Abstract
Stroke is a leading cause of death in Africa and a key modifiable risk factor for the index and recurrent stroke is through the adequate management of blood pressure. Recent guidelines encourage management beyond clinic settings, yet implementation of these guidelines can be challenging, especially in resource constrained regions, such as in Sub-Saharan Africa. Mobile health technology may offer an innovative and cost-effective approach to improve BP monitoring and facilitate adherence to antihypertensive medications. Stroke survivors (n = 16) and their caregivers (n = 8) who participated in a 3-month feasibility study were invited to share post-intervention insights via focus groups (n = 3). Clinician (n = 7) input on intervention delivery and clinical impressions was also obtained via a separate focus group (n = 1). Four major themes emerged highlighting the ability to self-monitor, the use of technology as an interventional tool, training and support, and post-intervention adherence. Overwhelming receptivity toward home blood pressure monitoring and the use of mobile health (mHealth) was noted. Feedback indicated benefits in having access to equipment and that message prompts facilitated adherence. Post-intervention adherence declined following study intervention, indicating a need for increased exposure to facilitate long-term behavioral change, although participants conveyed a heightened awareness of the importance of BP monitoring and lifestyle changes needed.
Keywords: Hypertension, Stroke, Mobile health, Self-monitoring, Sub-Saharan Africa, Medication adherence
1. INTRODUCTION
Stroke is currently the fourth leading cause of death in Africa1 where rates have continued to increase, compared with high-income countries where the trend in stroke incidence has declined.1,2 The World Health Organisation (WHO) estimates that death from stroke and disability adjusted life years lost to stroke are at least 7 times higher in low-and-middle-income countries (LMICs).2 The premier modifiable risk factor for index and recurrent stroke is hypertension, making up for 30–50% risk of stroke.3–5 A successful reduction of systolic blood pressure (SBP) results in significant reductions in the risk of recurrent strokes in developed countries. Recent hypertension guidelines recommend multifaceted approaches to monitor and contain hypertension in high-risk patients, including incorporating a systematic approach to monitor blood pressure (BP) outside of clinical settings.6 However, in sub-Saharan Africa (SSA), achieving and sustaining BP control is particularly challenging due to a number of factors including low literacy levels, misconceptions about hypertension, nonadherence, medication access and affordability, inappropriate medication selection, clinical inertia, and resistant hypertension.7 Thus, culturally-sensitive, efficacious BP control programs which are acceptable, feasible, timely, and sustainable are needed among stroke survivors in SSA.
Innovative approaches, such as mobile phone technology (mHealth) for electronic decision support in delivering evidence-based and integrated care for hypertension, may offer a promising approach towards enhancing BP control after stroke.8–9 In SSA approximately 73% of adults have a cell phone and about 35% own smartphones10, which has produced promising results in chronic disease management (such as HIV) locally.11 Moreover, receptivity toward the use of mHealth as an interventional tool among this population has been previously documented.12 In an attempt to fill this gap, we evaluated the feasibility and preliminary signals of clinical outcomes of a mHealth medication and BP self-management system for 60 recent stroke patients with uncontrolled hypertension at a tertiary hospital in SSA in the Phone-based Intervention under Nurse Guidance after Stroke (PINGS) study.13 Details of the intervention outcomes are reported elsewhere.14–15
Our objective was to explore post-intervention perspectives and gather in-depth insight into the experiences of stroke survivors and their caregivers following participation in a larger interventional arm of a mHealth blood pressure management study. We also sought to assess the contextual and organizational facilitators and barriers encountered in the implementation of the intervention within an operational setting.
2. METHODS
Methods and results are reported following the Consolidated Criteria for Reporting Qualitative Research.16 This study received ethical board approval from the Institutional Review Board at the Medical University of South Carolina (MUSC) and from the Committee on Human Research Publication and Ethics (CHRPE) of the School of Medical Sciences, Kwame Nkrumah University. Participants for the PINGS interventional trial were recruited from the Neurology clinic17 at the Komfo Anokye Teaching Hospital, a tertiary referral facility, located in Kumasi, Ghana.
Description of the PINGS Intervention:
The Phone-based Intervention under Nurse Guidance after Stroke is a mHealth technology-centered, multi-level, nurse-guided intervention aimed at improving blood pressure control after stroke in Ghana. This Smartphone application (app) enabled medical regimen management system is an iteration of a system developed and repeatedly refined and adopted for various patient populations.18–21 The iOS and android platform systems evolved using a patient and provider centered iterative design process involving socio-culturally preferred and low literacy based strategies, guided by principles of the Self-Determination Theory22 and Technology Acceptance Model23. Members of the MUSC Technology Applications Center for Healthful Lifestyles (TACHL) team (software developers, database administrators, and behavioral health scientists), along with software and web portal development expertise provided by Patient Guided Health Solutions, LLC, were involved at various stages of the app development and refinement.
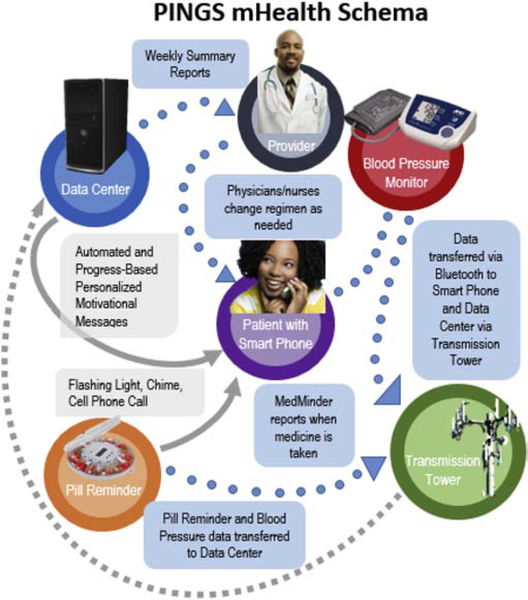
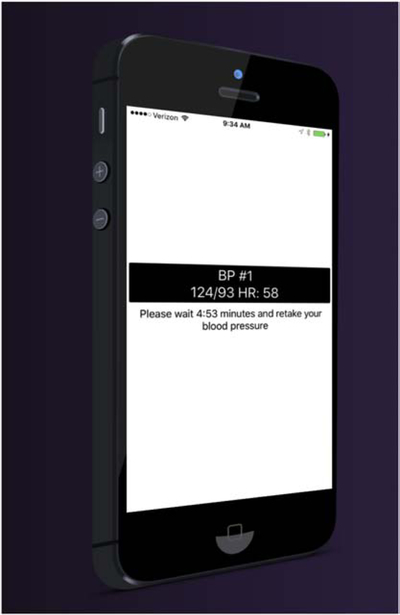
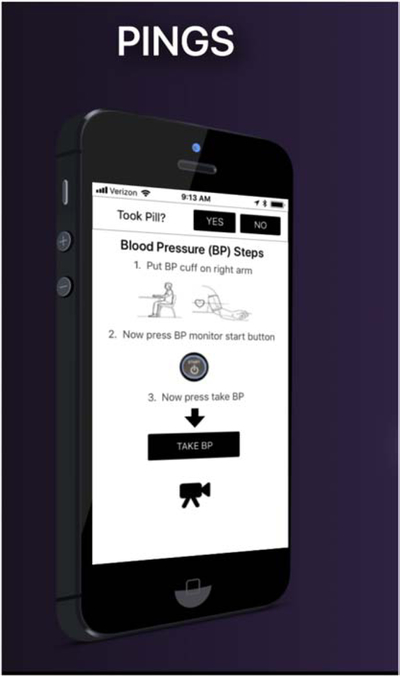
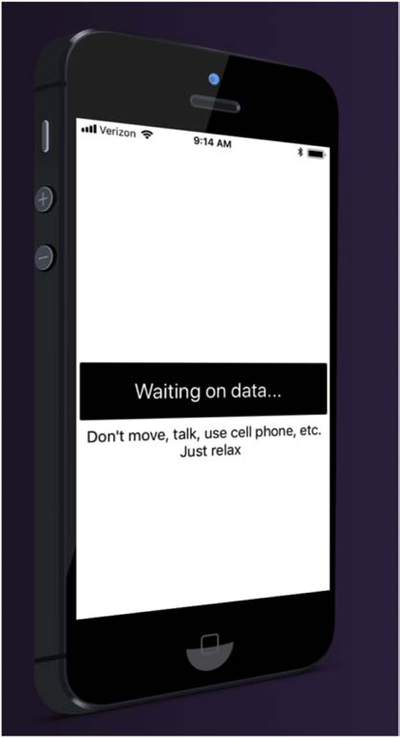
The PINGS feasibility trial used a two-arm cluster, randomized controlled design with the unit of randomization at the provider level (two physicians per arm) and patient outcomes as the unit of analysis.13 Patients in the intervention group were provided with an automated, battery powered, Blue-toothed UA-767Plus BT BP device (A&D, San Jose, CA, USA) along with a medical regiment assistance application for a Smartphone Galaxy J2 (which was given on loan to patients who did not own Smartphones) with the PINGS app embedded. The app is used for self-monitoring and auto transfer of encrypted BP measurements and medication intake. Encrypted blood pressure and medication adherence data, including time and date stamps, were relayed automatically to a HIPAA compliant central server at the Medical University of South Carolina (Figure 1.0). The patient and caregiver were shown how to successfully take three consecutive blood pressure readings using the app’s protocol and proper BP cuff placement and view the feedback chart and/or see their immediate BP data from that session on their phone (Figures 2.0–5.0). An easy to access and use push button entry format is provided to designate when medication have been taken (Figure 2.0). Participants receive immediate audio and visual feedback of BP and heart rate levels and can also select charts showing cumulative BP averages across weeks and months compared to BP control threshold levels. Participants randomized to the intervention received motivational and reinforcement messages in English using short message service (SMS) text messages tailored and delivered according to their medication adherence levels. Per the medication intake protocol, if the times stamp medication intake from the app was +/− 90 minutes of the pre-designated time, participants scored 100%; within +/− 180 minutes, 50%, and greater than 180 minutes outside of the designated window was rated at 0%. Tailored motivational and social reinforcement text messages were initially delivered the following day based on levels of adherence to the medication intake protocol. Following two consecutive weeks of 100% adherence, the schedule of SMS motivational and social reinforcement is taper ed to several days per week on a three-day average interval unless adherence drops below 90%. If this occurs, the daily feedback schedule was reactivated until 100% adherence criterion is met again. In addition, study participants received weekly messages on hypertension, stroke, and therapeutic lifestyle and behavioral modifications. This intervention lasted for 3 months. At the provider level, physicians and nurse navigators in the intervention arm received summary reports of their patients’ adherence to their medications and BP data tailored by them such as average and range of systolic or diastolic BP, percent of SBP/DBP controlled. They were also provided with summary charts of expert consensus BP management guidelines. If a patient’s mean BP exceeded the thresholds, the PINGS nurse navigator called the patient and conducted the BP protocol again and initiated a follow-up action as needed. Details on protocol schema are represented in Figure 1.0.
Fig. 1.
PINGS mHealth schema.
Fig. 2.
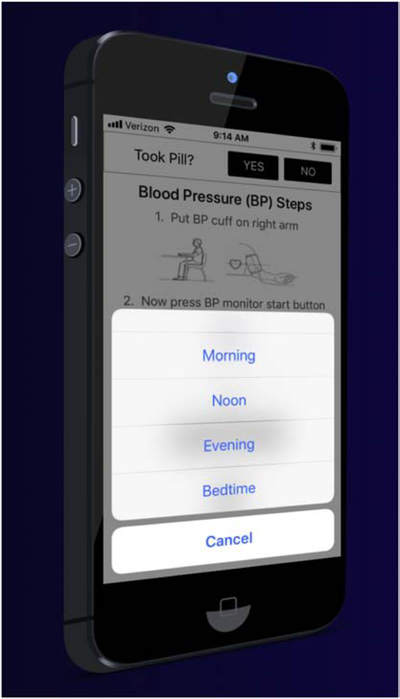
PINGS data capture.
Fig. 5.
Biometric integration.
A brief synopsis of the main outcomes of the PINGS trial:
The PINGS intervention was stopped after month 3 and both groups were followed up until month 9. Primary outcome measure was BP control defined at <140/90mmHg at month 9. Secondary outcome measures included: (i) medication adherence measured using the Medication possession ratio (MPR) at month 9 and (ii) technological glitches.
Outcomes:
(1) Blood pressure control at month 3 by intention to treat analysis was 20/30 (66.7%) vs 14/30 (46.7%), p=0.12 in the intervention and control arms respectively at interim analysis at end of intervention.14 At month 9, proportion on the intervention versus controls with systolic BP<140mmHg was 22/30 (73.3%) versus 13/30 (43.3%), p=0.035 in favor of the PINGS intervention.15 (2) Medication possession ratio scores at month 3 were better in the intervention arm (0.88 ± 0.40) versus standard care (0.64 ± 0.45) arm (p=0.03), and at month 9 was (0.95 ± 0.16) versus (0.98 ± 0.24), p=0.56. (3) Technology glitches reported among PINGS group included challenges with network connectivity.
Post-intervention focus groups:
Participants randomized to the interventional arm of the PINGS study, both stroke survivors and caregivers, were invited to participate in one of three focus group sessions upon completion of the 3-month post-intervention follow-up phase of the trial.13 Clinicians and members of the research team offered input through an additional focus group session designed to solicit their perspectives on the implementation of the pilot intervention and recommendations for broader scale implementation. Researchers (MN, AS) developed focus group interview questions guided by study objectives, outcomes, and the need for evaluative data to further guide intervention refinement (Tables 1 & 2).
Table 1.0.
Key Informant Interview Guide-Stroke Survivors and Caregivers
| Objective | Prompt |
|---|---|
| To explore participant’s perception and experiences with the PINGS App | 1) Before you joined this research study, do you feel you received the right amount of training on how to use the technology? Were there any things that we didn’t cover in the training that you would have found helpful? |
| 2) What did you think about using the smartphone to manage your blood pressure? How comfortable were you with this initially? How do you feel about using smartphones to manage your blood pressure now that you have been doing it for a while? | |
| 3) What are your thoughts on the app itself? What did you like about it? What was difficult about using it? | |
| 4) Did you have anyone help you with the smartphone, the app, or the pill box? If so, who helped you and what did they do to help? If your caregiver isn’t available to help, how could we better design the system to assist you? | |
| 5) What physical challenges do you have (if any) that made it more difficult to use the mobile phone to monitor your blood pressure? | |
| 5) What did you like most about using this technology for blood pressure control? | |
| 6) What changes would you recommend for us to improve using mobile phones or the app for patients in the future? Are there any particular things we could do to make the app easier to use? What suggestions do you have for training that may make it easier for other patients? How often should training occur? Are there any other topics that would be helpful to you and your family that we could deliver using mobile telephones and apps that would help you with your rehabilitation or maintaining your health? | |
| 7) What types of feedback did you receive from others when they heard about you using a smartphone and app to manage your blood pressure? How often did others encourage you to discontinue the PINGS intervention for alternative treatments? | |
| 8) What types of treatments or alternative treatments did you receive while you were in the PINGS study? | |
| 9) What challenges did you face in taking your blood pressure each day? What types did you have obtaining your blood pressure medications? How about your other cardiovascular medications? |
Table 2.0.
Focus Group Guide-Clinicians and Researchers
| Objective | Prompt |
|---|---|
| To explore the policy, organizational, provider and patient factors that may have influenced the implementation of the PINGS App in an operational setting |
|
Focus groups were conducted by an investigator trained in qualitative data collection (AS) and who had no prior interaction with study participants, thus minimizing response bias. Participant sessions were audio recorded and professionally translated from Twi, a Ghanaian native language, into English. Study participants received the equivalent of $5 and were provided with refreshments for their contributions and time completing the focus group session. The provider focus group session was conducted in English and each participating provider received the equivalent of $12. Translated transcripts were uploaded into NVivo 11.4.2 (QSR International, Pty, Doncaster, Victoria, Australia) for data analysis using a directed thematic content analytical approach.24 An experienced qualitative research methodologist (MN) conducted line-by-line coding of transcripts.25 An audit trail of analytical decision points, to include inductive coding and researcher perspectives, was maintained to increase confirmability of findings.26 Coded data were reviewed by the research team for agreement.
3. RESULTS
Four focus group (FG) sessions were conducted, three with stroke survivors and their caregivers (FGs 1–3) (N = 24) and one with representatives from the clinical and research team (FG 4) (N = 7). Demographic characteristics of participants are outlined in Table 3.0. All intervention participants were invited to participate in the FG sessions; however, some had moved out of the area following the intervention and others were not available due to scheduling or lack of transportation/no caregiver to assist. The participants of the FGs did not differ significantly from those who did not participate in the FGs by age, gender, location of residence, stroke severity nor blood pressure outcomes at month 3 and 9 (see Table 4).
Table 3.0.
Demographic Data on Participants
| Stroke Survivors (n=16) | Caregivers (n=8) | Research Team (n=7) | |
|---|---|---|---|
| Mean age (years) | 64.34 (range 43–89) | 36 (range 32–47) | 32.57 |
| Ethnicity | Akans (n=12) Hausa (n=2) Ewe (n=2) |
Akans (n=8) Hausa(n=0) Ewe (n=0) |
Akans(n=8) Hausa(n=0) Ewe (n=0) |
| Education | Uneducated (n=2) Secondary school, did not graduate (n=4) Secondary school graduate (n=10) |
Uneducated (n=4) Current student (n=2) University graduate (n=2) |
Uneducated (n=0) University graduate (n=7) |
| Occupation | Unemployed (n=3) Retired (n=13) |
Unemployed (n=4) Employed full-time (n=2) Student (n=2) |
Employed full-time (n=7) Physicians (n=4) Nurses (n=1) Research Assistants (n=2) |
Table 4.0.
Comparison of demographic, clinical characteristics, & blood pressure outcomes of PINGS participants who participated in a Focus Group (FG) session versus those who did not participate in a FG
| Characteristic | Participant in FG | Non-participant in FG | P-value |
|---|---|---|---|
| Age, mean | 54.3 ± 11.6 | 54.4 ± 12.8 | 0.98 |
| Female, % | 33.3% | 50.0% | 0.45 |
| Urban residence, % | 77.8% | 50.0% | 0.14 |
| National Institute of Health Stroke severity score, median (IQR) | 4.0 (2.0 – 5.0) | 5.5 (4.0 – 8.8) | 0.06 |
| Systolic BP at month 3, mean ± SD | 139.5 ± 19.8 | 133.8 ± 25.4 | 0.51 |
| Diastolic BP at month 3, mean ± SD | 89.6 ± 14.1 | 89.6 ± 16.4 | 0.99 |
| Systolic BP at month 9, mean ± SD | 137.9 ± 26.4 | 140.2 ± 19.1 | 0.81 |
| Diastolic BP at month 9, mean ± SD | 88.2 ± 17.6 | 94.5 ± 8.1 | 0.30 |
Categorization of major themes fell within four key areas: 1) barriers and facilitators toward intervention implementation; 2) adoption of BP screening; 3) increased antihypertensive medication adherence; and 4) perspectives on the use of technology as a means to monitor and control BP. Participants also offered recommendations for intervention refinement and ongoing BP maintenance. The four overarching themes present in all four focus group sessions and shared by stroke survivors, caregivers, and clinician/research team members were the ability to self-monitor BP, the use of technology as an interventional tool, training and support provided, and post-intervention adherence.
3.1. Theme 1: Ability to self-monitor BP
Overwhelming support was voiced regarding participants’ ability to monitor BP, evident in each of the focus group discussions. Stroke survivors and caregivers conveyed that the ability to monitor BP in the home setting facilitated medication adherence, increased awareness of BP, improved healthy dietary intake practices, and encouraged stress reduction. Benefits also included increased understanding of the importance of controlling BP and increased self-efficacy in becoming agents in the management of their care. Prior to participating in this trial, most individuals underwent BP monitoring only when hospitalized or during clinic visits with their providers. Access to home blood pressure monitoring (HBPM) was a novel and feasible approach welcomed by participants in the interventional arm.
Most of my friends used it to check their BPs and they were not even aware they had some…so they were very excited about it and said I was very lucky to have access to this technology from my hospital…even when I am asleep they would knock on my door to check their BPs.
(Stroke survivor #6, FG2)
For me what amused me was that this technology turned my wife into a nurse…. every morning she wakes up and she checks my BP and monitors my BP and checks everything for me…like a nurse. I am very happy with it.
(Stroke survivor #7, FG1)
It would alert me that my BP is high and then next time you will watch out for not eating such foods again.
(Caregiver #1, FG1)
I realized that sometimes when I was rushing to take the BP it would give me a very high reading. I think if you are calm, it would be normal.
(Stroke survivor #6, FG2)
Even if our BP is high we wouldn’t know unless we come to the clinic but that wasn’t the case when we had the machines.
(Caregiver #2, FG2)
3.2. Theme 2:Use of technology as an interventional tool
Technology was referenced both in terms of the devices used and process for engaging patients in routine monitoring of BP and medication adherence. Additionally, technology was addressed through the use of text messages, including patient perspectives on the messages. Researchers and clinicians from FG4 articulated the importance of identifying innovative strategies to fill the gap in the system of care, namely cost-effective and timely access to ongoing care and care management and felt this effort helped address these needs.
I want to say that my husband used to be checking my blood pressure when the phone and machine was there. Last Tuesday my BP went up when we didn’t have the machine but when we had the machines it was not the case; my BP was well controlled.
(Stroke survivor #6, FG1)
It was helping me control my BP very well. The last visit I came to the hospital, my BP was high but when I had the machine, it wasn’t the case.
(Stroke survivor #7, FG1)
It was good in terms of helping me take my medications at the right time.
(Stroke survivor #4, FG2)
The PINGS project is trying to correct a deficiency in the system in patient care. The use of mobile phones can aid in their care and also with regards to advice and the drugs they should take, what they should stop or what they should continue so they don’t have to travel all the way here for minor complaints.
(Participant #2, FG4)
While participants expressed the technology was extremely helpful in their ability to monitor their BP and improve their medication adherence, nearly all interventional participants shared a strong displeasure when the study ended and they no longer had access to the technology to meet their medical needs.
For me, I used to check for me mother. Her BP was always well controlled when we had the machine but since its gone, right now I don’t know whether her BP is high or low, so if we could have them back I would be really happy.
(Caregiver #5, FG2)
The next time you give us the machines I pray that you will not take it back….please next time don’t take the machines from us.
(Stroke survivor #1, FG3)
Since it was taken away now we don’t know the BP readings well. Although we take the medications, it is not the same. I will request that we could get them back.
(Stroke survivor #5, FG1)
Please try to give it back to us. Please, it was really helpful.
(Stroke survivor #4, FG3).
We plead that you consider giving it back to us to use as it helped a lot.
(Stroke survivor #4, FG2).
Most participants felt the text messages received were helpful and facilitated or reinforced positive health behaviors, as well as increased adherence to clinical recommendations. Participants also appreciated positive reinforcements received through messages when adherence was completed according to recommendations and expressed this helped motivate them to maintain consistency of these behaviors throughout the study.
For me, what helped was the messages that say you have done well…bravo for taking your medications on time. This was helpful for me and further motivates me to do so.
(Stroke survivor #4, FG2)
One message that was particularly helpful was that about our medication time…like if we miss a dose it would remind us to take in on time. That message was good.
(Stroke survivor #6, FG2)
I could follow the messages very well…it would say you didn’t take your medications on time yesterday and so the next day I am careful about the time my mother takes her pills, so this was really helpful.
(Caregiver #8, FG1)
Motivational and social reinforcement messages were based on the previous day’s reported medication adherence. Text message content included prompts for medication intake and BP monitoring. Additionally, messages encouraged promotion of healthy lifestyle behaviors. While most messages were easily understood and relevant to participants, several conveyed confusion regarding messages on smoking cessation. One participant stated “It didn’t really relate to me as I don’t smoke”. (Caregiver #5, FG 2)
3.3. Theme 3: Training and support
While prior familiarity with the use of smartphones and BP monitoring devices for home management of hypertension was non-existent among our sample, training and support provided allowed patients and caregivers to engage as active participants in their care, in collaboration with the care management team. Overall, participants expressed that initial training was helpful in acclimating to the equipment and process of BP monitoring; however, to ensure ongoing success of the project, study team members provided frequent support to stroke survivors and caregivers. When patients’ physical limitations precluded them from assessing their own BP, primary caregivers would take on this responsibility. However, for some patients, their caregiver was unable to be present consistently during the windows of time each day that were predesignated by the patient and/or caregiver for medication intake. Other support included troubleshooting equipment use difficulties (e.g., batteries needing replacement in BP monitor) and assistance with remembering passwords for access to the app. Focus group participants indicated that including more people in the training and having refresher-type sessions would have been helpful.
For me, I was not well when we started using it; my wife was the one who was trained and she taught the other children at home, so in this case, it would be helpful to train the family members.
(Stroke survivor #1, FG2)
I helped my husband. He couldn’t use it because of his sickness so I was doing it for him. I would check his BP, give him the medications, and also be reading the messages that would come on the phone.
(Caregiver #3, FG1)
Participants shared examples of problems faced during the interventional phase, such as occasional network connectivity problems, access to batteries needed to maintain operation of BP devices, and the need to re-enter codes or passwords for mobile phones, especially when powering phones off and on again. Additionally, participants had to remember to charge their phones, which was a challenge for some with no prior experience using a cellular phone. Support was provided by the research team; however, participants suggested future training include recommendations on how to trouble shoot technological challenges.
Beyond initial training and intermittent troubleshooting, participants received ongoing support from the team about BP monitoring, medication reminders, and in answering questions that arose among patients and caregivers. The use of mHealth facilitated access to clinical team and care needs between regular appointments. This was a key consideration for this population as travel to clinical appointments is often cost-prohibitive and logistically challenging. Ready access to study staff was welcomed by all and facilitated motivation and understanding on the rationale for some of the clinical recommendations.
Someone said to me, “It’s like you are living with your doctor.” It’s like you are getting all the advice and everything at home.
(Stroke survivor #6, FG1)
It’s like you are being watched by some health team and your BP is being managed.
(Stroke survivor #1, FG3)
For some participants, there was a steep learning curve in using technology, thus consideration for baseline training should account for varying levels of facility and familiarity with technology.
Some patients may be literate but technological literacy is also another thing. How to use an app is a new challenge on its own, like using an app whilst checking your BP. It is a huge challenge.
(Participant # 2, FG4)
I also got a lot of calls on the email and password. Sometimes patients could not do that themselves, so they used to call me numerous times to confirm that and we really had to teach them several times to do this.
(Participant # 5, FG4)
3.4. Theme 4: Post-intervention adherence
Participants noted increased medication and BP monitoring adherence during the study intervention; however, following conclusion of the 3-month study intervention period, adherence rates decreased. Commonly cited reasons for the lack of sustained level of adherence after intervention period ended and that participants no longer had access to BP monitoring and smartphone devices. Throughout each focus group, consensus was reached expressing the need for additional time to fully adopt practices as part of their normative routines.
Now we don’t know the BP readings well, although we take the medications…it is not the same. I will request that we could get the machines back.
(Stroke survivor #5, FG1)
I want to say that my husband used to be checking my blood pressure when the phone and machine was there. Last Tuesday my BP went up when we didn’t have the machine but when we had the machines it was not the case; my BP was well controlled.
(Stroke survivor #6, FG1)
With the machines, you get up in the morning and you check your BP and you do the same in the evening. You know your BP well but since it was taken away, we don’t’ know the BP readings well. Although we take the medications, it is not the same.
(Stroke survivor #5, FG1)
I had the machine and the phone for three months and it made me realize the importance of time in checking your BP…I was consistent. I learned a lot in the three months but now I don’t take my medications regularly.
(Stroke survivor #5, FG3)
Although I take my medications on time, since you took the machines, I have not checked my BP again. It is not good.
(Stroke survivor #3, FG3)
It makes you punctual with the time you take your medications but without the machine, it is difficult to stick to a time.
(Caregiver #2, FG2)
Since then I have not even checked my BP. I don’t even know how much my BP is these days. It would be very good to have them back.
(Stroke survivor # 6, FG3)
Consistent with patient and caregiver responses, providers similarly acknowledged a slight decline in medication adherence rates, although noting overall higher medication adherence rates continued among interventional group participants even after study period ended and the devices were removed.
I think despite the short time, we could still see a change in their habits. Those who had the machines had better control and even after we took them away their BPs were still controlled…it wasn’t as good as before, but it was better than the control arm.
(Participant #1, FG4)
3.5. RECOMMENDATIONS
Focus group participants offered recommendations for intervention refinement and ongoing BP maintenance. Suggestions encompassed a wide array of topics, including timing of message delivery, enhanced training, ongoing access to equipment, and provision for resources (i.e. batteries and additional remuneration for data coverage). Clinical team members from FG4 also recommended allowances for the study team to provide antihypertensive medications to participants either directly or through a dedicated pharmacist, which would facilitate access to medications, and subsequently increase medication adherence rates. All participants, stroke survivors, caregivers, and clinical team members, requested longer duration of the interventional period to fully adopt medication regimen and lifestyle practices, such as consistently, timely medication adherence, as part of their normative routines.
I would like to request that in the future we would be given these machines and smartphones for like 6 months or more instead of the 3 months.
(Caregiver #3, FG2)
Just give us back the machines…not for 3 months this time.
(Stroke survivor #4, FG3).
If we could have supplied the medications to the patients ourselves that would have made a great difference.
(Participant #1, FG4)
Timing of messages was discussed. Most participants expressed that it would be helpful to receive messages in the morning and evening, as some indicated that the messages were received quite late in the day.
4. DISCUSSION
Our study revealed several important factors for consideration in developing interventional approaches that use mobile technology to assist stroke survivors in Ghana. First, our research demonstrates an overwhelming receptivity toward home blood pressure monitoring (HBPM) within a LMIC setting to increase awareness of hypertension status (e.g., BP levels compared to hypertension cut-off levels) and to help facilitate adherence to antihypertensive medications. Second, novelty of HBPM yielded a positive impression among family members and the larger community and placement of home BP devices resulted in an unanticipated benefit to the larger community, as neighbors and the extended family network could also assess their own BP at no additional cost. Third, potential community level advantages may result from placing devices in the homes of stroke survivors since it could provide other high-risk patients living in resource limited areas with access to low-cost technology.
Targeted text messaging facilitated prompts for both BP monitoring to self-screen for hypertension status and medication intake. Moreover, the messages provided educational content on healthy lifestyle changes and provided participants with affirming messages for positive behavioral changes made. When participants forgot to meet targeted goals, the messages served as cues to action, providing necessary reminders. Furthermore, message content was found to be supportive, encouraging, motivating and easily understood.
Participants in the PINGS mHealth enabled intervention arm shared that they felt supported by the clinical team, fostering a sense of connectedness to providers between clinic visits, and conveying a sense of comfort knowing their BP was being closely monitored. While initial technological fluency was non-existent, with sustained training and support from the research team, stroke survivors and caregivers were able to utilize the devices and expressed increased comfort in using technology to meet their care needs over time.
While our study revealed several positive findings, some challenges were highlighted, which necessitate consideration in future iterations, and in achieving scalability. For example, intermittent cellular connectivity delayed message delivery and receipt at times and is a factor for real-time assessment of measurements. Our study was not reliant on real-time assessment and included a nursing support structure via telephonic follow-up in the event of missing data; however, for clinical considerations requiring immediate access to data this may pose as a limitation. Additionally, identifying methods to simplify the login process would prove beneficial. Participant recommendations for revision to our existing approach include increasing the level of financial support provided for data use and supplies (i.e. batteries for BP monitor), inclusion of a study pharmacist, and extending the intervention exposure period to improve likelihood of behavioral change and activation of long-term adoption of healthy habits and medical regimen recommendations.
4.1. Strengths and Limitations
The strengths of this post-intervention qualitative analysis include perspectives of stroke survivors, caregivers, and clinical/research team members, and adherence to rigorous qualitative methods. This post-intervention analysis was limited to 16 out of 30 individuals who participated in the intervention arm of the study or those involved in the care delivery or study implementation. Findings may not be generalizable to broader audiences or those from other geographic locations, although our results may inform researchers and clinicians interested in facilitating chronic disease monitoring and maintenance and medication adherence in resource limited regions. Although participants in our study were informed that devices would need to be returned post-intervention, initial understanding of potential benefits associated with access to these resources was not fully realized. Further funding should consider long-term placement of, at minimum, BP monitoring devices whenever possible, enabling participants to continue with self-monitoring of their hypertension status. Such information would help contribute to their medication adherence and also facilitate timely contact with healthcare providers when potential medication titrations are needed.
Gathering insight from end-users and those affected by clinical practice change can help facilitate intervention refinement and eventual uptake in adoption rates. Further study is needed to expand interventional exposure period, allowing assessment on long-term adoption of positive behavioral changes, and to determine the role and influence of social support through expanded engagement with the clinical team, in this case nurses. The potential for mobile phone-based interventions for stroke survivors in resource-limited settings27 may well extend beyond secondary vascular risk reduction to include domiciliary rehabilitation which been well-received and pilot-tested among Ghanaians with the overarching aim to improve longer-term outcomes of stroke survivors in the region beset by perennial shortage of skilled health personnel.28–32
5. CONCLUSION
Recent reports indicate that mobile technology usage in Sub-Saharan Africa is rapidly expanding. Notably, Ghana is highlighted as one of Africa’s largest mobile markets with penetration rates ranging between 119–128%.33–34 Ever increasing access to mobile technology, coupled with the tremendous burden of stroke within the region35 fueled by poor control of modifiable risk factors36–43, makes innovative low-cost strategies such as our PINGS mHealth approach to BP monitoring and antihypertensive medication adherence, not only a requisite but a practical and viable option to reduce subsequent morbidity and mortality among stroke survivors.
Fig. 3.
Blood pressure assessment.
Fig. 4.
Blood pressure measurement.
Highlights:
Blood pressure guidelines need to be culturally adapted for low-and-middle income countries
Mobile health offers a low-cost approach to blood pressure screening for stroke survivors
Targeted text messaging facilitated medication and blood pressure adherence
Intervention highly accepted and helped fill gaps in access to care
Targeted text messaging facilitated medication and blood pressure adherence
Increased intervention exposure needed to facilitate sustained adoption
Acknowledgments:
We would like to acknowledge the support of the following individuals for their assistance: Nathaniel Adusei-Mensah, Michael Ampofo, and Keesha Corbin.
Funding: This publication was supported by funding from the National Institutes of Health-National Institute of Neurological Disorders and Stroke Grant Number (R21NS094033) and the South Carolina Clinical and Translational Research Institute NIH - NCATS (Grant Number UL1 TR001450).
Financial Disclosures: The authors have no financial disclosures to report other than funding support provided for this research (listed below).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: None
References
- 1.Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1999–2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383(9913):245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics--2014 update: A report from the American heart association. Circulation. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Towfighi A, Markovic D, Ovbiagele B. Consistency of blood pressure control after ischemic stroke: prevalence and prognosis, Stroke J. Cereb. Circ 45 (2014) 1313–1317 [DOI] [PubMed] [Google Scholar]
- 4.Lewington S, Clarke R, Qizilbash N, et al. Prospective studies collaboration: age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360 (9349): 1093. doi: 10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 5.Biffi A, Anderson CD, Battey TW, et al. Association between blood pressure and risk of recurrent intracerebral hemorrhage. JAMA 2015; 319 (9): 904–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whelton Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017. doi: 10.1161/HYP. [DOI] [Google Scholar]
- 7.Owolabi MO. Taming the burgeoning stroke epidemic in Africa: stroke quadrangle to the rescue. West Indian Medical Journal 2011; 60:412–421. [PubMed] [Google Scholar]
- 8.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension, Cochrane database Syst. Rev (2010) CD005182. [DOI] [PubMed] [Google Scholar]
- 9.Sieverdes J, Gregoski M, Patel S, Williamson D. et al. Medication and blood pressure mhealth self management program with Hispanic hypertensives: a proof of concept trial, Smart Homecare Technol. TeleHealth 1 (2013) 1–10 [Google Scholar]
- 10.Okoro EO, Sholagberu HO, Kolo PM. Mobile phone ownership among Nigerians with diabetes. African Health Sciences 2010;10:183–6. [PMC free article] [PubMed] [Google Scholar]
- 11.Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet 2010;376:1838–45. [DOI] [PubMed] [Google Scholar]
- 12.Nichols M, Sarfo FS, Singh A, Qanungo S, Treiber F, Ovbiagele B, Saulson R, Patel S, Jenkins C. Assessing mobile health capacity and task shifting strategies to improve hypertension among Ghanaian stroke survivors. Am J Med Sci, 2017; 354(6): 573–580. doi: 10.1016/j.amjms.2017.08005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarfo FS, Treiber F, Jenkins C, Patel S, Gebregziabher M, Singh A, et al. Phone-based intervention under Nurse Guidance after stroke (PINGS): study protocol for a randomized controlled trial. Trials. 2016;17(1):436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarfo F, Treiber F, Gebregziabher M, Adamu S, Patel S, Nichols M, et al. PINGS (Phone-based Intervention under Nurse Guidance after Stroke): Interim results of a pilot randomized controlled trial. Stroke. 2018;49(1):236–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sarfo FS, Treiber F, Gebregziabher M, Adamu S, Nichols M, Singh A, Obese V, Sarfo-Kantanka O, Sayki A, Adu-Darko N, Tagge R, Agyei-Frimpong M, Kwarteng N, Badu E, Mensah N, Ampofo M, Jenkins C, Ovbiagele B, on behalf of PINGS Team. Phone-based intervention for blood pressure control among Ghanaian stroke survivors: A pilot randomized controlled trial. Int J Stroke, 2019; 14(6):630–638. DOI: 10.1177/1747493018816423 [DOI] [PubMed] [Google Scholar]
- 16.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care, 2007; 19(6):349–357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 17.Sarfo FS, Akassi J, Badu E, Okorozo A, Ovbiagele B, Akpalu A. Profile of neurological disorders in an adult neurology in Kumasi, Ghana. eNeurologicalSci. 2016;3:69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jenkins C, Burkett NS, Ovbiagele B, Mueller M, Patel S, Brunner-Jackson B, Saulson R, Treiber F. Stroke patients and their attitudes toward mHealth monitoring to support blood pressure control and medication adherence. mHealth. 2016; 2(24). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidson TM, McGillicuddy J, Mueller M, Brunner-Jackson B, Favella A, Anderson A, Torres M, Ruggiero KJ, Treiber F. Evaluation of an mHealth medication regimen self-management program for African American and Hispanic uncontrolled hypertensives. Journal of Personalized Medicine. 2015; 5(4): 389–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGillicuddy JW, Taber DJ, Mueller M, Patel S, Baliga PK, Chavin KD, Sox L, Favela A, Brunner-Jackson B, Treiber FA. Sustainability of improvements in medication adherence through a mobile health intervention. Progress in Transplantation. 2015; 25(3): 217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ovbiagele B, Jenkins C, Patel S, Brunner-Jackson B, Anderson A, Saulson R, Treiber F. Mobile health medication and blood pressure control in recent stroke patients. Journal of Neurological Sciences. 2015; 358: 535–537. [DOI] [PubMed] [Google Scholar]
- 22.Deci E, Ryan R. The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry. 2000; 11(4): 227–268. doi: 10.12017/S15327965PLI1104_01. [DOI] [Google Scholar]
- 23.Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: A comparison of two theoretical modules. Management Science. 1989; 35(8): 982–1003. [Google Scholar]
- 24.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res, 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 25.Saldaña J The Coding Manual for Qualitative Researchers. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 26.Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park, CA: Sage Publications; 1985. [Google Scholar]
- 27.Sarfo FS, Adamu S, Awuah D, Ovbiagele B. Tele-neurology in sub-Saharan Africa: a systematic review of the literature. J Neurol Sci. 2017;380:196–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B. Tele-rehabilitation after stroke: an updated systematic review of the literature. J Stroke Cerebrovasc Dis. 2018;27(9):2306–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sarfo FS, Adusei N, Ampofo M, Kpeme FK, Ovbiagele B. Pilot trial of a tele-rehab intervention to improve outcomes after stroke in Ghana: a feasibility and user satisfaction study. J Neurol Sci. 2018;387:94–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarfo FS, Adamu S, Awuah D, Sarfo-Kantanka O, Ovbiagele B. Potential role of tele-rehabilitation to address barriers to implementation of physical therapy among West African stroke survivors: a cross-sectional survey. J Neurol Sci. 381:203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sarfo FS, Ovbiagele B. Response by Sarfo and Ovbiagele to letter regarding “potential role of tele-rehabilitation to address barriers to implementation of physical therapy among West African stroke survivors: a cross-sectional survey. J Neurol Sci. 2017;382:162–163. [DOI] [PubMed] [Google Scholar]
- 32.Sarfo FS, Akassi J, Kyem G, Adamu S, Awuah D, Kantanka OS, et al. Long-term outcomes of stroke in a Ghanaian outpatient clinic. J Stroke Cerebrovasc Dis. 2018;27 (4):1090–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laary D Ghana: Mobile phone penetration soars to 128%. The Africa Report. 2016;13(46). https://www.theafricareport.com/1800/ghana-mobile-phone-penetration-soars-to-128/ [Google Scholar]
- 34.Ghanaians among top smartphone users in Africa. Citibusinessnews. (2018, March). http://citifmonline.com/2018/03/17/ghanaians-among-top-smartphone-users-in-africa/
- 35.Sarfo FS, Akassi J, Awuah D, Adamu S, Nkyi C, Owolabi M, et al. Trends in stroke admission and mortality rates from 1983 to 2013 in central Ghana. J Neurol Sci. 2015;357(1–2):240–5. [DOI] [PubMed] [Google Scholar]
- 36.Owolabi MO, Sarfo F, Akinyemi R, Gebregziabher M, Akpa O, Akpalu A, et al. Dominant modifiable risk factors for stroke in Ghana and Nigeria (SIREN): a case-control study. Lancet Glob Health. 2018;6(4):e436–e446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sarfo FS, Ovbiagele B, Gebregziabher M, Wahab K, Akinyemi R, Akpa O, et al. Stroke among young West Africans: evidence from the SIREN (Stroke Investigative Research and Educational Network) large multisite case-control study. Stroke. 2018; 49(5):1116–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sarfo FS, Mobula LM, Burnham G, Ansong D, Plange-Rhule J, Sarfo-Kantanka O, et al. Factors associated with uncontrolled blood pressure among Ghanaians: evidence from a multi-center hospital-based study. PLoS One. 2018;13(3):e0193494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sarfo FS, Mobula LM, Plange-Rhule J, Ansong D, Ofori-Adjei D. Incident stroke among Ghanaians with hypertension and diabetes: a multicenter, prospective cohort study. J Neurol Sci. 2018;395:17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sarfo FS, Mobula LM, Sarfo-Kantanka O, Adamu S, Plange-Rhule J, Ansong D, et al. Estimated glomerular filtration rate predicts incident stroke among Ghanaians with diabetes and hypertension. J Neurol Sci. 2019;396:140–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sarfo FS, Nichols M, Qanungo S, Teklehaimanot A, Singh A, Mensah N, et al. Stroke-related stigma among West Africans: patterns and predictors. J Neurol Sci. 2017;375:270–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ojagbemi A, Owolabi M, Akinyemi R, Arulogun O, Akinyemi J, Akpa O, et al. Prevalence and predictors of anxiety in an African sample of recent stroke survivors. Acta Neurol Scand. 2017;136(6):617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sarfo FS, Jenkins C, Singh A, Owolabi M, Ojagbemi A, Adusei N, et al. Post-stroke depression in Ghana: characteristics and correlates. J Neurol Sci. 2017;379:261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]