Abstract
Background:
Lockdown effectively can only result in relative freezing of populations that is expected to slow down the disease spread rather than zeroing it. Flattening of epidemic curve Current analysis was carried out to observe a pattern in the rise of CoVID-19 cases along with concurrent announcements of strategies to control the spread of disease.
Material and Methods:
Data in from of daily number of cases and issued notifications were studied from the official website of Government of India from 30/01/2020 to 03/05/2020. Qualitative assessment with thematic analysis was carried out for notifications issued by the government. The fit to data on cumulative cases was observed with R2 and checked for linearity, logarithmic, polynomial, and exponential growth. Daily growth fraction (Gt) was calculated based on the difference between current and previous number of cases, thereafter daily doubling time (Td(t)) was estimated.
Results:
Daily reported cases were entered and cumulative growth of cases observed with a polynomial increasing pattern (third-order) with better fit (R2: 0.999). Total 108 notifications were issued, and as compared to phase-0 and 1 (87.0%), few (12.9%) notifications were issued in phase-2 of study period. As compared to phase-0 and 1, rising trend of cumulative cases and Td(t) was high in phase-2.
Conclusion:
Across phases of lockdown along with a rising trend of COVID-19 cases, the country has managed to increase the doubling time of cases with an effort to flatten the epidemic curve.
Keywords: COVID-19, daily doubling time, lockdown
Introduction
The global spread of novel coronavirus (COVID-19) from China has resulted in widespread morbidity and relatively high mortality in some of the countries like Italy, Spain, Iran, and the United States of America. China was affected severely where it was reported to have been originated on 08/12/2019. COVID-19 was declared international health emergency by the World Health Organization (WHO) on 30/01/2020.[1,2] Most of the operated containment measures across the globe were lockdown of the population in their geography, advice to wear facemasks and regular maintenance of hand hygiene by washing. It addressed to reduce disease transmission coefficient by lowering an effective contact rate and the probability of transmission per contact.[3,4]
Decision of the nationwide lockdown comes with a potential to pay social and economic price for COVID-19 epidemic in a country. Putting entire population in quarantine has been unfathomable in past, but now is common advocated strategy. Eventually, COVID-19 epidemic expects significantly low participation in economic activities resulted due to pandemic fear and worries.[5] On the other hand, imposing lockdown by the governments assumed to bear significant economic loss for reduced disease transmission. In early period of lockdown, inherit hopes among people were zeroing the spread of disease by freezing of suspected and infected individuals. However, lockdown effectively can only result and resulted in relative freezing of populations with an expectation to slow down disease spread rather than zeroing it; flattening of epidemic curve. Low upsurge of infectives does not cause acute straining of health resources especially in developing countries which gives time for effective management of cases and results reduced mortality.[6,7] Crosscutting joint strategic efforts among scientists and academicians resulted in rapidly evolving preventive, diagnostic, and therapeutic trials to control the epidemic, whereas, program managers, non-governmental/community-based organizations, police/military personals, etc., worked tirelessly to effectively implement lockdown and helping people to stay back at their homes.[8]
Depiction of knowledge from demand and supply curve suggests that the efforts to reduce supply of cases to health system give effective time to prepare for essentials to manage the disease by fulfilling demands of health system related to logistics. Introduction of COVID-19 into an entirely suspectable population expects to spread at a faster rate in absence of aggressive nationwide intervention.[9,10] Since tertiary hospitals are busy in managing severe cases, role of primary health physicians becomes important not only to manage current pandemic but also ensuring management of diseases of national priority. Capacitating health system by arranging logistics and training workforce in health care especially primary physicians requires a trade-off, a parsimonious decision for degree and duration of lockdown. Large part of India, lives in areas largely dependent on primary care delivery system therefore require time to manage high rate of depletion and poor rate of accumulation of resources. Current analysis was carried out to observe a pattern in the rise of COVID-19 cases along with concurrent announcements of population level strategies to control the spread of disease.
Methods
Data in the from of daily number of cases and issued notifications were studied from the official website of Ministry of Health and Family Welfare, Government of India from 30/01/2020 to 03/05/2020 (68 days). Qualitative assessment with thematic analysis was carried out for notifications issued by the union government. Domains and categories of notifications were finalized beforehand through discussions among experts of public health and social scientists. Independently, two public health professional studied notifications and distributed into various domains first and later on specific categories. In a case of failed concordance for classified domains and categories of notifications, it was resolved by an independent expert.
Daily reported number of cases were entered in Microsoft excel 2003-07 version and pattern of growth for cumulative number of cases were observed. In addition, trend for fraction of recovered and died cases was also observed. The fit to data for cumulative number of cases was observed with R2 and checked for linear, logarithmic, polynomial, and exponential growth. Daily growth fraction (Gt) was calculated based on the difference between current and previous number of cases (Current-Previous/Previous), thereafter daily doubling time (Td(t)) was estimated using formula (Log(2)/Log (1+ Gt) and its trend was assessed with R2 for data fitting. Growth of cases was compared against three time periods as; Phase-0 (before lockdown) from 30/01/2020 to 24/03/2020; Phase-1 (lockdown) from 25/03/2020 to 14/04/2020 and Phase-2 (lockdown extended) from 15/04/2020 to 03/05/2020. Rise in cases in each phase was looked for data fitting (R2) and Td(t). Data used for analysis was secondary in nature, which was taken from public domain and did not involve patients. Therefore, ethical approval was not sought from institute ethics committee. Since data from public domain was used for analysis without discrete details of patients, ethical considerations were not apprehended, and no ethical clearance was sought for analysis of current study.
Results
Daily reported cases were entered and cumulative growth of cases observed with a polynomial increasing pattern (third-order) with better fit (R2: 0.999) [Figure 1]. Daily growth fraction (Gt) derived daily doubling time of cases (Td(t)) was also observed for trend, where data seems to be poorly fit for linear (R2:0.138), logarithmic (R2: 0.085), and polynomial (R2: 0.278) growth pattern [Figure 2]. After omission of outliers, for day 8 and 9, Td(t) trend observed to be a polynomial in nature with relatively better fit (R2: 0.733) as compared to linear (R2: 0.466) and logarithmic (R2: 0.312), therefore moving average (for last 2 periods) trend was assumed for Td(t). Fitting of data was assessed separately for phases of nationwide lockdown, wherein power trend in phase-0 (R2:0.966), but polynomial trend in phase-1 (R2:0.999), and 2 (R2:0.999) was observed [Figure 3]. Phasic trend for Td(t) observed with moving average trend for all three phases as a linear, logarithmic, polynomial, and exponential trend was observed with poor fit (R2< 0.401) [Figure 4]. Trend in each phase of lockdown for recovered and died fraction was observed to be moving average (second order) in nature wherein phase-0 has erratic but phase-1 and 2 have more stable trend [Figures 5 and 6].
Figure 1.
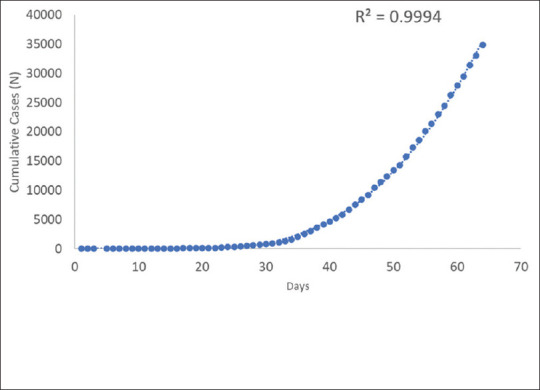
Fitting of curve for cumulative cases of COVID-19 from 30/01/2020 to 03/05/2020 in India.
Figure 2.
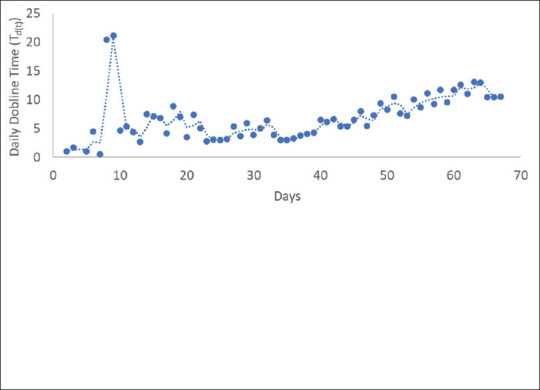
Moving average curve for daily doubling time (Td(t)) increasing number of COVID-19 cases from 30/01/2020 to 03/05/2020 in India
Figure 3.
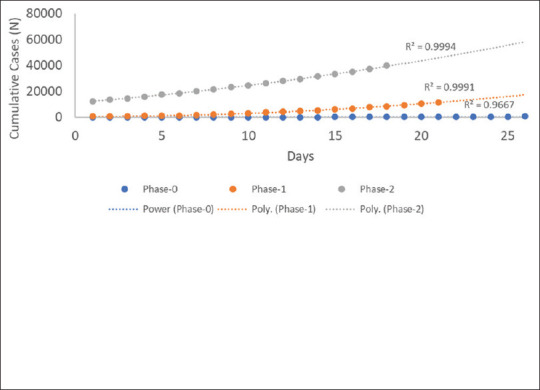
Fitting of curve for cumulative cases of COVID-19 in three phases of nationwide lockdown from 30/01/2020 to 03/05/2020 in India
Figure 4.
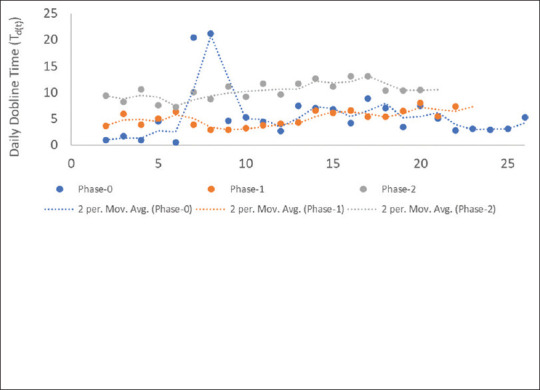
Moving average curve for daily doubling time (Td(t)) for increasing number of COVID-19 cases across three phases of nationwide lockdown from 30/01/2020 to 03/05/2020 in India
Figure 5.
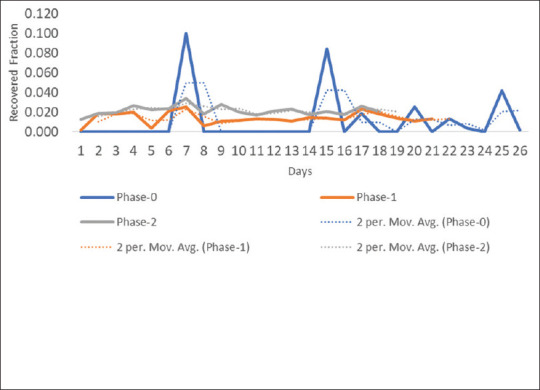
Fitting of curve for fraction of recovered cases of COVID-19 in three phases of nationwide lockdown from 30/01/2020 to 03/05/2020 in India
Figure 6.
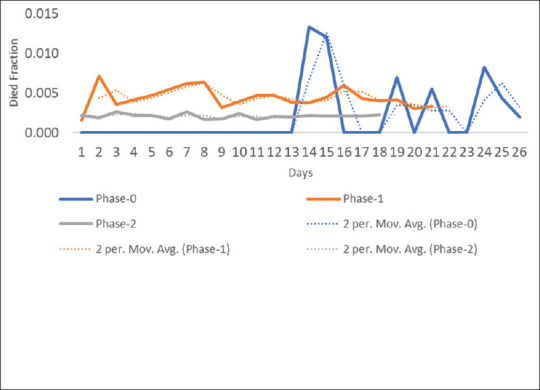
Fitting of curve for fraction of died cases of COVID-19 in three phases of nationwide lockdown from 30/01/2020 to 03/05/2020 in India
Total 108 notifications were issued from 30/01/2020 to 03/05/2020, and as compared to phase-0 and 1 (87.0%), few (12.9%) notifications were issued in phase-2. Of which 43 (39.8%) were targeted for public and 38 (35.2%) for health care professionals like doctors, nurses, pharmacists, etc., of government and private hospitals. Government issued 20 (18.5%) notifications as an advisory to state governments/union territories (UTs). Overall, that is in phase-0, most (seventeen) of notifications were issued related to travel advisories to people. In phase-0 notifications related to prohibition and/or avoidance of mass gathering,[5] guidance document to state governments/UTs,[4] and general CoVID-19 awareness for public.[3] Whereas, in phase-1 notifications related to social support,[8] human resource in health sector,[6] management[6] and testing[4] were issued [Figure 7].
Figure 7.
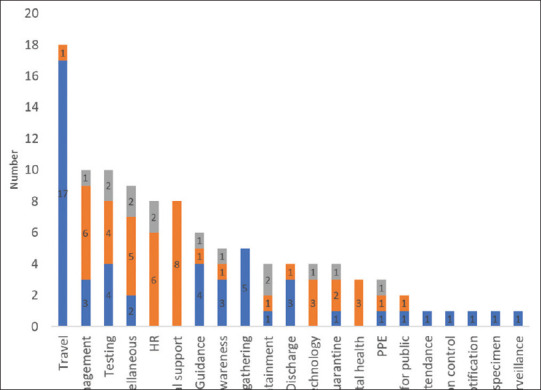
Categories of notifications issued by Government of India related to COVID-19 in three phases of lockdown from 30/01/2020 to 03/05/2020 in India
Discussion
Current analysis observed with a rising trend, polynomial in nature for India with Td(t) of moving average pattern. As compared to phase-0 and 1, rising trend of cumulative cases and Td(t) was high in phase-2. It indicates that across phases of lockdown along with a rising trend of COVID-19 cases country has managed to increase the doubling time of cases with an effort to flatten the epidemic curve. In phase-2, fraction of recovered patients was high and low for died patients as compared to phase-0 and 1. Overall, data suggest that efforts done by the country so far able to succeed to control the COVID-19 epidemic. Ground efforts were assumed in light of notifications issued by the government, where about 90.0% were issued in phase-0 and 1 of nationwide lockdown. The focus of efforts was to avoid effective contact rate among people to flatten the curve in parlay for building capacity of health care delivery system to manage epidemic.
Lockdown and adherence to “Social distancing” measures in locked habitats have ensured avoidance of people conglomeration.[11] It ensures reduction in effective contacts per person which plays a significant role in reducing instantaneous transmission coefficient (β) and reproduction (R0) rate.[12,13] It plays an important role in bringing down the force of infection (λ) over a period of time in community, which allows preparing responses towards disease. Apart from cordoning off the entire population from day-to-day activities, India responded as formulation of data-driven guidelines for diagnosis of presumptive COVID-19 cases and ensuring safety of health care professionals. India also ordered 15 million personal protective kits (PPEs) including gowns, masks, goggles, gloves, etc., along with 1.5 million rapid testing kits. The government informed that India received 170,000 PPEs in donation from China and as on 6 April 2020 India had 387,473 PPEs.[14]
India being a second-most populous country, exists with major challenges like large number of overcrowded settings, poor hygiene, and sanitation that pose threat not only in terms of rapid spread but also with high rate of mortality. Besides, prevalent tuberculosis and chronic respiratory diseases along with type-2 diabetes mellitus and hypertension are potential drivers in COVID-19 morbidity and mortality.[15] Although metropolitan cities with high population density observed with COVID-19 epicenters largely resulted due to immediate footfall from international community, now rural communities are at risk due to huge migration from metropolitan cities.[16] Epidemiological transition requires primary care needs to be prepared not only for effective measures but also for social distancing along with social support mechanisms to tackle disease spread.[17] Health facilities, especially in the primary health care delivery system, now need to be capacitated for screening and management of COVID-19 cases from rural area. Redistribution of efforts required to capacitate primary care physicians for early diagnosis and alleviation of fear in community. It will help to reduce if not, control the escalating demand for hospital services.[18,19]
Engagement of primary care physicians is required to play a significant role in providing social support to vulnerable population during this epidemic. Since COVID-19 pandemic has been testing the capacity of the tertiary facilities, primary care physicians play a crucial role to ensure effective provision of necessary health care services under various other ailments like HIV/AIDS, tuberculosis, diabetes mellitus, etc., They also strengthen the home base management of illness whose accessibility of health services have been disrupted during COVID-19 situation.[20] In addition, primary care can enhance the surveillance such as influenza like illness (ILI) and severe acute respiratory infection (SARI). They a have pivotal role in risk communication and community engagement for better self-preparedness of communities.[21]
In the end, current analysis showed slowing down of curve during lockdown with an effective time to capacitate primary health care delivery system along with tertiary centers. Primary care physicians have crucial role to play to manage COVID-19 in community-based settings and ensuring regular supply of essential primary care services. Conclusively, lockdown showed its initial effect in reducing the rise of epidemic curve of COVID-19 cases across its phases as appearance of new cases were imminent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hu Y, Sun J, Dai Z, Deng H, Li X, Huang Q, et al. Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol. 2020;127:104371. doi: 10.1016/j.jcv.2020.104371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kickbusch I, Leung G. Response to the emerging novel coronavirus outbreak. BMJ. 2020;368:m406. doi: 10.1136/bmj.m406. [DOI] [PubMed] [Google Scholar]
- 3.Suess T, Remschmidt C, Schink SB, Deng H, Li X, Huang Q, et al. The role of facemasks and hand hygiene in the prevention of influenza transmission in households: Results from a cluster randomised trial; Berlin, Germany, 2009-2011. BMC Infect Dis. 2012;12:26. doi: 10.1186/1471-2334-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCallum H, Fenton A, Hudson PJ, Lee B, Levick B, Norman R, et al. Breaking beta: Deconstructing the parasite transmission function. Philos Trans R Soc Lond B Biol Sci. 2017;372:20160084. doi: 10.1098/rstb.2016.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: Development and initial validation. Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kenyon C. Flattening-the-curve associated with reduced COVID-19 case fatality rates-an ecological analysis of 65 countries. J Infect. 2020;81:e98–9. doi: 10.1016/j.jinf.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matrajt L, Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis. 2020:26. doi: 10.3201/eid2608.201093. doi: 103201/eid2608201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. Features, Evaluation and Treatment Coronavirus (COVID-19) [PubMed] [Google Scholar]
- 9.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlos WG, Dela Cruz CS, Cao B, Pasnick S, Jamil S. Novel Wuhan (2019-nCoV) Coronavirus. Am J Respir Crit Care Med. 2020;201:7–8. doi: 10.1164/rccm.2014P7. [DOI] [PubMed] [Google Scholar]
- 11.Paital B, Das K, Parida SK. Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci Total Environ. 2020;728:138914. doi: 10.1016/j.scitotenv.2020.138914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akiyama MJ, Spaulding AC, Rich JD. Flattening the curve for incarcerated populations-Covid-19 in jails and prisons. N Engl J Med. 2020;382:2075–7. doi: 10.1056/NEJMp2005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kirkeby C, Halasa T, Gussmann M, Toft N, Græsbøll K. Methods for estimating disease transmission rates: Evaluating the precision of Poisson regression and two novel methods. Sci Rep. 2017;7:9496. doi: 10.1038/s41598-017-09209-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krishnan A. Coronavirus: India to get 15 million PPE kits from China. The Hindu. 2020. Apr 14, [Last accessed on 2020 May 8]. Available from: https://wwwthehinducom/news/national/coronavirus-india-to-get-15-million-ppe-kits-from-china/article31336317ece .
- 15.India State-Level Disease Burden Initiative Collaborators. Nations within a nation: Variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet. 2017;390:2437–60. doi: 10.1016/S0140-6736(17)32804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pandey G. Coronavirus in India: Migrants running away from quarantine. BBC News. 2020. Apr 15, [Last accessed on 2020 May 8]. Available from: https://wwwbbccom/news/world-asia-india-52276606 .
- 17.Kumar R, Kumar D, Jagnoor J, Aggarwal AK, Lakshmi PV. Epidemiological transition in a rural community of northern India: 18-year mortality surveillance using verbal autopsy. J Epidemiol Community Health. 2012;66:890–3. doi: 10.1136/jech-2011-200336. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Regional Office for the Western Pacific Role of Primary Care in the COVID-19 Response. Manila: WHO Regional Office for the Western Pacific; 2020. Available from: https://appswhoint/iris/handle/10665/331921 . [Google Scholar]
- 19.Casella G, Ingravalle F, Ingravalle A, Monti C, Bonetti F, Limonta A. COVID Emergency: An Opportunity to Increase the Interaction between Hepatologist and Primary Care. Physician Minerva Gastroenterol Dietol. 2020 doi: 10.23736/S1121-421X.20.02713-0. doi: 1023736/S1121-421X2002713-0. [DOI] [PubMed] [Google Scholar]
- 20.Barrett CL. Primary healthcare practitioners and patient blood management in Africa in the time of coronavirus disease 2019: Safeguarding the blood supply. Afr J Prim Health Care Fam Med. 2020;12:e1–3. doi: 10.4102/phcfm.v12i1.2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Sutter A, Llor C, Maier M, Mallen C, Tatsioni A, van Weert H, et al. Family medicine in times of ‘COVID-19’: A generalists’ voice. Eur J Gen Pract. 2020;26:58–60. doi: 10.1080/13814788.2020.1757312. [DOI] [PMC free article] [PubMed] [Google Scholar]


