Abstract
Background
The COVID-19 pandemic is favoring digital transitions in many industries and in society as a whole. Health care organizations have responded to the first phase of the pandemic by rapidly adopting digital solutions and advanced technology tools.
Objective
The aim of this review is to describe the digital solutions that have been reported in the early scientific literature to mitigate the impact of COVID-19 on individuals and health systems.
Methods
We conducted a systematic review of early COVID-19–related literature (from January 1 to April 30, 2020) by searching MEDLINE and medRxiv with appropriate terms to find relevant literature on the use of digital technologies in response to the pandemic. We extracted study characteristics such as the paper title, journal, and publication date, and we categorized the retrieved papers by the type of technology and patient needs addressed. We built a scoring rubric by cross-classifying the patient needs with the type of technology. We also extracted information and classified each technology reported by the selected articles according to health care system target, grade of innovation, and scalability to other geographical areas.
Results
The search identified 269 articles, of which 124 full-text articles were assessed and included in the review after screening. Most of the selected articles addressed the use of digital technologies for diagnosis, surveillance, and prevention. We report that most of these digital solutions and innovative technologies have been proposed for the diagnosis of COVID-19. In particular, within the reviewed articles, we identified numerous suggestions on the use of artificial intelligence (AI)–powered tools for the diagnosis and screening of COVID-19. Digital technologies are also useful for prevention and surveillance measures, such as contact-tracing apps and monitoring of internet searches and social media usage. Fewer scientific contributions address the use of digital technologies for lifestyle empowerment or patient engagement.
Conclusions
In the field of diagnosis, digital solutions that integrate with traditional methods, such as AI-based diagnostic algorithms based both on imaging and clinical data, appear to be promising. For surveillance, digital apps have already proven their effectiveness; however, problems related to privacy and usability remain. For other patient needs, several solutions have been proposed, such as telemedicine or telehealth tools. These tools have long been available, but this historical moment may actually be favoring their definitive large-scale adoption. It is worth taking advantage of the impetus provided by the crisis; it is also important to keep track of the digital solutions currently being proposed to implement best practices and models of care in future and to adopt at least some of the solutions proposed in the scientific literature, especially in national health systems, which have proved to be particularly resistant to the digital transition in recent years.
Keywords: COVID-19, SARS-CoV-2, pandemic, digital heath, review, literature, mitigate, impact, eHealth
Introduction
Background
The COVID-19 pandemic, like all global crises in human history, is causing unprecedented health and economic disruptions in many countries. However, at the same time, this new situation is favoring the transition to digital solutions in many industries and in society as a whole. One example of this transition is education [1]; this entire sector, from primary schools to universities, has developed new strategies for teaching remotely, shifting from lectures in classrooms to live conferencing or web-based courses [2]. Similarly, health care organizations have responded to the COVID-19 pandemic through the rapid adoption of digital solutions and advanced technology tools. During a pandemic, digital technology can mitigate or even solve many challenges, thus improving health care delivery. Digital tools have been applied to address acute needs that have arisen as a direct or indirect consequence of the pandemic (eg, apps for patient tracing, remote triage emergency services). However, many of the solutions that have been developed and implemented during the emergency could be consolidated in the future, contributing to the definition and adoption of new digital models of care.
The list of new digital solutions is rapidly growing [3]. In addition to “video visits,” these options include email and mobile phone apps as well as use of wearable devices, chatbots, artificial intelligence (AI)–powered diagnostic tools, voice-interface systems, and mobile sensors such as smart watches, oxygen monitors, or thermometers. A new category of service is the oversight of persons in home quarantine and large-scale population surveillance. Telemedicine and remote consultation have already proven to be effective at a time when access to health services for patients who do not have COVID-19 or for patients with nonacute COVID-19 is prevented, impeded, or postponed. In fact, according to Keesara et al [4], instead of using a model structured on the historically necessary model of in-person interactions between patients and their clinicians through a face-to-face model of care, current health care services and patient assistance can be guaranteed remotely through digital technologies.
Before the COVID-19 pandemic, it was expected that digital transformation in health care would be as disruptive as the transformations seen in other industries. However, as discussed by Hermann et al [5] and affirmed by Perakslis [6], “despite new technologies being constantly introduced, this change had yet to materialize.” The spread of COVID-19 appears to have finally provided an ineludibly sound reason to fully embrace the digital transformation. Moreover, simulations show that many countries will probably face several waves of contagion, and new lockdowns will probably occur [7]. Therefore, it has become necessary to review the digital technologies that have been used during the emergency period and consider them for continued use over time or cyclically in the event of recurring outbreaks.
Goal of This Study
According to Hermann et al [5], digital technologies can be categorized based on the patient needs they address in health care: diagnosis, prevention, treatment, adherence, lifestyle, and patient engagement. We argue that it is necessary to understand which digital technologies have been adopted to face the COVID-19 crisis and whether and how they can still be useful after the emergency phase. To achieve this, it is crucial to cover as many aspects as possible of digital technology use in health care in response to the COVID-19 pandemic.
The aim of this study is therefore to describe the digital solutions that have been reported in the early scientific literature to mitigate the impact of COVID-19 on individuals and health systems.
Methods
Literature Search
We conducted a systematic review of the early scientific literature, following the Preferred Reporting Items for Systematic Reviews (PRISMA) approach [8], to include quantitative and qualitative studies using diverse designs to describe which digital solutions have been reported to respond and mitigate the effects of the COVID-19 pandemic. This review focuses on health research, which includes biomedical, epidemiological, clinical, public health, and health systems research.
The initial search was implemented on May 11, 2020, and was limited to the timespan from January 1 to April 30, 2020. The search query consisted of terms considered adequate by the authors to review the literature on the use of digital technologies in response to COVID-19. Therefore, we searched the MEDLINE database using the following search terms and database-appropriate syntax:
(“COVID-19”[All Fields] OR “COVID-2019”[All Fields] OR “severe acute respiratory syndrome coronavirus 2”[Supplementary Concept] OR “severe acute respiratory syndrome coronavirus 2”[All Fields] OR “2019-nCoV”[All Fields] OR “SARS-CoV-2”[All Fields] OR “2019nCoV”[All Fields] OR ((“Wuhan”[All Fields] AND (“coronavirus”[MeSH Terms] OR “coronavirus”[All Fields])) AND (2019/12[PDAT] OR 2020[PDAT]))) AND (digital[Title/Abstract] OR technology[Title/Abstract])]
We also searched the COVID-19/SARS-CoV-2 section of medRxiv, a preprint server for health science papers that have yet to be peer-reviewed, for studies related to digital technologies, using the search string COVID-19 digital technology with the same timespan restriction applied to the MEDLINE search.
The search strategies and eligibility criteria used are provided in Multimedia Appendix 1.
Study Selection and Data Collection Process
We included articles for review if they were studies with original data or results referring to digital tools or interventions for COVID-19 and if they addressed the needs of patients or health care systems in the evaluation.
An article was excluded if it was not a study with original results; it did not focus on digital solutions for COVID-19; the full text was not available; or it was not written in English.
A two-stage screening process was used to assess the relevance of the identified studies. For the first level of screening, only the title and abstract were reviewed to preclude waste of resources in procuring articles that did not meet the minimum inclusion criteria. The titles and abstracts of the initially identified studies were checked by two independent investigators (DG and EB). For the second level of screening, all citations deemed relevant after the title and abstract screening were procured for subsequent review of the full-text article.
A spreadsheet in Excel (Microsoft Corporation) was developed to extract study characteristics such as the paper title, journal, publication date, type of technology, and patient needs addressed. In particular, we categorized the retrieved papers according to patient needs (diagnosis, prevention, treatment, adherence, lifestyle, and patient engagement). For the categorization of patient needs, we adapted the definition by Hermann et al [5], which reports the concept of “customer needs addressed” by the health care industry, to identify the patient health needs addressed by digital technology during the early phase of the COVID-19 pandemic.
The definition of patient needs is reported in Table 1. We added “surveillance” as an additional patient need to those identified by Hermann et al [5] given the importance of early identification and confinement of patients with COVID-19 to preserve population health, and a category of “other” to include any needs that were not considered in the previous categories.
Table 1.
Definitions of the patient needs addressed by digital technologies.
| Patient need | Definition |
| Diagnosis | The process of determining which disease or condition explains a person's symptoms and signs [9] |
| Prevention | Preventing the occurrence of a disease (eg, by reducing risk factors) or by halting a disease and averting resulting complications after its onset [10] |
| Adherence | The degree to which a patient correctly follows medical advice [11] |
| Treatment | The use of an agent, procedure, or regimen, such as a drug, surgery, or exercise, in an attempt to cure or mitigate a disease [12] |
| Lifestyle | Adoption and sustaining behaviors that can improve health and quality of life [13] |
| Patient engagement | Actively involving people in their health and health care [14] |
| Surveillance | The continuous, systematic collection, analysis, and interpretation of health-related data needed for the planning, implementation, and evaluation of public health practice [15] |
| Other | All patient needs, addressed by digital technology, which are not included in the previous categories |
We built a scoring rubric by cross-classifying the patient needs addressed by the technology (or technologies) reported in each article with the type of technology itself. We relied on the report “Assessing the impact of digital transformation of Health Services” by the Expert Panel on Effective Ways of Investigating in Health (EXPH) of the European Commission [16] to classify the types of digital technologies (ie, AI, big data, chatbots, electronic health records [EHRs], mobile apps, robotics, sensors, telehealth, and telemedicine), integrating it with terms found within the analyzed articles when necessary (ie, blockchain, Internet of Things [IoT], internet search engines, social media, and mobile tracing).
We also extracted information and classified each technology reported by the selected articles according to health care system targets, grade of innovation, and scalability to other geographical areas. To do this, we also relied on the classifications and definitions reported by the EXPH (Table 2) [16].
Table 2.
Classification of digital technologies and health services.
| Classification category | Definition | |
| Health care system targets | ||
|
|
Clients/patients | Members of the public who are potential or current users of health services, including caregivers. |
|
|
Health care providers | Members of the health care workforce who deliver health services. |
|
|
Health systems/resource managers | Systems and managers involved in the administration and oversight of public health systems. Interventions within this category reflect managerial functions related to supply chain management, health financing, and human resource management. |
|
|
Data services | Crosscutting functionality to support a wide range of activities related to data collection, management, use, and exchange. |
| Grade of innovation | ||
|
|
Supporting | Digital services or technologies that can be used to support old or established technologies for all or some health care system targets. These technologies may support or facilitate the performance of existing technologies. |
|
|
Complementing | Digital services or technologies that can be used in addition to old or established technologies for all or some health care system targets. These technologies may strengthen or enhance the performance of existing technologies. |
|
|
Substituting | Digital services or technologies that may replace old or established technologies for all or some health care system targets. |
|
|
Innovating | New digital services or technologies that may offer new possibilities that previously were not available for all or some health care system targets. These disruptive technologies may represent a new entry into the market. |
| Scalability to other geographical areas | ||
|
|
Not possible | Technologies strictly bonded to the context in which they were developed. |
|
|
Local | Technologies whose scalability is limited to a local context (ie, regional or national context) for normative, legislative, ethical, or technical reasons. |
|
|
Global | Technologies that do not present barriers to scalability that would prevent their possible global adoption. |
Some of the analyzed articles described multiple technologies. For these articles, we reported all the health care system targets addressed by the proposed technologies. However, we found it impractical to assign different grades of innovation and scalability for each technology reported. Therefore, we chose to report only the highest grade of innovation or scalability assigned to the technologies within each article (eg, innovating>substituting>complementing>supporting).
Two of the authors (DG and EB) independently classified all identified articles in the predefined categories. Any disagreements were resolved through discussion and consensus between the two reviewers. If disagreement persisted, another reviewer (GC) was called as a tiebreaker.
Given the characteristics of this literature review, which aims to describe proposed digital solutions, and the nature and design of the included studies, assessments of the risk of bias and the study quality were not possible and therefore were not performed.
Results
Literature Search
The search identified 269 articles (174 from PubMed and 95 from medRxiv), of which 124 full-text articles were assessed and included in the review after screening (Figure 1).
Figure 1.
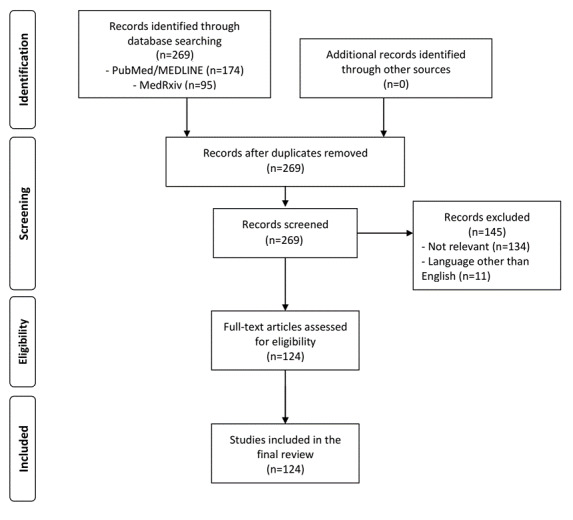
Preferred Reporting Items for Systematic Reviews (PRISMA) literature review flowchart.
Study Selection and Data Collection Process
Out of the 124 selected articles, 65 (52.4%) addressed the use of digital technologies for diagnosis (Figure 2), 46 (37.1%) addressed surveillance, 46 (37.1%) addressed prevention, 38 (30.6%) addressed treatment, 15 (12.1%) addressed adherence, 12 (9.7%) addressed lifestyle, 11 (8.9%) addressed patient engagement, and 6 (4.8%) addressed other purposes. Considering the share of peer-reviewed articles, we found that for diagnosis, 39/65 articles (60%) were peer-reviewed; for surveillance, 29/46 (63%); for prevention, 30/46 (65%); for treatment, 33/38 (87%); for adherence, 15/15 (100%); for lifestyle, 11/12 (92%); for patient engagement, 11/11 (100%); and for other, 5 (83.3%).
Figure 2.
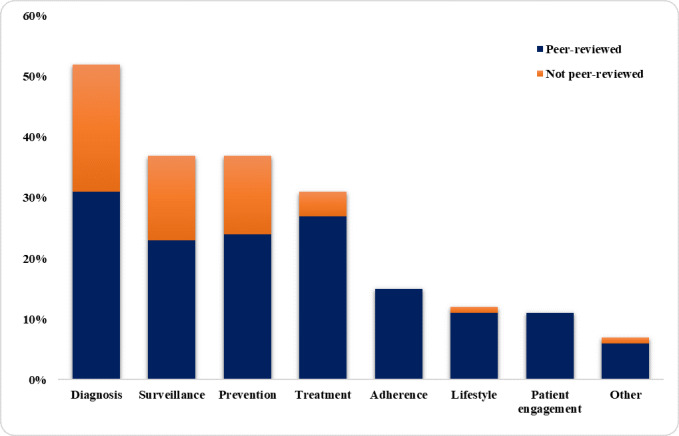
Frequency of appearance of each patient need within the 124 selected articles and the share of peer-reviewed articles for each need. The total percentage is higher than 100 because some articles include technologies used to address more than one patient need.
In Table 3, we provide an extract of the characteristics of the included articles. An extended version of this table is provided in the supplementary material (Table S1, Multimedia Appendix 2).
Table 3.
Articles included in the literature review with the main characteristics of each analyzed paper.
| ID | Reference | Health care system targets | Grade of innovation | Scalability |
| 1 | Zhai et al [17] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 2 | Wang W et al [18] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 3 | Wang et al [19] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 4 | Yan et al [20] | Clients/patients, health care providers | Supporting | Global |
| 5 | Hou et al [21] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 6 | Feng et al [22] | Health care providers | Complementing | Global |
| 7 | Jin et al [23] | Health care providers | Complementing | Global |
| 8 | Torous et al [24] | Clients/patients, health care providers, health systems/resource managers | Innovating | Global |
| 9 | Wang et al [25] | Health care providers | Complementing | Global |
| 10 | Zheng et al [26] | Health care providers | Complementing | Global |
| 11 | Galbiati et al [27] | Health care providers, health systems/resource managers | Supporting | Global |
| 12 | Bai et al [28] | Health care providers | Complementing | Global |
| 13 | Ienca et al [29] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 14 | Ting et al [30] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 15 | Hua et al [31] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 16 | Fu et al [32] | Health care providers | Complementing | Global |
| 17 | Zhou et al [33] | Health care providers | Complementing | Global |
| 18 | Lin et al [34] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 19 | Ferretti et al [35] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 20 | Calton et al [36] | Clients/patients, health care providers | Innovating | Global |
| 21 | Lin et al [37] | Health care providers | Complementing | Global |
| 22 | Mashamba-Thompson et al [38] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 23 | Salako et al [39] | Clients/patients, health care providers | Innovating | Local |
| 24 | Hernández et al [40] | Clients/patients, health systems/resource managers | Innovating | Local |
| 25 | Ohannessian et al [41] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 26 | Shanlang et al [42] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 27 | Turer et al [43] | Clients/patients, health care providers | Innovating | Global |
| 28 | Keesara et al [4] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 29 | Her [44] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 30 | Klum et al [45] | Clients/patients, health care providers | Supporting | Global |
| 31 | Calvo et al [46] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 32 | Dandekar et al [47] | Health systems/resource managers, data services | Innovating | Global |
| 33 | Drew et al [48] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 34 | Segal et al [49] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 35 | Hassanien et al [50] | Health care providers | Complementing | Global |
| 36 | Martin et al [51] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 37 | Yasaka et al [52] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 38 | Medford et al [53] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 39 | Salg et al [54] | Health systems/resource managers, data services | Complementing | Local |
| 40 | Abhari et al [55] | Health systems/resource managers, data services | Innovating | Global |
| 41 | Jarynowski et al [56] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 42 | Stommel et al [57] | Clients/patients, health care providers | Complementing | Global |
| 43 | Judson et al [58] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 44 | Ćosić et al [59] | Clients/patients, health care providers | Innovating | Local |
| 45 | Grange et al [60] | Clients/patients, health care providers | Innovating | Global |
| 46 | Castiglioni et al [61] | Clinets/patients, health care providers | Complementing | Global |
| 47 | Serper et al [62] | Clients/patients, health care providers | Innovating | Global |
| 48 | Robbins et al [1] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 49 | Crump [63] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 50 | Punn et al [64] | Health systems/resource managers, data services | Innovating | Global |
| 51 | Myers et al [65] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 52 | Noonan et al [66] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 53 | Loebet et al [67] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 54 | Price et al [68] | Health care providers | Innovating | Local |
| 55 | Vaishya et al [69] | Health care providers | Complementing | Global |
| 56 | Stubblefield et al [70] | Health care providers | Complementing | Global |
| 57 | Yuan et al [71] | Clients/patients, data services | Innovating | Local |
| 58 | Pollock et al [72] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 59 | Mahmood et al [73] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 60 | Gallotti et al [74] | Clients/patients, data services | Innovating | Local |
| 61 | Ren et al [75] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 62 | Goldschmidt [76] | Clients/patients, health care providers | Innovating | Global |
| 63 | Al-karawi et al [77] | Health care providers | Complementing | Global |
| 64 | Kumar et al [78] | Health care providers | Complementing | Global |
| 65 | Garg et al [79] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 66 | Kuziemski et al [80] | Health systems/resource managers, data services | Innovating | Local |
| 67 | Jakhar et al [81] | Clients/patients, health care providers | Innovating | Local |
| 68 | Marasca et al [82] | Clients/patients, health care providers | Innovating | Local |
| 69 | Bulchandani et al [83] | Clients/patients, health systems/resource managers, data services | Innovating | Local |
| 70 | Green et al [84] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 71 | Nagra et al [85] | Clients/patients, health care providers | Innovating | Global |
| 72 | O'Connor et al [86] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 73 | Wittbold et al [87] | Clients/patients, health care providers | Innovating | Local |
| 74 | Hightow et al [88] | Clients/patients, health care providers | Innovating | Local |
| 75 | Bonavita et al [89] | Clients/patients, health care providers | Innovating | Local |
| 76 | Wosik et al [90] | Clients/patients, HO | Innovating | Global |
| 77 | Yan et al [91] | Health care providers, health systems/resource managers, data services | Supporting | Global |
| 78 | Lin et al [92] | Clients/patients, health care providers, health systems/resource managers, data services | Supporting | Not possible |
| 79 | Kummitha [93] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 80 | Abbas et al [94] | Health care providers, data services | Complementing | Global |
| 81 | Ardabili et al [95] | Health systems/resource managers, data services | Supporting | Global |
| 82 | Zhang et al [96] | Clients/patients, health care providers, | Supporting | Global |
| 83 | Hart et al [97] | Clients/patients, health care providers | Innovating | Global |
| 84 | Parikh et al [98] | Clients/patients, health care providers | Innovating | Global |
| 85 | Rahman et al [99] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 86 | Alwashmi Hart [100] | Clients/patients, health care providers, health systems/resource managers, data services | Complementing | Global |
| 87 | Sedov et al [101] | Health care providers, health systems/resource managers, data services | Complementing | Global |
| 88 | Mahapatra et al [102] | Health care providers; health systems/resource managers | Innovating | Global |
| 89 | Azizy et al [103] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 90 | Madurai et al [104] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Global |
| 91 | Park et al [105] | Clients/patients, health care providers, health systems/resource managers, data services | Innovating | Local |
| 92 | Negrini et al [106] | Clients/patients, health care providers | Complementing | Global |
| 93 | Tanaka et al [107] | Clients/patients, health care providers | Complementing | Global |
| 94 | Randhawa et al [108] | Data services | Innovating | Global |
| 95 | Javaid et al [109] | Clients/patients, health care providers, health systems/resource managers, data services | Supporting | Global |
| 96 | Kyhlstedt et al [110] | Clients/patients, health care providers, health systems/resource managers, data services | Supporting | Global |
| 97 | Barbosa et al [111] | Health systems/resource managers, data services | Innovating | Global |
| 98 | Blake et al [112] | Clients/patients, health systems/resource managers | Supporting | Global |
| 99 | Reeves et al [113] | Clients/patients, health care providers, health systems/resource managers, data services | Substituting | Global |
| 100 | Khan et al [114] | Clients/patients, | Substituting | Global |
| 101 | Whelan et al [115] | Clients/patients, health care providers, health systems/resource managers | Complementing | Global |
| 102 | Meinert et al [116] | Clients/patients, health care providers, data services | Innovating | Global |
| 103 | Ekong et al [117] | Clients/patients, health care providers, health systems/resource managers | Supporting | Local |
| 104 | Pérez Sust et al [118] | Clients/patients, health care providers, health systems/resource managers, data services | Complementing | Global |
| 105 | Kim et al [119] | Clients/patients, health care providers, health systems/resource managers, data services | Complementing | Global |
| 106 | Krukowski et al [120] | Clients/patients, health care providers, health systems/resource managers | Complementing | Global |
| 107 | Liu et al [121] | Health care providers, health systems/resource managers | Supporting | Global |
| 108 | Vaid et al [122] | Health care providers, health systems/resource managers | Complementing | Local |
| 109 | Lee [123] | Clients/patients, health care providers | Supporting | Global |
| 110 | Ramsetty et al [3] | Clients/patients, health care providers, health systems/resource managers | Complementing | Global |
| 111 | Tarek et al [124] | Health systems/resource managers | Complementing | Global |
| 112 | Awasthi et al [125] | Health care providers, health systems/resource managers | Supporting | Global |
| 113 | Khan et al [126] | Health care providers, health systems/resource managers | Supporting | Global |
| 114 | Husnayain et al [127] | Health care providers, health systems/resource managers | Supporting | Global |
| 115 | Weemaes et al [128] | Health care providers, health systems/resource managers, data services | Innovating | Local |
| 116 | Espinoza et al [129] | Clients/patients, health care providers, health systems/resource managers | Innovating | Global |
| 117 | Shweta et al [130] | Health care providers, health systems/resource managers, data services | Complementing | Global |
| 118 | Brat et al [131] | Health care providers, health systems/resource managers, data services | Supporting | Local |
| 119 | Hegde et al [132] | Clients/patients, health care providers | Innovating | Global |
| 120 | Tobias et al [133] | Clients/patients, health care providers, health systems/resource managers, data services | Supporting | Local |
| 121 | Compton et al [134] | Clients/patients, health care providers, health systems/resource managers | Complementing | Global |
| 122 | Smith et al [135] | Health care providers, health systems/resource managers | Complementing | Local |
| 123 | Kalteh et al [136] | Health care providers, health systems/resource managers, data services | Supporting | Global |
| 124 | Woo et al [137] | Clients/patients, health care providers | Complementing | Global |
In Table 4, we cross-classify the use of technology and the type of technology. As an example, 24 articles describe the use of AI tools for the diagnosis of COVID-19, while 34 describe the use of telehealth or telemedicine for treatment purposes. All included articles and related analyses are reported in Multimedia Appendix 2 (Table S1).
Table 4.
Cross-classification of the published studies by the type of technology and the patient needs addressed by the technology.
| Technology | Diagnosis | Surveillance | Prevention | Treatment | Adherence | Lifestyle | Patient engagement | Other | ||||||||
|
|
n | Refsa | n | Refs | n | Refs | n | Refs | n | Refs | n | Refs | n | Refs | n | Refs |
| Artificial intelligence | 24 | [20,22,23,25,26, 28,30,32,33,38, 48,50,54,61,69, 70,77,78,94,100, 108,109,122,130] |
12 | [30,38,48,64,93, 95,100,104,109, 116,122,126] |
11 | [30,38,47,55,64, 95,100,109, 116,122,126] |
2 | [102,109] | 1 | [109] | 1 | [109] | 1 | [116] | 4 | [80, 104, 108, 125] |
| Big data analytics | 6 | [30,54,100,109, 118, 122] |
11 | [19,29,30,34,42, 93,100,109, 122,126, 136] |
12 | [19,30,34,42,55, 100,109,118, 122,124, 126,136] |
2 | [109,118] | 2 | [109,118] | 3 | [40, 109, 118] |
0 | N/Ab | 2 | [111, 128] |
| Blockchain | 2 | [30,38] | 2 | [30,38] | 2 | [30,38] | 0 | N/A | 0 | N/A | 0 | N/A | 0 | N/A | 0 | N/A |
| Chatbot | 3 | [51,58,129] | 0 | N/A | 1 | [51] | 0 | N/A | 0 | N/A | 0 | N/A | 0 | N/A | 0 | N/A |
| Electronic health records | 7 | [1,60,91,113,118, 130,131] |
5 | [1,37,91,113,133] | 4 | [113,118,131,133] | 5 | [1,60,91, 113,118] |
1 | [118] | 1 | [118] | 0 | N/A | 0 | N/A |
| Internet of Things | 3 | [92,103,109] | 5 | [92,93,99, 104,109] |
3 | [92,103,109] | 2 | [103,109] | 1 | [109] | 1 | [109] | 0 | N/A | 1 | [104] |
| Internet search engines, social media | 1 | [1] | 8 | [1,18,21,31,42, 56,74,127] |
3 | [18,42,127] | 1 | [1] | 0 |
|
1 | [53] | 0 | N/A | 1 | [121] |
| Mobile app | 8 | [85,87,88,91,92, 96,100,110] |
8 | [18,91-93,96,100, 110,116] |
9 | [18,71,88,92,96, 100,110,115,116] |
3 | [85,88,91] | 3 | [88,112, 115] |
2 | [71, 112] |
3 | [112,115, 116] |
0 | N/A |
| Mobile tracing | 6 | [48,49,73,100, 110,118] |
14 | [31,35,44,46,48, 49,52,73,83,100, 105,110,117,119] |
6 | [44,73,83,100,110, 118] |
2 | [73,118] | 1 | [118] | 1 | [118] | 0 | N/A | 0 | N/A |
| Robotics, mechanical tools, drones, sensors, wearable devices | 5 | [45,101,109, 114,132] |
3 | [101,104,109] | 3 | [101,109,114] | 2 | [27,109] | 3 | [45,109, 114] |
1 | [109] | 1 | [114] | 1 | [104] |
| Telehealth, tele-medicine | 29 | [1,17,39,57,59, 60,62,63,65-67, 72,73,75,76,81, 84-91,100,103, 107,118,120] |
7 | [1,73,75,89-91, 100] |
18 | [24,39,41, 43,71,73, 75,88-90, 100,103,115, 118,120,134, 135,137] |
34 | [1,3,17, 24,36,39, 57,59,60, 62,63,65 -68,72,73, 75,76,79, 84-86,88, 91,97,98, 103,106,107, 118,123,134, 135] |
11 | [24,82,88, 97,98,115, 118,120,134, 135,137] |
8 | [24, 65, 66, 71, 76, 79, 118, 137] |
8 | [59,76, 82,97, 115,120, 123,134] |
0 | N/A |
aRefs: references.
bN/A: not applicable.
Characteristics of the Digital Health Technologies Favored by the COVID-19 Pandemic
Given the heterogeneity of the included technologies and solutions, we summarized the findings through a narrative synthesis. In fact, some patient needs share the same technology for health issues, which can be considered superimposable (eg, prevention and surveillance are often addressed by the same technology, such as mobile surveillance apps); this is also evident from Table 4, where many articles report technologies addressing more than one health need. Accordingly, in the following paragraphs, we describe the digital technologies and solutions starting from the patient needs they are designed to mitigate. We then discuss some of the retrieved articles that we deemed most interesting for each patient need.
Diagnosis
In the early scientific literature, digital solutions and innovative technologies were mainly proposed for the diagnosis of COVID-19. In particular, within the reviewed articles, we identified numerous suggestions of the use of AI-powered tools for the diagnosis and screening of SARS-CoV-2 or COVID-19, as reported in Table 4 [20,22,23,25,26,28,30,32,33, 38,48,50,54,61,69,70,77,78,94,100,108,109,122,130]. Most studies propose the adoption of AI tools based on the use of computed tomography (CT) data [23,28,33]. For example, Zhou et al [33] developed and validated an integrated deep learning framework on chest CT images for autodetection of novel coronavirus pneumonia (NCP), with particular focus on differentiating NCP from influenza pneumonia (IP), ensuring prompt implementation of isolation. Their AI model potentially provides an accurate early diagnostic tool for NCP. This type of diagnostic tool can be useful during the pandemic, especially when tests such as nucleic acid test kits are short in supply, which is a common problem during outbreaks. However, performing CT scans as a screening method presents significant limitations, considering the risks of both radiation exposure and operator or machine-type dependence [25].
In addition to these studies, many authors proposed AI-powered diagnostic tools for COVID-19 that are not based on CT scan data [22,51,58]. Feng et al [22] developed and validated a diagnosis aid model without CT images for early identification of suspected COVID-19 pneumonia on admission in adult fever patients and made the validated model available via a web-based triage calculator that must be supplied with clinical and serological data (eg, age, % monocytes, interleukin-6). Similarly, Martin et al [51] proposed a chatbot and a symptom-to-disease digital health assistant that can differentiate more than 20,000 diseases with an accuracy of more than 90%. The authors tested the accuracy of the digital health assistant to identify COVID-19 using a set of diverse clinical cases combined with case reports of COVID-19, and they reported that the digital health assistant can accurately distinguish COVID-19 in 96% of clinical cases.
A further innovative digital technology proposed to support the diagnosis of COVID-19 is blockchain (or distributed ledger) technology. In one study [38], the authors recommended low-cost blockchain and AI-coupled self-testing and tracking systems for COVID-19 and other emerging infectious diseases in low- and middle-income countries. They developed a low-cost blockchain app that requests a user’s personal identifier before opening pretesting instructions. Following testing, the user uploads their results to the app, and the blockchain and AI systems enable the transfer to alert the outbreak surveillance. These types of solutions can also be of interest in high-income countries.
Another interesting digital tool proposed for the diagnosis and triage of patients is chatbots. Chatbots are applications that provide information through conversation-like interactions with users; they can be used for a broad range of purposes in health care (eg, patient triage, clinical decision support for providers, directing patients and staff to appropriate resources, and mental health applications). Chatbots can help evolve triage and screening processes in a scalable manner [129] and, as institutions become increasingly familiar with these tools, can be repurposed in the future for other public health emergencies as well as for more standard care uses.
Prevention and Surveillance
Our literature review suggests that digital technologies can be useful for COVID-19 diagnosis as well as for implementing prevention and surveillance measures.
Judson et al [58] deployed the Coronavirus Symptom Checker, a digital patient-facing self-triage and self-scheduling tool, to address the COVID-19 pandemic; it provides patients with 24-hour access to personalized recommendations, and it improves ambulatory surge capacity through self-triage, self-scheduling, and avoidance of unnecessary in-person care. The majority of patients who used this checker did not make any further contact with the health care system during subsequent days.
Another topic of paramount importance in the context of health care digitalization is epidemiological surveillance. Our review highlights that prevention and surveillance are often considered together in the scientific literature, given that “prevention of COVID-19” can be intended as “prevention of further spread,” which is mainly achieved through surveillance. For the COVID-19 pandemic, surveillance definitely overlaps with prevention, as the risk of infection can be reduced by applying a successful surveillance plan and controlling the interactions between infected persons and the healthy population.
A study by Ferretti et al [35] analyzed the key parameters of the COVID-19 epidemic spread to estimate the contributions of different transmission routes and determine the requirements for successful case isolation and contact tracing. The viral spread is too rapid to be contained by manual contact tracing. The solution is the implementation of a contact-tracing app that creates a temporary record of proximity events between individuals and immediately alerts recent close contacts of diagnosed cases and prompts them to self-isolate. An important limitation of this type of tracing technology is that to achieve its goal, it must be used by a significant portion of the population.
An example of successful use of a mobile app for contact tracing is the app that the Chinese government implemented in Wuhan [31]. Quick response (QR) code–based screening was implemented in Hubei Province to monitor people’s movement, especially on public transportation. Using big data and mobile phones, three color codes were attributed to each citizen: green (safe), yellow (need to be cautious), and red (cannot enter). A similar tool was implemented in Taiwan [19]. In fact, through Taiwan citizens’ household registration system and foreigners’ entry cards, it was possible to track individuals at high risk of COVID-19 infection because of their recent history of travel to affected areas. If an individual was identified as high risk when in quarantine, they were monitored electronically through their mobile phone. Then, the Entry Quarantine System was launched: through the completion of a health declaration form (requiring the scan of a QR code that leads to a web-based form, either prior to departure from or upon arrival at a Taiwan airport), travelers could receive rapid immigration clearance.
Our literature review suggests that another meaningful way to control the spread of an epidemic is through monitoring and surveillance of internet searches and social media usage. Wang et al [18] used WeChat, a Chinese social media platform, to plot daily data on the frequencies of keywords related to SARS-CoV-2. The authors found that the frequencies of several keywords related to COVID-19 showed abnormal behavior during a period ahead of the outbreak in China, and they stated that social media can offer a new approach to early detection of disease outbreaks. Similarly, the Italian words for “cough” and “fever” were searched in Google Trends to find useful insights to predict the COVID-19 outbreak in Italy, showing a significant association with hospital admissions or deaths in the two following weeks [138]. These two papers show that tracking public health information from web-based search engines may have a role in the prediction of future COVID-19 outbreaks, complementarily to traditional public health surveillance systems.
Furthermore, a technology that can aid the automatic, decentralized, and remote collection of data for surveillance purposes is the IoT. In [99], an IoT-based smart disease surveillance system showed potential to control the pandemic. In fact, with most people using smartphones and wearable technologies and having internet access, this technology can help limit the spread of the pandemic through the collection and analysis of default gathered data.
Although its potential is irrefutable, the technology behind surveillance and contact tracing apps raises many concerns; as discussed by Calvo et al [46], the most obvious concern is “surveillance creep,” which occurs when a surveillance tool developed for a precise goal (in the case of China and Taiwan, an app to monitor people’s movement) remains in use after the crisis is solved. Privacy must be a primary concern for policy makers and a key challenge for designers and engineers who design digital tools for epidemic control. As already outlined in previous work by Carullo [139], in the European Union, applications to combat COVID-19 should avoid processing personal data whenever possible. The General Data Protection Regulation (GDPR) [140] dictates the principle of privacy by default, that is, “by default, only personal data which are necessary for each specific purpose of the processing are processed.” In this regard, it should be reminded that according to the GDPR, data are “personal” only when and insofar they allow the identification of a natural person. Therefore, the processing of data, including clinical data, that cannot in any way identify a natural person does not involve personal data. Therefore, any privacy concerns are completely ruled out. To be compliant with this principle, a preferable approach is therefore to trace the spread of the virus, and therefore alert users, without collecting any personal data. A promising example in this direction was provided by Yasaka et al [52], who described an open-source proof-of-concept app for contact tracing that does not require registration or the divulgation of any private data, such as location. Instead, this tool uses an ingenious “checkpoint” system that allows users to create a peer-to-peer network of interactions and to determine if they have been exposed to any risk of infection; diagnosis of infection can be entered into the app, and the data are transferred to a central server but remain anonymous.
Although the aforementioned articles addressed surveillance and prevention in outpatients and the general population, an interesting point of view on inpatient surveillance comes from the study by Lin et al [37]. This paper describes a prospective active surveillance system with information technology (IT) services (ie, using a surveillance algorithm based on data from EHRs) to identify hospital inpatients whose pneumonia did not show marked improvement with antibiotic treatment and to alert the primary care medical teams on a daily basis. Similarly, EHR-based rapid screening processes, laboratory testing, clinical decision support, reporting tools, and patient-facing technology related to COVID-19 can be implemented using the EHR to build multiple COVID-19–specific tools to support outbreak management, including scripted triaging, electronic check-in, standard ordering and documentation, secure messaging, real-time data analytics, and telemedicine capabilities [113].
In the field of prevention, other important digital technologies proposed in the literature include telemedicine and telehealth. Telemedicine is not always applicable in emergencies, and many patients with COVID-19 may need to go to the hospital to receive higher level care. For this purpose, Turer et al [43] proposed using electronic personal protective equipment (ePPE) to protect staff (ie, prevent infection of health care workers) and conserve traditional PPE while providing rapid access to emergency care for low-risk patients during the COVID-19 pandemic. A very similar solution has been proposed by Wittbold et al [87]. They explored digital care delivery methods to reduce unnecessary exposure and conserve PPE through the deployment of iPads equipped with an app to evaluate and manage patients in a quaternary care academic and level one trauma center. Therefore, ePPE has been proved to be potentially applicable to settings such as emergency medical services, medical wards, and intensive care units.
Treatment and Adherence
Telemedicine and telehealth technologies are also used to increase patient adherence and for treatment purposes. Torous et al [24] describe the potential of digital health to increase access to and quality of mental health care by exploring the success of telehealth during the present crisis and how technologies such as apps can soon play larger roles. Telehealth is seen as a useful solution to deliver mental health care in general [141] and during social distancing and quarantine periods. In addition, digital therapy programs can be offered through courses of evidence-based therapies or using augmented reality and virtual reality systems. As another example, Calton et al [36] deliver some useful advice on the implementation of telemedicine to deliver specialty palliative care in the homes of seriously ill patients and their families. The authors state that the digital divide must be taken into account. Patients require access to an internet connection and to a digital device suited for videoconferencing. For older people or those less familiar with technology, it may be necessary to identify a caregiver as a “technological liaison” for the patient. To create a successful telemedicine-based treatment environment, many critical factors must be considered, including workforce training, high-quality evidence, digital equity, and patient adherence.
Lifestyle and Patient Engagement
In the early literature responding to the COVID-19 pandemic, fewer scientific contributions addressed the use of digital technologies for lifestyle empowerment or patient engagement. This is probably due to the current phase of the pandemic, which has conditioned scientific research to focus primarily on aspects related to more acute patient needs. However, some articles can be found. For instance, Krukowski et al [120] addressed the issue of remote obesity management through telehealth methodologies such as electronic scales to remotely measure patients’ weight and to maintain their engagement toward healthy lifestyles.
Discussion
Principal Results
Although SARS-CoV-2 is causing a pandemic worldwide, it is also favoring the rapid adoption of digital solutions and advanced technology tools in health care. On the one hand, physicians and health systems may need to track large populations of patients on a daily basis for surveillance purposes [4]. On the other hand, they may need rapid diagnostic tests for COVID-19 screening, to reduce the workload, and to enable patients to receive early diagnoses and timely treatments. This can also be achieved with the help of digital technologies, which were already available in different industries before the current crisis. These tools have now been quickly implemented in health care due to the pandemic [104].
In this systematic review of the early scientific literature in response to COVID-19, we describe numerous digital solutions and technologies addressing several patient and health care needs. The constantly updated scientific literature is a source of important ideas and suggestions for finding innovative solutions that guarantee patient care during and possibly after the COVID-19 crisis.
In the field of diagnosis, digital solutions that integrate with the traditional methods of clinical, molecular or serological diagnosis, such as AI-based diagnostic algorithms based both on imaging and clinical data, seem promising.
For surveillance, digital apps have already proven their effectiveness [142-144]; however, problems related to privacy and usability remain [145]. For other patient needs, several solutions have been proposed, such as telemedicine or telehealth tools. These tools have long been available; however, this historical moment could actually favor their definitive large-scale adoption.
The fact that the digital technologies proposed in the analyzed scientific literature mainly address the fields of diagnosis, prevention, and surveillance probably reflects the emergency phase of the COVID-19 pandemic. As time passes, well-known digital tools could be proposed for different purposes and patient needs, such as adherence, lifestyle, and patient engagement, which are considered to be important determinants of patient health [146] despite the lower attention paid to them in the early scientific literature.
In addition to the patient needs addressed by digital technologies, our review sheds light on the most used digital technology tools. Given the early phase of the pandemic and its reflection on the articles included in this review, the technologies that have shown to be more easily and quickly implementable can be also considered as the most scalable. In fact, the speed with which these technologies have been deployed demonstrates their ease of adoption and manageability in many different contexts, despite their deployment during the course of a pandemic. Many of these solutions have demonstrated a technical, economic, regulatory and usability weight that is sufficiently low to allow their rapid and effective use, at least during the emergency phase. Among these solutions, we report AI tools for diagnosis, big data analytics and mobile tracing for surveillance and prevention, and telemedicine and telehealth, which have proved to be transversal tools for diagnosis, prevention, and treatment.
We advocate that many of the digital technologies that have been quickly implemented in this emergency phase can also be adopted in the following phases of the pandemic, as also stated by Fagherazzi et al [147]. However, this implementation is easier said than done. According to the article by Keesara et al [4], “Covid-19 and Health Care’s Digital Revolution,” in the context of the digital leap caused by the COVID-19 pandemic in the United States (and worldwide) [4], while private corporations and education institutions have made rapid transitions to remote work and videoconferencing, the health care system is still lagging behind in adopting digital solutions. This is mainly due to the fact that clinical workflows and economic incentives have been developed for a face-to-face model of care that, during this pandemic, contributes to the spread of the virus to uninfected patients who are seeking medical care. In addition to the history of health care policies, there are limiting factors to the implementation of tools such as telemedicine, including a legal framework that is not yet fully designed to regulate the use of innovative IT systems in health care, as well as an inadequate information and communications technology infrastructure and an obsolete reimbursement and payment structure.
Many countries are facing these regulatory issues: the challenges for digital health have become a global issue in the public health response to COVID-19 and future outbreaks. Digital tools such as telemedicine should indeed be integrated into international and national guidelines for public health preparedness, alongside the definition of national regulations and funding frameworks in the context of public health emergencies. To switch to new digital models of care, increasing the digital expertise of health care professionals and educating the population are fundamental issues. Moreover, by implementing a data-sharing mechanism, digitally collected and stored data will be a precious tool for epidemiological surveillance that, as discussed earlier, is fundamental in controlling the epidemic spread. Lastly, to describe and assess the impact of digital tools during outbreaks, scientific evaluation frameworks should be defined [41].
Limitations
This literature review presents some limitations. First, the research was conducted in a period of epidemiological emergency. Thus, the number of daily publications is high, and it is difficult to keep up to date. As a result, we have been forced to select articles in a reduced time span, potentially missing some studies and including studies that have yet to be peer-reviewed. Secondly, due to the design of the review, the search could not be fully comprehensive, as it was conducted exclusively on the MEDLINE database and medRxiv to preserve both time and resources; however, PubMed/MEDLINE is reported to be the primary database used by health science faculties [148], and medRxiv is one of the main repositories of COVID-19 research [149]. Finally, the articles and concepts included in this preliminary review certainly need to be integrated at the end of this international emergency phase.
Conclusions
The COVID-19 pandemic is favoring the implementation of digital solutions with unprecedented speed and impact. It is therefore recommended to keep track of the ideas and solutions being proposed today to implement best practices and models of care tomorrow and to be prepared for future national and international emergencies. It is worth taking advantage of the impetus provided by the crisis we are currently experiencing to implement at least some of the solutions proposed in the scientific literature, especially in national health systems, which in recent years have proved to be particularly resistant to the digital transition.
Acknowledgments
The authors declare that they have not received any specific funding.
Abbreviations
- AI
artificial intelligence
- CT
computed tomography
- EHR
electronic health record
- ePPE
electronic personal protective equipment
- EXPH
Expert Panel on Effective Ways of Investigating in Health
- GDPR
general data protection regulation
- IoT
Internet of Things
- IP
influenza pneumonia
- IT
information technology
- NCP
novel coronavirus pneumonia
- PRISMA
Preferred Reporting Items for Systematic Reviews
- QR code
quick response code
Appendix
Eligibility criteria and search strategy.
Table S1. Articles included in the literature review.
Footnotes
Authors' Contributions: DG and EB conceived and designed the work; reviewed the literature and independently classified all identified articles in the predefined categories; acquired, analyzed, and interpreted the data; and wrote the manuscript. GC acted as a tiebreaker in case of disagreement between DG and EB during the classification of the identified articles. GC and AGN helped with the analyses, interpreted the data, and reviewed the manuscript. MPL and MPF interpreted the data and reviewed and edited the final manuscript in collaboration with DG and EB for intellectual content. All authors have read and approved the final version of the manuscript.
Conflicts of Interest: None declared.
References
- 1.Robbins T, Hudson S, Ray P, Sankar S, Patel K, Randeva H, Arvanitis TN. COVID-19: A new digital dawn? Digital Health. 2020;6:2055207620920083. doi: 10.1177/2055207620920083. https://journals.sagepub.com/doi/10.1177/2055207620920083?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gewin V. Five tips for moving teaching online as COVID-19 takes hold. Nature. 2020 Apr;580(7802):295–296. doi: 10.1038/d41586-020-00896-7. [DOI] [PubMed] [Google Scholar]
- 3.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020 Jul 01;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. http://europepmc.org/abstract/MED/32343813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keesara S, Jonas A, Schulman K. Covid-19 and Health Care's Digital Revolution. N Engl J Med. 2020 Jun 04;382(23):e82. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- 5.Herrmann M, Boehme P, Mondritzki T, Ehlers JP, Kavadias S, Truebel H. Digital Transformation and Disruption of the Health Care Sector: Internet-Based Observational Study. J Med Internet Res. 2018 Mar 27;20(3):e104. doi: 10.2196/jmir.9498. https://www.jmir.org/2018/3/e104/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perakslis ED. Strategies for delivering value from digital technology transformation. Nat Rev Drug Discov. 2017 Feb;16(2):71–72. doi: 10.1038/nrd.2016.265. [DOI] [PubMed] [Google Scholar]
- 7.Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020 May 22;368(6493):860–868. doi: 10.1126/science.abb5793. http://europepmc.org/abstract/MED/32291278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009 Aug 18;151(4):264–9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135. https://www.acpjournals.org/doi/10.7326/0003-4819-151-4-200908180-00135?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed. [DOI] [PubMed] [Google Scholar]
- 9.Langlois JP. Making a Diagnosis. In: Mengel MB, Holleman WL, Fields SA, editors. Fundamentals of Clinical Practice, 2nd Edition. Boston, MA: Springer; 2002. pp. 197–217. [Google Scholar]
- 10.Clarke EA. What is Preventive Medicine? Can Fam Physician. 1974 Nov;20(11):65–8. http://europepmc.org/abstract/MED/20469128. [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . Adherence to Long-Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 12.Drexler M, Institute of Medicine . What You Need to Know About Infectious Disease. Washington, DC: National Academies Press; 2010. Prevention and Treatment. [PubMed] [Google Scholar]
- 13.Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA. 2010 Jul 14;304(2):202–3. doi: 10.1001/jama.2010.903. [DOI] [PubMed] [Google Scholar]
- 14.James j. Patient Engagement. Health Affairs. 2013. Feb 14, [2020-11-03]. https://www.healthaffairs.org/do/10.1377/hpb20130214.898775/full/
- 15.Public health surveillance. World Health Organization. [2020-11-03]. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/en/
- 16.European Commission . Assessing the Impact of Digital Transformation of Health Services: Report of the Expert Panel on effective ways of investing in Health (EXPH) Luxembourg: Publications Office of the European Union; 2019. Nov, p. ckz185.769. [Google Scholar]
- 17.Zhai Y, Wang Y, Zhang M, Gittell JH, Jiang S, Chen B, Cui F, He X, Zhao J, Wang X. From Isolation to Coordination: How Can Telemedicine Help Combat the COVID-19 Outbreak? medRxiv. doi: 10.37473/dac/10.1101/2020.02.20.20025957. Preprint posted online on February 23, 2020. [DOI] [Google Scholar]
- 18.Wang W, Wang Y, Zhang X, Li Y, Jia X, Dang S. WeChat, a Chinese social media, may early detect the SARS-CoV-2 outbreak in 2019. medRxiv. doi: 10.1101/2020.02.24.20026682. Preprint posted online on February 26, 2020. [DOI] [Google Scholar]
- 19.Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: Big Data Analytics, New Technology, and Proactive Testing. JAMA. 2020 Apr 14;323(14):1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 20.Yan L, Zhang H, Xiao Y, Wang M, Sun C, Liang J, Li S, Zhang M, Guo Y, Xiao Y, Tang X, Cao H, Tan X, Huang N, Jiao B, Luo A, Cao Z, Xu H, Yuan Y. Prediction of criticality in patients with severe Covid-19 infection using three clinical features: a machine learning-based prognostic model with clinical data in Wuhan. medRxiv. doi: 10.1101/2020.02.27.20028027. Preprint posted online on March 03, 2020. [DOI] [Google Scholar]
- 21.Hou Z, Du F, Jiang H, Zhou X, Lin L. Assessment of public attention, risk perception, emotional and behavioural responses to the COVID-19 outbreak: social media surveillance in China. medRxiv. doi: 10.1101/2020.03.14.20035956. Preprint posted online on March 17, 2020. [DOI] [Google Scholar]
- 22.Feng C, Huang Z, Wang L, Chen X, Zhai Y, Zhu F, Chen H, Wang Y, Su X, Huang S, Tian L, Zhu W, Sun W, Zhang L, Han Q, Zhang J, Pan F, Chen L, Zhu Z, Xiao H, Liu Y, Liu G, Chen W, Li T. A Novel Triage Tool of Artificial Intelligence Assisted Diagnosis Aid System for Suspected COVID-19 Pneumonia in Fever Clinics. SSRN Journal. doi: 10.2139/ssrn.3551355. Preprint posted online on March 19, 2020. [DOI] [Google Scholar]
- 23.Jin S, Wang B, Xu H, Wei L, Zhao W, Hou X, Ma W, Xu Z, Zheng Z, Sun W, Lan L, Zhang W, Mu X, Shi C, Wang Z, Lee J, Jin Z, Lin M, Jin H, Zhang L, Guo J, Zhao B, Ren Z, Wang S, You Z, Dong J, Wang X, Wang J, Xu W. AI-assisted CT imaging analysis for COVID-19 screening: Building and deploying a medical AI system in four weeks. medRxiv. doi: 10.1101/2020.03.19.20039354. Preprint posted online on March 23, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Torous J, Jän Myrick K, Rauseo-Ricupero N, Firth J. Digital Mental Health and COVID-19: Using Technology Today to Accelerate the Curve on Access and Quality Tomorrow. JMIR Ment Health. 2020 Mar 26;7(3):e18848. doi: 10.2196/18848. https://mental.jmir.org/2020/3/e18848/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang S, Zha Y, Li W, Wu Q, Li X, Niu M, Wang M, Qiu X, Li H, Yu H, Gong W, Bai Y, Li L, Zhu Y, Wang L, Tian J. A fully automatic deep learning system for COVID-19 diagnostic and prognostic analysis. medRxiv. doi: 10.1101/2020.03.24.20042317. Preprint posted online on March 26, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng C, Deng X, Fu Q, Zhou Q, Feng J, Ma H, Liu W, Wang X. Deep Learning-based Detection for COVID-19 from Chest CT using Weak Label. medRxiv. doi: 10.1101/2020.03.12.20027185. Preprint posted online on March 26, 2020. [DOI] [Google Scholar]
- 27.Galbiati C, Bonivento W, Caravati M, Razeti M, DeCecco S, Fiorillo G, Gabriele F, Tartaglia R, Razeto A, Sablone D, Scapparone E, Testera G, Rescigno M, Franco D, Kochanek I, Kendziora C, Pordes SH, Wang H, Ianni A, McDonald A, Tosatti LM, Dinon T, Malosio M, Minuzzo D, Zardoni A, Prini A. Mechanical Ventilator Milano (MVM): A Novel Mechanical Ventilator Designed for Mass Scale Production in Response to the COVID-19 Pandemics. medRxiv. doi: 10.1101/2020.03.24.20042234. Preprint posted online on March 27, 2020. [DOI] [Google Scholar]
- 28.Bai X, Fang C, Zhou Y, Bai S, Liu Z, Xia L, Chen Q, Xu Y, Xia T, Gong S, Xie X, Song D, Du R, Zhou C, Chen C, Nie D, Qin L, Chen W. Predicting COVID-19 Malignant Progression with AI Techniques. SSRN Journal. doi: 10.2139/ssrn.3557984. Preprint posted online on March 31, 2020. [DOI] [Google Scholar]
- 29.Ienca M, Vayena E. On the responsible use of digital data to tackle the COVID-19 pandemic. Nat Med. 2020 Apr;26(4):463–464. doi: 10.1038/s41591-020-0832-5. http://europepmc.org/abstract/MED/32284619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ting DSW, Carin L, Dzau V, Wong TY. Digital technology and COVID-19. Nat Med. 2020 Apr;26(4):459–461. doi: 10.1038/s41591-020-0824-5. http://europepmc.org/abstract/MED/32284618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hua J, Shaw R. Corona Virus (COVID-19) "Infodemic" and Emerging Issues through a Data Lens: The Case of China. Int J Environ Res Public Health. 2020 Mar 30;17(7):2309. doi: 10.3390/ijerph17072309. https://www.mdpi.com/resolver?pii=ijerph17072309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fu M, Yi S, Zeng Y, Ye F, Li Y, Dong X, Ren YD, Luo L, Pan JS, Zhang Q. Deep Learning-Based Recognizing COVID-19 and other Common Infectious Diseases of the Lung by Chest CT Scan Images. medRxiv. doi: 10.1101/2020.03.28.20046045. Preprint posted online on March 30, 2020. [DOI] [Google Scholar]
- 33.Zhou M, Chen Y, Wang D, Xu Y, Yao W, Huang J, Jin X, Pan Z, Tan J, Wang L, Xia Y, Zou L, Xu X, Wei J, Guan M, Feng J, Zhang H, Qu J. Improved deep learning model for differentiating novel coronavirus pneumonia and influenza pneumonia. medRxiv. doi: 10.1101/2020.03.24.20043117. Preprint posted online on March 30, 2020. [DOI] [Google Scholar]
- 34.Lin C, Braund WE, Auerbach J, Chou J, Teng J, Tu P, Mullen J. Policy Decisions and Use of Information Technology to Fight COVID-19, Taiwan. Emerg Infect Dis. 2020 Jul;26(7):1506–1512. doi: 10.3201/eid2607.200574. doi: 10.3201/eid2607.200574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferretti L, Wymant C, Kendall M, Zhao L, Nurtay A, Abeler-Dörner L, Parker M, Bonsall D, Fraser C. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020 May 08;368(6491):eabb6936. doi: 10.1126/science.abb6936. http://europepmc.org/abstract/MED/32234805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Calton B, Abedini N, Fratkin M. Telemedicine in the Time of Coronavirus. J Pain Symptom Manage. 2020 Jul;60(1):e12–e14. doi: 10.1016/j.jpainsymman.2020.03.019. http://europepmc.org/abstract/MED/32240756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin C, Cheng C, Lu P, Shih D, Hung C, Lo H, Tsai M, Hung J. Active surveillance for suspected COVID-19 cases in inpatients with information technology. J Hosp Infect. 2020 Jun;105(2):197–199. doi: 10.1016/j.jhin.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mashamba-Thompson TP, Crayton ED. Blockchain and Artificial Intelligence Technology for Novel Coronavirus Disease-19 Self-Testing. Diagnostics (Basel) 2020 Apr 01;10(4):198. doi: 10.3390/diagnostics10040198. https://www.mdpi.com/resolver?pii=diagnostics10040198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salako O, Okunade K, Allsop M, Habeebu M, Toye M, Oluyede G, Fagbenro G, Salako B. Upheaval in cancer care during the COVID-19 outbreak. Ecancermedicalscience. 2020;14:ed97. doi: 10.3332/ecancer.2020.ed97. http://europepmc.org/abstract/MED/32269597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hernández-García Ignacio, Giménez-Júlvez Teresa. Assessment of Health Information About COVID-19 Prevention on the Internet: Infodemiological Study. JMIR Public Health Surveill. 2020 Apr 01;6(2):e18717. doi: 10.2196/18717. https://publichealth.jmir.org/2020/2/e18717/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ohannessian R, Duong TA, Odone A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill. 2020 Apr 02;6(2):e18810. doi: 10.2196/18810. https://publichealth.jmir.org/2020/2/e18810/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lin S, Ma C, Lin R, Huang J, Xu R, Yuan A. Research on the Influence of Information Diffusion on the Transmission of the Novel Coronavirus (COVID-19) medRxiv. doi: 10.1101/2020.03.31.20048439. Preprint posted online on April 02, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Turer RW, Jones I, Rosenbloom ST, Slovis C, Ward MJ. Electronic personal protective equipment: A strategy to protect emergency department providers in the age of COVID-19. J Am Med Inform Assoc. 2020 Jun 01;27(6):967–971. doi: 10.1093/jamia/ocaa048. http://europepmc.org/abstract/MED/32240303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Her M. How Is COVID-19 Affecting South Korea? What Is Our Current Strategy? Disaster Med Public Health Prep. 2020 Apr 03;:1–3. doi: 10.1017/dmp.2020.69. http://europepmc.org/abstract/MED/32241325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Klum M, Urban M, Tigges T, Pielmus A, Feldheiser A, Schmitt T, Orglmeister R. Wearable Cardiorespiratory Monitoring Employing a Multimodal Digital Patch Stethoscope: Estimation of ECG, PEP, LVETand Respiration Using a 55 mm Single-Lead ECG and Phonocardiogram. Sensors (Basel) 2020 Apr 04;20(7):2033. doi: 10.3390/s20072033. https://www.mdpi.com/resolver?pii=s20072033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Calvo R, Deterding C, Ryan R. Health surveillance during covid-19 pandemic. BMJ. 2020 Apr 06;369:m1373. doi: 10.1136/bmj.m1373. [DOI] [PubMed] [Google Scholar]
- 47.Dandekar R, Barbastathis G. Quantifying the effect of quarantine control in Covid-19 infectious spread using machine learning. medRxiv. doi: 10.1101/2020.04.03.20052084. Preprint posted online on April 06, 2020. [DOI] [Google Scholar]
- 48.Drew Da, Nguyen Lh, Steves Cj, Wolf j, Spector TD, Chan AT, COPE Consortium Rapid implementation of mobile technology for real-time epidemiology of COVID-19. medRxiv. doi: 10.1101/2020.04.02.20051334. Preprint posted online on April 06, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Segal E, Zhang F, Lin X, King G, Shalem O, Shilo S, Allen WE, Alquaddoomi F, Altae-Tran H, Anders S, Balicer R, Bauman T, Bonilla X, Booman G, Chan AT, Cohen O, Coletti S, Davidson N, Dor Y, Drew DA, Elemento O, Evans G, Ewels P, Gale J, Gavrieli A, Geiger B, Grad YH, Greene CS, Hajirasouliha I, Jerala R, Kahles A, Kallioniemi O, Keshet A, Kocarev L, Landua G, Meir T, Muller A, Nguyen LH, Oresic M, Ovchinnikova S, Peterson H, Prodanova J, Rajagopal J, Rätsch G, Rossman H, Rung J, Sboner A, Sigaras A, Spector T, Steinherz R, Stevens I, Vilo J, Wilmes P, CCC (Coronavirus Census Collective) Building an international consortium for tracking coronavirus health status. medRxiv. doi: 10.1101/2020.04.02.20051284. Preprint posted online on April 06, 2020. [DOI] [PubMed] [Google Scholar]
- 50.Hassanien AS, Mahdy LS, Ezzat KS, Elmousalami HS, Ella HJ. Automatic X-ray COVID-19 Lung Image Classification System based on Multi-Level Thresholding and Support Vector Machine. medRxiv. doi: 10.1101/2020.03.30.20047787. Preprint posted online on April 06, 2020. [DOI] [Google Scholar]
- 51.Martin A, Nateqi J, Gruarin S. An artificial intelligence based first-line defence against COVID-19: digitally screening citizens for risks via a chatbot. bioRxiv. doi: 10.1101/2020.03.25.008805. Preprint posted online on April 06, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yasaka TM, Lehrich BM, Sahyouni R. Peer-to-Peer Contact Tracing: Development of a Privacy-Preserving Smartphone App. JMIR Mhealth Uhealth. 2020 Apr 07;8(4):e18936. doi: 10.2196/18936. https://mhealth.jmir.org/2020/4/e18936/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Medford R, Saleh S, Sumarsono A, Perl TM, Lehmann CU. An "Infodemic": Leveraging High-Volume Twitter Data to Understand Public Sentiment for the COVID-19 Outbreak. medRxiv. doi: 10.1101/2020.04.03.20052936. Preprint posted online on April 07, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Salg G, Ganten M, Baumhauer M, Heussel C, Kleesiek J. A globally available COVID-19 - Template for clinical imaging studies. medRxiv. doi: 10.1101/2020.04.02.20048793. doi: 10.1101/2020.04.02.20048793. Preprint posted online on April 07, 2020. [DOI] [Google Scholar]
- 55.Abhari R, Marini M, Chokani N. COVID-19 Epidemic in Switzerland: Growth Prediction and Containment Strategy Using Artificial Intelligence and Big Data. medRxiv. doi: 10.1101/2020.03.30.20047472. Preprint posted online on April 07, 2020. [DOI] [Google Scholar]
- 56.Jarynowski A, Wojta-Kempa M, Belik V. Perception of emergent epidemic of COVID-2019 / SARS CoV-2 on the Polish Internet. medRxiv. doi: 10.1101/2020.03.29.20046789. Preprint posted online on April 07, 2020. [DOI] [Google Scholar]
- 57.Stommel WJP, van Goor H, Stommel MWJ. The Impact of Video-Mediated Communication on Closed Wound Assessments in Postoperative Consultations: Conversation Analytical Study. J Med Internet Res. 2020 May 05;22(5):e17791. doi: 10.2196/17791. https://www.jmir.org/2020/5/e17791/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Judson TJ, Odisho AY, Neinstein AB, Chao J, Williams A, Miller C, Moriarty T, Gleason N, Intinarelli G, Gonzales R. Rapid design and implementation of an integrated patient self-triage and self-scheduling tool for COVID-19. J Am Med Inform Assoc. 2020 Jun 01;27(6):860–866. doi: 10.1093/jamia/ocaa051. http://europepmc.org/abstract/MED/32267928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ćosić K, Popović S, Šarlija Marko, Kesedžić I. Impact of Human Disasters and COVID-19 Pandemic on Mental Health: Potential of Digital Psychiatry. Psychiatr Danub. 2020;32(1):25–31. doi: 10.24869/psyd.2020.25. http://www.psychiatria-danubina.com/UserDocsImages/pdf/dnb_vol32_no1/dnb_vol32_no1_25.pdf. [DOI] [PubMed] [Google Scholar]
- 60.Grange ES, Neil EJ, Stoffel M, Singh AP, Tseng E, Resco-Summers K, Fellner BJ, Lynch JB, Mathias PC, Mauritz-Miller K, Sutton PR, Leu MG. Responding to COVID-19: The UW Medicine Information Technology Services Experience. Appl Clin Inform. 2020 Mar;11(2):265–275. doi: 10.1055/s-0040-1709715. http://www.thieme-connect.com/DOI/DOI?10.1055/s-0040-1709715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Castiglioni I, Ippolito D, Interlenghi M, Monti CB, Salvatore C, Schiaffino S, Polidori A, Gandola D, Messa C, Sardanelli F. Artificial intelligence applied on chest X-ray can aid in the diagnosis of COVID-19 infection: a first experience from Lombardy, Italy. medRxiv. doi: 10.1101/2020.04.08.20040907. doi: 10.1101/2020.04.08.20040907. Preprint posted online on April 10, 2020. [DOI] [Google Scholar]
- 62.Serper M, Cubell AW, Deleener ME, Casher TK, Rosenberg DJ, Whitebloom D, Rosin RM. Telemedicine in Liver Disease and Beyond: Can the COVID-19 Crisis Lead to Action? Hepatology. 2020 Aug;72(2):723–728. doi: 10.1002/hep.31276. http://europepmc.org/abstract/MED/32275784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Crump WJ. Telemedicine: Has the Time Really Finally Arrived? J Rural Health. 2020 Apr 11; doi: 10.1111/jrh.12435. http://europepmc.org/abstract/MED/32277729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Punn N, Sonbhadra S, Agarwal S. COVID-19 Epidemic Analysis using Machine Learning and Deep Learning Algorithms. medRxiv. doi: 10.1101/2020.04.08.20057679. Preprint posted online on June 01, 2020. [DOI] [Google Scholar]
- 65.Myers US, Birks A, Grubaugh AL, Axon RN. Flattening the Curve by Getting Ahead of It: How the VA Healthcare System Is Leveraging Telehealth to Provide Continued Access to Care for Rural Veterans. J Rural Health. 2020 Apr 13; doi: 10.1111/jrh.12449. http://europepmc.org/abstract/MED/32282955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Noonan D, Simmons LA. Navigating Nonessential Research Trials During COVID-19: The Push We Needed for Using Digital Technology to Increase Access for Rural Participants? J Rural Health. 2020 Apr 13; doi: 10.1111/jrh.12446. http://europepmc.org/abstract/MED/32282959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, Levin AS. Departmental Experience and Lessons Learned With Accelerated Introduction of Telemedicine During the COVID-19 Crisis. J Am Acad Orthop Surg. 2020 Jun 01;28(11):e469–e476. doi: 10.5435/JAAOS-D-20-00380. http://europepmc.org/abstract/MED/32301818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Price A, Henke L, Maraghechi B, Kim T, Spraker MB, Hugo GD, Robinson CG, Knutson NC. Implementation of a Novel Remote Physician SBRT Coverage Process during the Coronavirus Pandemic. medRxiv. doi: 10.1101/2020.04.09.20059857. Preprint posted online on April 14, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vaishya R, Javaid M, Khan IH, Haleem A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab Syndr. 2020;14(4):337–339. doi: 10.1016/j.dsx.2020.04.012. http://europepmc.org/abstract/MED/32305024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stubblefield J, Hervert M, Causey J, Qualls J, Dong W, Cai L, Fowler J, Bellis E, Walker K, Moore JH, Nehring S, Huang H. Cardiac or Infectious? Transfer Learning with Chest X-Rays for ER Patient Classification. medRxiv. doi: 10.1101/2020.04.11.20062091. doi: 10.1101/2020.04.11.20062091. Preprint posted online on April 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yuan EJ, Hsu C, Lee W, Chen T, Chou L, Hwang S. Where to buy face masks? Survey of applications using Taiwan's open data in the time of coronavirus disease 2019. J Chin Med Assoc. 2020 Jun;83(6):557–560. doi: 10.1097/JCMA.0000000000000325. http://europepmc.org/abstract/MED/32304508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pollock K, Setzen M, Svider PF. Embracing telemedicine into your otolaryngology practice amid the COVID-19 crisis: An invited commentary. Am J Otolaryngol. 2020;41(3):102490. doi: 10.1016/j.amjoto.2020.102490. http://europepmc.org/abstract/MED/32307192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mahmood S, Hasan K, Colder Carras M, Labrique A. Global Preparedness Against COVID-19: We Must Leverage the Power of Digital Health. JMIR Public Health Surveill. 2020 Apr 16;6(2):e18980. doi: 10.2196/18980. https://publichealth.jmir.org/2020/2/e18980/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gallotti R, Valle F, Castaldo N, Sacco P, De Domenico M. Assessing the risks of ?infodemics? in response to COVID-19 epidemics. medRxiv. doi: 10.1101/2020.04.08.20057968. doi: 10.1101/2020.04.08.20057968. Preprint posted online on April 16, 2020. [DOI] [PubMed] [Google Scholar]
- 75.Ren X, Zhai Y, Song X, Wang Z, Dou D, Li Y. The Application of Mobile Telehealth System to Facilitate Patient Information Presentation and Case Discussion. Telemed J E Health. 2020 Jun;26(6):725–733. doi: 10.1089/tmj.2020.0084. [DOI] [PubMed] [Google Scholar]
- 76.Goldschmidt K. The COVID-19 Pandemic: Technology use to Support the Wellbeing of Children. J Pediatr Nurs. 2020;53:88–90. doi: 10.1016/j.pedn.2020.04.013. doi: 10.1016/j.pedn.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Al-karawi D, Al-Zaidi S, Polus N, Jassim S. Machine Learning Analysis of Chest CT Scan Images as a Complementary Digital Test of Coronavirus (COVID-19) Patients. medRxiv. doi: 10.1101/2020.04.13.20063479. Preprint posted online on April 17, 2020. [DOI] [Google Scholar]
- 78.Kumar R, Arora A, Bansal B, Sahayasheela VJ, Buckchash H, Imran J, Narayanan N, Pandian GN, Raman B. Accurate Prediction of COVID-19 using Chest X-Ray Images through Deep Feature Learning model with SMOTE and Machine Learning Classifiers. medRxiv. doi: 10.1101/2020.04.13.20063461. Preprint posted online on April 17, 2020. [DOI] [Google Scholar]
- 79.Garg SK, Rodbard D, Hirsch IB, Forlenza GP. Managing New-Onset Type 1 Diabetes During the COVID-19 Pandemic: Challenges and Opportunities. Diabetes Technol Ther. 2020 Jun;22(6):431–439. doi: 10.1089/dia.2020.0161. [DOI] [PubMed] [Google Scholar]
- 80.Kuziemski M, Misuraca G. AI governance in the public sector: Three tales from the frontiers of automated decision-making in democratic settings. Telecomm Policy. 2020 Jul;44(6):101976. doi: 10.1016/j.telpol.2020.101976. http://europepmc.org/abstract/MED/32313360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jakhar D, Kaur I, Kaul S. Screen mirroring, screen casting and screen sharing during COVID-19: what dermatologists should know. Clin Exp Dermatol. 2020 Aug;45(6):750–751. doi: 10.1111/ced.14247. http://europepmc.org/abstract/MED/32304574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Marasca C, Ruggiero A, Fontanella G, Ferrillo M, Fabbrocini G, Villani A. Telemedicine and support groups could be used to improve adherence to treatment and health-related quality of life in patients affected by inflammatory skin conditions during the COVID-19 pandemic. Clin Exp Dermatol. 2020 Aug;45(6):749. doi: 10.1111/ced.14245. http://europepmc.org/abstract/MED/32304587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bulchandani V, Shivam S, Moudgalya S, Sondhi S. Digital Herd Immunity and COVID-19. medRxiv. doi: 10.1101/2020.04.15.20066720. Preprint posted online on May 26, 2020. [DOI] [PubMed] [Google Scholar]
- 84.Green A, Ruchman S, Katz C, Singer E. Piloting Forensic Tele-Mental Health Evaluations of Asylum Seekers. medRxiv. doi: 10.1101/2020.04.15.20063677. Preprint posted online on April 18, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nagra M, Vianya-Estopa M, Wolffsohn JS. Could telehealth help eye care practitioners adapt contact lens services during the COVID-19 pandemic? Cont Lens Anterior Eye. 2020 Jun;43(3):204–207. doi: 10.1016/j.clae.2020.04.002. http://europepmc.org/abstract/MED/32336578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.O'Connor CM, Anoushiravani AA, DiCaprio MR, Healy WL, Iorio R. Economic Recovery After the COVID-19 Pandemic: Resuming Elective Orthopedic Surgery and Total Joint Arthroplasty. J Arthroplasty. 2020 Jul;35(7S):S32–S36. doi: 10.1016/j.arth.2020.04.038. http://europepmc.org/abstract/MED/32345566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wittbold KA, Baugh JJ, Yun BJ, Raja AS, White BA. iPad deployment for virtual evaluation in the emergency department during the COVID-19 pandemic. Am J Emerg Med. 2020 Apr 18;:0`. doi: 10.1016/j.ajem.2020.04.025. http://europepmc.org/abstract/MED/32317204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hightow-Weidman L, Muessig K, Claude K, Roberts J, Zlotorzynska M, Sanchez T. Maximizing Digital Interventions for Youth in the Midst of Covid-19: Lessons from the Adolescent Trials Network for HIV Interventions. AIDS Behav. 2020 Aug;24(8):2239–2243. doi: 10.1007/s10461-020-02870-w. http://europepmc.org/abstract/MED/32306214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bonavita S, Tedeschi G, Atreja A, Lavorgna L. Digital triage for people with multiple sclerosis in the age of COVID-19 pandemic. Neurol Sci. 2020 May;41(5):1007–1009. doi: 10.1007/s10072-020-04391-9. http://europepmc.org/abstract/MED/32303856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, Curtis S, Roman M, Poon EG, Ferranti J, Katz JN, Tcheng J. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020 Jun 01;27(6):957–962. doi: 10.1093/jamia/ocaa067. http://europepmc.org/abstract/MED/32311034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yan A, Zou Y, Mirchandani DA. How hospitals in mainland China responded to the outbreak of COVID-19 using information technology-enabled services: An analysis of hospital news webpages. J Am Med Inform Assoc. 2020 Jul 01;27(7):991–999. doi: 10.1093/jamia/ocaa064. http://europepmc.org/abstract/MED/32311036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lin B, Wu S. COVID-19 (Coronavirus Disease 2019): Opportunities and Challenges for Digital Health and the Internet of Medical Things in China. OMICS. 2020 May;24(5):231–232. doi: 10.1089/omi.2020.0047. [DOI] [PubMed] [Google Scholar]
- 93.Kummitha RKR. Smart technologies for fighting pandemics: The techno- and human- driven approaches in controlling the virus transmission. Gov Inf Q. 2020 Jul;37(3):101481. doi: 10.1016/j.giq.2020.101481. http://europepmc.org/abstract/MED/32313361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Abbas A, Abdelsamea M, Gaber M. Classification of COVID-19 in chest X-ray images using DeTraC deep convolutional neural network. medRxiv. doi: 10.1101/2020.03.30.20047456. Preprint posted online on May 18, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ardabili S, Mosavi A, Ghamisi P, Ferdinand F, Varkonyi-Koczy AR, Reuter U, Rabczuk T, Atkinson PM. COVID-19 Outbreak Prediction with Machine Learning. medRxiv. doi: 10.1101/2020.04.17.20070094. Preprint posted online on April 22, 2020. [DOI] [Google Scholar]
- 96.Zhang H, Dimitrov D, Simpson L, Singh B, Plaks N, Penney S, Charles J, Sheehan R, Flammini S, Murphy S, Landman A. A Web-based, Mobile Responsive Application to Screen Healthcare Workers for COVID Symptoms: Descriptive Study. medRxiv. doi: 10.1101/2020.04.17.20069211. Preprint posted online on April 22, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hart JL, Turnbull AE, Oppenheim IM, Courtright KR. Family-Centered Care During the COVID-19 Era. J Pain Symptom Manage. 2020 Aug;60(2):e93–e97. doi: 10.1016/j.jpainsymman.2020.04.017. http://europepmc.org/abstract/MED/32333961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Parikh A, Kumar AA, Jahangir E. Cardio-Oncology Care in the Time of COVID-19 and the Role of Telehealth. JACC CardioOncol. 2020 Jun;2(2):356–358. doi: 10.1016/j.jaccao.2020.04.003. https://linkinghub.elsevier.com/retrieve/pii/S2666-0873(20)30068-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rahman MS, Peeri NC, Shrestha N, Zaki R, Haque U, Hamid SHA. Defending against the Novel Coronavirus (COVID-19) outbreak: How can the Internet of Things (IoT) help to save the world? Health Policy Technol. 2020 Jun;9(2):136–138. doi: 10.1016/j.hlpt.2020.04.005. http://europepmc.org/abstract/MED/32322475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Alwashmi MF. The Use of Digital Health in the Detection and Management of COVID-19. Int J Environ Res Public Health. 2020 Apr 23;17(8):2906. doi: 10.3390/ijerph17082906. https://www.mdpi.com/resolver?pii=ijerph17082906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sedov L, Krasnochub A, Polishchuk V. Modeling quarantine during epidemics and mass-testing using drones. medRxiv. doi: 10.1101/2020.04.15.20067025. Preprint posted online on April 23, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mahapatra S, Nath P, Chatterjee M. Repurposing Therapeutics for COVID-19: Rapid Prediction of Commercially available drugs through Machine Learning and Docking. medRxiv. doi: 10.1101/2020.04.05.20054254. Preprint posted online on April 23, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Azizy A, Fayaz M, Agirbasli M. Do Not Forget Afghanistan in Times of COVID-19: Telemedicine and the Internet of Things to Strengthen Planetary Health Systems. OMICS. 2020 Jun;24(6):311–313. doi: 10.1089/omi.2020.0053. [DOI] [PubMed] [Google Scholar]
- 104.Madurai Elavarasan R, Pugazhendhi R. Restructured society and environment: A review on potential technological strategies to control the COVID-19 pandemic. Sci Total Environ. 2020 Jul 10;725:138858. doi: 10.1016/j.scitotenv.2020.138858. http://europepmc.org/abstract/MED/32336562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Park S, Choi GJ, Ko H. Information Technology-Based Tracing Strategy in Response to COVID-19 in South Korea-Privacy Controversies. JAMA. 2020 Jun 02;323(21):2129–2130. doi: 10.1001/jama.2020.6602. [DOI] [PubMed] [Google Scholar]
- 106.Negrini S, Kiekens C, Bernetti A, Capecci M, Ceravolo MG, Lavezzi S, Zampolini M, Boldrini P. Telemedicine from research to practice during the pandemic. Eur J Phys Rehabil Med. 2020 Apr 24;:327–330. doi: 10.23736/S1973-9087.20.06331-5. doi: 10.23736/S1973-9087.20.06331-5. [DOI] [PubMed] [Google Scholar]
- 107.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the Era of COVID-19: The Virtual Orthopaedic Examination. J Bone Joint Surg Am. 2020 Jun 17;102(12):e57. doi: 10.2106/JBJS.20.00609. doi: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Randhawa GS, Soltysiak MPM, El Roz H, de Souza CPE, Hill KA, Kari L. Machine learning using intrinsic genomic signatures for rapid classification of novel pathogens: COVID-19 case study. PLoS One. 2020;15(4):e0232391. doi: 10.1371/journal.pone.0232391. https://dx.plos.org/10.1371/journal.pone.0232391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Javaid M, Haleem A, Vaishya R, Bahl S, Suman R, Vaish A. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes Metab Syndr. 2020;14(4):419–422. doi: 10.1016/j.dsx.2020.04.032. http://europepmc.org/abstract/MED/32344370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kyhlstedt M, Andersson SW. Diagnostic and digital solutions to address the COVID-19 pandemic: The need for international collaboration to close the gap. Health Policy Technol. 2020 Jun;9(2):126–128. doi: 10.1016/j.hlpt.2020.04.010. http://europepmc.org/abstract/MED/32341908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Barbosa RDM, Fernandes MAC. Chaos game representation dataset of SARS-CoV-2 genome. Data Brief. 2020 Jun;30:105618. doi: 10.1016/j.dib.2020.105618. https://linkinghub.elsevier.com/retrieve/pii/S2352-3409(20)30512-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int J Environ Res Public Health. 2020 Apr 26;17(9):2997. doi: 10.3390/ijerph17092997. https://www.mdpi.com/resolver?pii=ijerph17092997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Reeves JJ, Hollandsworth HM, Torriani FJ, Taplitz R, Abeles S, Tai-Seale M, Millen M, Clay BJ, Longhurst CA. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020 Jun 01;27(6):853–859. doi: 10.1093/jamia/ocaa037. http://europepmc.org/abstract/MED/32208481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Khan F, Ghaffar A, Khan N, Cho SH. An Overview of Signal Processing Techniques for Remote Health Monitoring Using Impulse Radio UWB Transceiver. Sensors (Basel) 2020 Apr 27;20(9):2479. doi: 10.3390/s20092479. https://www.mdpi.com/resolver?pii=s20092479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Whelan P, Stockton-Powdrell C, Jardine J, Sainsbury J. Comment on "Digital Mental Health and COVID-19: Using Technology Today to Accelerate the Curve on Access and Quality Tomorrow": A UK Perspective. JMIR Ment Health. 2020 Apr 27;7(4):e19547. doi: 10.2196/19547. https://mental.jmir.org/2020/4/e19547/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Meinert E, Milne-Ives M, Surodina S, Lam C. Agile Requirements Engineering and Software Planning for a Digital Health Platform to Engage the Effects of Isolation Caused by Social Distancing: Case Study. JMIR Public Health Surveill. 2020 May 06;6(2):e19297. doi: 10.2196/19297. https://publichealth.jmir.org/2020/2/e19297/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ekong I, Chukwu E, Chukwu M. COVID-19 Mobile Positioning Data Contact Tracing and Patient Privacy Regulations: Exploratory Search of Global Response Strategies and the Use of Digital Tools in Nigeria. JMIR mHealth uHealth. 2020 Apr 27;8(4):e19139. doi: 10.2196/19139. https://mhealth.jmir.org/2020/4/e19139/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Pérez Sust P, Solans O, Fajardo JC, Medina Peralta M, Rodenas P, Gabaldà J, Garcia Eroles L, Comella A, Velasco Muñoz C, Sallent Ribes J, Roma Monfa R, Piera-Jimenez J. Turning the Crisis Into an Opportunity: Digital Health Strategies Deployed During the COVID-19 Outbreak. JMIR Public Health Surveill. 2020 May 04;6(2):e19106. doi: 10.2196/19106. https://publichealth.jmir.org/2020/2/e19106/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kim H, Paul A. Contact Tracing: a game of big numbers in the time of COVID-19. medRxiv. doi: 10.1101/2020.04.22.20071043. Preprint posted online on September 13, 2020. [DOI] [Google Scholar]
- 120.Krukowski RA, Ross KM. Measuring Weight with Electronic Scales in Clinical and Research Settings During the Coronavirus Disease 2019 Pandemic. Obesity (Silver Spring) 2020 Jul;28(7):1182–1183. doi: 10.1002/oby.22851. doi: 10.1002/oby.22851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Liu Q, Zheng Z, Zheng J, Chen Q, Liu G, Chen S, Chu B, Zhu H, Akinwunmi B, Huang J, Zhang CJP, Ming W. Health Communication Through News Media During the Early Stage of the COVID-19 Outbreak in China: Digital Topic Modeling Approach. J Med Internet Res. 2020 Apr 28;22(4):e19118. doi: 10.2196/19118. https://www.jmir.org/2020/4/e19118/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Vaid A, Somani S, Russak A, De Freitas JK, Chaudhry FF, Paranjpe I, Johnson KW, Lee SJ, Miotto R, Zhao S, Beckmann N, Naik N, Arfer K, Kia A, Timsina P, Lala A, Paranjpe M, Glowe P, Golden E, Danieletto M, Singh S, Meyer D, O'Reilly PF, Huckins LH, Kovatch P, Finkelstein J, Freeman RM, Argulian E, Kasarskis A, Percha B, Aberg JA, Bagiella E, Horowitz CR, Murphy B, Nestler EJ, Schadt EE, Cho JH, Cordon-Cardo C, Fuster V, Charney DS, Reich DL, Bottinger EP, Levin MA, Narula J, Fayad ZA, Just A, Charney AW, Nadkarni GN, Glicksberg BS. Machine Learning to Predict Mortality and Critical Events in COVID-19 Positive New York City Patients. medRxiv. doi: 10.1101/2020.04.26.20073411. Preprint posted online on April 28, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lee A. COVID-19 and the Advancement of Digital Physical Therapist Practice and Telehealth. Phys Ther. 2020 Jul 19;100(7):1054–1057. doi: 10.1093/ptj/pzaa079. http://europepmc.org/abstract/MED/32343836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tarek M, Elhefnawi M, Maricato J, Diaz RS, Shytaj IL, Savarino A. Custommune: a web tool to design personalized and population-targeted vaccine epitopes. medRxiv. doi: 10.1101/2020.04.25.20079426. Preprint posted online on April 29, 2020. [DOI] [Google Scholar]
- 125.Awasthi R, Pal R, Singh P, Nagori A, Reddy S, Gulati A, Kumaraguru P, Sethi S. CovidNLP: A Web Application for Distilling Systemic Implications of COVID-19 Pandemic with Natural Language Processing. medRxiv. doi: 10.1101/2020.04.25.20079129. Preprint posted online on April 29, 2020. [DOI] [Google Scholar]
- 126.Khan H, Hossain A. Countries are Clustered but Number of Tests is not Vital to Predict Global COVID-19 Confirmed Cases: A Machine Learning Approach. medRxiv. doi: 10.1101/2020.04.24.20078238. Preprint posted online on April 20, 2020. [DOI] [Google Scholar]
- 127.Husnayain A, Shim E, Fuad A, Su E. Assessing the community risk perception toward COVID-19 outbreak in South Koreavidence from Google and NAVER relative search volume. medRxiv. doi: 10.1101/2020.04.23.20077552. Preprint posted online on April 29, 2020. [DOI] [Google Scholar]
- 128.Weemaes M, Martens S, Cuypers L, Van Elslande J, Hoet K, Welkenhuysen J, Goossens R, Wouters S, Houben E, Jeuris K, Laenen L, Bruyninckx K, Beuselinck K, André E, Depypere M, Desmet S, Lagrou K, Van Ranst M, Verdonck AKLC, Goveia J. Laboratory information system requirements to manage the COVID-19 pandemic: A report from the Belgian national reference testing center. J Am Med Inform Assoc. 2020 Aug 01;27(8):1293–1299. doi: 10.1093/jamia/ocaa081. http://europepmc.org/abstract/MED/32348469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Espinoza J, Crown K, Kulkarni O. A Guide to Chatbots for COVID-19 Screening at Pediatric Health Care Facilities. JMIR Public Health Surveill. 2020 Apr 30;6(2):e18808. doi: 10.2196/18808. https://publichealth.jmir.org/2020/2/e18808/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wagner T, Shweta F, Murugadoss K, Awasthi S, Venkatakrishnan AJ, Bade S, Puranik A, Kang M, Pickering BW, O'Horo JC, Bauer PR, Razonable RR, Vergidis P, Temesgen Z, Rizza S, Mahmood M, Wilson WR, Challener D, Anand P, Liebers M, Doctor Z, Silvert E, Solomon H, Anand A, Barve R, Gores GJ, Williams AW, Morice WG, Halamka J, Badley AD, Soundararajan V. Augmented Curation of Unstructured Clinical Notes from a Massive EHR System Reveals Specific Phenotypic Signature of Impending COVID-19 Diagnosis. medRxiv. doi: 10.1101/2020.04.19.20067660. Preprint posted online on June 11, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Brat GA, Weber GM, Gehlenborg N, Avillach P, Palmer NP, Chiovato L, Cimino J, Waitman LR, Omenn GS, Malovini A, Moore JH, Beaulieu-Jones BK, Tibollo V, Murphy SN, L'Yi S, Keller MS, Bellazzi R, Hanauer DA, Serret-Larmande A, Gutierrez-Sacristan A, Holmes JH, Bell DS, Mandl KD, Follett RW, Klann JG, Murad DA, Scudeller L, Bucalo M, Kirchoff K, Craig J, Obeid J, Jouhet V, Griffier R, Cossin S, Moal B, Patel LP, Bellasi A, Prokosch HU, Kraska D, Sliz P, Tan ALM, Ngiam KY, Zambelli A, Mowery DL, Schiver E, Devkota B, Bradford RL, Daniar M, APHP/Universities/INSERM COVID-19 research collaboration. Daniel C, Benoit V, Bey R, Paris N, Jannot AS, Serre P, Orlova N, Dubiel J, Hilka M, Jannot AS, Breant S, Leblanc J, Griffon N, Burgun A, Bernaux M, Sandrin A, Salamanca E, Ganslandt T, Gradinger T, Champ J, Boeker M, Martel P, Gramfort A, Grisel O, Leprovost D, Moreau T, Varoquaux G, Wassermann D, Mensch A, Caucheteux C, Haverkamp C, Lemaitre G, Krantz ID, Cormont S, South A, The Consortium for Clinical Characterization of COVID-19 by EHR (4CE) Cai T, Kohane IS. International Electronic Health Record-Derived COVID-19 Clinical Course Profiles: The 4CE Consortium. medRxiv. doi: 10.1101/2020.04.13.20059691. doi: 10.1101/2020.04.13.20059691. Preprint posted online on June 08, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Hegde C, Jiang Z, Suresha P, Zelko J, Seyedi S, Smith MA, Wright DW, Kamaleswaran R, Reyna MA, Clifford GD. AutoTriage - An Open Source Edge Computing Raspberry Pi-based Clinical Screening System. medRxiv. doi: 10.1101/2020.04.09.20059840. Preprint posted online on April 30, 2020. [DOI] [Google Scholar]
- 133.Tobias A, Valls J, Satorra P, Tebe C. COVID19-Tracker: A shiny app to produce comprehensive data visualization for SARS-CoV-2 epidemic in Spain. medRxiv. doi: 10.1101/2020.04.01.20049684. Preprint posted online on April 30, 2020. [DOI] [Google Scholar]
- 134.Compton M, Soper M, Reilly B, Gettle L, List R, Bailey M, Bruschwein H, Somerville L, Albon D. A Feasibility Study of Urgent Implementation of Cystic Fibrosis Multidisciplinary Telemedicine Clinic in the Face of COVID-19 Pandemic: Single-Center Experience. Telemed J E Health. 2020 Aug;26(8):978–984. doi: 10.1089/tmj.2020.0091. [DOI] [PubMed] [Google Scholar]
- 135.Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation Guide for Rapid Integration of an Outpatient Telemedicine Program During the COVID-19 Pandemic. J Am Coll Surg. 2020 Aug;231(2):216–222.e2. doi: 10.1016/j.jamcollsurg.2020.04.030. http://europepmc.org/abstract/MED/32360960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kalteh EA, Rajabi A. COVID-19 and digital epidemiology. Z Gesundh Wiss. 2020 Apr 30;:1–3. doi: 10.1007/s10389-020-01295-y. http://europepmc.org/abstract/MED/32355606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Woo Baidal JA, Chang J, Hulse E, Turetsky R, Parkinson K, Rausch JC. Zooming Toward a Telehealth Solution for Vulnerable Children with Obesity During Coronavirus Disease 2019. Obesity (Silver Spring) 2020 Jul;28(7):1184–1186. doi: 10.1002/oby.22860. http://europepmc.org/abstract/MED/32352650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ciaffi J, Meliconi R, Landini M, Ursini F. Google trends and COVID-19 in Italy: could we brace for impact? Intern Emerg Med. 2020 May 25;:1555–1559. doi: 10.1007/s11739-020-02371-7. http://europepmc.org/abstract/MED/32451932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Carullo G. Digitalization of controls at the time of coronavirus. Article in Italian. CERIDAP. 2020. Mar 31, [2020-11-04]. https://ceridap.eu/digitalizzazione-dei-controlli-ai-tempi-del-coronavirus/
- 140.Article 25. Data protection by design and by default. GDPR Text. [2020-11-04]. https://gdpr-text.com/read/article-25/
- 141.Doran CM, Kinchin I. Economics of Mental Health: Providing a Platform for Efficient Mental Health Policy. Appl Health Econ Health Policy. 2020 Apr;18(2):143–145. doi: 10.1007/s40258-020-00569-6. [DOI] [PubMed] [Google Scholar]
- 142.Sweeney Y. Tracking the debate on COVID-19 surveillance tools. Nat Mach Intell. 2020 Jun 16;2(6):301–304. doi: 10.1038/s42256-020-0194-1. [DOI] [Google Scholar]
- 143.Wang S, Ding S, Xiong L. A New System for Surveillance and Digital Contact Tracing for COVID-19: Spatiotemporal Reporting Over Network and GPS. JMIR mHealth uHealth. 2020 Jun 10;8(6):e19457. doi: 10.2196/19457. https://mhealth.jmir.org/2020/6/e19457/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Garg S, Bhatnagar N, Gangadharan N. A Case for Participatory Disease Surveillance of the COVID-19 Pandemic in India. JMIR Public Health Surveill. 2020 Apr 16;6(2):e18795. doi: 10.2196/18795. https://publichealth.jmir.org/2020/2/e18795/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ienca M, Vayena E. On the responsible use of digital data to tackle the COVID-19 pandemic. Nat Med. 2020 Apr;26(4):463–464. doi: 10.1038/s41591-020-0832-5. http://europepmc.org/abstract/MED/32284619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Corrao G, Rea F, Di Martino M, Lallo A, Davoli M, DlE Pl A, Belotti L, Merlino L, Pisanti P, Lispi L, Skrami E, Carle F, working group ‘Monitoring and assessing diagnostic-therapeutic paths’ of the Italian Heath Ministry Effectiveness of adherence to recommended clinical examinations of diabetic patients in preventing diabetes-related hospitalizations. Int J Qual Health Care. 2019 Jul 01;31(6):464–472. doi: 10.1093/intqhc/mzy186. [DOI] [PubMed] [Google Scholar]
- 147.Fagherazzi G, Goetzinger C, Rashid MA, Aguayo GA, Huiart L. Digital Health Strategies to Fight COVID-19 Worldwide: Challenges, Recommendations, and a Call for Papers. J Med Internet Res. 2020 Jun 16;22(6):e19284. doi: 10.2196/19284. https://www.jmir.org/2020/6/e19284/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.De Groote SL, Shultz M, Blecic DD. Information-seeking behavior and the use of online resources: a snapshot of current health sciences faculty. J Med Libr Assoc. 2014 Jul 17;102(3):169–76. doi: 10.3163/1536-5050.102.3.006. http://europepmc.org/abstract/MED/25031557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Callaway E. Will the pandemic permanently alter scientific publishing? Nature. 2020 Jun;582(7811):167–168. doi: 10.1038/d41586-020-01520-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Eligibility criteria and search strategy.
Table S1. Articles included in the literature review.


