Abstract
Objective: To characterize patients who voluntarily enrolled in an electronic health information exchange (HIE) program designed to share data between Veterans Health Administration (VHA) and non-VHA institutions.
Materials and Methods: Patients who agreed to participate in the HIE program were compared to those who did not. Patient characteristics associated with HIE enrollment were examined using a multivariable logistic regression model. Variables selected for inclusion were guided by a health care utilization model adapted to explain HIE enrollment. Data about patients’ sociodemographics (age, gender), comorbidity (Charlson index score), utilization (primary and specialty care visits), and access (distance to VHA medical center, insurance, VHA benefits) were obtained from VHA and HIE electronic health records.
Results: Among 57 072 patients, 6627 (12%) enrolled in the HIE program during its first year. The likelihood of HIE enrollment increased among patients ages 50–64, of female gender, with higher comorbidity, and with increasing utilization. Living in a rural area and being unmarried were associated with decreased likelihood of enrollment.
Discussion and Conclusion: Enrollment in HIE is complex, with several factors involved in a patient’s decision to enroll. To broaden HIE participation, populations less likely to enroll should be targeted with tailored recruitment and educational strategies. Moreover, inclusion of special populations, such as patients with higher comorbidity or high utilizers, may help refine the definition of success with respect to HIE implementation.
Keywords: health information exchange, medical records systems, computerized, matched-pair analysis, veterans health
BACKGROUND AND SIGNIFICANCE
The US health system is fragmented, with an individual’s health care services frequently delivered across a variety of organizations, and sometimes financed by multiple payers. This complex system presents the risk of poor coordination of care. In a 2011 survey by the Commonwealth Fund, medically complex patients in 11 countries were asked about care coordination. One-quarter of American respondents reported that their test results were not available, or that duplicate tests were ordered during a medical appointment, and 17% reported that information was not shared among their multiple care providers.1 Lack of coordination, however, is not limited to the United States. A quarter of Canadian and a fifth of Australian, French, Dutch, and Norwegian respondents indicated similar gaps in the availability of test results or duplicate testing during a medical appointment.1 The Veterans Health Administration (VHA), a nationwide integrated health care delivery system, is not immune to care coordination challenges. Despite the fact that providers share a common infrastructure and health information system, a recent survey of VHA primary care providers revealed that primary-specialty care coordination is often a challenge.2 Coordination can be especially challenging when patients see a combination of VHA and non-VHA providers. In a survey of non-VHA providers who were part of a practice-based research network,3 respondents reported poor communication with VHA colleagues, and they perceived their interactions to be with a “system” rather than a colleague. Furthermore, non-VHA providers identified the veteran (or patient) as the main vehicle for information transfer among different providers. Relying on the patient as the means of information transfer was a workaround process that non-VHA providers viewed as undesirable.3
Health information exchange (HIE) is an intervention designed to improve care coordination, involving the electronic exchange of data and information among health care providers.4 The process of HIE is facilitated by information technology standards and interoperability among electronic health record (EHR) systems.5 Both enable messages and documents to be sent before, during, and following episodes of care. For example, HIE is used to deliver laboratory results to ordering providers,6 as well as to deliver hospital discharge summaries to a patient’s primary care provider.7
Although there are questions regarding the sustainability of HIE and its effect on health outcomes,8–11 public policies and programs (eg, the US Centers for Medicare and Medicaid Services’ “meaningful use” program) have encouraged its adoption.9,12 Nearly 40% of hospitals report exchanging data with other hospitals outside their “network” of affiliates,12 and 15% of office-based physicians report exchanging data with outside organizations.9
Like other health care providers, the VHA is implementing HIE to improve coordination of care. While the VHA has exchanged information among its own network of facilities for several years, it is now pursuing HIE with non-VHA institutions. The current HIE initiative is part of the US government’s Virtual Lifetime Electronic Record (VLER) Health program and is designed for military service members and veterans.13–15 This initiative facilitates electronic data exchange with the US Department of Defense, as well as more than 30 community-based HIE networks across the nation.
Through VLER Health, providers in the VHA can view information about both VHA and non-VHA health care. Available information from multiple non-VHA sources is displayed to the user, who can then access specific information or reports on the computer (Figure 1). While prior articles have described the development and early lessons from the implementation of VLER Health,13,15 there have been no published descriptions of VHA patients who elect to participate, nor any reports of factors that may predispose a patient to enroll in the HIE program.
Figure 1.
Screenshots from the VistA Web application as used in educational material from the Veterans Health Administration explaining to providers how they can access information available from non-VA providers.
In this article, we describe patients who opted in to VLER Health at one of its early demonstration sites. Understanding characteristics related to participation in VLER Health may facilitate HIE participation throughout the VA by clarifying recruitment and educational strategies. This information will also be useful to other HIE communities that require patients to opt in before data can be shared.
MATERIALS AND METHODS
Overview
As part of an evaluation of the VLER-Indiana Health Information Exchange demonstration project (VA IIR 11-058), we sought to characterize, from 1 VHA medical center, patients who voluntarily provided authorization for the VLER Health program (ie, opted in to HIE) to share medical records with non-VHA providers. We compared the patients who provided authorization to have their information exchanged with those who did not provide authorization over a 12-month period.
Setting
The Richard L. Roudebush VA Medical Center (RLR) in Indianapolis, Indiana, provides acute inpatient as well as outpatient services for more than 60 000 patients. Health care services are delivered at the tertiary medical center and 3 community-based outpatient clinics located across central and southern Indiana. October 2011 was the VLER Health “go-live” month, when VHA providers at RLR were first able to access non-VHA health information. The enrollment period covered the 12 consecutive months ending March 2012 (index date). Included in this period is an initial 6-month “run-in” period, implemented to allow providers to become oriented and accustomed to VLER Health.
During the 12-month period, staff at RLR, including primary care nurses, invited patients attending clinics or refilling prescriptions to enroll in VLER Health. A community coordinator was assigned to RLR during this time, whose primary responsibility was to facilitate implementation of the VLER Health program, including recruitment of patients. Any patient could enroll in VLER Health, including those on their first visit to RLR. Patients were not required to have sought non-VHA care before enrolling in VLER Health. In addition to providing brochures to patients, the medical center staff also responded to any patient queries. Staff members explained that authorization would allow patients’ non-VHA providers to view their VHA medical records electronically, and vice versa.16 Patients were then given an authorization form to complete.17 Patients were approached on varying days and times, depending on the availability of the VLER Health coordinator and primary care staff who enrolled patients.
Population
The study population was limited to those patients “actively seeking” VHA care at RLR during the 12-month enrollment period. This active patient population was defined as having at least 2 outpatient visits or 1 inpatient visit during a 12-month period extending from 6 months before the go-live date (April 2011) to 6 months after (March 2012). We limited the study to active patients because of an in-person authorization requirement for VLER Health. The inclusion of only patients actively seeking care ensured that the entire study population at least had the opportunity to be approached about authorization during the period under study. Patients also had to be at least 18 years of age and alive at the end of the 12-month enrollment period.
Theoretical model
Because the voluntary authorization for VLER Health is likely influenced by both access to the VA (where patients were recruited) and whether a patient sought care outside the VA (a key value proposition), we sought a theoretical model to assess determinants of the decision to enroll in HIE. We chose to adapt the Andersen model of health care utilization and access18 as reframed by Phillips et al.19 This theoretical model (Figure 2) guided the selection of variables for our analyses.
Figure 2.
Theoretical model depicting the determinants of enrollment in health information exchange. Adapted from Phillips et al.19
Our theoretical model groups potential determinants of HIE enrollment into 3 categories: environment, population characteristics, and health behavior. Environmental determinants pertain to system-level elements, including the structure of the health system as well as the implementation or availability of HIE. For this study, the environmental determinants did not vary across our population, since all patients had access to the same VHA health care system and the same eligibility to participate in VLER Health.
Population characteristics pertain to person-level factors that may be associated with HIE enrollment, including sociodemographic variables such as gender, race, and marital status. Both level of trust in the health care system20 and concern about the privacy of shared information vary across populations.21 Alternatively, individual characteristics may encourage participation.
“Enabling resources” pertains to determinants of where and how individuals seek care. In the context of this study, enrollment priority scores (patients with greater disability are charged lower out-of-pocket costs) or participation in multiple insurance plans could influence patients’ use of VA and non-VA health care services. Alternatively, these “enabling resources” could be broader determinants of access. For example, long driving distance to a provider can pose a logistical or transportation barrier. Medical need is assessed by comorbidity level. Finally, health behavior includes the utilization of health services, because the decision to obtain health care can be a discretionary behavioral choice; outpatient care, in particular, is preference-sensitive.22
Data sources
We linked the EHRs of patients who sought care at RLR with those from non-VHA institutions participating in the Indiana Network for Patient Care (INPC). The INPC is one of the largest and oldest community-based HIE networks in the United States.23,24 The INPC is managed by the Indiana Health Information Exchange (IHIE), an Indiana-based not-for-profit corporation that seeks to improve the quality, safety, and efficiency of health care in Indiana. The INPC connects over 90 health care facilities across the state, including hospitals, physician practices, pharmacy networks, long-term post–acute care facilities, laboratories, and radiology centers. The INPC maintains over 5 billion structured observations and more than 200 million text reports for over 12 million individuals. Nearly 1 million electronic health care transactions are processed every day by IHIE in support of its client services, including clinical results delivery25 and coordination of care.26
Records were linked using a combination of patient identifiers by a probabilistic algorithm used by the INPC.27 The combined records enabled use of covariates available from both the VHA and INPC, where data from both sources were available.
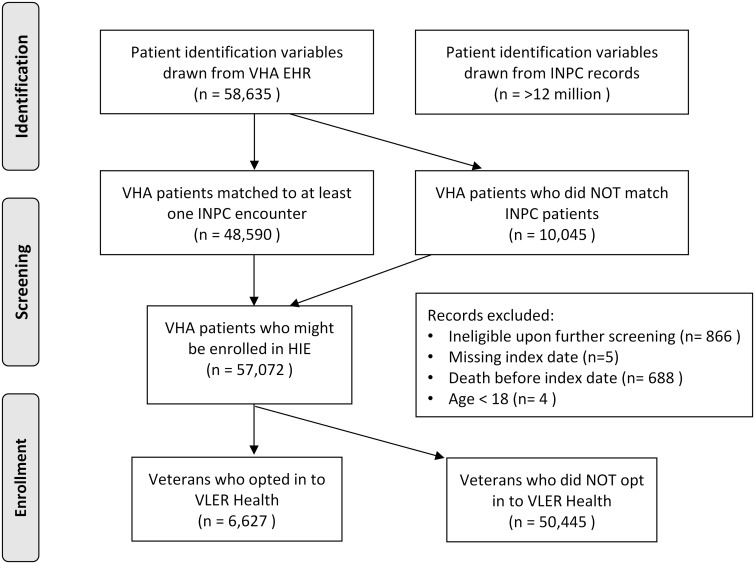
We attempted to match all patients actively seeking care at RLR prior to the go-live date (N = 58 635) with more than 12 million patients in the INPC. A total of 48 590 patients (83%) had at least 1 non-VHA health care datum in the INPC. Patients were included in the enrollment analysis even if they did not have any corresponding records in the INPC. However, electronic health data after the go-live date were needed from either VHA or HIE records. Figure 3 depicts a flow diagram showing how records were matched, how exclusion criteria affected the denominator, and the results of the record linkage process.
Figure 3.
Model of the study population depicting inclusion and exclusion criteria as well as proportion of the population that enrolled in health information exchange.
Measures
Determinants
As of March 2012, all patient demographics (age, gender, and marital status) and measures of enabling resources (insurance type, VA benefits priority group, and Euclidean distance as calculated from the patient’s postal ZIP code to RLR) were obtained from visit data in VHA administrative outpatient files. In addition to distance, we also calculated the population of the city or town in which the patient lived, because it provided a proxy to distinguish between urban and rural populations. We further calculated the Charlson comorbidity index based on ICD-9 codes entered at the time of patient encounters over the 12-month enrollment period. VA benefits priority group assignments (known within the VHA as enrollment priority scores) take into account disability and income.28 Furthermore, we determined the numbers of primary care outpatient visits, specialty care outpatient visits, and hospitalizations (over the 12-month enrollment period). Insurance type and race/ethnicity were ascertained using both VHA and INPC data.
Outcome
The dependent variable for this study was an authorization for the VLER Health program (yes or no), which was recorded in the VHA EHR.
Data analysis
Patient characteristics were summarized by VLER Health participation status and tested for significant differences by use of chi-square, Fisher’s exact test, and Wilcoxon rank sum test. Multivariable logistic models with binary outcome of enrollment in VLER Health were used to estimate odds ratios and 95% confidence intervals for each variable of interest. The c-statistic was calculated to assess the overall predictive ability of the model (0.5 = no predictive ability, 1 = perfect prediction). In addition, a pseudo R-square29 was calculated for the model. Partial pseudo R-squares for each theoretical model category (enabling resources, population characteristics, health utilization, morbidity) were also obtained by taking the difference between the pseudo R-square for the full model and the pseudo R-square from models fit by omitting that category. If the amount of missing data for a particular variable was >1%, an “unknown” category was created to enable use of records that would otherwise be excluded; otherwise, patients with missing data were omitted from the multivariable model (n = 48 or 0.08% omitted).
RESULTS
A total of 57 072 patients actively sought care during the enrollment period and therefore were potentially eligible to participate in VLER Health at RLR. The potential determinants of HIE enrollment among this population, grouped together based on the theoretical model, are summarized in Table 1. Most (92.8%) of the population was male, over age 50 (78.0%), from an urban environment (76.6%), and white (55.2%). Notably, the population was much more diverse than the general population of the state, with about one-fifth (18.1%) recorded as black or African-American. Approximately 40% of enrollees had a Charlson comorbidity index of at least 1. All demographics except gender were significantly related to participation in the VLER Health program.
Table 1.
Demographics and other covariates of the veteran population eligible to enroll in the VLER Health program at the Richard L. Roudebush VA Medical Center in Indianapolis, IN
| Block | Covariate | Value or Category | Overall Count (%) |
Control (%) |
Enrolled (%) |
P-value |
|---|---|---|---|---|---|---|
| N = 57 072 | N = 50 445 | N = 6627 | ||||
| 1 | Age (years) | <40 | 6355 (11.1) | 5869 (11.6) | 486 (7.3) | <.0001 |
| 40 to <50 | 6225 (10.9) | 5596 (11.1) | 629 (9.5) | |||
| 50 to <65 | 21 953 (38.5) | 19 166 (38.0) | 2787 (42.1) | |||
| 65+ | 22 539 (39.5) | 19 814 (39.3) | 2725 (41.1) | |||
| Gender | Female | 4120 (7.2) | 3606 (7.1) | 514 (7.8) | 0.0723 | |
| Male | 52 952 (92.8) | 46 839 (92.9) | 6113 (92.2) | |||
| Race or ethnicity | American Indian or Alaskan native | 232 (0.4) | 219 (0.4) | 13 (0.2) | <.0001 | |
| Black not of Hispanic origin | 10 311 (18.1) | 8847 (17.5) | 1464 (22.1) | |||
| Hispanic | 267 (0.5) | 219 (0.4) | 48 (0.7) | |||
| Other | 515 (0.9) | 449 (0.9) | 66 (1.0) | |||
| White not of Hispanic origin | 31 476 (55.2) | 27049 (53.6) | 4427 (66.8) | |||
| Unknown | 14 271 (25.0) | 13662 (27.1) | 609 (9.2) | |||
| Marital status | Married | 30 692 (53.8) | 26937 (53.4) | 3755 (56.7) | <.0001 | |
| Not married | 25 544 (44.8) | 22706 (45.0) | 2838 (42.8) | |||
| Unknown | 836 (1.5) | 802 (1.6) | 34 (0.5) | |||
| Residence location | Isolated small rural city | 1603 (2.8) | 1506 (3.0) | 97 (1.5) | <.0001 | |
| Small rural city | 3620 (6.3) | 3365 (6.7) | 255 (3.8) | |||
| Large rural city | 8130 (14.2) | 7404 (14.7) | 726 (11.0) | |||
| Urban | 43 719 (76.6) | 38170 (75.7) | 5549 (83.7) | |||
| 2 | Charlson index (1 year before index date) | 0 | 34 851 (61.1) | 31688 (62.8) | 3163 (47.7) | <.0001 |
| 1 | 10 881 (19.1) | 9367 (18.6) | 1514 (22.8) | |||
| 2+ | 11 340 (19.9) | 9390 (18.6) | 1950 (29.4) | |||
| 3 | Insurance | Commercial | 10 124 (17.7) | 8716 (17.3) | 1408 (21.2) | <.0001 |
| Medicaid | 3621 (6.3) | 3123 (6.2) | 498 (7.5) | |||
| Medicare or Medicare supplement | 10 383 (18.2) | 8898 (17.6) | 1485 (22.4) | |||
| Military | 1737 (3.0) | 1469 (2.9) | 268 (4.0) | |||
| None or self-pay | 2173 (3.8) | 1856 (3.7) | 317 (4.8) | |||
| Other or unknown | 22 993 (40.3) | 21490 (42.6) | 1503 (22.7) | |||
| Prison | 287 (0.5) | 236 (0.5) | 51 (0.8) | |||
| VA insurance alone | 5754 (10.1) | 4657 (9.2) | 1097 (16.6) | |||
| VA benefits priority group | Medicaid or other public assistance | 18 504 (32.4) | 16435 (32.6) | 2069 (31.2) | <.0001 | |
| Catastrophically disabled | 9407 (16.5) | 8127 (16.1) | 1280 (19.3) | |||
| Moderate disability | 16 997 (29.8) | 14933 (29.6) | 2064 (31.1) | |||
| No service-connected disability | 11 139 (19.5) | 9992 (19.8) | 1147 (17.3) | |||
| Unknown | 1025 (1.8) | 958 (1.9) | 67 (1.0) | |||
| Distance from postal ZIP code to VA medical center (miles) | N | 57 028 | 50407 | 6621 | ||
| Mean ± SD | 65.7 ± 167.0 | 68.4 ± 170.1 | 45.1 ± 139.9 | <.0001 | ||
| Median (Min–Max) | 31.4 (0–8273.2) | 37.3 (0–8273.2) | 13.9 (0–4262.4) | |||
| 4 | Primary care outpatient visits (1 year before index date) | N | 57 068 | 50441 | 6627 | |
| Mean ± SD | 2.8 ± 2.8 | 2.6 ± 2.7 | 3.9 ± 3.1 | <.0001 | ||
| Median (Min–Max) | 2 (0–73) | 2 (0–73) | 3 (0–32) | |||
| Specialty care outpatient visits (1 year before index date) | N | 57 068 | 50 441 | 6627 | ||
| Mean ± SD | 1.9 ± 3.5 | 1.7 ± 3.1 | 3.5 ± 5.7 | <.0001 | ||
| Median (Min–Max) | 1 (0–109) | 0 (0–86) | 2 (0–109) | |||
| Number of hospitalizations (1 year before index date) | 0 | 48 812 (85.5) | 43 620 (86.5) | 5192 (78.3) | <.0001 | |
| 1 | 5245 (9.2) | 4379 (8.7) | 866 (13.1) | |||
| 2+ | 3015 (5.3) | 2446 (4.8) | 569 (8.6) |
Blocks are derived from the theoretical model. Block 1 corresponds to sociodemographics. Block 2 corresponds to comorbidity. Block 3 corresponds to access to care (enabling resources). Block 4 corresponds to utilization of health services.
Among the study population, approximately 12% (n = 6627) provided authorization for VLER Health. The multivariable logistic regression results for predicting VLER Health authorization are summarized in Table 2. The following characteristics were significantly associated with greater odds of authorization: female vs male (OR = 1.12; 95% CI, 1.01-1.25); age 50–64 years vs 65+ years (OR = 1.10; 95% CI, 1.03-1.18); Charlson comorbidity index 1 vs 0 (OR = 1.25; 95% CI, 1.16-1.34) or 2 + vs 0 (OR = 1.29; 95% CI, 1.19-1.39); military co-insurance vs VA insurance alone (OR = 1.17; 95% CI, 1.01-1.37); and catastrophically disabled vs no service-connected disability (OR = 1.12; 95% CI, 1.02-1.23) or moderate disability vs no service-connected disability (OR = 1.26; 95% CI, 1.16-1.37). Lower odds of authorization were seen in those not married (OR = 0.90; 95% CI, 0.85-0.95) or with unknown marital status (OR = 0.42; 95% CI, 0.30-0.60) compared to married individuals. Living in isolated small rural (OR = 0.53; 95% CI, 0.43-0.66), large rural (OR = 0.75; 95% CI, 0.69-0.82), or small rural city (OR = 0.60; 95% CI, 0.52-0.69) vs urban environment was associated with lower odds of authorization. The odds of authorization were greater for each additional primary-care visit (OR = 1.08; 95% CI, 1.07-1.09) or specialty-care visit (OR = 1.08; 95% CI, 1.07-1.08).
Table 2.
Multivariable logistic regression model analyzing covariates that may influence whether a veteran enrolls in a health information exchange program
| Multivariable Model (n = 57 024) | |||||||
|---|---|---|---|---|---|---|---|
| Block | Covariate | Value or Category | Overall Test P-value | P-value | OR (95% CI) | Partial R2 | |
| 1 | Age (years) | <40 | <.0001 | 0.0440 | 0.89 (0.79, 1.00) | 0.019 | |
| 40 to <50 | 0.4586 | 0.96 (0.87, 1.07) | |||||
| 50 to <65 | 0.0041 | 1.10 (1.03, 1.18) | |||||
| 65+ | reference | ||||||
| Gender | Female | 0.0329 | 0.0329 | 1.12 (1.01, 1.25) | |||
| Male | reference | ||||||
| Race | American Indian or Alaskan native | <.0001 | 0.0021 | 0.41 (0.23, 0.72) | |||
| Black not of Hispanic origin | 0.5792 | 0.98 (0.91, 1.05) | |||||
| Hispanic | 0.2089 | 1.23 (0.89, 1.71) | |||||
| Other | 0.7827 | 0.96 (0.74, 1.26) | |||||
| Unknown | <.0001 | 0.40 (0.36, 0.44) | |||||
| White not of Hispanic origin | reference | ||||||
| Marital status | Married | <.0001 | reference | ||||
| Not married | 0.0003 | 0.90 (0.85, 0.95) | |||||
| Unknown | <.0001 | 0.42 (0.30, 0.60) | |||||
| Residence location | Isolated small rural city | <.0001 | <.0001 | 0.53 (0.43, 0.66) | |||
| Small rural city | <.0001 | 0.60 (0.52, 0.69) | |||||
| Large rural city | <.0001 | 0.75 (0.69, 0.82) | |||||
| Urban | reference | ||||||
| 2 | Charlson index (in year before index date) | 0 | <.0001 | reference | 0.002 | ||
| 1 | <.0001 | 1.25 (1.16, 1.34) | |||||
| 2+ | <.0001 | 1.29 (1.19, 1.39) | |||||
| 3 | Insurance | Commercial | <.0001 | 0.2731 | 0.95 (0.87, 1.04) | 0.010 | |
| Medicaid or other public assistance | 0.0464 | 0.88 (0.78, 1.00) | |||||
| Medicare or Medicare Supplement | 0.1518 | 0.93 (0.85, 1.03) | |||||
| Military | 0.0422 | 1.17 (1.01, 1.37) | |||||
| None/Self-pay | 0.6692 | 0.97 (0.84, 1.12) | |||||
| Other/Unknown | <.0001 | 0.60 (0.54, 0.66) | |||||
| Prison/Jail | 0.0925 | 1.31 (0.96, 1.80) | |||||
| VA insurance alone | reference | ||||||
| VA benefits priority group | Medicaid assistance/Low income | <.0001 | 0.5515 | 1.03 (0.94, 1.11) | |||
| Catastrophically disabled | 0.0131 | 1.12 (1.02, 1.23) | |||||
| Moderate disability | <.0001 | 1.26 (1.16, 1.37) | |||||
| No service-connected disability | reference | ||||||
| Unknown | 0.0441 | 0.76 (0.58, 0.99) | |||||
| Distance from ZIP code to VA medical center (10-mile increase) | <.0001 | 0.992 (0.990, 0.995) | |||||
| 4 | Primary care visit (1 visit increase) | <.0001 | 1.08 (1.07, 1.09) | 0.034 | |||
| Specialty care visit (1 visit increase) | <.0001 | 1.08 (1.07, 1.08) | |||||
| Number of hospitalizations | 0 | 0.1191 | reference | ||||
| 1 | 0.0411 | 1.09 (1.00, 1.19) | |||||
| 2+ | 0.9126 | 1.01 (0.90, 1.12) | |||||
Blocks are derived from the theoretical model. Block 1 corresponds to socio demographics. Block 2 corresponds to comorbidity. Block 3 corresponds to access to care (enabling resources). Block 4 corresponds to utilization of health services.
The c-statistic for the model was 0.716 with a pseudo R-square of 0.11. Partial pseudo R-square values suggest that utilization (R2 = 0.034) had the largest impact on VLER Health authorization, followed by personal characteristics (R2 = 0.019) such as age or geographic location (urban vs rural).
DISCUSSION
To characterize patients who voluntarily enrolled in the VLER Health program, we integrated clinical and administrative records from VHA and non-VHA sources. To our knowledge, this is the first study to examine which characteristics of patients are associated with enrollment in HIE using pooled data from both within and outside of an integrated health care delivery system.
We found that prior utilization had the strongest associations with authorization, as suggested by our theoretical framework. However, the association with utilization may be a product of the authorization process. Specifically, patients who make frequent visits to the medical center have increased opportunities to be approached by staff for enrollment. The same is true for higher comorbidity and disability. Theoretically, more medically complex patients may perceive a greater value in VLER Health, because they recognize the possibility that they are likely to need health care services (whether routine or emergent) outside the VHA system at some point in the future. At the same time, these patients also tend to seek care more frequently and may have had more opportunities to provide authorization. Finally, married patients may be more likely to take advantage of programs like VLER Health because informal caregivers like spouses are often information brokers in the absence of HIE.30,31
The importance and implications of HIE enrollment
Recent policy changes have heightened the importance of understanding what types of patients are most likely to authorize data sharing via VLER Health. For example, the Veterans Access, Choice, and Accountability Act32 expands access to care at non-VHA facilities when either the VHA is unable to provide access within a reasonable time frame or the patient lives more than 40 miles from the nearest VHA facility. Such a provision introduces new care coordination challenges. For patients who seek care both inside and outside the VHA, the VHA cannot rely on its integrated delivery system structure to coordinate care; it will need HIE to ensure that patient data are available regardless of provider. This challenge is similar to that faced by other health systems and accountable care organizations attempting to coordinate care in order to achieve the goals of the Accountable Care Act as well as the CMS meaningful use program.33 For HIE to be successful in any of these settings, patients will need to provide consent and be engaged in activities that share their health information with the range of providers they see both in and out of their primary network.
Patient enrollment challenges
We observed that just under 12% of the patients eligible for enrollment actually enrolled in the VLER Health program within its first year at RLR. These findings suggest that obtaining consent for HIE requires recruitment on a larger, more comprehensive scale than typically undertaken in new HIE initiatives. However, the 12% figure does not tell the full story, since not all patients were approached or asked to enroll in VLER Health. At the time of implementation, RLR chose not to send mass mailings about the program to all patients. In the first 12 months of the program, the target enrollment was 1000 veterans, given (1) a desire to introduce VLER Health incrementally so that clinicians and patients could become accustomed to the approach more gradually, and (2) other VHA facilities’ prior struggles to enroll patients via mass mailings.15 Thus, the enrollment of over 6000 veterans within 18 months, while much smaller than the eligible population (57 072), exceeded expectations. In future implementation efforts, tracking a denominator of patients contacted about HIE participation at a facility (vs patients actively seeking care) would provide the most accurate picture of the success of any recruitment approach.
Surveys of patients indicate a strong desire to provide consent before information is shared via HIE with other parties, including physicians.21,34 Thus, many health systems beyond VHA have also implemented opt-in models where patients provide authorization for HIE. While some communities have reported 90% enrollment rates,35,36 others have struggled to obtain authorization from large populations of patients. Studies in communities that struggle with enrollment suggest that the workflow in which authorization is obtained is an important factor.37,38 Therefore, authorization remains an ongoing target for improvement within VHA sites as they expand the VLER Health program. Given the widespread prevalence of EHR systems, as well as the ongoing need for outside information to inform care transitions, future research should explore multiple ways to obtain authorization and test optimal workflows for HIE.
Using enrollment to target priority populations
The use of enrollment data to identify specific patient populations who are less likely to authorize HIE could be helpful in promoting the development of strategies for reaching out to those populations. For example, patients who live farther from a VHA medical center could especially benefit from HIE, because they may have more occasion to use non-VHA care, either for unexpected medical events or to minimize driving time. However, patients living at a greater distance were less likely to provide authorization for VLER Health, as were patients who lived in rural areas. It is possible that rural populations have unique beliefs and attitudes toward local health care, the VA, or privacy that influence their decision to enroll in HIE. Therefore, development of tailored messages for rural patients or collaboration with known non-VHA providers in rural communities may be necessary to improve outreach among this population.
We also found that veterans younger than 40 (ie, former service members from the most recent military theaters) are less likely to enroll in HIE. This result is consistent with prior research demonstrating that younger people are less likely to value the importance of HIE.39 Our finding suggests the need for new, targeted approaches to reach this priority population. One approach may be to develop tailored messages through focus groups or other qualitative methods that address both the unique health care needs and the technology preferences of this younger age group. In another approach, partnerships could be created with the Returning Service Member Program or the Seamless Transition Integrated Care services within the medical center, which specialize in meeting the range of clinical, mental health, and social support needs of younger veterans. Overall, enrollment data can facilitate identification of priority populations to ensure that health systems develop appropriately targeted outreach programs. Outside the VHA, health systems may wish to target populations like the homeless, those who frequently use emergency or urgent care services, or those who may be at risk for hospital readmission.
Using enrollment to improve determination of HIE success
Characteristics associated with enrollment in VLER Health, including being female and having medical complexity, offer new insights into how an HIE initiative might define its success. HIE initiatives have long struggled to achieve value,40 and many early efforts to demonstrate success involved enrolling as large a proportion of the population as possible, regardless of whether that population was defined geographically or by a specific health plan. More targeted strategies may help HIEs achieve greater value by focusing enrollment on specific populations of patients.
A study by Schoen et al.1 suggests that medically complex patients have the greatest need for care coordination. Therefore, even if an HIE does not enroll all patients in a community but focuses instead on care coordination for medically complex patients, that can arguably be viewed as a success, because it achieved a SMART (specific, measurable, achievable, results-focused, and time-bound) goal. Likewise, women are the fastest growing segment among new veterans.41 Over the past 2 decades, the VHA has implemented numerous initiatives designed to improve access and quality of care for female veterans. We speculate that women’s disproportionately high rates of data- sharing authorization might relate to their higher use of non-VA medical providers while they simultaneously seek VA health services. Greater enrollment of medically complex and female patients, in the VHA context, could therefore be viewed as a mark of success for VLER Health, given the unique needs of these priority populations.
Future directions
The VHA continues to implement HIE nationwide with community-based initiatives, such as Maryland’s Chesapeake Regional Information System for our Patients (CRISP),42 as well as novel private partners such as Walgreens. Comparisons of the HIE experience in different settings will be informative. As VA and community HIE efforts continue to expand and new approaches to enrollment are adopted, future research will be necessary to measure progress across the metrics of patient enrollment, provider usage, and population health.
Limitations
Our study had 3 primary limitations. First, the study was conducted using data from a single medical center within the VHA. This focus may limit the generalizability of the results in describing VLER Health enrollees. Nonetheless, our findings provide a detailed examination of HIE enrollment from an early adopter (medical center) that accounts for a sizable number of enrollees. Enrollment numbers at RLR have generally been larger than at other pilot sites within the VHA.15 Second, some of the covariates used in the model had a large number of missing or unknown values. Race data were missing for 25% of the cohort, and insurance data were missing for 40%. Therefore, findings regarding the lack of racial disparities in enrollment are tentative, and the influence of insurance status is exploratory. Of note, these data are often missing in EHR systems and administrative datasets.43,44 Third, our study lacked a well-defined denominator for the number of veterans approached for enrollment. Since mass mailings were not used, it is difficult to say what proportion of the 57 000 veterans were invited to provide authorization for VLER Health. Such a denominator would make the assessment of enrollment success more straightforward, although direct mail strategies have their own set of limitations. In addition, our study did not include data about environmental factors, such as home and work environment, or personal health behavior choices, such as smoking and alcohol consumption. As recommended by the National Academy of Medicine, future research should study the impact of social and behavioral determinants upon HIE enrollment and utilization.45
CONCLUSION
An HIE initiative to exchange data with non-VHA providers at a Midwestern VHA medical center was more likely to enroll patients who were female, were more medically complex, had higher health care utilization, or lived in urban areas. In the future, HIE efforts could be tailored to improve reach to healthier, younger populations of veterans, as well as veterans in rural communities. This assessment of HIE enrollees has lessons not only for the VHA, but also for HIE initiatives in other health systems. Future work is needed to identify efficient practices for obtaining consent for HIE and to define more fully the assessment of implementation.
ACKNOWLEDGEMENTS
The authors thank Jason Larson of the Richard L. Roudebush VA Medical Center for his help in gathering the data and facilitating analysis as project manager of the Evaluation of VLER Indiana Health Information Exchange Demonstration Project. We further acknowledge the data management expertise and effort of Joe Kesterson of the Regenstrief Institute in extracting non-VA data and integrating them with VA data to facilitate analysis, and we acknowledge the assistance of Drs Joshua Vest and Saurabh Rahurkar who copy edited the manuscript prior to publication. Dr Weiner is chief of health services research and development at the Richard L. Roudebush Veterans Affairs Medical Center.
CONTRIBUTORS
B.E.D. and D.A.H. designed and guided the development of the article. B.E.D. drafted the article, created the figures, and managed revisions to the article. S.O. and S.P. provided critical statistical support for the analysis; S.O. prepared the tables for publication. L.J.M. and M.B.R. provided support for data access and management. D.D.F. and A.J.Z. provided input on data analysis and interpretation of results. All authors provided critical review and edits to the manuscript prior to submission.
FUNDING
This project was supported by the US Department of Veterans Affairs (VA) Health Services Research and Development (HSR&D) Service, grant number IIR 11-058, Evaluation of VLER Indiana Health Information Exchange Demonstration Project. This work was further supported by VA HSR&D grant number CIN 13-416. The content is solely the responsibility of the authors and does not necessarily represent the official views of the US Department of Veterans Affairs or the US government.
COMPETING INTERESTS
Several authors (B.E.D., L.J.M., D.D.F., M.W., D.A.H.) are employed as research scientists within the HSR&D service at the Richard L. Roudebush Veterans Affairs Medical Center in Indianapolis, Indiana, or the Edward Hines Jr VA Hospital in Chicago, Illinois. As such, they receive at least a portion of their annual salary from the US Department of Veterans Affairs.
REFERENCES
- 1. Schoen C, Osborn R, Squires D, Doty M, Pierson R, Applebaum S. New 2011 survey of patients with complex care needs in eleven countries finds that care is often poorly coordinated. Health Affairs (Project Hope). 2011;30(12):2437–2448. [DOI] [PubMed] [Google Scholar]
- 2. Zuchowski JL, Rose DE, Hamilton AB, et al. Challenges in referral communication between VHA primary care and specialty care. J Gen Intern Med. 2015;30(3):305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gaglioti A, Cozad A, Wittrock S, et al. Non-VA primary care providers' perspectives on comanagement for rural veterans. Military Med. 2014;179(11):1236–1243. [DOI] [PubMed] [Google Scholar]
- 4. Overhage JM. Health information exchange: ‘lex parsimoniae.' Health Affairs (Project Hope). 2007;26(5):w595–w597. [DOI] [PubMed] [Google Scholar]
- 5. Dixon BE, Vreeman DJ, Grannis SJ. The long road to semantic interoperability in support of public health: experiences from two states. J Biomed Inform. 2014;49:3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chang KC, Overhage JM, Hui SL, Were MC. Enhancing laboratory report contents to improve outpatient management of test results. J Am Med Inform Assoc. 2010;17(1):99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Johnson KB, Unertl KM, Chen Q, et al. Health information exchange usage in emergency departments and clinics: the who, what, and why. J Am Med Inform Assoc. 2011;18(5):690–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Furukawa MF, King J, Patel V, Hsiao CJ, Adler-Milstein J, Jha AK. Despite substantial progress in EHR adoption, health information exchange and patient engagement remain low in office settings. Health Affairs (Project Hope). 2014;33(9):1672–1679. [DOI] [PubMed] [Google Scholar]
- 9. Adler-Milstein J, Bates DW, Jha AK. Operational health information exchanges show substantial growth, but long-term funding remains a concern. Health Affairs (Project Hope). 2013;32(8):1486–1492. [DOI] [PubMed] [Google Scholar]
- 10. Rahurkar S, Vest JR, Menachemi N. Despite the spread of health information exchange, there is little evidence of its impact on cost, use, and quality of care. Health Affairs (Project Hope). 2015;34(3):477–483. [DOI] [PubMed] [Google Scholar]
- 11. Rudin RS, Motala A, Goldzweig CL, Shekelle PG. Usage and effect of health information exchange: a systematic review. Ann Intern Med. 2014;161(11):803–811. [DOI] [PubMed] [Google Scholar]
- 12. Furukawa MF, Patel V, Charles D, Swain M, Mostashari F. Hospital electronic health information exchange grew substantially in 2008-12. Health Affairs (Project Hope). 2013;32(8):1346–1354. [DOI] [PubMed] [Google Scholar]
- 13. Byrne CM, Mercincavage LM, Bouhaddou O, et al. The Department of Veterans Affairs' (VA) implementation of the Virtual Lifetime Electronic Record (VLER): findings and lessons learned from Health Information Exchange at 12 sites. Int J Med Inform. 2014;83(8):537–547. [DOI] [PubMed] [Google Scholar]
- 14. Bouhaddou O, Bennett J, Teal J, et al. Toward a virtual lifetime electronic record: the department of veterans affairs experience with the nationwide health information network. AMIA Annu Symp Proc. 2012; 2012:51–60. [PMC free article] [PubMed] [Google Scholar]
- 15. Bouhaddou O, Bennett J, Cromwell T, et al. The Department of Veterans Affairs, Department of Defense, and Kaiser Permanente Nationwide Health Information Network exchange in San Diego: patient selection, consent, and identity matching. AMIA Annu Symp Proc. 2011;2011: 135–143. [PMC free article] [PubMed] [Google Scholar]
- 16. VLER Health. December 8, 2015 [cited December 28, 2015]. http://www.va.gov/VLER/vler-health-exchange.asp. Accessed April 26, 2016. [Google Scholar]
- 17. Form No. 10-0485. Request for and authorization to release protected health information to eHealth Exchange 2015. http://www.va.gov/vaforms/form_detail.asp?formno=0485. Accessed December 28, 2015. [Google Scholar]
- 18. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 19. Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33 (3 Pt 1):571–596. [PMC free article] [PubMed] [Google Scholar]
- 20. Armstrong K, McMurphy S, Dean LT, et al. Differences in the patterns of health care system distrust between blacks and whites. J Gen Intern Med. 2008;23(6):827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dhopeshwarkar RV, Kern LM, O'Donnell HC, Edwards AM, Kaushal R. Health care consumers' preferences around health information exchange. Ann Fam Med. 2012;10(5):428–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wennberg JE, O'Connor AM, Collins ED, Weinstein JN. Extending the P4P agenda, part 1: how Medicare can improve patient decision making and reduce unnecessary care. Health Affairs (Project Hope). 2007;26(6): 1564–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Biondich PG, Grannis SJ. The Indiana network for patient care: an integrated clinical information system informed by over thirty years of experience. J Public Health Manag Pract. 2004;Suppl:S81–S86. [PubMed] [Google Scholar]
- 24. Zafar A, Dixon BE. Pulling back the covers: technical lessons of a real-world health information exchange. Stud Health Technol Inform. 2007;129(Pt 1): 488–492. [PubMed] [Google Scholar]
- 25. Barnes M. Lessons learned from the implementation of clinical messaging systems. AMIA Annu Symp Proc. 2007:36–40. [PMC free article] [PubMed] [Google Scholar]
- 26. Indiana Health Information Exchange. ADT Alerts for Reducing ED Admissions: A Case Study. 2013. http://www.ihie.org/aco-services. Accessed May 15, 2015. [Google Scholar]
- 27. Grannis SJ, Overhage JM, Hui S, McDonald CJ. Analysis of a probabilistic record linkage technique without human review. AMIA Annu Symp Proc. 2003:259–263. [PMC free article] [PubMed] [Google Scholar]
- 28. French DD, Bradham DD, Campbell RR, et al. Factors associated with program utilization of radiation therapy treatment for VHA and Medicare dually enrolled patients. J Commun Health. 2012;37(4):882–887. [DOI] [PubMed] [Google Scholar]
- 29. Nagelkerke NJD. A note on a general definition of the coefficient of determination. Biometrika. 1991;78(3):691–692. [Google Scholar]
- 30. Nazi KM, Hogan TP, Woods SS, Simon SR, Ralston JD. Consumer health informatics: engaging and empowering patients and families. In: Finnell JT, Dixon BE, eds. Clinical Informatics Study Guide: Text and Review. 1st ed.Zurich: Springer International Publishing; 2016: 459–500. [Google Scholar]
- 31. Zulman DM, Nazi KM, Turvey CL, Wagner TH, Woods SS, An LC. Patient interest in sharing personal health record information: a web-based survey. Ann Intern Med. 2011;155(12):805–810. [DOI] [PubMed] [Google Scholar]
- 32. Veterans Access, Choice, and Accountability Act of 2014. Pub. L. No. 113-146, 128 Stat. 1754 (Aug. 7, 2014). [Google Scholar]
- 33. Dixon BE, Haggstrom DA, Weiner M. Implications for informatics given expanding access to care for veterans and other populations. J Am Med Inform Assoc. 2015;22(4): 917–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Caine K, Hanania R. Patients want granular privacy control over health information in electronic medical records. J Am Med Inform Assoc. 2013;20(1): 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tripathi M, Delano D, Lund B, Rudolph L. Engaging patients for health information exchange. Health Affairs (Project Hope). 2009;28(2):435–443. [DOI] [PubMed] [Google Scholar]
- 36. Yaraghi N, Sharman R, Gopal R, Singh R, Ramesh R. Drivers of information disclosure on health information exchange platforms: insights from an exploratory empirical study. J Am Med Inform Assoc. 2015;22(6):1183–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ramos SR, Bakken S. Qualitative study of patient consent for health information exchange in an HIV clinic. Stud Health Technol Inform. 2014;201: 418–424. [PubMed] [Google Scholar]
- 38. Campion TR, Jr, Edwards AM, Johnson SB, Kaushal R. Health information exchange system usage patterns in three communities: practice sites, users, patients, and data. Int J Med Inform. 2013;82(9):810–820. [DOI] [PubMed] [Google Scholar]
- 39. Wen KY, Kreps G, Zhu F, Miller S. Consumers' perceptions about and use of the internet for personal health records and health information exchange: analysis of the 2007 Health Information National Trends Survey. J Med Internet Res. 2010;12(4):e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kansky JP. Managing the business of health information exchange: towards sustainability. In: Dixon BE, ed. Health Information Exchange: Navigating and Managing a Network of Health Information Systems. London: Academic Press; 2016:77–90. [Google Scholar]
- 41. Yano EM, Haskell S, Hayes P. Delivery of gender-sensitive comprehensive primary care to women veterans: implications for VA Patient Aligned Care Teams. J Gen Intern Med. 2014;29 (Suppl 2):S703–S707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kharrazi H, Horrocks D, Weiner J. Use of HIEs for value-based care delivery: a case study of Maryland's HIE. In: Dixon BE, ed. Health Information Exchange: Navigating and Managing a Network of Health Information Systems. 1st ed.London: Academic Press; 2016:313–332. [Google Scholar]
- 43. Chan KS, Fowles JB, Weiner JP. Review: electronic health records and the reliability and validity of quality measures: a review of the literature. Med Care Res Rev. 2010;67(5):503–527. [DOI] [PubMed] [Google Scholar]
- 44. Dixon BE, Siegel JA, Oemig TV, Grannis SJ. Electronic health information quality challenges and interventions to improve public health surveillance data and practice. Public Health Rep. 2013;128(6):546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hripcsak G, Forrest CB, Brennan PF, Stead WW. Informatics to support the IOM Social and Behavioral Domains and Measures. J Am Med Inform Assoc. 2015; 22(4):921–924. [DOI] [PMC free article] [PubMed] [Google Scholar]