Key Points
Question
What is the association of crowding in nursing homes, defined as the mean number of residents per bedroom and bathroom, with nursing home coronavirus disease 2019 (COVID-19) mortality?
Findings
In this cohort study that included more than 78 000 residents of 618 nursing homes in Ontario, Canada, COVID-19 mortality in homes with low crowding was less than half (578 of 46 028 residents [1.3%]) than that of homes with high crowding (874 of 32 579 residents [2.7%]).
Meaning
Shared bedrooms and bathrooms in nursing homes are associated with larger and deadlier COVID-19 outbreaks.
Abstract
Importance
Nursing home residents have been disproportionately affected by coronavirus disease 2019 (COVID-19). Prevention recommendations emphasize frequent testing of health care personnel and residents, but additional strategies are needed.
Objective
To develop a reproducible index of nursing home crowding and determine whether crowding was associated with COVID-19 cases and mortality in the first months of the COVID-19 epidemic.
Design, Setting, and Participants
This population-based retrospective cohort study included more than 78 000 residents across more than 600 nursing homes in Ontario, Canada, and was conducted from March 29 to May 20, 2020.
Exposures
The nursing home crowding index equaled the mean number of residents per bedroom and bathroom.
Main Outcomes and Measures
The cumulative incidence of COVID-19 cases confirmed by a validated nucleic acid amplification assay and mortality per 100 residents; the introduction of COVID-19 into a home (≥1 resident case) was a negative tracer.
Results
Of 623 homes in Ontario, we obtained complete information on 618 homes (99%) housing 78 607 residents (women, 54 160 [68.9%]; age ≥85 years, 42 919 [54.6%]). A total of 5218 residents (6.6%) developed COVID-19 infection, and 1452 (1.8%) died of COVID-19 infection as of May 20, 2020. COVID-19 infection was distributed unevenly across nursing homes; 4496 infections (86%) occurred in 63 homes (10%). The crowding index ranged across homes from 1.3 (mainly single-occupancy rooms) to 4.0 (exclusively quadruple occupancy rooms); 308 homes (50%) had a high crowding index (≥2). Incidence in high crowding index homes was 9.7% vs 4.5% in low crowding index homes (P < .001), while COVID-19 mortality was 2.7% vs 1.3%, respectively (P < .001). The likelihood of COVID-19 introduction did not differ (high = 31.3% vs low = 30.2%; P = .79). After adjustment for regional, nursing home, and resident covariates, the crowding index remained associated with an increased incidence of infection (relative risk [RR] = 1.73, 95% CI, 1.10-2.72) and mortality (RR, 1.69; 95% CI, 0.99-2.87). A propensity score analysis yielded similar conclusions for infection (RR, 2.09; 95% CI, 1.30-3.38) and mortality (RR, 1.83; 95% CI, 1.09-3.08). Simulations suggested that converting all 4-bed rooms to 2-bed rooms would have averted 998 COVID-19 cases (19.1%) and 263 deaths (18.1%).
Conclusions and Relevance
In this cohort of Canadian nursing homes, crowding was common and crowded homes were more likely to experience larger and deadlier COVID-19 outbreaks.
This cohort study examines the association between nursing home crowding and COVID-19 cases and mortality in the first months of the COVID-19 epidemic in Ontario, Canada.
Introduction
Nursing home residents have experienced the brunt of the coronavirus disease 2019 (COVID-19) epidemic. Recent estimates suggest that nursing home residents comprise approximately 35% of COVID-19 deaths in the US and between 66% and 81% of deaths in Canada.1,2 Compared with community-dwelling older adults, nursing home residents are 5 times more likely to die of COVID-19.3 The concentration of COVID-19 mortality among nursing home residents can be explained by the high risk of contracting infection because of congregate living, exposure to staff, and difficulties with physically distancing because of cognitive and functional impairment. Residents who acquire infection are at high risk of mortality because of advanced age (immunosenescence) and multimorbidity.4,5,6
It is more difficult to understand why COVID-19 may severely affect certain nursing homes but spare others. Incidence in the region surrounding a nursing home and nursing home size drive the probability of introduction of COVID-19 by visitors or staff.3 Past studies of other respiratory infections suggest that, once introduced, crowded nursing homes may be more susceptible to infection spread, and associations observed with domestic crowding would also suggest plausibility for COVID-19.7,8,9
In a recent cohort study of COVID-19 in Ontario nursing homes, we found that for-profit nursing homes in Ontario had a higher incidence of COVID-19 cases and mortality compared with nonprofit and municipal homes, which was partially explained by the fact that for-profit homes tended to be built to older design standards, a factor associated with crowding because 4-bed rooms were eliminated from design standards as of 1999.10,11 In this study, we used the same cohort that included 618 nursing homes and 78 607 residents to explicitly examine the association between nursing home crowding and COVID-19 incidence across the entire nursing home system of Ontario, Canada, during the first months of the COVID-19 pandemic in Ontario. Residents of Ontario nursing homes receive personal and nursing care, as well as subsidized accommodation, under a publicly funded long-term care program. The province provides a base amount of $4200 per resident per month, supplemented by regulated resident copayments varying between $1900 for a bed in a quadruple-occupancy room to $2700 per month for a bed in a single-occupancy room.12 Residents unable to afford the copayment are subsidized based on means testing.
Methods
Ethics Statement
The study was approved by the research ethics board of the University of Toronto and the Hamilton Integrated (Ontario, Canada) research ethics board. The boards waived the need for informed consent because there was no contact with nursing home residents and anonymity was assured.
Study Design and Data Sources
We conducted a retrospective cohort study of all nursing homes in Canada’s most populous province of Ontario from March 29, 2020, the date of the first reported Ontario nursing home outbreak, until May 20, 2020 (52 days). Data used for this study were obtained from the Ontario Ministries of Health and Long-Term Care as part of the province’s Emergency Modeling Table and were derived from 4 sources. The first source was data collected by the Ontario Ministry of Long-Term Care’s Inspections Branch, which include patients with COVID-19 and deaths through their COVID Tracking Tool. These data, collected by inspectors, include case counts and deaths among those who died in the nursing home or while temporarily discharged. Tracking tool case counts were correlated with laboratory data on infections from the Ontario Laboratory Information System (Pearson correlation, 0.93; 95% CI, 0.93-0.93), and death counts were correlated with data from the Ontario Office of the Chief Coroner (Pearson correlation = 0.90; 95% CI, 0.90-0.91). The second source was public health surveillance data from the Ontario Integrated Public Health Information System, which were used to identify the incidence of COVID-19 in the 35 public health regions surrounding nursing homes. Third, data from the Canadian Census were used to obtain neighborhood and region characteristics. Fourth, resident characteristics were obtained from the Resident Assessment Instrument Minimum Data Set.13
Exposure: Nursing Home Crowding Index
The nursing home crowding index was defined as the mean number of occupants per room and bathroom across an entire home according to the following equation: Nresidents ÷ (½Nbedrooms + ½Nbathrooms). This translated to weights per resident according to the room they occupied: single-occupancy room with private bathroom (1); single-occupancy room with a shared bathroom (1.5); double-occupancy room (with shared bathroom) (2); and quadruple-occupancy room (4). In Ontario nursing homes, there are no rooms with a maximum occupancy of 3 or greater than 4. Based on the distribution of the crowding index, we defined homes with values of 2 or greater (the median) as high crowding index homes and homes less than 2 as low. When reporting risk ratios for models with the linear crowding index, we compared estimates for homes with an index of 1.5 (an equal mix of single-occupancy and double-occupancy rooms) with homes with an index of 3 (an equal mix of double-occupancy and quadruple-occupancy rooms).
Outcomes
Residents with confirmed COVID-19 were residents with a laboratory confirmation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection using a validated assay consisting of a positive nucleic acid amplification test result (eg, real-time polymerase chain reaction or nucleic acid sequencing) on at least 1 genome target.14 The primary outcomes were the cumulative incidence of confirmed COVID-19 cases per 100 nursing home residents and the COVID-19–associated deaths per 100 nursing home residents. To identify potential confounding, we also examined COVID-19 introduction (defined as ≥1 confirmed COVID-19 resident case in a nursing home) as a negative tracer outcome, because crowding should only affect COVID-19 transmission within nursing homes rather than risk of importation.15
Nursing Home Characteristics
In addition to the crowding index, we examined 5 home characteristics, including (1) the type of ownership of the facility (private for-profit, private nonprofit, or municipal); (2) the size of the facility (<100, ≥100 beds); (3) the ratio of full-time–equivalent staff to beds; (4) the proportion of 1-bed, 2-bed, and 4-bed rooms; and (5) the design standard (pre-1999 vs 1999 or later) that each home met.11 Before 1999, there was no universal design standard in the province, and as such, the design of homes was heterogeneous. Changes to the standard since 1999 have been incremental.16 In terms of design elements of particular relevance for infection control, the 1999 design standard specifies (1) that all homes have separate and independent subunits with a maximum size of 40 occupants (known as home areas), separate entrances, and independent common and dining areas, and (2) that resident rooms have no more than 2 beds.
Region and Resident Characteristics
We examined the incidence of COVID-19 in the surrounding public health region, excluding nursing home infections, per 10 000 population, and community size (<10 000, 10 000 to 499 999, and ≥500 000 individuals), and the proportion of the neighborhood population born outside of Canada using Statistics Canada data.13 Eleven resident characteristics, measured at the home level, were obtained from the most recent Resident Assessment Instrument Minimum Data17 from August 2019: female sex (percentage), 85 years or older (percentage); 6 comorbidities (dementia, congestive heart failure, chronic obstructive heart failure, cancer, diabetes, and kidney failure) and the mean count of these comorbidities, the mean of the activities of daily living (ADL) impairment scale score (0, no impairment to 28, complete impairment), and university education completed (percentage).
Statistical Analysis
All analyses were conducted using SAS, version 9.4 (SAS Institute), and all reported P values were based on 2-sided testing. P values less than .05 were considered statistically significant. A quasi-Poisson regression was used to model cases and deaths using the logarithm of the number of beds in the home as an offset, while logistic regression was used to model introduction of COVID-19 into the home. For all analyses, we included region-level random effects.18 Unadjusted models adjusted for no additional covariates, while adjusted models included the crowding index, other nursing home factors (size, ownership, and the ratio of full-time–equivalent staff to beds), resident factors (age, sex, comorbidity count, ADL scale score, and education), and all 3 region characteristics as covariates.
As a sensitivity analysis, we used propensity score matching to adjust for potential confounding between the crowding index and resident or regional factors.19 The propensity score was the estimated probability for a home to have a high crowding index based on a logistic regression model that included nursing home size, ownership, staffing ratio, 10 resident characteristics (age, sex, 6 comorbidities, ADL scale, and education), and all 3 region characteristics. Homes with a high crowding index were matched 1:1 with homes with a low crowding index within a caliper of 0.2 of the logit of the propensity score using a greedy matching algorithm.20 We then assessed the balance using standardized differences and considered greater than 10% a meaningful difference.20 Quasi-Poisson regression, with random effects corresponding to matched pairs, was then used to estimate associations with the crowding index.
We used simulations to estimate the incidence of COVID-19 infections and deaths in scenarios in which nursing homes were less crowded.21 Specifically, we simulated scenarios in which (1) all 4-bed rooms were replaced with 2-bed rooms and (2) all 2-bed and 4-bed rooms were replaced with 1-bed rooms. These scenarios were estimated by modifying the underlying crowding indexes of homes; for instance, if a home had 40% 1-bed rooms, 30% 2-bed rooms, and 30% 4-bed rooms (crowding index = 2.2), we estimated incidence as if the home had 40% 1-bed rooms and 60% 2-bed rooms (crowding index = 1.6), then as if the home was fully 1-bed rooms (crowding index = 1.0). We then used regression coefficients from the adjusted regression model to estimate incidence for all homes using these 2 simulated interventions. The preventable fraction was the simulated incidence divided by the incidence observed.
Results
Cohort
Of the 623 homes in Ontario, we were able to obtain complete information on 618 homes (99%); information on room types was missing for 5 homes. There were 78 607 residents in these homes at the time of the first case on March 29, 2020. Across the homes, 42 919 residents (54.6%) were 85 years or older, 54 160 (68.9%) were women, 54 868 (69.8%) had dementia, and the mean (SD) ADL score was 17.5 (Table 1).
Table 1. Characteristics of Low and High Crowding Index Nursing Homes.
| Characteristic | All homes | Crowding index | P value | |
|---|---|---|---|---|
| Low, 1.3-1.9 | High, 2.0-4.0 | |||
| Homes, No. (%) | 618 (100) | 310 (50.1) | 308 (49.9) | NA |
| Resident characteristics, median % (IQR) | ||||
| Female | 69.2 (64.6-73.7) | 70.5 (67.3-73.9) | 67.3 (61.9-73.4) | <.001 |
| Age ≥85 y | 55.3 (48.7-61.0) | 58.3 (54.3-63.1) | 50.4 (43.9-58.1) | <.001 |
| Comorbidities, median % (IQR) | ||||
| Dementia | 70.0 (63.0-76.7) | 72.0 (66.3-78.0) | 67.1 (58.8-75.2) | <.001 |
| Congestive heart failure | 11.9 (8.9-14.9) | 11.6 (8.8-14.7) | 12.1 (9.0-15.0) | .38 |
| Chronic obstructive pulmonary disorder | 15.6 (11.8-19.8) | 13.8 (10.5-17.3) | 17.2 (13.7-21.5) | <.001 |
| Cancer | 11.4 (8.2-15.3) | 11.5 (8.6-15.4) | 11.1 (7.8-15.0) | .24 |
| Diabetes | 26.9 (23.0-31.4) | 25.9 (22.2-28.8) | 29.1 (24.0-34.0) | <.001 |
| Kidney failure | 10.8 (7.7-14.7) | 10.5 (7.7-14.8) | 11.2 (7.7-14.7) | .74 |
| Count of comorbidities, No. (IQR) | 1.47 (1.37-1.61) | 1.46 (1.37-1.58) | 1.50 (1.37-1.62) | .20 |
| ADL long score, No. (IQR) | 17.7 (16.0-19.0) | 18.0 (16.4-19.1) | 17.6 (15.8-18.8) | .03 |
| University education | 18.4 (11.0-27.2) | 20.0 (12.3-29.4) | 16.3 (9.2-24.8) | <.001 |
| Region characteristics | ||||
| Regional COVID-19 incidence (per 10 000 residents), No. (%) | ||||
| First quartile (0.11-0.46) | 148 (24.0) | 58 (18.7) | 90 (29.2) | .02 |
| Second quartile (0.51-0.93) | 141 (22.8) | 74 (23.4) | 67 (21.8) | |
| Third quartile (0.94-1.29) | 159 (25.7) | 88 (28.4) | 71 (23.1) | |
| Fourth quartile (1.30-1.88) | 170 (27.5) | 90 (29.0) | 80 (26.0) | |
| Community population size, No. (%) | ||||
| ≥500 000 | 253 (40.9) | 146 (47.1) | 107 (34.7) | <.001 |
| 10 000-499 999 | 224 (36.3) | 116 (37.4) | 108 (35.1) | |
| <10 000 | 141 (22.8) | 48 (15.5) | 93 (30.2) | |
| Neighborhood foreign-born residents, median % (IQR) | 15.0 (7.0-29.0) | 19.5 (10.0-36.0) | 12.0 (6.5-24.0) | <.001 |
| Nursing home characteristics | ||||
| Ownership, No. (%) | ||||
| Private for-profit | 358 (57.9) | 127 (41.0) | 231 (75.0) | <.001 |
| Private nonprofit | 159 (25.7) | 101 (32.6) | 58 (18.8) | |
| Municipal | 101 (16.3) | 82 (26.5) | 19 (6.2) | |
| Size of home, No. (%) | ||||
| <100 | 244 (39.5) | 69 (22.3) | 175 (56.8) | <.001 |
| ≥100 | 374 (60.5) | 241 (77.7) | 133 (43.2) | |
| Staff (full-time equivalent):bed ratio, median (IQR) | 0.70 (0.66-0.75) | 0.72 (0.68-0.77) | 0.69 (0.65-0.72) | <.001 |
| Design standard, No. (%) | ||||
| 1999 | 310 (50.2) | 310 (100) | 0 (0) | <.001 |
| Pre-1999 | 308 (49.8) | 0 (0) | 308 (100) | |
| Room occupancy, median % (IQR) | ||||
| Single | 45.0 (13.0-60.0) | 59.9 (59.0-60.0) | 13.1 (6.5-22.2) | <.001 |
| Double | 40.0 (33.1-41.2) | 40.1 (40,0-41.0) | 33.3 (21.7-41.8) | <.001 |
| Quadruple | 0 (0-50.0) | 0 (0-0) | 50.2 (40.3-57.1) | <.001 |
| Crowding index, median (IQR) | 2.0 (1.4-2.9) | 1.4 (1.4-1.5) | 2.9 (2.7-3.1) | <.001 |
| Outcomes | ||||
| Residents, No. | 78 607 | 46 028 | 32 579 | |
| Infections, No. (% of residents) | 5218 (6.64) | 2071 (4.50) | 3147 (9.66) | <.001 |
| Mortality, No. (% of residents) | 1452 (1.85) | 578 (1.26) | 874 (2.68) | <.001 |
| ≥1 Infection, No. (%) | 190 (30.7) | 97 (31.3) | 83 (30.2) | .79 |
Abbreviations: ADL, activities of daily living; COVID-19, coronavirus disease 2019; IQR, interquartile range; NA, not applicable.
Nursing Homes Characteristics
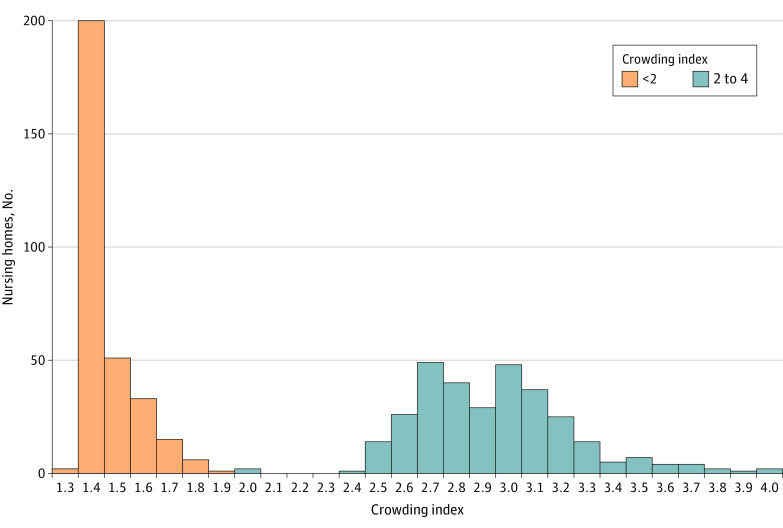
Across the province, 29 006 (36.9%), 29 320 (37.3%), and 20 281 (25.8%) residents were located in single, double, and quadruple-bedded rooms, respectively. Half (49.8%) of nursing homes were built according to a pre-1999 design standard that allowed quadruple-occupancy rooms. The nursing home crowding index varied from 1.3 to 4.0 (Figure 1). Homes meeting the 1999 design standard had a mix of single-occupancy and double-occupancy rooms and a crowding index between 1.3 and 1.9, while homes with older design standards had a mix of single, double and quadruple-occupancy rooms and crowding indices that ranged between 2.0 and 4.0. A sensitivity analysis demonstrated that the crowding index was correlated with the proportion of beds in single occupancy rooms (Pearson correlation = −0.91).
Figure 1. Crowding Index of Nursing Homes in Ontario, Canada.
Distribution of the nursing home crowding index across 618 homes in Ontario, Canada. The nursing home crowding index was measured as the mean number of occupants per room and bathroom across an entire nursing home according to the following equation: Nresidents ÷ (½Nbedrooms + ½Nbathrooms).
Outcomes
Of 78 607 residents, 5218 (6.6%) developed COVID-19 infection, and 1452 (1.8%) died of COVID-19 infection as of May 20, 2020. The case fatality rate was 27.8% (1452/5218). COVID-19 infection was distributed unequally across nursing homes in the province, with 4496 infections (86%) occurring in 63 homes (10%).
Association Between Crowding Index and COVID-19 Incidence and Mortality
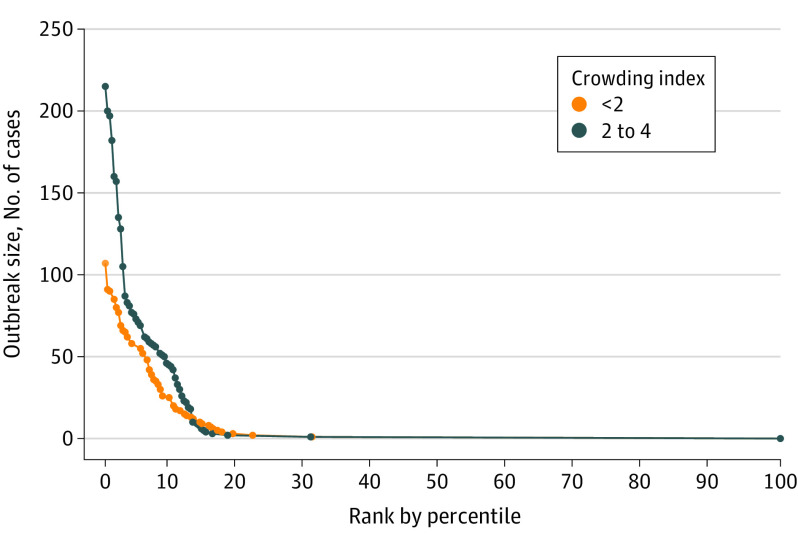
COVID-19 incidence in high crowding index homes was 9.7% compared with 4.5% in low crowding index homes (P < .001). Similarly, mortality was 2.7% in high crowding index homes vs 1.3% in low crowding index homes (P < .001). The probability of COVID-19 introduction into a home did not differ according to the crowding index (31.3% vs 30.2%; P = .79). Outbreaks in crowded nursing homes tended to be larger; there were 9 outbreaks involving more than 100 residents in high crowding index homes compared with 1 in low crowding index homes (Figure 2).
Figure 2. Ranked COVID-19 Outbreak Size in Nursing Homes in Ontario, Canada.
All 618 homes have been plotted according to the outbreak size and percentile rank of outbreak size (0 to 100) for homes with low (orange) and high (green) crowding index. Cases and deaths were identified between March 29 and May 20, 2020.
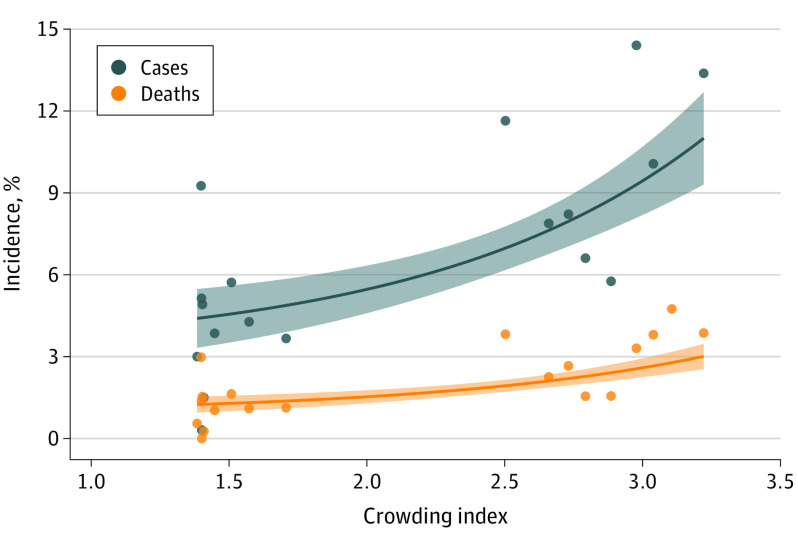
Regression models based on the linear crowding index (Table 2 and Figure 3) suggested that, compared with a home with an index of 1.5, homes with an index of 3 had double the COVID-19 incidence (relative risk [RR], 2.05; 95% CI, 1.49-2.70). After adjustment, the crowding index remained associated with increased risk (RR, 1.73; 95% CI, 1.10-2.72). The crowding index was similarly associated with COVID-19 mortality (unadjusted RR, 1.97; 95% CI, 1.36-2.84; adjusted RR, 1.69; 95% CI, 0.99-2.78). The crowding index was not associated with the probability of COVID-19 introduction (unadjusted odds ratio [OR], 1.10; 95% CI, 0.76-1.58; adjusted OR, 1.38; 95% CI, 0.88-2.18), but other factors, including regional incidence and nursing home size, were.
Table 2. Nursing Home Characteristics and Incidence of COVID-19 Infections and Mortality per 100 Residents.
| Characteristic | RR (95% CI) | OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| COVID-19 incidence | COVID-19 mortality | COVID-19 introduction (≥1 infection) | ||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Region factors, median (IQR) | ||||||
| Region COVID-19 incidence (per 10 000 residents) | ||||||
| First quartile (0.11-0.46) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Second quartile (0.51-0.93) | 1.79 (0.37-8.77) | 1.29 (0.28-6.00) | 2.57 (0.34-19.62) | 1.82 (0.28-11.92) | 1.35 (0.61-2.99) | 1.02 (0.52-2.01) |
| Third quartile (0.94-1.29) | 6.74 (1.70-26.78) | 2.87 (0.68-12.15) | 8.68 (1.40-53.65) | 3.16 (0.50-19.97) | 1.89 (0.87-4.09) | 0.85 (0.41-1.78) |
| Fourth quartile (1.30-1.88) | 10.00 (2.53-39.59) | 5.00 (1.19-21.11) | 13.94 (2.30-84.42) | 5.91 (0.96-36.47) | 2.69 (1.21-5.96) | 1.75 (0.85-3.61) |
| Community population size, median (IQR) | ||||||
| <10 000 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 10 000-499 999 | 1.95 (0.43-8.80) | 1.50 (0.35-7.39) | 2.15 (0.34-13.54) | 2.02 (0.33-12.21) | 2.50 (1.29-4.85) | 1.99 (0.96-1.11) |
| ≥500 000 | 8.64 (1.99-37.49) | 4.54 (0.94-22.00) | 9.94 (1.67-59.16) | 6.32 (0.97-41.31) | 6.11 (3.00-12.43) | 4.71 (1.97-11.25) |
| Neighborhood residents born outside Canada, median % (IQR) | 0.99 (0.98-1.01) | 0.99 (0.98-1.00) | 1.00 (0.98-1.01) | 0.99 (0.97-1.01) | 1.03 (1.02-1.04) | 1.01 (1.00-1.03) |
| Nursing home factors | ||||||
| Ownership, median (IQR) | ||||||
| Municipal | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Private, nonprofit | 2.00 (0.98-4.09) | 2.09 (0.89-4.94) | 2.48 (1.06-5.78) | 2.43 (0.88-6.68) | 1.22 (0.66-2.27) | 1.49 (0.77-2.91) |
| Private, for-profit | 3.30 (1.72-6.32) | 2.49 (1.14-5.45) | 3.67 (1.68-8.03) | 2.67 (1.04-6.84) | 1.23 (0.71-2.12) | 1.07 (0.59-1.96) |
| Size of home (beds), median (IQR) | ||||||
| <100 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| ≥100 | 0.83 (0.49-1.40) | 0.91 (0.51-1.64) | 0.70 (0.40-1.22) | 0.75 (0.39-1.43) | 1.77 (1.17-2.69) | 1.50 (0.93-2.41) |
| Crowding index | ||||||
| 1.5 (lowest) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2 | 1.27 (1.14-1.41) | 1.20 (1.03-1.39) | 1.25 (1.11-1.42) | 1.19 (1.00-1.42) | 1.03 (0.91-1.16) | 1.11 (0.96-1.30) |
| 2.5 | 1.61 (1.30-1.99) | 1.44 (1.07-1.95) | 1.57 (1.23-2.01) | 1.42 (1.00-2.02) | 1.06 (0.84-1.36) | 1.24 (0.92-1.68) |
| 3 | 2.05 (1.49-2.82) | 1.73 (1.10-2.72) | 1.97 (1.36-2.84) | 1.69 (0.99-2.87) | 1.10 (0.76-1.58) | 1.38 (0.88-2.18) |
| 3.5 (highest) | 2.60 (1.70-3.98) | 2.08 (1.13-3.80) | 2.47 (1.51-4.02) | 2.01 (0.99-4.08) | 1.13 (0.70-1.84) | 1.54 (0.84-2.82) |
Abbreviations: COVID-19, coronavirus disease 2019; IQR, interquartile range; OR, odds ratio; RR, relative risk.
Figure 3. Association Between Nursing Home Crowding Index and the Incidence of COVID-19 Cases and Deaths in Ontario, Canada.
Points represent the mean crowding index and the incidence of COVID-19 cases (gray; cases per 100 residents) and deaths (orange; deaths per 100 residents) for 20 equally sized groups of homes based on the crowding index. Specifically, each group of homes included 5% of homes in each group (30-31). Groups were based on homes and represented a vigintile of the crowding index. Solid lines represent quasi-Poisson regression estimates and shaded regions represent 95% CIs.
In the propensity analysis, a matched home with high crowding index was found for 149 (48%) of the low crowding index homes (standardized differences ≤10% for all variables; eTable in the Supplement). The resultant association estimates for incidence (RR, 2.09; 95% CI, 1.30-3.38), mortality (RR, 1.83; 95% CI, 1.09-3.08), and the odds of an outbreak (OR, 1.25; 95% CI, 0.74-2.11) were similar to those from regression analyses.
Preventable Fraction of COVID-19 Incidence and Mortality by Reducing Crowding
Simulation analyses suggested that 998 infections (19.1%) and 263 deaths (18.1%) in Ontario nursing homes may have been prevented if 4-bed rooms had been converted to 2-bed rooms. In this simulation scenario, an additional 5070 new 2-bed rooms would have been needed to maintain capacity across the province. In the simulation in which all multiple-occupancy rooms were converted to single-occupancy rooms, we estimated that 1641 infections (31.4%) and 437 deaths (30.1%) may have been prevented. In this scenario, an additional 29 871 new single-occupancy rooms would have been required, assuming current 4-bed and 2-bed rooms had been capped at single occupancy.
Discussion
In this study of nursing home crowding across 618 nursing homes in Ontario, Canada, we found that residents of highly crowded homes were more than twice as likely to develop infection with and die of COVID-19. Our findings extend those of a recent study based on the same cohort in which we showed that for-profit nursing homes experienced larger COVID-19 outbreaks involving more resident deaths, and that this may have been partially mediated by the older design standards of these homes.10
In Ontario, more than 60% of nursing home residents are housed in shared rooms, which contrasts with preferences among older adults, who favor single-bed rooms by a margin of 20 to 1 because they confer increased privacy and a sense of control.22,23 Benefits of multiple-occupancy rooms are sometimes touted by administrators and health care professionals because of lower construction costs and enhanced staffing efficiency.22,24 We also observed that crowded homes were more likely to be operated by private for-profit owners and had lower staffing ratios; these findings are associated with those of our previous study that showed that for-profit owners were more likely to operate homes with older design standards.10
Our findings align with a prior systematic review demonstrating that the risk of a respiratory infection in occupants of 2-bed rooms was double that of those in single-occupancy rooms.25 Physical barriers, such as walls separating bedrooms, predict deposition patterns of viral droplets more than absolute distances between beds in a shared room.26 Because of this, the crowding index, which is based on residents per bedroom and bathroom, is likely a better predictor than measures based on square footage per occupant.27 Crowding can affect an entire home because higher risk among occupants of shared rooms may spillover to private room occupants as residents come into contact with each other directly, in common areas, or indirectly via health care workers.28,29
Current guidance for COVID-19 prevention in nursing homes includes the following pillars: frequent testing of health care personnel and residents, face mask use for health care personnel and visitors, visitor restrictions, supply of hand hygiene and personal protective equipment, cohorting of known infections and new admissions, and adequate ratios of full-time, fairly paid staff who work at a single home.30,31,32 While this study did not evaluate the effectiveness of specific interventions, our results suggest that reinforcement of the previously described measures is needed in crowded homes. Further, our results suggest that cohorting may be ineffective in crowded homes with many shared rooms, as has been noted by nursing home administrators in Ontario.33
Insights from this study, and the experience of Ontario, suggest that interventions targeting crowding may reduce COVID-19 risk in nursing homes. Such interventions have been used in shelter systems, specifically by reducing capacity and adding new shelter beds in separate locations.34 In Ontario nursing homes, on the basis of early communication of these findings, the maximum room occupancy for incoming residents has been capped at 2 as of June 10, 2020.35 Additional measures, such as retrofitting of underoccupied hotels to act as temporary nursing homes and rapid structural adaptations to homes that are overly crowded, could be considered.36,37
Limitations
This study had several limitations. First, the nursing home crowding index and the 1999 design standard were strongly associated, and as such, other design features introduced by the new standard may have played a role in lowering COVID-19 incidence.11 These include larger square footage per room, improved ventilation systems, and resident home areas (smaller, self-contained units [<40 beds] within the home that facilitate cohorting). Second, our examination of crowding was at the nursing home level and we did not know which specific residents occupied single, double, or quadruple-occupancy rooms. Third, while we adjusted for aggregate characteristics of nursing home residents, we only had up-to-date information on nursing home resident characteristics until August 2019, the time of the most recent resident assessment. Fourth, we did not have access to information on nursing home resident race, immigration status, or ethnicity, although we were able to adjust for nursing home resident education levels. Fifth, adjustment of regional incidence when some community cases may have been secondary to nursing home cases may have caused overadjustment.
Conclusions
In this cohort study of Canadian nursing homes, we found that crowding is common, and crowded homes were more likely to experience larger and deadlier COVID-19 outbreaks.
eTable. Characteristics of nursing homes matched based on the propensity score (N=298)
References
- 1.Yourish K, Lai KKR, Ivory D, Smith M One-third of all U.S. coronavirus deaths are nursing home residents or workers. Accessed June 6, 2020. https://www.nytimes.com/
- 2.Hsu AT, Lane N, Sinha SK, et al. Impact of COVID-19 on Residents of Canada’s Long-Term Care Homes—Ongoing Challenges and Policy Responses. International Long-Term Care Policy Network; 2020. [Google Scholar]
- 3.Fisman DN, Bogoch I, Lapointe-Shaw L, McCready J, Tuite AR. Risk factors associated with mortality among residents with coronavirus disease 2019 (COVID-19) in long-term care facilities in Ontario, Canada. JAMA Netw Open. 2020;3(7):e2015957. doi: 10.1001/jamanetworkopen.2020.15957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669-677. doi: 10.1016/S1473-3099(20)30243-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan WJ, Liang WH, Zhao Y, et al. ; China Medical Treatment Expert Group for COVID-19 . Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi: 10.1183/13993003.00547-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382-386. doi: 10.15585/mmwr.mm6913e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drinka PJ, Krause P, Schilling M, Miller BA, Shult P, Gravenstein S. Report of an outbreak: nursing home architecture and influenza-A attack rates. J Am Geriatr Soc. 1996;44(8):910-913. doi: 10.1111/j.1532-5415.1996.tb01859.x [DOI] [PubMed] [Google Scholar]
- 8.Ryan A, Lazar K A new analysis: coronavirus death rate surged in Massachusetts locations that already faced challenges. Accessed June 9, 2020. https://www.bostonglobe.com/
- 9.Emeruwa UN, Ona S, Shaman JL, et al. Associations between built environment, neighborhood socioeconomic status, and SARS-CoV-2 infection among pregnant women in New York City. JAMA. 2020;324(4):390-392. doi: 10.1001/jama.2020.11370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stall NM, Jones A, Brown KA, Rochon PA, Costa AP. For-profit long-term care homes and the risk of COVID-19 outbreaks and resident deaths. CMAJ. 2020;192(33):E946-E955. doi: 10.1503/cmaj.201197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Long-Term Care Facility Design Manual Ministry of Health and long-term care. Accessed June 12, 2020. https://collections.ola.org/mon/ont/H/1999/LTCdesign_manual.pdf
- 12.Advantage Ontario About long term care homes. Accessed August 3, 2020. https://www.advantageontario.ca/
- 13.Statistics Canada Population projections for Canada (2018 to 2068), provinces and territories (2018 to 2043). Accessed June 18, 2020. https://www150.statcan.gc.ca/n1/pub/91-520-x/91-520-x2019001-eng.htm
- 14.Ministry of Health Case definition—COVID-19. Accessed September 17, 2020. https://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/2019_guidance.aspx
- 15.Lipsitch M, Tchetgen Tchetgen E, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology. 2010;21(3):383-388. doi: 10.1097/EDE.0b013e3181d61eeb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ministry of Health and Long-Term Care Long-term care home design manual 2015. Accessed June 12, 2020. http://health.gov.on.ca/en/public/programs/ltc/docs/home_design_manual.pdf
- 17.Mor V A comprehensive clinical assessment tool to inform policy and practice: applications of the minimum data set. Med Care. 2004;42(4)(suppl):III50-III59. doi: 10.1097/01.mlr.0000120104.01232.5e [DOI] [PubMed] [Google Scholar]
- 18.Austin PC, Merlo J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med. 2017;36(20):3257-3277. doi: 10.1002/sim.7336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haukoos JS, Lewis RJ. The propensity score. JAMA. 2015;314(15):1637-1638. doi: 10.1001/jama.2015.13480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Austin PC An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399-424. doi: 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poole C A history of the population attributable fraction and related measures. Ann Epidemiol. 2015;25(3):147-154. doi: 10.1016/j.annepidem.2014.11.015 [DOI] [PubMed] [Google Scholar]
- 22.Calkins M, Cassella C. Exploring the cost and value of private versus shared bedrooms in nursing homes. Gerontologist. 2007;47(2):169-183. doi: 10.1093/geront/47.2.169 [DOI] [PubMed] [Google Scholar]
- 23.Kane RA, Baker MO, Salmon J, Veazie W Consumer perspectives on private versus shared accommodations in assisted living settings. Accessed June 21, 2020. https://assets.aarp.org/rgcenter/consume/9807_living.pdf
- 24.Nichols J. Private rooms not always a better place for residents. Caring for the Ages. 2014;15(2):3. doi: 10.1016/j.carage.2014.01.004 [DOI] [Google Scholar]
- 25.Stiller A, Salm F, Bischoff P, Gastmeier P. Relationship between hospital ward design and healthcare-associated infection rates: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2016;5(1):51. doi: 10.1186/s13756-016-0152-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.King M-F, Noakes CJ, Sleigh PA, Camargo-Valero MA. Bioaerosol deposition in single and two-bed hospital rooms: a numerical and experimental study. Building and Environment. 2013;59:436-447. doi: 10.1016/j.buildenv.2012.09.011 [DOI] [Google Scholar]
- 27.MacIntyre CR, Kendig N, Kummer L, Birago S, Graham NMH. Impact of tuberculosis control measures and crowding on the incidence of tuberculous infection in Maryland prisons. Clin Infect Dis. 1997;24(6):1060-1067. doi: 10.1086/513632 [DOI] [PubMed] [Google Scholar]
- 28.Langford BJ, Daneman N, Leung V, et al. The second-hand effects of antibiotics: communicating the public health risks of drug resistance. JAC-Antimicrobial Resistance. 2019;1(3):dlz059. doi: 10.1093/jacamr/dlz059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown KA, Jones M, Daneman N, et al. Importation, antibiotics, and Clostridium difficile infection in veteran long-term care: a multilevel case-control study. Ann Intern Med. 2016;164(12):787-794. doi: 10.7326/M15-1754 [DOI] [PubMed] [Google Scholar]
- 30.US Centers for Disease Control and Prevention Preparing for COVID-19 in nursing homes. Accessed June 13, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
- 31.Gaur S, Dumyati G, Nace DA, Jump RLP. Unprecedented solutions for extraordinary times: helping long-term care settings deal with the COVID-19 pandemic. Infect Control Hosp Epidemiol. 2020;41(6):729-730. doi: 10.1017/ice.2020.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization Preventing and Managing COVID-19 across Long-Term Care Services: Policy Brief. World Health Organization; 2020. [Google Scholar]
- 33.Grant K, Ha TT How shoring up hospitals for COVID-19 contributed to Canada’s long-term care crisis. Accessed June 6, 2020. https://www.theglobeandmail.com/
- 34.Culhane D, Treglia D, Steif K, Kuhn R, Byrne T Estimated emergency bed need for the US homeless population related to COVID-19 exposure. Accessed June 8, 2020. https://endhomelessness.org/
- 35.Ministry of Health and Long-Term Care COVID-19 directive #3 for long-term care homes under the Long-Term Care Homes Act. Accessed June 6, 2020. http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/directives/LTCH_HPPA.pdf
- 36.Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305-1314. doi: 10.1016/S0140-6736(20)30744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kenette W. When a gym becomes a home: Highlighting the need for long-term care reform. healthydebate.ca. Accessed July 27, 2020. https://healthydebate.ca/opinions/highlighting-need-for-ltc-reform
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Characteristics of nursing homes matched based on the propensity score (N=298)