Abstract
Background/Aim: SARS-CoV-2 pandemic imposed extraordinary restriction measures and a complete reorganization of the Health System. The aim of the study was to evaluate the impact of COVID-19 on emergency surgical department accesses. Patients and Methods: Patients admitted to surgical emergency departments was retrospectively recorded during the Lockdown (March 11, 2020-May 3, 2020) and compared with the same number of days in 2019 and immediately before Lockdown (January 16, 2020-March 10, 2020). Diagnoses, priority levels, modes of patient’s trans-portation, waiting times and outcomes were analysed. Results: During the lockdown phase, we ob-served a reduction in the access to emergency surgical departments of 84.45% and 79.78%, com-pared with the Pre-Lockdown2019 and Pre-Lockdown2020 groups, respectively. Patient’s transportation, hospitalization and patients discharge with indications to an outpatient visit, waiting and total times exhibited a significant difference during the lockdown (p<0.005). Conclusion: We observed a reduction of surgical emergency accesses during the lockdown. Implementing the use of the regional systems and preventing overcrowding of emergency departments could be beneficial for reducing waiting times and improving the quality of treatments for patients.
Keywords: COVID-19, Emergency Department, SARS-CoV-2, surgical emergency, first aid, lockdown
SARS-CoV-2 incidence was dramatically increasing worldwide during the first months of 2020 (1). As of Mar 10, 2020, the government has implemented extraordinary measures to limit viral spread (2). The Italian Health System underwent a complete reorganization. According to the WHO recommendations regarding identification and isolation of COVID-19 suspected cases, some hospitals were turned into COVID-19 centers (3). Despite this selection, centers guaranteed to operate an emergency department for unsuspected COVID-19 patients as well.
Patients usually presenting with respiratory symptoms, fever and having been in contact with SARS-CoV-2 patients were addressed to specific isolated units. Otherwise, patients presenting with no previous symptoms were addressed in a conventional emergency department.
In the last few years, emergency departments in Italy have experienced overcrowding with more than 20 million accesses to first aid facilities (4). The overcrowding of emergency department has led to crowded waiting rooms and long waiting times. This could be a further problem during the lockdown. The aim of our retrospective study was to evaluate the impact of COVID-19 and the Italian Health System recommendations regarding surgical emergency department accesses.
Patients and Methods
Population and data collection. In this monocentric retrospective study, we evaluated the impact of COVID-19 on surgical emergency department access in the Tor Vergata University COVID-19 hospital. The Institutional review of our Department waived the need for a formal approval due to the retrospective nature of the study and in view of the emergency. Patients admitted to our surgical emergency department were retrospectively enrolled in the study during phase I of lockdown, from March 11, 2020 to May 3, 2020. These patients were considered as the lockdown group and were compared with similar patients admitted from March 11, 2019 to May 3, 2019 (Pre-Lockdown2019 group) and from January 16, 2020 to March 10, 2020 (Pre-Lockdown2020 group).
Variable and outcome definition. The number of surgical accesses to the emergency department of our COVID-19 hospitals are reported. For each patient admitted, a diagnosis was made. Patients were categorized into four priority levels according to triage system (5). The modes of patient’s transportation to the emergency department were reported and analyzed. Cases were classified according to outcome into: hospitalized, discharged home, transferred to other facility, patient to be followed in outpatient visits, death and hospitalization refusal by patient.
Age and sex data were retrospectively collected from clinical notes. Waiting time (WT) of patients and duration of treatment time (TT) were reported. WT was reported in minutes and considered as the time between assessment and emergency code assignment (Triage evaluation) to the initiation of medical treatments. The time between the beginning of medical treatment and discharge from the emergency department was reported in minutes and depicted as TT.
The aim of the study was to evaluate the impact of COVID-19 during the periods mentioned, on the previously described variables.
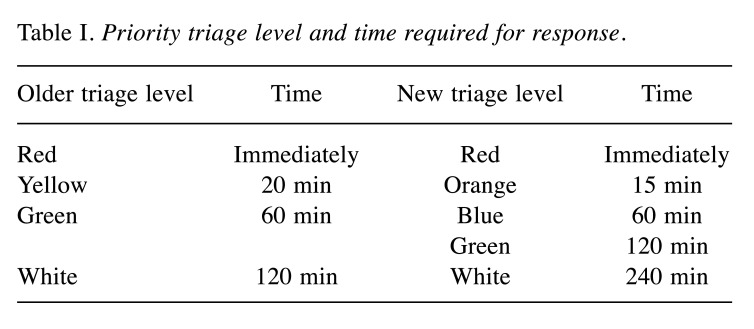
Triage system. The Triage system was introduced in the emergency departments in Italy in 2001. Patients were categorized in four priority levels according to the severity of their status. Patients assigned to the red level require immediate response, cases assigned to yellow, green and white levels require assessment within 20, 60, 120 minutes, respectively (5).
As of August 2019, in order to reduce of emergency departments overcrowding, the NHS implemented a new triage score system. Patients were categorized in five priority levels.
Red level requires immediate response, orange level requires urgent response within 15 min, patients assigned with blue, green and white levels require assessment within 60, 120 and 140 min, respectively (6).
Due to the different triage systems that were in place during the studying period, blue and green levels of the new score system were considered as green priority level of the older system, as described in Table I.
Table I. Priority triage level and time required for response.
Statistical analysis. All data were codified into the EXCEL database (Microsoft, Washington, DC, USA). For continuous variables, we calculated means and ranges. T test was used to determine whether there were significant differences between the two groups. Categorical data were recorded in numbers and percentages. Analysis was performed using the Fisher’s exact test. Different surgical procedures were classified as dichotomous variables and analyzed with fisher exact test. Variables with assigned p-values <0.05 were considered statistically significant. All the statistical analyses were performed in SPSS statistical package version 23.0 (SPSS Inc., Chicago, IL, USA).
Results
During the lockdown phase, a total of 318 patients (Lockdown group) were admitted to our surgical emergency department, with a reduction of 84.45% compared to the 2044 cases of the equivalent period in 2019 (Pre-Lockdown2019 group). In comparison with the Pre-Lockdown2020 group (n=1573) there was a reduction of 79.78%.
Age and sex were comparable between the groups without a statistically significant difference.
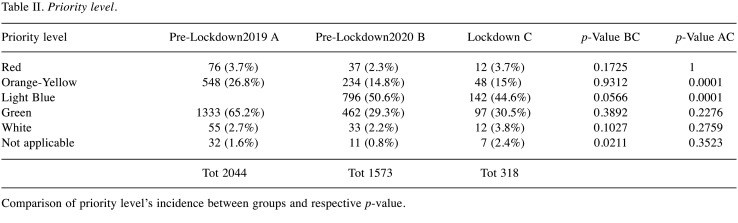
In the Lockdown group, priority level distribution was comparable with that in the Pre-Lockdown2020 group (Table I). Differently, orange priority level was higher (26.8%) in the Pre-Lockdown2019 group compared with the Lockdown group (15%, p=0.0001). Other priority levels and their respective p-values are resumed in Table II.
Table II. Priority level.
Comparison of priority level’s incidence between groups and respective p-value.
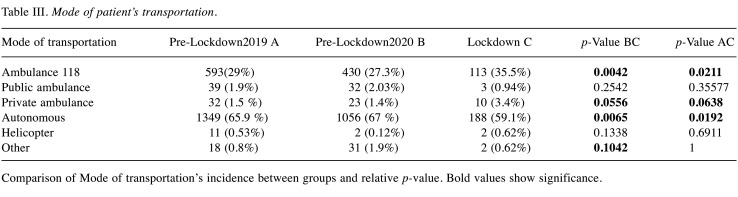
The use of ambulance transport to the emergency department was higher during the lockdown ,39.6% of the cases versus 32.5% and 30.8% of the 2019 and Pre-Lockdown2020 group with p=0.012 and p=0.002, respectively. The autonomous mode of transport to the emergency room was decreased in the Lockdown period as shown in Table III. This reduction showed a statistically significant difference between Lockdown group (59.1%) and the Pre-Lockdown2019 group (32.5%) and the Pre-Lockdown2020 group (30.8%), p-values were 0.019 and 0.006, respectively.
Table III. Mode of patient’s transportation.
Comparison of Mode of transportation’s incidence between groups and relative p-value. Bold values show significance.
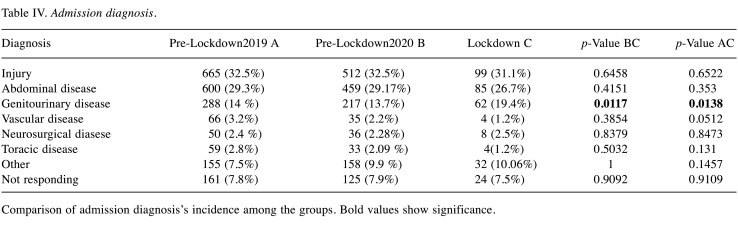
Admission diagnoses were comparable among the groups, except for urinary and vascular disease. During lockdown, the incidence of surgical emergency access for urinary diseases was 19.4% versus 13.7% in the Pre-Lockdown2020 group and 14% in Pre-Lockdown2019 group. Both differences were statistically significant with p-values of 0.011 and 0.013, respectively. Conversely, the incidence of vascular disease was lower in the Lockdown group, 1.2% versus Pre-Lockdown2019 and Pre-Lockdown2020 group which exhibited incidence of 2.2% and 3.2%, respectively, without statistically significant differences. Other admission diagnoses in the groups and their relative p-values are presented in Table IV.
Table IV. Admission diagnosis.
Comparison of admission diagnosis’s incidence among the groups. Bold values show significance.
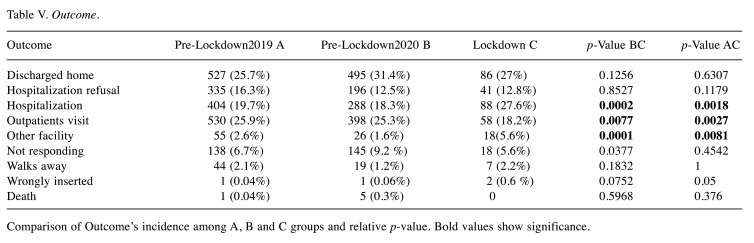
Among emergency patient’s outcome during the Lockdown, the incidence of hospitalization was higher (27.6%) when compared with the Pre-Lockdown2019 group (19.7%) and the Pre-Lockdown2020 (18.3%) groups, showing a statistically significant difference (p=0.001 and p<0.00,1, respectively). Incidence of transfer to other facility was also higher in the Lockdown group compared to the Pre-Lockdown2019 and the Pre-Lockdown2020 groups (Table V) with p-values of <0.001 and 0.008, respectively. Other emergency patient’s outcomes and their relative p-values are presented in Table V. None of these showed a statistically significant difference except for the discharging of patients to be followed in outpatient visits. We observed a reduction in this type of discharge during the lockdown with p-values of 0.007 and 0.002, respectively, among the Pre-Lockdown2020 and the Pre-Lockdown2019 group groups.
Table V. Outcome.
Comparison of Outcome’s incidence among A, B and C groups and relative p-value. Bold values show significance.
WT decreased significantly during lockdown with mean time of 33.2 min. This reduction was statistically significant (p<0.0001) compared with the Pre-Lockdown2020 and the Pre-Lockdown2019 groups which showed mean WT of 132.9 and 125.7 min, respectively. TT was also reduced during the COVID period; mean value of 360.3 min. Among the Pre-Lockdown2020 and Pre-Lockdown2019 groups, TT was 510.3 and 565.2 min, respectively, and both had a p-value <0.0001.
Discussion
Since the beginning of the lockdown we observed a clear reduction in the absolute number of accesses to the surgical emergency department compared to the same period in 2019 and the period immediately preceding the COVID19 era. This trend had previously been reported in an analysis of the Lazio region during the first 3 months of 2020 (7). In that study, the authors reported a reduction of approximately 21.5% (7). The peak of the reduction was reported in the first weeks of March, around 70%. Our results confirmed this trend with a reduction of around 85% and 75% compared to the Pre-Lockdown2019 and the beginning of 2020 periods, respectively (7,8).
In our study, we observed a reduction in the incidence rate of the yellow priority level during the Lockdown when compared with the Pre-Lockdown2019 period. Differently, we observed a corresponding increase of the green priority level rate during the new score period. We could attribute this discrepancy to the difference between the triage systems during the different periods (5,6).
In addition, the percentage of patients arriving to the surgical emergency department with health vehicles during the Lockdown was higher. This data is comparable with that data reported in the Lazio study during the first weeks of March (7). On the one hand, we had an increase in emergency access by ambulance and on the other, we had a reduction in autonomous access during the lockdown. This change was observed, in correspondence with the ordinances that limited access to emergency services only for serious and non-deferrable conditions (2). Furthermore, this result was confirmed by the marked decrease in emergency access. This suggests a tendency to avoid resorting to emergency department for symptoms that can be managed through other levels of regional assistance instead of territorial (7).
Admission diagnosis in the COVID19 era presented that a higher percentage of patients admitted to emergency department due to urinary disease and disorders. This relative increase is probably attributable to the fact that signs such as hematuria or urinary retention can frighten patients (9). Also, major pains like renal colic may have pushed patients to go to hospital instead of managing the symptoms with the care of the local health system (10,11).
Incidence of access for abdominal disease was not affected by the lockdown probably due to its strong impact on patients (12-14).
Many studies have reported a reduction of trauma, especially of severe ones (7,15,16). This decrease can be attributed to the reduction of movements with own vehicles and outdoor sports activities, which are among the main risk factors for traumatic events (17). In our study this reduction was not very evident. Probably due to the fact that we included mild trauma such as small domestic accidents as well. In fact, these injuries were more frequent during the lockdown, considering both adults and children (18-21).
A mild reduction in admission for vascular disease or neurosurgical disorders were also observed. Contrarily, severe reductions of emergency admissions were reported in the literature for cerebrovascular disease and myocardial infarction (7-22). These data are not comparable as most of these patients are evaluated in different departments of our hospital.
In the COVID19 era, we reported an increase in hospitalization following an emergency access. This can be explained by the fact that there have been fewer accesses for potentially delayable diseases (7).
According to the ordinances that limited access to health services only for serious and non-deferrable conditions, we observed a reduction in the discharge of patients to be followed with outpatient visits (2). This may have contributed, on the one hand, to the increase in the rate of hospitalizations, on the other, to delays in treatments (23). The incidence rate of patients transferred to other facilities was aslo higher during the Lockdown. this may be due to the fact that our facility was turned into a COVID-Hospital (3).
The reduction of WT is related to the decreased number emergency department access during the Lockdown. Indeed, in the last few years, emergency departments experienced overcrowding with long waiting times (4). For health professionals, working in overcrowding conditions can have an impact on their psychophysical state (24). In addition, long WT and emergency department overcrowding could discourage patients, especially frail ones, from using this emergency service (25).
TT was also reduced during the COVID19 era. This is probably due to the greater number of transfers and rapid hospitalization of patients in order to avoid facility overcrowding and to reduce the risk of patient’s infections during this emergency period.
The identification of the mechanism that led to the reduction of surgical emergency admissions to our department is beyond the scope of our study. It is worth considering the hypothesis that some patients may have gone to other No-COVID19 hospitals. From the analysis carried out in the Lazio Region, no significant variations were observed between the number of emergency accesses, for unrelated-COVID pathologies, between the COVID-19 and no-COVID19 facilities (7). Probably, some patients had turned to the territorial healthcare system. Other patients, due to COVID19 anxiety may have avoided accessing to treatments (25). It would be interesting to evaluate the outcome and fatality rates of these patients. We could observe a reduction of improper access to the emergency room, while seeing an increase in patients who died at home.
Conclusion
We observed a clear reduction of accesses to the surgical emergency department during the lockdown. Implementing the use of the territorial systems and avoidance of overcrowding of the Emergency Departments could be beneficial for reducing waiting times and improving the quality of treatments for patients. Furthermore, in the event of a new epidemic, it will certainly be necessary to be ready and consider that a number of patients may not have access to treatment due to the fear of infection and the consequences to their health.
Conflicts of Interest
The Authors declare no conflicts of interest regarding this study.
Authors’ Contributions
Study conception and design: Vanni Gianluca, Leonardo Palombi, Pellicciaro Marco, Legramante Jacopo Maria, Materazzo Marco, Buonomo Oreste Claudio; Collection and analysis of data: De Andreis Girolamo, Pellicciaro Marco, Cotesta Maria, Materazzo Marco, Santori Framcesca; Inter-pretation of data: Vanni Gianluca, Leonardo Palombi, Buonomo Chiara, Aiello Francesco, Chiocchi Marcello; Critical revision and draft approval: Gianluca Vanni, Jacopo Maria Legramante, Marco Pellicciaro, Gerardo De Carolis, Maria Cotesta, Marco Materazzo, Chiara Buonomo, Francesca Santori, Benedetto Ielpo, Francesco Aiello, Carla Paganelli, Michele Grande, Girolamo De Andreis, Federica Saraceno, Andrea Farinaccio, Marcello Chiocchi, Leonardo Palombi and Oreste Claudio Buonomo.
Acknowledgements
This study was funded by the non-conditional contribution of the Italian Ministry of Health.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA. 2020;2019:25–28. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Ministero della. Available at: http://www.salute.gov.it/portale/home.html [Last accessed Apr 24, 2020]
- 3.Buonomo OC, Materazzo M, Pellicciaro M, Caspi J, Piccione E, Vanni G. Tor Vergata University-Hospital in the beginning of COVID-19-era: Experience and recommendation for breast cancer patients. In Vivo. 2020;34(3 Suppl):1661–1665. doi: 10.21873/invivo.11958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Age.nas.s. Available at: http://pne.agenas.it [Last accessed July 8, 2020]
- 5.Parenti N, Manfredi R, Bacchi Reggiani ML, Sangiorgi D, Lenzi T. Reliability and validity of an Italian four level emergency triage system. Emerg Med J. 2010;27:495–498. doi: 10.1136/emj.2008.070193. [DOI] [PubMed] [Google Scholar]
- 6.Direzione Generale Della Programmazione Sanitaria. Ministero della Salute. Available at: http://www.salute.gov.it/imgs/C_17_notizie_3849_listaFile_itemName_1_file.pdf [Last accessed July 7, 2020]
- 7.Pinarelli L, Colais P, Mataloni F, Cascini S, Nera A, Fuschi D, Farchi S, Polo A, Lacalamita M, Spiga G, Ribaldi , Davoli M. Access to the emergency at times of COVID-19: an analysis of the first three months in the Lazio region. Available at: https://repo.epiprev.it/index.php/download/laccesso-al-prontosoccorso-ai-tempi-del-covid-19-una-analisi-dei-primi-tre-mesinella-regione-lazio/ [Last accessed July 7, 2020] [DOI] [PubMed]
- 8.Aiello F, Gallo Afflitto G, Mancino R, Li JO, Cesareo M, Giannini C, Nucci C. Coronavirus disease 2019 (SARS-CoV-2) and colonization of ocular tissues and secretions: a systematic review. Eye (Lond) 2020;18:1–6. doi: 10.1038/s41433-020-0926-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anselmo A, Iaria G, Pellicciaro M, Sforza D, Parente A, Campisi A, Cacciatore C, Calafiore E, Pisani G, Tisone G. Native nephrectomy in patients with autosomal dominant polycystic kidney disease evaluated for kidney transplantation. Transplant Proc. 2019;51(9):2914–2916. doi: 10.1016/j.transproceed.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Leveridge M, D’Arcy FT, O’Kane D, Ischia JJ, Webb DR, Bolton DM, Lawrentschuk N. Renal colic: current protocols for emergency presentations. Eur J Emerg Med. 2016;23(1):2–7. doi: 10.1097/MEJ.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 11.Sforza D, Parente A, Pellicciaro M, Morabito M, Iaria G, Anselmo A, Lindfors ER, Corrado F, Cacciatore C, Del Fabbro D, Ingrosso G, Tisone G. Prostate cancer recurrence in kidney transplant recipient 15 years after radical prostatectomy: A case report. Transplant Proc. 2019;51(9):2995–2997. doi: 10.1016/j.transproceed.2019.04.098. [DOI] [PubMed] [Google Scholar]
- 12.Ferroni P, Palmirotta R, Spila A, Martini F, Formica V, Portarena I, Del Monte G, Buonomo O, Roselli M, Guadagni F. Prognostic value of carcinoembryonic antigen and vascular endothelial growth factor tumor tissue content in colorectal cancer. Oncology. 2006;71(3-4):176–184. doi: 10.1159/000106072. [DOI] [PubMed] [Google Scholar]
- 13.Ielpo B, Mazzetti C, Venditti D, Buonomo O, Petrella G. A case of metachronous splenic metastasis from renal cell carcinoma after 14 years. Int J Surg. 2010;8(5):353–355. doi: 10.1016/j.ijsu.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Giarratano G, Toscana C, Shalaby M, Buonomo O, Petrella G, Sileri P. Endoscopic pilonidal sinus treatment: Long-term results of a prospective series. JSLS. 2017;21(3):e2017.00043. doi: 10.4293/JSLS.2017.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133(1513):81–88. [PubMed] [Google Scholar]
- 16.Zhen L, Lin T, Zhao ML, Chen H, Chen T, Guo WH, Zhao LY, Liu H, Hu YF, Yu J, Li GX. Management strategy for the resumption of regular diagnosis and treatment in gastrointestinal surgery department during the outbreak of coronavirus disease 2019 (COVID-19) Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23(4):321–326. doi: 10.3760/cma.j.issn.1671-0274.2020-0316-00146. [DOI] [PubMed] [Google Scholar]
- 17.Cassidy JD, Carroll LJ, Peloso PM, Borg J, von Holst H, Holm L, Kraus J, Coronado VG. Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;(43 Suppl):28–60. doi: 10.1080/16501960410023732. [DOI] [PubMed] [Google Scholar]
- 18.CoViD-19, containment and accidents in children’s domestic life. Bull Acad Natl Med. 2020 doi: 10.1016/j.banm.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bressan S, Gallo E, Tirelli F, Gregori D, Da Dalt L. Lockdown: more domestic accidents than COVID-19 in children. Arch Dis Child. 2020 doi: 10.1136/archdischild-2020-319547. [DOI] [PubMed] [Google Scholar]
- 20.Angelico R, Pietrobattista A, Candusso M, Tomarchio S, Pellicciaro M, Liccardo D, Basso MS, Grimaldi C, Saffioti MC, Torroni F, Dall’Oglio L, Torre G, Spada M. Primary prophylaxis for gastrointestinal bleeding in children with biliary atresia and portal hypertension candidates for liver transplantation: a single-center experience. Transplant Proc. 2019;51(1):171–178. doi: 10.1016/j.transproceed.2018.04.074. [DOI] [PubMed] [Google Scholar]
- 21.Pichard R, Kopel L, Lejeune Q, Masmoudi R, Masmejean EH. Impact of the Corona Virus Disease 2019 lockdown on hand and upper limb emergencies: experience of a referred university trauma hand centre in Paris, France centre in Paris, France. Int Orthop. 2020;2:1–5. doi: 10.1007/s00264-020-04654-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C, Società Italiana di Cardiologia and the CCU Academy investigators group Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;15:ehaa409. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vanni G, Pellicciaro M, Materazzo M, Palombi L, Buonomo OC. Breast cancer diagnosis in coronavirus-era: alert from Italy. Front Oncol. 2020;10:938. doi: 10.3389/fonc.2020.00938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vanni G, Materazzo M, Santori F, Pellicciaro M, Costesta M, Orsaria P, Cattadori F, Pistolese CA, Perretta T, Chiocchi M, Meucci R, Lamacchia F, Assogna M, Caspi J, Granai AV, DE Majo A, Chiaravalloti A, D’Angelillo MR, Barbarino R, Ingallinella S, Morando L, Dalli S, Portarena I, Altomare V, Tazzioli G, Buonomo OC. The effect of coronavirus (COVID-19) on Breast Cancer Teamwork: A multicentric survey. In Vivo. 2020;34(3):1685–1694. doi: 10.21873/invivo.11962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vanni G, Materazzo M, Pellicciaro M, Ingallinella S, Rho M, Santori F, Cotesta M, Caspi J, Makarova A, Pistolese CA, Buonomo OC. Breast cancer and COVID-19: The effect of fear on patients’ decision-making process. In Vivo. 2020;34(3 Suppl):1651–1659. doi: 10.21873/invivo.11957. [DOI] [PMC free article] [PubMed] [Google Scholar]