Abstract
Objectives
Real-time COVID-19 spread mapping and monitoring to identify lockdown and semi-lockdown areas using hotspot analysis and geographic information systems and also near future prediction modeling for risk of COVID-19 in Punjab, Pakistan.
Study design
Data for all COVID-19 cases were collected until 20 October 2020 in Punjab Province.
Methods
The methodology included geotagging COVID-19 cases to understand the trans-mobility areas for COVID-19 and characterize risk. The hotspot analysis technique was used to identify the number of areas in danger zones and the number of people affected by COVID-19. The complete lockdown areas were marked down geographically to be selected by the government of Pakistan based on increased numbers of cases.
Results
As per predictive model estimates, almost 9.2 million people are COVID-19 infected by 20 October 2020 in Punjab Province. The compound growth rate of COVID-19 decreased to 0.012% per day and doubling rate increased to 364.5 days in Punjab Province. Based on Pueyo model predictions from past temporal data, it is more likely that Punjab and Pakistan entered into peak around the first week of July 2020, and the decline of growth rate (and doubling rate) of reported cases started afterward. Hospital load was also measured through the Pueyo model, and mostly, people in the 60+ years age group are expected to dominate the hospitalized population.
Conclusions
Pakistan is experiencing a high number of COVID-19 cases, with the maximum share from Punjab, Pakistan. Statistical modeling and compound growth estimation formulation were done through the Pueyo model, which was applied in Pakistan to identify the compound growth of COVID-19 patients and predicting numbers of patients shortly by slightly modifying it as per the local context.
Keywords: COVID-19, Coronavirus, Real-time monitoring, Transmission, Geographic information system, Hotspot analysis
Introduction
The outbreak of a tragic coronavirus disease (COVID-19 also known as 2019-nCoV) led to a pandemic situation globally, which has subsequently affected all continents.1 It led to a public health emergency of international concern that has infected 40 M people in about 215 countries as of 20 October 2020. Person-to-person transmission and travel patterns across the USA make it the topmost country with total confirmed COVID-19 cases exceeding 8.4 M, and the deaths above the 200 K threshold,2 which is more than China, from where the outbreak initiated.3 The overall death rate per diagnosed case in China was increased from 4.5% to 15% in one week after 2 January, 20204 but reduced when more testing was done.
The COVID-19 pandemic that has a strong grip in developed and developing countries has already spread across Pakistan with the most rapid spread moving toward vulnerable conditions.5 Despite Pakistan being a neighboring country of China, the first patient of COVID-19 was confirmed three months later than in China, on 26 February 2020. The total rise in confirmed patients exceeded 304, including 208 in Sindh, 33 in Punjab, 19 in Khyber Pakhtunkhwa, 23 in Baluchistan, and 7 in Islamabad by 18 March 2020,6 which has increased in succeeding weeks.7
The health, social, and economic effects of this situation are alarming in the country. Health impacts could be minimized if physical distancing measures were adopted at the initial stages of this pandemic.7 Initial monitoring and identification of high-risk areas for complete lockdown and quarantine are important factors to legitimize the precautionary measures.3 All stages, from real-time monitoring to communicating results publicly, to combat the pandemic in countries are major challenges worldwide.8
Geographic information system (GIS) and other methods have been helpful in near real-time spatial monitoring, including disease spread, disease cases reported, measuring reaction of social media to disease spread, risk-mapping based on imported and locally transmitted cases, mapping and tracing of contacts across time and space, and monitoring of spread trajectories.9 It also provides a clear understanding of the disease source, dynamics and response mapping, and risk assessment and defines quarantine areas to restrict the COVID-19 patients.10 With real-time monitoring, forecasts of the situation of the pandemic into the future are also important for policymaking to minimize loss of life.11
One of the key challenges of forecasting COVID-19 is that better and more accurate predictions demand sufficient historical data.12 In the case of COVID-19, we are lacking in sufficient data, as it is a recent phenomenon and Pakistan is just in the early phases of its outbreak. In the recent and rapidly growing literature, various models for forecasting COVID-19 are being used to inform public health interventions and preparedness. Pueyo (2020) proposed a simple yet reliable model to predict the true case rates of the COVID-19 cases based on data from China.13
COVID-19 is defined as a category B infectious disease that was declared as a class A infection by the Chinese government, which is quite dangerous. Factors such as air pollution, adverse environmental conditions, and smoking may contribute to the severity and spread rate of COVID-19.14, 15, 16 Air pollution could exacerbate health outcomes of COVID-19 patients. Wang et al., 202017 argued that environmental conditions such as temperature and humidity could interrupt transmission of COVID-19 compared to other pandemic viruses, suggesting a possible decline in disease, although these conclusions have been disputed.17 The GIS is an important tool to analyze spatial variation and distribution of this disease, which can support the process of monitoring and controlling its progress.18, 19, 20
In recent studies, critical spatial models have been used successfully to investigate statistically the geographic relationship between disease outbreak and explanatory variables.21, 22, 23, 24 For instance, autoregressive spatial models and predictive models have been examined to assess COVID-19 in the USA based on demography, topography, and environmental factors, to provide intervention strategies to policymakers. For the present study, many people came into Pakistan from Iran, China, UK, USA, and other countries.25 , 26 Pakistan becomes reconciled with severe effects of COVID-19, with 323,452 patients suffering from the virus until 20 October 2020 and with a growth rate of 0.20%.27
The objective of this study is real-time monitoring of COVID-19 cases in Punjab Province, Pakistan. The real-time complete lockdown areas are also identified through hotspot analysis. Predictive models were created to predict numbers of cases of COVID-19 in the near future in Punjab, Pakistan.
Methods
Study Design
To analyze COVID-19 spread in Punjab, all positive and negative cases were considered up to 20 October 2020.
Study area
Punjab has the highest number of COVID-19 cases compared to other provinces of Pakistan.28 The number of confirmed cases in Punjab are 101,652 out of 323,452 total in Pakistan, which makes 31.4% of the total confirmed patients, according to the Government of Pakistan federal portal. It is situated in the center of Pakistan, with seven major airports, and having the most economic activity.29 , 30
Data collection and real-time monitoring of COVID-19
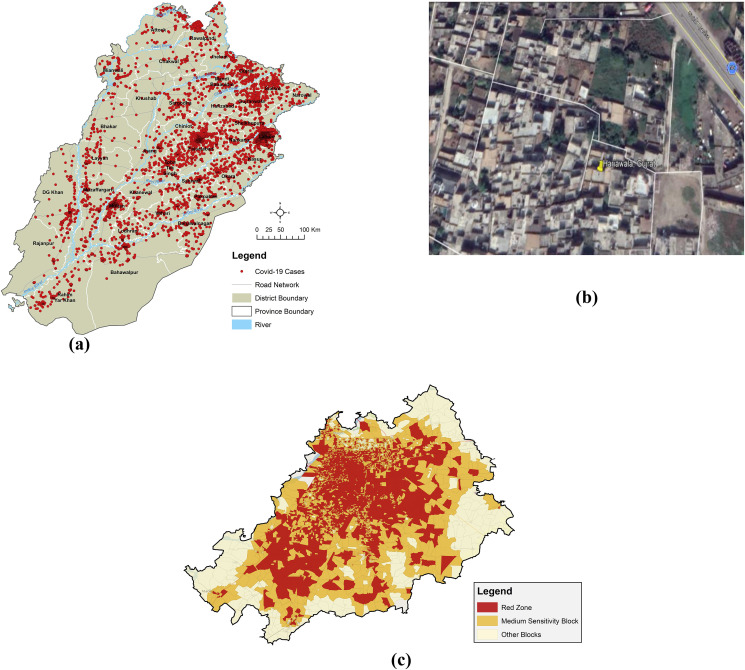
Detailed information was collected, such as travel history, gender, residential address (where infected), age, contact number, lab result (negative/positive), and so on. Raw data were processed and cleaned after collection through careful analysis of each case (Fig. 1 a–c). Based on the travel history of each patient, the data were divided into three categories including pilgrims (coming from religious events in Iran), religious center's patients (i.e. infected during a religious event in Lahore), and local spread. We have also collected information on the recovery of the COVID-19 patients in Punjab by capturing data from the follow-up of each case. Each case was geotagged to obtain the spatial distribution of COVID-19 cases by converting their addresses into real-time locations (Fig. 1b).
Fig. 1.
(a) Cumulative active and confirmed COVID-19 patients (Punjab) from 15 March 2020 to 21 October 2020, (b) physical addresses converted to spatial location, and (c) Lahore vulnerability (red zones lockdown areas). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Estimating the trans-mobility through hotspot analysis
The exact location was used to monitor the current trans-mobility areas for COVID-19 to identify the risk in neighboring areas.31 Hotspot analysis depending upon the number of patients in a 25 km radius vicinity was performed in ArcGIS 10.6 to identify vulnerable clusters across Punjab.32 This hotspot analysis utilizes the Gi∗ statistics technique,33 which is calculated as:
| (1) |
where Gi∗ defines the spatial autocorrelation statistics of any event denoted with i over n events; the equation xj shows the magnitude of the variable x at any event that occurs at j over n; the overall weight is determined by the weight value between the I and j variables that identify the interrelationship. The hotspot analysis and Gi∗ statistics considered the magnitude of all features in the dataset of neighboring values. The overall sum was compared to the local sum of all the neighboring values. If a significant difference is found between the local and expected local sum, and that the difference is large, then the significant z-score is counted as the final result.34 The hotspot analysis calculated the z-score and P score for each COVID-19 patient location, which helped to indicate hotspots and cold spots of different kinds of events. The statistical significance of clustering was identified through z-score for a specified distance, whereas P represents the probability of the unified spatial pattern. Transmissibility of patients was monitored across 25 km radius of each location of active COVID-19 cases in Punjab. However, at the city level, census blocks were used to microanalyze the patterns spatially. The red zones are the highly risky areas where the chances of being infected are relatively high in 25 km of radius (Fig. 3 a).
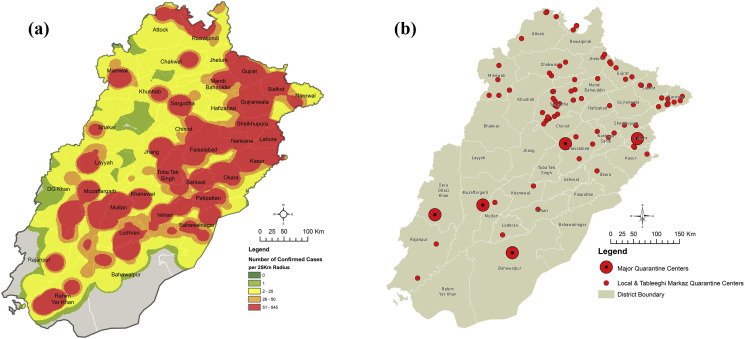
Fig. 3.
(a) Total number of confirmed cases found within a 25-km radius through hotspot analysis. (b) Quarantine centers allocated by the Government of Punjab.
Identifying lockdown areas and quarantine areas
We identified the complete lockdown areas where large numbers of patients were affected by COVID-19 in Punjab Province. Lockdown areas were selected geospatially based on patient addresses, and if five or above patients were in a house, it was marked as a lockdown house/street/town by the provincial government of Punjab. Patients’ real-time locations were overlaid onto satellite imagery and vulnerable areas were identified and marked in the GIS technique. Schools and hospitals were selected through accessibility analysis, which showed exact locations of quarantine locations where people coming from other countries will reside for 14 days or more in Punjab. Travel history of each of the patients was recorded in this study, which we summarized in terms of the number of countries from where people traveled to Punjab during the pandemic.
Socio-economic and statistical analysis of COVID-19
Pueyo (2020) proposed a framework to backtrack the true cases of COVID-19 from the reported death data. Based on the assumption about mortality rates, Pueyo estimated the number of the actual infected cases on the day of the onset of infection.35 The onset of infection is estimated based on the average number of days from infection to death of the countries under study.36 To better understand the model, we first discuss the assumptions of the author, which are not vague assumptions but are based on the average of the numbers reported by countries under study; the Pueyo 2020 model assumes a case-fatality rate of 0.87–1.00, the number of days from infection to death as 17, and a doubling time of 6.18–6.20, and it took 17 days for the cases to double.
Based on the assumptions, the basic postulation as the model is that one death reported today means 17 days back at least 100 persons were infected (as per the 1% fatality rate). These infections are doubling every 6.2 days, so 17 days later, those 100 cases have grown to 697. Then 697 cases will become 780 by the next day and 1528 by one week if no mitigation measures are taken. The present study attempts to apply the Pueyo 2020 model in Pakistan by slightly modifying it to local contexts.
Results
Hotspot analysis and lockdown areas
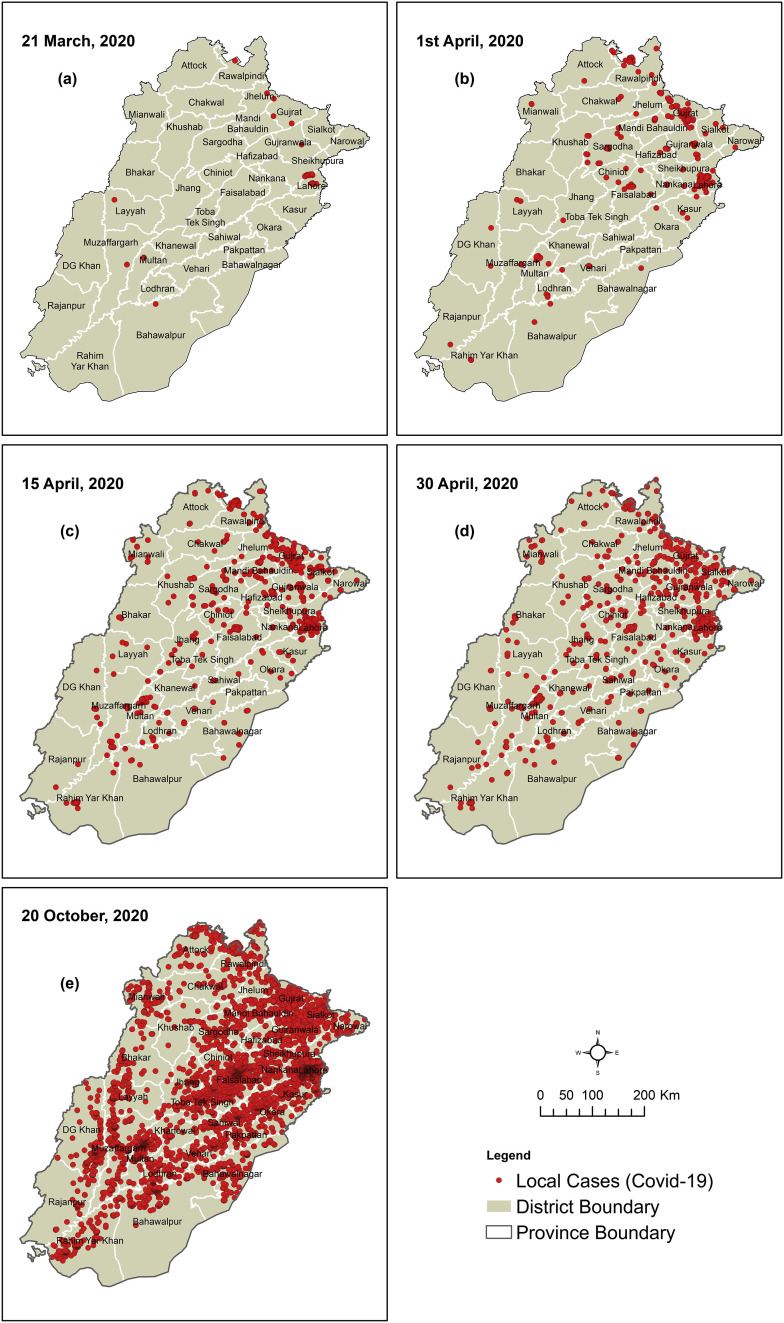
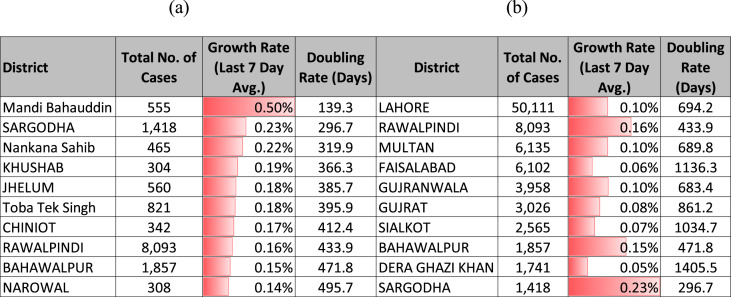
wMore than 101,652 cases have been recorded in Punjab Province, which is 31.3% out of 323,452 overall patients in Pakistan (21 March 2020 to 20 October 2020). Fig. 4 shows the cases through 30 May 2020 and the rate of increase doubled from 30 May 2020 to 11 June 2020 and 20 October 2020. In Punjab Province, the Lahore District is the most vulnerable area, with 50,111 cases as of 5 October 2020. The Rawalpindi District was identified as the second most affected area, with 8093 cases and a compound growth rate of 0.16% (Table 1 ).
Fig. 4.
Temporal analysis of COVID-19 cases from 21 March 2020 to 20 October 2020.
Table 1.
(a) Top 10 cities by the number of cases. (b) Top 10 cities by 7-day growth rate as on 5 October 2020.
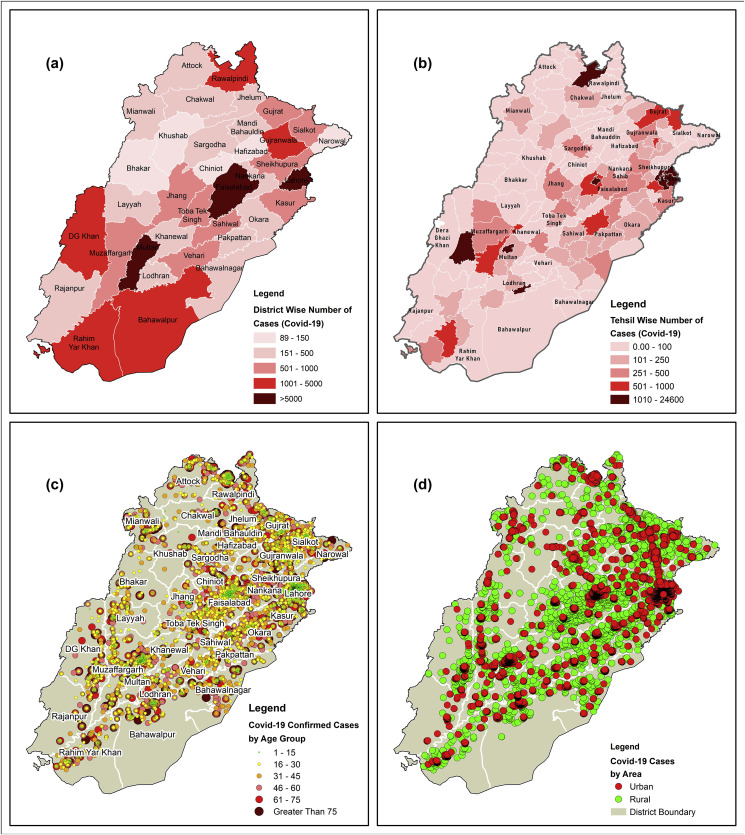
Each district and tehsil of Punjab have confirmed cases ranging from 20% to 90% (Fig. 2a and 2sb). The top ten cities, ranked from most affected to less affected, are Lahore (50,111 cases), Rawalpindi (8,093), Multan (6,135), Faisalabad (6,102), Gujranwala (3,958), Gujrat (3,026), Sialkot (2,565), Bahawalpur (1,857), Dera Ghazi Khan (1,741), Sargodha (1,418), and so on (Table 1). COVID-19 cases by the area (urban/rural) in 15 March 2020 to 21 October 2020 are shown in Fig. 2d.
Fig. 2.
(a) District-wise number of COVID-19 cases in Punjab Province, (b) tehsil-wise number of COVID-19 cases in Punjab Province, (c) classification of COVID-19 cases by age group, and (d) COVID-19 cases by the area (urban/rural) from 15 March 2020 to 21 October 2020.
Fig. 3a and c shows the high-risk zones identified through a geospatial analysis, where case numbers are greater than 50 within a 25 km radius in Punjab. The major hotspots area in terms of the total number of cases are Lahore, Ferozewala, Sheikhupura, Muridke, Kamoki, Gujranwala, Sialkot, Gujrat, Jhelum, Sargodha, Faisalabad, Multan, Muzaffargarh, D.G. Khan, and Rahim Yar Khan (Fig. 3a).
Lahore is the topmost vulnerable city in Punjab shown in Fig. 1c. The lockdown areas of Lahore include Raiwind, Chah Miran, Bahria Town, Sikandria colony, Bhatta Chowk, Bedian Road, China Scheme, Mughalpura, Samanabad, Shahdara, small industries, and some areas of Saddar, Rustam Park, and Gulshan-e-Ravi as of 15 May 2020. Areas unlocked after 5 May 2020 includes Bahria Town, Raiwind, and Sikandria colony.
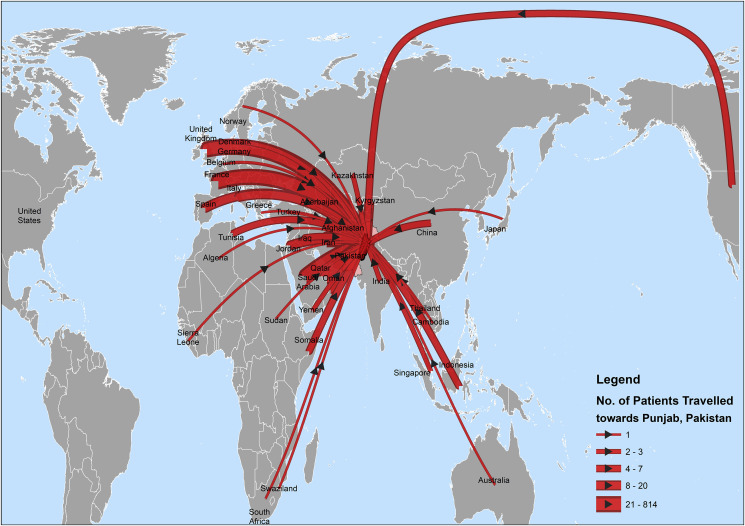
For traveling monitoring, it shows that more than 800+ people traveled from UK, France, Spain, and USA to Punjab, as of March 2020, and so on (Fig. 5 ). Many universities, hospitals, and restaurants were selected by the Government of Punjab for quarantine (Fig. 3b).
Fig. 5.
Direction map showing the number of patients traveled to Punjab from all over the world before 21 March 2020.
Affected age group in Punjab
COVID-19 cases by age group clearly show that the most affected age group in Punjab Province is 50–75 years (Fig. 2c). Many patients infected with COVID-19 of age 1 to 30 years are in Lahore, Ferozewala, Kamoke, Gujranwala, and Gujrat. Sahiwal has the highest number of patients in the 40–60 and 61–75 years age intervals; Faisalabad is also high in the 60–75 years age group (Fig. 2c).
Compound growth of COVID-19
The ten major infected cities are compared in terms of identifying the number of days to double COVID-19 (Table 1). Lahore is on the top of the list, where 50,111 cases and doubling in 694.2 days as shown in Table 1b. The compound growth was lower in Sargodha at only 0.23% and doubling in 296.7 days (Table 1b). Lahore has the highest number of cases reported. Rawalpindi is marked as second. Khushab has the lowest number of cases reported, only 304 as shown in Table 1a.
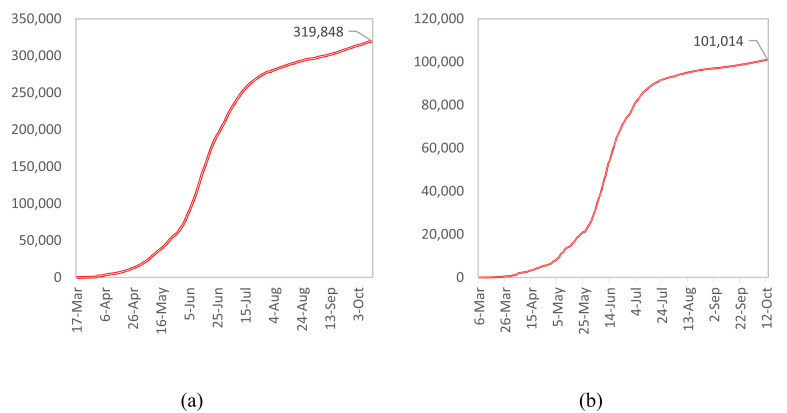
Predictive models
In Pakistan, on 10 March 2020, 19 cases were reported for the first time, and 2 deaths were reported on 18 March 2020. The temporal data of reported COVID cases are shown in Fig. 4 and the confirmed patient data are shown in Fig. 6 a across Pakistan. Similarly, in Punjab, 37 cases were reported on 19 March 2020, (excluding Zaireen which was quarantined), and the first death was reported on 24 March 2020 and it increased until to date (Fig. 6b). The projected and reported patients were interpreted from 20 March 2020 to 2 October 2020 (Fig. 7 ). The Pueyo 2020 model has been applied in Pakistan with assumptions slightly modified as per locally reported data. For instance, the key assumptions for the Pakistan model are a mortality rate of 1.46%, a prelockdown doubling-rate of 6.20 days, and a postlockdown (23 March) doubling rate of 11 days.
Fig. 6.
(a) Confirmed number of COVID-19 cases across Pakistan. (b) Confirmed number of COVID-19 cases across Punjab.
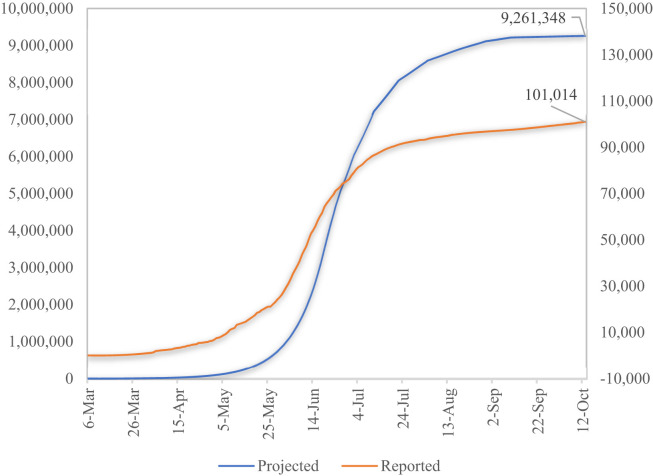
Fig. 7.
Real vs reported infections across Pakistan.
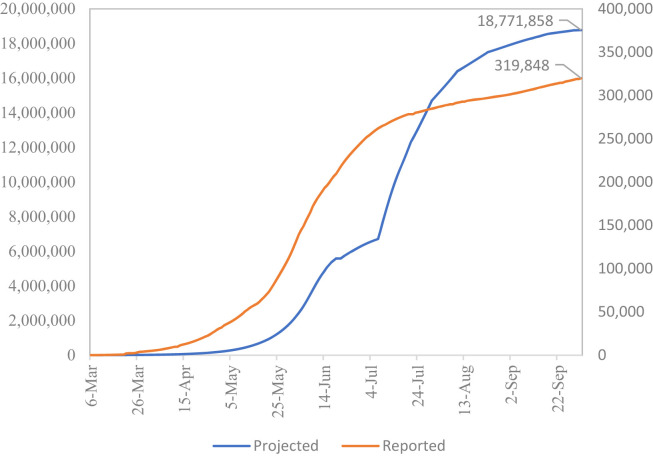
Our doubling rates are drawn from the actual reported data before and after lockdown, which shows that prelockdown average growth of reported cases is higher than the postlockdown average growth rate of reported cases. The results of the model applied in Punjab show that true cases projected as per model (9,261,348) are 92 times higher than actual reported cases (101,014) on 13 October 2020 (Fig. 8 ); if these calculations are true, definitely most of these cases are asymptomatic. The graphs (Fig. 8) show that the slope of the predicted model is almost closer to the actual but the only difference is in the quantum of numbers. This huge gap is attributed to a higher number of asymptomatic cases and low testing capacity and affordability. In Pakistan, currently, the facilities of testing are much lower than the requirement. Pakistan has a testing capacity of 9,878 tests per million.37 India is conducting 18,478 tests per million and USA is doing 202,508 tests per million.37
Fig. 8.
Total projected/real cases as of October 14 2020.
Estimation of peak in Punjab and Pakistan—prediction
Based on the model estimations and patterns of actual reported cases, it is more likely that Punjab and Pakistan entered into peak around the first week of July 2020 and a decline of growth rate (and doubling rate) of reported cases of COVID has been observed afterward. Table 1 shows growth of COVID cases with doubling rates in the top 10 cities of Punjab. Lahore is the topmost city in terms of the number of cases reported with a growth rate of 0.10% and a doubling rate of 694.2 days. Faisalabad stands fourth in the number of reported cases but has a low growth rate of 0.06% and a doubling rate of 1136 days. Similarly, the top 10 cities in terms of the 7-days average compound growth rate are shown in Table 1b. The confirmed ratio of patients varies by age; from age 1 to 15, most are recovering at home as the case fatality rate in percentage shows the hospital load and home load scenarios as of 14 October (Table 2 ).
Table 2.
Hospital load extreme scenario estimation based on literature and actual demographic dispersion of confirmed reported COVID-19 cases as on 14 October 2020.
| Age-group (years) | Percent of Population | Infected | Total Symptomatic | Total Clinical | Total Hospitalized | Case Fatality Rate (%) |
|---|---|---|---|---|---|---|
| 1 to 15 | 35% | 558,557 | 184,324 | 55,856 | 11,171 | 0.2% |
| 15 to 30 | 28% | 2,975,390 | 1,190,156 | 446,309 | 59,508 | 0.2% |
| 30 to 45 | 19% | 2,420,414 | 1,064,982 | 484,083 | 72,612 | 0.3% |
| 45 to 60 | 11% | 2,058,784 | 905,865 | 679,399 | 267,642 | 1.3% |
| 60 to 75 | 5% | 1,106,373 | 697,015 | 497,868 | 365,103 | 6.0% |
| Over 75 | 2% | 128,898 | 128,898 | 128,898 | 122,453 | 21.9% |
| Total | 100% | 9,262,737 | 4,171,239 | 2,292,411 | 898,489 | 1.3% |
Nevertheless, as for now in this study, the actual prediction was carried out based on previous and current data and concluded that the actual number of COVID-19 patients are 9.2 million until 14 October 2020 (Fig. 8). This gap is mostly attributed to a higher number of asymptomatic cases and very low testing capacity and affordability. Currently, the facilities of testing are much lower than the requirement. Pakistan has a testing capacity of 9878 tests per million.37
Discussion
The first patient of COVID-19 was confirmed on 26 February 2020 in Pakistan, a student who returned from Iran who tested positive. As of 20 October 2020, the number of total confirmed cases was 323,452, out of which 6,659 possible deaths were observed; the number of patients recovered are 307,409 with only 9,384 active in Pakistan. Punjab is found as the topmost affected province as the total confirmed cases are 101,652 out of which 2,310 possible deaths were observed, the number of patients recovered are 97,252 with only 4,400 active cases.
It has been predicted through the Pueyo 2020 model in this study that the actual number of confirmed cases are up to 9.2 million by 20 October 2020 in Punjab. This huge gap between reported and estimated COVID-19 cases is attributed to a higher number of asymptomatic cases and low testing ability and affordability.37 , 38 Furthermore, the claim of an enormous number of asymptomatic cases is further strengthened by the result of smart testing of random public done in mid-May to start of June 2020 by the Health Department of the Government of Punjab found that almost 95%–97% of the COVID-19 positive people were asymptomatic.
GIS and other methods are helpful in near-real-time monitoring including mapping of disease spread, disease cases reported, measuring reaction of social media about disease spread, risk mapping through patients traveling from outside country and local transmission through in-house traveling, mapping and tracing of contacts across time and space, and monitoring of spread trajectories.36 GIS as a tool can aid in providing a clear understanding of the disease source, dynamics and response mapping, and risk assessment and defining quarantine areas to restrict the COVID-19 patients.37
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2020.10.026.
Author statements
Acknowledgments
This paper is dedicated to Khalid Sherdil, who helped us in analysis and writing before he died in a Karachi plane crash on 23 May 2020. We thank the Primary and Secondary Health Department, Rescue 1122, Urban Unit, and all the team involved in geotagging and mapping activities of COVID-19, for providing the support in data collection and preparing the analysis. We also thanks to A. Townsend Peterson and Anonymous Reviewers for reviewing the manuscript.
Ethical approval
No ethical approval was required as all the data analyzed were publicly available.
Funding
No funding was received for this particular research.
Author contribution
US and KS have contributed to the writing and analysis and in all aspects of research. GM helped in making models and analysis and he also successfully recovered from COVID-19 during this study. HJ and UA contributed to the manuscript writing. IY and HJ have worked on the preparation of maps. HJ compiled and wrote the manuscript. All authors approved and revised the manuscript.
Data availability
All relevant data are available and also included in the paper and all other supporting files are also ready to publish.
Competing interests
The authors have no conflict of interest.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gilbert M. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395:871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raghvir M. COVID-19: emergence, spread, possible treatments, and global Burden. Front Publ Health. 2020;216:2296–2565. doi: 10.3389/fpubh.2020.00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chinazzi M. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020 doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kamel Boulos M.N., Geraghty E.M. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr. 2020;19:8. doi: 10.1186/s12942-020-00202-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou C. COVID-19: challenges to GIS with big data. Geogr Sustain. 2020;1:77–87. [Google Scholar]
- 6.Hassan A., Mahmood K. Primary & secondary health care department, healthcare system of Pakistan. Int J Acad Res Psychol. 2017;10 [Google Scholar]
- 7.Mukhtar S. Preparedness and proactive infection control measures of Pakistan during COVID-19 pandemic outbreak. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics. New Technology, and Proactive Testing. 2020;323:1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 9.Mollalo A. vol. 188. 2018. pp. 187–194. (Machine learning approaches in GIS-based ecological modeling of the sand fly Phlebotomus papatasi, a vector of zoonotic cutaneous leishmaniasis in Golestan province, Iran). [DOI] [PubMed] [Google Scholar]
- 10.Perc M., Gorišek Miksić N., Slavinec M., Stožer A. Forecasting COVID-19. Front Physiol. 2020;8 [Google Scholar]
- 11.Li L. Propagation analysis and prediction of the COVID-19. Infect Dis Model. 2020;5:282–292. doi: 10.1016/j.idm.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu Z., Ge Q., Li S., Jin L., Xiong M. 2020. Artificial intelligence forecasting of Covid-19 in China. arXiv:2002.07112 [q-bio] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pueyo T. 2020. Coronavirus: why you must act now. Politicians, community leaders and business leaders: what should you do and when. [Google Scholar]
- 14.Xu Z. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mollalo A., Vahedi B., Rivera K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci Total Environ. 2020;728:138884. doi: 10.1016/j.scitotenv.2020.138884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taghizadeh-Hesary F., Akbari H. The powerful immune system against powerful COVID-19: an hypothesis. J Med Hypotheses. 2020 doi: 10.20944/preprints202004.0101.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang J., Tang K., Feng K., Lv W. 2020. High temperature and high humidity reduce the transmission of COVID-19. Available at: SSRN 3551767. [Google Scholar]
- 18.Kamel Boulos M., Geraghty E. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr. 2020;19 doi: 10.1186/s12942-020-00202-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lakhani A. Which Melbourne metropolitan areas are vulnerable to COVID-19 based on age, disability, and access to health services? Using spatial analysis to identify service gaps and inform delivery. J Pain Symptom Manag. 2020 doi: 10.1016/j.jpainsymman.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gibson L., Rush D. Novel coronavirus in Cape Town informal settlements: feasibility of using informal dwelling outlines to identify high risk areas for COVID-19 transmission from a social distancing perspective. JMIR Publ Health Surveill. 2020;6 doi: 10.2196/18844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mollalo A., Alimohammadi A., Shirzadi M.R., Malek M.R. Geographic information system-based analysis of the spatial and spatio-temporal distribution of zoonotic cutaneous leishmaniasis in Golestan Province, north-east of Iran. Zoonoses Publ Health. 2015;62:18–28. doi: 10.1111/zph.12109. [DOI] [PubMed] [Google Scholar]
- 22.Last A. Spatial clustering of high load ocular Chlamydia trachomatis infection in trachoma: a cross-sectional population-based study. Pathog Dis. 2017;75 doi: 10.1093/femspd/ftx050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaney R.A., Rojas-Guyler L. Spatial analysis methods for health promotion and education. Health Promot Pract. 2016;17:408–415. doi: 10.1177/1524839915602438. [DOI] [PubMed] [Google Scholar]
- 24.Mann H.B., Whitney D.R. On a test of whether one of two random variables is stochastically larger than the other. Ann Math Stat. 1947;18:50–60. [Google Scholar]
- 25.Izumi K., Ohkado A., Uchimura K., Murase Y., Tatsumi Y., Kayebeta A., Watanabe Y., Ishikawa N. Detection of tuberculosis infection hotspots using activity spaces based spatial approach in an urban Tokyo, from 2003 to 2011. PloS One. 2015;10(9) doi: 10.1371/journal.pone.0138831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moran P.a.P. Notes on continuous stochastic phenomena. Biometrika. 1950;37:17–23. [PubMed] [Google Scholar]
- 27.Lloyd, C. Local models for spatial analysis. vol. 15.
- 28.Coronavirus Update (Live): 7,712,698 cases and 427,275 deaths from COVID-19 virus pandemic – Worldometer. https://www.worldometers.info/coronavirus/.
- 29.Largest airports and airlines in Pakistan. https://www.worlddata.info/asia/pakistan/airports.php.
- 30.Chohan U.W. 2020. Forecasting the economic impact of coronavirus on developing countries: case of Pakistan.https://papers.ssrn.com/abstract=3563616 [DOI] [Google Scholar]
- 31.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heiler G., Reisch T., Hurt J., Forghani M., Omani A., Hanbury A., Karimipour F. Country-wide mobility changes observed using mobile phone data during COVID-19 pandemic. arXiv preprint arXiv. 2020;vol. 2008:10064. [Google Scholar]
- 33.Jana M., Sar N. Modeling of hotspot detection using cluster outlier analysis and Getis-Ord Gi∗ statistic of educational development in upper-primary level, India. Model Earth Syst Environ. 2016;2:60. [Google Scholar]
- 34.Feltman J.A., Straka T.J., Post C.J., Sperry S.L. Geospatial analysis application to forecast wildfire occurrences in South Carolina. Forests. 2012;3:265–282. [Google Scholar]
- 35.COVID-19 Health advisory platform by Ministry of national health services regulations and coordination. http://covid.gov.pk/.
- 36.Malik A., Abdalla R. Mapping the impact of air travelers on the pandemic spread of (H1N1) influenza. Model Earth Syst Environ. 2016;2:91. [Google Scholar]
- 37.Li Q. A simple algorithm helps early identification of SARS-CoV-2 infection patients with severe progression tendency. Infection. 2020 doi: 10.1007/s15010-020-01446-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Waris A., Atta U.K., Ali M., Asmat A., Baset A. COVID-19 outbreak: current scenario of Pakistan. N Microbes N Infect. 2020;35:2052–2975. doi: 10.1016/j.nmni.2020.100681. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are available and also included in the paper and all other supporting files are also ready to publish.