Abstract
Objective: Assess parent use and perceptions of an inpatient portal application on a tablet computer that provides information about a child’s hospital stay.
Methods: This cross-sectional study was conducted with parents of children hospitalized on a medical/surgical unit at a tertiary children’s hospital. From December 2014 to June 2015, parents were provisioned a tablet portal application to use throughout the hospitalization. The portal includes real-time hospital vitals, medications, schedules, lab results, education, health care team pictures/roles, and request and messaging functionalities. Portal use information was gathered from tablet metadata. Parents completed discharge surveys on portal satisfaction, use, and impact on their information needs, engagement, communication, error detection, and care safety and quality. Data were analyzed using descriptive statistics and qualitative content analysis.
Results: Over 6 months, 296 parents used the portal, sending 176 requests and 36 messages. No tablets were lost or damaged. The most used and liked features included vitals, medication list, health care team information, and schedules. Overall, parent survey respondents (90) were satisfied with the portal (90%), reporting that it was easy to use (98%), improved care (94%), and gave them access to information that helped them monitor, understand, make decisions, and care for their child. Many parents reported that portal use improved health care team communication (60%). Most perceived that portal use reduced errors in care (89%), with 8% finding errors in their child’s medication list.
Conclusions: Overall, parents were satisfied with the inpatient portal. Portals may engage parents in hospital care, facilitate parent recognition of medication errors, and improve perceptions of safety and quality.
Keywords: patient portal, patient engagement, hospital medicine, pediatrics, family-centered care
INTRODUCTION
Patient-centered care, in which the patient is an active participant in managing his or her health, improves patient and health care team satisfaction1,2 and health outcomes.3–5 Patient portals, electronic personal health records tethered to electronic health records (EHRs), are endorsed as a way to engage patients in their care.6 Portals are intended to support engagement by providing patients and families access to their health care information and facilitating communication with the health care team.6 Portal use has also been suggested as a mechanism for patients and/or families to identify medical errors, thus having the potential to improve the safety and quality of care.6,7 Specifically, portals allow patients to review their prescribed medication list and identify and report discrepancies to their health care team, and thus potentially prevent adverse drug events.8
Access to outpatient patient portals has increased dramatically, driven in large part by meaningful use requirements from the Centers for Medicare and Medicaid Services EHR incentives program.9 The evidence of the impact of these portals on promoting patient-centered care and improved outcomes in adult patients is growing.10–14 In pediatrics, portal research is in its infancy, primarily describing use by families of children with chronic diseases15–20 or by a cohort of families of healthy children.21 While research has focused on outpatient portal use, recent literature suggests that patient portals may be just as, if not more, useful for engaging patients and their families in the inpatient setting.22–26 Before widespread adoption can be promoted, research is needed to understand how these portals are used and whether they provide value to hospitalized patients and/or their proxies.6
In this study, we evaluated an inpatient portal application on a tablet computer offered to parents of hospitalized children. Tethered to the inpatient EHR, this portal application was designed to engage families in hospital care through 2 main functionalities: (1) allowing access to real-time information (eg, vitals, medication lists, test results, daily schedule, education) and (2) providing a mechanism to recognize and communicate with their child’s inpatient health care team (eg, photographs, messaging). We utilized tablet metadata and parent user surveys to assess portal use and parent experiences and perceptions of the impact of portal use on inpatient care (parent information needs, communication, error detection, and care safety and quality).
METHODS
Study design, setting, and participants
This cross-sectional study was conducted in a 24-bed general medical/surgical unit within an 81-bed tertiary care children’s hospital in Wisconsin. This unit includes patients younger than 18 years old admitted to 1 of these pediatric services: pediatric hospitalist, cardiology, pulmonology, gastroenterology, neurology, surgery, trauma, orthopedics, transplant, or rehabilitation. This institution uses the Epic Systems EHR enterprise-wide. The EHR was implemented in the ambulatory setting in 2004 and in the inpatient setting in 2008. The outpatient portal (MyChart, Epic Systems) went live in 2009. The inpatient portal (MyChart Bedside, Epic Systems, see full description below) was implemented in December 2014.
Over 6 months, from December 15, 2014, to June 14, 2015, we enrolled a convenience sample of English-speaking parents or legal guardians of children younger than 12 years old admitted or transferred to the unit. Parents who were unavailable during tablet provisioning (7 am to 7 pm), who were identified by staff with concerns regarding a sensitive diagnosis (eg, nonaccidental trauma), or whose children had a short length of stay (eg, anticipated discharge within 8 hours of tablet provisioning) were excluded. Parents of children 12 years of age and older were not included due to legal differences in access to adolescent health information.
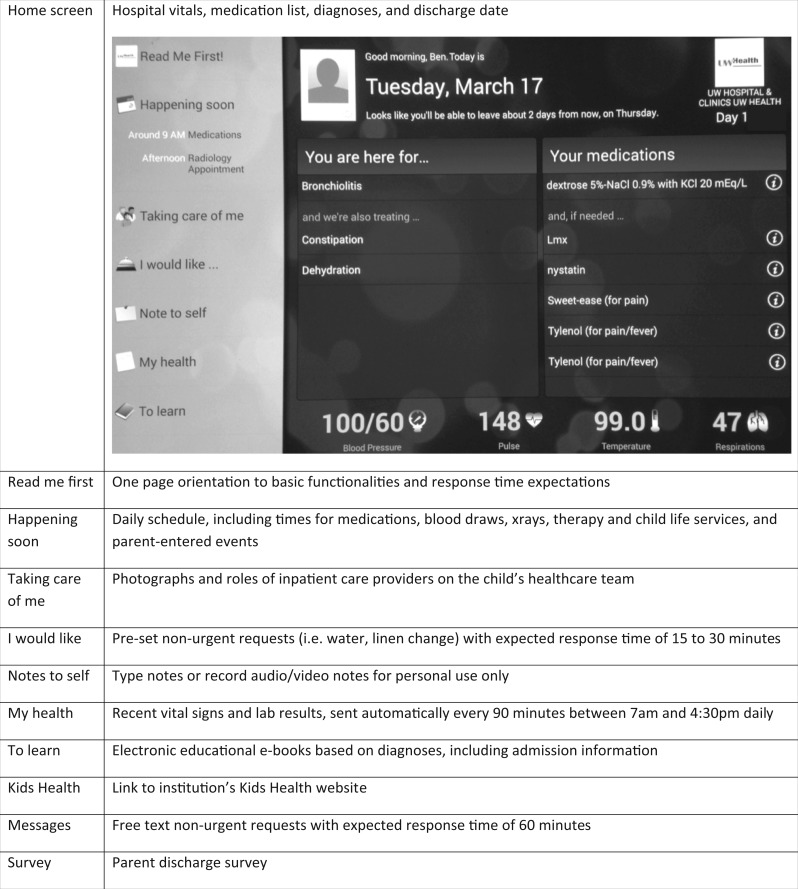
The inpatient portal
MyChart Bedside (Epic Systems, Madison, WI, Figure 1, subsequently referred to as the portal) is a patient portal application tethered to the inpatient EHR provided on a tablet computer that allows patients and/or their families to access real-time information specific to their hospital stay. Figure 1 describes the basic functionalities of the portal along with our institution-specific customizations, including expectations regarding response times, frequency of lab result release, user’s guide, and electronic versions of educational content previously developed within the institution. At our institution, these tablets are enabled for use only within the hospital network and do not include access to the Internet or other applications. During the month prior to portal go-live, the inpatient health care team, consisting of nurses, pediatric resident and attending physicians, nurse practitioners, and ancillary staff (unit coordinators, physical and occupational therapists, etc.), participated in didactic and hands-on training during departmental meetings. The training protocol included a standardized 15-minute didactic overview of how to identify eligible parents and provision the tablet, a description of all portal functionalities, expectations for response time to parent requests (15–30 minutes) and messages (60 minutes), and who to call with technical issues. This was followed by hands-on training lasting 15–25 minutes (depending on the number of participants), which allowed time for the health care team to ask questions and practice provisioning and using the portal.
Figure 1.
Home screen of the inpatient portal and descriptions of portal functionalities, with italicized text representing institutional-specific modifications (MyChart Bedside, screenshot, © 2016 Epic Systems Corp. Used with permission.)
Data collection procedure
Unit coordinators identified eligible parents through EHR prompts. Using a uniform EHR work list, a portal icon is displayed if a patient is younger than 12 years old, English is his or her preferred language, and he or she has an assigned bed on the unit. Of these parents, those who were unavailable (absent or sleeping), had staff concerned about sensitive diagnoses, and/or whose children had an anticipated short length of stay were excluded. Available parents were then offered the portal application on a hospital-provided electronic tablet computer between 7 am and 7 pm, 7 days a week, and were allowed to keep it throughout their child’s stay. Upon provisioning, parents were asked to complete a voluntary, anonymous survey on the tablet prior to their child’s discharge. On discharge, tablets were collected, cleared of data, and reprovisioned. Parent participant consent was implied upon survey completion and data were de-identified. The Institutional Review Board at the University of Wisconsin-Madison deemed this study quality improvement and exempt from review.
Data collection instruments
Tablet metadata. We created tablet reports using Clarity (www.epic.com) to assess actual parent use of the portal application. Data included parent access to functionalities, number of notes (text, audio, and video), and number and content of requests and messages to the health care team.
Parent survey. We constructed an electronic survey administered within the portal application using an online survey tool (www.qualtrics.com). We selected survey items from the published literature, which were adapted and piloted by our multidisciplinary portal implementation team (Centers for Disease Control and Prevention National Health Interview Study, http://www.cdc.gov/nchs/nhis.htm).27–30 This team included parents, health care team members, hospital administrators, information services representatives, health services researchers, and human factors and systems engineers. We included items to assess characteristics of the parent (relationship to child, age, education, Internet use, and health-related Internet activities) and the child (overall health, number of hospitalizations including birth and current hospitalization, and reason for hospitalization). Reasons for hospitalization included a list of hospital problems (eg, breathing problem) and a free-text “other” option. When multiple responses were recorded, all responses were analyzed. We included items assessing parent perceptions of the portal (ease of use, usefulness, satisfaction, and impact of portal use on engagement in the child’s care, communication with the child’s nurse/doctor, error reduction, and care quality). Response options for parent perception questions were on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). We also included an item listing previously described challenges to portal use with a free-text “other” option.
We used questions specifically created for this study to assess parents’ perceptions of their use of the portal (“How often did you use [the portal] during this hospital stay?”), the impact of portal use on the parents’ information needs (“What impact does [the portal] have on the amount of questions you have for your child’s doctors and nurses in the hospital?”), and detection of medication errors (“Did you find an error(s) in your child’s medication list when you used [the portal]?” Yes/No). The survey also included 3 open-ended questions: “What three things do you like most about [the portal],” “What do you dislike about [the portal],” and “What other [portal] features or tablet applications (apps) would be useful to you or your child?” The survey can be found at http://cqpi.wisc.edu/documents/MyChart_Bedside_Survey_Parents.pdf.
Data analysis
Data from parent surveys were downloaded into SPSS (version 20). We used percentages to describe our variables. In all 5-point Likert response questions, responses were combined to create 3 categories: (1) Disagree (combining strongly disagree and disagree), (2) Neither Agree nor Disagree, and (3) Agree (combining strongly agree and agree). We used chi-square tests to assess for differences between groups for nominal data, Somers' delta to examine differences for ordinal data, and the Mann-Whitney U test to examine differences between groups for nominal and ordinal data.
Qualitative content analysis31 of parent messages and survey comments on likes, dislikes, and suggestions for portal improvement was conducted by 2 independent investigators using Microsoft Excel (2011). One investigator read all the data while making notes, looking for distinctive key words and phrases, the second investigator reviewed the initial notes, and both created a preliminary node structure consisting of themes. Both researchers then coded all data separately, and inconsistencies were reconciled through discussion. Comments within nodes were quantified by aggregating the number of comments at each node.
RESULTS
Inpatient patient portal use
Over 6 months, 329 parents were offered the portal application on a hospital-provisioned tablet and 296 accepted it (90%). Out of 24 available tablets, none were stolen, lost, or damaged. We had 10 calls to our help desk and 17 reports filed for portal technical support. Examples included difficulty logging in outside of the hospital network and problems loading information. Information on parent use of the portal obtained from table metadata is demonstrated in Table 1. According to tablet reports, a majority of parents accessed all functionalities. The most frequently accessed functionalities per parent user were the homepage (vitals and the medication list), “Taking care of me” (pictures and roles of the health care team), “Happening Soon” (daily schedule), and “My Health” (lab results).
Table 1.
Parent use of the inpatient patient portal (n = 296)
| Portal functionality | Number of parents who accessed functionality, n (%)a | Number of times functionality was accessed, n | Number of times functionality was accessed per parent user, n |
|---|---|---|---|
| Homepage | 296 (100) | 4891 | 16.5 |
| Happening soon | 223 (75.3) | 2127 | 9.5 |
| Taking care of me | 255 (86.1) | 4270 | 16.8 |
| I would likeb | 225 (76.0) | 835 | 3.7 |
| Request sent | 85 (28.7) | 176 | 2.1 |
| Notes to selfb | 190 (64.1) | 540 | 2.8 |
| Note created | 23 (7.7) | 41 | 0.1 |
| Video created | 3 (1.0) | 6 | 2.0 |
| Audio created | 2 (0.7) | 2 | 1.0 |
| My health | 226 (76.3) | 1290 | 5.7 |
| To learn | 181 (61.1) | 492 | 2.7 |
| Messagesb | 155 (52.4) | 430 | 2.8 |
| Message sent | 16 (5.4) | 57 | 3.6 |
aPercentage of parents who accessed the functionality out of total who were provisioned the portal (n = 296). bThese represent parent access by clicking on the tab for each functionality. The numbers of actual notes, audio and video recordings created, and requests and messages sent are listed beneath each relevant functionality.
Out of 296 parents, 85 (28.7%) made 176 requests through the portal (1–13 requests per parent user). The most common requests included personal care items, child life volunteer, water, movie list, and linen change. Sixteen parents (5.4%) sent a total of 36 messages to their children’s health care teams (1–14 per parent user). Parent messages included questions regarding care (eg, “I would like to know reason why [medication was stopped]”) and updates on the patient’s condition and whereabouts (eg, “X-ray was just done, going to play room”). The remaining messages included requests (eg, “We would like to have a letter for school stating what she can and can’t do”) and thank you notes to the health care team (eg, “Thank you all for your help”). Health care team members on the unit sent a total of 21 messages in return. These included acknowledgement of parent messages, answers to parent questions, or referrals to contact the doctor. Only 25 parents (8.4%) recorded information within the “Notes to self” functionality. These included 2 audio recordings by 2 parents, 6 video recordings by 3 parents, and 41 text notes by 23 parents.
Parent and child characteristics
Discharge surveys were completed and submitted by 90 parents. Parent respondent characteristics are shown in Table 2. Respondents were predominantly mothers (76%) who were 25–44 years old (76%) with varying educational levels. Overall, parent respondents were frequent Internet users, with 82% using the Internet or computer applications daily. Most parents reported using the Internet for health-related activities. Over half (59%) had used an outpatient portal before their child’s current hospitalization. Forty percent of parents reported that their child was generally in very good to excellent health, with over 30% hospitalized 2 or fewer times (including birth and current hospital stay). Per parent report, children were hospitalized on this general medical/surgical unit for various medical conditions, such as vomiting and diarrhea, pneumonia, febrile illness, headache, urinary tract infection, or trauma after a motor vehicle accident (Table 2).
Table 2.
Parent and child characteristics, n = 90a
| Parent characteristic | n (%) |
|---|---|
| Relationship to child | |
| Mother | 68 (76) |
| Missing | 6 (7) |
| Age, years | |
| Under 24 | 11 (12) |
| 25–34 | 34 (38) |
| 35 and older | 39 (44) |
| Missing | 6 (7) |
| Education | |
| High school or less | 14 (15) |
| Some college | 35 (39) |
| Bachelor’s degree or more | 35 (39) |
| Missing | 6 (7) |
| Internet use | |
| Daily | 74 (82) |
| Several times a week | 6 (7) |
| Once a week or less | 2 (2) |
| Missing | 8 (9) |
| Health-related Internet activity prior to current hospitalization | |
| Look up health information | 69 (77) |
| Use outpatient portal | 53 (59) |
| Look up test results | 53 (59) |
| Communicate with provider | 50 (56) |
| Review medications | 44 (49) |
| Refill a prescription | 31 (34) |
| Schedule an appointment | 29 (32) |
| Child characteristic | n (%) |
| General health | |
| Very good to excellent | 36 (40) |
| Missing | 9 (10) |
| Number of hospitalizationsb | |
| 2 or less | 31 (34) |
| 3–5 | 23 (26) |
| 6 or more | 22 (24) |
| Missing | 14 (16) |
| Hospitalization problem | |
| Stomach or intestinal problem | 27 (30) |
| Breathing problem | 19 (21) |
| Fever | 16 (18) |
| Seizure and/or headache | 6 (7) |
| Hospitalization problem | |
| Kidney or urinary tract infection | 4 (4) |
| Otherc | 37 (41) |
| Missing | 7 (8) |
aTotals may exceed 100% due to rounding or parent ability to choose multiple items in health-related Internet activities and hospitalization problem. bHospitalizations include birth and current hospitalization, as adapted from a standard questionnaire.30cFor instance, transplant or other surgery, metabolic disorder, or burn.
Parent perceptions
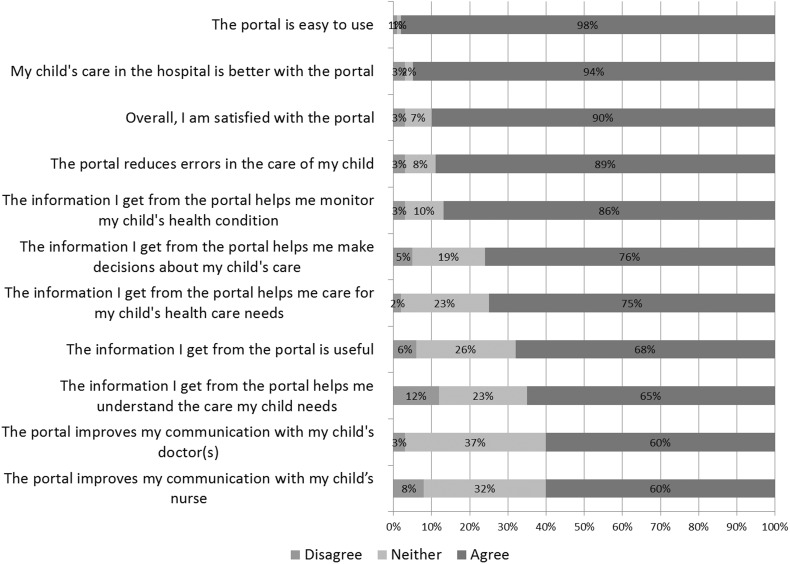
Out of 90 respondents, 2 parents (2%) reported never using the portal, 7 (8%) used it once, 44 (50%) 2–5 times, 13 (15%) 6–10 times, and 22 (25%) used it more than 10 times during their child’s hospitalization. Results in Figure 2 show that most respondents were generally very positive about the portal. They reported that it was easy to use (98%), their child’s care was better with it (94%), and they were satisfied with it overall (90%). Using the portal, 8% of parents reported finding errors in their child’s medication list, while 89% of all respondents thought the portal reduced errors in their child’s care. Most parents (51%) responded that the portal provided the information they needed, and therefore reduced the number of questions they had for doctors or nurses. Forty percent responded that the portal did not change the amount of questions they had, and 6% responded that the portal increased their number of questions. Parents were less positive about the impact of portal use on communication with the health care team, with 60% reporting that it improved communication with their child’s nurse or doctor.
Figure 2.
Parent perceptions of the inpatient portal, n = 87
Individual parent and child characteristics were associated with few differences in portal perceptions. Fathers, younger parents, and parents of children who were in poorer general health and had a history of more hospitalizations were more positive about the portal; however, differences were not statistically significant. Parents with lower levels of education were more satisfied with the portal than parents with higher education (Somers’ d = −0.195, P < .05). Parents who had not previously used an outpatient portal were more satisfied with the portal than parents who had used an outpatient portal (χ2 = 9.67, df = 4, P < .05). Although we did not distinguish the service (eg, hospitalist vs general surgery) of survey respondents, there were no differences in perceptions among parents of children with different health problems, with the exception of those hospitalized for fever. The parents of these children were more positive about the portal overall and specifically more likely to agree that the portal was useful (U = 373, P < .05), it helped them monitor their child’s health (U = 307.5, P < .01), and their child’s care was better with it (U = 343.5, P < .01).
Challenges using the portal reported by parents surveyed were rare, but included these: the information is not very useful (n = 7), staff did not respond to messages in a timely manner (n = 5), they were too busy to use it (n = 3), and they were not able to use it due to technical difficulties (n = 2). No parents reported that the portal was too hard to use, there was not enough technical support, they were concerned that they would lose or damage the tablet, or that staff were skeptical of the portal. When asked what 3 things they liked most about the portal, about two-thirds of the parents provided 1 or more responses (Table 3). When asked what they disliked, 37 parents provided 44 comments and 16 parents wrote “nothing” or “none” (Table 3). About half of respondents had suggestions for portal improvement (Table 4).
Table 3.
What parents liked and disliked about the inpatient patient portal
| Parent likes and dislikes | Number of responses | Example quote |
|---|---|---|
| Likes (n = 159 responses) | ||
| General information | 22 | “Love the fact that it kept me informed about my child's health” |
| Ease of use | 12 | “It's very easy to use” |
| Vitals | 22 | “Being able to monitor his vitals” |
| Medication list | 21 | “Knew what meds (and times) were administered to my child” |
| Taking care of me (staff pictures) | 24 | “Liked seeing who was going to take care of my child” |
| My Health (lab results) | 17 | “Quick access to test results” |
| I would like (requests) | 17 | “Can ask for things without using the call light” |
| Happening Soon (schedule) | 13 | “Seeing what the plan is going forward” |
| Communication with providers, including messaging | 11 | “I can message the team of doctors and they do get back to you very timely” |
| Dislikes (n = 60 responses) | ||
| Information not updated | 9 | “Not updating the profiles/pictures of who is taking care of my child” |
| Lack of educational resources | 8 | “It would have been handy to have an easier way to learn about tests my son would be getting done” |
| Technical problems | 7 | “It stopped recognizing me as a user for about 2 hours so I couldn't use it” |
| Missing useful EHR information | 5 | “I would have liked to have seen a tracking of her weight and height” |
| No link to outpatient portal | 5 | “It would be nice to have labs from recent clinic visits available to compare to new labs since my son had two urgent care visits related to this hospitalization” |
| Lack of family-/child-friendly content | 3 | “The dosages of the medications are all in mg. Most parents don't know how many mg a syrup or pill contains per unit, especially if the drug is new to them” |
| Other | 7 | “There aren't many options in the ‘I would like’ section” |
Table 4.
Parent suggestions for portal improvement, n = 47 responses
| Suggestions for portal improvement | Number of responses | Example quote |
|---|---|---|
| Games, movies, Internet | 15 | “I wish they had Internet or simple games to keep kids entertained.” |
| Access to more EHR information | 8 | “Weights,” “radiology results,” “more detailed med schedule,” “link to regular [outpatient] account” |
| More educational links and resources | 8 | “Link to diagnostic definitions” |
| Room service | 6 | “It would also be nice to have a meal menu or ordering service.” |
| Facility information | 5 | “A map of the unit with our location, the location of the lounge” |
| Other | 5 | “If it could work while I was at Ronald McDonald House… and that's where I am when I am not with her” |
DISCUSSION
To our knowledge, this is the first study to assess the use and perceptions of a tethered inpatient portal application for parents of hospitalized children. A majority of parent respondents in this convenience sample were very satisfied with the portal and reported that it improved their child’s hospital care. Most reported that it gave them access to the information they needed to help monitor, understand, make decisions, and care for their child. Portal use had less impact on facilitating communication, with 60% of parents reporting that it improved communication with their child’s nurse or doctor. The portal functionalities parents most liked and accessed were vitals, medication list, pictures and roles of the care team, and the child’s daily schedule. Almost 90% of parents perceived that portal use reduced errors in their child’s care, with 8% reporting finding errors in the hospital medication list. Overall, parents found the portal easy to use, there were relatively few technical issues, and no tablets were lost or damaged.
Patient portal literature shows mixed findings regarding patient and/or proxy user satisfaction and impact on patient activation and decision-making.32,33 One study provided parents of children with asthma with decision support through an outpatient portal, which was shown to improve shared decision-making in this population.20 In contrast, a recent study of hospitalized adults found no difference in patient activation with the use of a tablet computer with a patient portal application.26 In our study, parent respondents were satisfied with the inpatient portal overall. Most parents also reported that portal use improved their child's hospital care and helped them to monitor the child's health condition, and that the information they received helped them make care decisions (see Figure 2).
Another area of investigation is in the use of patient portals to facilitate patient and/or proxy communication with the health care team. Recent literature suggests that a minority of patients may actually use portals, and relatively few use them specifically to communicate with their care team. For example, Liedermann and colleagues34 examined the impact of outpatient portal secure messaging on patient, provider, and staff satisfaction. Although satisfaction was high overall, results of the study showed that less than 5% of patients had enrolled in secure messaging 1 year after implementation. Of these, nearly 50% sent only a single message in 6 months, 30% sent 2–3 messages, and about 20% sent 4 or more messages. Results of our inpatient portal evaluation show similar findings. Only 5.6% of parents used the portal to communicate via messaging with their child’s nurse or doctor, sending a total of 36 messages. Compared to other outcomes, parents were also less positive about the portal improving communication with the health care team. The asynchronous character of communicating through a portal does have certain advantages, but perhaps parents prefer face-to-face communication because it provides them with more context and also the opportunity to ask real-time follow-up questions.35 Additional interviews with parents may provide more information on why they like certain aspects of the inpatient portal, and why they are relatively less satisfied with the opportunity to communicate electronically with their child’s health care team.
Our data suggest that a patient portal tethered to an inpatient EHR may provide a mechanism for parents to identify medication errors during a child’s hospital stay. Medication-related morbidity and mortality make up a large part of patient safety events, with an estimated annual cost of $76 billion.36 Hospitalized children are especially vulnerable to medication errors,37 and recent literature highlights the potential role of parents in identifying and reporting errors in the hospital.38 By empowering parents to become active participants in their child’s inpatient care, portals have the potential to address medication safety issues. Some have suggested medication reconciliation modules allowing patients and/or their proxies to access medication information and identify discrepancies.6,7,39 Concerns could then be reported to a patient’s physician, who could take action and potentially prevent harm both in the hospital and in the transition to home. Further research is needed to characterize these medication errors that parents identified using the portal, whether parents reported these errors to the health care team, and any actions taken by the provider.
Parents had multiple suggestions for improvement that could inform future implementation and dissemination of hospital-based patient portals. Parents would like to see additional information included within the portal application, such as a link to the outpatient portal, radiology results, and more explanations of diagnoses, tests, and results (eg, reference ranges, access to the Internet so they can find information they need). Some functionalities requested were specific to the care of a hospitalized child, including tracking of weight, height, and head circumference, and providing child-friendly education. Multiple respondents requested that information be updated more quickly (eg, lab results in real time instead of every 90 minutes, updated care team information during care transitions). In general, parents would like the tablet to include more functionality outside of the portal application, such as games and movies for children, Internet access, facility information, room service, etc. Our hospital-provisioned tablets did not function outside the building; however, parents expressed interest in being able to take the application with them so they could monitor their child from outside the facility. This may be particularly relevant for children who have prolonged hospital stays and also highlights the possibility of a bring-your-own-device model. Finally, one parent proposed using the portal application to provide real-time hospital and health care team feedback.
This study has several limitations. Although we provisioned tablets to parents across multiple medical and surgical services, our results represent portal use and perceptions of parents of children hospitalized at a single Midwest tertiary children’s hospital. We also used a portal that was designed for only English-speaking users. Additional studies need to be conducted to examine whether our results are replicable in other settings and populations. We also only have data on those parents who accepted the tablet and responded to the survey. The parent and child characteristics of our survey respondents, however, are similar to those in a different study that took place in the same hospital.40 It is possible that our study selectively enrolled parents with characteristics that allowed them to be available at the bedside to accept the portal and complete the survey, and these characteristics influenced their portal experiences. The survey was programmed within the portal application and parents had to scroll down completely to access it. Nurses were asked to refer to the survey on the tablet on admission. In practice, this did not always happen, and many parents likely forgot to complete it by the time their child was ready for discharge. Interviews with parents who adopted and those who refused the portal may more comprehensively identify more or different challenges and perceptions of the portal. Our surveys were anonymous and not linked to EHR or tablet use data. Therefore, we could not fully evaluate the association between survey responses, such as parent characteristics and perceptions, and actual use or clinical patient profiles within the EHR. However, use data obtained from the EHR are of limited value. These data can indicate what parts of the portal parents visited most often, but do not show what they actually did on that page. Nevertheless, in a follow-up study, more attention should be given to a comparison of users and nonusers of the inpatient portal and of respondents and nonrespondents. Ideally, the user and respondent characteristics could be linked to EHR and use data. Finally, this study did not describe the health care team’s perceptions of the portal, which is a potential direction for future research.
In conclusion, this study suggests that patient portals may be a feasible and effective way to engage parents in hospital care. According to parent respondents in our study, the information provided in a portal improves a child's care in the hospital and helps parents monitor their child's health condition, and the information parents receive from the portal helps them make decisions about their child's care. Finally, the portal may facilitate parent recognition of medication errors and improve perceptions of hospital safety, quality, and patient and/or family satisfaction.
ACKNOWLEDGEMENTS
We would like to thank the parent portal users for their valuable insight and the portal implementation and steering committees for their feedback and support.
Contributors
M.M.K. conceived and designed the study, obtained funding, participated in data analysis and interpretation, drafted and revised the manuscript, and approved the final version for submission. P.H. assisted with study design, oversaw all data analyses, made critical manuscript revisions, and approved the final version for submission. S.D. assisted with study conception and design and data interpretation, made critical manuscript revisions, and approved the final version for submission. All authors take responsibility for the integrity of the data and accuracy of data analysis.
Funding
This work was supported by a Department of Pediatrics research and development grant at the University of Wisconsin School of Medicine and Public Health.
Competing interests
The authors have no competing interests to declare.
REFERENCES
- 1. Wanzer MB, Booth-Butterfield M, Gruber K. Perceptions of health care providers' communication: relationships between patient-centered communication and satisfaction. Health Commun. 2004;16(3):363–383. [DOI] [PubMed] [Google Scholar]
- 2. Wolf DM, Lehman L, Quinlin R, Zullo T, Hoffman L. Effect of patient-centered care on patient satisfaction and quality of care. J Nursing Care Qual. 2008;23(4):316–321. [DOI] [PubMed] [Google Scholar]
- 3. Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 4. Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323(7318):908–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Maeng DD, Graf TR, Davis DE, Tomcavage J, Bloom FJ., Jr Can a patient-centered medical home lead to better patient outcomes? The quality implications of Geisinger's ProvenHealth Navigator. Am J Med Qual. 2012;27(3):210–216. [DOI] [PubMed] [Google Scholar]
- 6. Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schnipper JL, Gandhi TK, Wald JS, et al. Design and implementation of a web-based patient portal linked to an electronic health record designed to improve medication safety: the Patient Gateway medications module. Inform Primary Care. 2008;16(2):147–155. [DOI] [PubMed] [Google Scholar]
- 8. Agrawal A. Medication errors: prevention using information technology systems. Brit J Clin Pharmacol. 2009;67(6):681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. [DOI] [PubMed] [Google Scholar]
- 10. Ammenwerth E, Schnell-Inderst P, Hoerbst A. The impact of electronic patient portals on patient care: a systematic review of controlled trials. J Med Internet Res. 2012;14(6):e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159(10):677–687. [DOI] [PubMed] [Google Scholar]
- 12. Davis Giardina T, Menon S, Parrish DE, Sittig DF, Singh H. Patient access to medical records and healthcare outcomes: a systematic review. J Am Med Inform Assoc. 2014; 21(4):737–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kalra D, Fernando B. A review of the empirical evidence of the healthcare benefits of personal health records. Yearbook Med Inform. 2013;8(1):93–102. [PubMed] [Google Scholar]
- 14. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17(2):e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Britto MT, Jimison HB, Munafo JK, Wissman J, Rogers ML, Hersh W. Usability testing finds problems for novice users of pediatric portals. J Am Med Inform Assoc. 2009;16(5):660–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Byczkowski TL, Munafo JK, Britto MT. Variation in use of Internet-based patient portals by parents of children with chronic disease. Arch Pediatrics Adolesc Med. 2011;165(5):405–411. [DOI] [PubMed] [Google Scholar]
- 17. Tom JO, Mangione-Smith R, Solomon C, Grossman DC. Integrated personal health record use: association with parent-reported care experiences. Pediatrics. 2012;130(1):e183–e90. [DOI] [PubMed] [Google Scholar]
- 18. Byczkowski TL, Munafo JK, Britto MT. Family perceptions of the usability and value of chronic disease web-based patient portals. Health Inform J. 2014;20(2):151–162. [DOI] [PubMed] [Google Scholar]
- 19. Britto MT, Hesse EA, Kamdar OJ, Munafo JK. Parents' perceptions of a patient portal for managing their child's chronic illness. J Pediatrics. 2013;163(1):280–1 e1-e2. [DOI] [PubMed] [Google Scholar]
- 20. Fiks AG, Mayne SL, Karavite DJ, et al. Parent-reported outcomes of a shared decision-making portal in asthma: a practice-based RCT. Pediatrics. 2015;135(4):e965–e973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tom JO, Chen C, Zhou YY. Personal health record use and association with immunizations and well-child care visits recommendations. J Pediatrics. 2014;164(1):112–117. [DOI] [PubMed] [Google Scholar]
- 22. Burke RP, Rossi AF, Wilner BR, Hannan RL, Zabinsky JA, White JA. Transforming patient and family access to medical information: utilisation patterns of a patient-accessible electronic health record. Cardiol Young. 2010;20(5):477–484. [DOI] [PubMed] [Google Scholar]
- 23. Greysen SR, Khanna RR, Jacolbia R, Lee HM, Auerbach AD. Tablet computers for hospitalized patients: a pilot study to improve inpatient engagement. J Hosp Med. 2014;9(6):396–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vawdrey DK, Wilcox LG, Collins SA, et al. A tablet computer application for patients to participate in their hospital care. AMIA Annual Symposium Proceedings/AMIA Symposium. 2011;2011:1428–1435. [PMC free article] [PubMed] [Google Scholar]
- 25. Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc. 2014;21(4):742–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O'Leary KJ, Lohman ME, Culver E, Killarney A, Randy Smith G, Jr, Liebovitz DM. The effect of tablet computers with a mobile patient portal application on hospitalized patients' knowledge and activation. J Am Med Inform Assoc. 2016;23(1): 159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hoonakker PL, Cartmill RS, Carayon P, Walker JM. Development and Psycho metric Qualities of the SEIPS Survey to Evaluate CPOE/EHR Implem entation in ICUs. Int J Healthcare Inform Systems Inform. 2011;6(1):51–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cox ED, Carayon P, Hansen KW, et al. Parent perceptions of children's hospital safety climate. BMJ Qual Safety. 2013;22(8):664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Delbanco T, Walker J, Darer JD, et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153(2):121–125. [DOI] [PubMed] [Google Scholar]
- 30. Adams PF, Hendershot GE, Marano MA, Centers for Disease Control and Prevention/National Center for Health Statistics. Current estimates from the National Health Interview Survey, 1996. Vital Health Stat 10. 1999;200:1–203. [PubMed] [Google Scholar]
- 31. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. [DOI] [PubMed] [Google Scholar]
- 32. Kruse CS, Argueta DA, Lopez L, Nair A. Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J Med Internet Res. 2015;17(2):e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Neuner J, Fedders M, Caravella M, Bradford L, Schapira M. Meaningful use and the patient portal: patient enrollment, use, and satisfaction with patient portals at a later-adopting center. Am J Med Qual. 2015;30(2): 105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Liederman EM, Lee J, Baquero V, Seites P. Patient-physician web messaging: the impact on message volume and satisfaction. J General Int Med. 2005;20(1): 52–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hoonakker PLT, Carayon P, Walker JM, Brown RL, Cartmill RS. The effects of Computerized Provider Order Entry implementation on communication in Intensive Care Units. Int J Med Inform. 2013;82(5):e107–e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Johnson JA, Bootman JL. Drug-related morbidity and mortality. A cost-of-illness model. Arch Intern Med. 1995;155(18):1949–1956. [PubMed] [Google Scholar]
- 37. Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114–2120. [DOI] [PubMed] [Google Scholar]
- 38. Khan A, Furtak SL, Melvin P, Rogers JE, Schuster MA, Landrigan CP. Parent-reported errors and adverse events in hospitalized children. JAMA Pediatrics. 2016;170(4):e154608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kaushal R, Barker KN, Bates DW. How can information technology improve patient safety and reduce medication errors in children's health care? Arch Pediatrics Adolesc Med. 2001;155(9): 1002–1007. [DOI] [PubMed] [Google Scholar]
- 40. Benjamin JM, Cox ED, Trapskin PJ, et al. Family-initiated dialogue about medications during family-centered rounds. Pediatrics. 2015; 135(1):94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]