Abstract
BACKGROUND:
Despite widespread prevalence of lubricant use and rectal douching for receptive anal intercourse (RAI) among men who have sex with men (MSM), research evaluating the association of these behaviors with STIs is limited.
METHODS:
This is an observational analysis of a longitudinal cohort of predominantly Black/Latino MSM in Los Angeles. Every six months from 8/2014–1/2018, participants received STI screening and surveys evaluating lubricant use, douching, substance use, and sexual risk behaviors. GEEs evaluated the association between consistent lubricant use and douching for RAI with positive rectal Neisseria gonorrhoeae, Chlamydia trachomatis, and/or syphilis (positive STI).
RESULTS:
Among 313 participants across 552 study visits, 16.5% (91/552) had positive STI. Consistent lubricant use was reported in 52.7% (243/552) and rectal douching in 57.6% (318/552) of study visits. Consistent lubricant use was associated with STI diagnosis (AOR 1.81; 95% CI 1.11–2.96; p=0.018). Each episode of rectal douching before RAI was associated with 2% increased odds of positive STI (AOR 1.02; 95% CI 1.00–1.04; p=0.041).
CONCLUSIONS:
Among this cohort of HIV-positive and high-risk HIV-negative MSM, lubricant use and douching was common and independently associated with an STI, suggesting the utility of prevention messaging around barrier methods/condoms for sexual encounters involving douching/lubricant use.
Keywords: chlamydia, gonorrhea, syphilis, North America, sexual behavior
INTRODUCTION
Men who have sex with men (MSM) are at increased risk for sexually transmitted infections (STIs), particularly anorectal infections.1 Rectal Neisseria gonorrhoeae and/or Chlamydia trachomatis (GC/CT) as well as ulcerative genital infections (such as syphilis) are of particular public health importance as they have been associated with increased risk for HIV acquisition.2 As such, understanding behaviors and practices that confer increased risk for rectal GC/CT and syphilis are critical to the development of meaningful public health interventions to reduce HIV transmission.
Commercial lubricants are frequently used among MSM, with 59–74% reporting lubricant use during anal intercourse.3,4 Commonly cited reasons for using lubricants include to increase pleasure and facilitate anal intercourse.5 However, data suggest that use of certain lubricants may damage the rectal mucosa, increasing risks for HIV acquisition and transmission of STIs, with mechanisms of injury that vary depending on type of lubricant used.6,7 For example, nonoxynol-9, found in most spermicides, has been demonstrated to be directly cytotoxic to rectal epithelial cells, causing rapid sloughing of rectal epithelium after administration.8 Additionally, hyperosmolar gels similar to commercially available lubricants, such as ID Glide, have been shown to cause erosion of rectal mucosa, likely due to an osmotic effect of the lubricant on rectal epithelium.9
In addition to lubricants, rectal douching (enema use) is a common peri-sexual behavior reported among MSM, with up to 88% of MSM reporting enema use prior to receptive anal intercourse (RAI).10 Commonly cited reasons for rectal douching include hygiene, enhancing pleasure during RAI, request from a sexual partner, and having peers that participate in the behavior.11 Rectal douching is so commonly reported among MSM that research has been conducted exploring the feasibility of using rectal douching as a tool for HIV prevention, specifically as a vehicle for rectal microbicides.12 However, despite the frequency of rectal douching and its possible utility as a tool for HIV prevention, use of enemas with tap water and common household products has been associated with damage to the rectal epithelium, potentially resulting in increased risk for HIV/STI transmission.13
Despite evidence of plausible biologic mechanisms that may predispose individuals who use lubricants and rectal enemas to increased risk of rectal HIV/STI acquisition, research investigating the association of these peri-sexual behaviors with anorectal STIs is limited. Furthermore, existing research exploring this relationship have limitations that may restrict the understanding of the biological and temporal associations of these behaviors with STIs, such as self-report of STIs with no lab confirmation, long recall periods that may prevent temporal sequencing of risk behaviors with STIs, or under-representation of MSM of color.7,14,15 To address these knowledge gaps, this study seeks to evaluate the association of lubricant use and douching for RAI in the last month with rectal STIs. To answer this question, we utilized data from a cohort study of HIV-positive and high-risk HIV-negative, predominantly Black/Latino MSM in Los Angeles. We hypothesize that use of rectal lubricants and enemas for RAI will be positively associated with rectal GC/CT and/or syphilis. Since minority MSM are disproportionately affected by the HIV/STI epidemic,1 investigating peri-sexual behaviors that could be contributing to HIV/STI transmission is crucial toward understanding health disparities experienced by this population and development of effective public health programming.
MATERIALS AND METHODS
Participants and Recruitment
We analyzed data collected as part of an ongoing longitudinal cohort study, designed to evaluate the impact of substance use on HIV transmission dynamics among minority MSM in Los Angeles (NIDA U01 DA036267), in order to evaluate the association of peri-sexual behaviors (lubricant use and rectal douching) during the last month with infectious syphilis and rectal GC/CT. The mSTUDY enrolled primarily Black and Latino MSM, half with active substance use, and participants were recruited to include half HIV-positive and half HIV-negative men. HIV-positive participants were recruited from HIV and sexual health clinics associated with the Los Angeles LGBT Center, which provides a broad spectrum of clinical and community resources for the lesbian, gay and transgender community in Los Angeles. MSM without HIV infection were recruited from the UCLA Vine Street Clinic (a community-based university research clinic) through community flyers and online advertisements. Inclusion criteria for the cohort were: 1) 18–45 years old, 2) born male, 3) condomless anal intercourse (CAI) with a man in past 6 months (if HIV-negative). Participant enrollment for the mSTUDY started in August 2014 with all participants having follow-up every six months. This analysis focused on participants who completed study visits between August 2014 (study inception) and January 2018, who reported receptive anal intercourse (RAI) within the last 6 months and provided information on last month lubricant use and douching for RAI. January 2018 was used as the cut-off for this analysis, as this was when the survey module on rectal/anal hygiene behaviors concluded. As recruitment for the mSTUDY was still ongoing in January 2018, participants who were enrolled later in the study had fewer follow-up visits than those who were enrolled at study inception. A total of 313 unique individuals, with 552 study visits were eligible and included in this analysis.
Study Procedures and Data Collection
The study protocol was reviewed and approved by the Office of Human Research Participant Protection (OHRPP) at the University of California, Los Angeles. Methods regarding the mSTUDY have been previously described.16,17 Briefly, following written informed consent, participants underwent clinician interview, specimen collection (blood and rectal swabs) for STI screening, and completion of computer-assisted self-interview survey at each study visit that collected sociodemographic data as well as information including lubricant use, rectal douching, sexual risk behaviors, and substance use.
Commercial lubricant use was reported as frequency (never, sometimes, always) in past month during RAI and was dichotomized to consistent (always) or inconsistent lubricant use during RAI (never or sometimes). Rectal douching was reported as frequency of douching before RAI in the past month and was evaluated on the event-level (i.e., per episode of RAI). Reports of behaviors representing risk of exposure to STIs/HIV in the last 6 months included number RAI partners, number of main/regular partners, and concurrent (overlapping) sexual partnerships. Substance use variables included methamphetamine and popper use (amyl nitrate and butyl nitrate) and were measured by self-reported frequency of use (daily, weekly, monthly, less than monthly, once, or never) within the last 6 months. For this analysis, substance use was dichotomized to “regular” (daily, weekly, or monthly) and “not regular” use (never, once, or less than monthly).
STI testing was conducted at each visit using rectal swabs that were tested for GC/CT infection with nucleic acid amplification testing (NAAT) (Aptima Combo 2, GenProbe, San Diego, CA), and blood samples were collected for syphilis and HIV testing at each visit. Syphilis testing used rapid plasma reagin (RPR) with confirmatory testing via the Treponema pallidum particle agglutination test (TPPA). HIV screening used antibody testing (ELISA) with Western blot confirmation. Infectious syphilis was defined using the Centers for Disease Control determination following positive test results and confirmation from the local health department. Our STI outcome variable was defined as positive rectal GC/CT NAAT and/or positive syphilis testing identified as infectious syphilis (primary, secondary, or early latent syphilis), as these STIs can be transmitted rectally. STI testing results were made available to participants, and study personnel assisted with notifying participants of their test results and facilitated linkages to care for positive test results.
Data Analysis
Descriptive statistics including mean, median, range, and frequency distributions were utilized to characterize the study sample. Differences between participant demographic factors, sexual risk behaviors, rectal douching and lubricant use, and STIs were assessed in bivariate analyses using chi-square analysis for categorical predictors and Kruskal-Wallis tests for non-parametric, continuous variables. The association between frequency of lubricant use and rectal douching with our outcome of interest – positive STI (rectal GC/CT and/or infectious syphilis) was analyzed using regression analysis with general estimating equations (GEE). We used an exchangeable working correlation matrix and robust standard errors to calculate unadjusted and adjusted odds ratios (OR) of lubricant use, rectal douching, and substance use with STI controlling for demographics,1,18 HIV status, and the following HIV/STI risk behaviors: number RAI partners, number main/regular partners,19 concurrent sexual partnerships,20 and substance use (methamphetamine21 and poppers22). Variables with a p-value <0.10 in bivariate analysis, or important conceptually based on the literature, were included in our final multivariable GEE model. Pearson correlation coefficients were calculated between all predictors to ensure no multicollinearity in the final model. Complete case analysis was performed for all models. All analyses were conducted using Stata 15.1 (StataCorp, College Town, TX).
RESULTS
This sample consisted of 313 participants over 552 study visits, with 43.8% participants having ≥2 visits during the study period relevant to this analysis. Among the 313 participants, median age was 30 years (IQR: 25–36), 40.6% identified as Black/African American, and 40.9% Latino. Across all visits, recent sexual risk behaviors were common with 56.5% reporting concurrent sexual partnerships (312/552) and 19.6% reporting regular methamphetamine use (108/552). Positive rectal GC/CT and/or infectious syphilis was diagnosed in 16.5% (91/552) visits with 8.0% having rectal CT, 7.6% rectal GC, and 3.8% infectious syphilis (Figure 1).
Figure 1: Percent of STIs Diagnosed at Study Visits by Lubricant Use and Rectal Douching in Last Month.
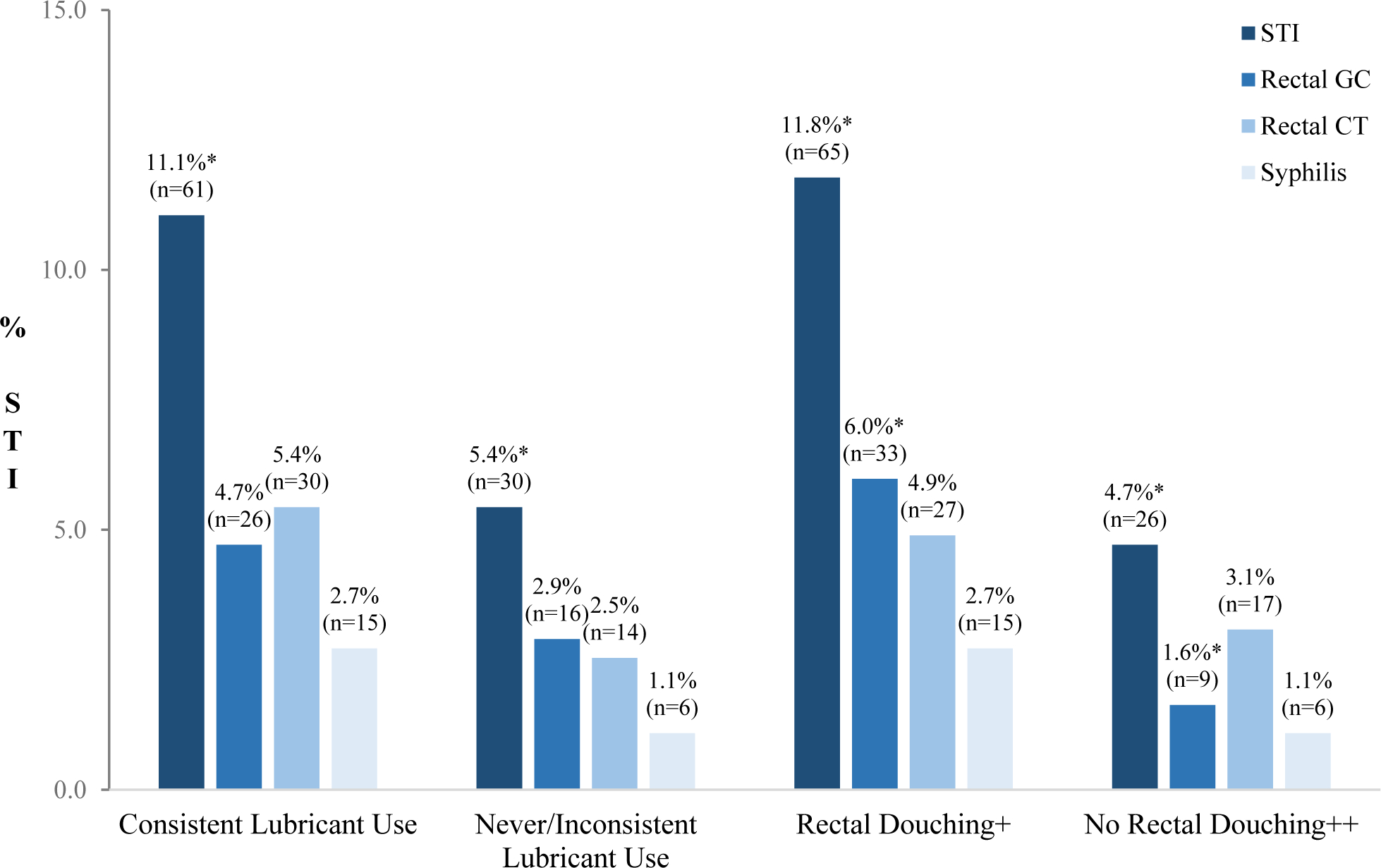
STI = sexually transmitted infection (rectal GC, rectal CT, and/or syphilis)
rectal GC = rectal Neisseria gonorrhoeae
rectal CT = rectal Chlamydia trachomatis
+ 1+ episode of rectal douching prior to receptive anal intercourse (RAI) in last month
++ No episodes of rectal douching prior to RAI in last month
* p≤0.05
Note: discrepancies in percentage totals are due to multiple STIs diagnosed at the same visit
Consistent lubricant use (i.e., reporting ‘always’ using lubricants) was reported in 55.1% (304/552) and rectal douching was reported in 57.6% (318/552) of visits. Both douching and consistent lubricant use in the past month was reported at 39.1% (216/552) of visits. Prevalence of STIs was higher among participants who reported consistent lubricant use compared to those with inconsistent lubricant use (20.1%=61/304 vs. 12.1%=30/248, respectively; p=0.012) (Table 1). Men with positive STI reported douching for RAI a median of 2 times (IQR 0–5) while those with negative STI reported a median of 1 time (0–3; p-value <0.001) in the past month. Approximately 69.2% of visits with positive STI occurred among individuals who were HIV-positive (n=63/91). STI positivity was higher for visits where regular methamphetamine use was reported (25.9%=28/108) as compared to visits without regular methamphetamine use (14.2%=63/444; p=0.003).
Table 1:
Descriptive Statistics and Bivariate Analysis of Selected Variables with Syphilis, Rectal Neisseria gonorrhoeae and/or Chlamydia trachomatis (GC/CT) During Study Visits among Men Who Have Sex with Men Reporting Receptive Anal Intercourse (RAI) in Last 6 Months 8/2014–1/2018 (N=552)
| Negative STI* (n=461) | Positive STI* (n=91) | p-value** | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Consistent lubricant use during RAI∫ | 243 | 52.71 | 61 | 67.03 | 0.012 | |
| Rectal douching before RAI∫ | 1 (0–3) | 2 (0–5) | <0.001 | |||
| Age | 31 (26–37) | 31 (25–38) | 0.541 | |||
| Race/Ethnicity | ||||||
| White/Caucasian | 67 | 14.53 | 15 | 16.48 | 0.963 | |
| Latino | 183 | 39.70 | 35 | 38.46 | ||
| Black/African American | 183 | 39.70 | 35 | 38.46 | ||
| Other | 28 | 6.07 | 6 | 6.59 | ||
| HIV Positive | 226 | 49.02 | 63 | 69.23 | <0.001 | |
| Number RAI partners∫∫ | 2 (1–5) | 5 (2–10) | <0.001 | |||
| Number main/regular partners∫∫ | 1 (1–3) | 2 (0–3) | 0.967 | |||
| Regular poppers use∫∫ | 57 | 12.36 | 17 | 18.68 | 0.106 | |
| Regular methamphetamine use∫∫ | 80 | 17.35 | 28 | 30.77 | 0.003 | |
| Sexual concurrency∫∫ | 256 | 55.53 | 56 | 61.54 | 0.291 | |
STI defined as infectious syphilis and/or rectal GC/CT
Results are presented as either median (IQR) or n (%). P-values <0.05 are in bold.
last month,
last 6 months
In unadjusted analysis, consistent lubricant use during RAI in last month was associated with increased odds of positive STI (OR 1.81; 95% CI 1.12–2.93), compared to those who reported inconsistent or no lubricant use (Table 2). Additionally, for every episode of douching prior to RAI in the last month, there was 2% increased odds of positive STI (OR 1.02; 95% CI 1.00–1.03). Respondents who were HIV-positive had more than twice higher odds of positive STI than those who were HIV-negative (OR 2.23; 95% CI 1.35–3.67). Regular methamphetamine use was associated with positive STI (OR 2.06; 95% CI 1.15–3.70), compared to men who did not report regular methamphetamine use.
Table 2:
Peri-Sexual Behaviors and Participant Characteristics Associated with Syphilis, Rectal Neisseria gonorrhoeae and/or Chlamydia trachomatis (GC/CT) among Men Who Have Sex with Men Reporting Receptive Anal Intercourse (RAI) in Last 6 Months 8/2014–1/2018
| Unadjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
|---|---|---|---|---|
| Lubricant use during RAI∫ | ||||
| Never/Inconsistent | Ref | -- | Ref | -- |
| Consistent | 1.81 (1.12–2.93) | 0.015 | 1.81 (1.11–2.96) | 0.018 |
| Rectal douching before RAI∫ | 1.02 (1.00–1.03) | 0.035 | 1.02 (1.00–1.04) | 0.041 |
| Age | 0.99 (0.95–1.03) | 0.486 | 0.96 (0.92–1.00) | 0.066 |
| Race/Ethnicity | ||||
| White/Caucasian | Ref | -- | Ref | -- |
| Latino | 1.36 (0.53–3.50) | 0.529 | 1.16 (0.49–2.75) | 0.731 |
| Black/African American | 1.29 (0.50–3.34) | 0.597 | 1.29 (0.55–3.05) | 0.559 |
| Other | 1.14 (0.27–4.80) | 0.853 | 1.00 (0.25–3.96) | 0.995 |
| HIV | ||||
| Negative | Ref | -- | Ref | -- |
| Positive | 2.23 (1.35–3.67) | 0.002 | 2.42 (1.36–4.31) | 0.003 |
| Number RAI partners∫∫ | 1.00 (1.00–1.01) | 0.341 | 1.00 (0.99–1.01) | 0.968 |
| Number main/regular partners∫∫ | 0.99 (0.95–1.03) | 0.475 | 0.95 (0.90–1.01) | 0.083 |
| Regular poppers use∫∫ | ||||
| No | Ref | -- | Ref | -- |
| Yes | 1.75 (0.96–3.20) | 0.069 | 1.27 (0.64–2.54) | 0.492 |
| Regular methamphetamine use∫∫ | ||||
| No | Ref | -- | Ref | -- |
| Yes | 2.06 (1.15–3.70) | 0.015 | 1.80 (0.93–3.48) | 0.079 |
| Sexual concurrency∫∫ | ||||
| No | Ref | -- | Ref | -- |
| Yes | 1.28 (0.81–2.01) | 0.285 | 1.23 (0.75–2.02) | 0.404 |
Note: bold indicates statistical significance
last month,
last 6 months
In multivariable analyses, consistent lubricant use was independently associated with STI (adjusted OR[AOR] 1.81; 95% CI 1.11–2.96), compared to men who reported inconsistent or no lubricant use in past month. For every episode of rectal douching prior to RAI in last month, there was an associated 2% increased odds of STI diagnosis (AOR 1.02; 95% CI 1.00–1.4). Additionally, men who were HIV-positive had higher odds of positive STI (AOR 2.42; 95% CI 1.36–4.31) compared to respondents who were HIV-negative. While regular methamphetamine use was associated with STI in our unadjusted analysis, this behavior was not associated with STI in our adjusted analysis. Additionally, interaction between lubricant use and rectal douching was tested for in our adjusted model and was found not to be significant (data not shown).
DISCUSSION
Findings from this study demonstrate that reported lubricant use and rectal douching associated significantly with rectal GC/CT and/or infectious syphilis after adjusting for demographics, HIV status, substance use, and sexual risk behaviors for HIV/STI transmission. Lubricants are frequently used by MSM during anal intercourse, and rates of reported lubricant use in our analysis were similar to those in previous studies.3,4 However, we extend the current literature by using laboratory diagnosis (not self-report) of rectal GC/CT and infectious syphilis, which are STIs that have the highest chance of being impacted by these peri-sexual behaviors. Additionally, our findings demonstrate an association with HIV seropositivity and STI diagnosis, highlighting the importance of STI prevention and screening in this population, given the known implications of STI co-infection on HIV transmission.2
Two observational studies have investigated associations of lubricant use with rectal STI. Our findings are consistent with that of Gorbach et al. which demonstrated that lubricant use during RAI in the past month was associated with an increased prevalence of rectal GC/CT and syphilis among a cohort of men and women from Baltimore and Los Angeles.7 In the only study exclusively asking this research question among MSM, Maierhofer et al. demonstrated that rectal GC was significantly associated with use of specific lubricant brands, but failed to demonstrate an association of rectal GC/CT with any consistent commercial lubricant use, though very few MSM did not use any commercial lubricants in their analysis.15
In addition to lubricant use, rectal douching is extremely common among MSM.4,11 Our results demonstrated an association of douching with rectal GC/CT and/or syphilis infection and are consistent with previous studies that have demonstrated an association between rectal enema use with STIs and HIV among MSM.23 Possible biologic mechanisms thought to be responsible for this association are sloughing of the rectal epithelium, mucosal injury from improper use of douching tools, rectal trauma from large volume enemas, removal of bacterial flora resulting in changes to the microbiome that facilitate pathogen entry, and transmission of pathogens through shared equipment.14,23 In addition, rectal douching may be associated with risky behaviors for HIV/STI acquisition, such as HIV seropositivity, history of prior STI diagnosis, and CAI with multiple partners.23,24 However, the association between rectal STI and douching, as well as lubricant use, changed very little when logistic models adjusted for risky behaviors – suggesting that there is an association between lubricant use and douching with rectal STI independent of frequency of self-reported sexual risk behaviors. Furthermore, while methamphetamine use has been associated with increased STI prevalence in prior studies,21 it was not significantly associated with rectal STI in our adjusted analysis. We suspect this observation was due to relatively high prevalence of methamphetamine use in this sample in addition to our study being slightly underpowered to detect a small effect size; however, this is an important area for future study.
There are multiple strengths associated with our study. First, this is a cohort study which allows for repeated assessment of time-varying behaviors such as sexual practices and substance use among high-risk MSM with systematic laboratory testing of STIs. Additionally, this study controlled for multiple factors that are high-risk for STI acquisition, such as sexual concurrency, number RAI partners, and substance use, all of which were systematically self-reported by participants using computer-assisted survey at all visits. Furthermore, our study contains a cohort of predominantly Latino and Black MSM, which is especially important as MSM of color are particularly vulnerable to the ongoing HIV/STI epidemic.
As with any study, our analysis must be interpreted within the context of limitations. Factors associated with STI transmission are extremely complex and involve constructs that are difficult to measure or were not included in this analysis (such as risk perception, trust, event-level condom use, and beliefs surrounding health protective behaviors) and there is the possibility for omitted variables bias. Our study does attempt to account for this by including numerous variables that are high-risk for STI acquisition in our analysis. As our data is self-reported, there is the potential for recall bias. Our study sample contains an overrepresentation of Black/Latino MSM by design, thus limiting the generalizability of our findings to all MSM populations. However, as Black and Latino MSM are disproportionately affected by the HIV/STI epidemic, we feel that this is actually a strength of our analysis, as this population is one of the most vulnerable to HIV/STI acquisition/transmission and should be prioritized in public health efforts. Finally, we did not assess the type of lubricant or enema solution used. As previous studies have suggested that risk of STI acquisition may differ based on type of rectal lubricant and douching solution,6,23 future research evaluating rectal STIs based on type of rectal lubricant and/or enema used for RAI is warranted.
CONCLUSIONS
Our analysis demonstrates a positive association between consistent lubricant use and douching for RAI with rectal GC/CT and/or syphilis infection among this cohort of MSM predominantly of color. Both behaviors were associated with increased odds of positive STI among these MSM and over time. Our findings suggest that these practices, or implicit risk behaviors that commonly occur with these practices, may contribute to the HIV/STI epidemic among MSM and indicate the need for future research evaluating these peri-sexual behaviors in relation to STI transmission. Furthermore, as rectal lubricant use and douching are extremely common peri-sexual behaviors among MSM, our findings suggest the utility of prevention messaging around barrier methods/condoms for sexual encounters involving douching/lubricant use.
FUNDING ACKNOWLEDGEMENT:
mSTUDY is funded by the National Institute of Drug Abuse (U01 DA036267). CSB was supported by the National Institute of Mental Health (T32 MH080634). WSC, SS, and PMG were supported by the Center for HIV Identification, Prevention, and Treatment Services (CHIPTS; P30 MH058107).
Footnotes
DECLARATION OF CONFLICTING INTERESTS:
The authors declare that there is no conflict of interest.
REFERENCES
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2017. 2018. Atlanta. [Google Scholar]
- 2.Ward H and Rönn M. The contribution of STIs to the sexual transmission of HIV. Curr Opin HIV AIDS 2010; 5: 305 DOI: 10.1097/COH.0b013e32833a8844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Javanbakht M, Stahlman S, Pickett J, et al. Prevalence and types of rectal douches used for anal intercourse: results from an international survey. BMC Infect Dis 2014; 14: 95 DOI: 10.1186/1471-2334-14-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rolle CP, Bolton MD and Kelley CF. Use of a prospective sex diary to study anal lubricant and enema use among high risk men who have sex with men - implications for human immunodeficiency virus prevention. Sex Transm Dis 2016; 43: 476–478. DOI: 10.1097/olq.0000000000000473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dodge B, Hubach RD, Schick V, et al. Lubricant use at last sexual encounter with a male partner: findings from a nationally representative sample of self-identified gay and bisexual men in the United States. Sex Health 2015; 12: 300–307. DOI: 10.1071/SH14186. [DOI] [PubMed] [Google Scholar]
- 6.Sudol KM and Phillips DM. Relative safety of sexual lubricants for rectal intercourse. Sex Transm Dis 2004; 31: 346–349. DOI: 10.1097/00007435-200406000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Gorbach PM, Weiss RE, Fuchs E, et al. The slippery slope: lubricant use and rectal sexually transmitted infections: a newly identified risk. Sex Transm Dis 2012; 39: 59–64. DOI: 10.1097/OLQ.0b013e318235502b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phillips DM, Sudol KM, Taylor CL, et al. Lubricants containing N-9 may enhance rectal transmission of HIV and other STIs. Contraception 2004; 70: 107–110. DOI: 10.1016/j.contraception.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Guidos AM, Hendrix CW, Bakshi RP, et al. Hyperosmolar sexual lubricant causes epithelial damage in the distal colon: potential implication for HIV transmission. J Infect Dis 2007; 195: 703–710. DOI: 10.1086/511279. [DOI] [PubMed] [Google Scholar]
- 10.Javanbakht M, Stahlman S, Pickett J, et al. Prevalence and types of rectal douches used for anal intercourse: results from an international survey. BMC Infect Dis 2014; 14: 95 DOI: 10.1186/1471-2334-14-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carballo-Dieguez A, Lentz C, Giguere R, et al. Rectal douching associated with receptive anal intercourse: a literature review. AIDS Behav 2018; 22: 1288–1294. DOI: 10.1007/s10461-017-1959-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoang T, Date AA, Ortiz JO, et al. Development of rectal enema as microbicide (DREAM): Preclinical progressive selection of a tenofovir prodrug enema. Eur J Pharm Biopharm 2019; 138: 23–29. DOI: 10.1016/j.ejpb.2018.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmelzer M, Schiller LR, Meyer R, et al. Safety and effectiveness of large-volume enema solutions. Appl Nurs Res 2004; 17: 265–274. DOI: 10.1016/j.apnr.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Achterbergh R, van der Helm J, van den Boom W, et al. Is rectal douching and sharing douching equipment associated with anorectal chlamydia and gonorrhoea? A cross-sectional study among men who have sex with men. Sex Transm Infect 2017; 93: 431–437. DOI: 10.1136/sextrans-2016-052777. [DOI] [PubMed] [Google Scholar]
- 15.Maierhofer C, Rice CE, Wang S-H, et al. Lubricant use and rectal chlamydial and gonococcal infections among men who engage in receptive anal intercourse. Sex Transm Dis 2016; 43: 423–428. DOI: 10.1097/olq.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 16.Gorbach PM, Javanbakht M, Shover CL, et al. Associations between cannabis use, sexual behavior, and sexually transmitted infections/human immunodeficiency virus in a cohort of young men who have sex with en. Sex Transm Dis 2019; 46: 105–111. DOI: 10.1097/OLQ.0000000000000919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Javanbakht M, Ragsdale A, Shoptaw S, et al. Transactional sex among men who have sex with men: differences by substance use and HIV status. J Urban Health 2019; 96: 429–441. DOI: 10.1007/s11524-018-0309-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. HIV Surveillance Report 2017. 2018. Atlanta. [Google Scholar]
- 19.Sullivan PS, Salazar L, Buchbinder S, et al. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS 2009; 23: 1153–1162. DOI: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 20.Pines HA, Karris MY and Little SJ. Sexual partner concurrency among partners reported by MSM with recent HIV infection. AIDS Behav 2017; 21: 3026–3034. DOI: 10.1007/s10461-017-1855-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoenigl M, Chaillon A, Moore DJ, et al. Clear links between starting methamphetamine and increasing sexual risk behavior: a cohort study among men who have sex with men. J Acquir Immune Defic Syndr 2016; 71: 551–557. DOI: 10.1097/QAI.0000000000000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heiligenberg M, Wermeling PR, van Rooijen MS, et al. Recreational drug use during sex and sexually transmitted infections among clients of a city sexually transmitted infections clinic in Amsterdam, the Netherlands. Sex Transm Dis 2012; 39: 518–527. DOI: 10.1097/OLQ.0b013e3182515601. [DOI] [PubMed] [Google Scholar]
- 23.Li P, Yuan T, Fitzpatrick T, et al. Association between rectal douching and HIV and other sexually transmitted infections among men who have sex with men: a systematic review and meta-analysis. Sex Transm Infect 2019; 95: 428–436. DOI: 10.1136/sextrans-2019-053964. [DOI] [PubMed] [Google Scholar]
- 24.Noor SW and Rosser BS. Enema use among men who have sex with men: a behavioral epidemiologic study with implications for HIV/STI prevention. Arch Sex Behav 2014; 43: 755–769. DOI: 10.1007/s10508-013-0203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


