Abstract
Introduction and Aims.
Young adults have the highest rates of drug use and contribute significantly to the growing population of medical cannabis patients (MCP). This study examined relationships between longitudinal patterns of illicit/prescription drug use/misuse and cannabis practices among young adult cannabis users.
Design and Methods.
In 2014–2015, 210 young adult MCP and 156 nonpatient users were recruited in Los Angeles and surveyed annually over four waves. The analytical sample was limited to completers of all four waves (n = 301). Distinct developmental trajectories of illicit drug use and prescription drug misuse were identified. Fixed effects regression analysis evaluated changes in cannabis practices by trajectory groups.
Results.
Results supported two-trajectory solutions (high/low) for illicit drug use and prescription drug misuse. Decreases in use within all four trajectories occurred by wave 4. Low illicit drug use trajectory members were more likely to self-report medical cannabis use. Membership in both types of high-use trajectories was associated with use of concentrates and edibles. The prevalence of MCP, edibles use and cannabis days decreased significantly by wave 4.
Discussion and Conclusions.
While alternative cannabis forms use was associated with membership in high drug use trajectories, self-reported medical cannabis use (not MCP) was negatively associated with high illicit drug use trajectory membership. Reductions in the prevalence of MCP, cannabis days, edibles use and other drug use by wave 4 alongside stable levels of self-reported medical cannabis use might reflect the changing legal status of cannabis in California, maturing out phenomenon and safer patterns of cannabis use.
Keywords: medical marijuana, drug use trajectories, illicit drug use, prescription drug misuse, young adults
Introduction
Young adults in the United States have the highest prevalence of illicit drug use and prescription drug misuse as compared to adolescents and older adults [1]. In 2017, 24.2% of young adults reported drug use in the past month which included misuse of prescription drugs and use of cannabis, cocaine, heroin, hallucinogens, inhalants or methamphetamine. Cannabis, prescription stimulants and cocaine were the top three drugs used by young adults with past month prevalence of 22.1%, 2.1% and 1.9%, respectively.
Thirty-three states and the District of Columbia have legalised medical cannabis [2]. California was the first state to legalise medical cannabis in 1996 [3], where young adults comprise a significant proportion of the total population of medical cannabis patients (MCP) [4]. In California, medical cannabis may be recommended to individuals aged 18 years and older or with a parental permission by a physician for any health condition ‘for which marijuana provides relief’, which allows medical cannabis purchases through medical cannabis dispensaries and delivery services [5,6]. Cannabis became legal for recreational use in California with a passage of Proposition 64 in November 2016 permitting adults aged 21 years and older to purchase, possess and grow cannabis [3].
Illicit drug use and prescription drug misuse peak among young adults in their early 20s while a majority stops use between their mid- and late 20s [7]. Compared to illicit drug use, prescription drug misuse has relatively later initiation and earlier decline in use [7,8]. Careers of heroin, crack cocaine and methamphetamine use can span for decades with multiple cycles of cessation and relapse [9,10]. In contrast, use of cocaine powder [11], MDMA [12,13] and other hallucinogens [14,15] is often sporadic, infrequent, socially conditioned or short-lived.
Drug use trajectory research explores heterogeneity in the longitudinal patterns of drug use by capturing changes in the intensity or likelihood of use over time (e.g. consistent nonuse, inconsistent use, consistent use and decreasing use) and examining the impact of covariates on these changing patterns [11]. While a plethora of studies has been focused on developmental trajectories of alcohol, cigarette and recreational cannabis use among adolescents [16,17], only four studies have investigated trajectories of illicit drug use other than cannabis and prescription drug misuse among young adults. Those studies identified four trajectories of illicit/prescription drug use [18], four trajectories of cocaine use [11] and three trajectories of MDMA use [13], as well as growth trajectories of nonmedical use of prescription opioids, sedatives, stimulants and tranquilizers [19]. Importantly, while these studies report rates of cannabis use, no trajectory studies have focused specifically on populations of young adult cannabis users despite recent changes in laws regarding medical and recreational cannabis use.
Drug use trajectory studies of young adults have found a high degree of overlap between intensity of cannabis use and frequency of drug use within other drug use trajectories [13,18,19]. A cross-sectional study of young adult cannabis users found a positive association between illicit drug use and cannabis concentrates use, and greater odds of prescription drug misuse among cannabis edibles users while controlling for legal access to medical cannabis [20]. Studies of adults have found a protective effect of being MCP on the rates of illicit and prescription drug use/misuse [21-24]. Finally, self-reported medical cannabis use was associated with lower drug use problem severity [25] and lower prevalence of illicit drug use while no differences were observed for prescription drug misuse [20].
In summary, no trajectory study has investigated the role of MCP status, self-reported medical cannabis use or use of alternative cannabis forms in the longitudinal patterns of illicit or prescription drug use/misuse within a population of young adults. Given these gaps, the present analysis was undertaken to investigate drug use trajectories and cannabis use correlates among young adult cannabis users. We addressed the following research questions: (i) what are the trajectories of illicit drug use and prescription drug misuse among young adult cannabis users; and (ii) what are the relationships between those trajectories and cannabis practices?
Methods
Data source
Data utilised in the present analysis were collected within the Cannabis, Health & Young Adults (CHAYA) project [26,27], which collected four waves of quantitative data.
Study sample
The wave 1 sample was recruited in Los Angeles using targeted [28] and chain referral [29] sampling approaches. Eligibility requirements were as follows: aged between 18 to 26 years; used cannabis at least four times within 30 days prior to recruitment; resided in the Los Angeles metro area; and able to speak and read English. The sample was stratified between persons who had a current medical cannabis recommendation issued by a California-based physician for MCP and persons who had never had a medical cannabis recommendation for nonpatient users. There were no statistically significant demographic differences between enrolled and screened but nonenrolled participants [27].
Data collection
The wave 1 sample (n = 366) was surveyed between February 2014 and April 2015 followed by wave 2 (n = 339, April 2015-June 2016), wave 3 (n = 322, March 2016-June 2017), and wave 4 (n = 302, April 2017–April 2018). Wave 1, 2, and 3 surveys were interviewer-administered, while the wave 4 survey was self-administered through an online survey link. Data collection instruments and all study procedures were approved by the Institutional Review Boards at Children’s Hospital Los Angeles and Drexel University.
Measures
Data on demographic characteristics such as age (range 18–26 years), age at first cannabis use, assigned sex at birth (male vs. female), sexual identity (heterosexual vs. other categories) and race/ethnicity (non-Hispanic White, Non-Hispanic African American, non-Hispanic Multiracial, non-Hispanic Asian/Pacific Islander or Hispanic/Latino) were collected during wave 1 surveys. Data on all dependent and independent variables were collected at all four waves.
Independent variables were past 90-day illicit drug use and prescription drug misuse in each wave assessed through the following question: How long has it been since you last used [specific substance]? Past 90-day use (yes/no) was determined by selecting either Within the past 30 days or More than 30 days ago, but within the past 3 months for any of the listed illicit or prescription drugs (see Table 1 for the full list of drugs).
Table 1.
Illicit drug use and prescription drug misuse in the past 90 days by wave and by trajectory group among young adult cannabis users in Los Angeles ( n = 301)
| High illicit drug use trajectory, n = 105 |
Low illicit drug use trajectory, n = 196 |
|||||||
|---|---|---|---|---|---|---|---|---|
| % (n) |
% (n) |
|||||||
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 1 | Wave 2 | Wave 3 | Wave 4 | |
| Any illicit drug use | 70.5 (74) | 75.2 (79) | 72.4 (76) | 61.9 (65) | 11.2 (22) | 10.7 (21) | 7.7 (15) | 5.6 (11) |
| LSD | 21.0 (22) | 28.6 (30) | 25.7 (27) | 8.6 (9) | 1.0 (2) | 1.0 (2) | 0.5 (1) | 0.5 (1) |
| Psilocybin | 20.0 (21) | 19.0 (20) | 20.0 (21) | 18.1 (19) | 2.6 (5) | 4.1 (8) | 2.6 (5) | 2.6 (5) |
| MDMA | 22.9 (24) | 29.5 (31) | 25.7 (27) | 18.1 (19) | 4.1 (8) | 2.6 (5) | 3.6 (7) | 0.5 (1) |
| Cocaine | 27.6 (29) | 35.2 (37) | 37.1 (39) | 35.2 (37) | 3.6 (7) | 3.1 (6) | 3.6 (7) | 2.0 (4) |
| Crack | 1.0 (1) | 0.0 (0) | 0.0 (0) | 1.0 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Heroin | 1.0 (1) | 1.0 (1) | 2.9 (3) | 1.9 (2) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Methamphetamine | 2.9 (3) | 3.8 (4) | 4.8 (5) | 2.9 (3) | 0.0 (0) | 0.5 (1) | 0.0 (0) | 0.0 (0) |
| GHB | 1.0 (1) | 1.0 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Ketamine | 2.9 (3) | 5.7 (6) | 4.8 (5) | 1.9 (2) | 0.5 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Synthetic cathinone | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Synthetic cannabis | 2.9 (3) | 2.9 (3) | 3.8 (4) | 0.0 (0) | 2.6 (5) | 1.0 (2) | 0.5 (1) | 0.0 (0) |
| Salvia divinorum | 4.8 (5) | 1.9 (2) | 1.0 (1) | 1.0 (1) | 0.5 (1) | 0.5 (1) | 0.0 (0) | 0.0 (0) |
| High Rx drug misuse trajectory, n = 60 |
Low Rx drug misuse trajectory, n = 241 |
|||||||
| % (n) |
% (n) |
|||||||
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 1 | Wave 2 | Wave 3 | Wave 4 | |
| Any Rx drug misuse | 61.7 (37) | 71.7 (43) | 66.7 (40) | 56.7 (34) | 13.7 (33) | 5.4 (13) | 5.8 (14) | 5.4 (13) |
| Opioids | 25.0 (15) | 20.0 (12) | 18.3 (11) | 11.7 (7) | 5.0 (12) | 1.7 (4) | 1.2 (3) | 0.4 (1) |
| Tranquilizers | 20.0 (12) | 46.7 (28) | 36.7 (22) | 25.0 (15) | 4.1 (10) | 1.7 (4) | 2.1 (5) | 1.7 (4) |
| Stimulants | 35.0 (21) | 26.7 (16) | 30.0 (18) | 18.3 (11) | 3.7 (9) | 1.7 (4) | 1.2 (3) | 1.2 (3) |
| Sleeping pills | 6.7 (4) | 10.0 (6) | 11.7 (7) | 10.0 (6) | 2.9 (7) | 0.8 (2) | 1.7 (4) | 2.1 (5) |
| Muscle relaxants | 10.0 (6) | 6.7 (4) | 10.0 (6) | 10.0 (6) | 1.7 (4) | 0.8 (2) | 0.4 (1) | 0.8 (2) |
| Anti-depressants | 0.0 (0) | 1.7 (1) | 1.7 (1) | 5.0 (3) | 0.0 (0) | 0.0 (0) | 0.4 (1) | 0.0 (0) |
Dependent variables were cannabis practices, including current MCP status, past 90-day use of cannabis concentrates (wax, shatter, dab, oil), edibles, days of cannabis use (range 0–90) self-reported medical and problematic cannabis use. Irrespective of MCP status, participants who characterised their cannabis use as exclusively medical, primarily medical or equally medical and recreational were categorised as ‘self-reported medical cannabis users’ versus others who characterised their use as primarily recreational or exclusively recreational [20]. Problematic cannabis use was evaluated with the Severity of Dependence Scale (SDS), a 5-item valid and reliable measure of problematic cannabis use [30]. Problematic drug use of substances other than alcohol and tobacco was measured with a 10-item Drug Abuse Screening Test (DAST-10) [31,32]. Final scores for both SDS (4-point ordinal scale) and DAST (yes/no) were calculated by adding all items where higher scores indicate more problematic patterns of use [30,31]. Alcohol and tobacco were not included in this analysis; however, wave 1 data have been reported earlier [27].
Data analysis
We limited data analysis to participants who completed surveys in all four waves of data collection resulting in a subsample of n = 301 (83% of the wave 1 sample). There were no statistically significant differences in age, sex or race/ethnicity between the wave 1 sample and the sample selected for present analysis.
Data analysis was performed in two phases. First, we identified separate developmental trajectories of illicit drug use and prescription drug misuse by fitting discrete mixture models using PROC TRAJ macro in SAS [33-35]. Some prior trajectory studies, conducted among young adults, either developed trajectories based on frequency of use of specific drugs (e.g. MDMA or cocaine trajectories) [11,13], or used a total count of illicit/prescription drugs used at each assessment period as trajectory indicators [18]. These approaches were not chosen in the present study since the frequency of use for any specific drug was relatively low, even for the most prevalent drugs (i.e. cocaine, MDMA, LSD) [20], while the total number of drugs used within each assessment period as trajectory indicator assumes the same addiction potential for all drugs, e.g. heroin vs. LSD. Rather, we selected presence or absence (yes/no) of either past 90-day illicit drug use or past 90-day prescription drug misuse in each wave as trajectory indicators. Models with a different number of trajectory groups and shapes (e.g. linear, quadratic or cubic) were compared through the difference in Bayesian Information Criterion (BIC). Specifically, we compared BIC for models with the same number of trajectories but different shapes, and models with the same shapes but different number of trajectories to select the best fitting model.
Second, once the number and shapes of trajectory groups were identified, we extracted variables indicating trajectory group membership for both types of drug use and merged them with the analytical dataset that contained outcomes of interest. Then, bivariate associations between trajectory groups and outcomes at each wave were examined with chi-square or Kruskal-Wallis tests. Longitudinal patterns of cannabis practices conditioned on a trajectory group membership were investigated by fitting a fixed effects regression model (general linear model framework) with trajectory group as a between-subject effect and wave as a within-subject effect. Binary outcomes were evaluated through logistic regression models while count outcomes were examined through negative binomial regression models (i.e. cannabis days, DAST and SDS). We fitted two regression models for each outcome: one with an illicit drug use trajectory membership as independent variable and second one with a prescription drug misuse trajectory membership as independent variable. Regression models were adjusted for demographic variables such as age, race/ethnicity or sex whenever we found statistically significant associations (P < 0.05) with either trajectory group or outcome variables in at least two waves or both. All analyses were performed in SAS (version 9.4). Observations with missing values on the outcome variable or covariate were excluded from the model.
Results
Mixture modelling
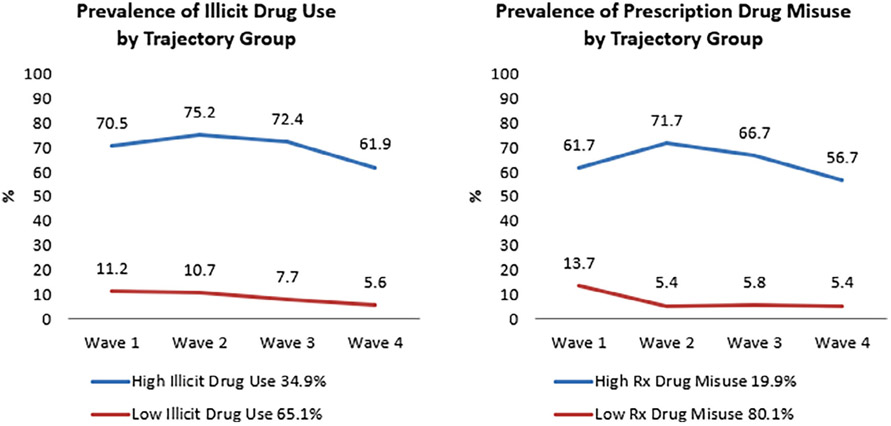
Results from the mixture modelling phase revealed that a two-class solution with a linear trend, interpreted as high- and low-use trajectories (Figure 1), had the best fit for both illicit drug use and prescription drug misuse showing the smallest BIC and the largest difference in BIC between model with greater number of trajectory groups and null model (Table S1). The DAST-10 corroborated a two-trajectory solution by showing significant differences cross-sectionally and longitudinally between high-and low-use trajectories for both types of drug use (adjusted incidence rate ratio (AIRR) 1.76, 95% confidence interval (CI) 1.46, 2.12 for illicit drug use, AIRR 1.71, 95% CI 1.43, 2.04 for prescription drug misuse) (data not shown). Low-use trajectories of illicit and prescription drug use/misuse demonstrated decreasing trends between waves 1 and 4. High illicit drug use trajectory was primarily driven by use of LSD, psilocybin, MDMA and cocaine (Table 1). Psilocybin use remained relatively stable, LSD and MDMA use spiked in wave 2 and then declined, while cocaine use remained stable high after wave 2 spike. High prescription drug misuse trajectory was primarily driven by prescription tranquilizer, opioid and stimulant misuse. While opioid and stimulant misuse showed approximately two-fold decrease by wave 4, prevalence of tranquilizer misuse spiked in wave 2 and then continued to decrease but remained above wave 1 levels.
Figure 1.
Prevalence of illicit drug use and prescription misuse in the past 90 days in each wave by trajectory group among young adult cannabis users in Los Angeles (n = 301).
Demographics
At wave 1 mean age of the participants in the analytical sample was 21.2 years old while mean age of first cannabis use was 15.3 years old (Table 2). A majority were male (64.8%), heterosexual (80.3%) and Hispanic/Latino (44.1%). We did not find any significant trajectory group effect for age, age of first cannabis use, sex or sexual identity. However, the high illicit drug use and high prescription drug misuse trajectory group members were more likely to be non-Hispanic White (P < 0.01) and less likely to be non-Hispanic African American (P <0.01 for illicit drug use; P <0.05 for prescription drug misuse). When examining associations between key demographic (age, sex and race/ethnicity) and cannabis practices variables, we found a consistent positive association between male sex and concentrates use (P <0.001 in wave 1; P <0.05 in wave 3). Therefore, all regression models were adjusted for non-Hispanic White while regression models with concentrates use as an outcome were also adjusted for sex.
Table 2.
Demographic characteristics in wave 1 by trajectory group among young adult cannabis users in Los Angeles(n = 301)
| Outcomes | Illicit drug use trajectories |
Prescription drug misuse trajectories |
|||
|---|---|---|---|---|---|
| Total |
High illicit drug use trajectory |
Low illicit drug use trajectory |
High Rx drug misuse trajectory |
Low Rx drug misuse trajectory |
|
|
n = 301 |
n = 105 |
n = 196 |
n = 60 |
n = 241 |
|
| % (n) | % (n) | % (n) | % (n) | % (n) | |
| Age, mean (SD)a | 21.2 (2.5) | 21.3 (2.6) | 21.2 (2.4) | 20.9 (2.5) | 21.3 (2.5) |
| Age at first cannabis use, mean (SD)a | 15.3 (2.3) | 15.2 (2.3) | 15.3 (2.4) | 15.0 (2.2) | 15.4 (2.3) |
| Assigned sex at birthb | |||||
| Male | 64.8 (195) | 65.7 (69) | 64.3 (126) | 63.3 (38) | 65.1 (157) |
| Sexual identityb | |||||
| Heterosexual | 80.3 (233) | 79.2 (80) | 81.0 (153) | 75.9 (44) | 81.5 (189) |
| Race/ethnicityb | |||||
| Non-Hispanic White | 26.4 (78) | 38.5 (40) | 19.9 (38)** | 44.1 (26) | 22.0 (52)** |
| Non-Hispanic African American | 19.3 (57) | 9.6 (10) | 24.6 (47)** | 8.5 (5) | 22.0 (52)* |
| Non-Hispanic Multiracial | 6.4 (19) | 4.8 (5) | 7.3 (14) | 6.8 (4) | 6.4 (15) |
| Non-Hispanic Asian/Pacific Islander | 3.7 (11) | 4.8 (5) | 3.1 (6) | 3.4 (2) | 3.8 (9) |
| Hispanic/Latino | 44.1 (130) | 42.3 (44) | 45.0 (86) | 37.3 (22) | 45.8 (108) |
P < 0.05.
P < 0.01.
Kruskal-Wallis test.
χ2 test.
Cannabis practices by trajectory groups
At the bivariate level (Table 3), we found positive associations between cannabis concentrates and edibles use, days of cannabis use (for prescription drug misuse in wave 2 only) and high-use trajectories while there was a negative association between self-reported medical cannabis use and high illicit drug use trajectory. Additionally, concentrates and edibles use, cannabis days and prevalence of MCP were declining from wave 1 through wave 4, while self-reported medical cannabis use had somewhat increasing prevalence, and SDS scores showed an increasing trend.
Table 3.
Cannabis practices by wave and by trajectory group among young adult cannabis users in Los Angeles (n = 301)
| Outcomes | Illicit drug use trajectories |
Prescription drug misuse trajectories |
|||
|---|---|---|---|---|---|
| Total |
High illicit drug use trajectory |
Low illicit drug use trajectory |
High Rx drug misuse trajectory |
Low Rx drug misuse trajectory |
|
|
n = 301 |
n = 105 |
n = 196 |
n = 60 |
n = 241 |
|
| % (n) | % (n) | % (n) | % (n) | % (n) | |
| Concentratesa,b | |||||
| Wave 1 | 58.1 (175) | 67.6 (71) | 53.1 (104)* | 70.0 (42) | 55.2 (133)* |
| Wave 2 | 58.8 (170) | 74.5 (76) | 50.3 (94)*** | 81.0 (47) | 53.2 (123)*** |
| Wave 3 | 61.7 (169) | 75.0 (75) | 54.0 (94)** | 72.4 (42) | 58.8 (127) |
| Wave 4 | 54.7 (151) | 70.3 (71) | 45.7 (80)*** | 67.8 (40) | 51.2 (111)* |
| Ediblesa,b | |||||
| Wave 1 | 59.5 (179) | 67.6 (71) | 55.1 (108)* | 71.7 (43) | 56.4 (136)* |
| Wave 2 | 55.7 (161) | 66.7 (68) | 49.7 (93)** | 67.2 (39) | 52.8 (122)* |
| Wave 3 | 59.5 (163) | 69.0 (69) | 54.0 (94)* | 60.3 (35) | 59.3 (128) |
| Wave 4 | 41.7 (115) | 46.5 (47) | 38.9 (68) | 49.2 (29) | 39.6 (86) |
| Cannabis daysc mean (SD) | |||||
| Wave 1 | 69.2 (26.2) | 72.5 (22.2) | 67.4 (28.1) | 75.4 (22.4) | 67.7 (26.9) |
| Wave 2 | 64.7 (30.9) | 67.1 (29.2) | 63.4 (31.8) | 73.4 (25.5) | 62.5 (31.8)* |
| Wave 3 | 60.9 (33.3) | 63.8 (31.6) | 59.3 (34.2) | 65.4 (30.8) | 59.8 (33.9) |
| Wave 4 | 53.8 (36.7) | 59.1 (33.5) | 51.0 (38.2) | 60.0 (35.3) | 52.2 (37.0) |
| MCP statusb | |||||
| Wave 1 | 59.5 (179) | 62.9 (66) | 57.7 (113) | 63.3 (38) | 58.5 (141) |
| Wave 2 | 53.2 (160) | 53.3 (56) | 53.1 (104) | 58.3 (35) | 51.9 (125) |
| Wave 3 | 50.8 (153) | 50.5 (53) | 51.0 (100) | 48.3 (29) | 51.5 (124) |
| Wave 4 | 38.2 (115) | 38.1 (40) | 38.3 (75) | 38.3 (23) | 38.2 (92) |
| Self-reported medical cannabis usea,b | |||||
| Wave 1 | 58.1 (175) | 49.5 (52) | 62.8 (123)* | 51.7 (31) | 59.8 (144) |
| Wave 2 | 54.3 (157) | 42.2 (43) | 61.0 (114)** | 53.4 (31) | 54.5 (126) |
| Wave 3 | 59.5 (163) | 54.0 (54) | 62.6 (109) | 56.9 (33) | 60.2 (130) |
| Wave 4 | 60.5 (155) | 51.0 (50) | 66.5 (105)* | 61.8 (34) | 60.2 (121) |
| Severity of Dependence Scalea,c mean (SD) | |||||
| Wave 1 | 2.5 (2.7) | 2.7 (2.9) | 2.4 (2.7) | 2.7 (2.9) | 2.5 (2.7) |
| Wave 2 | 2.7 (2.6) | 2.9 (2.7) | 2.6 (2.6) | 2.7 (2.4) | 2.7 (2.7) |
| Wave 3 | 2.8 (2.8) | 2.7 (2.6) | 2.8 (2.9) | 2.7 (2.5) | 2.8 (2.9) |
| Wave 4 | 2.9 (3.0) | 2.8 (2.9) | 3.0 (3.0) | 2.5 (2.7) | 3.0 (3.1) |
P < 0.05.
P < 0.01.
P < 0.001.
Only those who reported cannabis use in the past 90 days were included in denominator.
χ2 test.
Kruskal-Wallis test.
In adjusted models (Table 4), high illicit drug use trajectory members were more likely to report concentrates (adjusted odds ratio (AOR) 2.40, 95% CI 1.67, 3.44) and edibles (AOR 1.76, 95% CI 1.28, 2.41) use, and less likely to self-report medical cannabis use (AOR 0.59, 95% CI 0.41, 0.85), while there was no association with MCP status. High prescription drug misuse trajectory membership was associated with higher probability of concentrates (AOR 2.16, 95% CI 1.49, 3.15) and edibles (AOR 1.58, 95% CI 1.10, 2.27) use, and greater days of cannabis use (AIRR 1.15, 95% CI 1.03, 1.27) as compared to low prescription drug misuse trajectory.
Table 4.
Repeated measures analyses of cannabis practices and drug use trajectories among young adult cannabis users in Los Angeles (n = 301)
| Outcomes | Illicit drug use model AORb (95% CI) |
Rx drug misuse model AORb (95% CI) |
||||||
|---|---|---|---|---|---|---|---|---|
| High illicit drug use trajectorya |
Wave 2c | Wave 3c | Wave 4c | High Rx drug misuse trajectorya |
Wave 2c | Wave 3c | Wave 4c | |
| Concentratesd,e,n = 251 | 2.40 (1.67, 3.44)*** |
1.01 (0.76, 1.34) |
1.12 (0.83, 1.52) |
0.81 (0.60, 1.11) |
2.16 (1.49, 3.15)*** |
1.01 (0.77, 1.33) |
1.12 (0.84, 1.51) |
0.82 (0.60, 1.11) |
| Ediblesd,n = 251 | 1.76 (1.28, 2.41)*** |
0.85 (0.64, 1.13) |
0.95 (0.71, 1.29) |
0.47 (0.34, 0.66)*** |
1.58 (1.10, 2.27)* |
0.85 (0.64, 1.13) |
0.96 (0.71, 1.29) |
0.48 (0.35, 0.66)*** |
| Cannabis daysf,n = 283 | 1.10 (1.0, 1.21) |
0.93 (0.89, 0.98)** |
0.87 (0.82, 0.93)*** |
0.78 (0.73, 0.85)*** |
1.15 (1.03, 1.27)* |
0.93 (0.88, 0.98)** |
0.88 (0.82, 0.93)*** |
0.78 (0.73, 0.85)*** |
| MCP status, n = 295 | 1.07 (0.76, 1.49) |
0.76 (0.59, 0.97)* |
0.70 (0.53, 0.92)** |
0.41 (0.31, 0.55)*** |
1.10 (0.75, 1.61) |
0.76 (0.60, 0.97)* |
0.70 (0.53, 0.92)** |
0.41 (0.31, 0.55)*** |
| Self-reportedd medical cannabis use, n = 231 | 0.59 (0.41, 0.85)** |
0.86 (0.67, 1.10) |
1.06 (0.81, 1.40) |
1.16 (0.90, 1.51) |
0.93 (0.60, 1.45) |
0.86 (0.68, 1.09) |
1.06 (0.81, 1.39) |
1.16 (0.89, 1.50) |
| SDSd,f,n = 249 | 1.07 (0.88, 1.30) |
1.08 (0.96, 1.22) |
1.08 (0.95, 1.24) |
1.18 (1.03, 1.35)* |
0.99 (0.78, 1.26) |
1.08 (0.96, 1.22) |
1.08 (0.95, 1.24) |
1.18 (1.03, 1.35)* |
P < 0.05.
P < 0.01.
P < 0.001.
Low-use trajectory is a reference group.
Adjusted for non-Hispanic White vs. other categories.
Wave 1 is a reference group.
Only those who reported cannabis use in the past 90 days were included in the model.
Adjusted for male sex.
Negative binomial distribution with adjusted incidence rate ratios as estimates. AOR, adjusted odds ratio; CI, confidence interval, MCP, medical cannabis patients; SDS, Severity of Dependence Scale.
We found a significant effect of time for edibles use, cannabis days, MCP status and SDS scores for both model types, indicating a decline between waves 1 and 4, except for SDS which increased in wave 4.
Discussion
This is the first study to describe developmental trajectories of illicit drug use and prescription drug misuse among young adult cannabis users with and without legal access to medical cannabis. We identified a two-class solution (high- and low-use trajectories) for both illicit drug use and prescription drug misuse with decreasing trends for both low-use trajectories and increasing and then decreasing trends for high-use trajectories with some exceptions. Relatively stable high rates of cocaine use in our study are consistent with the dominance of a persistent use trajectory group in a study of cocaine users [11]. Decreasing prescription drug misuse is similar to findings from an earlier study of young adults showing decreasing trends in misuse after the age of 18 [19]. Notably, the very low prevalence of heroin use [20] and decrease in misuse of prescription opioids in our sample are reflective of the national trends observed among adults aged 18 to 25 years [1,36].
We found notable differences in the correlates of the high-use trajectory groups for illicit and prescription drug use. Key findings include lack of an association between MCP status and either trajectory type, and a strong negative association between high illicit drug use trajectory and self-reported medical cannabis use. This lends support to the results from our crosssectional analysis [20], but contradicts other crosssectional studies on the relationship between MCP status and other drug use among adults in the general population showing negative associations between MCP status and illicit/prescription drug use/misuse [21-23]. Only one study among 12th graders showed a positive association between past year illicit and prescription drug use/misuse and MCP status [37]. This might be due the fact that the MCP group consists of both medical and recreational cannabis users with a greater proportion of recreational users among younger adult MCP [38]. Therefore, the protective effect of medical motivations for cannabis use does not necessarily translate into a protective effect of MCP status within a population of young adults. Importantly, prevalence of MCP decreased progressively from wave 1 through wave 4, while there was a slight increase in the prevalence of self-reported medical cannabis use. This decline in MCP status might reflect changes in the legal landscape due to legalisation of recreational cannabis in California in 2016 while individuals who use cannabis medically continue to do so with or without medical cannabis recommendation.
We found that greater days of cannabis use were associated with membership in the high prescription drug misuse trajectory which supports findings from other prospective studies on prescription drug misuse conducted among emerging adults [19,39,40]. In contrast, we found no association between days of cannabis use and the illicit drug use trajectories. Previous longitudinal studies among young adults yielded conflicting results on the relationship between cannabis use frequency and illicit drug use showing positive association with MDMA use [12,13] and negative association with cocaine use [11]. Moreover, trajectories of both types did not differ on the SDS scores. In contrast, positive associations between high-use trajectories for both types of drug use and cannabis concentrates and edibles use are concerning due to the growing number of the reports on overdoses (e.g. passing out) after the use of these alternative forms [41,42]. However, frequency of cannabis use and proportion of cannabis edibles users decreased significantly by wave 4, similarly to the decrease in use/misuse of illicit and prescription drugs, which might indicate a maturing out phenomenon and movement towards more responsible and safe use or even abstinence as young adults grow older and adult roles increase [7,43,44]. Significantly, the declining trends in use/misuse of illicit and prescription drugs as well as cannabis by wave 4 coincided with the legalisation of cannabis for personal use. These results suggest that the legalisation of cannabis for personal use did not accelerate cannabis or illicit/prescription drug use among current cannabis users.
This study has several implications for future research. First, our study explored trajectories of illicit drug use and prescription drug misuse separately and within the same study among a population of young adult cannabis users. In contrast, all previous trajectory studies have been focused either on illicit [9,11,13], prescription [19,45] or illicit and prescription drug use/misuse as a single category [10,18,46]. Further research is needed to prospectively monitor patterns of illicit drug use and prescription drug misuse as well as their correlates within a population of young adults transitioning into adulthood as recreational cannabis continues to be legally available. Second, we assessed prospectively the role of both MCP status and self-reported medical cannabis use in the illicit drug use and prescription drug misuse trajectories. While the association between MCP status and other drug use received attention in several cross-sectional studies [21-24,37,47,48], the impact of medical motivations for cannabis use on the rates of other drug use was explored only in one study that was conducted among adults within primary care settings [25]. It is critical to evaluate whether the protective role of medical motivations for cannabis use will persist in a fully legalised environment. Third, this was the first prospective study assessing the relationship between other drug use and an array of cannabis practices, including use of high potency forms, which has never been assessed prospectively. Even though we observed reduction in the rates of use over time, given possible extreme effects associated with use [41,42] and the evidence of a link to other drug use, policy makers may consider limiting potency of edibles and concentrates legally available for recreational use. Finally, future studies should investigate the impact of various aspects of cannabis use on the longitudinal patterns of legal drug use, such as alcohol and tobacco use, among a population of young adults who have the highest rates of binge drinking and tobacco products use [1].
Our study also had some limitations. First, our findings may not be generalisable to all young adult cannabis users in Los Angeles since our sample was not randomly selected. Second, while it is recommended to estimate trajectory groups separately for each variable of interest, which accounts for uncertainty in trajectory membership [49], this approach is likely to result in different classification of trajectory groups for each cannabis use outcome. Therefore, given the exploratory nature of the current study, treating trajectory group membership as a fixed variable was the most suitable approach despite inherent limitations of this approach. Third, roughly one-third of wave 3 and a majority of wave 4 interviews were completed after recreational cannabis became legal in California, but only one-fifth of wave 4 interviews were conducted after recreational cannabis sales began. Therefore, inferences on the impact of recreational cannabis legalisation on our findings should be interpreted with caution, since longer follow-up is needed to evaluate the legalisation effect in a more robust manner.
In conclusion, we found a two-trajectory solution (high/low) for both illicit drug use and prescription drug misuse. High-use trajectories showed decrease in use for majority of the most prevalent illicit/prescription drugs by wave 4 along with a decrease in cannabis days and edibles use suggesting maturing out phenomenon. Both types of high-use trajectories were positively associated with use of alternative cannabis forms. Legal access to medical cannabis was not associated with either trajectory type, while self-reported medical cannabis use was negatively associated with high illicit drug use trajectory. We found a significant reduction in the proportion of MCP over the course of the study, while prevalence of self-reported medical cannabis use among current cannabis users slightly increased by wave 4 indicating continued medical use regardless of changing legal landscape. Future research should continue to evaluate prospectively the potential effects of cannabis legalisation on patterns of cannabis use and illicit/prescription drug use/misuse as young adult cannabis users age.
Supplementary Material
Table S1: Model fit for semiparametric group-based modelling
Acknowledgements
The authors would like to acknowledge the National Institute on Drug Abuse (DA034067) for funding this research study and the following individuals who supported the development of this manuscript: Miles McNeely, Megan Treese, Ali Johnson, Chaka Dodson, Maral Shahinian, Avat Kioumarsi, Janna Ataiants, Salini Mohanti and Megan Reed. This manuscript is the sole responsibility of the authors and does not reflect the views of the National Institute on Drug Abuse.
Footnotes
Conflict of Interest
The authors have no conflict of interest to declare.
References
- [1].Center for Behavioral Health Statistics and Quality. Results from the 2017 National Survey on Drug Use and Health: detailed tables. Rockville: Substance Abuse and Mental Health Services Administration, 2018. [Google Scholar]
- [2].National Conference of State Legislatures. State Medical Marijuana Laws. 5 March 2019. Available at: http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx (accessed March 2020).
- [3].California Department of Public Health, Center for Environmental Health, Division of Food, Drug, and Cannabis Safety. Laws and regulations. 25 January 2018. Available at: https://www.cdph.ca.gov/Programs/CEH/DFDCS/MCSB/Pages/Legislation.aspx (accessed March 2020).
- [4].Nunberg H, Kilmer B, Pacula RL, Burgdorf JR. An analysis of applicants presenting to a medical marijuana specialty practice in California. J Drug Policy Anal 2011;4:387–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].California Code, Health and Safety Code—HSC § 11362.5. Available at: https://codes.findlaw.com/ca/health-and-safety-code/hsc-sect-11362-5.html (accessed March 2020).
- [6].Lankenau SE, Kioumarsi A, Reed M, Mcneeley M, Iverson E, Wong CF. Becoming a medical marijuana user. Int J Drug Policy 2018; 52:62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. Am J Public Health 1995;85:41–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lipari RN, Ahrnsbrak RD, Pemberton MR, Porter JD. Risk and protective factors and estimates of substance use initiation: results from the 2016 National Survey on Drug Use and Health. NSDUH Data Review. 2017. Available at: https://www.samhsa.gov/data/sites/default/files/NSDUH-DR-FFR3-2016/NSDUH-DR-FFR3-2016.htm (accessed March 2020). [PubMed]
- [9].Hser Y-I, Huang D, Brecht M-L, Li L, Evans E. Contrasting trajectories of heroin, cocaine, and methamphetamine use. J Addict Dis 2008;27: 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kertesz SG, Khodneva Y, Richman J et al. Trajectories of drug use and mortality outcomes among adults followed over 18 years. J Gen Intern Med 2012;27:808–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ramo DE, Grov C, Delucchi KL, Kelly BC, Parsons JT. Cocaine use trajectories of club drug-using young adults recruited using time-space sampling. Addict Behav 2011;36:1292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Von Sydow K, Lieb R, Pfister H, Höfler M, Wittchen HU. Use, abuse and dependence of ecstasy and related drugs in adolescents and young adults—a transient phenomenon? Results from a longitudinal community study. Drug Alcohol Depend 2002;66:147–59. [DOI] [PubMed] [Google Scholar]
- [13].Smirnov A, Najman JM, Hayatbakhsh R et al. Young adults’ trajectories of ecstasy use: a population based study. Addict Behav 2013;38:2667–74. [DOI] [PubMed] [Google Scholar]
- [14].Halpern JH. Hallucinogens: an update. Curr Psychiatry Rep 2003;5: 347–54. [DOI] [PubMed] [Google Scholar]
- [15].Nichols DE. Hallucinogens. Pharmacol Ther 2004;101:131–81. [DOI] [PubMed] [Google Scholar]
- [16].Nelson SE, Van Ryzin MJ, Dishion TJ. Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: demographic correlates and young adult substance use problems. Dev Psychopathol 2014;27:253–77. [DOI] [PubMed] [Google Scholar]
- [17].Jackson KM, Sartor CE. The natural course of substance use and dependence. Oxford library of psychology In: The Oxford handbook of substance use and substance use disorders. Oxford: Oxford University Press, 2016:67–131. [Google Scholar]
- [18].Derefinko KJ, Charnigo RJ, Peters JR, Adams ZW, Milich R, Lynam DR. Substance use trajectories from early adolescence through the transition to college. J Stud Alcohol Drugs 2016;77:924–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].McCabe SE, Kloska DD, Veliz P, Jager J, Schulenberg JE. Developmental course of non-medical use of prescription drugs from adolescence to adulthood in the United States: national longitudinal data. Addiction 2016;111:2166–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Fedorova EV, Schrager SM, Robinson LF et al. Illicit drug use and prescription drug misuse among young adult medical cannabis patients and non-patient users in Los Angeles. Drug Alcohol Depend 2019;198:21–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Richmond MK, Pampel FC, Rivera LS, Broderick KB, Reimann B, Fischer L. Frequency and risk of marijuana use among substance-using health care patients in Colorado with and without access to state legalized medical marijuana. J Psychoactive Drugs 2015;47:1–9. [DOI] [PubMed] [Google Scholar]
- [22].Lin LA, Ilgen MA, Jannausch M, Bohnert KM. Comparing adults who use cannabis medically with those who use recreationally: results from a national sample. Addict Behav 2016;61:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Compton WM, Han B, Hughes A, Jones CM, Blanco C. Use of marijuana for medical purposes among adults in the United States. JAMA 2017;317:209–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Ilgen MA, Bohnert K, Kleinberg F et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend 2013;132:654–9. [DOI] [PubMed] [Google Scholar]
- [25].Roy-Byrne P, Maynard C, Bumgardner K et al. Are medical marijuana users different from recreational users? The view from primary care. Am J Addict 2015;24:599–606. [DOI] [PubMed] [Google Scholar]
- [26].Lankenau SE, Ataiants J, Mohanty S, Schrager S, Iverson E, Wong CF. Health conditions and motivations for marijuana use among young adult medical marijuana patients and non-patient marijuana users. Drug Alcohol Rev 2018;37:237–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Lankenau SE, Fedorova EV, Reed M, Schrager SM, Iverson E, Wong CF. Marijuana practices and patterns of use among young adult medical marijuana patients and non-patient marijuana users. Drug Alcohol Depend 2017;170:181–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Watters JK, Biernacki P. Targeted sampling: options for the study of hidden populations. Soc Probl 1989;36:416–30. [Google Scholar]
- [29].Biernacki P, Waldorf D. Snowball sampling: problems and techniques of chain referral sampling. Sociol Methods Res 1981;10:141–63. [Google Scholar]
- [30].Martin G, Copeland J, Gates P, Gilmour S. The Severity of Dependence Scale (SDS) in an adolescent population of cannabis users: reliability, validity and diagnostic cut-off. Drug Alcohol Depend 2006;83:90–3. [DOI] [PubMed] [Google Scholar]
- [31].Skinner HA. The drug abuse screening test. Addict Behav 1982;7:363–71. [DOI] [PubMed] [Google Scholar]
- [32].Bohn MJ, Babor TF, Kranzler HR. Validity of the Drug Abuse Screening Test (DAST-10) in inpatient substance abusers. Probl Drug Depend 1991;119:233–5. [Google Scholar]
- [33].Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods 1999;4:139–57. [DOI] [PubMed] [Google Scholar]
- [34].Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res 2001;29:374–93. [Google Scholar]
- [35].Nagin D. Group-based modeling of development. Cambridge, MA: Harvard University Press, 2005. [Google Scholar]
- [36].Center for Behavioral Health Statistics and Quality. Results from the 2015 National Survey on Drug Use and Health: detailed tables. Rockville: Substance Abuse and Mental Health Services Administration, 2016. [Google Scholar]
- [37].Boyd CJ, Veliz PT, McCabe SE. Adolescents’ use of medical marijuana: a secondary analysis of monitoring the future data. J Adolesc Health 2015;57:241–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Haug NA, Padula CB, Sottile JE, Vandrey R, Heinz AJ, Bonn- Miller MO. Cannabis use patterns and motives: a comparison of younger, middle-aged, and older medical cannabis dispensary patients. Addict Behav 2017;72:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Catalano RF, White HR, Fleming CB, Haggerty KP. Is nonmedical prescription opiate use a unique form of illicit drug use? Addict Behav 2011;36:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Mccabe SE, Schulenberg JE, O’Malley PM, Patrick ME, Kloska DD. Nonmedical use of prescription opioids during the transition to adulthood: a multi-cohort national longitudinal study. Addiction 2014;109:102–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Benjamin DM, Fossler MJ. Edible cannabis products: it is time for FDA oversight. J Clin Pharmacol 2016;56:1045–7. [DOI] [PubMed] [Google Scholar]
- [42].Cavazos-Rehg PA, Sowles SJ, Krauss MJ, Agbonavbare V, Grucza R, Bierut L. A content analysis of tweets about high-potency marijuana. Drug Alcohol Depend 2016;166:100–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Winick C. Maturing out of narcotic addiction. Bull Narc 1962;14:1–7. [Google Scholar]
- [44].Walters GD. Spontaneous remission from alcohol, tobacco, and other drug abuse: seeking quantitative answers to qualitative questions. Am J Drug Alcohol Abuse 2000;26:443–60. [DOI] [PubMed] [Google Scholar]
- [45].Boyd CJ, Cranford JA, McCabe SE. Longitudinal trajectories of nonmedical use of prescription medication among middle and high school students. J Addict Dis 2016;35:258–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Guo J, Chung IJ, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. J Adolesc Health 2002;31: 354–62. [DOI] [PubMed] [Google Scholar]
- [47].Woodruff SI, Shillington AM. Sociodemographic and drug use severity differences between medical marijuana users and non-medical users visiting the emergency department. Am J Addict 2016;25:385–91. [DOI] [PubMed] [Google Scholar]
- [48].Park JY, Wu LT. Differences in behavioral health disorders and unmet treatment needs between medical marijuana users and recreational marijuana users: results from a national adult sample. Drug Alcohol Depend 2017;180:311–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Clark SL, Muthén B. Relating latent class analysis results to variables not included in the analysis. 2009. Available at: https:/www.statmodel.com/download/relatinglca.pdf (accessed March 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Model fit for semiparametric group-based modelling