Abstract
Background:
Takotsubo cardiomyopathy (TC), also known as stress-induced cardiomyopathy, has been increasingly described in relation to psychiatric illness.
Methods:
We performed a literature review to identify the key findings related to psychiatric illness in TC that may be relevant to the practice of mental health and other health care providers.
Results:
The association of psychiatric illness with TC in addition to the spectrum of psychiatric illness found in TC, the role of exacerbation or treatment of psychiatric illness in triggering TC, different modes of presentation, prognostic implications, and long-term management of psychiatric illness in TC are discussed. Additionally, we review the limitations of the pre-existing literature and suggest areas of future research.
Conclusions:
There is a strong association between pre-existing psychiatric illness, particularly anxiety and mood spectrum disorders, and TC. Acute exacerbation of psychiatric illness, rapid uptitration or overdose of certain psychotropic agents, and electroconvulsive therapy may trigger TC. Further studies are needed to better evaluate the prognostic significance and long-term management of psychiatric illness in TC.
Keywords: Takotsubo, stress cardiomyopathy, psychiatric illness, depression, anxiety
INTRODUCTION
Takotsubo cardiomyopathy (TC), also known as stress-induced cardiomyopathy, apical ballooning syndrome, and broken heart syndrome, is an increasingly diagnosed condition.1 TC is commonly recognized as transient left ventricular dysfunction that may mimic acute coronary syndrome but is without angiographic evidence of obstructive coronary artery disease.2 Basic demographics of TC are provided in Table 1.3–5 The condition is typically diagnosed in the setting of an acute emotional or physical stressor (also referred to as triggers) and should resolve with time. However, despite the general conception as a benign disorder, TC is associated with a similar rate of severe in-hospital complications (including death) as acute coronary syndrome and can recur with time.3
TABLE 1.
Baseline Characteristics in TC. Ranges Are Derived From Select Larger-Cohort Studies.3–5 Typical TC Variant Refers to Apical Predominant Wall Motion Abnormality
| Age, years | 60–69 |
| Female (%) | 78–92 |
| White (%) | 72–84 |
| Medicaid insurance (%) | 5–11 |
| Chest pain (%) | 47–76 |
| Dyspnea (%) | 46–47 |
| Physical trigger (%) | 36–72 |
| Typical TC variant (%) | 81–86 |
| Pre-existing psychiatric illness (%) | 29–37 |
| Pre-existing mood disorder (%) | 18–26 |
| Pre-existing anxiety disorder (%) | 14–22 |
In recent years, there has been an ever-increasing number of studies linking psychiatric illness and TC.3–5 Most of these studies have been retrospective in nature and include a large number of case reports/series of patients with pre-existing or active psychiatric illness experiencing TC. In this article, we seek to summarize the key findings of the pre-existing literature on this topic that may be useful for mental health and other health care providers involved in the care of patients with TC. We also attempt to point out the limitations of the pre-existing literature and suggest areas of future research.
METHODS
We conducted a comprehensive search of the pre-existing English language literature using the MEDLINE (U.S. National Library of Medicine) and PubMed (U.S. National Library of Medicine and National Institutes of Health) databases (1966–2017). Search terms included the keywords takotsubo, takot-subo, stress cardiomyopathy, stress-induced cardiomyopathy, apical ballooning syndrome, and broken heart syndrome, in addition to psychiatric illness, mood disorder, depression, anxiety disorder, panic attack, panic disorder, schizophrenia, psychosis, antidepressant, antipsychotic, and electroconvulsive therapy. The reference lists of the published articles retrieved in the literature search were also reviewed for additional relevant studies. The largest scale studies with sufficient data on pre-existing psychiatric illness were used to provide baseline demographics for the review.3–5 Figure 1 was borrowed from a prior publication from our group; the data from that publication was used to create Figure 2.4
FIGURE 1.
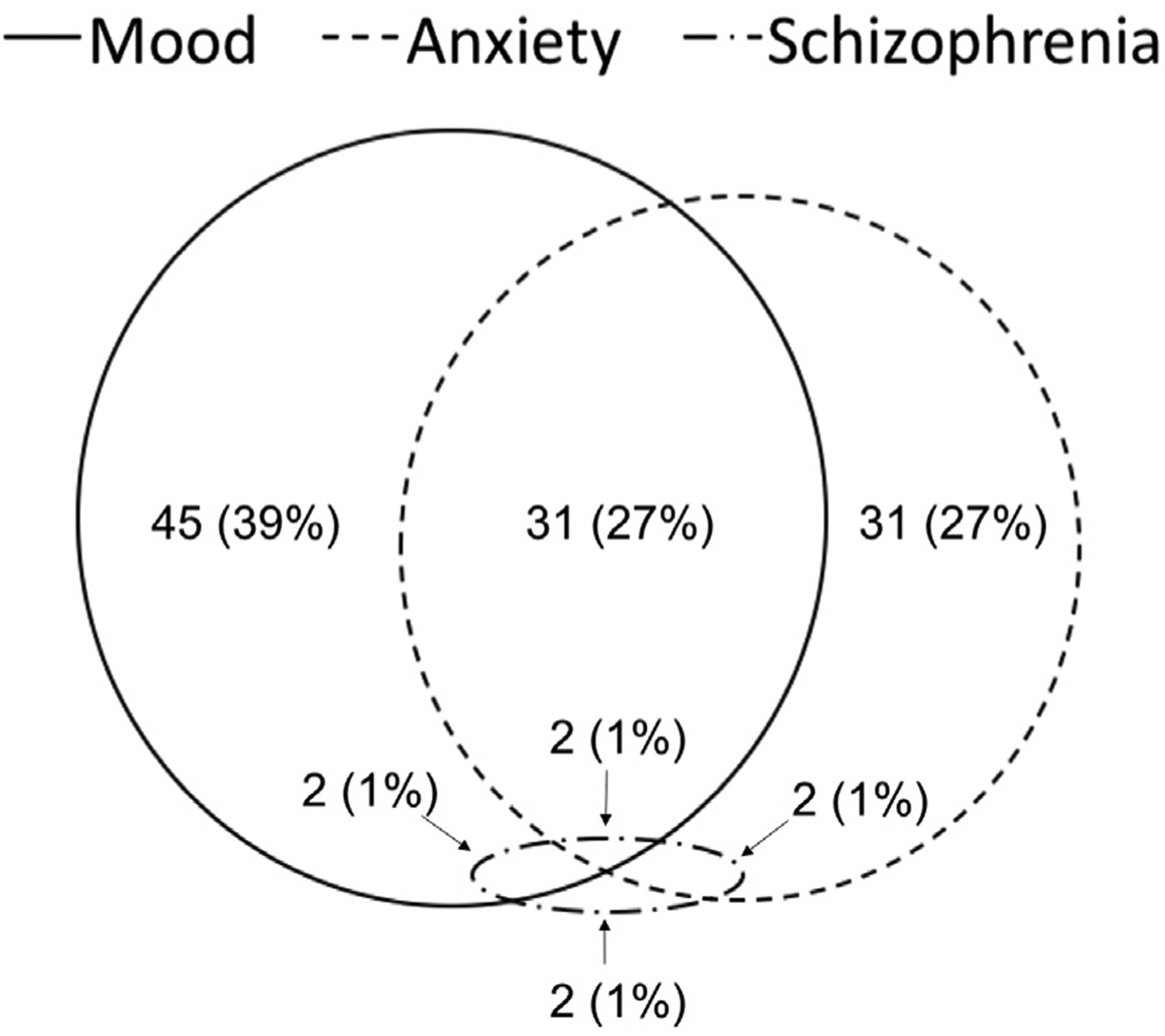
Spectrum of Pre-existing Psychiatric Illness in TC (Borrowed, With Permission, From the Original Source)4.
FIGURE 2.
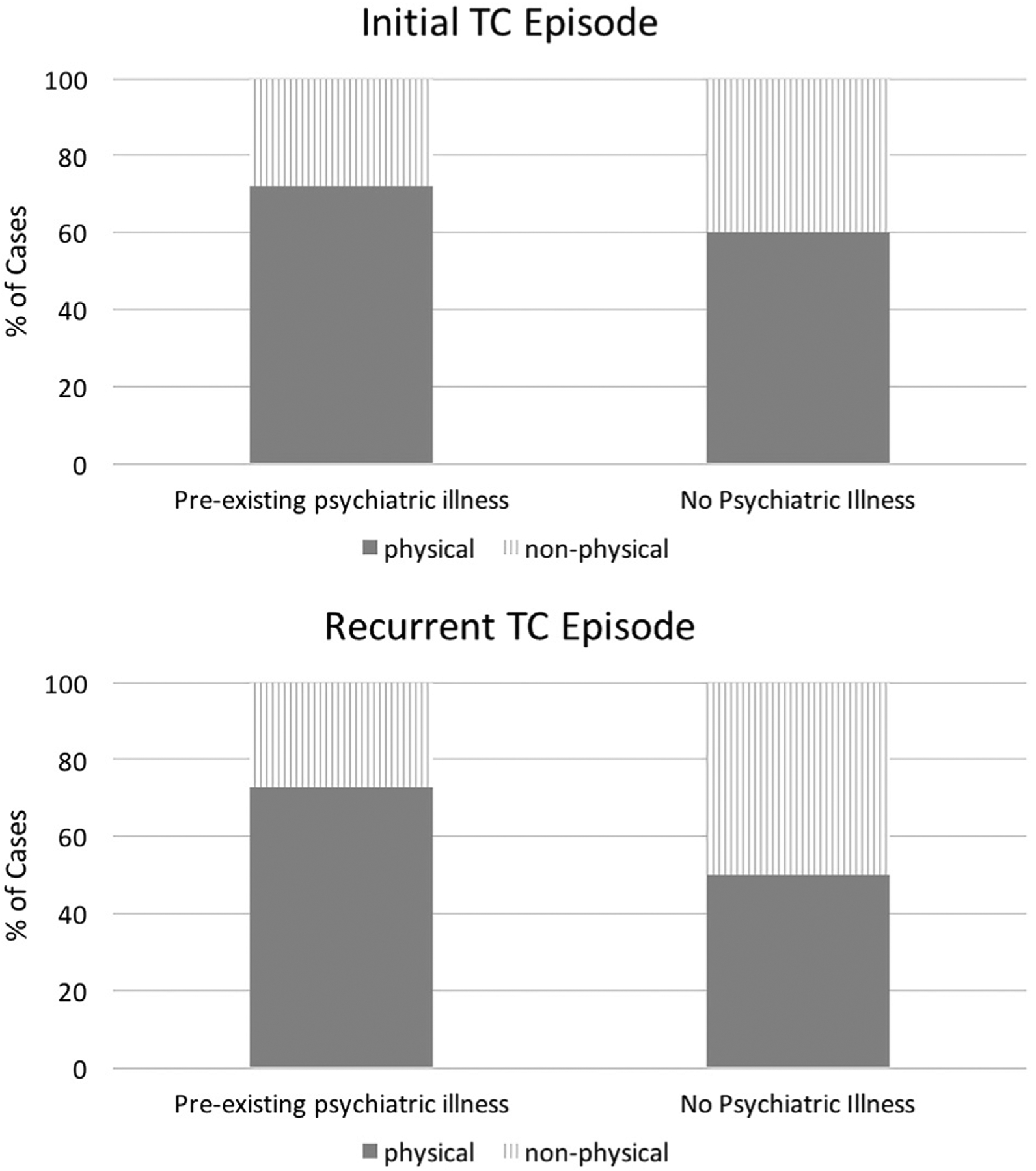
Mode of TC Trigger. Percent of Cases Triggered By Physical vs Nonphysical (Including Emotional) Stressors Are Shown4.
PRE-EXISTING PSYCHIATRIC ILLNESS AND TAKOTSUBO CARDIOMYOPATHY
The association of TC with comorbid psychiatric illness has been previously reported.3,5 Of note, increased age and female sex are known risk factors for certain psychiatric illnesses, such as depression, and TC is most classically described among postmenopausal women.3,6,7 Nevertheless, even when controlling for age and sex, there is a higher burden of pre-existing psychiatric comorbidity in TC patients compared to controls with acute coronary syndrome.3
The true etiology behind the association of TC and psychiatric illness is largely unknown, and explanations are speculative in nature. The role of the brain-heart axis in the pathophysiology of TC is thought to account for cases of TC secondary to primary neurological processes.3,8,9 One of the leading postulated mechanisms behind TC is that of catecholamine excess, and patients with pre-existing psychiatric illness have been thought to be at increased risk of TC due to disproportionately high catecholaminergic responses in addition to increased cardiac sympathetic sensitivity.10 Additionally, as described below, pharmacotherapy for psychiatric illness has also been described as a potential trigger of TC.11 Overall, the pathophysiology of TC, and hence the cause for its demographic and clinical associations, need further elucidation.
SPECTRUM OF PRE-EXISTING PSYCHIATRIC ILLNESS IN TAKOTSUBO CARDIOMYOPATHY
As noted in Table 1, roughly one-third of patients with TC have some form of pre-existing psychiatric illness. In prior case reports and retrospective cohort studies, diagnoses of mood disorders, anxiety disorders, schizophrenia-spectrum and other psychotic disorders, adjustment disorders, and neurocognitive disorders have been described in relation to TC.3,4,12,13 In a previous study, we described the spectrum of psychiatric illness in TC (Figure 1).4 There is a high prevalence of mood and anxiety disorders with a significant proportion of patients with multiple diagnoses.4
Despite the clear association of TC with psychiatric illness as a broad entity, its independent association with individual disorders remains disputed. The largest point of debate and inconsistency in the literature remains the association of TC with mood vs anxiety disorders. In a few small retrospective case-control studies, only pre-existing anxiety disorders (and not mood disorders) were associated with TC.14,15 However, in the International Takotsubo Registry, patients with TC had significantly higher rates of depression and anxiety compared to controls.3 A large observational study with over 24,000 patients from the National Inpatient Sample also found higher prevalence of anxiety and mood disorders in patients with TC compared to controls.5 Overall, the larger studies on TC have demonstrated a link of TC with both anxiety and mood disorders, and the confounding data come from largely underpowered studies. The association of other psychiatric illnesses, including schizophrenia-spectrum and other psychotic disorders, with TC remains largely unknown and an area for future research.
EXACERBATION OF PSYCHIATRIC ILLNESS AS TAKOTSUBO CARDIOMYOPATHY TRIGGER
In addition to the association of TC with pre-existing psychiatric illness, there is evidence for acute exacerbations of psychiatric disorders as potential triggers of TC. Prior case reports have described exacerbations of anxiety, depression, mania, and psychosis as potential causes of TC episodes.12,16 In the International Takotsubo Registry, ~10% of patients were diagnosed with “acute psychiatric disorders” with 4% and 1% with mood and anxiety disorders, respectively.3 However, whether or not acute psychiatric decompensation was the trigger of each TC case was not reported. Currently, the proportion of TC cases clearly triggered by exacerbation of psychiatric illness, remains unknown.
The pathophysiology linking exacerbation of psychiatric illness with TC is largely speculative. As noted above, catecholamine excess is one of the most commonly cited potential mechanisms behind TC.10 Increased serum catecholamine levels have been demonstrated in patients with mood and anxiety disorders and may explain the association between exacerbations of these disorders and onset of TC.17,18 These findings invite questions regarding the role of psychiatric treatment in patients with pre-existing psychiatric illness in potentially reducing the risk of TC.
TREATMENT OF PSYCHIATRIC ILLNESS: POTENTIAL TRIGGER OF TAKOTSUBO CARDIOMYOPATHY?
In addition to acute exacerbation of psychiatric illness, changes in psychotropic medications have also been shown to trigger TC. Multiple reports have linked both the uptitration and overdose of serotonin-norepinephrine reuptake inhibitors (SNRI) with cases of TC.19,20 Atomoxetine, a selective norepinephrine reuptake inhibitor (S-NRI), has also been reported to trigger TC.21 A recent review of the literature identified 22 cases of TC secondary to SNRI or S-NRI use.11 Notably, to date, there have been no clear cases of selective serotonin reuptake inhibitors (SSRIs) as a trigger of TC.
Endogenous increase in serum norepinephrine is thought to be the potential trigger of TC in the setting of S-NRI or SNRI use.11 Lithium has also been linked with increased serum catecholamine levels and has been reported as a trigger of TC.22,23 Most of the cases of TC trigger secondary to S-NRI, SNRI, or lithium use were in the setting of relatively rapid uptitration or in overdose.19–21,23 The risk of TC trigger when these medications are appropriately dosed and slowly uptitrated is less clear.
Electroconvulsive therapy (ECT), an effective treatment option for mood and psychotic disorders, has also been shown to trigger TC.24–26 ECT is known to transiently and abruptly increase serum catecholamine levels during the induced seizure, which as stated above, is a proposed mechanism behind TC.27,28 Moreover, primary epileptic seizures have been consistently described as triggers of TC; this may further explain the association of ECT with TC.29,30 The absolute risk of TC with each ECT therapy remains unknown. Further research is needed to determine whether or not ECT is a safe treatment option for patients with pre-existing psychiatric illness and a history of TC.
EMOTIONAL VERSUS PHYSICAL TRIGGERS OF TAKOTSUBO CARDIOMYOPATHY
Differential modes of triggering TC in patients with pre-existing psychiatric illness have been scarcely studied. In a prior study, we found that somewhat surprisingly, patients with pre-existing psychiatric illness present with TC more often following physical stressors than patients without pre-existing psychiatric illness (Figure 2).4 Overall, there is no evidence that patients with pre-existing psychiatric diagnoses have initial presentations or recurrences of TC due to emotional triggers at a higher rate than patients with no psychiatric illness.4 The current evidence seems to suggest that patients with pre-existing psychiatric illness are at increased risk of TC and that the diagnosis should be considered when appropriate even in the absence of clear emotional distress.
PROGNOSTIC IMPLICATIONS
There are scant data on long-term outcome predictors in patients with TC. In a previous study, we demonstrated increased risk of TC recurrence in patients with pre-existing psychiatric illness.4 As noted above, each episode of TC can be associated with considerable risk of morbidity and mortality.3 However, psychiatric illness has not been associated with different long-term survival in patients with TC.3,4 There is concern for insufficient statistical power to detect smaller associations given the relative rarity of TC and the low risk of recurrence (~2% per patient year).3 Larger scale studies with lengthier follow-up periods are needed to further assess any long-term prognostic significance of acute or chronic psychiatric illness in TC.
LONG-TERM MANAGEMENT
The ideal long-term management in TC, regardless of underlying psychiatric illness, is poorly delineated. In the International Takotsubo Registry, angiotensin-converting–enzyme inhibitors (ACEIs) and angiotensin-receptor blockers (ARBs), but not beta blockers, were associated with survival at 1 year of index diagnosis.3 However, there are no large randomized trials assessing the use of ACEIs, ARBs, or beta blockers following diagnoses of TC.
It is less known about the role of psychotropic medications in the management of patients with TC and psychiatric illness. As mentioned earlier, there is some evidence that rapid uptitration or overdose of SNRIs may trigger TC.11,19,20 Given the lack of similar reports with SSRIs, it may be reasonable to consider an agent from this class for the treatment of mood or anxiety disorders in patients with TC. Of note, a relatively underpowered retrospective study of 78 patients with TC showed increased mortality and decreased recovery of ventricular function in patients taking SSRIs.31 However, the findings of this study have not been confirmed in other studies, including those with substantially larger cohorts. Overall, there is no evidence of benefit of psychotropic treatment in patients with TC, and in fact, there is concern for association with trigger of TC or even mortality. Yet, there is evidence that patients with pre-existing psychiatric illness are at increased risk of recurrence; whether or not aggressive management of the underlying psychiatric disorders can reduce the rate of TC recurrence is unknown.4
As noted above, ECT can be associated with triggering of TC through several postulated mechanisms.24–30 Although there is no evidence to suggest that ECT is in some way contraindicated in patients with pre-existing TC, a heightened degree of clinical suspicion may be warranted for such patients.
LIMITATIONS OF THE LITERATURE
As aforementioned, the current understanding of the underlying pathophysiology, clinical associations, and long-term management of TC is very limited. Despite increased recognition and higher rates of diagnosis in recent years, the disorder remains rare, and most published studies are in the form of case reports, case series, or retrospective observational studies based on small cohorts. The resulting limitations in statistical power hinder the study of TC in general, and even more so in the association of other variables, such as psychiatric disorders. Most importantly, in the absence of large-scale randomized controlled trials, the long-term management of TC is often subject to the clinician’s gestalt and carried out in the absence of significant evidence.
Regarding the study of psychiatric illness in TC, there is significant limitation in the accurate assessment and analysis of the individual psychiatric diagnoses as reported in the medical record. In most cases, psychiatric diagnoses are obtained from review of the medical record and without real-time assessment of each patient for consistency with Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria. This can lead to the under-, over-, or misdiagnosis of psychiatric disorders in such studies. Additionally, insufficient statistical power often limits the ability to analyze different psychiatric illnesses individually, and multiple diagnoses are commonly grouped together in the analyses. Hence, findings from such studies must be interpreted in the context of how “psychiatric illness” was defined with appropriate suspicion for potential confounding.
FUTURE DIRECTIONS AND CONCLUSIONS
Having established an association between psychiatric disease and TC, further studies are needed to better assess the spectrums of such disease. In particular, there is very little known regarding any association between nonanxiety and nonmood disorders with TC. Studies looking at such disorders, including schizophrenia, for a potential association with TC could add significant insight to this field. Where an association is already established (that is with mood and anxiety spectrum disorders), we suggest larger scale studies to better evaluate for the prognostic implications of these particular psychiatric illnesses in TC.
Assessment of a patient’s emotional state at the time of presentation is often exclusively done per patient report, and there is concern for underreporting of emotional distress due to denial, minimization, and alexithymia.32 Potential interviews with the significant others of patients with TC may help reveal any undereported degree of emotional distress among patients with or without pre-existing psychiatric illness. Illicit substance abuse which is also often assessed per patient report may be underestimated in patients with TC. Given the known high degree of co-occurrence between psychiatric illness and substance abuse, studies with urine toxicology screens may yield interesting results regarding any potential relationship between substance abuse and TC in patients with psychiatric illness.33
The management of psychiatric illness in TC, as a reflection of TC in general, is in great need of larger scale prospective studies and randomized trials. The safety and utility of treatment of psychiatric illness via pharmacotherapy or ECT in patients with history of TC are largely unknown. In the absence of trials, observational studies comparing outcomes of TC patients based on pharmacological treatment for psychiatric illness may help better evaluate the safety profile of these agents. Here, we suggest careful documentation of drug dosages to further evaluate the notion that the trigger of TC with these agents is often in the setting of overdose or rapid uptitration. Regarding ECT, a case series of patients with a history of TC who subsequently undergo ECT may provide a starting point to better estimate the safety profile of this treatment modality in this patient population.
A summary of the current knowledge regarding psychiatric illness in TC is provided in Table 2.
TABLE 2.
Key Points Summarizing the Current Knowledge of Psychiatric Illness in TC
| Key points |
|---|
| There is a strong association between psychiatric illness and TC. |
| The pathophysiology behind this association is largely speculative. Postulated mechanisms include the role of the brain-heart axis and catecholamine excess in patients with psychiatric illness. |
| The spectrum of psychiatric illness associated with TC likely includes both anxiety and mood spectrum disorders. The association of other psychiatric illnesses, including psychoses, with TC remains largely unknown. |
| In patients with psychiatric illness, TC may be triggered by physical or emotional stress. |
| There are reports linking uptitration or overdose of SNRIs and S-NRIs with triggering of TC. The long-term safety profiles and ideal choice of psychotropic agents in patients with TC is poorly delineated. |
| ECT has been extensively reported as a potential trigger of TC and should be used with caution in patients with a history of TC. |
| Pre-existing psychiatric illness may be associated with increased recurrence of TC; however, other long-term prognostic implications are unknown. |
| Further studies are needed to better evaluate the management of psychiatric illness in TC, with a focus on the role and safety profile of pharmacotherapy and ECT. |
Footnotes
Disclosure: The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- 1.Khera R, Light-mcgroary K, Zahr F, Horwitz PA, Girotra S: Trends in hospitalization for takotsubo cardiomyopathy in the United States. Am Heart J 2016; 172:53–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prasad A, Lerman A, Rihal CS: Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008; 155(3):408–417 [DOI] [PubMed] [Google Scholar]
- 3.Templin C, Ghadri JR, Diekmann J, et al. : Clinical features and outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med 2015; 373(10):929–938 [DOI] [PubMed] [Google Scholar]
- 4.Nayeri A, Rafla-yuan E, Farber-eger E, et al. : Pre-existing psychiatric illness is associated with increased risk of recurrent Takotsubo cardiomyopathy. Psychosomatics. 2017; 58:527–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-sayed AM, Brinjikji W, Salka S: Demographic and comorbid predictors of stress (Takotsubo) cardiomyopathy. Am J Cardiol 2012; 110(9):1368–1372 [DOI] [PubMed] [Google Scholar]
- 6.Pedersen CB, Mors O, Bertelsen A, et al. : A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry 2014; 71(5):573–581 [DOI] [PubMed] [Google Scholar]
- 7.Birkhäuser M: Depression, menopause and estrogens: is there a correlation? Maturitas 2002; 41(Suppl 1):S3–S8 [DOI] [PubMed] [Google Scholar]
- 8.Samuels MA: The brain-heart connection. Circulation 2007; 116(1):77–84 [DOI] [PubMed] [Google Scholar]
- 9.Suzuki H, Matsumoto Y, Kaneta T, et al. : Evidence for brain activation in patients with takotsubo cardiomyopathy. Circ J 2014; 78(1):256–258 [DOI] [PubMed] [Google Scholar]
- 10.Ziegelstein RC: Depression and tako-tsubo cardiomyopathy. Am J Cardiol 2010; 105(2):281–282 [DOI] [PubMed] [Google Scholar]
- 11.Y-hassan S: Serotonin norepinephrine re-uptake inhibitor (SNRI)-, selective norepinephrine reuptake inhibitor (S-NRI)-, and exogenously administered norepinephrine-induced takotsubo syndrome: analysis of published cases. Int J Cardiol 2017; 231:228–233 [DOI] [PubMed] [Google Scholar]
- 12.Corrigan FE, Kimmel MC, Jayaram G: Four cases of takotsubo cardiomyopathy linked with exacerbations of psychiatric illness. Innov Clin Neurosci 2011; 8(7):50–53 [PMC free article] [PubMed] [Google Scholar]
- 13.Yaqub Y, Jenkins LA, Nugent KM, Chokesuwattanaskul W: Postpartum depression and apical ballooning syndrome (takotsubo syndrome). J Obstet Gynaecol Can 2009; 31(8):736–739 [DOI] [PubMed] [Google Scholar]
- 14.Salmoirago-blotcher E, Rosman L, Wittstein IS, et al. : Psychiatric history, post-discharge distress, and personality characteristics among incident female cases of takotsubo cardiomyopathy: A case-control study. Heart Lung 2016; 45(6):503–509 [DOI] [PubMed] [Google Scholar]
- 15.Goh AC, Wong S, Zaroff JG, Shafaee N, Lundstrom RJ: Comparing anxiety and depression in patients with Takotsubo stress cardiomyopathy to those with acute coronary syndrome. J Cardiopulm Rehabil Prev 2016; 36(2):106–111 [DOI] [PubMed] [Google Scholar]
- 16.Maldonado JR, Pajouhi P, Witteles R: Broken heart syndrome (Takotsubo cardiomyopathy) triggered by acute mania: a review and case report. Psychosomatics 2013; 54(1):74–79 [DOI] [PubMed] [Google Scholar]
- 17.Fell D, Derbyshire DR, Maile CJ, et al. : Measurement of plasma catecholamine concentrations. An assessment of anxiety. Br J Anaesth 1985; 57(8):770–774 [DOI] [PubMed] [Google Scholar]
- 18.Wyatt RJ, Portnoy B, Kupfer DJ, Snyder F, Engelman K: Resting plasma catecholamine concentrations in patients with depression and anxiety. Arch Gen Psychiatry 1971; 24(1):65–70 [DOI] [PubMed] [Google Scholar]
- 19.Christoph M, Ebner B, Stolte D, et al. : Broken heart syndrome: Tako Tsubo cardiomyopathy associated with an overdose of the serotonin-norepinephrine reuptake inhibitor Venlafaxine. Eur Neuropsychopharmacol 2010; 20(8):594–597 [DOI] [PubMed] [Google Scholar]
- 20.Selke KJ, Dhar G, Cohn JM: Takotsubo cardiomyopathy associated with titration of duloxetine. Tex Heart Inst J 2011; 38(5):573–576 [PMC free article] [PubMed] [Google Scholar]
- 21.Naguy A, Al-mutairi H, Al-tajali A: Atomoxetine-related Takotsubo cardiomyopathy. J Psychiatr Pract 2016; 22(3):232–233 [DOI] [PubMed] [Google Scholar]
- 22.Terao T, Yanagihara N, Abe K, Izumi F: Lithium chloride stimulates catecholamine synthesis and secretion in cultured bovine adrenal medullary cells. Biol Psychiatry 1992; 31(10):1038–1049 [DOI] [PubMed] [Google Scholar]
- 23.Kitami M, Oizumi H, Kish SJ, Furukawa Y: Takotsubo cardiomyopathy associated with lithium intoxication in bipolar disorder: a case report. J Clin Psychopharmacol 2014; 34(3):410–411 [DOI] [PubMed] [Google Scholar]
- 24.Kellner CH, Knapp RG, Petrides G, et al. : Continuation electroconvulsive therapy vs pharmacotherapy for relapse prevention in major depression: a multisite study from the Consortium for Research in Electroconvulsive Therapy (CORE). Arch Gen Psychiatry 2006; 63(12):1337–1344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vuksan Ćusa B, Klepac N, Jakšić N, et al. : The effects of electroconvulsive therapy augmentation of antipsychotic treatment on cognitive functions in patients with treatment-resistant schizophrenia. J ECT 2017; 34(1):31–34 [DOI] [PubMed] [Google Scholar]
- 26.Narayanan A, Russell MD, Sundararaman S, Shankar KK, Artman B: Takotsubo cardiomyopathy following electroconvulsive therapy: an increasingly recognised phenomenon. BMJ Case Rep 2014. pii: bcr2014206816 Available from: 10.1136/bcr-2014-206816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rudorfer MV, Risby ED, Hsiao JK, Linnoila M, Potter WZ: Disparate biochemical actions of electroconvulsive therapy and antidepressant drugs. Convuls Ther 1988; 4(2):133–140 [PubMed] [Google Scholar]
- 28.Nikisch G, Mathé AA: CSF monoamine metabolites and neuropeptides in depressed patients before and after electroconvulsive therapy. Eur Psychiatry 2008; 23(5):356–359 [DOI] [PubMed] [Google Scholar]
- 29.Lemke DM, Hussain SI, Wolfe TJ, et al. : Takotsubo cardiomyopathy associated with seizures. Neurocrit Care 2008; 9(1):112–117 [DOI] [PubMed] [Google Scholar]
- 30.Stöllberger C, Wegner C, Finsterer J: Seizure-associated Takotsubo cardiomyopathy. Epilepsia 2011; 52(11):e160–e167 [DOI] [PubMed] [Google Scholar]
- 31.Dias A, Franco E, Figueredo VM, Hebert K, Quevedo HC: Occurrence of Takotsubo cardiomyopathy and use of antidepressants. Int J Cardiol 2014; 174(2):433–436 [DOI] [PubMed] [Google Scholar]
- 32.Ketterer MW, Smith TW: Self-reported versus other-reported distress and coronary artery calcification. Psychosom Med 2011; 73(8):721. [DOI] [PubMed] [Google Scholar]
- 33.Kerfoot KE, Petrakis IL, Rosenheck RA: Dual diagnosis in an aging population: prevalence of psychiatric disorders, comorbid substance abuse, and mental health service utilization in the Department of Veterans Affairs. J Dual Diagn 2011; 7(1–2):4–13 [DOI] [PubMed] [Google Scholar]


