Abstract
Background
The COVID-19 pandemic has significantly affected patient care across specialties. Ramifications for neurosurgery include substantial disruptions to surgical training and changes in nonurgent patient presentations to the emergency department. This study quantifies the effects of the COVID-19 pandemic on the number of emergency department patients who were referred to the neurosurgery department for further consultation and treatment and identifies and describes trends in the characteristics of these visits.
Methods
A retrospective review was performed of neurosurgical consultations at a single high-volume institution for 28 call-day periods before and after the official announcement of the pandemic. Primary outcomes included consultations per call-day, patient presentation category, and patient admission.
Results
The neurosurgical service was consulted regarding 629 patients (367 male patients) during the study period, with 471 (75%) and 158 (25%) patients presenting before and after the announcement of the COVID-19 pandemic, respectively. The mean number of neurosurgical consultations per call-day was significantly lower in the COVID-19 period (5.6 consultations) compared with the pre–COVID-19 period (16.8 consultations) (P < 0.001). After adjusting for patient demographics, the rate of presentation for general nonurgent concerns, such as back pain, headaches, and other general weaknesses, significantly decreased (odds ratio [95% confidence interval], 0.60 [0.47–0.77], P < 0.001).
Conclusions
Neurosurgical consultations significantly decreased after the onset of the COVID-19 pandemic, with a substantially lower overall number of consultations necessitating operative interventions. Furthermore, the relative number of patients with nonemergent neurological conditions significantly decreased during the pandemic.
Key words: Coronavirus disease 2019, COVID-19, Neurosurgery consultation volume
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; ED, Emergency department
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has become a major public health crisis that has substantially altered the ways in which patients seek and receive care. The number of patients treated by most specialties, including neurosurgery, has decreased since the onset of the pandemic.1 , 2 Because COVID-19 is highly contagious and associated with high morbidity, many centers have faced an increased strain on resources as they handle an unprecedented number of virus-related admissions. Simultaneously, the pandemic has caused notable decreases in admissions unrelated to COVID-19. A recent study conducted by the Centers for Disease Control and Prevention found that US emergency department (ED) visits decreased by 42% between March 29 and April 25, 2020, when compared with the same period in 2019.3 Other global studies also found sharp decreases in rates of hospital visits and diagnoses,4, 5, 6, 7 which may be attributable to a fear of becoming infected during a hospital visit.
Government orders that limit nonessential procedures have further contributed to the diminished surgical volume. This decrease has important ramifications for specialties such as neurosurgery, including significant disruptions to surgical training.8 Thus, analysis of the effect of the pandemic on provider services and patient experiences is essential to provide the highest and most coordinated level of care. Having noticed a decrease in neurosurgical consultations at a large tertiary center during the COVID-19 pandemic, with a decrease in patients presenting with either pain and/or nonspecific neurological symptoms, we sought to quantify the effects of the COVID-19 pandemic on the number of ED patients who were referred to the neurosurgery department for further consultation and treatment. We also sought to identify and describe trends in the characteristics of these visits.
Methods
On March 12, 2020, the Arizona governor declared a statewide public health emergency and mandated an indefinite stay-at-home ordinance. This directive also cancelled elective surgeries until May 1, 2020. To analyze the effect on call volume in the ED for neurosurgery, a retrospective review was performed of all neurosurgical consultations for 28 call-day periods before and after the official announcement of the pandemic in Arizona. One call-day was defined as all the patients seen for neurosurgery consultations during a single 24-hour call period, giving a total of 672 hours of observation in both time periods. Neurosurgical consultations were obtained via the call consultation logs of 3 junior residents. Data drawn from neurosurgical call logs from January 2, 2020, to February 25, 2020, were designated as pre–COVID-19 pandemic data, and data on patients seen from March 20, 2020, to April 27, 2020, were designated as COVID-19 pandemic data.
The study protocol was approved by the institutional review board for human research at St. Joseph's Hospital and Medical Center (Phoenix, AZ). The need for patient consent for the research study was waived. Observed characteristics of each visit included date of admission, sex, age, ethnicity, type of insurance, past medical history, reason for admission to the ED, 1-year surgical history, ED discharge location, whether the nature of the visit was postoperative or due to complications, whether the patient was admitted to the floor or the intensive care unit, and whether the patient underwent an operation. Patient presentations were categorized according to emergent cases, which included trauma, brain bleed, tumor, cerebrovascular issues (including nonruptured aneurysms, arteriovenous malformations and fistulas, cavernous malformations, and vessel stenosis), seizures, and postoperative complications; and nonemergent cases, which included back pain or other nonemergent spinal issues (e.g., radiculopathy), and headache, pain, and weakness (nonemergent idiopathic intracranial hypertension, chronic hydrocephalus with or without a shunt, and other general nonemergent neurological issues).
Primary outcomes included consultations per call, patient presentation category, and whether the patient was admitted to the hospital. Statistical analyses performed included data aggregation, exploratory analysis, and multivariate analysis using R, version 4.0.1 (R Foundation for Statistical Computing, Vienna, Austria). Subsequently, propensity-adjusted regression modeling was used to compare the pre–COVID-19 and COVID-19 patient groups controlling for age, sex, ethnicity, insurance, and whether the patient presented at a postoperative visit.
Results
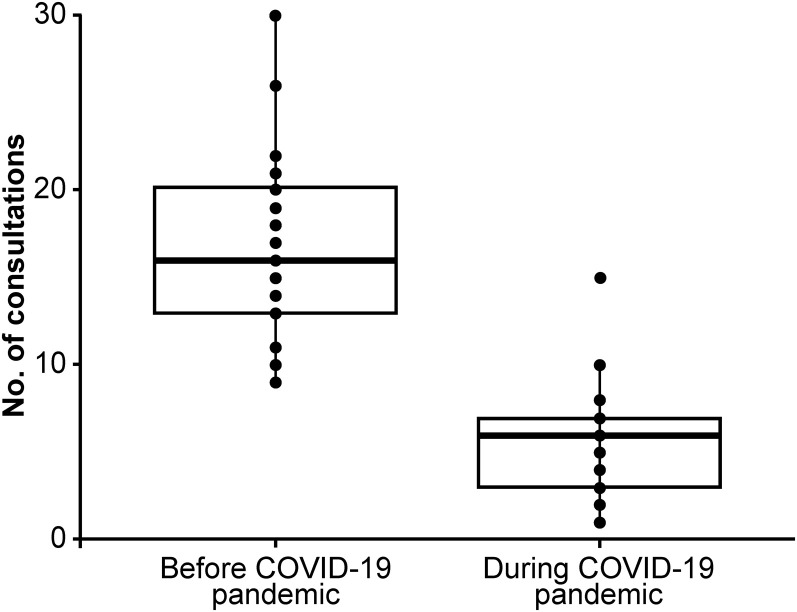
The neurosurgical service was consulted regarding 629 patients during the study period. Of these, 471 (75%) presented before the announcement of COVID-19 as a statewide emergency, and 158 (25%) were seen during the pandemic period. Comparisons of age, sex, insurance, postoperative status, and ethnicity revealed no major differences or trends between the 2 groups (Table 1 ). The mean number of neurosurgical consultations per call-day in the COVID-19 period (5.6 consultations) was significantly lower compared with the pre–COVID-19 period (16.8 consultations) (P < 0.001). This trend is also illustrated in a comparison between the total consultation volume per call-day and individual call-days (Figure 1 ). There was also a significantly greater percentage of hospital admissions during the COVID-19 period compared with the pre-COVID-19 period (85% [134 of 158] vs. 76% [359 of 471], P = 0.03) (Table 2 ).
Table 1.
Demographic and Clinical Characteristics of Neurosurgery Patients Treated at the Emergency Department of a Single Tertiary Center Before and During the Coronavirus Disease 2019 (COVID-19) Pandemic
| Characteristic | Before the COVID-19 Pandemic,∗ N = 471 | During the COVID-19 Pandemic,† N = 158 | P Value |
|---|---|---|---|
| Male sex | 276 (59) | 91 (58) | 0.90 |
| Age, years, mean (SD) | 58 (18) | 56 (18) | 0.16 |
| Ethnicity | 0.98 | ||
| White | 307 (65) | 105 (66) | |
| Hispanic | 80 (17) | 26 (16) | |
| Black | 27 (6) | 7 (4) | |
| American Indian | 15 (3) | 4 (3) | |
| Asian | 6 (1) | 3 (2) | |
| Other | 29 (6) | 10 (6) | |
| Unknown | 7 (1) | 3 (2) | |
| Insurance | 0.30 | ||
| Commercial | 259 (55) | 96 (61) | |
| Medicare or Medicaid | 128 (27) | 43 (27) | |
| Uninsured | 33 (7) | 9 (6) | |
| Veterans Affairs | 22 (5) | 2 (1) | |
| Unknown | 29 (6) | 8 (5) | |
| Postoperative condition | 149 (32) | 56 (35) | 0.43 |
| Acute | 52 (11) | 23 (15) | 0.30 |
| Nonacute | 97 (21) | 33 (21) | 0.98 |
Data are presented as no. (%) of patients unless otherwise indicated.
January 2 to February 25, 2020.
March 20 to April 27, 2020.
Figure 1.
Number of neurosurgery consultations stratified by call-day at a single large tertiary center before (January 2 to February 25, 2020) versus during (March 20 to April 27, 2020) the coronavirus disease 2019 (COVID-19) pandemic. The horizontal line in the middle of each box indicates the mean value; the top and bottom of each box indicate the 75th and 25th percentile, respectively; the whiskers above and below each box indicate the 90th and 10th percentile, respectively. Points beyond the whiskers indicate outliers beyond the 90th and 10th percentile. (Used with permission from Barrow Neurological Institute, Phoenix, Arizona.)
Table 2.
Reasons for Emergency Department Visit, Emergency Department Course, and Hospital Course Among Neurosurgery Consultations at a Single Tertiary Center Before and During the Coronavirus Disease 2019 (COVID-19) Pandemic
| Characteristic | Before the COVID-19 Pandemic,∗ N = 471 | During the COVID-19 Pandemic, † N = 158 | P Value |
|---|---|---|---|
| Reason for visit | 0.10 | ||
| Back pain or spinal issue | 102 (22) | 27 (17) | |
| Headache, pain, or weakness | 93 (20) | 17 (11) | |
| Trauma | 87 (18) | 41 (26) | |
| Cerebrovascular issue | 53 (11) | 15 (9) | |
| Brain bleed | 46 (10) | 15 (9) | |
| Tumor | 40 (8) | 25 (16) | |
| Postoperative complication | 40 (8) | 16 (10) | |
| Seizure | 10 (2) | 2 (1) | |
| Emergency department consultations admitted | 359 (76) | 134 (85) | 0.03 |
| Admitted to floor | 137 (29) | 46 (29) | >0.90 |
| Admitted to intensive care unit | 222 (47) | 88 (56) | 0.08 |
| Neurosurgery operation | 176 (37) | 63 (40) | 0.64 |
| Mean (SD) consultations per call day | 16.8 (4.9) | 5.6 (3.1) | <0.001 |
Data are presented as no. (%) of patients unless otherwise indicated. Boldface indicates P less than 0.05.
January 2 to February 25, 2020.
March 20 to April 27, 2020.
On a normal call day before the pandemic, the ED typically saw a considerable number of nonemergent cases (accounting for approximately 41% [195 of 471] of cases; Table 2). After the start of the pandemic, this number decreased to 28% (44 of 158), revealing a decreasing trend in cases such as backpain and headache. Further analysis demonstrated that a larger percentage of emergent cases, such as those involving trauma, tumor, and postoperative complications, were seen after the start of the pandemic relative to before the pandemic (Table 2), but neither of these results were statistically significant (P = 0.10) before a propensity adjustment.
After correcting for age, sex, insurance, ethnicity, and whether the patient visit was postoperative, the rate of presentation for these general, nonurgent concerns, such as back pain, headaches, and other general weaknesses, significantly decreased (odds ratio [95% confidence interval], 0.60 [0.47–0.77]; P < 0.001; Table 3 ). Compared with the pre–COVID-19 period, ED visits that resulted in a hospital admission significantly increased during the pandemic (odds ratio [95% confidence interval], 1.46 [1.04–2.05]; P = 0.03), but there was no significant difference in the number of patients admitted to the intensive care unit (1.17 [0.90–1.53]; P = 0.20; Table 3).
Table 3.
Propensity-Adjusted Analysis Comparing General Reasons for Admission, Admission from the Emergency Department, and Admission to the Intensive Care Unit Before and During the COVID-19 Pandemic
| Characteristic | Number (%) of Patients |
Propensity-Adjusted Analysis |
|||
|---|---|---|---|---|---|
| Before the COVID-19 Pandemic,∗ N = 471 | During the COVID-19 Pandemic, † N = 158 | OR | 95% CI | P Value | |
| General pain | 195 (41) | 44 (28) | 0.60 | 0.47–0.77 | <0.001 |
| Admitted from emergency department | 359 (76) | 134 (85) | 1.46 | 1.04–2.05 | 0.03 |
| Admitted to intensive care unit | 222 (47) | 88 (56) | 1.17 | 0.90–1.53 | 0.20 |
Characteristics analyzed include volume of admissions for general pain (headache, backpain, other pain, and weakness), admission to the hospital, and admission to the intensive care unit. OR >1 indicates that the characteristic is more likely to occur during the COVID-19 pandemic. Boldface indicates P less than 0.05.
CI, confidence interval; OR, odds ratio.
January 2 to February 25, 2020.
March 20 to April 27, 2020.
Discussion
We report data on how the COVID-19 pandemic has significantly affected the neurosurgical service at a single, major, metropolitan institution. At this high-volume neurosurgical center, a mean of 16.8 consultations to the neurosurgical service were seen per call-day during the pre–COVID-19 period. Following the announcement of a statewide stay-at-home order because of the COVID-19 pandemic, however, this number significantly decreased to 5.6 consultations per call-day. There are several plausible explanations for this trend. Beginning in March 2020, the United States began to see surges in the number of COVID-19 cases, which resulted in many cities instituting lockdowns and stay-at-home orders. Most people experienced major disruptions in their lifestyle, with the general population becoming less active, attending fewer social gatherings, and adhering to a quarantine regimen. Because of the severity and transmissibility of the disease, many people were also hesitant to visit the ED of major hospitals for nonemergent issues because of concerns about contracting or spreading the virus. Our data demonstrate a significant decrease in total cases per call-day, supporting this observation.
Our analysis also indicates differences with respect to the severity of illness among neurosurgical consultations after the onset of the pandemic. During the pandemic, we observed that a larger proportion of consultations required hospital admission, with a higher percentage of patients being admitted to the intensive care unit. Additionally, the proportion of consultations involving nonemergent presentations decreased. This indicates that patients who presented to the ED during the pandemic had cases that were typically more severe, which is likely a reflection of the reduction in nonemergent cases. Nonurgent ED use, particularly related to postoperative visits,9 can greatly increase hospital costs and ED wait times.10 One beneficial effect of the pandemic was this reduction in nonurgent ED use and its associated expense. Therefore, this observation highlights a beneficial area of discussion around how to limit nonurgent ED use after the end of the COVID-19 pandemic.
The reduction in the number of neurosurgery consultations was accompanied by a decrease in the number of overall neurosurgical procedures performed. Although the percentage of consultations regarding cases that required an operation remained stable, the number of patients was almost threefold greater during the pre–COVID-19 period than during the COVID-19 period (176 vs. 63 consultations involving an operation). This decrease in caseload may have repercussions on the educational experience of residents who are seeking exposure to a variety of operative pathologies.11 , 12 A possibility remains that individuals who require surgical care are deliberately postponing treatment because of concerns regarding infection or because of the negative economic consequences of the pandemic, which could result in a surge of surgical cases after the end of the COVID-19 pandemic. Whether these potential surgical cases are deferred or will never be treated remains uncertain, however. A lower volume of consultations also translates into fewer opportunities to practice interactions and assessments with patients, another skill that it is important to develop during residency. It is necessary to acknowledge these issues to develop teaching approaches that promote the continuation of resident training during the pandemic.
The trends in patient volume and illness severity provide insight into the pandemic's significant indirect effects on public health for patients without COVID-19.13 The pandemic has led to patient reluctance to seek care, even for acute, life-threatening events such as stroke14 , 15 and incarcerated hernias.16 Although EDs are experiencing a drastic decrease in patient visits, it is unlikely that the incidences of stroke, ruptured vascular malformations, seizures, acute hydrocephalus, and other morbidities requiring emergent neurosurgical attention and care have decreased in the population. Postponing medical care for these conditions can have dire consequences, resulting in a higher likelihood of severe, long-lasting neurological deficits or death. This trend can also be seen in patients with tumor and cerebrovascular disease withot hemorrhage, where patients may have been reluctant to present in an emergent setting with mild symptoms because they feared being exposed to COVID-19, which may have delayed diagnosis. Quantifying trends in neurological patient outcomes before and during the pandemic warrants further study.
This study has several limitations. The retrospective nature of our data collection could result in both observer bias and interpretation bias. Our data are drawn from ED consultations to the neurosurgery service at a single institution and may not be representative of other hospitals that have different experiences. Because our data represent oune of the highest-volume centers for neurosurgery in the United States, however, we believe our analysis highlights important areas of discussion for the practice. Only ED consultations were included in this study, and in-house and transfer consultations were excluded from our analysis. This poses a limitation insofar as the full volume of all types of neurosurgical consultations was not included. The small sample size of patients seen after the start of the COVID-19 pandemic means that the study is statistically underpowered. Regardless, we were still able to identify important trends in the data.
Conclusions
Neurosurgical consultations during the COVID-19 pandemic have significantly decreased, with a substantially lower overall number of consultations necessitating operative interventions. Importantly, a greater percentage of patients are presenting with more severe concerns, reflecting the significant decrease in the relative number of cases involving nonemergent neurological conditions. Further studies on the effect of the decreased volume of neurosurgical consultations on resident education and patient care are warranted.
CRediT authorship contribution statement
Stefan W. Koester: Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Visualization, Writing - original draft. Joshua S. Catapano: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation. Kevin L. Ma: Data curation, Formal analysis, Investigation, Writing - original draft. Anna R. Kimata: Data curation, Formal analysis, Investigation, Writing - original draft. Joseph M. Abbatematteo: Writing - review & editing. Corey T. Walker: Writing - review & editing. Tyler S. Cole: Writing - review & editing. Alexander C. Whiting: Writing - review & editing. Francisco A. Ponce: Writing - review & editing. Michael T. Lawton: Funding acquisition, Resources, Validation, Writing - review & editing.
Acknowledgments
The authors thank the staff of the Neuroscience Publications office at Barrow Neurological Institute for help with manuscript preparation.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Hemingway J.F., Singh N., Starnes B.W. Emerging practice patterns in vascular surgery during the COVID-19 pandemic. J Vasc Surg. 2020;72:396–402. doi: 10.1016/j.jvs.2020.04.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir. 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hartnett K.P., Kite-Powell A., DeVies J., et al. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nopp S., Janata-Schwatczek K., Prosch H., et al. Pulmonary embolism during the COVID-19 pandemic: decline in diagnostic procedures and incidence at a University Hospital. Res Pract Thromb Haemost. 2020;4:835–841. doi: 10.1002/rth2.12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Filippo O., D'Ascenzo F., Angelini F., et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. New Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tam C.F., Cheung K.S., Lam S., et al. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13:e006631. doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Jabir A., Kerwan A., Nicola M., et al. Impact of the coronavirus (COVID-19) pandemic on surgical practice—part 1. Int J Surg (London, England) 2020;79:168–179. doi: 10.1016/j.ijsu.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hills J.M., Khan I., Sivaganesan A., et al. Emergency department visits after elective spine surgery. Neurosurgery. 2019;85:E258–E265. doi: 10.1093/neuros/nyy445. [DOI] [PubMed] [Google Scholar]
- 10.Uscher-Pines L., Pines J., Kellermann A., Gillen E., Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manage Care. 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 11.Bambakidis N.C., Tomei K.L. Editorial. Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg. 2020;133:12–13. doi: 10.3171/2020.3.JNS20965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi B.D. Editorial. A neurosurgery resident's response to COVID-19: anything but routine. J Neurosurg. 2020;133:16–17. doi: 10.3171/2020.4.JNS201028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenbaum L. The untold toll—the pandemic's effects on patients without Covid-19. N Engl J Med. 2020;382:2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 14.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of COVID-19 on stroke evaluation in the United States. N Engl J Med. 2020;383:400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lange S.J., Ritchey M.D., Goodman A.B., et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. MMWR Morbid Mortal Wkly Rep. 2020;69:795–800. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lima D.L., Pereira X., Dos Santos D.C., Camacho D., Malcher F. Where are the hernias? A paradoxical decrease in emergency hernia surgery during COVID-19 pandemic. Hernia. 2020;24:1141–1142. doi: 10.1007/s10029-020-02250-2. [DOI] [PMC free article] [PubMed] [Google Scholar]