Abstract
Background
The social media site Twitter has 145 million daily active users worldwide and has become a popular forum for users to communicate their health care concerns and experiences as patients. In the fall of 2018, a hashtag titled #DoctorsAreDickheads emerged, with almost 40,000 posts calling attention to health care experiences.
Objective
This study aims to identify common health care conditions and conceptual themes represented within the phenomenon of this viral Twitter hashtag.
Methods
We analyzed a random sample of 5.67% (500/8818) available tweets for qualitative analysis between October 15 and December 31, 2018, when the hashtag was the most active. Team coders reviewed the same 20.0% (100/500) tweets and the remainder individually. We abstracted the user’s health care role and clinical conditions from the tweet and user profile, and used phenomenological content analysis to identify prevalent conceptual themes through sequential open coding, memoing, and discussion of concepts until an agreement was reached.
Results
Our final sample comprised 491 tweets and unique Twitter users. Of this sample, 50.5% (248/491) were from patients or patient advocates, 9.6% (47/491) from health care professionals, 4.3% (21/491) from caregivers, 3.7% (18/491) from academics or researchers, 1.0% (5/491) from journalists or media, and 31.6% (155/491) from non–health care individuals or other. The most commonly mentioned clinical conditions were chronic pain, mental health, and musculoskeletal conditions (mainly Ehlers-Danlos syndrome). We identified 3 major themes: disbelief in patients’ experience and knowledge that contributes to medical errors and harm, the power inequity between patients and providers, and metacommentary on the meaning and impact of the #DoctorsAreDickheads hashtag.
Conclusions
People publicly disclose personal and often troubling health care experiences on Twitter. This adds new accountability for the patient-provider interaction, highlights how harmful communication affects diagnostic safety, and shapes the public’s viewpoint of how clinicians behave. Hashtags such as this offer valuable opportunities to learn from patient experiences. Recommendations include developing best practices for providers to improve communication, supporting patients through challenging diagnoses, and promoting patient engagement.
Keywords: social media, patient engagement, Twitter messaging, missed diagnosis, internet, physician patient relationship
Introduction
Twitter is a social media platform for users to share 280-character posts. Globally, Twitter included an average of 145 million daily active users in 2019; [1] 22% of Americans use the platform [2]. Twitter serves as an appealing resource to 61% of American adults who look for web-based health information [3], of which 12% use Twitter or social networking to share health updates [4-6]. Patients and families can develop communities for specific medical conditions and health care–related education [7,8]. Health care professionals utilize Twitter for networking, disseminating medical information, policy and research, disease and health communication monitoring, and advocacy for specific issues [9-11]. By providing this open forum, Twitter enables novel forms of dialogue among and across patients, patient advocacy groups, and health care professionals.
Twitter hashtags are words or phrases that Twitter users include in their posts to demarcate posts by a common theme or content. The hashtag can be entered as a search term and demarcate a particular dialogue on the website; therefore, it is a method of indexing conversations. In October 2018, a hashtag titled #DoctorsAreDickheads emerged on Twitter. The term originated from a professional YouTube video maker, who posted a video on Twitter explaining that she had been diagnosed with Ehlers-Danlos syndrome and postural orthostatic tachycardia syndrome (POTS) [12]. After describing her 8-year-long process with various health care professionals to receive the diagnosis, she closed the video with the phrase, “doctors are dickheads.” As users began to respond, #DoctorsAreDickheads emerged as a viral hashtag; patients, caregivers, and health professionals responded to the phrase by sharing their own experiences and criticizing the use of the hashtag. As of July 2020, the hashtag had been used in a total of 37,624 tweets by 12,731 Twitter user accounts and is still in active use (personal communication with Symplur, August 7, 2020).
We sought to describe the concepts represented in this hashtag as part of a broader depiction of patient-driven communications about health. To this end, we conducted a qualitative, phenomenological analysis of this hashtag. Our goal was to describe the who, the what, and the how of this phenomenon: who is posting the hashtag (as per their health care–related role), what is being stated with this hashtag or what are the common medical conditions associated with the hashtag, and how dialogue and prevalent concepts related to it arose. These concepts highlight specific patient and clinician challenges that are voiced publicly on social media and will inform future efforts to improve the patient’s experience of care.
Methods
Data Collection
We reviewed all tweets with the hashtag using a report generated from Symplur, a health care social media analytics company [13]. The greatest peak of this hashtag was in late October 2018 (see Multimedia Appendix 1 for the frequency of hashtags over time).
We then obtained tweets containing the hashtag dated between October 24 and December 31, 2018, comprising the predominant wave of use of the hashtag. We were able to obtain all tweets in this period, except for October 25, 2018, because of Symplur’s export limit of 2000 tweets at a time. In total, there were 9670 original tweets during the selected period, of which we were able to extract 8818. We randomly sampled 5.67% (500/8818) tweets for analysis using a random number generator. We selected 500 as the sample size based on a precedent social media analysis; Chan et al [14] demonstrated that a qualitative analysis of a sample of 540 tweets was sufficient to identify themes in how individuals understand and engage in health behaviors. We downloaded all tweets into Google Sheets spreadsheets (Google) for data abstraction and coding and used Microsoft Excel (Microsoft) for tabulation and thematic analysis.
Data Processing of User Characteristics
We excluded tweets from abstraction if they were not in English, were nonsensical in content, or clearly posted by a bot (eg, had bot in the Twitter user profile). As Symplur exported the link to the original tweet, coders in the team reviewed the original Twitter post on the web and read the first tweet above or below the tweet of interest for context when necessary, as tweets can be either standalone comments or part of a conversation or thread. Team members abstracted the demographic role of Twitter users by reviewing the user profile and content of the tweet. For example, if a user described an experience while receiving medical care in their tweet, we abstracted their role as patient. If a user described themselves as an advocate for a clinical issue in their Twitter profile, we classified them as advocate. As there was a substantial overlap in role between patient and patient advocate, as evidenced by tweet content or profile, we developed a shared category called patient or patient advocate. The team also abstracted the clinical conditions mentioned in the tweets, for example, depression or fibromyalgia.
Analysis of Themes
This was an interpretative phenomenological analysis, in which a phenomenon or lived experience is described by exploring the perspectives and shared meaning of those who have experienced it [15]. We sought to understand for whom, for what, and how the viral hashtag #DoctorsAreDickheads became a way to frame and represent patients’ lived experiences on Twitter. We used the iterative process known as a hermeneutic cycle, moving continuously between data collection, interpretation, and theorization and incorporating awareness of our subjective perspectives as researchers in order to develop a nuanced analysis of the phenomenon [16]. This helped us understand how patients interpolate their individual experiences into a wider discourse of patient experience through the hashtag #DoctorsAreDickheads.
Team members (AS, ZM, RC, JY, and JD) coded 20.0% (100/500) sampled tweets together and the remainder individually. Each team member first independently reviewed the content of 50 tweets, selecting a short code of a word or short phrase describing the conceptual topics represented in tweets with the hashtag #DoctorsAreDickheads. These codes ascribed what phenomenologically could be called the essence or the core meaning of a tweet. Afterward, the team compared codes into a preliminary codebook. The team then reapplied the preliminary codebook to the 50 previously coded tweets and then used it to code another 50 tweets independently. The team then met once more to review code application, discuss new codes, and begin the process of interpretation. Two research team members reconciled differences in code application for the initial 100 tweets that were coded by the entire research team. Once consensus and agreement had been established, we divided the remaining 400 posts among 5 members of the team and coded them independently using the codebook and developing new codes when necessary.
Throughout the process, team members wrote memos or notes to describe shared meaning from the individual codes. After all remaining tweets were coded, the team sorted and categorized memos based on thematic content, developing an interpretive framework of the hashtag #DoctorsAreDickheads to result in final themes. When discussing possible themes, we also conducted frequency checks to prioritize the themes that were most frequently identified in the data. We aimed to identify all meanings of the phenomenon included in the sample; thematic saturation is not a priority in a phenomenological approach [17].
This study was reviewed by the University of San Francisco, California, institutional review board and categorized as exempt, with the approval number 19-27965.
Results
User Characteristics
Of the 500 tweets analyzed in our sample, 9 were excluded. Reasons for exclusion included being in a language other than English (n=2), written by a bot owing to having bot in the profile or nonsensical content (n=5), or containing no content (n=2). The sample included 344 independent Twitter users, with a median tweet frequency of 1 per user; 1 account had 7 posts, 1 had 20 posts, and 1 had 22 posts. In total, 50.5% (248/491) of tweets were posted by patients or patient advocates. Almost one-third or 31.6% (155/491) of tweets were posted by people in the other or unknown category. Health care professionals contributed 9.6% (47/491) of tweets; 4.3% (21/491) tweets were posted by caregivers, 3.7% (18/491) were posted by academics or researchers, and 1.0% (5/491) were posted by media or non–health care organizations. A list of roles identified in the coded sample is available in Table 1.
Table 1.
Characteristics of Twitter users posting the hashtag #DoctorsAreDickheads (N=491).
| Demographics represented in the samplea | Values, n (%) |
| Patient and/or patient advocate | 248 (50.5) |
| Health care provider | 47 (9.6) |
| Caregiver and/or family member | 21 (4.3) |
| Researcher or academic | 18 (3.7) |
| Media, non–health care organization | 5 (1.0) |
| Non–health care individuals or unknown or other | 155 (31.6) |
aSome Twitter posts pertained to multiple demographics.
In our sample, 60.2% (296/491) tweets mentioned a clinical condition. The most common condition mentioned was chronic pain (44 tweets). Mental health, musculoskeletal, and obstetrical or gynecologic conditions and procedures were also common. Ehlers-Danlos syndrome was the most common specific condition, followed by fibromyalgia, chronic fatigue syndrome (also known as myalgic encephalitis), POTS, and mast cell activation syndrome. A full list of conditions is available in Table 2.
Table 2.
Clinical conditions mentioned in sample tweets (n=296).
| Condition | Number of tweets |
| Chronic pain | 44 (general pain: 38; fibromyalgia: 5) |
| Mental health | 31 |
| Musculoskeletal conditions | 26 (Ehlers-Danlos syndrome: 19; other: 7) |
| Obstetrical or gynecological conditions or procedures | 21 |
| Neurological conditions | 18 (chronic fatigue syndrome or myalgic encephalitis: 5; POTSa: 4; other conditions: 9) |
| Disability | 17 |
| Chronic illness (unspecified condition) | 14 |
| Gastrointestinal conditions | 8 |
| Autoimmune conditions | 7 (mast cell activation syndrome: 4; other autoimmune conditions: 3) |
aPOTS: postural orthostatic tachycardia syndrome.
Major Themes
We identified 3 core thematic results that were manifested in the experiences represented within our sample. Full definitions of each theme and additional exemplar quotes are found in Table 3. Of note, we are publishing verbatim tweets with usernames to give credit to Twitter users and their contributions to this discourse when possible. We obtained permission from cited users to publish these tweets. For tweets about which we received no response, we anonymized the content in accordance with recommendations regarding social media research [18].
Table 3.
Major themes and definitions identified in the content analysis of the Twitter hashtag.
| Theme | Definition | Example tweets |
| Belief and diagnosis | Describing experiences with medical providers being skeptical, dismissive, or “gaslighting”; this disbelief then causing delayed or incorrect diagnosis and/or medical harm |
|
| Power inequity in the patient-provider interaction | Differential in power (due to medical hierarchy as well as misogyny, White supremacy, and ableism) affecting communication and behaviors between clinicians and patients |
|
| Metacommentary | Discussion about the rationale for and impact of this hashtag in public discourse |
|
Belief and Diagnosis
Patients and caregivers described a common experience of clinicians not listening, not believing, minimizing, or not valuing their accounts of illness. The experience of being disbelieved was often linked to experiencing an incorrect, delayed, or missed diagnosis. These diagnostic adverse events were associated with physical harm:
Had terrible blood clots for several years–they said my legs were hurting from fibro and they couldn’t do anything. Then I started having trouble breathing and we dashed to the ER. The clots had ended up spreading from my legs to my lungs.
In addition to physical harm, others described emotional harm and guilt:
I felt horrible. I was ruining all the holidays, and I could not do a single thing about it. I felt like a worthless piece of crap. And all because... the doctors didn't look at me, did not see my pain as valid. Even now, with my diagnosis.. it is hard… #DoctorsAreDickheads.
@WheelieNick
The narratives with this theme described prevalent gaslighting, meaning a manipulative tactic in which someone questions a person’s perceptions, memories, and sense of reality. They also described egotistical behavior from clinicians, lording medical training or expertise over patients or being dismissive of patient input when their diagnosis or assessment was challenged:
A doc told me that I had a cancer syndrome. I said no way – I had been in an accident right before my symptoms started. He told me, “I have an Ivy League degree, so don’t ask questions.” Turns out he was incorrect. No cancer. #DoctorsAreDickheads.
Within this theme, we observed how patients countered the narrative of being dismissed by using #DoctorsAreDickheads to create a community where people are believed. In response to a thread in which a patient shared how they “sobbed . . . heaved with the realization that yet again (I’m) being gaslighted about (my) own damn body,” another Twitter user responded:
...please, consider the #DoctorsAreDickheads conversation. This hashtag shows that you're not on your own in this. It isn’t just you imagining things. Look at all the people here who believe your words.
Power Inequity in the Patient-Provider Interaction
Twitter users described their experiences using this hashtag as a result of the power inequity and hierarchy in medical care. Clinicians hold power in decision making and medical orders, serving as gatekeeper for desired services. This included experiences where clinicians denied patient bodily autonomy:
And then after I was finished having kids and wanted my tubes tied, the first two doctors I asked, refused. For non evidence based reasons. It took me 2.5 years to find a doctor who would. #DoctorsAreDickheads.
@MxPeachyKi
The power imbalance impacts communication, and a number of patients described being aware of what they felt they could or could not say, or self-edit what they would express in the visit, to protect themselves from consequences that would affect their care:
Honestly, if we suddenly go very silent and compliant, we're actually fighting back rage and tears bc we know damn well if we let it show you'll just label us hysterical and FIRE us as patients. Like we somehow serve YOU. #DoctorsAreDickheads.
@rhysfelis
Many of the accounts recounted experiences where patients felt that the clinicians were abusing their power. These experiences ranged from subtler, verbal diminishments of the patient experience to physical, verbal, and even sexual abuse and/or severely unethical care:
cw: sexual assault I had many doctors actively try to cover up or push under the rug the fact that their coworker sexually assaulted me when I was 14. All these people are still practicing at a major hospital, including assaulter. Suffice to say those #DoctorsAreDickheads.
@atoradegay
Within this theme was a call for attention to how the patient or clinician power differential is compounded by structural inequities in society. Tweets addressed how White, cisgender, and neurotypical patients have more privileges in medical visits because of structural power imbalances. People of color, lesbian, gay, bisexual, transgender, queer individuals, and people living with disabilities described an intersectional experience, shaped from their identities as members of marginalized groups, in which there was a higher risk of a negative encounter or inappropriate care:
My #DoctorsAreDickheads story: before I’m a physician, I’m a queer woman. Physicians, nurses, and everyone in healthcare have a long systemic history of abuse of power and broken trust with the LGBTQ+ community. My family & my community fear medicine because of it. Don’t @ me.
@ShannonOMac
THANK YOU. It was a little frustrating bc most of the participants were white and I didn't quite know how to articulate that #DoctorsAreDickheads is different when you have other marginalized IDs outside of being disabled or sick.
@Twitchyspoonie
Metacommentary on Hashtag
Although much of the conversation using this hashtag focused on narratives of experiences with clinicians, there was also a meta conversation about the meaning of the hashtag’s use on Twitter. This included the risks and benefits of using such an inflammatory term:
Yes this #DoctorsAreDickheads represents poor experiences of care. We try to and should improve this if needed.But doctors are humans, patients, parents, and professionals. Attacking us is counterintuitive when we campaign for improvements. #twitter is this really helpful?
@dr_nigel_lane
Patient advocates noted that the hashtag got attention, precisely because it was sensational:
The provocative hashtag #DoctorsAreDickheads drew people's attention to widespread, systemic medical maltreatment. A more polite hashtag couldn't have done this.
@jeff_says_that
Patients, advocates, and health care providers shared their frustration and hoped that this attention and dialogue would allow better understanding and possibly change:
The medical professionals getting butthurt by #doctorsaredickheads need to read it for what it is - our cries to be treated as PEOPLE first, CONDITIONS second. A desire for inclusivity and a genuine desire to help IMPROVE patient care and the doctor-patient relationship.
@Chrisa_Hickey
Within the metacommentary, a parallel hashtag emerged, #DoctorIRespect, used to share accounts of laudable or appropriate medical care. These tweets contained recommendations for improved communication during medical visits. Some tweets contained suggestions for engaging patients as partners in their care and system redesign to ensure more patient-centered care:
So how do you become a #DoctorIRespect? It’s really easy. If you have no clue what is going on, just say so. Tell us you don’t know. That’s all.
If you’re not involving patients, I urge you to begin doing so. Heck, there are many patients that have experience in orchestrating such change within large medical spaces (insert: waving hand emoji)We’re here with experience and even degrees. Hire us to help you. #DoctorsAreDickheads
@GraysonGoal
Discussion
Our study paints a picture of patients living with chronic conditions, lacking power within the medical encounter, and turning to social media to share testimonies of being disbelieved and disrespected. Our study is the first empirical approach to analyze the phenomenon of this hashtag on Twitter, utilizing a random sample. Another response was an editorial piece, which concluded that the degree of rancor in the conversation would not aid in improving medical care [19]. Rare or challenging clinical syndromes were commonly mentioned, such as Ehlers-Danlos syndrome, chronic pain, and chronic fatigue syndrome, which have been seen in other analyses of medical topics discussed on Twitter [20,21]. Twitter may be an underutilized resource for understanding the patient’s perspective and provider dynamics within the diagnostic pathway, particularly for challenging-to-diagnose conditions; social media data can be mined to monitor care quality and patient experience [22].
The connection between communication within the clinical encounter and the ability to make a correct and timely diagnosis was an unexpected finding. The hashtag #DoctorsAreDickheads highlighted how clinician engagement with patients is not just a matter of patient experience, but a priority for diagnostic safety. Patients shared how disrespectful treatment was connected to a missed, delayed, or incorrect diagnosis. Several previous studies on Twitter data found descriptions of procedural, medication, and diagnostic errors [17,23]; our larger sample validates that patients can self-identify and report diagnostic adverse events. How information is conveyed or received is highly dependent on belief and respect throughout the encounter. Improvements are urgently needed in how clinicians communicate and how patients are involved in the diagnostic pathway [24,25].
The central takeaway from our analysis was how patients felt disempowered, disrespected, and disbelieved. Patients described a range of ways in which they are vulnerable during a health care encounter [26]. Beginning with the existing power differential between provider and patient, tweets described how patients enter the health care system struggling with active symptoms of illness or health needs and can be further burdened by bias, including racism, misogyny, or ableism in the medical system, or by previous traumatic experiences with health care. These vulnerabilities could lead to avoidance or self-editing, which hashtag users described as trying to behave like a good patient rather than continuing to share their knowledge or expertise in their condition. When experiencing mistreatment, patients are not engaged in sharing knowledge and expertise in their conditions, further reducing the quality of the clinical encounter. Our findings resonate with other works detailing the impacts of power and hierarchy in medicine, in which the lack of agency or respect further perpetuates harm [27,28].
In addition to describing harm from misdiagnosis, patients described assaultive behavior from health care professionals, ranging from hurtful comments (eg, ableist or sexist remarks, carelessness about prognosis) to egregious, unethical, or illegal acts (including sexual abuse). Traditionally, the patient-clinician interaction is private, with few witnesses. Should there be abuse, patients do not have clear-cut routes of action. In the climate of #MeToo and the Black Lives Matter movement, people in positions of power are being held to greater accountability for their behavior. As this hashtag demonstrates, Twitter provides greater transparency to clinician behaviors in a public forum.
Using this hashtag, tweets demanded empathy on behalf of both clinicians and patients. Within the metacommentary theme, some hashtag users accused patients of exacerbating clinician burnout and mental illness. Patients and advocates responded by highlighting clinicians’ privilege, encouraging them to be less defensive and listening to critiques. This opposition between patient needs and clinician burnout is a false dichotomy and speaks to the deeper shortcomings of a medical system that erodes empathy both for patients and for health care personnel. As health care systems continue to explore changes to improve quality and patient experience, work to achieve the quadruple aim is aligned with improving both clinician workplace satisfaction and patient experience [29]. Both patient and clinician wellness are priorities; however, the #DoctorsAreDickheads conversation shows how power differentials and limitations in the current health care system disproportionately impact patients, putting their needs in conflict with providers.
Figure 1 shows how the themes relate to each other. The direct experiences of gaslighting, minimization, and ignoring patient expertise (Theme 2) are couched in the overarching themes of power differential, the burden of illness, and historically marginalized identities (Theme 1). In metacommentary, clinicians have responded both defensively and in support, and patients and advocates noted the hashtag’s utility to gain attention for advocacy for systemic changes (Theme 3).
Figure 1.
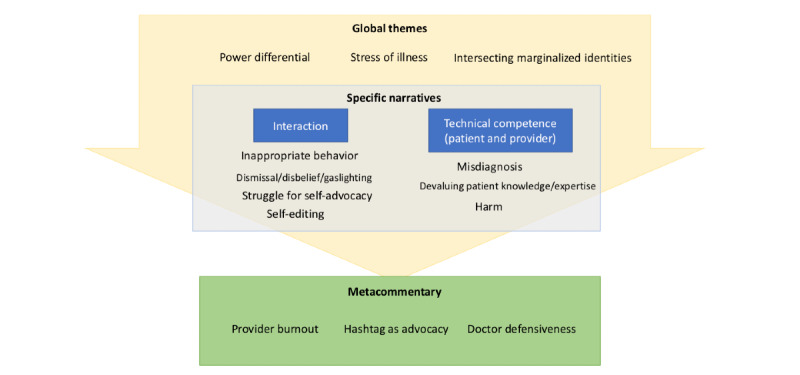
Map of major themes identified in Twitter hashtag.
We organized the experiences described in a process map of the patient and clinician encounter, showing how major themes function in a cyclical fashion (Figure 2). First, contextual factors, including the power differential, the patient’s intersectional identity, and provider well-being, affect the clinical interaction before a visit. During the encounter, the power differential affects the interaction in which the clinician may disbelieve, devalue, or gaslight the patient, who may engage in various coping behaviors such as self-advocacy, self-editing, or questioning care. In this interaction, downstream negative outcomes include misdiagnosis, medical harm, and negative patient experience or trauma. In this conceptual map, harmful outcomes are shared, highlighting the message of the #DoctorsAreDickheads hashtag as a call to action to improve outcomes for both patients and clinicians.
Figure 2.
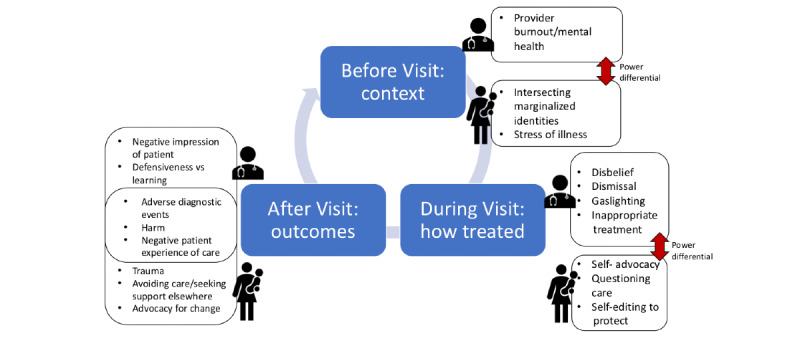
Cyclical process map of themes identified in Twitter hashtag.
Actionable recommendations for clinicians were provided with this phenomenon. First, clinicians can strive to diminish their defensiveness when patients share a negative experience. Second, there is the potential to improve how clinicians communicate in a clinical encounter. Trainings may improve clinician capacity to listen about a health concern, voice diagnostic uncertainty, even by stating “I don’t know,” and accompany patients through challenging diagnoses or chronic conditions. Third, patients encouraged increased patient engagement within health care systems, such as through community advisory boards or hiring patients as consultants, to develop more patient-centered care systems [30].
Limitations
Limitations of this study include a relatively small sample of events; however, our initial sample of 500 is similar to other qualitative analyses of social media posts [8,11]. Those who post on Twitter are not representative of all patients; however, given that 55.2 million people in the United States use Twitter, it is clear that Twitter’s users are a sizable proportion of enrolled patients [31]. We do not know if patients who are higher utilizers of health care are more or less likely to post content on Twitter using this hashtag. Finally, we do not know detailed demographic information about Twitter users or their geographic location.
Conclusions
Twitter and social media are growing platforms where patients discuss health care; this public forum holds clinicians to a higher level of accountability and transparency. #DoctorsAreDickheads is an intentionally sensational hashtag, born out of frustration with health care interactions. The hashtag is meant to raise awareness of common negative patient experiences, particularly for those living with challenging, rare, and chronic conditions. Patients experience disbelief, mistrust, and lack of listening from their clinicians, which they link to delayed or missed diagnoses. Patients asked for a deeper recognition of the capacity and expertise they bring to the clinical visit and awareness of how power and bias affect the encounter. Although clinicians may feel resistant to concerns expressed through social media, patient advocates on Twitter advocate for system-level improvements to improve medical treatment and patient experience. By systematically exploring views expressed on these platforms, clinicians and health care leaders may identify important areas for improvement, such as improved communication during a challenging diagnosis.
Acknowledgments
AS was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under award number KL2TR001870. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
The authors wish to thank those who generously shared their original posts for this manuscript. The authors thank Jane Lee for assistance with formatting.
Abbreviations
- NIH
National Institutes of Health
- POTS
postural orthostatic tachycardia syndrome
Appendix
Prevalence of hashtag #DoctorsAreDickheads over time.
Footnotes
Authors' Contributions: AS and US conceived of the original research idea. AS assembled the research team with input and support from US. RC compiled the data sample. AS, RC, ZM, JD, and JY developed an analytic protocol and conducted data coding, analysis, and interpretation with leadership from AS. AS composed the bulk of the manuscript, with RC contributing to the Methods section, ZM contributing to the Discussion section, and JD and JY contributing to the Introduction and Discussion sections. RC, ZM, JD, JY, and US provided edits to the manuscript. AS, ZM, and US developed the conceptual figures.
Conflicts of Interest: None declared.
References
- 1.Q3 2019 Letter to Shareholders. Twitter Investor Relations. 2019. [2020-08-04]. https://s22.q4cdn.com/826641620/files/doc_financials/2019/q3/Q3-2019-Shareholder-Letter.pdf.
- 2.Omnicore Agency. 2019. [2020-08-04]. https://www.omnicoreagency.com/twitter-statistics/
- 3.Perrin A, Anderson M. Share of US Adults Using Social Media, Including Facebook, is Mostly Unchanged Since 2018. Pew Research Center. 2018. Apr 10, [2020-08-04]. https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018/
- 4.The Social Life of Health Information. Pew Research Center. [2020-08-04]. https://www.pewresearch.org/internet/2009/06/11/the-social-life-of-health-information/
- 5.Pershad Y, Hangge P, Albadawi H, Oklu R. Social medicine: Twitter in healthcare. J Clin Med. 2018 May 28;7(6):-. doi: 10.3390/jcm7060121. https://www.mdpi.com/resolver?pii=jcm7060121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rivas R, Sadah SA, Guo Y, Hristidis V. Classification of health-related social media posts: evaluation of post content-classifier models and analysis of user demographics. JMIR Public Health Surveill. 2020 Apr 1;6(2):e14952. doi: 10.2196/14952. https://publichealth.jmir.org/2020/2/e14952/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Attai DJ, Cowher MS, Al-Hamadani M, Schoger JM, Staley AC, Landercasper J. Twitter social media is an effective tool for breast cancer patient education and support: patient-reported outcomes by survey. J Med Internet Res. 2015 Jul 30;17(7):e188. doi: 10.2196/jmir.4721. https://www.jmir.org/2015/7/e188/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Himelboim I, Han JY. Cancer talk on twitter: community structure and information sources in breast and prostate cancer social networks. J Health Commun. 2014;19(2):210–25. doi: 10.1080/10810730.2013.811321. [DOI] [PubMed] [Google Scholar]
- 9.McClellan C, Ali MM, Mutter R, Kroutil L, Landwehr J. Using social media to monitor mental health discussions - evidence from Twitter. J Am Med Inform Assoc. 2017 May 1;24(3):496–502. doi: 10.1093/jamia/ocw133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JL, DeCamp M, Dredze M, Chisolm MS, Berger ZD. What are health-related users tweeting? A qualitative content analysis of health-related users and their messages on twitter. J Med Internet Res. 2014 Oct 15;16(10):e237. doi: 10.2196/jmir.3765. https://www.jmir.org/2014/10/e237/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alnemer KA, Alhuzaim WM, Alnemer AA, Alharbi BB, Bawazir AS, Barayyan OR, Balaraj FK. Are health-related tweets evidence based? Review and analysis of health-related tweets on twitter. J Med Internet Res. 2015 Oct 29;17(10):e246. doi: 10.2196/jmir.4898. https://www.jmir.org/2015/10/e246/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boebi S. Stevie's On Twitter: New Video! My Biggest Secret: I'm Disabled. Twitter. 2018. Oct 22, [2019-12-09]. https://twitter.com/stevieboebi/status/1054467827447386112.
- 13.Symplur - Connecting the Dots in Healthcare Social Media. [2019-12-16]. https://www.symplur.com/
- 14.Chan B, Lopez A, Sarkar U. The canary in the coal mine tweets: social media reveals public perceptions of non-medical use of opioids. PLoS One. 2015;10(8):e0135072. doi: 10.1371/journal.pone.0135072. https://dx.plos.org/10.1371/journal.pone.0135072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biggerstaff D, Thompson AR. Interpretative Phenomenological Analysis (IPA): A Qualitative Methodology of Choice in Healthcare Research. Qualitative Research in Psychology. 2008 Sep 20;5(3):214–224. doi: 10.1080/14780880802314304. [DOI] [Google Scholar]
- 16.Neubauer BE, Witkop CT, Varpio L. How phenomenology can help us learn from the experiences of others. Perspect Med Educ. 2019 Apr;8(2):90–7. doi: 10.1007/s40037-019-0509-2. http://europepmc.org/abstract/MED/30953335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brocki JM, Wearden AJ. A critical evaluation of the use of interpretative phenomenological analysis (IPA) in health psychology. Psychol Health. 2007 Feb 1;21(1):87–108. doi: 10.1080/14768320500230185. [DOI] [Google Scholar]
- 18.Ayers JW, Caputi TL, Nebeker C, Dredze M. Don't quote me: reverse identification of research participants in social media studies. NPJ Digit Med. 2018;1:30. doi: 10.1038/s41746-018-0036-2. doi: 10.1038/s41746-018-0036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oliver D. David Oliver: incendiary healthcare hashtags. Br Med J. 2018 Nov 2;363:k4593. doi: 10.1136/bmj.k4593. [DOI] [PubMed] [Google Scholar]
- 20.Nicholl H, Tracey C, Begley T, King C, Lynch AM. Internet use by parents of children with rare conditions: findings from a study on parents' web information needs. J Med Internet Res. 2017 Feb 28;19(2):e51. doi: 10.2196/jmir.5834. https://www.jmir.org/2017/2/e51/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kloth YM, Deutsch KM, Danielson KA, Strack J, Law C. What Twitter teaches us about patient-provider communication on pain. PLoS One. 2019;14(12):e0226321. doi: 10.1371/journal.pone.0226321. https://dx.plos.org/10.1371/journal.pone.0226321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hawkins JB, Brownstein JS, Tuli G, Runels T, Broecker K, Nsoesie EO, McIver DJ, Rozenblum R, Wright A, Bourgeois FT, Greaves F. Measuring patient-perceived quality of care in US hospitals using Twitter. BMJ Qual Saf. 2016 Jun;25(6):404–13. doi: 10.1136/bmjqs-2015-004309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakhasi A, Bell SG, Passarella RJ, Paul MJ, Dredze M, Pronovost PJ. The potential of twitter as a data source for patient safety. J Patient Saf. 2019 Dec;15(4):e32–5. doi: 10.1097/PTS.0000000000000253. [DOI] [PubMed] [Google Scholar]
- 24.Singh H, Naik AD, Rao R, Petersen LA. Reducing diagnostic errors through effective communication: harnessing the power of information technology. J Gen Intern Med. 2008 Apr;23(4):489–94. doi: 10.1007/s11606-007-0393-z. http://europepmc.org/abstract/MED/18373151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McDonald KM, Bryce CL, Graber ML. The patient is in: patient involvement strategies for diagnostic error mitigation. BMJ Qual Saf. 2013 Oct;22(Suppl 2):ii33–9. doi: 10.1136/bmjqs-2012-001623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berry LL, Danaher TS, Beckham D, Awdish RL, Mate KS. When patients and their families feel like hostages to health care. Mayo Clin Proc. 2017 Sep;92(9):1373–81. doi: 10.1016/j.mayocp.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 27.Sharma M. 'Can the patient speak?': postcolonialism and patient involvement in undergraduate and postgraduate medical education. Med Educ. 2018 May;52(5):471–9. doi: 10.1111/medu.13501. [DOI] [PubMed] [Google Scholar]
- 28.Abraar K. Medicine’s Power Problem. Scientific American Blogs. 2019. Nov 09, [2020-08-04]. https://blogs.scientificamerican.com/voices/medicines-power-problem/
- 29.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–6. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bombard Y, Baker GR, Orlando E, Fancott C, Bhatia P, Casalino S, Onate K, Denis J, Pomey M. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018 Jul 26;13(1):98. doi: 10.1186/s13012-018-0784-z. https://implementationscience.biomedcentral.com/articles/10.1186/s13012-018-0784-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rimma K. How Many People Are Using Twitter? eMarketer: Data and Research on Digital for Business. 2018. Oct 24, [2020-08-02]. https://www.emarketer.com/content/the-social-series-who-s-using-twitter-infographic.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Prevalence of hashtag #DoctorsAreDickheads over time.


