Abstract
Lung ultrasound (LUS) is a practical diagnostic tool for several lung pathologies. Pocket sized USG devices (PSUDs) are more affordable, accessible, practical, and learning to use them is easier than standard ultrasound devices (SUDs). Their capability in image quality have been found as comparable with standard USG machines. Studies have been showing that these devices can be useful as much as SUDs in the evaluation of heart, abdomen, vascular structures, diaphragm and optic nerve. The aim of this study is to compare PSUD with a standard ultrasound devices (SUD) in the evaluation of LUS patterns such as alveolar, interstitial syndromes and lung aeration score (LAS). Study performed in an University Hospital Pulmonary ICU. All patients older than 18 years old were included in this study. The sector probe of SUD (Vivid-Q) and PSUD (Vscan) were used for investigation of A lines, interstitial (B lines), alveolar syndromes (consolidation, hepatisation, air bronchograms) and pleural effusion. 33 patients were included in the study. When PSUD was compared with SUD in terms of total B2 count, and LAS in the right, left and both lung, there was an agreement without proportional bias according to Bland Altman test. There was also good inter class correlation coefficient value as greater than 0.8 and 0.7 between two physicians in terms of counting of total B1, B2, total B lines and calculating of total LAS for SUD and PSUD respectively. PSUDs is a reliable and valid method for evaluation of LUS patterns like SUDs.
Keywords: Alveolar syndrome, Interstitial syndrome, Lung aeration score, Pocket sized ultrasonography, Pleural effusion, ICU
Introduction
Nowadays, lung ultrasound (LUS) has increasingly used in the emergency department(ED) and intensive care units (ICUs). It is a noninvasive, radiation-free, cost effective, and easy to perform tool for critically ill patients. LUS is generally more accurate than X-ray for assessment of pneumothorax, pleural effusion(PE), interstitial syndrome, and alveolar syndrome [1, 2]. Also, ultrasound might be a promising technique used in the ICU for assessment of heart failure, lung edema, pneumonia, management of acute respiratory distress syndrome (ARDS) and differantial diagnosis of dyspnea [1–5]. More importantly, recently lung ultrasound have been using frequently and found to be useful to evaluate lung aeration in lung edema, pneumonia, ARDS, trauma. Several lung aeration scoring systems (LAS) are developed for this aim [1]. Some of them are used to evaluate lung edema counting B lines and frequently preffered in cardiology and nephrology. Most frequently used one in ICUs evaluates loss of lung aeration assessing alveolar and intertitial patterns. This score has been successfully used in different clinical situations such as prediction of postextubation distress, as an early warning tool during fluid resuscitation in patients with sepsis, evaluation of treatment response in patient with ventilator associated pneumonia, and evaluation of reaeration or PEEP response in patients with ARDS [1, 3, 6–8].
On the other hand, standard ultrasonography (USG) devices (SUDs) are expensive and are not easy to access for every ICU. Pocket sized USG devices (PSUDs) are more affordable and accessible than SUDs. Their capability in image quality have been found as compatible with standard USG machines. They are practical, and learning to use them is easier [9]. Lots of studies have been showing that these devices can be useful as much as SUDs in the evaluation of heart, abdomen, vascular structures, diaphragm and optic nerve [9–12].
Despite existance of some studies using them to evaluate dyspnea or pleural patologies in the ED and ICU, there is no study systematically evaluating and validating them in the use of lung ultrasound and LAS [13, 14]. In this study, we aimed to compare PSUD with SUD in the imaging of pleura, interstitial and alveolar syndromes and in the calculation of LAS.
Materials and methods
Patient population
This prospective observational study was carried out between October.01/2018 and March.01/2019 at the pulmonary critical care unit of our hospital. The study protocol was approved by the ethics committee of our institution (28.12.2015/166), and written informed consent was obtained from the patient or his/her next of kin. Patients who had severe thoracic deformity, thoracic open wound or thoracic bandage were not included in this study. A total of 33 patients who were older than 18 years of age were included in this study.
Clinical data of patients
Acute Physiology and Chronic Health Evaluation (APACHE) II scores, admission diagnosis, underlying chronic diseases, arterial blood gas analysis, and vital signs were recorded for all patients. Then, patients' lung were examined by two physicians independently for A lines, B lines, consolidation pattern, dynamic and static air bronchograms, PE [2]. All measurements were performed at the same region of lung by using SUD and PSUD in randomized order.
USG device
We used Vivid-Q (full range of standard modalities and measurements: MM, 2D, PW, CW, Colour, TVI, and TEE, GE Systems) as a SUD and Vscan (with dual probe, GE Systems) as a PSUD (2D and colour Doppler). LUS was carried out with sector probes of the 2 devices. We used pre-set for abdominal examination option of these two ultrasonography devices to examine lungs.
Measurement methods
Each lung was carefully examined in 11 regions by each ultrasonography devices. We did not evaluate region 8 because of presence of the heart. Patients were taken to the lateral decubitus position to examine 5th, 6th, 11th and 12th areas of lung and supine position was used to assess for other areas of lung. Attention was taken to ensure that the transducer was perpendicular to the ribs and the lung surface. Then the zones were carefully scanned for the presence of A, B1, B2 lines, consolidation pattern, dynamic air bronchograms, static air bronchograms and PE. A lines were defined as reverberation artifact of the pleura which is continuing at equal intervals under pleura with the parallel way of the pleura. B-lines defined as continuous reflections of ultrasound waves caused by small particles entering resonance within lung parenchyma or lung surface as a result of alveolar edema. B1 line is known as non-coalescent or non-attached B line and it can be clearly visualised as a single thin line. B1 lines indicate moderate loss of aeration in the lung, associated with presence of three well-defined spaced B lines in the intercostal space. B2 pattern defined as severe loss of lung aeration displays multiple coalescent B lines/intercostal space [15].
Consolidation pattern were defined as lung becomes to look like a liver (hepatisation) and bronchial tree can visualise in this consolidated tissue by LUS like a punctate echogenic area. If there are moving echogenic small changes with respiratory cycle in this bronchial tree, this mean there are dynamic air bronchogram, if not this mean there are static air bronchogram. For the statistical analysis of data related with PE, we visualized it in the regions of 3, 4, 9, 10 of right and left lungs. At least three different video images were recorded from each region and two intensive care physician (GG, TG) independently examined these recorded video images for all findings offline. Finally, the LAS was calculated for each ultrasonography devices using all these parameters as previously described [2, 6]. The orginal LAS score we used distinguishes four steps of progressive loss of aeration [7, 8], each corresponding to a score: A-lines or two or fewer B-lines (normal aeration, score 0), three or more well-spaced B-lines (moderate loss of aeration, score 1), coalescent B-lines (severe loss of aeration, score 2), tissue-like pattern (complete loss of aeration, score 3;). This score is computed in six region per hemithorax: sternum, anterior, and posterior axillary lines identify anterior, lateral, and posterior areas, each divided into superior and inferior fields. The LAS score of each region (regional LAS score) corresponded to the rounded average score of all pertaining intercostal spaces and ranged from 0 to 3. The global lung ultrasound score corresponds to the sum of each region’s score and ranges from 0 (all regions are well aerated) to 36 (all regions are consolidated) [7, 8]. In our study we did not evaluate zone 8 and our maximum score was 33.
Statistical analysis
The evaluation was carried out with IBM SPSS statistical program version 22. Kappa statistics were used to evaluate the consistency between the devices in the evaluation of alveolar syndrome and pleura. Bland–Altman analysis was used to assess presence of agreement or presence of any significant proportional bias between two ultrasonography devices and to calculate maximum acceptable difference. Upper and lower limits of agreement and the limits of maximum acceptable differences were also calculated. Medcalc statistical analysis programme was used to plot Fig. 1. Interobserver reliability was assessed using the intraclass correlation test. Intraclass correlation coefficient (ICC) greater than 0.7 was taken to indicate a strong correlation.
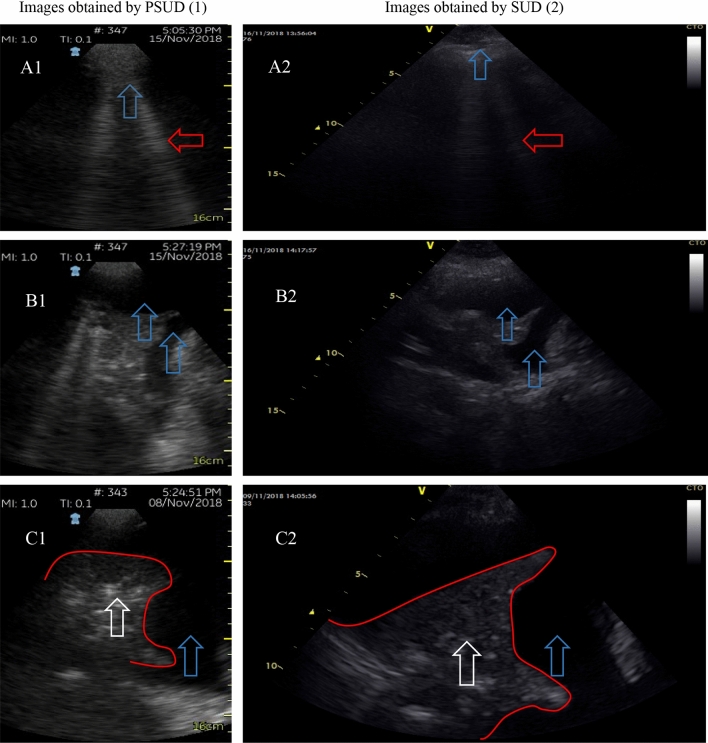
Fig. 1.
Blant Altman test chart comparing standart ultrasonography device and pocked sized ultrasonography device in terms of total aeration score and count of total B2 lines. MAD Maximum accepted difference
Results
Demographic and clinical information of the patients were presented in Table 1. The total LAS, total count of B1, B2, and all B lines were presented in Table 2. According to Bland Altman test, an agreement was found between PSUD and SUD in terms of counting B2 lines and LAS for each lung and for total lung. Also, no proportional bias was detected between PSUD and SUD in terms of counting B2 lines and LAS for each lung and for total lung. But, there was not an agreement between PSUD and SUD according to total number of B1 and B lines. And there was proportional bias between PSUD and SUD according to total number of B1 and B lines (Table 2). The Bland Altman test plots related with the count of B2 lines and LAS values were shown in Fig. 1. Upper and lower limits of agreement and the limits of maximum acceptable differences were given in Fig. 1 also. Maximum acceptable difference for B2 lines was 9 and for LAS was 11. Kappa values for the evaluation of presence or absence of AL was moderate and good. There was good inter class correlation coefficient value as greater than 0.8 between two physicians in terms of counting of total B1, B2, B lines and calculating of total LAS for SUD. Also, there was good inter class correlation coefficient value as greater than 0.7 between two physicians in terms of counting of total B1, B2, B lines and calculating of total LAS for PSUD (Table 2). The compatibility between SUD and PSUD for determination of static air bronchogram, dynamic air bronchogram, consolidation pattern, pleural line, lung sliding was shown in Table 3. Figure 2 shows images recorded with the two devicies in the evaluation of interstitial patterns, consolidation patterns and PE of the patients.
Table 1.
Demographics and clinical findings of the patients
| N = 33 | |
|---|---|
| Age (Years)* | 69.6 ± 15.7 |
| Gender, F/M n (%) | 13 (39.4) / 20 (60.6) |
| BMI (kg/m2)* | 31.0 ± 9.8 |
| APACHE II* | 17.8 ± 6.4 |
| No mechanical ventilation, n (%) | 18 (55) |
| Invasive mechanical ventilation, n (%) | 9 (27) |
| Non-invasive mechanical ventilation, n (%) | 6 (18) |
| Arterial blood gas analysis | |
| PH** | 7.43 (7.39–7.48) |
| PaO2 (mmHg)** | 73.25 (65.47–98.47) |
| PaCO2 (mmHg)** | 42.85 (33.60–50.37) |
| SpO2 (%)** | 95.05 (93.27–98.00) |
| HCO3 (mmol/L)** | 28.05 (23.35–30.05) |
| Lactat (mmol/L)** | 1.40 (1.20–1.90) |
| Admission diagnosis | |
| Cardiovascular disease, n (%) | 24 (72.7) |
| Infection, n (%) | 21 (63.6) |
| COPD, n (%) | 19 (57.6) |
| Renal disease, n (%) | 17 (51.5) |
| Pulmonary edema, n (%) | 17 (51.5) |
| Pleural effusion, n (%) | 17 (51.5) |
| Pneumonia, n (%) | 14 (42.4) |
| Endocrinological disease, n (%) | 12 (36.4) |
| Obstructive sleep apnea syndrome, n (%) | 9 (27.3) |
| Neurological disease, n (%) | 9 (27.3) |
| Pulmonary hypertension, n (%) | 8 (24.2) |
| Sepsis, n (%) | 8 (24.2) |
| Atelectasis, n (%) | 8 (24.2) |
| Bronchiectasis, n (%) | 5 (15.2) |
| Septic shock, n (%) | 2 (6.1) |
| Asthma, n (%) | 2 (6.1) |
N, n number, F female, M male, BMI body mass index, kg/m2 kilogram per square meter, APACHE-II acute physiology and chronic health evaluation score, SOFA sequential organ failure assessment, PaO2 partial arterial oxygen pressure, PaCO2 partial arterial carbon dioxide pressure, SpO2 oxygen saturation
*Mean ± standard deviation
**Median (interquartile range)
Table 2.
Results of Bland Altman and consistency statistics between standard ultrasonography device and pocket sized ultrasound device for B lines and LAS
| Parameter | SUD | PSUD | Agreement P value |
Proportional bias P value |
ICC (SUD) | ICC (PSUD) | |
|---|---|---|---|---|---|---|---|
| Number of B1 lines** | Left lung | 12 [7–15] | 14 [7–20] | 0.003 | 0.001 | 0.864 | 0.834 |
| Right lung | 12 [9–18] | 16 [11–22] | 0.008 | 0.001 | 0.835 | 0.824 | |
| Total | 24 [17–33] | 32 [15–43] | 0.001 | 0.0001 | 0.887 | 0.845 | |
| Number of B2 lines** | Left lung | 4 [1–6] | 3 [2–5] | 0.724*** | 0.271**** | 0.826 | 0.765 |
| Right lung | 4 [2–7] | 3 [1–5] | 0.027 | 0.136 | 0.945 | 0.847 | |
| Total | 6 [3–13] | 6 [2–10] | 0.214*** | 0.138**** | 0.901 | 0.859 | |
| Number of total B lines** | Left lung | 16 [4–20] | 16 [9–25] | 0.003 | 0.045 | 0.938 | 0.857 |
| Right lung | 18 [13–23] | 18 [12–30] | 0.075*** | 0.002 | 0.875 | 0.889 | |
| Total | 35 [22–40] | 38 [20–51] | 0.003 | 0.0001 | 0.962 | 0.885 | |
| LAS** | Left lung | 7 [3–9] | 7 [4–9] | 1.000*** | 0.859**** | 0.846 | 0.657 |
| Right lung | 8 [4–11] | 7 [4–10] | 0.365*** | 0.989**** | 0.944 | 0.954 | |
| Total | 15 [10–19] | 13 [8–16] | 0.510*** | 0.853**** | 0.948 | 0.885 | |
SUD Standart ultrasonography device (Vivid-Q), PSUD pocket sized ultrasonography device (Vscan), LAS lung aeration score, ICC interclass correlation coefficients
*Number (percentage)
**Median value [interquartile range]
***There is agreement (If there is agreement, values were marked as bold under agreement column)
****There is no proportional bias (If there is no proportional bias, values were marked as bold under proportional bias column)
Table 3.
Compatibility for different values of Vivid-Q and Vscan ultrasound devices in different regions of the lung
| Lung area | AL* | SAB* | DAB* | CP* | PL* | LS* | PE* |
|---|---|---|---|---|---|---|---|
| 1 | 0.71 | 0.87 | 0.87 | 0.87 | 0.65 | 0.81 | |
| 2 | 0.61 | 0.75 | 0.80 | 0.75 | 0.51 | 0.64 | |
| 3 | 0.72 | 0.89 | 0.87 | 0.89 | 0.57 | 0.74 | 0.65 |
| 4 | 0.63 | 0.68 | 0.67 | 0.74 | 0.60 | 0.63 | |
| 5 | 0.77 | 0.82 | 0.70 | 0.57 | 0.52 | ||
| 6 | 0.64 | 0.86 | 0.77 | 0.72 | 0.68 | 0.71 | |
| 7 | 0.58 | 0.66 | 0.81 | 0.66 | 0.63 | 0.72 | |
| 8 | 0.59 | 0.88 | 0.88 | 0.89 | 0.57 | 0.81 | 0.73 |
| 9 | 0.62 | 0.60 | 0.65 | 0.65 | 0.55 | 0.67 | |
| 10 | 0.70 | 0.63 | 0.82 | 0.56 | 0.53 | 0.57 | |
| 11 | 0.86 | 0.68 | 0.81 | 0.74 | 0.50 | 0.77 |
AL A lines, SAB static air bronchogram, DAB dynamic air bronchogram, CP consolidation pattern, PL pleural line, LS lung sliding, PE pleural effusion
*Kappa value
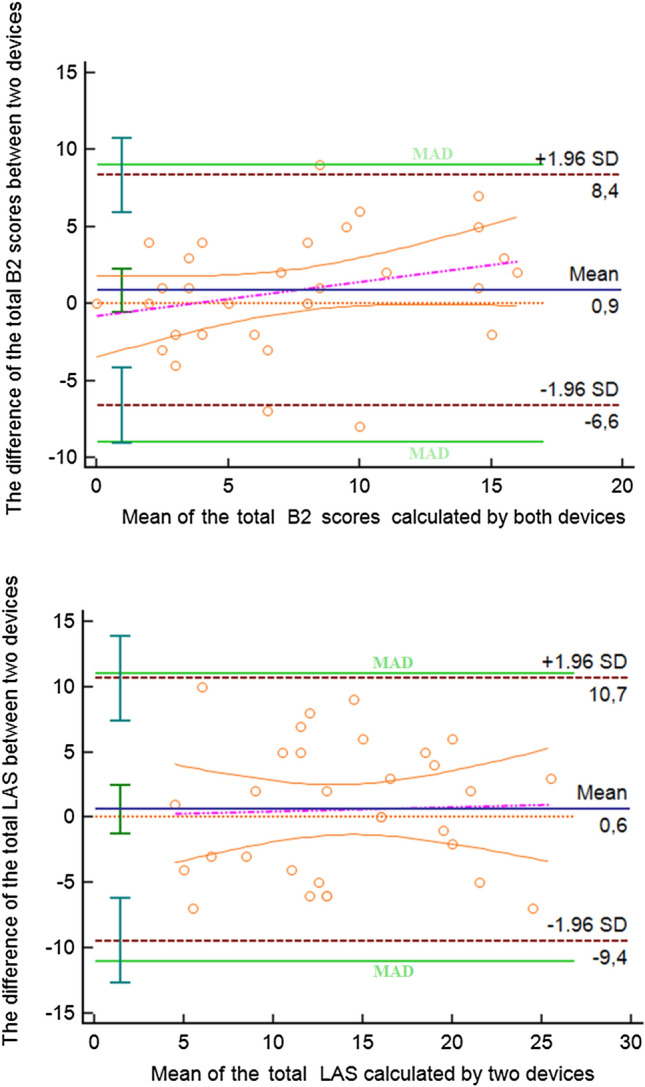
Fig. 2.
Images recorded in the same area with PSUD (1 numbered after letter) and SUD (2 numbered after letter) for (A1,2): pleural line (Blue arrows) and B lines (Red arrows), (B1,2): pleural effusion (Blue arrows), (C1,2): pleural effusion (Blue arrows), atelectatic lung (Red lines) and static air bronchograms (White arrows)
Discussion
A focused lung ultrasound can allow quick assessment of pulmonary edema, pneumonia, PE, and pneumothorax in ICU patients and PSUD has the potential to increase practicality, and usage rate of LUS. Our study showed that PSUD is compatible with SUD in the visualization of consolidation, interstitial patterns, PE and calculation of LAS.
There was good overall agreement for detecting and visualization of PE in our ICU patient population. In PE, ultrasound is useful for diagnosis, prognosis and to guide therapeutic interventions, and it has been used to detect PE for more than 50 years [14]. PE are seen in more than 60% of ICU patients and can be associated with increased duration of mechanical ventilation (MV) and ICU stay [14]. The evidence suggests that ultrasound is superior to chest radiography for detecting PE in ICU patients lying supine position [16]. Additionally, it is known that when ultrasonography is used for pleural imaging, there are some evidence that there is an improvement in patients outcome [17, 18]. Because of these reasons quick, accurate and reliable imaging of PE is very important, and PSUD may have additional value in the increasing of practicality and utility of the pleural assessment. In our study there was good agreement between the visualization of PE with both devices and in both side of the lung. These results suggest that PSUDs can be used for this aim with high reliability. In two previous studies, Dalen [19] and Graven [20] evaluated usability of PSUD for compare it with SUD. Both articles investigating the pleural applications of hand-held ultrasound showed good overall agreement when comparing with high-tech ultrasound systems. In these studies, it was understood that patients were evaluated either in a hospital or in an outpatient clinic. Dalen et al. found a high sensitivity, specificity and positive and negative predictive values when evaluating PE with a PSUD. Graven et al. found that nurses from cardiology department can successfully assess and obtain reliable measurements of the pleural and pericardial cavities in all participating patients [19, 20]. PSUDs detect PE with higher sensitivity and specificity than chest X-Ray, and provide valuable information about the size and depth of the PE, the echogenicity of the fluid, the presence of septated or loculated fluid, pleural thickening and nodularity, and the presence of any contralateral PE.
As can be seen on the Table 3, agreement between both devices was very low in the evaluation of pleural line. This can be explained by the use of sector probe [21]. We used this probe in order to better visualize deep part of the lung. If the indication of LUS examination is pleural evaluation for example pneumothorax, linear probe should be used.
The second important LUS pattern that we evaluated in this study was alveolar sydrome, including dynamic and static air bronchograms and consolidation patterns. When the lung density increases and the tissue air ratio is high, LUS will reveal an anatomical solid tissue-like pattern that has been named as alveolar syndrome. Like interstitial syndrome, alveolar syndrome is a non-specific sonographic finding in many different lung conditions. They can be seen in pneumonia, ARDS, atelectasis, pulmonary contusions and pulmonary infarcts [22]. In our study, we compared two devices in the imaging of consolidation pattern region by region, and we found that there was very good agreement in both lung as in many regions of lung. Our results suggest that PSUDs can be used in the evaluation of consolidation pattern with similar reliability of SUDs. But, we could not find any study evaluating PSUDs in the evaluation of alveolar sydrome. Additionaly as we can see in Fig. 2c it is possible to detect alveolar patterns under the PE with LUS as we can see thorax CT. It is difficult to detect pneumonia or atelectasis under the PE with chest x-ray in lying ICU patients. Our results suggest that PSUD can be very useful in the evaluation of alveolar syndrome in ICU patients but further studies are necessary to confirm these findings.
After evaluation of pleura the most frequent use of LUS in the clinical practice is the evaluation of B lines. In recent years, the usage of LUS and B lines in the evaluation of lung edema and decision for diuretics and ultrafiltration requirement have been increased [2, 23]. Recently, recommendations related with these usage can be found in the cardiology guidelines [24, 25]. Counting of the B-line can allow serial monitoring of patients for pulmonary edema. The higher number of B-line in heart failure and dialysis patients are associated with higher risk of death.
In our study both device showed very similar mean number of B lines in each lung and the same results were also obtained for the total number of B1 and B2 lines. While there was no significant difference between the devices in terms of total B2 lines in Blant Altman analysis, there were no agreement and proportional bias was exist beween the two devices in total B1 lines and total B lines. Most likely explanation would be related with clip duration. This explanation is supported by when we look at the mean number of B lines, we can see that the number of B lines is higher with PSUD than obtained with by SUD. Because, it has been shown that shorter clips can underestimate the number of B-lines seen [26, 27]. Platz et al. compared a PSUD with high-end USG device for the impact of different duration of ultrasound clips on the measured number of B lines [26]. They identified that there was a higher number of B-lines on the 4 s LUS clips by comparison with 2 s LUS clips and on the 6 s LUS clips by comparasion with 4 s LUS clips. In our study, devices clip duration was 3 s for SUD and 6 s for PSUD. This can explane why mean number of B lines higher with PSUD than SUD. Second reason would be that there can be poor intra-class agreement between measurements of the same physician. Gullett et al. evaluated inter-rater and intra-rater agreement in the counting of B line numbers by using ICC test for the patients who admitted to the ED with acute undifferentiated dyspnea [28]. In this study, the inter-rater correlation coefficients were found to be 0.697 for 733 zones and 0.647 for 266 zones, respectively and intra-rater correlation coefficients were found to be 0.676 and 0.586, respectively. These results could suggest that there was potential bias perceived by the sonographers for ordinal assessment of B-line concentration [28]. In our study, we did not calculate intra-rater agreement but our results could have been influenced from this factor. Thirdly, it may be related with time difference and changing in the patient position during this period. Earlier studies showed that changing in patient position from supine to the semirecumbent may decrease B line numbers in the same lung regions [29]. The number of B-lines may also change within minutes following a change in position from sitting to supine [29]. All these findings suggest that measurement of B lines with PSUDs is reliable, but further studies require to standardize the method. Lastly and interestingly, despite the existence of statistically significant difference between the mean number of B lines recorded and counted with both devices, there was no significant difference the calculated LAS or extravascular lung water (EVLW) scores between two devices [1]. Unlike the LAS system EVLW scoring system is based on B line scoring, evaluates 28 zones and generally is used in patients with heart failure and pulmonary edema and both system screen similar lung areas (Table 4). Our mean B line number with PSUD and SUD were 38 and 35 respectively and if we were used 28 zone EVLW scoring system, these numbers were going to be classified as score 3.
Table 4.
The scoring systems for the severity of the B lines
| Score | Number of B-Lines | EVLW |
|---|---|---|
| 0 | ≤ 5 | Absent |
| 1 | 6–15 | Mild degree |
| 2 | 16–30 | Moderate degree |
| 3 | > 30 | Severe degree |
EVLW Extravascular lung water score. Referance 1
At the end of the study, we aimed to investigate the agreement between the calculated LASs by the two devices. We found that the best consistency between the devices was seen in the evaluation of LAS. When we analyse the mean scores of the measurements they were very similar, and there were no significant difference between the mean scores. A LAS was proposed and successfully applied to assess rearation in ventilator associated pneumonia, predict weaning failure from mechanical ventilation and monitor aeration in ECMO patients [3, 7, 30, 31]. A daily LAS assessment can be used to monitor of the respiratory disease. The LAS may guide fluid management in septic ARDS patients: in this setting, the LAS score variations are more sensitive than oxygenation in early detection of lung aeration deterioration due to fluid loading [32–34]. In patients with ARDS, the regional lung ultrasound score is strongly correlated with tissue density assessed with quantitative computed tomography (CT), and the increase in lung volume induced by positive end-expiratory pressure (PEEP) in patients with ARDS [33, 34]. The LAS can help in the weaning from mechanical ventilation. After a successful weaning trial, patients who will experience post-extubation distress have a higher LAS than those successfully extubated [30].
To date, however, the comparison of PSUD and SUD in the evaluation of LAS has never been performed. To our knowledge, this is the first study comparing PSUD with SUD to assess LAS in these patients through bedside ultrasound.
Limitations of the study
We have some limitations in our study; we used phased array probe for the measurements although it would be more reliable to use linear probe [21]. Default recording time of our devices were different and this might have beeen cause to count B lines differently.
In our study we used 12 area scoring system but we evaluated only 11 areas; Because of bad image quality we excluded zone 8. But we believe that absence of zone 8 evaluation negatively influenced our conclusion since our study is a technical study comparing devices’ capability of imaging zone by zone. Additionally we didnt make a clinical decision according to our results such as to start or stop antibiotic or diuretic therapy. Lastly it is possible to find other studies in literature which use 11 zones [35, 36]. Patients changed position, affecting measures and limiting any form of standardising. Lastly we didn’t evaluated intra-operator agreement.
Conclusions
We have found PSUD to be in good overall agreement with high-end ultrasound systems in the detections of PE, alveolar syndrome, consolidation patterns and calculation of LAS. Further research is needed with more standardized comparison for B-line evaluation by PSUDs.
Acknowledgements
This work was supported by a Gazi University Scientific Research Foundation grant (BAP 01/45/2015)
Compliance with ethical standards
Conflicts of interest
The authors declare that they have no conflicts of interest.
Informed consent
The study protocol was approved by the ethics committee of our institution (28.12.2015/166), and written informed consent was obtained from the patient or his/her next of kin.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tuba Güney, Email: kartolum@gmail.com.
Gül Gürsel, Email: gurselgl@gmail.com.
Uğur Özdemir, Email: ugureuzdemir@gmail.com.
Ömer Tekin, Email: omertek90@hotmail.com.
Meltem Çimen, Email: meltem.cimen35@gmail.com.
Ayşen Mamadova, Email: aysenmammadova665@gmail.com.
Nur Karaaslan, Email: nurkaraaslan@outlook.com.
References
- 1.Picano E, Pellikka PA. Ultrasound of extravascular lung water: a new standard for pulmonary congestion. Eur Heart J. 2016;37(27):2097–2104. doi: 10.1093/eurheartj/ehw164Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ren H, Song B, Li P, et al. The effects of high-volume hemofiltration by different ultrasound directing on extra vascular lung water index in patients with septic shock. Iran J Public Health. 2018;47(9):1245–1253. [PMC free article] [PubMed] [Google Scholar]
- 3.Mongodi S, Pozzi M, Orlando A, et al. Lung ultrasound for daily monitoring of ARDS patients on extracorporeal membrane oxygenation: preliminary experience. Intensive Care Med. 2018;44(1):123–124. doi: 10.1007/s00134-017-4941-7. [DOI] [PubMed] [Google Scholar]
- 4.Volpicelli G, Elbarbary M, Blaivas M, et al. International liaison committee on lung ultrasound (ILC-LUS) for ınternational consensus conference on lung ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38(4):577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 5.Mayo PH, Copetti R, Feller-Kopman D, et al. Thoracic ultrasonography: a narrative review. Intensive Care Med. 2019;45(9):1200–1211. doi: 10.1007/s00134-019-05725-8. [DOI] [PubMed] [Google Scholar]
- 6.Bello G, Blanco P. Lung ultrasonography for assessing lung aeration in acute respiratory distress syndrome: a narrative review. J Ultrasound Med. 2019;38(1):27–37. doi: 10.1002/jum.14671. [DOI] [PubMed] [Google Scholar]
- 7.Bouhemad B, Liu ZH, Arbelot C, et al. Ultrasound assessment of antibiotic-induced pulmonary reaeration in ventilator-associated pneumonia. Crit Care Med. 2010;38:84–92. doi: 10.1097/CCM.0b013e3181b08cdb. [DOI] [PubMed] [Google Scholar]
- 8.Bouhemad B, Brisson H, Le-Guen M, et al. Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med. 2011;183:341–347. doi: 10.1164/rccm.201003-0369OC. [DOI] [PubMed] [Google Scholar]
- 9.Rykkje A, Carlsen JF, Nielsen MB. Hand-held ultrasound devices compared with high-end ultrasound systems: a systematic review. Diagnostics Basel. 2019 doi: 10.3390/diagnostics9020061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gursel G, Inci K, Alasgarova Z. Can diaphragm dysfunction be reliably evaluated with pocket-sized ultrasound devices in intensive care unit? Crit Care Res Pract. 2018 doi: 10.1155/2018/5192647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Özdemir U, Çimen M, Güney T, et al. Validity and reliability of pocket-sized ultrasound devices in measurement of optic nerve sheath diameter in ICU patients. J Clin Monit Comput. 2019 doi: 10.1007/s10877-019-00351-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pujol S, Laurent J, Markarian T, et al. Compression with a pocket-sized ultrasound device to diagnose proximal deep vein thrombosis. Am J Emerg Med. 2018;36(7):1262–1264. doi: 10.1016/j.ajem.2018.03.076. [DOI] [PubMed] [Google Scholar]
- 13.Sforza A, Mancusi C, Carlino MV, et al. Diagnostic performance of multi-organ ultrasound with pocket-sized device in the management of acute dyspnea. Cardiovasc Ultrasound. 2017;15(1):16. doi: 10.1186/s12947-017-0105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mattison LA, Coppage L, Alderman DF, et al. Pleural effusions in the medical ICU: prevalence, causes, and clinical implications. Chest. 1997;111:1018–1023. doi: 10.1378/chest.111.4.1018. [DOI] [PubMed] [Google Scholar]
- 15.Goffi A, Kruisselbrink R, Volpicelli G. The sound of air: point-of-care lung ultrasound in perioperative medicine. Can J Anaesth. 2018;65(4):399–416. doi: 10.1007/s12630-018-1062-x. [DOI] [PubMed] [Google Scholar]
- 16.Winkler MH, Touw HR, van de Ven PM, et al. Diagnostic accuracy of chest radiograph, and when concomitantly studied lung utrasound, in critically ill patients with respiratory symptoms: a systematic review and meta-Analysis. Crit Care Med. 2018;46(7):707–714. doi: 10.1097/CCM.0000000000003129. [DOI] [PubMed] [Google Scholar]
- 17.Perazzo A, Gatto P, Barlascini C, et al. Can ultrasound guidance reduce the risk of pneumothorax following thoracentesis? J Bras Pneumol. 2014;40(1):6–12. doi: 10.1590/S1806-37132014000100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goligher EC, Leis JA, Fowler RA, et al. Utility and safety of draining pleural effusions in mechanically ventilated patients: a systematic review and meta-analysis. Crit Care. 2011;15(1):46. doi: 10.1186/cc10009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dalen H, Gundersen GH, et al. Feasibility and reliability of pocket-size ultrasound examinations of the pleural cavities and vena cava inferior performed by nurses in an outpatient heart failure clinic. Eur J Cardiovasc Nurs J Work Group Cardiovasc Nurs Eur Soc Cardiol. 2015;14:286–293. doi: 10.1177/1474515114547651. [DOI] [PubMed] [Google Scholar]
- 20.Graven T, Wahba A, Hammer AM, et al. Focused ultrasound of the pleural cavities and the pericardium by nurses after cardiac surgery. Scand Cardiovasc J. 2015;49(1):56–63. doi: 10.3109/14017431.2015.1009383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mongodi S, Bouhemad B, Orlando A, et al. Modified lunf ultrasound score for assessing and monitoring pulmonary aeration. Ultraschall Med. 2017;38(5):530–537. doi: 10.1055/s-0042-120260. [DOI] [PubMed] [Google Scholar]
- 22.Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J, et al. Accuracy of Lung Ultrasonography in the Diagnosis of pneumonia in adults: systematic review and meta-analysis. Chest. 2017;151(2):374–382. doi: 10.1016/j.chest.2016.10.039. [DOI] [PubMed] [Google Scholar]
- 23.Russell FM, Ehrman RR, Ferre R, et al. Design and rationale of the B-lines lung ultrasound guided emergency department management of acute heart failure (BLUSHED-AHF) pilot trial. Heart Lung. 2019;48(3):186–192. doi: 10.1016/j.hrtlng.2018.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 25.Mebazaa A, Tolppanen H, Mueller C, et al. Acute heart failure and cardiogenic shock: a multidisciplinary practical guidance. Intensive Care Med. 2016;42(2):147–163. doi: 10.1007/s00134-015-4041-5. [DOI] [PubMed] [Google Scholar]
- 26.Platz E, Pivetta E, Merz AA, et al. Impact of device selection and clip duration on lung ultrasound assessment in patients with heart failure. Am J Emerg Med. 2015;33(11):1552–1556. doi: 10.1016/j.ajem.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pivetta E, Baldassa F, Masellis S, et al. Sources of variability in the detection of B-lines. Using Lung Ultrasound Ultrasound Med Biol. 2018;44(6):1212–1216. doi: 10.1016/j.ultrasmedbio.2018.02.018. [DOI] [PubMed] [Google Scholar]
- 28.Gullett J, Donnelly JP, Sinert R, et al. Interobserver agreement in the evaluation of B-lines using bedside ultrasound. J Crit Care. 2015;30(6):1395–1399. doi: 10.1016/j.jcrc.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 29.Frasure SE, Matilsky DK, Siadecki SD, et al. Impact of patient positioning on lung ultrasound findings in acute heart failure. Eur Heart J Acute Cardiovasc Care. 2015;4(4):326–332. doi: 10.1177/2048872614551505. [DOI] [PubMed] [Google Scholar]
- 30.Soummer A, Perbet S, Brisson H, et al. Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress. Crit Care Med. 2012;40:2064–2072. doi: 10.1097/CCM.0b013e31824e68ae. [DOI] [PubMed] [Google Scholar]
- 31.Lu X, Arbelot C, Schreiber A, et al. Ultrasound assessment of lung aeration in subjects supported by venovenous extracorporeal membrane oxygenation. Respir Care. 2019 doi: 10.4187/respcare.06907. [DOI] [PubMed] [Google Scholar]
- 32.Yin W, Zou T, Qin Y, et al. Chinese Critical Ultrasound Study Group (CCUSG). Poor lung ultrasound score in shock patients admitted to the ICU is associated with worse outcome. BMC Pulm Med. 2019;19(1):1. doi: 10.1186/s12890-018-0755-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mongodi S, Algieri I, Mojoli F, et al. CT-scan and ultrasound comparative assessment of lung aeration In ARDS. Intensive Care Med. 2014;40(1):127–128. [Google Scholar]
- 34.Chiumello D, Mongodi S, Algieri I, et al. Assessment of lung aeration and recruitment by CT scan and ultrasound in acute respiratory distress syndrome patients. Crit Care Med. 2018;46(11):1761–1768. doi: 10.1097/CCM.0000000000003340. [DOI] [PubMed] [Google Scholar]
- 35.Volpicelli G, Caramello V, Cardinale L, et al. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med. 2008;26:585–591. doi: 10.1016/j.ajem.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 36.Cortellaro F, Ceriani E, Spinelli M, et al. Lung ultrasound for monitoring cardiogenic pulmonary edema. Intern Emerg Med. 2017;12:1011–1017. doi: 10.1007/s11739-016-1510-y. [DOI] [PubMed] [Google Scholar]