Abstract
Background:
National efforts to reduce maternal mortality with respect to community services have primarily focused on upgrading transportation infrastructure and formalizing training for care providers. There is, however, a paucity of baseline data on the profile and outcomes of pregnant women presenting to the Emergency Department (ED) in India.
Methods:
This retrospective study enrolled all pregnant women presenting to a large tertiary medical care center in India, between November 2016 and November 2017.
Results:
There were 696 ED visits by pregnant women during the study period. The mean age was 26.85 (SD: 4.88) years. Pregnant women in the first trimester contributed to 50.8% of all visits, and 54% being multigravida. The most common presenting complaints were bleeding/spotting per vaginum (PV) (38.2%) and abdominal pain (37.6%) followed by fever (21.6%) and vomiting (21.5%). Obstetric causes contributed to 53.2% of the ED visits, while nonobstetric causes amounted to 43.2%. Over a third (39.7%) required hospital admission. Of these patients, 73% delivered in CMC with live births amounting to 62.3% while 3.5% ended in fetal deaths. The miscarriages rate was as high as 28%. More than half (51.1%) of the deliveries were by normal vaginal delivery. There were no maternal deaths during the time of admission.
Conclusions:
Our study sheds new light on the profile of emergency visits among pregnant patients and their relationship to the outcome of pregnancy. First trimester visits were most common with complaints of bleeding PV and abdominal pain. This could explain the high rate of miscarriages among this population.
Keywords: Abortions, bleeding PV, nonobstetric emergency visit in pregnancy, pregnancy, pregnancy-related emergencies
Introduction
Pregnancy is an undoubtedly magical period in a woman's life with its unique set of joys and challenges. There is something quite remarkable about the process, the excitement mingling with fear, delight with discomfort, preparedness with the feeling that nothing you do is just quite enough. As peaceful as she may want it to be, it can be a stressful time too, filled with trepidation for the baby's health and her own. Every pregnant woman faces the risk of unforeseeable complications that can harm her or her unborn baby. These women represent a vulnerable section of our population, where early childbearing age, poor nutrition, limited access to healthcare, education, and sanitation pose threats to pregnant women. Therefore, health care system needs to be geared to combat complications and effectively prepare the mother for birth and requires widespread community support to do so. It becomes increasingly vital to characterize the spectrum of pregnancy-related emergencies to minimize maternal and infant mortality.[1,2,3]
Pregnant women presenting to the Emergency Department (ED) require thorough evaluation for early identification of life-threatening complications. Common obstetric issues seen in ED are hyperemesis gravidarum, abortions, eclampsia/preeclampsia, etc., Nonobstetric causes include urinary tract infections including pyelonephritis, lower respiratory tract infections, acute undifferentiated febrile illnesses, deep venous thrombosis, etc.[2,4] Majority of the emergencies in these women have been found to be symptoms suggestive of a miscarriage, some of which can be prevented if early and efficient treatment is instituted. Improved access to preventive care in India, particularly in rural areas, could be beneficial to countering high rates of maternal and child morbidity.[5,6] According to recent studies, India had an estimated institutional delivery of 78.9% in 2015-16 with a maternal mortality ratio of 174, and infant mortality rate of 44.[7] These numbers have improved due to the schemes and interventions implemented by the Indian government under various acts including the Reproductive and Child Health-2 program and Janani Suraksha Yojana where Community health workers (CHW) have been an integral part.[7,8] The Indian government has worked to fix this urban-rural gap by starting various initiatives to improve health outcomes in rural and remote areas, particularly through promoting the use of CHW.[2,6] In addition to educating health care professionals, what is a growing demand and urgent need is the dissemination of knowledge to pregnant women and their caretakers as well as the community as a whole. This builds self-reliance among people and promotes early recognition of issues that are otherwise either ignored or go unnoticed. Unfortunately, studies done on this subject show most pregnant women and their families either lack knowledge or lack concern regarding pregnancy-related complications. We need to strive to ensure a healthy, informed outlook among the community toward pregnancies and their challenges.
This study aims to understand the demographic and symptoms of the pregnant women who present to the ED. In addition, we have graded the severity of presentation and assessed the outcome of the visit as well the pregnancy. In doing so, we aim to better educate the emergency physicians, obstetricians, and community physicians regarding pregnancy-related emergencies, which can eventually help in developing a viable protocol for each primary health care centers, hospitals as well as the country.
Materials and Methods
Design
Our study was a retrospective study.
Setting
We conducted this study in the Emergency Department (ED) of Christian Medical College Hospital, Vellore, which is a tertiary medical care center. The ED is a 49-bed department and tends to attend about 300 patients per day including pregnant and non-pregnant patients.
Participants
All pregnant patients who presented to the ED from November 2016 to November 2017. Patients in active labor, however, present to the Labour Room which is a different department.
Inclusion criteria
All pregnant women presenting to the ED during the study period.
Exclusion criteria
Charts with missing data.
Variables
Data of the patients were obtained from the electronic hospital records and the details of history and physical examination findings of all patients were recorded on a standard data collection sheet. The following were extracted: Mean age of patients, gestational age at presentation, parity, comorbidities, presenting complaints, outcome of ED visit, and outcome of the pregnancy.
Outcome variable
The outcome of ED visit was categorized as hospital admission, discharge in a stable condition with advice, and leave against medical advice. The outcome of the pregnancy was assessed in terms of time of delivery, mode of delivery, and birth outcome.
Bias
This is a retrospective study, and therefore we could not control exposure or outcome assessment, and instead relied on others for accurate recordkeeping.
Sample size calculation
A pilot study done from August 2016 to November 2016 showed an average of 53 pregnant patients visiting the ED per month. The required sample size was calculated accordingly for 12 months as 636 patients.
Laboratory tests
Investigations such as complete blood count, serum electrolytes, urea/creatinine, B-HCG, and urinalyses were done as applicable, based on the initial history and clinical examination. This was followed by ultrasound scans for all patients to check for the viability of the pregnancy as well as fetal health.
Statistical analysis
All categorical variables were expressed as frequencies and percentages. The data was extracted from ED triage software and Clinical Workstation and entered in Statistical Package for Social Science (SPSS Inc, Released 2018) software, Version 25.0.0.0. Data was summarized using mean with standard deviation for continuous variables and frequencies with percentages.
Ethical considerations
This study was approved by the Institutional Review Board prior to the commencement of the study. Approval from the Institutional Review Board Ethical Committee was obtained (IRB Min no: 11353 dated 4th June 2018). Patient confidentiality was maintained using unique identifiers and by password-protected data entry software with restricted users.
Results
A total of 65,660 patients presented to ED during this study period of 1 year, of which 696 (1.06%) were pregnant women and hence included in the study. Among these, majority were triaged as priority 2, i.e., 474 (68.1%), while 26 (3.8%) were triaged as priority 1 [Figure 1].
Figure 1.
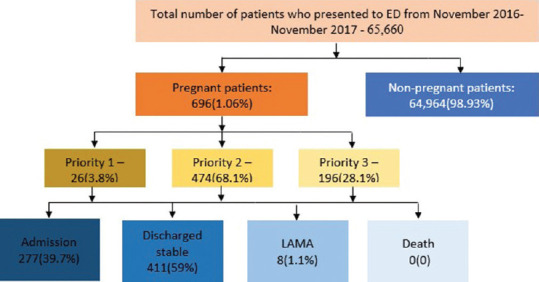
STROBE diagram
Demographics and baseline characteristics
The mean age of the patient at presentation was 26.85 (SD: 4.88) years. Gestational age of presentation is given in Figure 2. A higher number of multigravida patients, i.e., 376 (54%), presented to ED compared to 320 (46%) primigravida patients. In this geographical location, it was noted that a majority of the population had the previous comorbidity of hypothyroidism with 51 patients (7.3%), followed by asthma with 22 (3.1%), diabetes mellitus with 19 (2.7%), hypertension with 17 (2.4%), polycystic ovarian disease with 11 (1.6%), heart disease with 10 (1.4%), seizure disorder with 8 (1.1%), HIV positivity with 4 (0.6%), and psychiatric disorders with 3 (0.4%)
Figure 2.
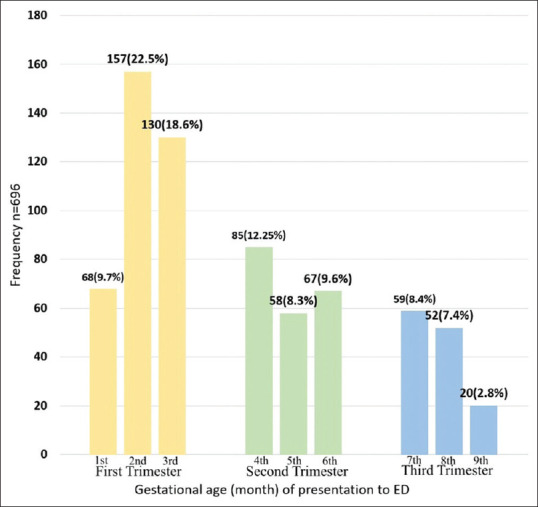
Gestational age and parity at presentation
Presenting complaints and probable diagnosis
The patients presented with a multitude of symptoms which including obstetric (66%) and nonobstetric (34%) causes. Among these, bleeding/spotting PV with 266 (38.2%) patients and abdominal pain with 262 (37.6%) were the most common. Other complaints included fever, vomiting, respiratory symptoms, malaise with body aches, loose stools, headache, urinary symptoms, giddiness, rashes with itching, retrosternal chest discomfort with dyspnea, nausea, trauma, and others such as seizures, lower limb swelling (DVT/pedal edema), blurring of vision, etc., [Table 1]. After initial history, examination, and targeted investigations, the details of probable diagnoses which were categorized into obstetric and nonobstetric causes are given in Table 2.
Table 1.
Presenting complaints
| Presenting complaints | Frequency n=696 (%) |
|---|---|
| Bleeding/spotting PV | 266 (38.2) |
| Abdominal pain | 262 (37.6) |
| Fever | 150 (21.5) |
| Vomiting | 150 (21.5) |
| Upper respiratory infection | 88 (12.6) |
| Malaise | 58 (8.3) |
| Loose stools | 51 (7.3) |
| Headache | 35 (5.0) |
| Urinary symptoms | 33 (4.7) |
| Rashes with itching | 18 (2.6) |
| Retrosternal chest discomfort | 17 (2.4) |
| NAusea | 15 (2.2) |
| Trauma | 13 (1.9) |
| Others (seizures, lower limb swelling, blurring of vision, etc.) | 58 (8.3) |
Table 2.
Diagnosis of obstetrics and nonobstetric causes in ED
| Obstetric Causes n-459 (65.9%) | |
| Threatened abortion | 117 (16.8%) |
| Hyperemesis Gravidarum | 88 (12.7%) |
| Incomplete abortion | 87 (12.6%) |
| Missed abortion | 58 (8.4%) |
| Physiological symptoms (nausea, pedal edema, dizziness, loose stools) | 57 (8.2%) |
| Ectopic pregnancy | 31 (4.3%) |
| Complete abortion | 21 (3%) |
| Nonobstetric Causes n-237 (34.1%) | |
| Respiratory tract infections | 71 (10%) |
| Acute undifferentiated febrile illness | 64 (9.2%) |
| Urinary tract infections | 67 (9.5%) |
| Acute gastroenteritis | 14 (2%) |
| Others (blurring vision, DVT, etc.) | 21 (3.3%) |
The patients were followed up to ascertain the outcome of their ED visit, and most of them, i.e., 411 (59%), were discharged in a stable condition with advice. Among the others, 277 (39.7%) required admission for further evaluation and management. A small proportion, i.e., eight patients, (1.1%) were advised admission but left against medical advice.
Outcome of the pregnancy and mode of delivery
Among all the pregnant patients who visited ED, 509 (73%) followed up in our hospital for delivery. Three variables were considered to judge the outcome of pregnancy i.e. time of delivery, mode of delivery, and the birth outcome as given in Figure 3. Among the deliveries conducted, i.e., 335 (ending in either live births or fetal deaths), more than half, i.e., 171 (51%), were by normal vaginal delivery, 107 (31.9%) by cesarean section, and 57 (17.1%) by instrumental delivery. Among the instrumental deliveries, forceps deliveries amounted to 38 (11.4%) while vacuum deliveries to 19 (5.7%). There were no maternal deaths during the time of admission.
Figure 3.
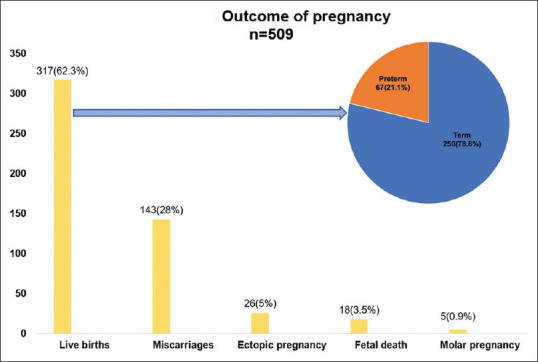
Outcome of pregnancy
Discussion
In our country, and in certain others around the world, cultural beliefs, lack of awareness and resources impede birth preparedness and the readiness to tackle complications. Issues are recognized late and more often than not, presentation to the hospital is typically delayed. Safe motherhood programs try to alleviate some of this burden of ignorance and encourage proper planning among families to prepare for birth and allocate resources for any complications that may arise.[2,4,6] Obstetric emergencies have exhaustive effects on the mother and fetus which can cause significant maternal and fetal/infant morbidity and mortality. Maternal mortality is a vital index of the quality and efficiency of obstetric services prevailing in a country. Women face a multitude of problems during pregnancy ranging from simple physiological symptoms to life-threatening complications. Globally, about 800 women die every day of preventable causes related to pregnancy and childbirth; 20% of these women are from India and remains a major public-health challenge. Annually, it is estimated that 44,000 women die due to preventable pregnancy-related causes in our country.[7,9,10,11] An extensive literature review has revealed that about 15% of all pregnant women in the first trimester develop a potentially life-threatening complication that calls for emergency care, and some will require a major obstetrical intervention to survive.[12,13,14] As seen in our study as well, majority of the pregnant women who presented to the ED as well as those who required intervention/care were found to be in the vulnerable first trimester. Symptoms suggestive of a threatened abortion such as bleeding/spotting PV and abdominal pain were the most common, reiterating the need for early and effective management to prevent fetal loss. Other studies have additionally demonstrated that mothers in the lower economic brackets have about a two and a half times higher mortality rate, primarily due to the inability to access affordable and reliable emergency health care.[2,13,15] However, in our study period and population, no maternal deaths were found, which could be due to a plethora of reasons. It could be argued that women from the lower socioeconomic classes would not have the capacity to present to our hospital, it being a private tertiary care center. Another reason could be the prompt and dependable treatment available to them in our ED, aided with the backbone of a multispecialty team of surgeons and obstetricians.
In our study population, majority of the patients were triaged as priority 2, and a third of them required hospital admission for either conservative or urgent surgical intervention. The patients who were discharged with medical advice, underwent an ultrasound scan during the ED visit and were further encouraged repeated follow-up visits in the OPD. This could explain the large proportion of women who opted to continue further ante-natal care in our hospital. Of these pregnancies, around two-thirds resulted in live births, with over half of those being at term. Miscarriages were also seen in a third of the population, which were later followed up in OPD for evaluation of preventable/treatable causes. Based on our results, we emphasize the role of regular prenatal and ante-natal check-ups including ultrasound scans and blood tests for the early detection of comorbidities, preexisting disease conditions, and pregnancy-related issues to ensure fetal and maternal well-being. Compared to other studies in this region, our study had the capacity to recruit more patients in a similar study period since our hospital has a large patient flow partly also due to our affiliations with multiple primary and secondary health centers in the region, where the limitations of resources or infrastructure encourage them to refer high-risk patients to us. Hence, it could be considered that our study population reflects reasonably well the profile of obstetric emergencies in south India.
Strengths of our study
This is one of the first studies of its kind done in an Emergency Department and especially in one with such a large patient population. It can be inferred then that the challenges faced in our study group are likely to be representative of those seen within the community as a whole. Hence, we believe this to be a valuable source of information that should guide not just hospital protocols but the education of a population in need.
Limitations
This is data from a single large tertiary care center which may have resulted in patient selection and an inherent referral pattern bias. Missing patient records and incomplete data were other limitations of this retrospective study.
Conclusions
Obstetric emergencies can develop as a result of complications that are not properly identified, monitored or managed, and are to a large extent, preventable. The purpose of this study was to understand the contributing factors of obstetric emergencies, their clinical presentation and maternal outcomes. From this data, it is our hope that hospitals in south India as well as the country develop a system where trained ED personnel, obstetricians, and surgeons with the help of clear guidelines in place will result in safer and more secure pregnancies for all women.
Research quality and ethics statement
The authors of this manuscript declare that this scientific work complies with reporting quality, formatting, and reproducibility guidelines set forth by the EQUATOR Network. The authors also attest that this clinical investigation was determined to require Institutional Review Board/Ethics Committee review, and the corresponding protocol/approval number is IRB Min no: 11353 dated 4th June 2018. We also certify that we have not plagiarized the contents in this submission and have done a plagiarism check.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
None declared.
References
- 1.Gabrysch S, Campbell OM. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9:34. doi: 10.1186/1471-2393-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rasheed P, Al-Sowielem LS. Health education needs for pregnancy: A study among women attending primary health centers. J Fam Community Med. 2003;10:31–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Filippi V, Goufodji S, Sismanidis C, Kanhonou L, Edward F, Ronsmans C, Alihonou E, Patel V. Effects of severe obstetric complications on women's health and infant mortality in Benin. Trop Med Int Health. 2010;15:733–42. doi: 10.1111/j.1365-3156.2010.02534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Islam M, Sultana N. Risk factors for pregnancy related complications among urban slum and non-slum women in Bangladesh. BMC Pregnancy Childbirth. 2019;19:235. doi: 10.1186/s12884-019-2392-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arpana A, M RB, V L. Maternal outcomes among emergency obstetric admissions at a tertiary care teaching hospital in Chitradurga, South India. Int J Reprod Contracept Obstet Gynecol. 2018;7:4906–11. [Google Scholar]
- 6.Gogoi M, Unisa S, Prusty RK. Utilization of maternal health care services and reproductive health complications in Assam, India. J Public Health. 2014;22:351–9. [Google Scholar]
- 7.International Institute for Population Sciences (IIPS) and Macro International. National Family Health survey (NFHS-3), 2005-06: India. I. Mumbai: IIPS; 2007. [Google Scholar]
- 8.Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: An overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health. 2014;35:399–421. doi: 10.1146/annurev-publhealth-032013-182354. [DOI] [PubMed] [Google Scholar]
- 9.EC/UNFPA, Making Pregnancy and Childbirth Safer [fact sheet] EC/UNFPA Initiative for Reproductive Health in Asia in cooperation with the German Foundation for World Population. 2000 [Google Scholar]
- 10.Ministry of Health and Family Welfare. Reproductive and Child Health –II programme. New Delhi: Government of India; 2015. [Google Scholar]
- 11.Mohapatra A, Gomare M. A critical appraisal of the maternal and child health scenario in a metropolitan city in India with reference to achievements of millennium development goals. J Family Med Prim Care. 2019;8:995–1001. doi: 10.4103/jfmpc.jfmpc_379_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goswami P, Bindal J, Chug N. To study pattern of obstetric cases referred at tertiary care centre in Central India. Int J Reprod Contracept Obstet Gynecol. 2017;6:2370–4. [Google Scholar]
- 13.Jakhar R, Choudhary A. Study of maternal outcome in referral obstetric cases in a tertiary care centre. J Fam Med Prim Care. 2019;8:2814–9. doi: 10.4103/jfmpc.jfmpc_402_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hashim TJ. Pregnancy experience, knowledge of pregnancy, childbirth and infant care and sources of information among obstetric patients at King Khalid Hospital, Riyadh. J R Soc Health. 1994;114:240–4. doi: 10.1177/146642409411400505. [DOI] [PubMed] [Google Scholar]
- 15.Gilmore B, McAuliffe E. Effectiveness of community health workers delivering preventive interventions for maternal and child health in low- and middle-income countries: a systematic review. BMC Public Health. 2013;13:847. doi: 10.1186/1471-2458-13-847. [DOI] [PMC free article] [PubMed] [Google Scholar]


