 m), Bolivia, residents have perfectly healthy lives with tolerable hypobaric hypoxic levels: SpO2 = 90% (> 98% standard at sea level). This value is remarkably similar to SpO2 < 90% (even with FIO2 60%) in COVID-19 patients requiring ventilators at sea level. Likewise, when sea level travelers arrive at La Paz, their SpO2 drops to around 88–92% and around 25% of them can present mild Acute Mountain Sickness (AMS). Spontaneous resolution or adequate treatment resolves AMS in a couple of days. The other 75% are asymptomatic at rest with mild hyperventilation (almost unnoticeable) and some tachycardia, but can feel shortness of breath upon increasing physical activity or climbing stairs. This, until hemoglobin rises to the optimal level [14]. Patients living at high altitudes with SpO2 > 85%, are generally asymptomatic. Chronic low SpO2 at high altitude is compensated with a higher hematocrit as in Chronic Mountain Sickness (CMS), precisely referred to as poly-erythrocythemia (poly = many, erythrocyt = red blood cells, hemia = in the blood) [15]. Poly-erythrocythemic patients can sustain breath-holding far longer than normal hemoglobin count subjects [16]. They can even survive with a Mount Everest summit-like PaO2 = 35 mmHg [15]. The RBCs increase in poly-erythrocythemia is an adaptation process of lung, heart, and other underlying diseases to a chronic hypobaric hypoxic environment [15]. Despite increased blood viscosity, circulation time in these patients is not altered [17]. At sea level, post-COVID-19 patients with resulting lung fibrosis could also develop sea level poly-erythrocythemia (higher than normal hemoglobin values) [15] and reduced tolerance to exercise. At high-altitude, blood flow compensating mechanisms such as elevated erythropoietin production (potent vasodilator nitric-oxide stimulator) and perhaps angiogenesis [6], facilitate increased RBC transport. Endothelial compromise due to ACE2 binding by the virus could lead to platelet site aggregation resulting in thrombus formation. At 3500 m, normal hemoglobin count for men is 16 g/dl, and for women 14 g/dl. At sea-level, with progressive pneumolysis, normal hemoglobin count cannot supply sufficient oxygen to the tissues. Furthermore, mild anemia can be a significant disadvantage in a COVID-19 infection [11]. In these pandemic times, asymptomatic patients with low pulse oximetry values (< 90% at sea level and < 85% at 3,600 m) should be considered probable COVID-19. Pulse oximetry checks in public places should be mandatory.
Death rate tends to increase, following CoV-2 infection, in the presence of underlying conditions such as cancer, obesity, diabetes, old age, type-A blood, and others [18]. Antibiotic overuse with microbiome alterations could also be associated with a deficient immune system [19]. Chronic inflammation processes determine the permanent production of cytokines, interleukins, and other inflammatory molecules [20]. Likewise, "healthy" subjects suffering from asymptomatic underlying inflammation could have an over-reactive capacity to produce an abundance of inflammatory markers that add to the inflammation triggered by the virus. The so-called "cytokines storm" reaction could thus be explained (chronic inflammation + acute inflammation). Likewise, comorbidity in any disease implies worse outcomes. The inflammatory changes and immune dysregulation could give rise to irreversible damage [20]. Fast contagion of susceptible and immunosuppressed individuals could explain the epidemiological curve peak and subsequent fall, interpreted as nature’s cleansing.
COVID-19 lung CAT scans include a well delimited heterogeneous significant compromise simulating a "sheer curtain" image, rather than “ground glass”. This image suggests interstitial edema and localized inflammatory hemorrhagic processes [6] due to viral pneumolysis (Fig. 1). Many aspects of the evolution of these patients need to be further studied. A periodic follow-up of PaCO2 levels and/or ETCO2 could help give a clearer picture. It is also possible that once the PaCO2 starts rising, the speed of the rise could be of prognostic value. The SpO2 drop slope could also give a prognosis if followed carefully.
Treatment Proposal
We propose early administration of erythropoietin (EPO) 4000 IU, IV once or twice a week and/or blood transfusions depending on the severity. Hyperimmune plasma therapy should also be considered to be administered as whole blood, improving the hemoglobin levels and tolerance to hypoxia, provided there is a compatible blood typing. At high altitude, in the High Altitude Pulmonary and Pathology Institute (HAPPI-IPPA), for a couple of years, EPO has been used to improve the life quality of patients with pulmonary fibrosis or central ventilation alterations. Erythropoietin will not only stimulate RBC production but also help effective oxygen transport through nitric oxide stimulation, neuroprotection, and multiple-organ hypoxemia protective effects. These can be favorable in COVID-19 [21, 22]. Erythropoietin administration had positive results in one COVID-19 patient [23]. Thus raising the hemoglobin count strengthens the oxygen reservoir countering hypoxia.
At sea level, patients with a SpO2 < 95% (at 3500 m SpO2 < 85%), should immediately be placed on oxygen via nasal prongs, to avoid HAPE-type superimposed edema (superimposed pulmonary shunt), and rapid progression of hypoxemia. Waiting for diagnosis and treatment can lead to advanced pneumolysis. Adequate oral hydration is mandatory, as dehydration can result in additional clot formation. Prompt use of anti-inflammatory drugs such as acetylsalicylic-acid and corticosteroids, antibiotics due to superinfection, antitussive medication (promoting lung rest as bronchi are not compromised, nor is this a sputum productive pathology), and anticoagulants should also be considered.
Finally, we suggest a novel short-term strategy: "Earth open-circuit astronaut-resembling suits" with adequate outside air viral electric filtering re-breathing mechanisms to return to work and daily activities. This system could reduce contamination risk significantly. The increasing number of infections could be flattened without a quarantine. If built massively at lower prices, the economy could recover until immune supremacy takes over.
Acknowledgments
We acknowledge Dr. Giuseppe Miserocchi for some comments regarding COVID-19 evolution and the late Prof. Dr. Gustavo Zubieta-Castillo (Sr.), our mentor. We also thank Lucrecia DeUrioste and Rafaela Zubieta-DeUrioste for their collaboration and suggestions.
Funding
None
Compliance with Ethical Standard
Conflicts of interest
The authors declare that they have no Conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Gustavo R. Zubieta-Calleja and Natalia Zubieta-DeUrioste have contributed equally to this work.
References
- 1.Mitra P, Misra S, Sharma P. COVID-19 pandemic in India: what lies ahead. Indian J Clin Biochem. 2020;35(3):257–9. doi: 10.1007/s12291-020-00886-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with covid-19 in the New York City area. JAMA. 2020;323:2052–9. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zubieta-Calleja G. The advantages of ultraviolet radiation in controlling the coronavirus at high altitude [Internet]. 2020 [cited 2020 Jul 28]. Available from: https://altitudeclinic.com/blog/2020/04/u_v-radiation-covid-2-at-high-altitude/
- 4.Arias-Reyes C, Zubieta-DeUrioste N, Poma-Machicao L, Aliaga-Raduan F, Carvajal-Rodriguez F, Dutschmann M, et al. Does the pathogenesis of SARS-CoV-2 virus decrease at high-altitude? Respir Physiol Neurobiol. 2020;277:103443. doi: 10.1016/j.resp.2020.103443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zubieta-Calleja GR, Ardaya G, Zubieta N, Paulev PE, Z-CG. Tolerance to Hypoxia [Internet]. J Fisiol; 2013. p. 65–71. Available from: https://zuniv.net/pub/TolerancetoHypoxiaFiziol.pdf
- 6.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rockx B, Kuiken T, Herfst S, Bestebroer T, Lamers MM, Munnink BBO, et al. Comparative pathogenesis of COVID-19, MERS, and SARS in a nonhuman primate model. Science (80-) 2020;368:1012–5. doi: 10.1126/science.abb7314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zubieta-Calleja G, Zubieta-DeUrioste N, Venkatesh T, Das KK, Soliz J. COVID-19 and pneumolysis simulating extreme high-altitude exposure with altered oxygen transport physiology; multiple diseases, and scarce need of ventilators: andean condor's-eye-view. Rev. Recent Clin. Trials. 2020;15:1. doi: 10.2174/1574887115666200925141108. [DOI] [PubMed] [Google Scholar]
- 9.Braimbridge MV. The history of thoracoscopic surgery. Ann Thorac Surg. 1993;56(3):610–4. doi: 10.1016/0003-4975(93)90929-C. [DOI] [PubMed] [Google Scholar]
- 10.Grocott MPW, Martin DS, Levett DZH, McMorrow R, Windsor J, Montgomery HE. Arterial blood gases and oxygen content in climbers on Mount Everest. N Engl J Med. 2009;360:140–149. doi: 10.1056/NEJMoa0801581. [DOI] [PubMed] [Google Scholar]
- 11.Lippi G, Mattiuzzi C. Hemoglobin value may be decreased in patients with severe coronavirus disease 2019. Hematol. Transfus Cell Ther. 2020;42(2):116–117. doi: 10.1016/j.htct.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tobin MJ, Laghi F, Jubran A. Why COVID-19 silent hypoxemia is baffling to physicians. Am J Respir Crit Care Med. 2020;202:356–360. doi: 10.1164/rccm.202006-2157CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paulev PE, Zubieta-Calleja GR. Essentials in the diagnosis of acid-base disorders and their high altitude application. J Physiol Pharmacol. 2005;56:155–170. [PubMed] [Google Scholar]
- 14.Zubieta-Calleja GR, Paulev P, Zubieta-Calleja L, Zubieta-Castillo G. Altitude adaptation through hematocrit changes. J Physiol Pharmacol. 2007;58(5):811–8. [PubMed] [Google Scholar]
- 15.Zubieta-Castillo GR, Zubieta-Calleja GR, Zubieta-Calleja L. Chronic mountain sickness: the reaction of physical disorders to chronic hypoxia. J Physiol Pharmacol. 2006;57:431–442. [PubMed] [Google Scholar]
- 16.Zubieta-Castillo G, Zubieta-Calleja G, Zubieta-Calleja L. Pulse oximetry in chronic mountain sickness-long breath holding time and oscillation at lowest saturation. In: Ohno H, Kobayashi T, Masuyama S, Nakashima MI, editors. Prog Mt Med High Alt Physiol. Matsumoto: Press Committe of the 3rd World Congress on Mountain Medicine and High Altitude Physiology; 1998. [Google Scholar]
- 17.Zubieta-Calleja GR, Zubieta-Castillo G, Paulev PE, Zubieta-Calleja L. Non-invasive measurement of circulation time using pulse oximetry during breath holding in chronic hypoxia. J Physiol Pharmacol. 2005;56:251–256. [PubMed] [Google Scholar]
- 18.Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pandiyan P, Bhaskaran N, Zou M, Schneider E, Jayaraman S, Huehn J. Microbiome dependent regulation of Tregs and Th17 cells in mucosa. Front Immunol. 2019 doi: 10.3389/fimmu.2019.00426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lingeswaran M, Goyal T, Ghosh R, Suri S, Mitra P, Misra S, et al. Inflammation, immunity and immunogenetics in COVID-19: a narrative review. Indian J Clin Biochem. 2020;35(3):260–73. doi: 10.1007/s12291-020-00897-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ehrenreich H, Weissenborn K, Begemann M, Busch M, Vieta E, Miskowiak KW. Erythropoietin as candidate for supportive treatment of severe COVID-19. Mol Med. 2020;26:58. doi: 10.1186/s10020-020-00186-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soliz J, Schneider-Gasser EM, Arias-Reyes C, Aliaga-Raduan F, Poma-Machicao L, Zubieta-Calleja G, et al. Coping with hypoxemia: could erythropoietin (EPO) be an adjuvant treatment of COVID-19? Respir Physiol Neurobiol. 2020;279:103476. doi: 10.1016/j.resp.2020.103476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hadadi A, Mortezazadeh M, Kolahdouzan K, Alavian G. Does recombinant human Erythropoietin administration in critically ill COVID-19 patients have miraculous therapeutic effects? J Med Virol. 2020;92:915–918. doi: 10.1002/jmv.25839. [DOI] [PMC free article] [PubMed] [Google Scholar]