Abstract
Context:
Trauma is an immediate cause of patients flowing to the emergency department of any hospital. Besides epidemiology, clinical profile and treatment strategy forms an important aspect to reflect the gap in the existing public sector health-care system and the requirement.
Aims:
To evaluate the clinicoepidemiological profile of trauma patients admitting to an apex trauma hospital in east India.
Settings and Design:
A prospective observational study was performed during the time period of December 2018 to July 2019 on trauma patients admitted to the Trauma and Emergency department.
Methods and Material:
Patient's demographic profile, injury type, mechanism, the vehicle involved in the accident, and transportation were recorded. Various trauma scores (clinical) and outcome measures were recorded.
Statistical Analysis Used:
Statistical analysis was done by R version 3.6.1.
Results:
Male: female ratio was 407:93 with the 21–30 age group predominantly. 2–6 PM was the most common time of injury and ambulance was the predominant mode of transport (58%). Road traffic injury (RTI) accounted for 75% victims; two-wheelers (68%) dominated over others. Thirty percent (drivers 18%, pillion riders 12%) were wearing helmet; 41% were wearing seat belts (drivers 34%, passenger 12%). Twenty-five percent of drivers consumed alcohol. The median ± Interquartile range of injury severity score (ISS), revised trauma and trauma score and injury severity score were 17 (11–26), 7.8 (4.1–7.8), and 98.41 (95.95–99.30), respectively. Extremity injury (54% fractures) and head injury (50%) were the frontrunners in the pattern of injury, with half of the victims were polytrauma (ISS > 15).
Conclusions:
The injury was prominently RTI and the trauma victims/patients were young male drivers on two wheelers. The focus should be directed to make use of safety measures among the youth.
Keywords: Injury pattern, injury severity score, road traffic accidents, trauma
Introduction
Trauma is an immediate cause of patients flowing to the emergency department of any hospital. The consequence of modernization has led to a variety of unintentional injury that has become a global epidemic.[1] Every year around 5.8 million people of all age and economic groups die due to accidental injuries and violence that brings the data close to nine people every minute.[2] The nonfatal injury burden is even more significant, accounting for 18% of the world's health issues.[2] A report of the Ministry of Road, Transport, and Highways, Government of India (2017) has declared 4, 64, 910 road accidents leading to injuries of 4, 70, 975 in a single year in our country.[3] Odisha has on the record seen an upward trend in terms of the number of accident victims every passing year.[3] In a country of the diverse geographical, cultural, and developmental profile, there ought to be a difference in the pattern of trauma that presents to treating centers. Therefore, epidemiology of injury victims in northern India will be different from eastern India, and similarly, the urban population will have a different set of problems than an industrialized setup or rural community thereof.
Previous studies have tried to analyze the cause of death arising due to external causes and found that one-third of all is attributed to road traffic accidents (RTI).[1,4,5] Any untoward outcome has a lot of bearing on the sufferer as the first center may not be the treating center and patients being ferried from one place to another in search of proper management. We are a hugely populated country with overcrowded public domain hospital and an enormous deficit of an appropriate center of trauma.
There are some reports on epidemiological factors of patients having a footfall in some rural and urban-based level-1 tertiary centers in our country.[5,6,7,8,9,10] What is lacking in the studies is the clinical profile and treatment strategy of these patients. A mapping of these elements is fundamental to reflect the gap in the existing public sector health-care system and the requirement. The researchers, thus, aim to study varying epidemiological factors, and more importantly, the clinical silhouette and type of interventions rendered to the patients in a newly developing level-1 trauma center that carries the expectations of being an institute of national importance in the eastern region.
Material and Method
Study design
This prospective observational study was performed in our institution from December 2018 to July 2019 after approval from Institution Ethics Committee (IEC No: T/IM -NF /T&EM/ 17/31 dated 26/06/2018) and CTRI clearance CTRI/2018/12/016496 dated 26/06/2018.
Participants
The patient admitted to the trauma and emergency (T&E) department of AIIMS Bhubaneswar with more than 6 h of hospital stay were included in the study. Patients admitted after being referred from or have sought care from any other health care, those refused to give consent or not able to comprehend questions and not accompanied by caregivers who can provide full information were excluded from the study. We took patients admitted on alternate days for recruitment to our research, and systematic random sampling was used in which every third patient was included until the requisite sample size was attained. To reduce the willful manipulation, the participants were assured that the information provided by them would not be shared with anybody even to the police team and will be kept confidential. A detailed consent was taken from the caregiver/the attendant of the patients.
Data collection and variables
Information was collected using a prepared structured format, which included the following details: i) sociodemographic profile, ii) clinical profile, iii) injury grading and scoring. The demographic profile included items on age, sex, address, place of occurrence, type and mechanism of injury, the vehicle involved in the accident, brought by the vehicle, and time to reach the hospital were recorded. The primary and secondary survey was undertaken as per the Advanced Trauma Life Support (ATLS) guidelines. A clinical profile like vitals, airway, breathing, circulation, Glasgow coma scale (GCS), the reaction of the pupil to light was also evaluated. The injury was classified according to the anatomical area of injury like head injury (HI), maxillofacial injury (MF), chest injury, abdominal injury, extremity injury, and external injuries. A physiological score of the injury was calculated using GCS and revised trauma score (RTS). Anatomical injury score was calculated from abbreviated injury score (AIS) and injury severity score (ISS). A combination of both physiological and anatomical, i.e., trauma score and injury severity score (TRISS), was calculated and recorded. Outcome in terms of admission, emergency treatment, discharge, mortality, for referral was documented.
Statistical methods
Descriptive analysis was used for the clinical and epidemiological characteristics. Statistical analysis was done by R version 3.6.1. Categorical variables were expressed as a percentage. Numerical variables (nonparametric) are expressed as median with IQR. Bivariate analysis between categorical variables was done by the Chi-square test, and between categorical and numeric variables (nonparametric) was done using the Wilcoxon Rank-sum test in two groups and Kruskal–Wallis test in more than two groups. P < 0.05 regarded as statistically significant.
Results
Out of 1934 patients presenting to a casualty during the study period, 500 injury patients recruited from our center (alternate days as per protocol). We had had a majority of male (n = 407, 82%) and 18% female (n = 93). The age group 21–30 years were affected the most, and complete distribution is shown in Figure 1. The data analysis showed that the time of injury was afternoon (2–6 PM) in the majority, as shown in Figure 2. Ambulance (57%) was the most common mode of transport of victims to the hospital [Figure 3]. The mode of injury is shown in Table 1. RTI (75%) was the most common mechanism of injury, and among them, two-wheelers (68%) dominated over other modes of transportation used by victims during RTI. Among the two-wheelers, only about 18% of drivers and 12% of pillion riders were wearing a helmet. Forty-one percent were wearing seat belts (drivers 34%, passenger 12%) in four-wheelers and others. Helmet protection (drivers P value = 0.0009 and pillion riders P value = 0.0006) significantly reduced ISS as compared to nonhelmet wearers. Among four-wheelers, usage of seat belt significantly reduced ISS for copassengers (P-value = 0.0079) though the reduction was not statistically significant for drivers (P-value = 0.46). Twenty-five percent of drivers confessed to having used alcohol. The median ± IQR ± range of ISS, RTS, and TRISS was 17 (11–26) [4–75], 7.8 (4.1–7.8) [4.1–7.8], 98.41 (95.95–99.30) [36.60–99.92], respectively. Among the pattern of injury recorded, extremity injury (54% fractures) and head injury (50%) were the frontrunners, as shown in Table 1. Polytrauma (ISS > 15) was seen in 261 (52%) cases. The proportion of ISS among drivers and passengers not wearing safety gear is shown in Figure 4.
Figure 1.
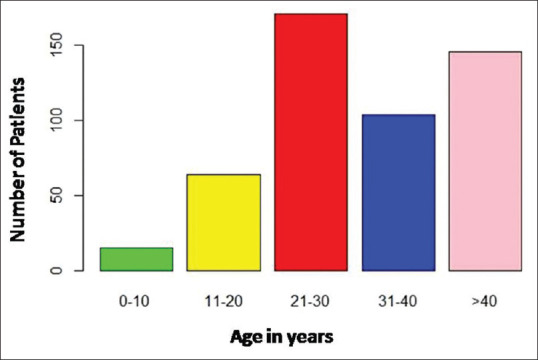
Bar diagram showing age distribution of the trauma patients
Figure 2.
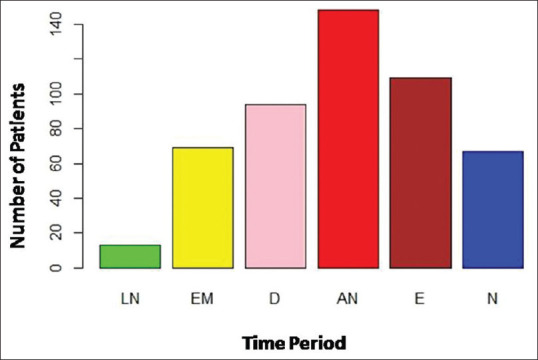
Bar diagram showing time of injury of the victims
Figure 3.
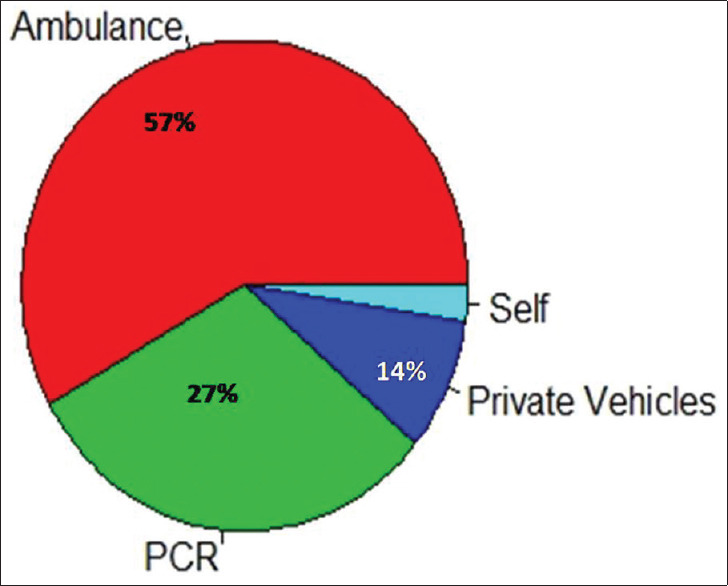
Pie diagram showing mode of transport of the injured patients
Table 1.
Clinicoepidemiology profile of trauma victims presenting to our center
| Variable | Class | frequency | Percentage | |
|---|---|---|---|---|
| Demographic Profile | ||||
| 1 | Age | 0-10 | 15 | 3.00 |
| 11-20 | 64 | 12.80 | ||
| 21-30 | 171 | 34.20 | ||
| 31-40 | 104 | 20.80 | ||
| >40 | 146 | 29.20 | ||
| 2 | Sex | Male | 407 | 81.40 |
| Female | 93 | 18.60 | ||
| 3 | Mode of Injury | Road traffic injuries | 371 | 74.20 |
| Fall from height/ Self-injury | 51 | 10.20 | ||
| Physical assault | 29 | 5.80 | ||
| Mass casualty incidents | 42 | 8.40 | ||
| Pvt vehicle | 15 | 3.00 | ||
| Self | 2 | 0.04 | ||
| Clinical Profile | ||||
| 4 | Type of Injury | Head injury | 254 | 50.80 |
| Maxillofacial injury | 138 | 27.60 | ||
| Blunt trauma chest | 71 | 14.20 | ||
| Blunt trauma abdomen | 39 | 7.80 | ||
| Extremity injury/fracture | 271 | 54.20 | ||
| External injury | 220 | 44.00 | ||
| 5 | Procedures | Suturing and dressing | 165 | 33.00 |
| Cast/Splint application | 191 | 38.00 | ||
| Rapid sequence intubation | 18 | 3.00 | ||
| Chest tube | 32 | 6.40 | ||
Figure 4.
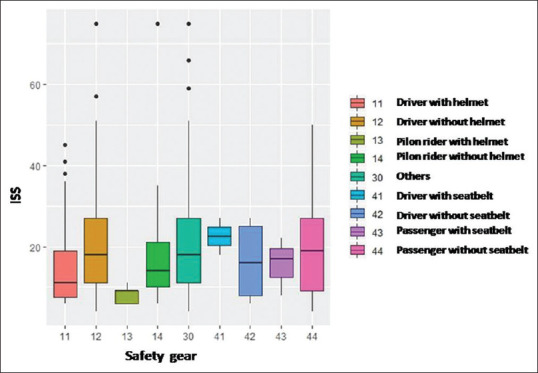
Box whisker plot demonstrating the ISS among the victims
The procedural details were the application of sutures in casting in 191 (38%), suturing and dressing 165 (33%), chest tube insertion in 32 (6.4%), and rapid sequence intubation in 18 (3%). Two hundred and fifty-four (52%) patients were discharged from T&E, 45 (9%) were referred, and 146 (29%) were admitted to the T&E ward, and 32 (6.4%) were admitted to ICU. There were five deaths (1%) in the T&E itself, and 6 (1%) patients left against medical advice.
Discussion
The present study is a data of the emergency department of a level-1 tertiary care trauma center in a newly established medical college of national importance in the eastern part India based in Bhubaneswar, the capital city of Odisha. The hospital became function from the year 2012 and presently there are 30 trauma beds and 515 indoor beds and a single functional trauma and emergency operation theater. There is a substantial deficit in terms of required and available logistics and personnel which inadvertently has a bearing on the management and outcomes of patient care. This is reflected in proportionate high referrals in our study as compared to other studies.[5,7,10] We also have a high footfall in our center considering the advantage that we are sole public medical college in the city and located strategically near to a national highway, surrounded by clusters of industrial estates in the neighboring regions, and most importantly the repute we have earned in our patient care over a short period. The trauma burden, hence, remains enormous as we see in our monthly statistics.
The prevalence rate of injury (PRI) in our study was 19.8%, which makes roughly one in every five admissions. The PRI has been lower as reported by some studies to be between 24% and 31% but is lacking in Indian studies.[11,12] RTI remains the leading cause followed by the causes of self-accidents. Apart from RTI, the nuisance of stray animals (n = 32, 6.4%) remains an important issue that needs to be addressed by the administration as an important preventable etiology. Self-inflicted injuries such as falls are common among the elderly. We also included two mass casualties (n = 35, 7.0%). One was the collision of the small bus with a van (n = 28 casualties) and in another incident one bus that fell over the bridge (n = 46 casualties, where seven survivors reported to our center).[13] Sharma et al. have reported fall followed by RTI as a common mode of unintentional injury.[14] This is their geographical location of survey which was done at hilly terrain.
We also noted that in injury victims, males are high compared with females similar to many studies.[8,9,15,16] Clearly, the men being outdoor are the reason for this gender polarization. The age group we found was highest in 21–30 years (31.4% participants). As depicted in our study, most studies report young adults (20–40) are more prone to injuries.[8,9,11,15,16,17,18] It is a matter of concern as they represent the most economically productive age group leading to damages in terms of loss of wages and productive work hours lost.
The majority of RTI happened between 2 and 6 PM (afternoon) in our study (28%). Kumar et al. have reported evening time as the commonest time, which they attributed to traffic congestion and low visibility as compounding factors.[9] This might be the case in our study, too, due to the congestion of the major roads during these hours due to end of office duty hours and allowance of movement of heavy vehicles. Another study by Misra et al. in the national capital has seen higher accident rates in the midnight to early morning slot where they blamed the nightlife culture of cosmopolitan cities.[10]
Victim's vehicle involved in the majority of cases was a motorized two-wheeler (53.4%). A motorcycle remains the most popular mode of transpiration in our belt in both rural and urban places. Awasthi et al. found that young (16–30 years) and male victims used two wheelers, whereas the older (31–40) or females used light motor vehicles in their series.[8] Pathak et al. pointed out a higher odds of the severity of ISS among the two-wheeler occupants.[6] We also found that helmet protection (drivers and pillion riders) significantly reduced ISS as compared to non-helmet wearers in some other studies.[6,7,10,15,19] But an interesting finding we noted that seat belt usage significantly reduced ISS for copassengers in four-wheelers as compared to those who did not wear. For drivers, the difference was not statistically significant. This may be due to quick reflexes response of drivers and at least the mandatory airbags for driver seat. Fitzharris et al. have also reported five-times higher head injury and prehospital deaths among riders not wearing safety gear.[20] Onyemaechi also reported traumatic brain injury (TBI) to be higher among nonhelmet users.[15] Alcohol consumption among riders is also associated with higher risks, as shown in our study and other studies.[21] Mitra et al. and Hadaye et al. have also reported drunkenness as an important distracter with higher odds ratio of injury.[17,22] Islam et al. also found that ignorance for traffic rules is an important factor RTI.[16] There is a need for behavioral changes among the users for better implementation of road traffic regulations. The implementation of new motor vehicle (amendment) act in 2019 by the Government of India has shown some promising results in the early months.[23] Hadaye et al. have reported speed of vehicle >60 km/h and usage of mobile phones as an important factor leading to RTI.[17] We believe there is a lot of concealment among the drivers to admit these; hence, we have ignored this factor.
The transportation to the trauma center in the hospital has been from the ambulance (57%), followed by PCR (29%). The government policy of making a 108-universal code for transportation is mainly responsible for timely and quick transportation. The other advantage was the closeness of the national highway to our center that is under constant police patrolling.
Fractures were the most common injuries in our study similar to Pathak et al. and Mitra et al.[6,22] Wui et al. and Kashid et al. have seen head injury as the most prevalent injury in their data,[24,25] while Onyemaechi and co-workers have reported soft tissue injury as highest among their victims.[11] The lower limb and more so the tibia and fibula remain the common bone universally to have broken and compounding due to its location and most common sites for primary impact.
We found higher ISS compared among the male victims. Polytrauma (ISS > 15) was seen in 52% of cases. Similarly, Onyemaechi has found ISS > 15 in 60% of cases though their mean ISS was 9.2 ± 2.9.[15] This is higher than Kashid et al. who have reported a mean ISS of 13.82 ± 6.2, in a multicentric study in tertiary trauma centers across the country.[24] We are constrained by a number of ICU beds and indoor and operation theater at present as the hospital is still in the building process. ISS has been reported to predict outcomes and mortality in trauma patients.[10,15] We also measured the TRISS score and RTS as they are essential components for triage. No other studies have recorded these values.
The death rate in our series was 1%. This is far less than other reported values in different studies. We have recorded only the early deaths (<24 h of admission) and not the late-onset deaths. Singh et al. have reported a death rate of 6.3% successful treatment in rest, 93.7% with no referral.[5] We have larger catering areas with more footfalls and in our T&E department as compared to theirs. TBI was the most common cause of death and reported similarly in other studies. Our study corroborates that ISS > 15 was associated with increased morbidity and mortality. Onyemaechi found potential risk factors for mortality: higher ISS scores, TBI, and open vehicle injuries.[15]
The strengths of the study are clinicoepidemological profile rather than the simple epidemiology as we were more focused on outcomes. We also measured the TRISS score and RTS as they are essential components for triage. To our knowledge, no other studies have recorded these values. The pattern and determinants of trauma victims were well captured in our survey as we collected first-hand information and followed up until the outcome as defined in our study. There are some limitations in the present study. We lack specific data like the speed of vehicles, conditions of the road, and use of mobile phones while driving that, which could have helped in interpreting the results. We also did establish alcohol blood levels but gathered information firsthand. Some factors might have been underestimated due to fear of medico-legal complications. The present trend predicts that the number of injuries especially the RTI will rise with the coming times, particularly in the developing countries.[2,3] In view of that, the government has come up with stringent new rules under the motor vehicle act 2019.[26] Future studies can be taken up to see the changes in trend after effective implementation of the regulations.
This study highlights the challenges of a budding trauma center. Though there are studies from different parts of the country, there is a need for a national trauma registry. Gopalakrishnan has also suggested the need of an RTI surveillance.[27] Recently Pal et al. also advocated for an Indian road crash registry.[28] Nevertheless, studies like this help in providing valuable inputs to the lawmakers for formulating guidelines.
Primary care and family physician can play a crucial role in creating public awareness and bring about behavioral changes in the public regarding the personal safety measures, following traffic rules that ultimately aim to reduce the incidence of RTI and the associated mortality and morbidity.
Conclusion
The injury was prominently RTI, and the victims were young male drivers on two-wheelers. More than 50% were polytrauma victims with skeletal injury dominating the regional pattern. Usage of safety gears like helmet reduced ISS among the drivers. Primary resuscitation with specialized trauma care reduced early mortality though some patients were referred for definitive care. Future studies can be directed to long-term outcomes and follow-up of injury victims to account exact mortality and morbidity due to such unfortunate events.
Declaration of ethical committee clearance
The approval obtained from the Institution Ethics Committee IEC No: T/IM -NF /T&EM/ 17/31 dated 26/06/2018.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Byun CS, Park IH, Oh JH, Bae KS, Lee KH, Lee E. Epidemiology of trauma patients and analysis of 268 mortality cases: Trends of a single center in Korea. Yonsei Med J. 2015;56:220–6. doi: 10.3349/ymj.2015.56.1.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global status report on road safety [Internet] 2018. Available from: https://wwwwhoint/violence_injury_prevention/road_safety_status/2018/en/
- 3.Annual Report 2018-19 [Internet] New Delhi: 2018. Available from: https://morth.nic.in/sites/default/files/other_files/Annual_Report_English_2018-19.pdf . [Google Scholar]
- 4.Fararoei M, Sadat SJ, Zoladl M. Epidemiology of trauma in patients admitted to an emergencyward in Yasuj. Trauma Mon. 2017;22:1–5. [Google Scholar]
- 5.Singh NP, Singh RC, Singh V, Jain PK, Gupta P, Singh A. Clinico-epidemiological profile of trauma victims in a tertiary care hospital in rural setting of central Uttar Pradesh. Indian J Community Heal. 2017;29:424–8. [Google Scholar]
- 6.Pathak SM, Jindal AK, Verma AK, Mahen A. An epidemiological study of road traffic accident cases admitted in a tertiary care hospital. Med J Armed Forces India. 2014;70:32–5. doi: 10.1016/j.mjafi.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chandrasekharan A, Nanavati AJ, Prabhakar S, Prabhakar S. Factors impacting mortality in the pre-hospital period after road traffic accidents in Urban India. Trauma Mon. 2016;21:e22456. doi: 10.5812/traumamon.22456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Awasthi B, Raina S, Verma L. Epidemiological determinants of road traffic accidents in a largely rural hilly population. J Sci Soc. 2019;46:79–85. [Google Scholar]
- 9.Kumar S, Mahima, Srivastava DK, Kharya P, Sachan N, Kiran K. Analysis of risk factors contributing to road traffic accidents in a tertiary care hospital. A hospital based cross-sectional study. Chin J Traumatol. 2020;23:159–62. doi: 10.1016/j.cjtee.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Misra P, Majumdar A, Misra M, Kant S, Gupta S, Gupta A. Epidemiological study of patients of road traffic injuries attending emergency department of a trauma center in New Delhi. Indian J Crit Care Med. 2017;21:678–83. doi: 10.4103/ijccm.IJCCM_197_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Onyemaechi NC, Nwankwo O, Ezeadawi R. Epidemiology of injuries seen in a nigerian tertiary hospital. Niger J Clin Pract. 2018;21:752–7. doi: 10.4103/njcp.njcp_263_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prekker ME, Miner JR, Rockswold EG, Biros MH. The prevalence of injury of any type in an urban emergency department population. J Trauma-Inj Infect Crit Care. 2009;66:1688–95. doi: 10.1097/TA.0b013e31817db0f1. [DOI] [PubMed] [Google Scholar]
- 13.Sharma B. Who is Responsible for the Cuttack Bus Accident OMMCOM News [Internet] 2018. Available from: https://wwwommcomnewscom/author/Bikash-Sharma .
- 14.Sharma D, Panta P, Amgai K. An epidemiological study of injuries in Karnali, Nepal. J Emerg Trauma Shock. 2020;13:30–4. doi: 10.4103/JETS.JETS_14_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Onyemaechi N. Road traffic injuries in a Nigerian referral trauma center: Characteristics, correlates, and outcomes. Int J Crit Illn Inj Sci. 2020;10:64–9. doi: 10.4103/IJCIIS.IJCIIS_18_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Islam M, Khan M, Hossain M, Mani K, Min R. Road traffic accidents in Bangladesh: Why people have poor knowledge and awareness about traffic rules? Int J Crit Illn Inj Sci. 2020;10:70–5. doi: 10.4103/IJCIIS.IJCIIS_65_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hadaye R, Rathod S, Shastri S. A cross-sectional study of epidemiological factors related to road traffic accidents in a metropolitan city Rujuta. J Fam Med Prim Care. 2020;9:168–72. doi: 10.4103/jfmpc.jfmpc_904_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh R, Singh HK, Gupta SC, Kumar Y. Pattern, severity and circumtances of injuries sustained in road traffic accidents: A tertiary care hospital-based study. Indian J Community Med. 2014;39:30–4. doi: 10.4103/0970-0218.126353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lilhare S, Swarnkar M. A study of injury characteristics in road traffic accidents by different road user category. Int Surg J. 2016;4:395. [Google Scholar]
- 20.Fitzharris M, Dandona R, Kumar GA, Dandona L. Crash characteristics and patterns of injury among hospitalized motorised two-wheeled vehicle users in urban India. BMC Public Health. 2009;9:11. doi: 10.1186/1471-2458-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang Y, Lu H, Qu W. Geographical detection of traffic accidents spatial stratified heterogeneity and influence factors. Int J Environ Res Public Health. 2020;17:572. doi: 10.3390/ijerph17020572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mitra S, Sarkar A, Saren A, Haldar D, Saha I, Sarkar G. Road traffic injuries: A study on severity and outcome among inpatients of a tertiary care level hospital of West Bengal, India. J Emerg Trauma Shock. 2018;11:247–52. doi: 10.4103/JETS.JETS_138_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sasmal PK, Mohanty CR, Jain M, Radhakrishnan RV, Sahoo S, Krishna VS, et al. The effect of 'THE MOTOR VEHICLES (AMENDMENT) ACT, 2019'on the clinico-epidemiological profile of road traffic accident patients presenting to a tertiary care trauma centre in Bhubaneswar. J Family Med Prim Care. 2020;9:3682–7. doi: 10.4103/jfmpc.jfmpc_293_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kashid M, Rai S, Nath S, Gupta T, Shaki O, Mahender P, et al. Epidemiology and outcome of trauma victims admitted in trauma centers of tertiary care hospitals – A multicentric study in India. Int J Crit Illn Inj Sci. 2020;10:9–15. doi: 10.4103/IJCIIS.IJCIIS_77_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wui LW, Shaun GE, Ramalingam G, Wai KMS. Epidemiology of trauma in an acute care hospital in Singapore. J Emerg Trauma Shock. 2014;7:174–9. doi: 10.4103/0974-2700.136860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Notification- Ministry of Road Transport and Highways. The Gazette of India [cited 2019 Aug 30] Available from: https://morthnicin/sites/default/files/notifications_document/SO%203147%28E%29%20dated%2030%20August%202019%20regarding%20implementation%20of%20 Section%201%20of%20the%20MV%20%28Amendment%29%20Act%2C%202019pdf .
- 27.Gopalakrishnan S. A public health perspective of road traffic accidents. J Family Med Prim Care. 2012;1:144–50. doi: 10.4103/2249-4863.104987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pal R, Ghosh A, Kumar R, Galwankar S, Paul SK, Pal S, et al. Public health crisis of road traffic accidents in India: Risk factor assessment and recommendations on prevention on the behalf of the Academy of Family Physicians of India. J Family Med Prim Care. 2019;8:775–83. doi: 10.4103/jfmpc.jfmpc_214_18. [DOI] [PMC free article] [PubMed] [Google Scholar]


