Abstract
A previously well 59-year-old man required a prolonged intensive care unit stay due to severe COVID-19 symptoms. During the admission, he developed a cytokine storm, also known as secondary haemophagocytic lymphohistocytosis, and multiorgan failure. Despite recovering from his other organ failures, his liver function continued to deteriorate. Magnetic resonance cholangiopancreatography and subsequent endoscopic retrograde cholangiopancreatography revealed extensive intrahepatic duct dilatation with ‘beading’ but common bile duct sparing. Given the patient had no primary liver disease prior to admission, we considered secondary causes of cholestatic liver injury; this led us to an unusual diagnosis of secondary sclerosing cholangitis in critically ill patients. This case demonstrates a rare disease that has developed specifically in the context of SARS-CoV-2 infection. A review of current literature and the underlying pathophysiology for this rare disease are discussed, particularly in relation to COVID-19.
Keywords: liver disease, infectious diseases, adult intensive care
Background
Secondary sclerosing cholangitis (SSC) is diagnosed when a cause for progressive cholestatic liver injury is identified in patients who have no prior history of hepatobiliary disease.1 Several secondary causes have been identified over recent years, including ischaemia and iatrogenic, yet the SSC in critically ill patients (SSC-CIP) subgroup is particularly rare and was first described in 2001 by Leonhardt et al.2
The underlying pathophysiology in patients with SSC-CIP is thought to be a combination of bile duct ischaemia and changes to the composition of bile.3 This results in cholangiocyte necrosis and formation of bile casts that obstruct the biliary system, giving rise to recurrent cholangitis.1
The most important factor distinguishing SSC-CIP from other hepatobiliary diseases related to critically ill patients is the persistent cholestasis despite clinical recovery of other organ injuries.4 This progressive cholestasis is reflective of irreversible cellular damage, and hence a relatively poor prognosis often with rapid deterioration to biliary cirrhosis, requiring transplantation as an only means of cure.5
SSC-CIP is not widely appreciated by physicians and intensivists, such that it may go unrecognised in some patients. This case therefore provides an excellent learning opportunity to inform readers of this rare disease, particularly in the context of COVID-19, with the aim of promoting earlier disease recognition to allow timely investigation and optimal management strategies, including referral for transplant assessment.
Here a rare case of SSC-CIP is reported after a prolonged intensive care admission due to SARS-CoV-2 infection.
Case presentation
A previously fit and well 59-year-old man was admitted to the intensive care unit (ICU) with a 2-week history of cough, fever and breathlessness. Admission blood profile revealed lymphopenia, with a d-dimer of >20 000 μg/L and ferritin of 3991 μg/L. He was intubated and ventilated for severe hypoxia on day 1 and was subsequently confirmed SARS-CoV-2 positive via oropharyngeal swab. Shortly after admission, the patient developed a cytokine storm, known as secondary haemophagocytic lymphohistocytosis (sHLH) and multiorgan failure. He was also treated with levofloxacin for presumed superimposed bacterial pneumonia. During his ICU admission, the patient was also treated for staphylococcus septicaemia and cellulitis with vancomycin and co-trimoxazole and later developed Candida albicans infection from the central line, bile and urine cultures, which was managed with a course of caspofungin. He intermittently required inotrope support and developed necrotic toes on his left foot. The patient was slow to wake up from his sedation and had a prolonged respiratory wean, leading to tracheostomy insertion 3 weeks into his admission, with a successful decannulation 1 month later.
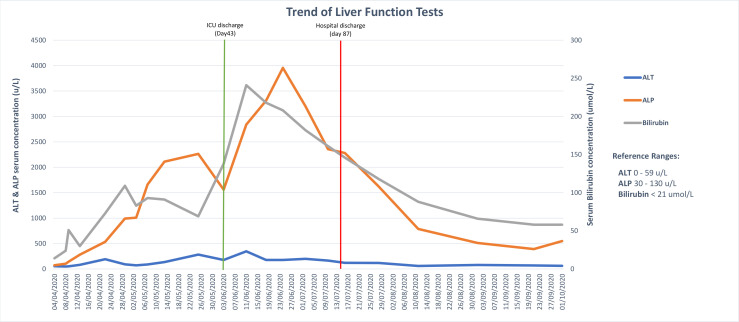
While in ICU, it was noted that the patient’s liver function tests (LFTs) were becoming deranged with a cholestatic pattern, having been normal on admission (figure 1). Prothrombin time peaked at 20.4 s, but normalised promptly with intravenous vitamin K. His cholestasis has continued to improve slowly since the date of discharge.
Figure 1.
Cumulative figures of serum bilirubin, alanine transaminase (ALT) and alkaline phosphatase (ALP) concentrations throughout the patient’s secondary care admission. The green vertical line demonstrates discharge from intensive care unit (ICU), and the red vertical line demonstrates discharge from secondary care.
Investigations
Imaging while on ICU included two abdominal ultrasound scans, which did not reveal any parenchymal or biliary tree abnormality. However, a magnetic resonance cholangiopancreatography (MRCP) undertaken when the patient was discharged from ICU revealed a few hypointense filling defects within the common bile duct (CBD) suspicious of choledocholithiasis. The intrahepatic bile ducts were also dilated and demonstrated some beading (figure 2). A subsequent endoscopic retrograde cholangiopancreatography (ERCP) revealed ‘bizarre appearances’ with a large column of sludge within the whole CBD and a sclerosing cholangitis type picture within the intrahepatic ducts (figure 3). As part of a non-invasive liver screen, serology revealed negative Anti-Neutrophilic Cytoplasmic Autoantibody (ANCA), IgG-4 and liver autoantibodies.
Figure 2.
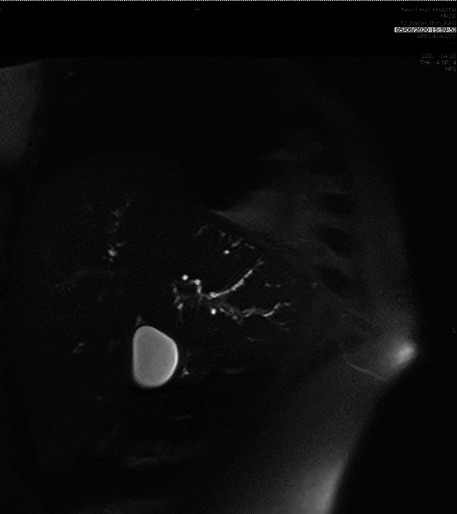
Magnetic resonance cholangiopancreatography image showing ‘beading’ effect of intrahepatic bile ducts.
Figure 3.
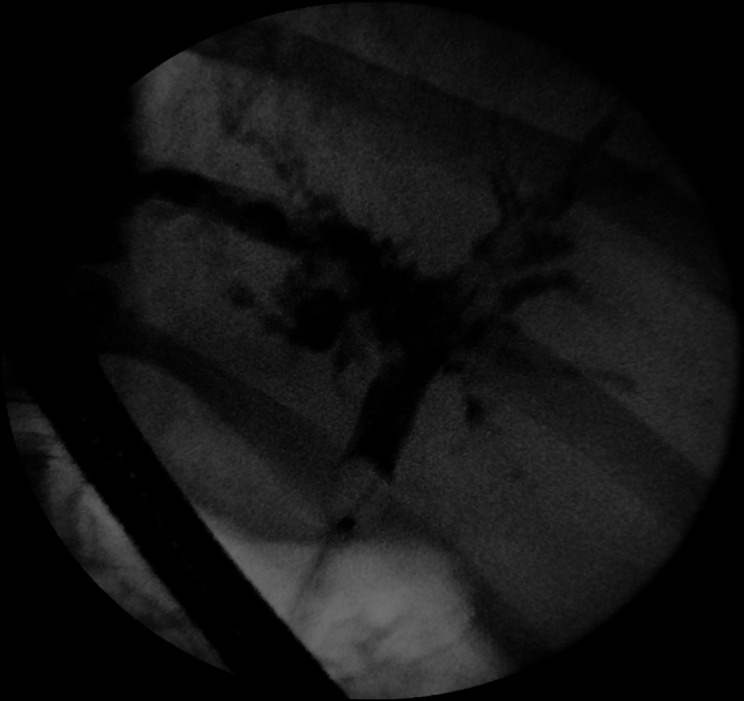
Cholangiogram taken during endoscopic retrograde cholangiopancreatography revealing a sclerosing cholangitis type picture within the intrahepatic ducts.
Differential diagnosis
When this man was initially reviewed on ICU, the deteriorating LFTs were thought to be caused by a combination of pathophysiological factors accumulating in multiorgan failure, driven by COVID-19 and superimposed bacterial septicaemia. At that time, given the normal appearance on ultrasound scanning, a ‘watch and wait’ approach was taken on the assumption the LFTs would normalise as the patient improved clinically. However, despite other organ systems recovering, the LFTs continued to deteriorate. Differentials at this point were vast, however, primary liver disease, such as autoimmune hepatitis or primary sclerosing cholangitis (PSC), was low on the list of differentials given the patient had no known hepatobiliary disease prior to admission. Hence, we considered secondary causes of cholestatic liver injury in the context of critically unwell adults; drug-induced liver injury was considered a potential contributory factor, although not the sole cause given the degree of cholestasis and subsequent findings on imaging. This led us to an unusual diagnosis of SSC-CIP.
Treatment
The patient underwent two ERCP procedures; on the first occasion, endoscopic sphincterotomy and balloon trawl of sludge were performed. His bilirubin peaked at 241 μmol/L just before this procedure and slowly fell during subsequent weeks. A trial of ursodeoxycholic acid was also initiated after the first procedure. A further ERCP and balloon trawl of sludge with bile taken for culture were performed 1 month later. At the time of write-up, the patient is awaiting liver biopsy to further evaluate the degree of hepatocyte and sinusoidal injury.
Outcome and follow-up
The patient, who’s admission was precipitated by SARS-CoV-2 infection, has since been discharged from the secondary care setting. Liver biopsy will further inform as to the degree of resulting parenchymal and portal tract architectural disturbance, and whether or not referral to a regional transplant centre will be required.
Discussion
Unlike PSC, which is an idiopathic disease process,6 SSC is diagnosed when a cause for the progressive cholestatic injury is identified in patients with no prior history of hepatobiliary disease.1 Many secondary causes have been identified over recent years inclusive of ischaemia, drug-induced and auto-immune IgG-4,7 however, the SSC-CIP subgroup is a particularly rare disease that was first reported in 2001 by Scheppach et al.8 It has an estimated prevalence of 1 in 2000 ICU admissions, but only 250 cases have so far been reported worldwide.1 The patients documented with SSC-CIP have all been treated in an ICU setting for multiple reasons including that of severe infection, trauma, burns and postcardiothoracic surgery.9 Typically, in such patients, the cholestatic pattern of deranged LFTs persists beyond the recovery of the disease that initially precipitated ICU admission.4
The underlying pathophysiology in patients with SSC-CIP is not completely understood but is generally thought to be due to a combination of bile duct ischaemia (ischaemic cholangiopathy) and changes to the composition of bile (toxic bile), which together results in cholangiocyte necrosis and cast formation.2 This relative bile duct obstruction can precipitate infection, thus causing further disease progression to irreversible intrahepatic bile duct destruction and subsequent secondary biliary cirrhosis.2
Both ischaemic cholangiopathy and toxic bile formation can develop for multiple reasons relating to critical illness and management within an ICU setting.
Ischaemic cholangiopathy
Intrahepatic biliary epithelium is particularly susceptible to ischaemia because anatomically it only has a singular blood supply via the hepatic arteries, unlike the CBD and hepatocytes that have a dual blood supply.9 Bile duct ischaemia is thought to occur for several reasons within a critical care setting; macrocirculatory haemodynamic instability with reduced mean arterial pressures requiring vasopressor support occurs in up to a third of patients admitted to ICU10; this figure ranges between 60% and 100% in those patients developing SSC-CIP.2 4 11 While vasopressors help to increase systemic blood pressure, they often have a negative effect on hepatosplanchnic blood supply; for example, norepinephrine, which is commonly used in ICU to aid haemodynamic stability, has a vasoconstrictive property that reduces splanchnic blood flow, thus precipitating relative ischaemia.12
Additionally, microcirculatory compromise within the peribiliary vascular plexus is a significant feature of SSC-CIP; Deltenre and Valla demonstrated that the degree of ischaemic cholangiopathy was inversely proportional to the calibre of the supplying occluded artery.13 According to Leonhardt et al,2 reasons for microcirculatory blood flow disturbance when a patient is critically unwell include increased blood viscosity and hypercoagulable states. This is particularly relevant in the context of severe SARS-CoV-2 infection in which a number of alterations in prothrombotic factors have been demonstrated,14 resulting in a hypercoagulable state. Hyperviscosity, which promotes a hypercoagulable state, has also been reported by Maier et al15 in patient with COVID-19 who require critical care intervention. Hypercoagulable states in the context of SARS-CoV-2 infection, known as COVID-19-associated coagulopathy, have demonstrated a higher risk of both venous and arterial thromboembolisation.16 Given that the predominant clinical finding in patients with COVID-19 is thrombosis, rather than bleeding, helps distinguish this pathological process from a disseminated intravascular coagulation-like state.17 Arterial thrombosis has been documented in patients infected with SARS-CoV-2, whereby D-dimer levels have been recorded in excess of 9000 μg/L.18 19 This is reflective of the patient described in our case study whose D-dimer exceeded 20 000 μg/L on admission. Formation of microvascular thrombi has also been demonstrated in postmortem studies of those who have died with severe COVID-19 infection, the underlying cause of which is thought to be linked to hypercoagulopathy, direct endothelial damage and hyperviscosity states.16 20
Mechanical ventilation with high positive end-expiratory pressures (PEEP) greater than 10 cm H2O has also been shown to contribute to microcirculatory ischaemia within the hepatosplanchnic vascular plexus.21 Additionally, excessive use of prone positioning of mechanically ventilated patients has been linked to the development of SSC-CIP.22 Both these factors are particularly relevant in the context of severe SARS-CoV-2 infection, whereby mechanical ventilation with high PEEP for prolonged periods due to the challenges of weaning23 plus the use of proning in such patients for up to 16 hours per day are relatively common.24
Overall, disturbances in the arterial supply of the peribiliary vascular plexus lead to cholangiocyte necrosis with subsequent formation of biliary casts and inflammation of intrahepatic bile ducts. This results in cholestasis and recurrent biliary infection, which risks further biliary obstruction and cirrhosis through ongoing scarring and inflammation.4
Toxic bile
Toxic bile is also implicated as a causative factor of SSC-CIP. Usually defence mechanisms rely on hepatobiliary transporters to protect cholangiocytes from the toxic bile salts. Ischaemia predisposes to failure of such transporter systems which subsequently contribute to cholestasis and cell necrosis.25 An additional defence mechanism that is adversely affected by ischaemia is that of bicarbonate secretion via the chloride–bicarbonate anion exchanger 2 (AE2). Normally, this process promotes an alkaline pH on the apical surface of cholangiocytes and thus prevents permeation of bile acids.26 In addition, proinflammatory cytokines have been shown to inhibit the activity of AE2.27 This is important in the context of severe SARS-CoV-2 infection due to its association with a syndrome of uncontrolled immune activation leading to a cytokine storm, also known as HLH.28 Indeed Leonhardt et al2 found that all 16 patients in their study had features of a systemic hyperinflammatory syndrome prior to their diagnosis of SSC-CIP. This further suggests that a heightened systemic inflammatory response through the release of proinflammatory cytokines adds to the development of toxic bile, hence contributing to cholangiocyte necrosis, and as such has an important association with SARS-CoV-2 infection.
Diagnosing SSC-CIP is challenging for several reasons, particularly given the disease is not well recognised and the underlying pathophysiological mechanisms are not completely understood.1 Also, patients with SSC-CIP are largely asymptomatic initially, presenting only with a cholestatic pattern of deranged LFTs, for which there are many more common differentials in patients who are critically unwell. Here, the differentials that one must consider include sepsis cholestasis, choledocholithiasis, drug-induced liver injury or adverse effects of intravenous nutrition.5
While ultrasound imaging can be undertaken at the bedside, it is operator dependent and cannot always be relied on in the diagnosis of intrahepatic biliary diseases; while some authors report visible changes within the hepatobiliary complex in accordance with sclerosing cholangitis,29 others have reported unremarkable ultrasound imaging30 in keeping with the case discussed. MRCP or ERCP are more likely to aid the diagnosis of SSC-CIP, but these investigations are often delayed due to patients not being sufficiently stable to be moved out of the critical care environment.30 Early MRCP findings comprise of intrahepatic biliary filling defects due to accumulation of biliary casts. This subsequently progresses to diffuse biliary stricturing and dilatations with the classic beaded appearance.3 The main hallmark however of SSC-CIP that differentiates it from other potential diagnoses is that the extrahepatic biliary system is typically spared.9 MRCP and/or ERCP remain the gold standard in imaging for patients with suspected SSC-CIP.31
SSC-CIP carries with it a relatively poor prognosis; mortality rates in such patients are as high as 50% during an ICU admission, and adverse prognostic factors include associated renal failure, higher model for end-stage liver disease (MELD) scores and rapid deterioration to liver cirrhosis.30 A study by Lin et al32 revealed that 60% of patients with SSC-CIP survived ICU admission; of these, 40% developed stable biliary cirrhosis and the remaining 20% progressed to transplantation. Without transplant, median survival in such patients is 12–44 months, compared with 89 months for patients with PSC.33
Endoscopic procedures to aid biliary drainage such as sphincterotomy, balloon dilatation and stenting may bring about a transient improvement in clinical and biochemical status.4 As such, sphincterotomy and balloon trawl of sludge may have helped in our patient. Ursodeoxycholic acid has also been used to improve hyperbilirubinaemia, but its effect is somewhat limited in SSC-CIP cases.33 Importantly, however, these interventions do not affect prognosis,33 with orthoptic liver transplantation being the only cure once biliary cirrhosis is established.34 Appropriate allocation of liver transplantation is primarily based on model for end stage liver disease (MELD) or United Kingdom model for end-stage liver disease (UKELD) scoring, with 75% of patients with SSC-CIP referred within 12 months of initial diagnosis.9 Survival rates post-transplant are reassuring at 85% after 3 years.35
Learning points.
Consider secondary sclerosing cholangitis in critically ill patients (SSC-CIP) as a differential diagnosis for those critically unwell patients who have a persistent cholestasis despite clinical recovery of other organ failures.
Ultrasound imaging cannot be relied on in patients with SSC-CIP, and therefore patients require further imaging with MRCP and/or endoscopic retrograde cholangiopancreatography as gold standard.
The main hallmark of SSC-CIP that differentiates it from other potential diagnoses is that the extrahepatic biliary system is typically spared.
Prognosis is relatively poor with rapid progression to biliary cirrhosis. Endoscopic procedures for biliary drainage and ursodeoxycholic acid do not alter the prognosis.
The only cure for SSC-CIP is liver transplantation, and referral should be guided primarily by the model for end-stage liver disease (MELD) or United Kingdom model for end-stage liver disease (UKELD) scoring.
Footnotes
Twitter: @KateEd89
Contributors: KE, MA and SG participated in the management of the patient with MA undertaking the ERCPs specifically. KE and MA reviewed the literature and KE drafted the manuscript. All the authors were involved in the production of the final edit and have approved the manuscript submitted.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Martins P, Verdelho Machado M, Machado MV. Secondary sclerosing cholangitis in critically ill patients: an underdiagnosed entity. GE Port J Gastroenterol 2020;27:103–14. 10.1159/000501405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leonhardt S, Veltzke-Schlieker W, Adler A, et al. Trigger mechanisms of secondary sclerosing cholangitis in critically ill patients. Crit Care 2015;19:131. 10.1186/s13054-015-0861-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laurent L, Lemaitre C, Minello A, et al. Cholangiopathy in critically ill patients surviving beyond the intensive care period: a multicentre survey in liver units. Aliment Pharmacol Ther 2017;46:1070–6. 10.1111/apt.14367 [DOI] [PubMed] [Google Scholar]
- 4.Gelbmann CM, Rümmele P, Wimmer M, et al. Ischemic-like cholangiopathy with secondary sclerosing cholangitis in critically ill patients. Am J Gastroenterol 2007;102:1221–9. 10.1111/j.1572-0241.2007.01118.x [DOI] [PubMed] [Google Scholar]
- 5.Aronsohn A, Jensen D. Hepatobiliary manifestations of critically ill and postoperative patients. Clin Liver Dis 2011;15:183–97. 10.1016/j.cld.2010.09.004 [DOI] [PubMed] [Google Scholar]
- 6.Williamson KD, Chapman RW. Primary sclerosing cholangitis: a clinical update. Br Med Bull 2015;114:53–64. 10.1093/bmb/ldv019 [DOI] [PubMed] [Google Scholar]
- 7.Brooling J, Leal R. Secondary sclerosing cholangitis: a review of recent literature. Curr Gastroenterol Rep 2017;19:44. 10.1007/s11894-017-0583-8 [DOI] [PubMed] [Google Scholar]
- 8.Scheppach W, Druge G, Wittenberg G, et al. Sclerosing cholangitis and liver cirrhosis after extrabiliary infections: report on three cases. Crit Care Med 2001;29:438–41. 10.1097/00003246-200102000-00042 [DOI] [PubMed] [Google Scholar]
- 9.Leonhardt S, Veltzke-Schlieker W, Adler A, et al. Secondary sclerosing cholangitis in critically ill patients: clinical presentation, cholangiographic features, natural history, and outcome: a series of 16 cases. Medicine 2015;94:e2188. 10.1097/MD.0000000000002188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sakr Y, Reinhart K, Vincent J-L, et al. Does dopamine administration in shock influence outcome? results of the sepsis occurrence in acutely ill patients (soap) study. Crit Care Med 2006;34:589–97. 10.1097/01.CCM.0000201896.45809.E3 [DOI] [PubMed] [Google Scholar]
- 11.Benninger J, Grobholz R, Oeztuerk Y, et al. Sclerosing cholangitis following severe trauma: description of a remarkable disease entity with emphasis on possible pathophysiologic mechanisms. World J Gastroenterol 2005;11:4199–205. 10.3748/wjg.v11.i27.4199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meier-Hellmann A, Reinhart K, Bredle DL, et al. Epinephrine impairs splanchnic perfusion in septic shock. Crit Care Med 1997;25:399–404. 10.1097/00003246-199703000-00005 [DOI] [PubMed] [Google Scholar]
- 13.Deltenre P, Valla D-C. Ischemic cholangiopathy. J Hepatol 2006;44:806–17. 10.1016/j.jhep.2006.01.009 [DOI] [PubMed] [Google Scholar]
- 14.Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost 2020;18:1738–42. 10.1111/jth.14850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maier CL, Truong AD, Auld SC, et al. COVID-19-associated hyperviscosity: a link between inflammation and thrombophilia? The Lancet 2020;395:395:1758–9. 10.1016/S0140-6736(20)31209-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost 2020;18:1559–61. 10.1111/jth.14849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levi M, Toh CH, Thachil J, et al. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for standards in haematology. Br J Haematol 2009;145:24–33. 10.1111/j.1365-2141.2009.07600.x [DOI] [PubMed] [Google Scholar]
- 18.Bellosta R, Luzzani L, Natalini G, et al. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg 2020. 10.1016/j.jvs.2020.04.483. [Epub ahead of print: 29 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perini P, Nabulsi B, Massoni CB, et al. Acute limb ischaemia in two young, non-atherosclerotic patients with COVID-19. Lancet 2020;395:1546. 10.1016/S0140-6736(20)31051-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res 2020;220:1–13. 10.1016/j.trsl.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kirchner GI, Rümmele P. Update on sclerosing cholangitis in critically ill patients. Viszeralmedizin 2015;31:178–84. 10.1159/000431031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weig T, Schubert MI, Gruener N, et al. Abdominal obesity and prolonged prone positioning increase risk of developing sclerosing cholangitis in critically ill patients with influenza A-associated ARDS. Eur J Med Res 2012;17:30. 10.1186/2047-783X-17-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 2020;323:1574–81. 10.1001/jama.2020.5394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pan C, Chen L, Lu C, et al. Lung Recruitability in COVID-19-associated acute respiratory distress syndrome: a single-center observational study. Am J Respir Crit Care Med 2020;201:1294–7. 10.1164/rccm.202003-0527LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoekstra H, Tian Y, Jochum W, et al. Dearterialization of the liver causes intrahepatic cholestasis due to reduced bile transporter expression. Transplantation 2008;85:1159–66. 10.1097/TP.0b013e31816b2465 [DOI] [PubMed] [Google Scholar]
- 26.Beuers U, Hohenester S, de Buy Wenniger LJM, et al. The biliary HCO(3)(-) umbrella: a unifying hypothesis on pathogenetic and therapeutic aspects of fibrosing cholangiopathies. Hepatology 2010;52:1489–96. 10.1002/hep.23810 [DOI] [PubMed] [Google Scholar]
- 27.Spirlì C, Nathanson MH, Fiorotto R, et al. Proinflammatory cytokines inhibit secretion in rat bile duct epithelium. Gastroenterology 2001;121:156–69. 10.1053/gast.2001.25516 [DOI] [PubMed] [Google Scholar]
- 28.McGonagle D, Sharif K, O'Regan A, et al. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev 2020;19:102537. 10.1016/j.autrev.2020.102537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weiss KE, Willmann JK, Jeffrey RB, et al. Secondary sclerosing cholangitis in a critically ill patient. Quant Imaging Med Surg 2016;6:224–8. 10.21037/qims.2016.04.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Voigtländer T, Negm AA, Schneider AS, et al. Secondary sclerosing cholangitis in critically ill patients: model of end-stage liver disease score and renal function predict outcome. Endoscopy 2012;44:1055–8. 10.1055/s-0032-1325733 [DOI] [PubMed] [Google Scholar]
- 31.Schade I, Radakovic D, Hoffmann J, et al. Secondary sclerosing cholangitis in cardiac surgical patients: a complication with a dismal prognosis. J Thorac Cardiovasc Surg 2017;154:906–12. 10.1016/j.jtcvs.2017.04.041 [DOI] [PubMed] [Google Scholar]
- 32.Lin T, Qu K, Xu X, et al. Sclerosing cholangitis in critically ill patients: an important and easily ignored problem based on a German experience. Front Med 2014;8:118–26. 10.1007/s11684-014-0306-6 [DOI] [PubMed] [Google Scholar]
- 33.Kulaksiz H, Heuberger D, Engler S, et al. Poor outcome in progressive sclerosing cholangitis after septic shock. Endoscopy 2008;40:214–8. 10.1055/s-2007-967024 [DOI] [PubMed] [Google Scholar]
- 34.Engler S, Elsing C, Flechtenmacher C, et al. Progressive sclerosing cholangitis after septic shock: a new variant of vanishing bile duct disorders. Gut 2003;52:688–93. 10.1136/gut.52.5.688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Voigtländer T, Jaeckel E, Lehner F, et al. Liver transplantation for critically ill patients with secondary sclerosing cholangitis: outcome and complications. Liver Transpl 2015;21:1295–9. 10.1002/lt.24192 [DOI] [PubMed] [Google Scholar]