Abstract
Urinary bladder is an adjacent viscus susceptible for intraoperative injury during cesarean section (CS). Prolonged labor, scarred uterus, intraabdominal adhesion, emergency CS, advanced labor, cesarean hysterectomy etc., are the predisposing factors for bladder injury during CS. While operating on such conditions, one should be meticulous to explore the possibility of bladder injury. Family physician practicing community obstetrics should be aware of this and know how to tackle this. Usually the dome of the bladder is injured and the trigonal area remains away from the injury field by 6–10 cm. Bladder rent is repaired in two layers either by continuous simple or interrupted suture with 3-0 & 2-0 polyglycolic acid suture. Suprapubic cystostomy and transurethral catheter are kept for 10–14 days. While postoperative adhesion, CS during full dilatation of cervix, abnormal anatomy etc., may not proceed for negligence, bladder injury in normal patients and unrecognized intraoperative bladder injury may attract penalty from the consumer court.
Keywords: Cesarean section, injury, layer repair, medico-legal, urinary bladder
Introduction
Urinary bladder being the nearest anterior organ to the uterus, its injury during cesarean section (CS) is not so rare. Bladder injury during primary CS is about 0.2% and during repeat CS is about 0.6%.[1] So, primary care physicians, who are dealing with the obstetrics, should be conversant about dealing with such cases as cesarean delivery are currently within the scope of Family Physician. The American Academy of Family Physicians (AAFP)/American College of Obstetricians and Gynecologists (ACOG) jointly stated that surgical delivery is within the scope of family medicine.[2] AAFP's resident training incorporated the core obstetric skill & advanced obstetric skill that include CS.[3] AAFP's fellowship training is designed to make a family physician perform CS independently.[4]
Due to the wider application of cesarean section, nowadays the incidence of morbid adherent placenta in subsequent pregnancies is increasing. Morbid adherent placenta (accreta, increta, and percreta) are associated with more number of bladder involvement during pregnancy and hence more number of bladder injury (Total urinary tract injury 21.7%, bladder 11.7%, ureter 4.7%, and bladder with ureter 5.3%).[5] Apart from this, other conditions which an obstetrician should remember while doing cesarean section so as to avoid bladder injury are
Prolonged labor with bladder distension
Pregnancy with scarred uterus, e.g., myomectomy, metroplasty, repaired uterine perforation (septic abortion) etc.
Suspected intra-abdominal adhesions, e.g., postoperative (nonuterine) pregnancy, chronic pelvic inflammatory disease, malignancy, irradiation etc.
Distorted local anatomy – cervical/lower segment fibroid, urogenital system anomaly, obstructed labor (though the incidence is less nowadays due to wider application of partograph) etc.
Cesarean done for an advanced labor woman, station ≥ +1 (due to well taken-up of cervix uterine incision may fall over anterior vaginal wall leading to difficult dissection of bladder from the field)[6]
Cesarean hysterectomy
Cesarean hysterectomy causes about 1–4% of bladder injury.[7] Increasing number of previous CS increases the chance of bladder injury.[8] Woman with >3 post CS are 5 times more prone to have bladder injury than the woman who is 1 post CS.[9] Emergency CS has more chance of bladder injury compared to elective CS (31% vs 11%). CS in laboring women also carries more risk of bladder injury compared to nonlaboring women (83% vs 61%).[10]
Prevention of bladder injury
Whenever dense adhesion is anticipated, sharp dissection of the bladder is advocated instead of blunt dissection by gauze piece.[7] Bladder used to be made full during cord prolapse management as this will elevate the presenting part and hence cord compression will get relieved. While doing CS for this kind of patient, the bladder should be made empty before incising. In suspected intraabdominal adhesion cases, entering of peritoneum preferably by blunt dissection or in case of sharp dissection, the surgeon should check twice that there are no visceral structures within the vicinity of the peritoneal incision. For diagnosing the intra-abdominal adhesion, sliding sign in ultrasound can be used. In the absence of adhesion, during deep breathing the uterus will slide below the parietal fascia of the abdomen whereas in case of severe adhesion, this sliding is absent.[11] In morbidly adherent placenta cases, filling-up of the bladder with 200 ml normal saline prior to CS would reduce the bladder injury.[12,13]
Diagnosis of bladder injury
While operating the abovementioned patients, it would be prudent to look for any injuries during and at the end of the operation. Usually, urine dribbles out in the operative field. If no leaking of urine but there is a doubt about injury, then the color of urine should be observed. Hematuria might occur in 95% cases.[14] Foley's bulb may become visible in the operative field. If there is a doubt of injury, it can be confirmed by instillation of dye (methylene blue/trypan blue etc.) or sterile milk through transurethral catheter into the urinary bladder and observing the colored leak. If necessary cystoscopy, ureteric catheterization, or indigo carmine intravenous administration should be done. IV indigo carmine 10–15 minutes prior to cystoscopy reveals efflux of dye-stained urine from the ureters. In the absence of cystoscope, hysteroscope can be used.[7] Most of the bladder injuries during cesarean section are intraperitoneal injury and usually it occurs at the dome of the bladder, more than 6 cm—and often more than 10 cm—away from the trigone.[15] Iatrogenic bladder injury can be classified as follows[16]
Grade 1: contusion, intramural hematoma or partial thickness laceration
Grade 2: extraperitoneal bladder wall laceration <2 cm
Grade 3: extraperitoneal >2 cm or intraperitoneal <2 cm laceration
Grade 4: intraperitoneal bladder wall laceration >2 cm
Grade 5: intra- or extraperitoneal bladder wall laceration involving the trigone or bladder neck
The involvement of the posterior area of bladder may raise the suspicion of trigonal and ureteral involvement. Grade 5 injury warrants calling the urologist or urogynecologist.
When to do the repair
Immediate repair is always better. Even for cesarean hysterectomy, it is suggested to repair the bladder rent and then complete the hysterectomy.[17]
Exceptions to immediate repair include some cases of placenta percreta with intractable haemorrhage that can be repaired in stages after controlling the bleeding. The second surgery is usually done within 24–48 hours.[18]
Technique of bladder repair
Repair
Usually done in two layers,[7,19] although some surgeons advocate single-layer[20] closure. Polyglycolic acid suture no. 3-0 is used. In the absence of this suture, in resource poor setting, atraumatic chromic catgut no 2-0 can be used. An interrupted simple suture is made. The first layer closes the mucosa by through-&-through repair. The second layer includes the muscularis and peritoneum.[19] It can be repaired by simple running stitches of both layers - first layer consists of mucosa & muscularis and second layer consists of serosa. The first layer is sutured with 3-0 and second layer with 2-0 polyglycolic acid suture.[21] [Figure 1] The authors have used atraumatic chromic catgut in their initial carrier, followed by polyglycolic acid; all the combination of repair—simple continuous suturing, interrupted suturing; excluding the bladder mucosa, through-&-through bladder mucosa—all healed adequately. The important point is the recognition of the injury intra-operatively and meticulous repair in the same sitting, which yield best result. From the description, it is understandable that bladder dome injury repair is not difficult and mastering it could save many women from developing vesicovaginal fistula afterward.
Figure 1.
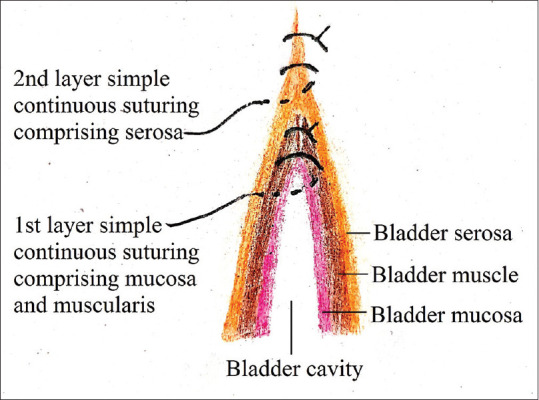
Bladder injury repair done by simple continuous suturing with polyglycolic acid suture. First layer is bladder mucosa and muscularis layer (3-0) and second layer is serosa (2-0). Mucosa pierced through-&-through. Repair can be done by interrupted suturing also
After completion of the two layers, at least 300 mL of saline with or without dye (e.g., methylene blue) should be instilled into the bladder through a transurethral Foley catheter. If leakage is present through sutures, then a top-up layer of imbricating suture should be added, thus attaining a water tight closure.[22] In case of placenta percreta with bladder invasion, some placental tissue may be left behind with the bladder wall and complete the repair.[23,24] Postoperatively placental tissue may get autolysed or methotrexate can be given.[23]
Urine drainage
Dual drains by suprapubic cystotomy (SPC) catheter with Malecot/Foley catheter and transurethral Foley catheter is better although gynecologists prefer only transurethral catheter. The size of the catheter should be SPC catheter (28–24) Fr and Foley catheter (16–18) Fr. Based on the authors’ experience, only transurethral catheter works well if postoperative urinary drainage is checked meticulously. Another dictum is that SPC recommended for large bladder rent, and a large transurethral Foley catheter would be sufficient for small rent.[19] A closed suction drain can be kept at the perivesical space and pelvis to look for urinary leakage.[24]
Postoperative period
The closed suction drain usually dries within 48–72 hours by which time it can be removed. Indwelling transurethral and SPC catheters are kept for at least 10 to 14 days.[25] In dual catheter insertion, the SPC catheter is clamped on day 10 and is removed on day 12. The transurethral catheter is removed on day 14. Barbieri RL[15] in his editorial has stated that the catheter should be kept for a minimum of 7 days. Urine should be tested for culture and sensitivity every third day when the patient is on prolonged catheterization.
Medicolegal aspect
From a medicolegal point of view, identification of the bladder and ureters should be described in the operation record.[7]
Bladder injury as a consequence of postoperative adhesion is defendable.[26]
Abnormal anatomy, e.g., when the bladder is high-up over the uterus inadvertent bladder injury is not negligent.[27]
When cesarean section is done during full dilatation of cervix, as the head lies deep in the pelvis, inadvertent bladder injury is not negligent.[27]
In the absence of abnormal anatomy, bladder injury may invite penalty. And if injury is not recognized intraoperatively, it may also be proven as negligence.
So as to avoid the medicolegal issues, it is always a wise approach to discuss the possibility of urinary tract injuries during cesarean section of the vulnerable patients during counselling and maintain a written documentation of it.
Key points
Bladder injury during cesarean section is not so rare nowadays (during primary CS 0.2% and repeat CS 0.6%).
Dome is commonly gets injured.
Recognition of the injury intraoperatively and immediate repair yields best result.
Usually two layer repair, simple continuous or interrupted, with polyglycolic acid suture 3-0/2-0 done.
Postoperative bladder catheterization for 10–14 days recommended.
Sharp dissection in the presence of dense adhesion can prevent bladder injury.
Proper preoperative counseling and good operative note may help to avoid litigation.
Conclusion
According to the new recommendation of Family physician training academy, primary care physicians are also need to be trained in performing cesarean section. The knowledge of bladder injury repair is an invaluable armamentarium—how to deal with the bladder dome injury which is the commonest; simultaneously, asking for the help of urologist or urogynecologist for trigonal injury. Although preventive measures to avoid bladder injury are always desired, adequate preoperative counselling can avoid medicolegal litigation.
Key message: Bladder injury during cesarean section (0.2% during primary CS & 0.6% during repeat CS) should be tried to prevent it and if at all occurred, it should be diagnosed intraoperatively and immediate repair in two layers can prevent many comorbidities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Eisenkop SM, Richman R, Platt LD, Paul RH. Urinary tract injury during cesarean section. Obstet Gynecol. 1982;60:591–6. [PubMed] [Google Scholar]
- 2.AAFP-ACOG joint statement on cooperative practice and hospital privileges. [Last accessed on 2020 Mar 10]. Available from: https://wwwaafporg/about/policies/all/aafp-acoghtml .
- 3.Recommended curriculum guidelines for family medicine residents. Maternity care AAFP Reprint No 261. [Last accessed on 2020 Mar 10]. Available from: https://wwwaafporg/dam/AAFP/documents/medical_education_residency/program_directors/Reprint261_Maternitypdf .
- 4.Peterson LE, Blackburn B, Phillips RL, Jr, Puffer JC. Structure and characteristics of family medicine maternity care fellowships. Fam Med. 2014;46:354–9. [PubMed] [Google Scholar]
- 5.Alanwar A, Al-Sayed HM, Ibrahim AM, Elkotb AM, Abdelshafy A, Abdelhadi R, et al. Urinary tract injuries during cesarean section in patients with morbid placental adherence: Retrospective cohort study. J Matern Fetal Neonatal Med. 2019;32:1461–7. doi: 10.1080/14767058.2017.1408069. [DOI] [PubMed] [Google Scholar]
- 6.Gungorduk K, Asicioglu O, Celikkol O, Sudolmus S, Ark C. Iatrogenic bladder injuries during caesarean delivery: A case control study. J Obstet Gynaecol. 201;;0:667–70. doi: 10.3109/01443615.2010.486086. [DOI] [PubMed] [Google Scholar]
- 7.Baskett TF, Calder AA, Arulkumaran S. Munro Kerr's Operative Obstetrics. 11th ed. Edinburgh: Saunders Elsevier; 2007. Obstetrics hysterectomy; pp. 309–14. [Google Scholar]
- 8.Narava S, Pokhriyal SC, Singh SB, Barpanda S, Bricker L. Outcome of multiple cesarean sections in a tertiary maternity hospital in the United Arab Emirates: A retrospective analysis. Eur J Obstet Gynecol Reprod Biol. 2020;247:143–8. doi: 10.1016/j.ejogrb.2020.01.035. [DOI] [PubMed] [Google Scholar]
- 9.Abdelazim I, Alanwar A, Shikanova S, Kanshaiym S, Farghali M, Mohamed M, et al. Complications associated with higher order compared to lower order cesarean sections. J Matern Fetal Neonatal Med. 2020;33:2395–402. doi: 10.1080/14767058.2018.1551352. [DOI] [PubMed] [Google Scholar]
- 10.Tarney CM. Bladder injury during cesarean delivery. Curr Womens Health Rev. 2013;9:70–6. doi: 10.2174/157340480902140102151729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baron J, Tirosh D, Mastrolia SA, Ben-Haroush Y, Schwartz S, Kerner Y, et al. Sliding sign in third-trimester sonographic evaluation of intra-abdominal adhesions in women undergoing repeat Cesarean section: A novel technique. Ultrasound Obstet Gynecol. 2018;52:662–5. doi: 10.1002/uog.19057. [DOI] [PubMed] [Google Scholar]
- 12.Celik S, Celik H, Soyer Calıskan C, Tosun M, Hatirnaz S. Bladder filling before accreta surgery is a very effective method for preventing bladder injury: A retrospective cohort study. J Matern Fetal Neonatal Med. 2019 doi: 10.1080/14767058.2019.1670809. doi: 101080/1476705820191670809. [DOI] [PubMed] [Google Scholar]
- 13.Kuznetsova N, Bushtyreva I, Barinova V, Shmakova K. Bladder filling technique to prevent complications of the urinary system during placenta accrete surgery. J Matern Fetal Neonatal Med. 2020;4:1–3. doi: 10.1080/14767058.2020.1723077. [DOI] [PubMed] [Google Scholar]
- 14.Corriere JN, Jr, Sandler CM. Diagnosis and management of bladder injuries. Urol Clin North Am. 2006;33:67–71. doi: 10.1016/j.ucl.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Barbieri RL. How to repair bladder injury at the time of cesarean delivery. OBG Management. 2011;23:6–9. [Google Scholar]
- 16.Vaidya B, Chaudhari M, Parmar D, Chaudhari V, Daginawala T, Shah R. Bladder injuries during obstetrical and gynecological surgeries. Int Surg J. 2017;4:2177–80. [Google Scholar]
- 17.Buchsbaum HJ, Walton LA. Strategies in Gynecological Surgery. 1st ed. New York: Springer-Verlag; 1986. pp. 77–104. [Google Scholar]
- 18.Caliskan E, Tan O, Kurtaran V, Dilbaz, Haberal A. Placenta previa percreta with urinary bladder and ureter invasion. Arch Gynecol Obstet. 2003;268:343–4. doi: 10.1007/s00404-002-0402-8. [DOI] [PubMed] [Google Scholar]
- 19.Wheeless CR, Jr, Roenneburg ML. Wedge resection of bladder. Atlas of Pelvic Surgery (on-line edition) [Last accessed on 2020 Mar 21]. Available from: www.atlasofpelvicsurgery.com/3bladderandUreter/10WedgeResectionOfBladder .
- 20.Rochelle JL, Shuch B, Belldegrun A. Urology. In: Brunicardi FC, Andersen DK, Billiar TR, Dunn DL, Hunter JG, editors. Schwartz's Principles of Surgery. 9th ed. New York: McGraw- Hill Companies Inc; 2010. pp. 1459–74. [Google Scholar]
- 21.Cunningham KG, Karam JA. Management of urologic complications in gynecologic oncology surgery. In: Ramirez PT, Frumovitz M, Abu-Rustum NR, editors. Principles of Gynecologic Oncology Surgery. 1st ed. Amsterdam: Elsevier; 2018. pp. 259–71. [Google Scholar]
- 22.Glaser LM, Milad MP. Bowel and bladder injury repair and follow-up after gynecologic surgery. Obstet Gynecol. 2019;133:313–22. doi: 10.1097/AOG.0000000000003067. [DOI] [PubMed] [Google Scholar]
- 23.Konijeti R, Rajfer J, Askari A. Placenta percreta and urologist. Rev Urol. 2009;11:173–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Matsubara S, Ohkuchi A, Yashi M, Izumi A, Ohwada M, Kuwata T, et al. Opening the bladder for cesarean hysterectomy for placenta previa percreta with bladder invasion. J Obstet Gynaecol Res. 2009;35:359–63. doi: 10.1111/j.1447-0756.2008.00941.x. [DOI] [PubMed] [Google Scholar]
- 25.Gill BC, Vasavada SP, Rackley RR. Bladder trauma treatment and management. Medscape Updated. 2019. Mar 26, [Last accessed on 2020 Mar 27]. Available from: https://emedicinemedscapecom/article/441124-treatment#d12Updated .
- 26.Ellis H, Crowe A. Medico-legal consequences of post-operative intra-abdominal adhesions. Int J Surg. 2009;7:187–91. doi: 10.1016/j.ijsu.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 27.Medical negligence – Cesarean section and bladder injury. [Last accessed on 2020 Mar 27]. Available from: https://wwwglynnscouk/articles/caesarean-section-and-bladder-injuryphp .


