Abstract
Objective
To provide a report on year 1 results of a national study investigating nursing home information technology (IT) adoption, called IT sophistication.
Methods
A reliable and valid survey was used to measure IT sophistication. The target goal was 10% from each state in the United States, 1570 nursing homes. A random sample of homes from each state was recruited from Nursing Home Compare.
Results
The team reached 2627 nursing home administrators, among whom 1799 administrators agreed to participate and were sent a survey. A total of 815 surveys were completed (45.3% response rate), which was below the goal. Facilities in the participating sample have similar demographic characteristics (ownership, total population in a location, and bed size) to the remaining homes not participating. There are greater IT capabilities in resident care and administrative activities, less in clinical support. The extent of use of these capabilities appears to be highest in administrative activities and lowest in clinical support. IT in resident care appears to be the most integrated with internal and external stakeholders. IT capabilities appear to be greater than IT extent of use in all health domains, with the greatest difference in resident care.
Discussion
National evaluations of nursing home IT are rare. Measuring trends in IT adoption in a nationally representative sample provides meaningful analytics that could be more useful for policy makers and nursing home leaders in the future.
Conclusion
Discovering national baseline assessments is a first step toward recognizing nursing home trends in IT adoption.
Keywords: nursing homes, health information technology, surveys
INTRODUCTION
The most recent push for information technology (IT) adoption in the United States came through the Health Information Technology for Economic and Clinical Health (HITECH) Act of the American Reinvestment and Recovery Act in 2009.1 This law created substantial payments for health care organizations such as hospitals and physician clinics that adopt electronic health records (EHRs) and use them meaningfully. Long-term care organizations, including nursing homes, were excluded from receiving these payments, regardless of their progress in EHR adoption. Despite funding exclusions, some nursing homes have continued to make progress in the use of technology because there remains evidence supporting the notion that IT will make patient care safer for patients, improve communication among staff members, and make delivery of clinical work more efficient.2 The purpose of this paper is to report on year 1 results of a 3-year national survey investigating nursing home IT adoption, called IT sophistication. The study aim addressed in this paper is to describe IT sophistication (which includes 3 dimensions and 3 domains) and nursing home facility attributes (regional variation, ownership, and bed size) in a national sample of nursing homes.
Theoretical Underpinnings of IT Sophistication
The concept of IT sophistication originally developed from Nolan’s stage theory, proposed in 1973.3 Nolan’s theory has been used to understand the progress of national economies, biological growth patterns, issues of supply and demand, and organizational maturation, including technology adoption. Nolan’s stage theory “is based on a premise that elements in a system move through a pattern of distinct stages over time and that these stages can be described.”3 There are 6 stages of growth proposed in Nolan’s stage model.4 The first, initiation, occurs as IT is introduced into the organization. The second, contagion, is characterized by intense system development, greater innovation, and technological penetration into operations. The third stage is control. This stage, brought on by increasing chaos and perhaps uncertainty, introduces formalized project management and management reporting systems to manage IT growth. Integration, the fourth stage, occurs as users become more adept at using technology and perceive real value from the technology. Stages 5 and 6 are data administration and maturity, respectively. During these latter stages, technological structure and processes reflect organizational workflows, increasing data ownership by end users and stability commensurate with vision and mission.5
In research described in this paper, the concept of IT sophistication is being applied to trend IT adoption over a period of 3 years in nursing homes. The concept of IT sophistication was developed during a series of rigorous studies used to define 3 dimensions: functional IT sophistication (IT capabilities), technological sophistication (extent of IT use), and integration sophistication (degree of internal and IT external integration).6,7 Utilizing the IT sophistication instrument (Appendix 1) developed specifically for nursing homes, each of the dimensions can be measured over time at specific intervals to describe different stages of IT adoption. Further, stages that are identified can be trended over time to understand how IT development impacts a number of organizational factors related to nursing home care, such as quality measures or compliance with annual patient safety audits.
Assessments of Nursing Home IT
Research about nursing home IT adoption is important because it addresses gaps in knowledge about IT development in this sector. The increasing interest in and attention paid to nursing home IT adoption around the world8–10 signals the importance of studies that can close the gaps in knowledge pertaining to IT development. For instance, there is growing international recognition that quality indicators are needed to predict the impacts of technology on patient outcomes and services delivered,11 such as telemedicine, laboratory, and radiology indicators for assessing levels of computerization in hospitals. Furthermore, Hypponen et al.12 suggest that indicators are necessary to understand the progress of EHR functionality to monitor diffusion and advancement of policy initiatives.
In the United States, IT development has been inspired by programs incentivizing hospitals and providers to interface with other health care sectors, such as nursing homes. Some national programs encourage IT implementation in health care facilities, such as building health information exchanges with health care partners like nursing homes, to enable safer transitions in care and to reduce avoidable hospitalizations by improving care coordination activities and communication.13,14 Other statewide assessments of EHR adoption, such as in New York, revealed that 1 in 5 respondents to a nursing home survey had a fully implemented and operational EHR, and one-third had partially implemented and operational EHRs.15 Similar research and findings in other states have been identified.16–18 In addition, the types and extent of technology used in nursing homes can vary by type of organization. For instance, nonprofit homes, which must use all revenue within the nursing facility, commonly have higher investments in IT (greater IT sophistication) than for-profit homes, which look to reduce costs.19 In these instances, if better quality of care is realized, the difference may be seen in investments in IT capabilities, extent of use, and degree of IT integration, which facilitate superior care coordination activities and communication.
Research regarding the importance of IT is necessary because it can assist in the elimination of common perceptions of implementation caused by incomplete information about the benefits and costs of health IT.20 For example, although some perceive that IT is costly to implement, research has shown that IT can save on facility costs in the future through time savings, increased safety measures, and better resident health outcomes.21 Studies in nursing home IT adoption should aim to change perceptions of IT and encourage its implementation in facilities led by administrators that do not yet fully understand the advantages. Furthermore, rigorous IT studies in these settings can provide insights into prospective policies and the future of IT.
METHODS
Design
This research includes a cross-sectional design using surveys of US nursing homes that were randomly selected from each state using the publicly available Nursing Home Compare dataset, which is maintained by the Centers for Medicare and Medicaid.22 Nursing home sites were recruited between January 1, 2014, and July 31, 2015.
Sample
Nursing Home Compare files were downloaded in September 2013 in preparation for this study. Inclusion criteria were all nursing homes in the dataset located within the continental US, Alaska, and Hawaii. Nursing homes in Guam, Puerto Rico, and the US Virgin Islands were excluded. Veterans Administration government facilities were also excluded. A total of 15 653 nursing homes were identified in the final dataset. From the total sample, it is estimated that the majority of US nursing homes are for-profit and in metropolitan areas. Most facilities in this group have 60–120 beds. The smallest proportion of for-profit homes are located in rural areas with fewer than 2500 people and are smaller facilities with fewer than 60 beds. Conversely, most nonprofit nursing homes have 60–120 beds per facility and are located in metropolitan areas. Rural areas have the fewest homes with large bed size (>120 beds). The target goal for the sample was 10% from each state in the US, which amounted to 1570 nursing homes total. Nursing facilities were oversampled in each state by approximately 15% to help reach the recruitment goal.
Recruitment
Drawing on Nursing Home Compare, 10% of the nursing homes that met the inclusion criteria were recruited. The number of facilities selected in each state was proportional to the number of nursing homes located in that state. For example, because California had the largest number of homes (1241) and Alaska the smallest (15), 124 homes were randomly selected from California and 2 from Alaska. It was expected that not all nursing homes would be willing or able to participate, so at least 15% more homes were randomly selected in each state to help reach the recruitment goal. Nursing homes were not stratified prior to the random selection process, because it was suspected there would not be nursing homes within some strata in some states. Wyoming, for example, has only 38 homes, so there may not be any large homes in rural areas. Including every nursing home in the random selection process prior to stratification in each state regardless of ownership, bed size, or regional status meant that each facility had an equal opportunity to participate regardless of characteristics.
Measures
IT sophistication in nursing homes
IT sophistication measures have been defined in several series of studies conducted by the primary author dating back to 2007. In initial studies, the concept of IT sophistication, borrowed from industrial and acute care settings, was explored using qualitative techniques with 12 nursing home experts, who used sophisticated IT systems in their facilities in 3 states, to define and develop a relevant and reliable survey to measure IT sophistication.6 The definition of IT sophistication has evolved into a measure of IT capabilities (functional sophistication), extent of use (technological sophistication), and degree of internal/external integration (integration sophistication) in 3 domains of care: resident care, clinical support, and administrative activities (See Tables 1–3 and Instrument in Appendix 1). The survey instrument measuring IT sophistication has been tested and demonstrated to be reliable in a statewide sample of nursing homes in the Midwest US.7
Table 1.
Measures in IT Capabilities
| Resident care | Clinical support | Administrative activities |
|---|---|---|
|
|
|
Table 2.
Measures of IT Extent of Use
| Resident care | Clinical support | Administrative activities |
|---|---|---|
|
|
|
Table 3.
IT Integration Measures (Internal and External)
| Resident care | Clinical support | Administrative activities |
|---|---|---|
|
|
|
Cronbach’s alpha values for the ITS dimensions among 3 clinical domains were: resident care, .87–.88; clinical support, .86–.91; and administrative activities, .69–.80. Further proof of the reliability and validity of the instrument was gained through extensive qualitative observations of staff communication and documentation processes about skin and wound care management protocols in nursing homes with widely ranging IT sophistication measures.23,24 In these preliminary studies, social network analysis methodologies were used to evaluate the communication patterns between nurses and certified nurse assistants (CNAs) in nursing homes with diverse IT sophistication scores. Social network analysis allowed researchers to assess the efficiency of direct interactions between CNAs and registered nurses or licensed practical nurses. Interactions were found to be more frequent in homes with low IT sophistication and occurred in more centralized locations (eg, the nursing station) than those with high IT sophistication.23 All of this preparation led to the current 3-year study, which is assessing trends in IT sophistication in a national sample of nursing homes across the United States for the first time since 2004.25
Survey method
The entire survey has 61 questions; of those, 50 questions relate to the IT sophistication dimensions and domains of nursing home care and 11 questions gather descriptive information. Most of the survey questions assess the degree of IT integration with other care delivery systems. In the section addressing functional sophistication, respondents indicate a presence or absence of computerized IT capabilities by using checkboxes. For the analysis, respondents’ checkmarks are coded as IT either Available or Not Available and scored 1 or 0, respectively. In this section, an “Other” checkbox with a space for free text allows respondents to include any IT used in resident care not identified on the survey. In the technological dimension, respondents choose the most appropriate response after evaluating the extent of IT use in each domain of health care. Responses range from 0 to 7. A response of 0 indicates that IT capabilities for that domain are not used. If IT capabilities, such as a clinical decision support system, are being used, respondents will rate the extent of use of each capability on a scale from 1 (barely used) to 7 (extensively used). In the integration dimension, respondents indicate the extent of integration (electronic and automatic transfer of information) among internal and external stakeholders of the nursing home. Responses range from 0 (not at all) to 6 (very much) integration.
Survey respondents in each state were contacted and offered an electronic or paper survey. Respondents received a small compensation for completing the survey. All electronic links and paper surveys were managed using facility provider numbers available in Nursing Home Compare. Electronic links for the paper surveys were created for each one received and were entered into a database by 2 research staff members at 2 separate times. Electronic files were downloaded after all paper surveys were entered, and data entries were assessed by the statistician for discrepancies between data entry personnel. Discrepancies were immediately assessed and corrected by consensus between the 2 raters who entered the data. Every discrepancy was rectified by the end of the year 1 data collection period. All protocols related to recruitment, survey mechanisms, and compensation were approved by the university’s Institutional Review Board under project No. 1209004 and exempt application No. 116979.
Statistical methods
The software SAS V9.4 (SAS Institute Inc., Cary, NC, USA) was used for analysis. State was used as a stratifying variable. The weight assigned to each home in a state was determined by the total number of eligible homes in the state and the number of homes completing surveys in that state. Procedures that take into account the survey design were used for analysis. These were SURVEYFREQ, SURVEYMEANS, and SURVEYREG.
Scoring IT sophistication surveys
Possible scores for every dimension and domain were calculated for each survey. Here is an example of how scores were tabulated: The Resident Care sections include 4 questions about IT capabilities (functional IT sophistication). Question 1 is a general question about how IT is used to support resident care management, such as in admission processes; its scoring range is 0–6. Question 4 asks whether physicians use technology for resident care activities, such as documenting progress notes; its scoring range is 0–7. Question 9 asks about the use of technology to support nursing activities such as medication administration, documenting nursing flowsheets, and incident reporting; its scoring range is 0–14. Question 12 asks about technology supporting physical/occupational therapy activities such as care planning or consultations; its scoring range is 0–9. The sum of these questions’ maximum scores (6 + 7 + 14 + 9 = 36) gives a total possible range of 0–36 for functional IT sophistication in the Resident Care domain. The maximum overall raw score for IT sophistication that a nursing home facility can receive for all dimensions and domains is 628. In the analysis, each IT sophistication dimension and domain was weighted so that the maximum total for each of the 9 domain-dimension combinations was 100, resulting in a maximum total score of 900.
RESULTS
The research team made over 27 600 phone calls during the recruitment period. The recruitment team reached 2627 nursing home administrators across the United States. Of these, 1799 administrators agreed to participate and were sent a survey. Of those, 815 completed surveys were received (45.3% response rate) by the end of the recruitment period. A total of 735 facilities (90%) completed electronic surveys. A US map is provided, with tick marks indicating the locations of the nursing homes that completed the survey (see Figure 1). Although the goal was to have 10% from each state, that goal was not reached. However, facilities from each state included in the recruitment were represented.
Figure 1.
Nursing Homes Participating in IT Sophistication Survey Located by Zip Code
An assessment of the nursing home demographics in our sample was compared to the remainder of nursing homes in the national population (Table 4). All but 2 ownership categories have similar national statistics represented (within 1%) for each ownership type. In the sample, the majority of nursing homes that completed surveys are corporately owned for-profit (54.9%) and nonprofit (25.9%) agencies. The 2 types of ownership not as well represented in the sample were county-owned government facilities and nonprofit corporations. County-owned government facilities are slightly underrepresented and nonprofit corporations were slightly overrepresented in the sample compared to national statistics.
Table 4.
Characteristics of Nursing Home Samples
| Ownership | National Sample |
Study Sample |
|---|---|---|
| N (%) | N (%) | |
| For-profit | ||
| corporation | 8558 (57.7) | 448 (54.9) |
| Individual | 535 (3.6) | 25 (3.1) |
| Limited liability | 104 (0.7) | 6 (0.7) |
| Partnership | 1123 (7.6) | 64 (7.9) |
| Government | ||
| City | 86 (0.6) | 0 |
| City/County | 94 (0.6) | 3 (0.4) |
| County | 456 (3.1) | 3 (0.4) |
| Federal | 6 (0.04) | 0 |
| Hospital district | 131 (0.9) | 0 |
| State | 149 (1) | 0 |
| Nonprofit | ||
| Church related | 663 (4.5) | 43 (5.3) |
| Corporation | 2645 (17.8) | 211 (25.9) |
| Other | 288 (1.9) | 12 (1.5) |
| *Region | ||
| Metro (>50 000) | 9448 (63.8) | 478 (58.7) |
| Micro (10 000–49 999) | 2186 (14.8) | 126 (15.5) |
| Small town (2500–9999) | 1801 (12.2) | 114 (14) |
| Rural (<2500) | 1373 (9.3) | 97 (12) |
| *Bed size | ||
| >120 | 4354 (29.4) | 191 (23.4) |
| 60–120 | 7580 (51.1) | 472 (57.9) |
| <60 | 2903 (19.6) | 152 (18.6) |
Similar to other homes in the US, the majority of nursing homes sampled were located in metropolitan areas with a population greater than 50 000. In the sample, 97 facilities (11.9%) were located in rural locations with fewer than 2500 people. This is compared with 9.3% of the nursing homes in rural locations nationally.
Finally, the majority of facilities in the sample were medium-sized facilities with 60–120 beds. The proportion of our sample comprising smaller facilities, those with <60 beds, were within 1% of national averages. Mean nursing home bed size was calculated as 100.2 per facility, compared to the national mean of 106.6 certified beds per facility. Means were also calculated for total residents occupying a certified bed. Nationally, an average of 87.7 residents per facility occupied certified nursing home beds, versus 82.3 residents per facility in this nursing home sample.
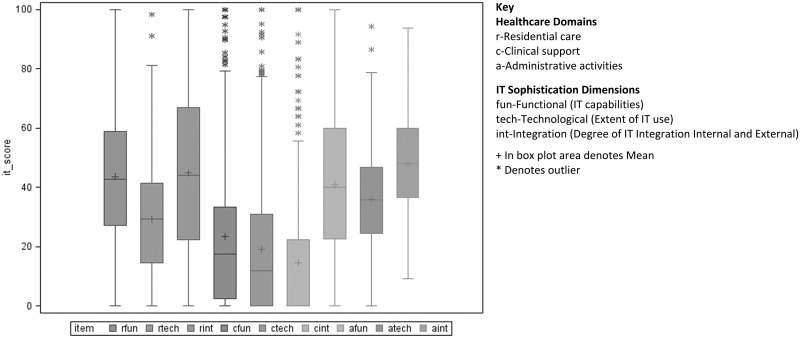
Figure 2 illustrates the box plots for each of the combined health care domains and IT sophistication dimensions for total IT sophistication in the sample. Comparing across health care domains in Figure 2, there appear to be greater IT capabilities in resident care (rfun) and administrative activities (afun) than clinical support (cfun). The extent of use of IT across the 3 health care domains overall appears to be greatest in administrative activities (atech), followed by resident care (rtech). The extent of use of IT appears to be lowest in clinical support (ctech) dimensions of care. There is a higher level of IT integration in resident care (rint) than in administrative activities (aint) or clinical support (cint). IT for clinical support activities has the lowest IT sophistication scores across each survey dimension, capabilities, extent of use, and integration. However, in the clinical support dimension a few outlier facilities reported greater IT capabilities, extent of use, and integration than the majority of facilities. A particularly interesting finding, occurring in each health care domain, is that IT capabilities appear to be greater than IT extent of use, with the greatest difference appearing in resident care. This could indicate that facilities may not be using IT capabilities to their fullest extent possible.
Figure 2.
National Scores by Health Care Domains and IT Sophistication Dimensions r: Residential care; fun: functional (IT capabilities); c: clinical support; tech: technological (extent of IT use); a: administrative activities; int: integration (degree of IT integration internal and external); + in box plot area denotes mean; *denotes outlier
DISCUSSION
National evaluations of nursing home IT adoption are rare. Early assessments indicate that nursing home IT was primarily used for administrative tasks (eg, billing), and not for other activities associated with resident care or even clinical support, where it can have a major impact on care.26 The most recent assessment of IT adoption in a national sample of nursing homes occurred in 2004, and was conducted by the National Center for Health Statistics.27 This most recent assessment demonstrated that IT adoption in nursing homes was gaining ground even before HITECH and meaningful use incentives were created. This immediate assessment of IT adoption in a national sample of nursing homes demonstrates that IT capabilities being adopted are not solely for administrative services or billing, but also include capabilities bolstering resident care and clinical support activities. However, just because a specific nursing home indicates that certain capabilities exist, such as creating an electronic progress note in resident care, does not mean they are extensively used in such activities, which means there is room for improvement.
In this assessment, the extent of use of IT capabilities provides a mechanism to discover the impacts of certain technologies on quality within different domains of health care. An example would be determining which IT capabilities being used most often, like those shown in Table 1, lead to higher-quality care. In each health care domain in this sample, the extent of IT use was lower than the total capabilities available to the nursing homes, with the greatest difference seen in resident care. This discovery will allow comparative benchmarks between best practices of IT implementation and influence on quality measures in nursing homes nationally. For instance, sustained use of EHRs via sophisticated handheld mobile devices in nursing homes over a period of years has been shown to improve resident outcomes in activities of daily living, range of motion, and high-risk pressure sores.28 However, these studies have limited generalizability due to the small number of facilities included in the research. Measuring trends in the extent of use in a nationally representative sample will provide meaningful analytics that could be more useful for policy makers and nursing home leaders in the future.
Another important measure incorporated into this study is IT integration with internal and external stakeholders. Low rates of integration, especially in clinical support activities, suggests that only a few nursing homes have adopted IT systems that allow for electronic exchange of clinical information, such as reporting of laboratory results or pharmacy orders for reconciliation purposes. Identifying early stages of IT integration and incorporating trend detection in IT adoption research will allow for better recognition of early tipping points between IT adoption stages and quality measure outcomes in the future.
No national studies are currently available to link nursing home IT adoption and publicly available quality measures available in Nursing Home Compare. This study is innovative because it will be the first to explore trends in relationships between nursing home IT sophistication measures (capabilities, extent of IT use, and how integrated IT is with other care systems) and nationally reported nursing home quality measures (resident outcomes). A next step in this research will be to evaluate the relationship between national trends in IT adoption and relationships with nursing home quality measures reported by the sample in the Nursing Home Compare database over the next 2 years.
Limitations
A limitation of this research may be a response bias for nursing homes that chose not to participate. In preliminary work, 40% of Missouri nursing homes participated, which is below the current response rate (45%). It can be assumed that some nursing homes may not participate because they have no technology, which could result in a reported overall higher level of IT sophistication than actually exists. Some nursing homes may not join the study because administrators do not have the requisite knowledge to complete the survey. Administrators were offered help to overcome these barriers in the form of contact information for the team and having questions answered during recruitment. Increased availability and support should reduce respondent burden, which should increase participation. Additionally, the large sample size and multiple sites should provide greater representation across different types of homes in different states.
CONCLUSION
As in other health care sectors, IT innovations have the potential to change the clinical practice paradigm in nursing homes by changing the way providers monitor and communicate resident needs and care processes. Discovering national baseline assessments of IT capabilities, extent of use, and integration with internal and external stakeholders is a first step toward recognizing nursing home trends in IT adoption. However, IT innovation is more appealing when it can be shown to sustain improvements in care delivery. Next steps in this research will be to continue assessing IT sophistication trends during the next 2 years and to evaluate relationships to national quality indicators reported by nursing homes.
FUNDING
This project was supported by grant No. R01HS022497 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
All authors made substantial contributions to the work through research design and participation in research methods, including recruitment, analysis, and reporting of results in this manuscript. All authors have agreed to be responsible for their part of this work.
REFERENCES
- 1. Department of Health and Human Services. HealthIT.gov. https://www.healthit.gov/policy-researchers-implementers/select-portions-hitech-act-and-relationship-onc-work 2012 March 14 [cited October 16, 2015]. https://www.healthit.gov/policy-researchers-implementers/select-portions-hitech-act-and-relationship-onc-work. Accessed 04/01/2016. [Google Scholar]
- 2. Matusitz J, Breen GM, Wan T. The use of eHealth services in US nursing homes as an improvement of healthcare delivery to residents. Aging Health. 2013;9(1):25–33. [Google Scholar]
- 3. Nolan RL. Managing the computer resource: a stage hypothesis. Communications of the ACM. 1973;16(7):399–405. [Google Scholar]
- 4. Nolan R. Managing the crises in data processing. Harvard Business Rev. 1979;57(3/4):115–126. [Google Scholar]
- 5. Hollyhead A, Robson A. A little bit of history repeating itself—Nolan's Stages Theory and the modern IS auditor. Inform Syst Audit Control Assoc J. 2012;5:46–49. [Google Scholar]
- 6. Alexander GL, Wakefield DS. IT sophistication in nursing homes. J Am Med Directors Assoc. 2009;10(6):398–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alexander GL, Madsen R, Wakefield DS. A regional assessment of information technology sophistication in Missouri nursing homes. Policy, Politics Nurs Pract. 2010;11(3):214–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fossum M, Ehnfors M, Svensson E, Hansen LM, Ehrenberg A. Effects of a computerized decision support system on care planning for pressure ulcers and malnutrition in nursing homes: an intervention study. Int J Med Inform. 2013;82(10):911–921. [DOI] [PubMed] [Google Scholar]
- 9. Georgiou A, Marks A, Braithwaite J, Westbrook J. Gaps, disconnections, and discontinuities—the role of information exchange in the delivery of quality long-term care. The Gerontologist. 2013;53(5):770–779. [DOI] [PubMed] [Google Scholar]
- 10. Holup AA, Dobbs D, Meng H, Hyer K. Facility characteristics associated with the use of electronic health records in residential care facilities. J Am Med Inform Assoc. 2013;20:787–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schuers M, Joulakian M, Griffon N, et al. Quality indicators from laboratory and radiology information systems. Medinfo: eHealth enabled Health. Sao Paulo, Brazil: IMIA and IOS Press; 2015:212–216. [PubMed] [Google Scholar]
- 12. Hypponen H, Faxvaag AGH, Hardardottir G, et al. Nordic eHealth indicators: Organisation of research, first results and plan for the future. Medinfo. IMIA and IOS Press; 2013: 273–277. [PubMed] [Google Scholar]
- 13. Alexander GL, Rantz M, Galambos C, et al. Preparing nursing homes for the future of health information exchange. Appl Clin Inform. 2015;6(2): 248–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rantz MJ, Alexander GL, Galambos C, et al. Initiative to test a multidisciplinary model with advanced practice nurses to reduce avoidable hospitalizations among nursing facility residents. J Nurs Care Qual. 2014;29(1):1–8. [DOI] [PubMed] [Google Scholar]
- 15. Abramson EL, McGinnis S, Moore J, Kaushal R, Investigators HITEC. A statewide assessment of electronic health record adoption and health information exchange among nursing homes. Health Services Res. 2014;49(1 Pt 2):361–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang T, Biedermann S. Adoption and Utilization of Electronic Health Record Systems by Long-Term Care Facilities in Texas. Perspectives in Health Information Management / AHIMA, American Health Information Management Association. 2012;9(Spring):1g. [PMC free article] [PubMed] [Google Scholar]
- 17. Jones M, Samore MH, Carter M, Rubin MA. Long term care facilities in Utah: a description of human and information technology resources applied to infection control practice. Am J Infection Control. 2012;40:446–450. [DOI] [PubMed] [Google Scholar]
- 18. Filipova AA. Electronic health records use and barriers and benefits to use in skilled nursing facilities. Comput Inform Nurs. 2013;31(7):305–318. [DOI] [PubMed] [Google Scholar]
- 19. Hamann DJ, Bezboruah KC. Utilization of technology by long-term care providers: Comparisons between for-profit and nonprofit institutions. J Aging Health. 2013;25(4):535–554. [DOI] [PubMed] [Google Scholar]
- 20. Bezboruah KC, Paulson D, Smith J. Management attitudes and technology adoption in long-term care facilities. J Health Organ Manag. 2014;28(3): 344–365. [DOI] [PubMed] [Google Scholar]
- 21. Kruse CS, Mileski M, Alaytsev V, Carol E, Williams A. Adoption factors associated with electronic health record among long term care facilities: a systematic review. BMJ Open. 2015;5(1):e006615. doi:10.1136/bmjopen-2014-006615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Centers for Medicare and Medicaid. Nursing Home Compare. http://www.medicare.gov. Accessed February 4, 2005.
- 23. Alexander GL, Steege L, Pasupathy K, Strecker EB. Case studies of IT sophistication in nursing homes: a mixed method approach to examine communication strategies about pressure ulcer prevention practices. Int J Industrial Eng. 2015;49:156–166. [Google Scholar]
- 24. Alexander GL, Pasupathy KS, Steege LM, Strecker EB, Carley KM. Multidisciplinary communication networks for skin risk assessment in nursing homes with high IT sophistication. Int J Med Inform. 2014;83(8): 581–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Resnick HE, Manard BB, Stone RI, Alwan M. Use of electronic information systems in nursing homes: United States, 2004. J Am Med Inform Assoc. 2009;16:179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Abbott PA, Brocht D. Challenges for data management in long-term care. In: Saba VK, McCormick KA, eds. Essentials of Computers for Nurses. 3rd ed New York: McGraw-Hill; 2001:357–364. [Google Scholar]
- 27. Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 Overview. National Center for Health Statistics.Vital Health Stat; 2009. Report No.:13(167). [PubMed] [Google Scholar]
- 28. Rantz MJ, Hicks L, Petroski GF, et al. Cost, staffing, and quality impact of bedside electronic medical record (EMR) in nursing homes. J Am Med Directors Assoc. 2010;11(7):485–493. [DOI] [PubMed] [Google Scholar]