Abstract
Aim:
To evaluate the survival rate, tissue response, and patient satisfaction of different attachments used in implant overdenture.
Settings and Design:
Systematic Review and Meta-analysis.
Materials and Methods:
Electronic search of peer-review articles published between 2001 and 2019 assessing the attachments used for implant-supported overdentures was done according to PRISMA Guidelies. The review evaluated sixteen articles related to survival of the attachments, the reaction of the soft and hard tissues along with repair and maintenance of the attachments, and overall performance of the overdenture attachments.
Statistical Analysis Used:
There is statistically significant heterogeneity (Q =374.7403, df = 15, and P < 0.0001). The statistics of fixed-effect model reported an MD of − 0.0880 (95% CI = −0.1536; 0.0225).
Result:
The review evaluated the 16 articles that met with the inclusion and search criteria. The studies were the combination of bar and ball attachments and their subtypes, magnetic and bar attachments, and locator in combination with other attachments. The meta-analysis of combined 16 studies reported acceptable heterogeneity among 16 studies (I 2 = 96%) and reported to be statistically significant (P < 0.01).
Conclusion:
The survival rate of attachments was in the range of 95.8%–97.5% for bar, 96.2%–100% for ball, 90%–92% for magnet and locator attachments were in the range of 97% after a mean follow-up period of 3 years. The bar attachments reported moderate tissue reaction in the form of mucosal changes, gingival inflammation, and bone resorption. The locator attachments require higher maintenance and repair. The magnetic attachments produce higher bone resorption and readily displace under functional force. Patient satisfaction and compliance was higher for ball, locator, and bar attachments as well as low for magnetic attachment. Thus, the ball and locator attachments excellently perform in terms of survival rate, tissue response, and patient satisfaction.
Keywords: ”O” ring attachment, ball and bar, implant-supported overdenture, locator attachment, overdenture attachments
INTRODUCTION
Implant-supported attachment overdenture is the most advanced treatment as the attachments secure the retention and improve the masticatory efficiency and overall performance of the complete denture.[1,2,3]
Tooth-supported dentures have certain inaccuracies due to the strategic location of the abutment tooth, hard and soft tissues supporting the abutment, angulation of the abutment teeth, and presence of the existing caries and attachment loss and type of maxillomandibular relation. The selection of attachments is totally dependent on the support and angulation of the abutment.[4,5] However, tooth-supported denture still provide better support in the guarded prognosis case as it has its periodontal proprioception.[6] In case of implant-supported overdenture, the implant provides rigid and stable support to the overdenture attachment. The location, selection, angulation, and placement are not significant problems as there are wide varieties of attachments available in relation to the width, diameter, and length of the implant. The implant-supported overdenture has a scope of specific selection and customization of the attachments in relation to the ridge contour and the type of force (axial and/or nonaxial force).[2,3]
Retrospectively, the attachment concept was in practice since the 1960s, with the bar and ball attachments being the first ones and were proven both clinically predictable and effective by Mericske-Stern et al. in 1997.[7] The locator attachments were introduced in 2001 (Zest Anchors, Inc., homepage, Escondido, CA, USA).[8] Progressively, attachments were much popular due to their inherent ability to enhance retention and stability of the complete denture.[9] The absolute retentive capacity of overdenture attachments was reported by Wismeijer et al. (1999)[10] and Epstein et al.[11] The resiliency of the attachments in relation to stress dissipation was suggested by Leung and Preiskel.[12] Petropoulos et al.[13] defined the “release period” as the time required for the attachment system to lose retention or disengage from the abutment during forced separation, indicating the clinical significance of retention and stability of the prosthesis under function. According to retentive means, the attachments can be classified into 1) frictional, 2) mechanical, 3)frictional-mechanical and 4) magnetic attachments.[14] They can be rigid or resilient based on the type of movement.
There are several attachments used for implant-supported overdenture, which includes studs, bar, bar with clip, bar with coping, recently “O” ring attachment, and locator attachment (Zest Anchors, Inc., homepage, Escondido, CA, USA). All attachments produce excellent retention, stability, and support; however, the survival is the most valuable criterion for the long-term prognosis, hence the follow-up is crucial to study the behavior of attachments under axial and nonaxial forces. Tissue response, peri-implant mucosal changes, bone resorption, and loss of attachment indirectly assess the survival of attachment. Eventual patient response in terms of compliance in placement and removal of the prosthesis, oral hygiene, and overall satisfaction are the most significant criteria for evaluation of the success of the attachments.
Eventually, the success of the overdenture attachment depends on the selection of the attachment-related factors that simulate the clinical situation. The factors that govern the selection of attachment are based on proper diagnosis of intraoral structures and various factors such as bone type, inter-arch space, cost-effectiveness, amount of retention needed, expected level of oral hygiene, amount of available bone, patient's social status, patient's expectation, maxilla–mandibular relationship, inter-implant distance, and status of the antagonistic jaw.[15] The primary objective of the systematic review and meta-analysis is to study the survival rate, tissue response, and patient satisfaction of different attachments used in implant overdenture.
METHODS
This systematic review was designed according to the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement.[16,17]
Study protocol
Before the start of the systematic review, a protocol was developed and registered (Prospero ID: 163013) aiming to answer the P.I.C.O. question that rendered the following P.I.C.O. definitions:
Population: Patients, older than 18 years and in good general health, with complete edentulism requiring placement of implant-supported overdentures in either one or both the arches
Interventions: Any attachment designed for implant-supported overdentures. The attachments used were ball, bar, ball-bar, magnetic, locator, ERA, Dalla Bona, conus, and combinations of various attachments
Comparison: Attachments were compared with the objective of evaluating various attachments and their combinations on the basis of survival rate, tissue response, and patient satisfaction
Outcomes: Primary outcomes was the survival rate of the attachments with various follow-up periods, maintenance visits by the patients, tissue response evaluated both clinically as well as radiographically, patient satisfaction using Visual Analog Scales (VAS) whereas Retention, stability, support were the additional outcomes.
Study design
A combination of in vivo studies involving either or both the arches, comparative prospective and retrospective case–control studies, and randomized clinical trials were included.
Exclusion criteria
Review articles on the topic
Studies with partially edentulous subjects with implant supported prosthesis
Preclinical studies in animal models
In vitro studies
Articles published in a different language than English.
Search strategy
Three electronic databases were used as sources in the search for studies satisfying the inclusion criteria: (a) The National Library of Medicine (MEDLINE via Pubmed); (b) Google Scholar; and (c) Cochrane library. These databases were searched for studies published until June 2019. Keywords used were: Overdenture, implant supported denture, precision attachment denture, and dental implant. Two independent investigators performed the study selection. Data extraction was performed independently by two investigators, and duplicates were removed using Mendeley and thereafter discussed to find an agreement. All reference lists of the selected studies were checked for cross-references. In addition, the following journals were hand-searched from the years 2001 to 2019: Journal of Prosthetic Dentistry, Journal of British Dental Association, Journal of Oral Implantology, The International Journal of Oral and Maxillofacial Implants, The International Journal of Prosthodontics, and Journal of Advanced Prosthodontics. Related articles were identified from the existing reviews and study design (networking meta-analysis) PICOS framework [Table 1].
Table 1.
Patient or population, intervention, comparison, outcome, study type table
| PICOS | |
|---|---|
| P (patient or population) | Completely edentulous subjects |
| I (intervention) | Implant supported overdenture in maxillary or mandibular arch with various attachments |
| C (comparison) | Attachments were compared with the objective of evaluating various attachments and their combinations on the basis of survival rate, tissue response and patient satisfaction |
| O (outcome) | The survival rate of the attachments with various follow-up periods and the requirement of maintenance visits by the patients, tissue response evaluated both clinically as well as radiographically, patient satisfaction using VASs were considered as primary outcomes whereas Retention, stability, support were the secondary outcomes |
| S (study type) | A combination of in vivo studies involving either or both the arches, comparative prospective and retrospective case control studies and randomized clinical trials were included |
VAS: Visual analog scale
Eligibility
The initial phase is the primary screening of the identified articles. Due to the broad nature of the initial search, references were further filtered according to title, abstract, and keyword. Following the initial search, a reference list of the retrieved articles was manually searched for additional articles that met the inclusion criteria. Additionally, authors and keywords were searched again in Google Scholar to ensure that all relevant articles were uncovered.
Inclusion criteria
Peer-reviewed articles published between January 2001 and June 2019
Studies that discuss the use of attachments in implant-supported overdentures in relation to survival rates of various attachments for varied follow-up periods
Studies that discuss the comparison between tissue response considering the clinical and radiographic findings
Studies that discuss the patient compliance and satisfaction with various attachment retained implant-supported overdentures.
Quality assessment
The risk of bias was assessed using the Cochrane Collaboration tool. The selected articles were assessed by the first author, and any variant view of selected articles was further assessed by the second author. The randomized controlled trial studies were evaluated using the following domains: random sequence generation, allocation concealment, blinding of the participant and personal blinding of the outcome assessment, incomplete outcome data, selective outcome reporting, and other bias. The studies were rated further as a risk of bias (low, medium, and high) by the reviewers.
Data management
Data extraction was independently done by two reviewers using the specific format. The specific information was as follows: year of publication, baseline data, study population, diagnostic tool, various available attachments, and follow-up period.
Tools for measuring outcomes: 1)clinical performance was evaluated by scanning electron-microscope, hardness and elastic modulus of attachment systems; 2) fatigue resistance of attachments was measured by strain gauge; 3) Clinical and radiographic evaluation of peri-implant parameters include plaque and bleeding on probing index and marginal bone loss; 4) cumulative survival rates on overall performance and 5)Questionnaires to assess patient satisfaction (OHIP (Oral Health Impact Profile) and VAS (Visual Analog Scale)).
The outcomes were presented for relevant studies in a graphical format where possible. The studies were graphed according to the mean difference (MD) with the level of significance at P < 0.01. In the meta-analysis, heterogeneity was measured as a final calculation of effect size and the confidence interval (CI) around that effect size was calculated by using random-effects and fixed-effects models in the forest plot.
Data analysis
The statistical heterogeneity among studies was assessed using the Q test based on Chi-square statistics (Cochran, 1954) as well as the I2 index[18] in order to know the percentage of variation in the global estimate that was attributable to heterogeneity (I2 = 25%: low; I2 = 50%: moderate; and I2 = 75%: high heterogeneity).
To summarize and compare studies, the mean values of primary (the survival rate of the attachments with various follow-up periods and the requirement of maintenance visits by the patients, tissue response evaluated both clinically and radiographically, and patient satisfaction using VAS) and secondary quantitative outcomes (retention, stability, and support) were directly pooled and analyzed with weighted MDs and 95% CIs. In the case of dichotomous outcome (exposure events), the estimates of the effect were expressed in risk ratios and 95% CIs. Study-specific estimates were pooled with both the fixed- and random-effect models. The publication bias was evaluated using the Begg's and Egger's tests for small-study effects for the main outcome variable.
RESULTS
Study characteristics
The review identified 1360 articles. A review of 89 full-text articles identified 45 articles for qualitative synthesis and 28 articles that met the inclusion criteria, search criteria, and confidence in implant-supported overdenture cases [Figure 1]. A total of 44 articles were excluded from the study with subsequent reason: the studies that were not peer reviewed and the studies that show very less information about the attachment in relation to retentive force, survival under complex axial or nonaxial force, simplicity in use, and outcome of the attachment (inter-reader agreement = 93.02%; kappa = 0.85, P < 0.001; 95%CI: 0.77; 0.98). The articles were distributed according to (1) The clinical and radiographic evaluation of the attachments used in implant-supported overdentures and randomized clinical trials. Finally, a total of 16 studies were evaluated for meta-analysis, out of that six are prospective case–control or comparative analysis, one is retrospective comparative analysis, and nine are randomized clinical trials.
Figure 1.
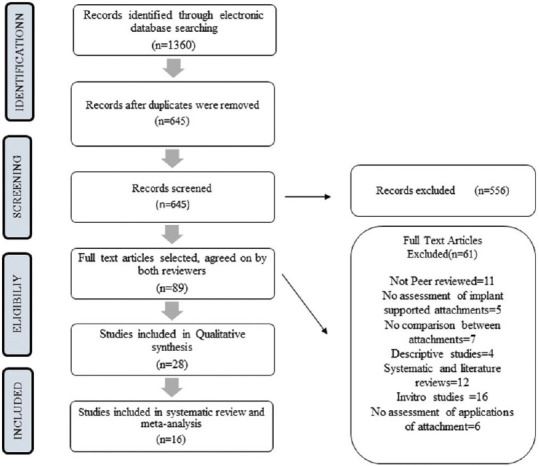
Preferred Reporting Items for Systematic Review and Meta-Analysis flowchart
Quality assessment of the included studies
In Table 2, the results of the quality assessment are summarized. Six studies of the included studies were designed as randomised controlled trials (RCTs). Three studies had a crossover clinical trial design. Five were prospective case–control studies, one was a comparative analysis, and another one was a retrospective case–control study. In addition, follow-up data were provided in all the 16 studies. The full checklist (Cochrane Collaboration's tool for assessing the risk of bias) was applied for RCTs and clinical crossover trials. Six studies were considered as low and three as unclear risk of bias.
Table 2.
Risk of bias assessment of randomized controlled trials
| Study | Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blinding of participant (performance bias) | Blinding of personnel (personal bias) | Blinding outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Other bias |
|---|---|---|---|---|---|---|---|
| Macentee (2005) | |||||||
| Christache CM (2009) | |||||||
| Cune (2009) | |||||||
| Kappel S (2015) | |||||||
| Cepa S (2016) | |||||||
| Albuquerque RFD (2018) | |||||||
| Boven GC (2019) | |||||||
| Park JS (2019) | |||||||
| Taha NEKS (2019) | |||||||
| High risk of bias | |||||||
| Unclear risk of bias | |||||||
| Low risk of bias | |||||||
Included studies
The 16 publications meeting the inclusion criteria described randomized controlled trials (n = 6), crossover clinical trials (n = 3), prospective case–controls (n = 5), comparative analysis (n = 1), and retrospective case–control (n = 1). Publication dates ranged between 2001 and 2019. Overall, 917 patients with a mean age of 62.15 years had been treated with 2390 dental implants. The dropout rate ranged between 0% and 20.6%, resulting in a total number of 734 patients providing data for the primary outcome. The observation period ranged between 3 months and 10 years. 43 implants were lost, resulting in a cumulative implant survival rate of 98.2%.
Meta-analysi
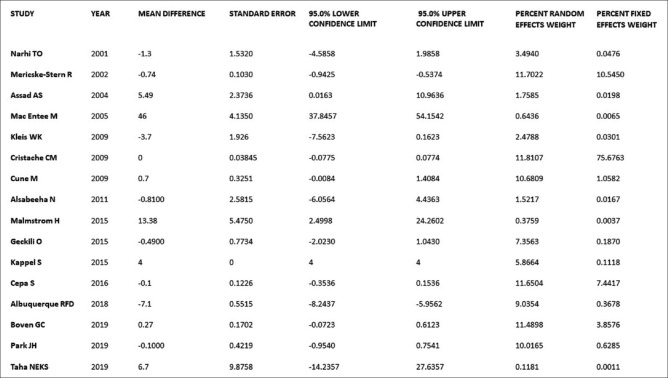
The meta-analysis as shown in Figures 2-5 was performed by combining the results of 16 studies by using fixed- and random-effect meta-analysis, with an overall acceptable heterogeneity among the studies (I2 = 96%). The result of various attachments used in implant-supported overdenture reported statistically significant heterogeneity (Q = 374.7403, df = 15, and P < 0.0001). The statistics of fixed-effect model reported an MD of − 0.0880 (95% CI = −0.1536; −0.0225). The random-effect model reported an MD of − 0.1440 (95% CI − 0.8126–0.5247) [Figures 2-5]. The combined results of 16 studies reported to be statistically significant (P < 0.01). The studies related to ball attachments show significant values of retention, survival, and overall performance and the bar attachments produce moderate tissue changes and bone resorption. The locator attachments require constant maintenance and repair. The magnetic attachments reported higher bone resorption under functional force. The evaluation of the funnel plot as per Graph 1 reported no asymmetry as only a small amount of studies are included, publication bias is unlikely to be present. Summarization of all the studies included is given in Table 3 and outcome is presented in Graph 2.
Figure 2.
Data for the forest plot of meta-analysis
Figure 5.
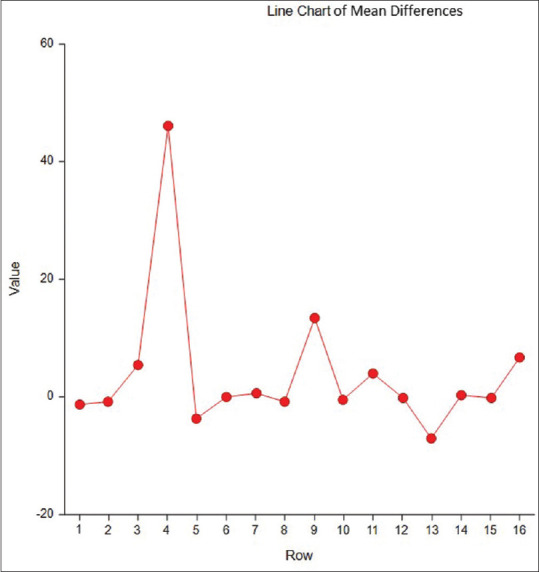
Line chart of mean differences
Graph 1.
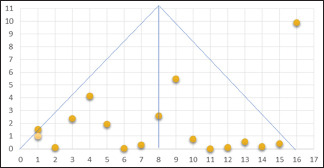
Funnel plot for publication bias
Table 3.
Summarization of all the studies included in meta-analysis
| References | Age of patients | Number of implants | Follow-up | Objective parameters | Type of study | Sample size | Intervention | Primary end point | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Narhi TO (2001) Finland | Not reported | 2-6 (Branemark, IMZ, Dyna) | 72 months cumulative | Clinical examination and interview | In vivo-retrospective comparative analysis | Bar group: 11 Ball group: 5 | Bar and ball attachments | The cumulative survival rate for the implants after 72 months was 90%. Loss of bone support correlated with peri-implant probing depth (r=0.29; P<0.02). No differences in mean bone loss between the subjects with ball-retained or bar-retained overdentures were found. The presence of plaque or peri-implant bleeding was not associated with the type of attachment | More mucosal changes were seen with bar superstructures. However, an increased possibility of peri-implant bone loss should be considered when un-splinted implants are used |
| Mericske-Stern R (2002) Switzerland | 40-89 years | 4-6 screw-type ITI implants (Straumann, Waldenburg, Switzerland), well spaced, in the anterior part of the maxilla | 1-9 years average=4.1 years | Peri-implant parameters: plaque index, bleeding index, probing attachment level, radiographic distance, crestal bone level on radiograph | In vivo prospective case-control | Baseline sample: 173 After loading: 173 | Dolder bar, ball anchors or telescopic copings | The 5-year cumulative survival rate of all implants was 94.2%. The peri-implant parameters gave evidence of healthy soft tissues and good oral hygiene. The increase in probing depths and attachment loss were significant (P<0.05). The mean marginal crestal bone loss was about 0.7 mm and was statistically significant at mesial and distal sites (P<0.001). | In planned maxillary overdenture treatment, it is possible to achieve a satisfactory survival rate of the implants |
| Assad AS (2004) Egypt | 48-60 years | 2 (Dyna Dental Implant; Dyna Dental Engineering, Bergen op Zoom, The Netherlands) with 13 mm length and 3.6 mm diameter | 6 months, 12 months, 18 months | Clinical evaluation Implant mobility Pocket depth (sensor probe on 4 surfaces) Gingival index by Loe and Silness Plaque index Radiographic evaluation Marginal bone height Bone density | In vivo comparative analysis | Magnetic group: 5 Bar group: 5 | Magnetic (mucosa supported) and bar (mucosa-implant supported) | Plaque index was significantly high in magnetic group, After 18 months bar supported showed significant increase in gingival inflammation | Mucosa supported (magnetic) overdentures showed less bone resorption distal to implants as compared to bar type. Both the attachments lead to increased functional load and hence affect bone density and resorption |
| Macentee M (2005) Vancouver , Canada | Average: 61-63 years | 2 Nobel Biocare, Canada Inc. Richmond Hill, Ontario, Canada | 1 month, 1 year, 2 years, 3 years | Patient satisfaction using 100 mm VAS | Randomized control trial (In vivo) | Baseline group: 100 Attachment group: 100 | Bar clip, ball/spring | Over 3 years of follow up, mean numbers of repairs per subject differed significantly between groups, 6.7 repairs in ball spring group, compared to 0.8 in bar clip group (P<0.001) | Subjects were satisfied with new dentures. However, ball-spring attachments required more repairs |
| Kleis WK (2009) Germany | 46-95 years | 2 Osseotite® TGStandard implants (BIOMET3iImplant Innovations, Palm Beach Gardens, FL, USA) | 12 months | OHIP-G 49 survey for patient satisfaction | In vivo prospective case control | Self-aligning locator group: 25 Traditional ball group: 31 | Self-aligning locator, traditional ball attachment | After 1-year of clinical service, locator had 34 prosthetic complications especially the need for change of the male parts or activation because of loss of retention and TG-O ring had 14 prosthetic complications, most of them the change of the O-rings. Dal-Ro abutment had 7 minor complications | Prosthodontic maintenance was restricted to loss of retention for all systems. Locator shows higher rate of maintenance |
| Cristache CM (2009) Bucharest, Romania | 42-84 years | 2 Screw Type Standard Straumann Implants (Institut Straumann Ag, Basel, Switzerland) | 5 years | Gingival index, plaque index, calculus, bleeding index, probing pocket depth, implant stability, radiographic outcome, prosthetic maintenance, complications and patient satisfaction | Randomized control trial | Ball attachment group (B): 23 Magnetic group (M):23 | Retentive anchors (ball attachments) and magnets | The mean bone loss in the 1st year for B group 0.51±0.20 and in M group was 0.51±0.19, and the annual bone loss from 1 to 5 years was 0.05 for both the attachments | With the low initial cost of treatment in B group require high maintenance cost as compared to the M group, initial high cost and low maintenance cost. Both the attachments function well after 5 years |
| Cune M (2009) Netherland | 33-56 years | 2 (F Rialit 2, Friadent) | 10 years | VAS for patient satisfaction, marginal probing depths, bleeding index and radiographic marginal bone loss were assessed | Crossover clinical trial | Ball group: 7 Bar group: 7 | Ball socket attachment: Frialit-2 Friadent Bar- clip, round bar in conjunction with metal omega shaped IMZ clip, Friadent | The differences in the mean scale and VAS scores did not reach a statistically significant level neither at the initial or after 10 years | The probing depth for ball attachments were quite shallower than that of the bar group |
| Alsabeeha N (2011) New Zealand | Not reported | 1 | 1 year | Mechanical testing: Hardness and elastic modulus measured using nanoindentation technique Clinical performance: Prosthodontic maintenance events Scanning electron microscope | In vivo prospective case control | Ball attachment group: 24 Locator group: 12 | Large ball attachment, Standard 2.25 ball attachment, locator attachment | The titanium nitride-coated particles, regardless of system, appeared unchanged and did not require any maintenance. Extensive wear was evident in the uncoated titanium alloy particles and Dalla Bona-type gold alloy matrices, resulting in high maintenance (15 activations). Minimal wear was observed in the plastic matrices with minimal maintenance (2 replacements). The locator nylon matrices showed extensive deformation and deterioration with a substantial need for maintenance (16 replacements). | Large ball attachment systems of titanium nitride-coated particles and plastic matrices reflect favorable wear behavior and clinical performance. These attachments are recommended for patients receiving mandibular single-implant overdentures |
| The performance of the particles was related to hardness, while that of the matrices was related to the creep response | |||||||||
| Malmstrom H (2015) Rochester, New York | 18 years or older | 2 Zimmer Tapered Screw-Vent implants (Zimmer Dental Inc, Carlsbad, Calif; 3.75 mm in diameter, 11 mm or 13 mm in length) were placed at intraforaminal area at either the canine or lateral incisor location | 2 weeks, 3 months, 1 year, 2 years | To determine the implant success: 1. Gingival index by Loe and Silness, 2. Plaque index, 3. Pocket depths at 6 sites, 4. Mobility measured manually, 5. Bone loss on radiographs Overdenture prosthesis Evaluation: Stability, retention and esthetics on a scale of 0 to 10 Patient satisfaction: VAS scale of 100 mm | In vivo prospective case-control | Baseline: 45 Locator group: 45 | Locator attachment (median force pink locator male) | Though there was 11% incidence of replacement of locator male in 2 years, the subjects’ overall satisfaction with fit and ability to chew hard foods with their mandibular overdentures improved significantly (P<0.05) following the denture attachment to the dental implants | 97.7% success rate |
| Geckili O (2015) Istanbul, Turkey | 55-72 years | 2 (Astra Tech) | 6 months, 1 year, 2 years | Measurement of momentary retention forces using dynamic testing machine Patient satisfaction and quality of life 100 mm VAS questionnaire and OHIP-14. | In vivo prospective case-control | Momentary retentive force group: 55 Patient satisfaction group: 55 | Ball or locator attachments | No statistically significant association between momentary retention forces and VAS scores (P>0.05). But, higher retention forces presented significantly better quality of life, OHIP score 14 (P<0.05) | Higher retention surely provides better quality of life, it doesn’t affect patient satisfaction |
| Kappel S (2015) Heidelberg, Germany | Mean age: 73.4 years | 2 (BEGO Semados®, BEGO Implant GmbH and Co. KG, Bremen, Germany). | 3, 6, 12, 24 months | Implant survival was defined on the basis of clinical stability, plaque index gingival index, radiographic marginal bone loss analysis, prosthetic complication and patient satisfaction using VAS | Randomized clinical study | Bar group: 23 Locator group: 23 | Dolder bar and locator | Marginal bone loss after 2 years for locator was 6 mm at both mesial as well as distal surface and 10 mm for bar attachment | Survival was 89.1% and 93.5% for the bar and locator groups, respectively. Survival of the original dentures was 93.5% and 95.7% for the bar and locator groups, respectively |
| Cepa S (2016) Riegel, Germany | Mean age: 65.2 years | 2 (Ankylos, Dentsply Implants, Mannheim, Germany | 1, 2, 3 years | Bleeding index, modified plaque index, gingival index, probing depth, radiographic evaluation of marginal bone loss | Randomized clinical trial | Ball group: 12 conus Group: 13 | Ball attachments (Ankylos ball heads, Dentsply implants, Mannheim, Germany) or prefabricated conus attachments (Ankylos SynCone, Dentsply Implants, Mannheim, Germany) were used for prosthesis retention` | Compared to the conus group (0.97, 0.66), the mean Modified Plaque Index of the ball attachments (0.39±0.39) was significantly lower (P=0.024) at baseline | Patient satisfaction was 64% for the ball- and 100% for the conus-retained IODs. For the conical attachment, the recommendation of the manufacturer is to use four interforaminal implants to support a removable prostheses |
| Albuquerque RFD (2018) São Paulo, Brazil | Mean age: 73.2 | 2 regular tissue-level 4.8 mm diameter Straumann implants in the canine regions of the mandible, conventionally loaded | 1 week, and 3, 6, and 12 months | Attachment retention as minimum tensile load, 100 mm VAS questionnaire for patients response | Randomized crossover clinical trial | Ball group (RA): 12 Locator group (LA): 12 | Ball attachments (retentive anchor, ref. 048.439, Straumann, Basel, Switzerland) with gold matrices. cylindrical attachment system (LA - Locator, Zest Anchors Inc., Escondido, CA) | Mean retention of worn attachments and patient satisfaction with denture retention assessed in the preintervention phase were 3.2 N (SD 4.9) and 23.5 mm (IQR 6.5-65.5), respectively. Overall mean retention along the study was higher for RA than LA (difference of 5.0 N, 95% CI: 2.5-7.6; P=0.0005), declining significantly overtime (P<0.0001), more steeply for the cylindrical attachment | Ratings of retention decreased significantly overtime for both systems and earlier for LA than RA. Satisfaction was lower when retention was either too low or too high, although there was large variation in this association. At the end of the study, all participants chose to remain with the attachment system that they had received last |
| Boven GC (2019) Netherland | Mean age: 60.1-63.8 years | 4 dental implants 3.5 mm in diameter (Nobel Active Narrow Platform, Nobel Biocare AB, Gothenburg, Sweden) in maxilla | 1 year | Radiographic bone level, implant survival, overdenture survival, peri-implant hygiene, soft tissue conditions, and patient satisfaction | Randomized clinical trial | Bar group: 25 Locator group: 25 | Bar (Nobel Biocare AB), locator attachment | Marginal bone loss was estimated 0.58±0.71 for locators and 0.31±0.47 for bar group over 1 year | Implant survival was 96.7% in locator group and 97.9% in bar group |
| Park JH (2019) Seoul, Korea | Mean age 61.6±10.6 | 4 roughened surface dental implants (NRline®, Dentium) 3.1-5.0 mm in diameter and 7-13 mm in length were placed in each anterior maxilla | 1 year | PI, BOP and GI and were assessed at definitive denture delivery (T0) and at 3 months (T3) and 12 months (T12) after definitive prosthesis delivery | Randomized control trial | Bar group: 20 Ball group: 20 | a bar group (Hader bar, Preci-Horix, Alphadent NV) and a ball group (Mini-ball attachment, Dentium | The mean marginal bone loss after 1 year of loading was 0.34±0.88 mm, and there were no significant differences between the two groups. Plaque index, gingival index and bleeding on probing were significantly higher in the bar group (P<0.001), and the implant success rate of the bar group was significantly lower than that of the ball group (P=0.028) | The bar group was more vulnerable than the ball group with respect to maintaining peri-implant tissue health |
| Taha NEKS (2019) Goiania, Brazil | Not reported | A cylindrical Morse taper implant (TitamaxCM Cortical, NeodentImplants), 3.75 mm diameter, was inserted in the mandible midline, 1-2 mm infrabony | 1 week, 3 months | Patient satisfaction with the mandibular denture according to six items: comfort, speech, chewing ability, retention, stability and overall satisfaction. Each item was measured as scored by the patient in a VAS ranging from 0 to 100 | Randomized cross over clinical trial | Ball group: 9 Equator group: 9 | The ball-type attachment (Bola Mini CM, Neodent Implants) The “stud” type Equator attachment (Equator CM, Neodent Implants) | No significant differences were observed when comparing the ball and Equator at the initial (P=0.330) and final (P=0.08) periods | The use of a single midline implant to retain a mandibular overdenture significantly improves patient satisfaction irrespective of the attachment used |
VAS: Visual analogue scale, PI: Plaque index, BOP: Bleeding on probing, GI: Gingival index, SD: Standard deviation, CI: Confidence interval, OHIP: Oral Health Impact Profile, IMZ: Intramobile Cylinder Implant System, RA: Retentive Anchors for ball attachment group, LA: Locator Attachment group
Graph 2.
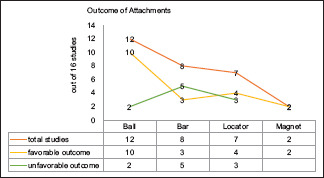
Outcome of attachments
Figure 3.
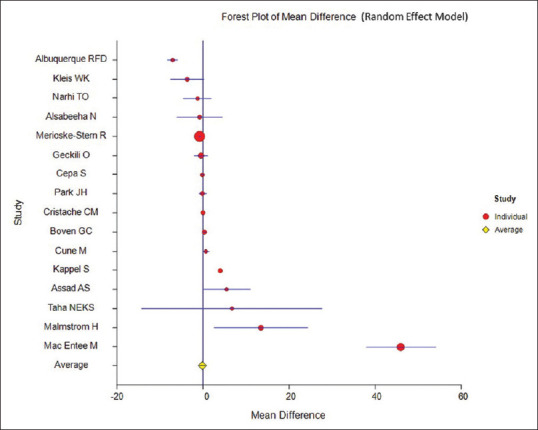
Forest plot of mean differences (random-effects model)
Figure 4.
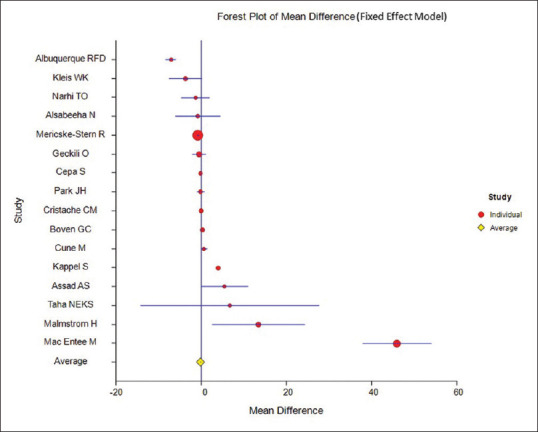
Forest plot of mean differences (fixed-effects model)
DISCUSSION
This systematic review and meta-analysis identified 16 studies that gave maximum comparable outcome and follow-up results, out of which nine were randomized and crossover clinical trials. The most commonly used attachments in all the studies were the ball attachments followed by bar, locator, magnet, conus and equator, and various combinations.
Twelve studies reported the significance of ball attachment. The mean bone loss in the 1st year for ball group (0.51 ± 0.20) was comparable with magnetic attachment.[19] The larger diameter ball attachment reported less replacement than locator attachment.[20] The combined effect of ball and locator attachment results in higher retention that surely provides better quality of life.[21] A randomized crossover clinical trial stated that the overall mean retention was higher for retentive anchors than locator attachments (difference of 5.0 N, 95% CI: 2.5–7.6; P = 0.0005); the patients preferred the attachments that were delivered the last.[22] Patient satisfaction was 64% for the ball and 100% for the conus-retained implant overdentures.[23] The probing depth for ball attachments was quite shallower than that of the bar group and showed excellent peri-implant tissue response as reported by a crossover clinical trial.[24] Eight studies evaluated and compared the significance of bar attachments. The bar attachment has an excellent 5-year survival rate, i.e., 94.2%.[25] However, the bar attachment reported mucosal changes, gingival inflammation, and bone resorption under functional load.[26,27] Plaque index was significantly high in magnetic group initially, but after 18 months, bar–supported group showed significant increase in gingival inflammation. The follow-up repair and maintenance of the bar attachment was significantly low (0.8/individual).[28] Survival was 89.1% for the bar and 93.5% for locator groups (marginal bone loss: 6 mm).[29] Implant survival was 96.7% in the locator group and 97.9% in the bar group.[30] Thus, the bar group was more vulnerable than the ball group with respect to maintaining peri-implant tissue health as compared to all the attachments. There are seven studies reporting the significance of locator attachment. One year observational study that evaluated the wear pattern of locator attachments using scanning electron microscope reported 16 replacements of locator housing and 34 prosthetic complications.[20,31] Locator attachments reported a 97.7% success rate and 11% incidence of replacement of locator male among 50 subjects in 2 years of treatment period.[32] Marginal bone loss was estimated at 0.58 ± 0.71 after 1 year and up to 6 mm after 2 years for locators and 0.31 ± 0.47 after 1 year and up to 10 mm after 2 years for bar group.[29,30] The two studies reported the significance of magnetic attachment. The magnetic attachment reported more plaque retention, high bone resorption under functional force, and high displacement in all directions as compared to bar attachment.[27]
Out of the total nine randomized and crossover clinical trials included in the review, eight studies compared ball attachments with other attachments such as bar, magnet, locators, conus, and equators and reported that ball attachments require 6.7 repairs in 3 years,[28] has high maintenance cost,[19] show shallower probing depths even after 10 years of use[24] and a modified plaque index of the (0.39 ± 0.39) lowest in 3 years.[23] Thus, the ball attachments fair well with the highest retention values and lowest peri-implant inflammation but high maintenance visits.[33,34] One of the randomized controlled trials compared ball and locator, of which bar group showed lower marginal bone loss and a slightly higher survival rate as compared to locators.[30] Extensive studies should be done with a long-term follow-up and maintenance data for the new emerging locator attachments as they can be a breakthrough treatment of choice.
The meta-analysis of the four studies reported the survival rate of maxillary implant-supported overdenture.[25,26,30,33] Mericske Stern et al. reported that there is minimum requirement of 4–6 implants to achieve 94.2% of cumulative survival rate with 5-year follow-up period.[25] In regards of maxillary arch, there is a definite requirement of 4–6 implants along with bar attachment[26,30,33] in order to distributes the stresses more on multiple attachment, thereby it improves the cross-arch stabilization for maxillary overdenture.[25] However, use of fewer implant (< 4 implants) increases the peri-implant mucosal changes and patient compliance in terms of oral hygiene maintenance are potent risk factors for failure of maxillary implant-supported overdentures.[33,35,36] The fixed restoration is more logical treatment of choice than overdenture when the situation dictates the use of 4–6 implants for maxillary overdenture,[26] as addition of two or more implant or use of zygomatic implant or angular implant favors fixed restorations than overdenture. The current scenario of zygomatic implant. The current scenario of zygomatic implant with anterior two implants or zygomatic Quad implant reported a survival rate of 97.4% over 7 years for fixed restorations.[37] Similarly, combinations of axial and angular implant showed comparable survival rates. The angled implants had an overall success rate of 96.5% and the straight implants had a 97% success rate for 1–12 years with fixed restorations.[38] The current concept of 6–8 short implant (4–6 mm length, depends on the availability of space) reported similar survival rate (pooled cumulative survival rate of 99.060% for 1845 implants after a mean follow-up of 3.2 ± 1.7 in posterior maxilla)[39] to long conventional implant with augmentation of bone along with lateral sinus floor elevation. The advantage of short implant is that it completely eliminates the donor site morbidity as no grafting procedure is required, which is used for the traditional conventional implant. The use of short implant reduces the treatment time as grafting procedure of autogenous bone graft needs minimum 6 months to 1-year healing time before the placement of conventional long implant, and there is no contact of removable prosthesis to grafting site during healing time.[39] Hence, it can be concluded that fixed restoration is the logical choice instead of overdenture for the rehabilitation of maxillary arch. However, the cost of the zygomatic implant placement or conventional implant with bone grafting is higher than that of the implant-supported overdenture, but with the use of short or angular implant, the cost of the fixed restorations is almost equal to the combined cost of implant, attachment, and the denture.[37,40,41] In the similar situation of mandibular arch, only two to four implants with adequate attachment are sufficient to provide support, stability, and retention for mandibular denture provided the support of the residual ridge is sufficient in terms of height and width. Bhargava et al. proposed the classification for mandibular implant-supported overdenture on the basis of inter-foramina distance (IFD) and available vertical restorative space (AVRS).[42] The practical advantage of the classification is the safe distance for implant placement and attachment selection. The classification is divided into three classes, i.e., Class I, Class II, and Class III. Class I: the Class I has two subtypes of class Ia (IFD >40 mm and AVRS >14 mm) and Class Ib (IFD 30–40 mm and AVRS >14 mm). The class Ia advises five or fewer implants with bar and clip attachment or bar and locator attachment and Class Ib advises four or fewer implants with bar and clip or ball and locator attachment. Class II: the Class II has similar subtypes such as Class II: Class IIa (IFD >30 mm and AVRS 8–14 mm) and Class IIb (IFD <30 mm and AVRS 8–14 mm). The Class IIa advises four implants with ball and locators/Dalla-Bona attachment's and Class IIb advises two implants with ball and stud type of attachment. Class III: the Class III has again two subtypes. Class IIIa (IFD >30 mm and AVRS 6–8 mm) and Class IIIb (IFD <30 mm and AVRS 6–8 mm). Class IIIa advises four implants with ball or locator attachment's and Class IIIb advises two implants with locator attachments.[42] Cost-wise mandibular implant-supported overdenture is more economical than fixed restorations as compared to maxillary overdenture.[30,40,41] However, there are few listed prosthetic complications associated with implant-supported mandibular overdenture, which are: overdenture loss of retention or adjustment (30%), overdenture rebasing or relining (19%), clip or attachment fracture (17%), overdenture fracture (12%), opposing prosthesis fracture (12%), acrylic resin base fracture (7%), abutment screw loosening (4%), abutment screw fracture (2%), and implant fracture (1%).[43] Recently, there are various emerging attachment systems like Kerators provide higher degree retention and patient satisfaction[44] but with more mucosal changes.[45] The rate of retention loss in attachments was higher in attachments with plastic parts within their components, rather than those totally made up of noble metals.[46] Further Randomised Controlled trials are required for evaluation of newer attachment systems in terms of retention loss and mucosal changes.[47]
CONCLUSION
The implant-supported overdenture is one of the economic options as compared to fixed implant prosthodontics as it not only secures the retention and stability, but also significantly increases the masticatory efficiency, survival rate, and patient satisfaction. The meta-analysis evaluated the various attachments by combining the results of 16 studies and suggests that ball attachments give excellent outcome when the number of implants is less and if more than two implants are placed, bar or locator attachments give better outcome but require extensive follow-ups. Similarly, in maxillary arch splinted bar attachments[26] are favorable and in mandibular arch, un-splinted ball or locators are favorable. Thus, according to the clinical situation, AVRS, and the quality of hard and soft tissues, the attachments and their combinations have to be selected.[42] Ball and locator attachments show excellent survival, favorable tissue response, and efficient patient satisfaction for mandibular overdentures. Excluding the cost factor, implant-supported fixed prosthesis is the ideal treatment alternative as compared to implant-supported overdentures in maxillary arch.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Steffen RP, White V, Markowitz NR. The use of ball clip attachments with an implant-supported primary-secondary bar overdenture. J Oral Implantol. 2004;30:234–9. doi: 10.1563/0.661.1. [DOI] [PubMed] [Google Scholar]
- 2.Awad MA, Feine JS. Measuring patient satisfaction with mandibular prostheses. Community Dent Oral Epidemiol. 1998;26:400–5. doi: 10.1111/j.1600-0528.1998.tb01978.x. [DOI] [PubMed] [Google Scholar]
- 3.Fueki K, Garrett NR. Effect of implant-supported or retained on masticatory performance: A systematic review. J Prosthet Dent. 2007;980:470–7. doi: 10.1016/S0022-3913(07)60147-4. [DOI] [PubMed] [Google Scholar]
- 4.Bernhart G, Koob A, Schmitter M, Gabbert O, Stober T, Rammelsberg P. Clinical success of implant-supported and tooth-implant-supported double crown-retained dentures. Clin Oral Investig. 2012;16:1031–7. doi: 10.1007/s00784-011-0592-1. [DOI] [PubMed] [Google Scholar]
- 5.Robbins JW. Success of overdentures and prevention of failure. J Am Dent Assoc. 1980;100:858–62. doi: 10.14219/jada.archive.1980.0284. [DOI] [PubMed] [Google Scholar]
- 6.Samra R K, Bhide SV, Goyal C, Kaur T. Tooth supported overdenture: A concept overshadowed but not yet forgotten. J Oral Res Rev. 2015;7:16–21. [Google Scholar]
- 7.Mericske-Stern R, Sirtes G, Piotti M, Jäggi C. Biomechanics and implants Which is the best denture anchorage on implants in the edentulous mandible An in vivo study. Schweiz Monatsschr Zahnmed. 1997;107:602–13. [PubMed] [Google Scholar]
- 8.Locator Implant Attachment Quick Reference Guide. [Last accessed on 2020 Jun 04]. Available from: http://wwwmcdowell-servicecom/pdfs/Locator_Implant_Attachment_Quick_Reference_Guidepdf .
- 9.Mahajan N, Thakkur RK. Overdenture locator attachment for atrophic mandible. Contemp Clin Dent. 2013;4:509–11. doi: 10.4103/0976-237X.123060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wismeijer D, van Waas MA, Mulder J, Vermeeren JI, Kalk W. Clinical and radiological results of patients treated with three treatment modalities for overdentures on implants of the ITI Dental Implant System. A randomized controlled clinical trial. Clin Oral Implants Res. 1999;10:297–306. doi: 10.1034/j.1600-0501.1999.100406.x. [DOI] [PubMed] [Google Scholar]
- 11.Epstein DD, Cohen BI, Pagnillo MK. Comparison of the retentive properties of six prefabricated post overdenture attachment systems. J Prosthet Dent. 1999;82:925–84. doi: 10.1016/s0022-3913(99)70057-0. [DOI] [PubMed] [Google Scholar]
- 12.Leung T, Preiskel HW. Retention profiles of stud-type precision attachments. Int J Prosthodont. 1991;4:175–9. [PubMed] [Google Scholar]
- 13.Petropoulos VC, Smith W, Kousvelari E. Comparison of retention and release periods for implant overdenture attachments. Int J Oral Maxillofac Implants. 1997;12:176–85. [PubMed] [Google Scholar]
- 14.Kaddah AF. Principles of Removable Complete Prosthodontics. Advanced Clinical Course Egypt Dental online Community. 2008 [Google Scholar]
- 15.SShafie H. Manual of Implant Overdentures. Ames Iowa: Blackwell Munksgaard; 2007. Principles of Attachment Selection Clinical and Laboratory. [Google Scholar]
- 16.Fleming PS, Seehra J, Polychronopoulou A, Fedorowicz Z, Pandis N. A PRISMA assessment of the reporting quality of systematic reviews in orthodontics. Angle Orthod. 2013;83:158–63. doi: 10.2319/032612-251.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mother D, Liberati A, Tetzleff J, Altman DG The Prisma Group. Preferred reporting items for systematic reviews and meta-analysis: The PRISMA statement. PLoS Med. 2009. [Last accessed on 2020 Jun 04]. p. 6. e1000097. Available from: http://wwwprism-statmentorg . [DOI] [PMC free article] [PubMed]
- 18.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta- analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cristache C, Ionescu C, Cristache G. A 5-year prospective randomised clinical trial on the efficiency of two different attachment systems as retention for implant-supported mandibular overdenture. Radiographic. 2009;14:2016–9. [Google Scholar]
- 20.Alsabeeha NH, Swain MV, Payne AG. Clinical performance and material properties of single-implant overdenture attachment systems. Int J Prosthodont. 2011;24:247–54. [PubMed] [Google Scholar]
- 21.Geckili O, Cilingir A, Erdogan O, Kesoglu AC, Bilmenoglu C, Ozdiler A, et al. The Influence of momentary retention forces on patient satisfaction and quality of life of two-implant-retained mandibular overdenture wearers. Int J Oral Maxillofac Implants. 2015;30:397–402. doi: 10.11607/jomi.3774. [DOI] [PubMed] [Google Scholar]
- 22.de Albuquerque RF, Jr, Fromentin O, Lassauzay C, Pereira Saraiva MC. Patient satisfaction versus retention of implant overdentures with two attachment systems. Clin Implant Dent Relat Res. 2018:1–11. doi: 10.1111/cid.12675. [DOI] [PubMed] [Google Scholar]
- 23.Cepa S, Spies BC. Implant-retained prostheses: ball vs conus attachments – A randomized controlled clinical trial. Clin Oral Impl Res. 2016:1–9. doi: 10.1111/clr.12779. [DOI] [PubMed] [Google Scholar]
- 24.Cune M, Burgers M. Mandibular overdentures retained by two implants: 10-year results from a crossover clinical trial comparing ball-socket and bar- clip attachments. Int J Prosthodont. 2010;23:310–7. [PubMed] [Google Scholar]
- 25.Mericske-Stern R, Oetterli M, Kiener P, Mericske E. A follow-up study of maxillary implants supporting an overdenture: Clinical and radiographic results. Int J Oral Maxillofac Implants. 2002;17:678–86. [PubMed] [Google Scholar]
- 26.Narhi TO, Hevinga M, Voorsmit RA, Kalk W. Maxillary overdentures retained by splinted and unsplinted implants: A retrospective study. Int J Oral Maxillofac Implants. 2001;16:259–66. [PubMed] [Google Scholar]
- 27.Assad AS, Abd El-Dayem MA, Badawy MM. Comparison between mainly mucosa-supported and combined mucosa-implant-supported mandibular overdentures. Implant Dent. 2004;13:386–94. doi: 10.1097/01.id.0000144512.43654.08. [DOI] [PubMed] [Google Scholar]
- 28.MacEntee MI, Walton JN, Glick N. A clinical trial of patient satisfaction and prosthodontic needs with ball and bar attachments for implant-retained complete overdentures: Three-year results. J Prosthet Dent. 2005;93:28–37. doi: 10.1016/j.prosdent.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 29.Kappel S, Dent M, Giannakopoulos NN, Dent M. Immediate loading of dental implants in edentulous mandibles by use of locator ® attachments or Dolder ® Bars: Two-year results from a prospective randomized clinical study. Clin Implant Dent Relat Res. 2016;18:752–61. doi: 10.1111/cid.12349. [DOI] [PubMed] [Google Scholar]
- 30.Boven GC, Meijer HJ, Vissink A, Raghoebar GM. Maxillary implant overdentures retained by use of bars or locator attachments: 1-year findings from a randomized controlled trial. J Prosthodont Res. 2020;64:26–33. doi: 10.1016/j.jpor.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 31.Kleis WK, Kammerer PW, Hartmann S, Al-Nawas B, Wagner W. A comparison of three different attachment systems for mandibular two-implant overdentures: One year report. Clin Implant Dent Relat Res. 2010;12:209–18. doi: 10.1111/j.1708-8208.2009.00154.x. [DOI] [PubMed] [Google Scholar]
- 32.Malmstrom HS, Xiao J, Romanos G, Ren YF. Two-year success rate of implant-retained mandibular overdentures by novice general dentistry residents. J Oral Implantol. 2015;41:268–75. doi: 10.1563/AAID-JOI-D-13-00148. [DOI] [PubMed] [Google Scholar]
- 33.Park J-H, Shin S-W, Lee J-Y. Bar versus ball attachments for maxillary four-implant retained overdentures: A randomized controlled trial. Clin Oral Impl Res. 2019;00:1–9. doi: 10.1111/clr.13521. [DOI] [PubMed] [Google Scholar]
- 34.Taha NEKS, Dias DR, Oliveira TMC, Souza JAC, Leles CR. Patient satisfaction with ball and Equator attachments for single-implant mandibular overdentures: A short-term randomised crossover clinical trial. J Oral Rehabil. 2019;00:1–9. doi: 10.1111/joor.12895. [DOI] [PubMed] [Google Scholar]
- 35.Sadowsky SJ, Fitzpatrick B, Curtis DA. Evidence-based criteria for differential treatment planning of implant restorations for the maxillary edentulous patient. J Prosthodontics. 2015;24:433–46. doi: 10.1111/jopr.12226. [DOI] [PubMed] [Google Scholar]
- 36.Di Francesco F, De Marco G, Gironi Carnevale UA, Lanza M, Lanza A. The number of implants required to support a maxillary overdenture: A systematic review and meta-analysis. J Prosthodontic Res. 2019;63:15–24. doi: 10.1016/j.jpor.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 37.Centenero SA. Zygoma quad compared with 2 zygomatic implants: A systematic review and meta-analysis. Implant Dent. 2018;27:1. doi: 10.1097/ID.0000000000000726. [DOI] [PubMed] [Google Scholar]
- 38.Block MS, Haggerty CJ. Nongrafting implant options for restoration of the edentulous maxilla. YJOMS. 2009;67:872–81. doi: 10.1016/j.joms.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 39.Annibali S, Cristalli MP, Aquila DD, Bignozzi I, Monaca La G, Pilloni A. Short dental implants: A systematic review. J Dent Res. 2012;91:25–32. doi: 10.1177/0022034511425675. [DOI] [PubMed] [Google Scholar]
- 40.Sadowsky S. Treatment considerations for maxillary implant overdentures: A systematic review. J Prosthet Dent. 2007;97:340–8. doi: 10.1016/S0022-3913(07)60022-5. [DOI] [PubMed] [Google Scholar]
- 41.Att W, Bernhart J, Strub JR. Fixed restoration of edentulous maxilla: Possibilities and clinical outcome. J Oral Maxillofac Surg. 2009;67(Suppl 3):60–73. doi: 10.1016/j.joms.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 42.Bhargava A, Sehgal M, Gupta S, Mehra P. Classification system on the selection of number of implants and superstructure design on the basis available vertical restorative space and inter-foraminal distance for implant supported mandibular overdenture. J Indian Prosthodont Soc. 2016;16:131–5. doi: 10.4103/0972-4052.176541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121–32. doi: 10.1016/S0022-3913(03)00212-9. [DOI] [PubMed] [Google Scholar]
- 44.Varshney N, Aggarwal S, Kumar S, Singh SP. Retention and patient satisfaction with bar-clip, ball and socket and kerator attachments in mandibular implant overdenture treatment: An in vivo study. J Indian Prosthodont Soc. 2019;19:49–57. doi: 10.4103/jips.jips_281_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Varshney N, Gupta S, Aggarwal S, Kumar S, Sadish M, Khan M. Hard and soft-tissue evaluation of bar-clip, ball-socket, and kerator attachments in mandibular implant overdenture treatment: An in vivo study. J Indian Prosthodont Soc. 2019;19:296–306. doi: 10.4103/jips.jips_143_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reda KM, El-Torky IR, EL-Gendy MN. In vitro retention force measurement for three different attachment systems for implant-retained overdenture. J Indian Prosthodont Soc. 2016;16:380–5. doi: 10.4103/0972-4052.191284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shastry T, Anupama NM, Shetty S, Nalinakshamma M. An in vitro comparative study to evaluate the retention of different attachment systems used in implant-retained overdentures. J Indian Prosthodont Soc. 2016;16:159–66. doi: 10.4103/0972-4052.176520. [DOI] [PMC free article] [PubMed] [Google Scholar]