Key Points
Question
Is patient-physician racial/ethnic or gender concordance associated with the patient experience as measured by scores on the Press Ganey Outpatient Medical Practice Survey?
Findings
In this cross-sectional analysis of 117 589 Press Ganey surveys completed for the adult outpatient practices of an urban, academic health system from 2014 to 2017, physicians among racially/ethnically discordant patient-physician dyads had significantly lower odds of receiving the maximum patient experience score compared with those among concordant dyads.
Meaning
In this study, higher Press Ganey survey scores were associated with racial/ethnic concordance between patients and their physicians; thus, efforts to improve the patient experience among racially/ethnically discordant patient-physician dyads may be necessary to improve health care delivery.
This cross-sectional study evaluates the associations between the patient experience as measured by scores on the Press Ganey Outpatient Medical Practice Survey and patient-physician racial/ethnic and gender concordance.
Abstract
Importance
The Press Ganey Outpatient Medical Practice Survey is used to measure the patient experience. An understanding of the patient- and physician-related determinants of the patient experience may help identify opportunities to improve health care delivery and physician ratings.
Objective
To evaluate the associations between the patient experience as measured by scores on the Press Ganey survey and patient-physician racial/ethnic and gender concordance.
Design, Setting, and Participants
A cross-sectional analysis of Press Ganey surveys returned for outpatient visits within the University of Pennsylvania Health System between 2014 and 2017 was performed. Participants included adult patient and physician dyads for whom surveys were returned. Data analysis was performed from January to June 2019.
Exposures
Patient-physician racial/ethnic and gender concordance.
Main Outcomes and Measures
The primary outcome was receipt of the maximum score for the “likelihood of your recommending this care provider to others” question in the Care Provider domain of the Press Ganey survey. Secondary outcomes included each of the remaining 9 questions in the Care Provider domain. Generalized estimating equations clustering on physicians with exchangeable intracluster correlations and cluster-robust standard errors were used to investigate associations between the outcomes and patient-physician racial/ethnic and gender concordance.
Results
In total, 117 589 surveys were evaluated, corresponding to 92 238 unique patients (mean [SD] age, 57.7 [15.6] years; 37 002 men [40.1%]; 75 307 White patients [81.6%]) and 747 unique physicians (mean [SD] age 45.5 [10.6] years; 472 men [63.2%]; 533 White physicians [71.4%]). Compared with racially/ethnically concordant patient-physician dyads, discordance was associated with a lower likelihood of physicians receiving the maximum score (adjusted odds ratio [OR], 0.88; 95% CI, 0.82-0.94; P < .001). Black (adjusted OR, 0.73; 95% CI, 0.68-0.78; P < .001) and Asian (adjusted OR, 0.55; 95% CI, 0.50-0.60; P < .001) patient race were both associated with lower patient experience ratings. Patient-physician gender concordance was not associated with Press Ganey scores (adjusted OR, 1.00; 95% CI, 0.96-1.04; P = .90).
Conclusions and Relevance
In this study, higher Press Ganey survey scores were associated with racial/ethnic concordance between patients and their physicians. Efforts to improve physician workforce diversity are imperative. Delivery of health care in a culturally mindful manner between racially/ethnically discordant patient-physician dyads is also essential. Furthermore, Press Ganey scores may differ by a physician’s patient demographic mix; thus, care must be taken when publicly reporting or using Press Ganey scores to evaluate physicians on an individual level.
Introduction
The patient experience is at the heart of patient-centered medical care. There have been increasing efforts not only to measure the patient experience but also to publicly share patient ratings for individual physicians, sometimes linking patient ratings to physician employment and compensation,1 with the ultimate goal of motivating improvements in health care delivery. The Press Ganey (PG) Outpatient Medical Practice Survey2 is used by many practices to evaluate the patient experience. Despite its wide use, the associations between the patient experience and patient, physician, and clinical encounter characteristics remain unclear.
Much work has focused on patient and physician race/ethnicity or gender and their associations with the patient experience and specific aspects of the patient-physician relationship.3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21 The existing studies on this topic are quite heterogenous in terms of populations evaluated, methods used, and outcomes measured, which may, in part, contribute to mixed findings. Although some studies suggest that there are benefits associated with patient-physician racial/ethnic or gender concordance,8,10,11,12,19 others do not.5,13,14,15,16,17,18,19,21 In light of existing racial/ethnic and gender health and health care disparities,22 as well as increasing diversification of the US population,23 a better understanding of the associations between patient and physician demographics and the patient experience of health care is a necessary and important step toward our collective goal of achieving health equity. Furthermore, an evaluation of these associations is critical to quality improvement efforts and appropriate interpretation and use of patient experience ratings. Many of the existing studies of the PG survey have been limited by relatively narrow patient populations, exclusion of patient and physician characteristics that may be important determinants of the patient experience, or focus on specific medical specialties.5,10,20,24 We evaluated the associations between the patient experience as measured by the PG survey and patient-physician racial/ethnic and gender concordance among a diverse, urban, ambulatory patient population across all medical specialties.
Methods
Study Design and Data Sources
We conducted a cross-sectional analysis to evaluate the associations between the patient experience, as measured by PG scores obtained from the PG Outpatient Medical Practice Survey, and patient-physician racial/ethnic and gender concordance. Our primary data source was patient experience surveys, including the complete PG survey and components of the Clinician and Group Consumer Assessment of Healthcare Providers and Systems (CG CAHPS) surveys (eAppendix in the Supplement)25 for outpatient visits within the University of Pennsylvania Health System (UPHS) between July 2, 2014, and May 30, 2017. Patient and clinical encounter characteristics were obtained from the survey and the electronic medical record; physician characteristics were obtained from the University of Pennsylvania faculty database.
This study was approved by the University of Pennsylvania institutional review board. A waiver of informed consent was approved because the data were deidentified. The study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.26
The PG survey evaluates 6 domains (Access, Moving Through Your Visit, Nurse/Assistant, Care Provider, Personal Issues, and Overall Assessment) with 2 to 10 Likert-type item questions per domain and 5 answer options ranging from 1 (very poor) to 5 (very good).2 Paper or electronic surveys were sent to all patients who received outpatient care within UPHS. Patients did not receive surveys if they declined solicitation or did not have a valid mailing or email address on file. The survey response rate during the study period was 19.9%.
Study Population
The study included returned surveys for all adult (aged ≥18 years old) outpatient visits with nontrainee physicians within UPHS during the study period. Surveys were excluded if any of the following applied: (1) clinician lacked MD or DO credentials; (2) patient or physician age, gender, or race/ethnicity was missing; (3) patient or physician race/ethnicity other than non-Hispanic White (hereafter referred to as White), non-Hispanic Black (hereafter referred to as Black), non-Hispanic Asian (including Southeast Asians and Pacific Islanders; hereafter referred to as Asian), or Hispanic ethnicity of any race (hereafter referred to as Hispanic); or (4) the primary outcome was missing. Only the first survey for any patient-physician pair was included, resulting in 1 survey for each unique patient-physician pair (eFigure 1 in the Supplement).
Definitions of Exposures and Covariates
Exposures
The primary exposures were patient-physician racial/ethnic and gender concordance. Concordance was evaluated both as a binary measure and by specific patient-physician racial/ethnic and gender pairs. Patient race/ethnicity was obtained from self-report in the CG CAHPS survey or, if unavailable, from the medical record. Patient gender was obtained from the medical record. Self-reported physician race/ethnicity and gender were obtained from the university’s faculty database. Race/ethnicity was categorized as White, Black, Asian, or Hispanic. Gender was categorized as male or female.
Covariates: Patient, Physician, and Clinical Encounter Variables
Other patient characteristics included age, marital status, insurance, highest education level, median annual household income of the patient’s zip code of residence, primary language, overall health, overall mental or emotional health, and level of assistance with survey completion. Highest education level, overall health, overall mental or emotional health, and level of assistance with survey completion were patient-reported from the survey. All other variables were self-reported and obtained from the medical record.
Other physician characteristics were obtained from the university’s faculty database and included self-reported age, type of medical degree, additional degrees, and faculty track and rank. Clinical encounter characteristics were obtained from the medical record and included medical specialty, visit type, location, and year.
Definitions of Outcomes
Primary Outcome
The primary outcome was derived from the score for the item, “Likelihood of your recommending this care provider to others” in the Care Provider domain of the PG survey. Because the responses were highly skewed, with most scores clustered at the high values, we primarily used the top box scoring method, whereby scores were dichotomized as 5 (maximum score) vs less than 5.2 This method is consistent with current practices for patient experience score reporting.10,24,27,28 We also reported mean scores on a 1 to 5 scale.29
Secondary Outcomes
Each of the remaining 9 questions under the Care Provider domain of the PG survey served as secondary outcomes. Each secondary outcome score was dichotomized as 5 vs less than 5.
Statistical Analysis
Patient, physician, and clinical encounter characteristics were summarized with descriptive statistics. To investigate associations between each outcome and patient-physician racial/ethnic and gender concordance, we used generalized estimating equations clustering on physicians with exchangeable intracluster correlations and cluster-robust standard errors to obtain population-averaged estimates of statistical associations. We used purposeful selection to build the multivariable regression model for the primary outcome.30 Patient and physician age, gender, and race were included in all models, as well as any patient, physician, or clinical encounter characteristics that were significantly associated with the primary outcome at α level of .05 in univariable analyses. For the models using binary racial/ethnic or gender concordance, physician race/ethnicity or gender, respectively, were excluded to avoid overfitting. For the regression models evaluating the associations between specific patient-physician racial/ethnic or gender pairs and the primary outcome, indicator variables for race/ethnicity or gender of the patient and physician and their interaction term (product), respectively, were included. To compare the odds of the outcome for each specific patient-physician racial/ethnic or gender pairs, we computed the odds ratios (ORs) from the linear combinations of each discordant pair from their respective final regression models. Associations between secondary outcomes and patient-physician racial/ethnic and gender concordance were evaluated using the final multivariable models for the association between the primary outcome and racial/ethnic and gender concordance, respectively. Concordant race/ethnicity or gender served as the reference in all models. P values were not adjusted for multiplicity for the secondary outcomes because they were exploratory in nature. Statistical analyses were performed using Stata statistical software version 15 (StataCorp). Statistical significance was determined by 2-sided P values at P < .05. Data analysis was performed from January to June 2019.
Results
Study Population
The total number of surveys during the study period was 246 138, representing 124 957 unique patients and 2249 unique physicians. After application of study selection criteria (eFigure 1 in the Supplement), the number of surveys was 117 589, representing 92 238 unique patients and 747 unique physicians.
Patient, Physician, and Clinical Encounter Characteristics
Patient characteristics are summarized in Table 1. The mean (SD) age was 57.7 (15.6) years, and 37 002 patients (40.1%) were men. The racial/ethnic distribution was majority White (75 307 patients [81.6%]) followed by Black (11 759 patients [12.7%]), Asian (3087 patients [3.3%]), and Hispanic (2085 patients [2.3%]). Most patients had commercial insurance (49 537 patients [53.7%]) and reported being at least a 4-year college graduate (55 255 patients [59.9%]). The mean (SD) median annual household income was $78 834 ($31 470).
Table 1. Patient Characteristics.
| Characteristic | Unique patients, No. (%) (N = 92 238) |
|---|---|
| No. of surveys per patient | |
| Mean (SD) | 1.27 (0.65) |
| Median (IQR) | 1 (1-1) |
| Age, y | |
| Mean (SD) | 57.7 (15.6) |
| Median (IQR) | 60 (48-69) |
| Male | 37 002 (40.1) |
| Race/ethnicity | |
| White | 75 307 (81.6) |
| Black | 11 759 (12.7) |
| Asian | 3087 (3.3) |
| Hispanic | 2085 (2.3) |
| Marital status | |
| Single | 21 241 (23.0) |
| Married or with a partner | 59 590 (64.6) |
| Divorced or widowed | 10 987 (11.9) |
| Other | 420 (0.46) |
| Insurance | |
| Commercial | 49 537 (53.7) |
| Medicare | 30 328 (32.9) |
| Medicaid | 3617 (3.9) |
| Tricare or Veterans Affairs | 589 (0.64) |
| Workers’ compensation | 383 (0.42) |
| Mixed | 5462 (5.9) |
| Other | 2322 (2.5) |
| Education | |
| Up to high school or general education diploma | 15 408 (16.7) |
| Some college | 20 593 (22.3) |
| 4-y College graduate | 20 034 (21.7) |
| More than 4-y college graduate | 35 221 (38.2) |
| Unknown | 982 (1.1) |
| Median annual household income, $ | |
| Mean (SD) | 78 834 (31 470) |
| Median (IQR) | 76 464 (56 634-97 452) |
| Primary language English | 91 363 (99.1) |
| Survey assistance | |
| Read questions | 578 (0.63) |
| Wrote answers | 688 (0.75) |
| Answered for me | 1294 (1.4) |
| Translation | 115 (0.12) |
| Other | 250 (0.27) |
| None | 88 312 (95.7) |
| Unknown | 1001 (1.1) |
| Overall health | |
| Poor | 2807 (3.0) |
| Fair | 12 790 (13.9) |
| Good | 29 582 (32.1) |
| Very good | 33174 (36.0) |
| Excellent | 13 327 (14.4) |
| Unknown | 558 (0.60) |
| Overall mental or emotional health | |
| Poor | 1293 (1.4) |
| Fair | 7748 (8.4) |
| Good | 19 861 (21.5) |
| Very good | 32 049 (34.7) |
| Excellent | 30 765 (33.4) |
| Unknown | 522 (0.57) |
Abbreviation: IQR, interquartile range.
Physician characteristics are summarized in Table 2. The mean (SD) age was 45.5 (10.6) years, and 472 (63.2%) were men. Racial/ethnic distribution was majority White (533 physicians [71.4%]) followed by Asian (157 physicians [21.0%]), Black (34 physicians [4.6%]), and Hispanic (23 physicians [3.1%]). Most physicians had an MD degree (737 physicians [98.7%]) and were assistant professors (375 physicians [50.2%]). Patient characteristics stratified by physician race/ethnicity are summarized in eTable 1 in the Supplement.
Table 2. Physician Characteristics.
| Characteristic | Unique physicians, No. (%) (N = 747) |
|---|---|
| No. of surveys per physician | |
| Mean (SD) | 157.4 (162.2) |
| Median (IQR) | 114 (46-213) |
| Age, y | |
| Mean (SD) | 45.5 (10.6) |
| Median (IQR) | 43 (37-53) |
| Male | 472 (63.2) |
| Race/ethnicity | |
| White | 533 (71.4) |
| Black | 34 (4.6) |
| Asian | 157 (21.0) |
| Hispanic | 23 (3.1) |
| Credentials | |
| MD | 737 (98.7) |
| DO | 10 (1.3) |
| Additional degree | |
| PhD | 69 (9.2) |
| Other | 84 (11.2) |
| None | 594 (79.5) |
| Faculty track | |
| Clinician | 91 (12.2) |
| Academic clinician | 255 (34.1) |
| Clinician educator | 274 (36.7) |
| Tenure | 57 (7.6) |
| Other | 70 (9.4) |
| Faculty rank | |
| Assistant professor | 375 (50.2) |
| Associate professor | 163 (21.8) |
| Professor | 165 (22.1) |
| Other | 44 (5.9) |
Abbreviation: IQR, interquartile range.
Clinical encounter characteristics are summarized in Table 3. Most encounters represented return visits (75 844 encounters [64.5%]) and were for medical (40 010 encounters [34.0%]) and surgical (35 116 encounters [29.9%]) specialties.
Table 3. Clinical Encounter Characteristics.
| Characteristic | Clinical encounters, No. (%) (N = 117 589) |
|---|---|
| Specialtya | |
| Medical | 40 010 (34.0) |
| Surgical | 35 116 (29.9) |
| Dermatology | 16 289 (13.9) |
| Other | 26 174 (22.3) |
| Visit type | |
| New | 39 428 (33.5) |
| Return | 75 844 (64.5) |
| Procedure | 2316 (2.0) |
| Location | |
| Main | 49 051 (41.7) |
| Affiliated, Philadelphia | 42 569 (36.2) |
| Satellite, Pennsylvania | 22 568 (19.2) |
| Satellite, New Jersey | 3401 (2.9) |
| Survey year | |
| 2014 | 16 654 (14.2) |
| 2015 | 37 836 (32.2) |
| 2016 | 43 340 (36.9) |
| 2017 | 19 759 (16.8) |
Medical specialties included family practice, general internal medicine, and all internal medicine specialties. Surgical specialties included anesthesia or pain, and cardiac; colorectal; ear, nose, and throat; gastrointestinal; neurologic; oncologic; orthopedic; plastic; thoracic; trauma; transplant; urologic; and vascular surgery. The other specialty category includes neurology, obstetrics-gynecology, ophthalmology, palliative care, physical medicine and rehabilitation, psychiatry, and radiology.
Racial/Ethnic Concordance
Primary Outcome
Overall, physicians in 67 504 of 77 051 (87.6%) racially/ethnically concordant patient-physician encounters received the maximum score, compared with physicians in 33 280 of 40 538 (82.1%) discordant patient-physician encounters (a 5.5-point difference). In adjusted analyses, physicians in racially/ethnically discordant patient-physician pairs were significantly less likely to receive the maximum score compared with those in concordant pairs (adjusted OR, 0.88; 95% CI, 0.82-0.94; P < .001).
The proportions of encounters in which physicians received the maximum score and the mean scores for encounters by specific patient-physician racial/ethnic pairs are summarized in Table 4. The distribution of scores differs by physician race/ethnicity within each patient racial/ethnic group but also differs by patient racial/ethnic group. White patients were generally most likely to provide the maximum score for their physicians across all physician racial/ethnic groups (range, 84.9% [3025 of 3562 encounters] to 87.9% [65 775 of 74 850 encounters]; mean score, 4.80 among all physicians), whereas Asian patients were the least likely to provide the maximum score for their physicians (range 70.3% [116 of 165 encounters] to 76.5% [78 of 102 encounters]; mean score, 4.61 among all physicians).
Table 4. Distribution of Press Ganey Scores by Patient-Physician Racial/Ethnic Pairs.
| Physician race/ethnicity and Press Ganey score | Patients, No. (%) | P valuea | |||
|---|---|---|---|---|---|
| White | Black | Asian | Hispanic | ||
| Any race/ethnicity | |||||
| Very good | 84 669 (87.4) | 11 292 (78.3) | 2767 (73.4) | 2056 (81.5) | <.001 |
| Good | 8302 (8.6) | 2307 (16.0) | 715 (19.0) | 305 (12.1) | |
| Fair | 1895 (2.0) | 433 (3.0) | 175 (4.6) | 80 (3.2) | |
| Poor | 774 (0.8) | 156 (1.1) | 51 (1.4) | 25 (1.0) | |
| Very poor | 1227 (1.3) | 241 (1.7) | 63 (1.7) | 56 (2.2) | |
| Overall score, mean (SD)b | 4.80 (0.63) | 4.68 (0.74) | 4.61 (0.78) | 4.70 (0.78) | <.001 |
| White | |||||
| Very good | 65 775 (87.9) | 7757 (78.3) | 1974 (73.8) | 1511 (81.9) | <.001 |
| Good | 6219 (8.3) | 1595 (16.1) | 499 (18.6) | 221 (12.0) | |
| Fair | 1396 (1.9) | 275 (2.8) | 121 (4.5) | 55 (3.0) | |
| Poor | 569 (0.8) | 116 (1.2) | 39 (1.5) | 16 (0.9) | |
| Very poor | 891 (1.2) | 159 (1.6) | 43 (1.6) | 42 (2.3) | |
| Overall score, mean (SD)b | 4.81 (0.62) | 4.68 (0.73) | 4.62 (0.78) | 4.70 (0.77) | <.001 |
| Black | |||||
| Very good | 3025 (84.9) | 1059 (82.4) | 116 (70.3) | 105 (77.8) | .04 |
| Good | 358 (10.1) | 149 (11.6) | 40 (24.2) | 22 (16.3) | |
| Fair | 75 (2.1) | 39 (3.0) | 7 (4.2) | 5 (3.7) | |
| Poor | 49 (1.4) | 11 (0.9) | 0 | 2 (1.5) | |
| Very poor | 55 (1.5) | 27 (2.1) | 2 (1.2) | 1 (0.7) | |
| Overall score, mean (SD)b | 4.75 (0.70) | 4.71 (0.75) | 4.62 (0.68) | 4.69 (0.69) | <.001 |
| Asian | |||||
| Very good | 14 197 (85.9) | 2173 (76.2) | 599 (72.3) | 369 (81.3) | <.001 |
| Good | 1548 (9.4) | 501 (17.6) | 158 (19.1) | 50 (11.0) | |
| Fair | 390 (2.4) | 104 (3.6) | 43 (5.2) | 17 (3.7) | |
| Poor | 138 (0.8) | 21 (0.7) | 11 (1.3) | 7 (1.5) | |
| Very poor | 255 (1.5) | 53 (1.9) | 17 (2.1) | 11 (2.4) | |
| Overall score, mean (SD)b | 4.77 (0.68) | 4.65 (0.75) | 4.58 (0.82) | 4.67 (0.82) | <.001 |
| Hispanic | |||||
| Very good | 1672 (86.8) | 303 (77.7) | 78 (76.5) | 71 (80.7) | <.001 |
| Good | 177 (9.2) | 62 (15.9) | 18 (17.6) | 12 (13.6) | |
| Fair | 34 (1.8) | 15 (3.8) | 4 (3.9) | 3 (3.4) | |
| Poor | 18 (0.9) | 8 (2.1) | 1 (1.0) | 0 | |
| Very poor | 26 (1.3) | 2 (0.5) | 1 (1.0) | 2 (2.3) | |
| Overall score, mean (SD)b | 4.79 (0.65) | 4.68 (0.69) | 4.68 (0.69) | 4.70 (0.75) | .009 |
P values were calculated using χ2 test for categorical Press Ganey scores and analysis of variance test for continuous Press Ganey scores.
Scores were calculated on a scale of 1 to 5.
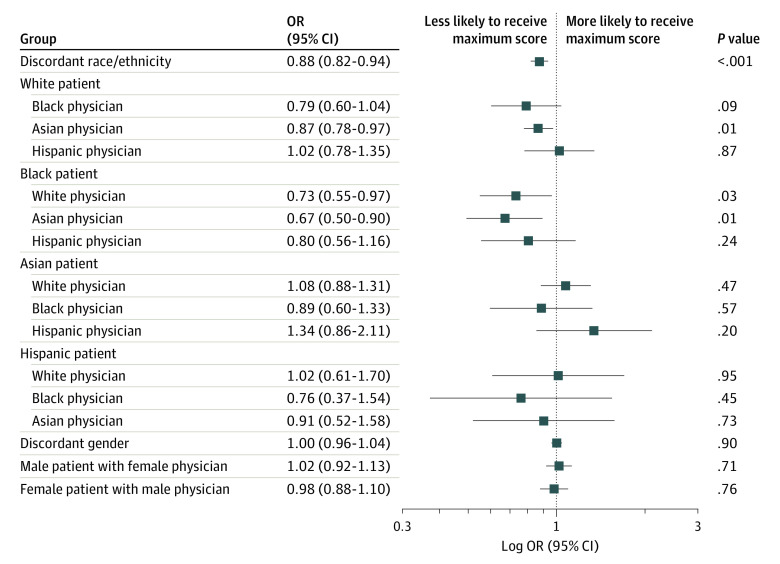
Adjusted ORs for the primary outcome by specific patient-physician racial/ethnic pairs are summarized in the Figure. Among White patients, Asian physicians had lower odds of receiving the maximum score compared with White physicians (adjusted OR, 0.87; 95% CI, 0.78-0.97; P = .01); Black physicians also had lower odds of receiving the maximum score vs White physicians but the difference was not significant (adjusted OR, 0.79; 95% CI, 0.60-1.04; P = .09). The absolute difference in mean score between White and Asian physicians was 0.03, and that between White and Black physicians was 0.05. The likelihood of receiving the maximum score was similar between Hispanic and White physicians (adjusted OR, 1.02; 95% CI, 0.78-1.35; P = .87). Among Black patients, White (adjusted OR, 0.73; 95% CI, 0.55-0.97; P = .03) and Asian (adjusted OR, 0.67; 95% CI, 0.50-0.90; P = .01) physicians were each less likely to receive the maximum score compared with Black physicians. The OR for Hispanic physicians was not statistically significant (adjusted OR, 0.80; 95% CI, 0.56-1.16; P = .24). The absolute difference in mean score between Black and White physicians was 0.03, and that between Black and Asian physicians was 0.06. The ORs among Asian and Hispanic patients were not significant for any of the patient-physician pairs.
Figure. Adjusted Odds Ratios (ORs) for Maximum Press Ganey Score by Patient-Physician Racial/Ethnic and Gender Discordant Pairs.
Patient-physician racial/ethnic and gender concordance regression models included the following variables: patient age, gender, race/ethnicity, education, income, marital status, insurance, primary language, overall health, and mental and emotional health; physician age, gender, race/ethnicity, academic track (gender concordance only), and academic rank; and clinical encounter type, location, and specialty. Scores refer to scores on the Press Ganey Outpatient Medical Practice survey. Patient-physician concordant pairs serve as the reference.
Secondary Outcomes
ORs for the secondary outcomes by discordant patient-physician racial/ethnic pairs are summarized in eTable 2 in the Supplement. The ORs are similar to those for the primary outcome.
Gender Concordance: Primary and Secondary Outcomes
Overall, physicians in 57 924 of 67 290 (86.1%) gender-concordant patient-physician encounters received the maximum score, compared with physicians in 42 860 of 50 299 (85.2%) gender-discordant patient-physician encounters. In adjusted analyses, physicians in gender discordant patient-physician pairs were equally as likely to receive the maximum score as those in concordant pairs (adjusted OR, 1.00; 95% CI, 0.96-1.04; P = .90). Adjusted ORs for the primary outcome by specific patient-physician gender pairs are summarized in the Figure and reveal no significant differences. Adjusted ORs for the secondary outcomes by patient-physician gender pairs are shown in eFigure 2 in the Supplement.
Other Patient, Physician, and Clinical Encounter Characteristics
Associations between other patient, physician, and clinical encounter characteristics and the primary outcome are summarized in eTable 3 and eTable 4 in the Supplement. Patient characteristics consistently associated with higher odds of giving the maximum score in both race/ethnicity and gender concordance models include older age, male gender, married or partnered or divorced or widowed marital status, Medicare or Medicaid insurance, and better self-reported overall and mental or emotional health. Patient characteristics consistently associated with lower odds of giving the maximum score include Black (race/ethnicity concordance model, adjusted OR, 0.73; 95% CI, 0.68-0.78; P < .001) and Asian race (race/ethnicity concordance model, adjusted OR, 0.55; 95% CI, 0.50-0.60; P < .001), higher education levels, and non-English primary language. Higher physician rank (professor) was consistently associated with higher odds of receiving the highest score; older physician age was associated with lower odds of receiving the highest score. Return and procedural visits were each associated with higher odds of receiving the top score. Clinical encounters in specialties outside of medicine were associated with lower odds of receiving the highest score.
Discussion
In this study of PG scores from patients seen in the ambulatory practices of an urban, academic medical center, we found that patient-physician racial/ethnic concordance was associated with patients’ reported experience with their physicians. Compared with physicians in racially/ethnically concordant patient-physician encounters, physicians in discordant dyads were less likely to receive the maximum patient rating. On an absolute level, there was a 5.5-point difference between the percentages of physicians receiving the highest score in discordant vs concordant dyads. Among specific patient-physician racial/ethnic dyads, relative and absolute measures showed that White patients who saw Asian (0.03 difference in mean score) or Black (0.05 difference in mean score) physicians were less likely to rate their physicians favorably than their counterparts who saw White physicians; the latter difference was underpowered to reach statistical significance in adjusted analyses. Black patients who saw White (0.03 difference in mean score) or Asian (0.06 difference in mean score) physicians were less likely to rate their physicians favorably compared with those who saw Black physicians. To put these differences into perspective, in another study of the PG survey,2 a decrease in mean score of 0.02 on the 1-to-5 scoring scale was associated with a substantial decrease in physician ranking from the 100th to 70th percentile.
Our findings add to the existing literature by presenting new information that supports the positive associations between the patient experience as measured by the PG survey and patient-physician racial concordance. Although 2 prior studies20,24 evaluated PG scores in broad medical settings, the associations between physician ratings and patient and physician characteristics were mixed. These studies were limited by the patient populations included (predominantly White and Asian patients24 and inpatients20) and the exclusion of characteristics that we found to be important determinants of physician ratings. We evaluated patient-physician racial/ethnic dyads beyond those of White and Asian racial groups and accounted for a more comprehensive group of patient, physician, and visit characteristics. As such, our study lends further support to the clinical benefits that others have found to be associated with racially/ethnically concordant patient-physician interactions.8,11,12,19 These benefits include better patient-physician communication,6,31,32 patient care,33 and outcomes34 and have been suggested to be attributable to decreased bias between patients and physicians.6,7 Together, this information should be viewed as a call to action to vigorously support the training of underrepresented minority medical students and residents while also ensuring the promotion and retention of underrepresented minority physicians. However, the provision of health care to minority patients should not fall solely to minority physicians. It is, therefore, imperative that we also improve cultural mindfulness among all physicians so that they are prepared to care for a diverse patient population in an equitable manner.
We also identified other PG score patterns that raise questions about how these scores should be used. PG scores for physicians who saw White patients were numerically higher than for physicians who saw non-White patients. In adjusted analyses, Black and Asian patient race were each associated with lower odds of the physician receiving the maximum score compared with White patient race. These findings are consistent with and expand upon prior studies24,35 that observed that Asian patients rate their physicians lower than do White patients. We also found that, among all patients except for Black patients, the absolute proportion of physicians who received the maximum score was lowest among Black physicians. Furthermore, among White patients, the odds of receiving the maximum score were similar between White and Hispanic physicians, the latter of whom may, in some cases, be less obviously identifiable by White patients as being ethnically discordant. Although these patterns may reflect truly different patient experiences, they also raise the possibility that there are racial/ethnic differences in patient expectations of or biases toward their physicians that may influence PG scores. This is especially relevant in our current environment of #WhatADoctorLooksLike,36 in which examples of the lay public questioning the medical authority of underrepresented minority physicians are too common. Thus, care should be taken in publicly reporting individual PG scores or using them for physician compensation and promotion decisions so as not to disincentivize physicians from caring for a diverse patient population or accelerate job dissatisfaction.1,37
With respect to gender, in contrast to some studies, we did not find an association between patient-physician gender concordance and PG scores. As suggested in prior work,10 it is possible that associations between patient-physician gender concordance and patient experience ratings are particular to specific medical specialties.
Strengths and Limitations
Study strengths include a large survey sample; robust patient-level, physician-level, and visit-level data; examination of all Care Provider domain PG survey questions; and inclusion of a racially/ethnically diverse patient population. Limitations include the low survey response rate and the potential for nonresponse bias, small numbers among some racial/ethnic groups (especially Black and Hispanic physicians), and lack of generalizability to patient and physician populations with different sociodemographic compositions. The survey response rate for our study is typical of the PG survey, as has been reported in other literature,2,10,20,24,38 and, although it is beyond the scope of the present study, the presence of nonresponse bias has been suggested in at least one study of the PG survey.38 Nonresponse bias may contribute to skewed responses in both the positive and negative directions. Future studies aimed at quantifying the effects of nonresponse bias are necessary for appropriate interpretation of PG scores.
Conclusions
This cross-sectional analysis provides new insights about the associations between the patient experience as measured by PG scores and patient-physician racial/ethnic concordance as well as patient race/ethnicity. Further investigation to understand the reasons for differential scoring across specific patient and physician characteristics is warranted. In the meantime, although we recognize the value of PG scores as a measure of the patient experience, we also encourage health care leaders, administrators, and insurers to reevaluate the appropriateness of using PG scores as a primary and reportable measure of physician performance on an individual level.
eAppendix. Patient Survey
eFigure 1. Study Selection Flow Diagram
eFigure 2. Adjusted Odds Ratios for Secondary Patient Experience Outcomes by Patient-Physician Gender Discordant Pairs
eTable 1. Patient Characteristics by Physician Race/Ethnicity
eTable 2. Adjusted Odds Ratios for Secondary Patient Experience Outcomes by Patient-Physician Racial/Ethnic Discordant Pairs
eTable 3. Primary Model for Patient-Physician Racial/Ethnic Binary Concordance
eTable 4. Primary Model for Patient-Physician Gender Binary Concordance
References
- 1.Zgierska A, Rabago D, Miller MM. Impact of patient satisfaction ratings on physicians and clinical care. Patient Prefer Adherence. 2014;8:437-446. doi: 10.2147/PPA.S59077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Presson AP, Zhang C, Abtahi AM, Kean J, Hung M, Tyser AR. Psychometric properties of the Press Ganey® Outpatient Medical Practice Survey. Health Qual Life Outcomes. 2017;15(1):32. doi: 10.1186/s12955-017-0610-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haviland MG, Morales LS, Reise SP, Hays RD. Do health care ratings differ by race or ethnicity? Jt Comm J Qual Saf. 2003;29(3):134-145. doi: 10.1016/S1549-3741(03)29016-X [DOI] [PubMed] [Google Scholar]
- 4.Bertakis KD, Franks P, Azari R. Effects of physician gender on patient satisfaction. J Am Med Womens Assoc (1972). 2003;58(2):69-75. [PubMed] [Google Scholar]
- 5.Milano A, Dalawari P, McGregor AJ, et al. Emergency department evaluation of patient satisfaction: does physician gender impact Press Ganey scores? a multicenter study. Am J Emerg Med. 2018;36(9):1708-1709. doi: 10.1016/j.ajem.2018.01.067 [DOI] [PubMed] [Google Scholar]
- 6.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907-915. doi: 10.7326/0003-4819-139-11-200312020-00009 [DOI] [PubMed] [Google Scholar]
- 7.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979-987. doi: 10.2105/AJPH.2011.300558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43(3):296-306. doi: 10.2307/3090205 [DOI] [PubMed] [Google Scholar]
- 9.Murray-García JL, Selby JV, Schmittdiel J, Grumbach K, Quesenberry CP Jr. Racial and ethnic differences in a patient survey: patients’ values, ratings, and reports regarding physician primary care performance in a large health maintenance organization. Med Care. 2000;38(3):300-310. doi: 10.1097/00005650-200003000-00007 [DOI] [PubMed] [Google Scholar]
- 10.Rogo-Gupta LJ, Haunschild C, Altamirano J, Maldonado YA, Fassiotto M. Physician gender is associated with Press Ganey patient satisfaction scores in outpatient gynecology. Womens Health Issues. 2018;28(3):281-285. doi: 10.1016/j.whi.2018.01.001 [DOI] [PubMed] [Google Scholar]
- 11.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583-589. doi: 10.1001/jama.282.6.583 [DOI] [PubMed] [Google Scholar]
- 12.Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159(9):997-1004. doi: 10.1001/archinte.159.9.997 [DOI] [PubMed] [Google Scholar]
- 13.Sandhu H, Adams A, Singleton L, Clark-Carter D, Kidd J. The impact of gender dyads on doctor-patient communication: a systematic review. Patient Educ Couns. 2009;76(3):348-355. doi: 10.1016/j.pec.2009.07.010 [DOI] [PubMed] [Google Scholar]
- 14.Meghani SH, Brooks JM, Gipson-Jones T, Waite R, Whitfield-Harris L, Deatrick JA. Patient-provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethn Health. 2009;14(1):107-130. doi: 10.1080/13557850802227031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar D, Schlundt DG, Wallston KA. Patient-physician race concordance and its relationship to perceived health outcomes. Ethn Dis. 2009;19(3):345-351. [PubMed] [Google Scholar]
- 16.Traylor AH, Subramanian U, Uratsu CS, Mangione CM, Selby JV, Schmittdiel JA. Patient race/ethnicity and patient-physician race/ethnicity concordance in the management of cardiovascular disease risk factors for patients with diabetes. Diabetes Care. 2010;33(3):520-525. doi: 10.2337/dc09-0760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flocke SA, Gilchrist V. Physician and patient gender concordance and the delivery of comprehensive clinical preventive services. Med Care. 2005;43(5):486-492. doi: 10.1097/01.mlr.0000160418.72625.1c [DOI] [PubMed] [Google Scholar]
- 18.Schmittdiel J, Grumbach K, Selby JV, Quesenberry CP Jr. Effect of physician and patient gender concordance on patient satisfaction and preventive care practices. J Gen Intern Med. 2000;15(11):761-769. doi: 10.1046/j.1525-1497.2000.91156.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blanchard J, Nayar S, Lurie N. Patient-provider and patient-staff racial concordance and perceptions of mistreatment in the health care setting. J Gen Intern Med. 2007;22(8):1184-1189. doi: 10.1007/s11606-007-0210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen JG, Zou B, Shuster J. Relationship between patient satisfaction and physician characteristics. J Patient Exp. 2017;4(4):177-184. doi: 10.1177/2374373517714453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jerant A, Bertakis KD, Fenton JJ, Tancredi DJ, Franks P. Patient-provider sex and race/ethnicity concordance: a national study of healthcare and outcomes. Med Care. 2011;49(11):1012-1020. doi: 10.1097/MLR.0b013e31823688ee [DOI] [PubMed] [Google Scholar]
- 22.LaVeist TA, Gaskin DJ, Richard P; Joint Center for Political and Economic Studies The economic burden of health inequalities in the United States. Published September 2009. Accessed June 1, 2019. https://hsrc.himmelfarb.gwu.edu/cgi/viewcontent.cgi?article=1224&context=sphhs_policy_facpubs
- 23.US Census Bureau 2012 National population projection tables: table 6—percent of the projected population by race and Hispanic origin for the United States: 2015 to 2060. Published 2012. Accessed October 15, 2020. https://www.census.gov/data/tables/2012/demo/popproj/2012-summary-tables.html
- 24.Garcia LC, Chung S, Liao L, et al. Comparison of outpatient satisfaction survey scores for Asian physicians and non-Hispanic white physicians. JAMA Netw Open. 2019;2(2):e190027. doi: 10.1001/jamanetworkopen.2019.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dyer N, Sorra JS, Smith SA, Cleary PD, Hays RD. Psychometric properties of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) Clinician and Group Adult Visit Survey. Med Care. 2012;50(suppl):S28-S34. doi: 10.1097/MLR.0b013e31826cbc0d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-1457. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 27.Siddiqui ZK, Zuccarelli R, Durkin N, Wu AW, Brotman DJ. Changes in patient satisfaction related to hospital renovation: experience with a new clinical building. J Hosp Med. 2015;10(3):165-171. doi: 10.1002/jhm.2297 [DOI] [PubMed] [Google Scholar]
- 28.Giordano LA, Elliott MN, Goldstein E, Lehrman WG, Spencer PA. Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010;67(1):27-37. doi: 10.1177/1077558709341065 [DOI] [PubMed] [Google Scholar]
- 29.Press Ganey Guide to interpreting: part 2—statistics. Published 2014. Accessed August 10, 2020. https://helpandtraining.pressganey.com/lib-docs/default-source/ip-training-resources/guide-to-interpreting---part-2.pdf?sfvrsn=2
- 30.Hosmer DW, Lemeshow S. Applied Logistic Regression, 2nd edition John Wiley and Sons; 2000. doi: 10.1002/0471722146 [DOI] [Google Scholar]
- 31.Shen MJ, Peterson EB, Costas-Muñiz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5(1):117-140. doi: 10.1007/s40615-017-0350-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288(6):756-764. doi: 10.1001/jama.288.6.756 [DOI] [PubMed] [Google Scholar]
- 33.Malhotra J, Rotter D, Tsui J, Llanos AAM, Balasubramanian BA, Demissie K. Impact of patient-provider race, ethnicity, and gender concordance on cancer screening: findings from Medical Expenditure Panel Survey. Cancer Epidemiol Biomarkers Prev. 2017;26(12):1804-1811. doi: 10.1158/1055-9965.EPI-17-0660 [DOI] [PubMed] [Google Scholar]
- 34.Greenwood BN, Carnahan S, Huang L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A. 2018;115(34):8569-8574. doi: 10.1073/pnas.1800097115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mayer LA, Elliott MN, Haas A, Hays RD, Weinick RM. Less use of extreme response options by Asians to standardized care scenarios may explain some racial/ethnic differences in CAHPS scores. Med Care. 2016;54(1):38-44. doi: 10.1097/MLR.0000000000000453 [DOI] [PubMed] [Google Scholar]
- 36.Cooke M. Implicit bias in academic medicine: #WhatADoctorLooksLike. JAMA Intern Med. 2017;177(5):657-658. doi: 10.1001/jamainternmed.2016.9643 [DOI] [PubMed] [Google Scholar]
- 37.Poole KG., Jr Patient-experience data and bias: what ratings don’t tell us. N Engl J Med. 2019;380(9):801-803. doi: 10.1056/NEJMp1813418 [DOI] [PubMed] [Google Scholar]
- 38.Tyser AR, Abtahi AM, McFadden M, Presson AP. Evidence of non-response bias in the Press-Ganey patient satisfaction survey. BMC Health Serv Res. 2016;16(a):350. doi: 10.1186/s12913-016-1595-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Patient Survey
eFigure 1. Study Selection Flow Diagram
eFigure 2. Adjusted Odds Ratios for Secondary Patient Experience Outcomes by Patient-Physician Gender Discordant Pairs
eTable 1. Patient Characteristics by Physician Race/Ethnicity
eTable 2. Adjusted Odds Ratios for Secondary Patient Experience Outcomes by Patient-Physician Racial/Ethnic Discordant Pairs
eTable 3. Primary Model for Patient-Physician Racial/Ethnic Binary Concordance
eTable 4. Primary Model for Patient-Physician Gender Binary Concordance