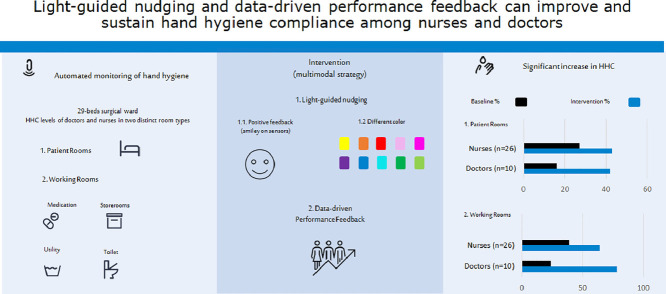
Graphical Abstract
Key Words: Electronic monitoring, Surveillance, Health care-acquired, Infection prevention, Adherence
Abstract
Background
Evidence-based practices to increase hand hygiene compliance (HHC) among health care workers are warranted. We aimed to investigate the effect of a multimodal strategy on HHC.
Methods
During this 14-month prospective, observational study, an automated monitoring system was implemented in a 29-bed surgical ward. Hand hygiene opportunities and alcohol-based hand rubbing events were measured in patient and working rooms (medication, utility, storerooms, toilets). We compared baseline HHC of health care workers across periods with light-guided nudging from sensors on dispensers and data-driven performance feedback (multimodal strategy) using the Student's t test.
Results
The doctors (n = 10) significantly increased their HHC in patient rooms (16% vs 42%, P< .0001) and working rooms (24% vs 78%, P= .0006) when using the multimodal strategy. The nurses (n = 26) also increased their HHC significantly from baseline in both patient rooms (27% vs 43%, P = .0005) and working rooms (39% vs 64%, P< .0001). The nurses (n = 9), who subsequently received individual performance feedback, further increased HHC, compared with the period when they received group performance feedback (patient rooms: 43% vs 55%, P< .0001 and working rooms: 64% vs 80%, P< .0001).
Conclusions
HHC of doctors and nurses can be significantly improved with light-guided nudging and data-driven performance feedback using an automated hand hygiene system.
Hospital-acquired infections (HAIs) continue to burden patients, health care workers (HCWs) and society by increasing morbidity, mortality, absenteeism and treatment costs.1, 2, 3
The coronavirus disease 2019 pandemic has underlined the importance of effective infection prevention measures in hospitals, including proper hand hygiene. HCWs are at the front-line, and their constant exposure to infected patients and contaminated surfaces puts them at risk of acquiring and transmitting pathogens.4 Their adherence to hand hygiene guidelines is vital in combatting infectious diseases in hospitals, especially HAIs and now also severe acute respiratory syndrome coronavirus 2.5 Adequate hand hygiene among HCWs can prevent an estimated 15%-30% of the HAIs6, 7, 8 but compliance remains suboptimal.9
Many strategies have tried to improve the hand hygiene compliance (HHC) of HCWs but most effects are small to moderate and often short term.6 , 10 , 11 A recent Cochrane review identified 26 studies which assessed the combinations of the following strategies: availability, education, reminders (verbal and written), performance feedback, administrating support, and staff involvement. The authors conclude that the strategies may improve the HHC, but the certainty of evidence varies from low to moderate and the most effectful method remains unclear.12 Two systematic reviews found that multimodal strategies were more successful in improving HHC rates of HCWs than single interventions.13 , 14 Moreover, the improvement strategies directed toward education, motivation, and continuous feedback proved to be effective. The authors also conclude that we should be more creative in the application of alternative improvement activities.
Now automated hand hygiene monitoring systems create an opportunity to provide real-time data and feedback using light-guided nudging (Sani nudge; Copenhagen, Denmark, https://saninudge.com. Accessed September 20, 2020). The author group has previously described their experiences with the automated hand hygiene monitoring system from a development and implementation perspective.15
Nudging is a friendly reminder to encourage desired behavior. It can be anything from posters to sounds or dynamic lights that change over time to mitigate “banner blindness.” However, the impact of nudges on clinicians’ behavior has only recently started to be formally evaluated and it is mostly investigated using static interventions, such as posters, signs, stickers, brochures, letters and emails.16 , 17 Given the potential of “nudge” strategies to impact on clinicians’ behaviors, efforts to describe the application and potential effect of such strategies on HHC are warranted.
We aimed to determine if a multimodal strategy, consisting of light-guided nudging and data-driven performance feedback on group and individual levels, can be used in a clinical context as a supporting tool to improve HHC among HCWs.
Methods
Study design and setting
We conducted a single-site, prospective, observational, quality improvement study between February 2018 and April 2019 in a surgical department with 29 beds (3 single, 1 twin, and 8 multibedrooms) as a substudy of a multiregional project.15 Some data from the present cohort have been published elsewhere.15 However, the hand hygiene improvement data have not previously been reported. This ward was chosen because it had a history of infectious disease outbreaks and, although normally contained within few weeks, we had the assumption that hand hygiene could be improved.
In Denmark, WHO's “My 5 Moments for Hand Hygiene” is the standard practice.18 , 19 We focused on alcohol-based hand rubbing based on the Danish national hygiene guidelines for HCWs stating that hand washing must always be followed by alcohol-based hand rubbing.19
Study subjects and data collection
We included both doctors and nurses from the surgical ward of which 17 of the nurses were also included in our previous study.15 Participation in the study was voluntary and data were anonymized to both study participants and investigators, except from a group of 9 nurses who volunteered to receive their own hand hygiene results via a weekly email to test how individualized performance data affect the performance. No information about the study subjects besides health care profession was obtained to ensure anonymity. All participants were briefed about the study purposes and placement of the hand hygiene system prior to study initiation.
Data were collected using an automated hand hygiene monitoring system (Sani nudge, Copenhagen, Denmark, https://saninudge.com. Accessed September 20, 2020). Sensors were placed on the existing alcohol-based hand rub dispenser solutions from where every hand hygiene event was registered, as previously described.15
In brief, the sensors had a built-in nudging feature with discrete light symbols which was activated during selected periods of the study (Fig 1 A). Other sensors were placed above the patient beds, creating a patient zone around each bed (Fig 1B). This allows the system to be used for monitoring WHO moments 1 (before touching a patient), 4 (after touching a patient), and 5 (after touching patient near surroundings). Moments 2 (before clean/aseptic procedures) and 3 (after body fluid exposure/risk) were included in the data because many of these procedures also take place in the patient zone. However, it was not possible to distinguish them from the other moments. Finally, anonymous Bluetooth sensors were placed on the existing name badge of the HCWs and were coded to be either a doctor or a nurse (Fig 1C). The sensors made it possible to measure when an HCW had a hand hygiene opportunity and whether alcohol-based hand rubbing was performed in that moment. A hand hygiene data report was sent on a weekly basis to the infection control nurses and the head nurse who would then show it to the HCWs in the ward during bi-weekly meetings (Fig 1D). After the meeting a copy of the data were put on a bulletin board for display.
Fig 1.
The Sani nudge hygiene system: (A) Sensor on a dispenser registering the number of alcohol-based hand rubbing events and displaying a nudge (green smiley) as a reward when a sanitization is performed. (B) The patient zone (illustrated with blue) created by the sensor near the head of the patient bed. (C) An anonymous sensor on the name badge of each health care worker. The sensor is coded according to staff profession (doctors and nurses). (D) Data captured by the sensors are sent to a secure cloud-based server and stored at the device level. Weekly performance data on group level is sent to the infection control nurses and ward managers, shown at staff meetings and put up on bulletin boards.
The system did not measure physical contact but used clinically validated algorithms based on time and distance measurements in the patient zone to calculate whether contact was most likely to have taken place.
Hand hygiene improvement strategy
The study was divided into three phases (Table 1 ): In phase 1 (baseline), the system was implemented, and a compliance baseline was measured. The baseline functioned as a control period with data representing the current HHC status of the ward before the improvement initiatives began. All study participants were blinded to data during this period to minimize the risk of bias.
Table 1.
Study overview and description of the phases
| Phase | Period (months) | Description |
|---|---|---|
| 1. Baseline period | 2 | Control period: A period without any interventions, reflecting the current hand hygiene compliance of the ward. |
| 2. Group intervention (team data and nudging) | 12 | Data-driven performance feedback: The head nurse and hygiene coordinator presented the department's hand hygiene compliance for each room type (patient room, mediation room, staff toilet, dirty and clean utility rooms) followed by an open discussion on how to overcome hand hygiene barriers. A copy of the results would be put on a bulletin board for display. Light-guided nudging: The Sani nudge sensors, located on existing alcohol-based hand rub dispensers, used visual nudges (lights and symbols) to bring staff's attention towards hand hygiene. The visual nudges appeared when staff was in a situation that required hand sanitization. Once a sanitization was performed, a smiley appeared to complete the positive feedback loop. The nudging was switched on and off with different intervals and in a random manner to avoid banner blindness. |
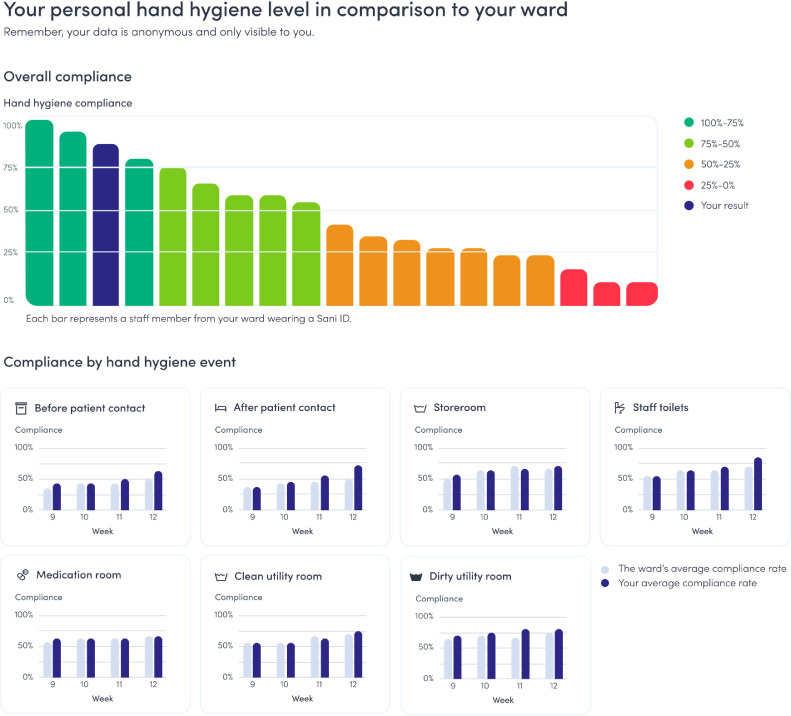
| 3. Individual intervention | 4 | Data-driven performance feedback: 8 months into phase 2, 9 nurses started receiving individual performance feedback which consisted of weekly reports send by email directly to each of them. The nurses were able to see their own compliance data in each room as well as before and after patient contact. They were also able to compare their own results with the rest of their colleagues’ group compliance. |
During phase 2 (group intervention: Data-driven performance feedback and light-guided nudging), the head nurse and the hygiene coordinator in the ward presented the HHC to their colleagues in the ward at short (5-10 minutes) bi-weekly meetings. All HCWs at work participated in the meetings. The data were shown as a general compliance number of the ward and stratified according to the following 6 room types: Patient room, medication room, dirty utility room (sluice room for soiled goods), clean utility room (sluice room for storage of clean goods), storeroom and staff toilet. The agenda of the meetings were:
-
1
Summary (awareness and follow-up): The head nurse and hygiene coordinator provided an overview on the previous week's HHC to make sure that everyone was updated on the most recent data. They also followed up on the previous week's goal as an evaluation of the performance.
-
2
Open discussion (knowledge distribution): The summary was followed by an open discussion in plenum assessing barriers towards hand hygiene. The question was: Why do you think we see these compliance numbers and how can we improve even further? Based on the input during the meetings and identification of potential knowledge gaps, the hygiene coordinator would host additional training sessions with the HCWs on a regular basis.
-
3
Focus (guided practice): The head nurse and hygiene coordinator selected and presented a specific hand hygiene opportunity to improve for the next week(s). The head nurse repeated the hygiene guidelines related to the specific focus of the week and gave clear and simple instructions on how to be compliant. An example: “Focus of the week is the ‘before patient contact’-moments. The guidelines state that we must perform hand hygiene before touching a patient (moment 1). As a goal the following week, we must all remember to sanitize hands every time we are walking into a patient room, before touching a patient.”
In addition, the nudging feature of the system was switched on periodically during phase 2. The nudges consisted of lights in 10 different colors (yellow, orange, red, pink, magenta, purple, blue, turquoise, dark green, and lime) which were displayed by the sensors on the dispensers (Fig 1A). A nudge was provided when staff approached a dispenser and once alcohol-based hand rubbing was performed. In order to avoid banner blindness (ie, unconsciously desensitization of a stimuli over time due to repeated exposure), the nudging mode (light) and length of time were switched on and off at random. The nudging colors were also displayed in a random manner. The symbols switched between random lights (cue) to increase awareness and green smileys after sanitizations (reward) to reinforce the desired behavior and create a persistent routine.
During phase 3 (individual intervention: Performance data on an individual level), 9 nurses volunteered to receive weekly individual compliance data by email in order to personalize the feedback. This was done automatically by the system and was blinded to the head nurse, hygiene coordinator or the rest of the staff. Those not receiving individualized data continued as described in phase 2 for the rest of the study period.
Ethics
Pursuant to the Danish law, approval was queried and evaluated as not needed by both the Ethics Committee (J. no. H-16020755) and the Danish Data Protection Agency (J. no. 2018-312-0169).
Outcome
Our primary analysis focused on the effect of light-guided nudging and data-driven performance feedback as a combined intervention (multimodal strategy). We compared the mean HHC between the baseline period and the intervention period. The secondary analysis evaluated the effect of individual performance feedback.
Statistical analysis
Hand hygiene performance rates were calculated by dividing hand hygiene events (number of hand disinfections using alcohol-based hand rub dispensers) by hand hygiene opportunities. Statistical analyses were performed using Microsoft Power BI (version 2.66.5376.2521, Microsoft, Redmond, Washington, DC) and GraphPad Prism (version 8.4.2.GraphPad Inc., La Jolla, CA).
Kolmogorov-Smirnov and Shapiro-Wilk normality tests were performed. Due to parametric distribution, continuous variables are presented as means with standard error of the mean. For the primary analysis, the differences between means were assessed using the Student's unpaired t test. The unpaired t test was chosen as a predefined analysis because the hand hygiene events were aggregated on day level and not on person level due to anonymity of the HCWs . P values <.05 were considered to indicate statistical significance.
Results
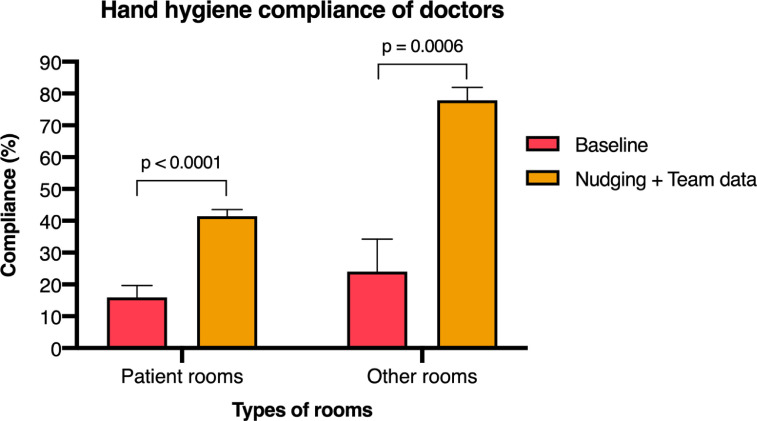
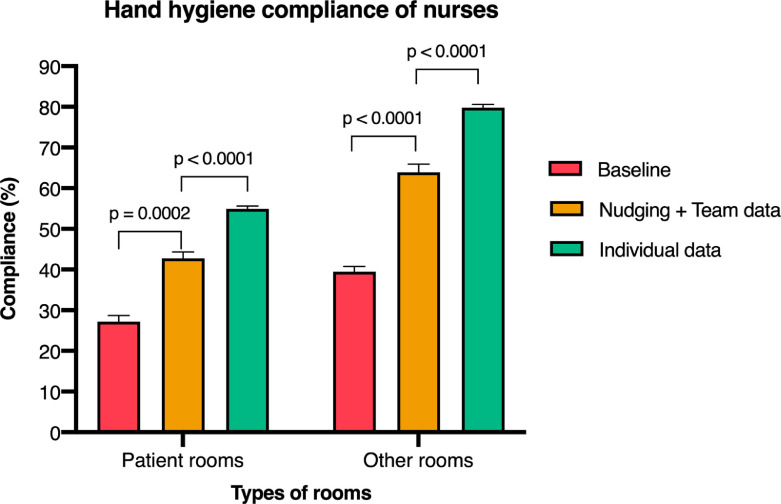
We enrolled 26 nurses and 10 doctors. The system registered an average of 5,000 hand hygiene opportunities in the ward per week for these 36 HCWs during the study period. In general, the HHC was lowest in the patient rooms compared with the other rooms for both the doctors and the nurses (Fig. 2 and 3 ).
Fig 2.
Individualized data-driven performance feedback. Nine nurses received individualized performance feedback consisting of weekly reports send by emails directly to each of them. The nurses were able to see their own compliance data in each room as well as before and after patient contact. They were also able to compare their own results with the rest of their colleagues’ group compliance.
Fig 3.
Hand hygiene compliance of the doctors (n = 10) in the surgical ward before and after nudging and performance feedback was introduced. Compliance is calculated as an average standard error of the mean during the study period.
Hand hygiene compliance of the doctors
The doctors had a baseline HHC of 16% in the patient rooms and 24% in the other rooms in the ward. HHC increased significantly to 42% (P< .0001) in the patient rooms and to 78% (P = .0006) in all other situations once the nudging feature was activated and the group performance feedback used (Fig 3).
The doctors were more likely to sanitize hands after rather than before patient contact during the baseline period (21% vs 11%, respectively). The same behavioral pattern was observed during the period with nudging and performance feedback (53% vs 21%).
Hand hygiene compliance of the nurses
The nurses had a baseline HHC of 27% in the patient rooms and 39% in the rest of the rooms in the ward. HHC increased significantly to 43% (P= .0002) in the patient rooms and to 64% (P< .0001) in all other situations once the nudging feature was activated and the group performance feedback provided (Fig 4 ). The HHC of the nurses receiving individual performance feedback further increased to 55% (P< .0001) in the patient rooms and to 80% (P< .0001) in all other situations compared with the period when group level data and nudging were provided (Fig 4).
Fig 4.
Hand hygiene compliance of the nurses (n = 26) in the surgical ward before and after nudging and performance feedback was introduced, and hand hygiene compliance of the 9 nurses receiving individual data. Compliance is calculated as an average standard error of the mean during the study period.
As with the doctors, the nurses were more likely to sanitize hands after rather than before patient contact during the baseline period (35% vs 19%, respectively). The same pattern was observed during nudging and group performance feedback (50% vs 36%) as well as during individual performance feedback (61% vs 49%).
Discussions
To our knowledge, this is the first study to examine the combinatory effect of data-driven performance feedback and light-guided nudging on HHC. The multimodal intervention significantly increased HHC of both doctors and nurses. The doctors had the lowest baseline compliance but seemed to be very responsive to the intervention and reached the same compliance levels as the nurses in the patient rooms and even higher levels in the working rooms. However, the nurses receiving individual performance feedback demonstrated the best performance in all the different room types.
A reason for the improvements observed could be the reduction in cognitive biases. When HAIs manifest several days after exposure, HCWs do not encounter the consequences of poor hand hygiene and they could consider their risk of causing infections negligible.16 When being reminded about the importance of good hand hygiene through performance feedback and via nudges in the moment, some of these cognitive barriers are removed.20
The baseline HHC was low but comparable to other studies using automated hand hygiene monitoring systems while the improvements seen in this study are some of the highest reported.21 The HHC was lowest in the patient rooms both before and after the intervention period. One possible factor could be that the highest number of opportunities was measured in these rooms, making higher performance more difficult. This is an important factor because most other monitoring systems only measure compliance upon room entry and exit despite that several hand hygiene opportunities occur near the patient during a single visit.21 The Sani nudge system measures compliance around the patient bed, providing a more detailed picture of the hand hygiene behavior when performing patient-centered clinical tasks. This is of particular relevance in multiple bedrooms where HCWs risk moving from patient to patient without performing hand hygiene.
The HHC is comparable to studies using video-monitored direct observation systems which is often considered the highest technical standard but has limited implementation possibilities due to privacy.22 , 23 The findings of this study suggest that the Sani nudge system can be used when you want to measure HHC in hospital settings according to WHO's “My 5 Moments” or hospitals who needs a more nuanced picture of the hand hygiene situation in the patient rooms than room entry and exit measurements can provide.
Some limitations should be considered when interpreting the results. First, a small number of HCWs (n = 36) were included and their behavior might not be representative for other HCWs. However, the system collected a high number of opportunities compared with studies performing direct observations which provides robustness to the analyses and increases the validity. In addition, data collection was done 24/7 for 14 months whereas direct observation studies normally do it sporadically during daytime and on weekdays only, presenting a limited picture of the true hygiene performance.
Second, there might have been some degree of selection bias toward the nurses choosing to receive individual data. As this was based on volunteering, it is possible that those whom felt confident about their own performance were more likely to volunteer. It was not possible to investigate if they were also the top performers during the baseline period because their data was anonymized up until they consented to have individual data collected. Despite this consideration, the nurses significantly improved once they started receiving individualized data compared to when they received data on group level. An explanation could be that the increased insights into their own performance reduced the Dunning-Kruger effect even further.24
Third, the hand hygiene system did not measure the quality of the alcohol-based hand rubbing which also has a significant impact on the effectiveness to prevent the spread of pathogens. Instead we learned that the hand hygiene system should be used as a prioritization tool for the hygiene organization to identify wards, professions and hygiene moments (eg, before and after patient contact) where hand hygiene performance is good and where there is room for improvement. It allows the management or infection prevention team to direct their limited resources to where it is mostly needed and have the highest impact in terms of infection prevention risk. Creating a transparent hand hygiene performance system also enhances an ongoing knowledge sharing of best practices which is highly needed in infection prevention during routine and outbreak situations.25
Finally, we did not note down the HCWs who attended the bi-weekly data presentation meetings and we can therefore not assure that all HCWs got exposed to the data performance intervention. We did put a copy of the performance results on a bulletin board for display after each meeting to mitigate the risk of not being exposed to the information. Future studies should consider sending out emails or using other relevant approaches to ensure that all team members get exposed to the performance feedback interventions.
Conclusions
We found that HHC with sanitizer of both doctors and nurses can be significantly improved with light-guided nudging and data-driven performance feedback on group and individual level using an automated hand hygiene system. This study provides justification for continued investigation on how improvement strategies can be designed to achieve an optimal HHC with limited efforts and resources.
Acknowledgments
We thank all the HCWs who took part in the study.
Footnotes
Conflicts of interest: None to report.
Funding: This study was partly funded by the Danish Ministry of Health (J. no. 1608966).
References
- 1.Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene infect control programme. Lancet Lond Engl. 2000;356:1307–1312. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 2.Burke JP. Infection control—a problem for patient safety. N Engl J Med. 2003;348:651–656. doi: 10.1056/NEJMhpr020557. [DOI] [PubMed] [Google Scholar]
- 3.Bates DW, Larizgoitia I, Prasopa-Plaizier N, Jha AK. Research priority setting working group of the WHO world alliance for patient safety. Global priorities for patient safety research. BMJ. 2009;338:b1775. doi: 10.1136/bmj.b1775. [DOI] [PubMed] [Google Scholar]
- 4.Phan LT, Sweeney DM, Maita D, et al. Respiratory viruses in the patient environment. Infect Control Hosp Epidemiol. 2020;41:259–266. doi: 10.1017/ice.2019.299. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of healthcare workers, including key considerations for occupational safety and health Available at:https://www.who.int/docs/default-source/coronaviruse/who-rights-roles-respon-hw-covid-19.pdf?sfvrsn=bcabd401_0. Assessed September 20, 2020.
- 6.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet Lond Engl. 2003;362:1225–1230. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 7.Harbarth S, Sax H, Gastmeier P. The preventable proportion of nosocomial infections: an overview of published reports. J Hosp Infect. 2003;54:258–266. doi: 10.1016/s0195-6701(03)00150-6. quiz 321. [DOI] [PubMed] [Google Scholar]
- 8.Sickbert-Bennett EE, DiBiase LM, Willis TMS, Wolak ES, Weber DJ, Rutala WA. Reduction of healthcare-associated infections by exceeding high compliance with hand hygiene practices. Emerg Infect Dis. 2016;22:1628–1630. doi: 10.3201/eid2209.151440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31:283–294. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 10.Pittet D. Improving compliance with hand hygiene in hospitals. Infect Control Hosp Epidemiol. 2000;21:381–386. doi: 10.1086/501777. [DOI] [PubMed] [Google Scholar]
- 11.Stewardson AJ, Sax H, Gayet-Ageron A, et al. Enhanced performance feedback and patient participation to improve hand hygiene compliance of health-care workers in the setting of established multimodal promotion: a single-centre, cluster randomised controlled trial. Lancet Infect Dis. 2016;16:1345–1355. doi: 10.1016/S1473-3099(16)30256-0. [DOI] [PubMed] [Google Scholar]
- 12.Gould DJ, Moralejo D, Drey N, Chudleigh JH, Taljaard M. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev. 2017;9 doi: 10.1002/14651858.CD005186.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naikoba S, Hayward A. The effectiveness of interventions aimed at increasing handwashing in healthcare workers—a systematic review. J Hosp Infect. 2001;47:173–180. doi: 10.1053/jhin.2000.0882. [DOI] [PubMed] [Google Scholar]
- 14.Huis A, van Achterberg T, de Bruin M, Grol R, Schoonhoven L, Hulscher M. A systematic review of hand hygiene improvement strategies: a behavioural approach. Implement Sci. 2012;7:92. doi: 10.1186/1748-5908-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iversen A-M, Kavalaris CP, Hansen R, Hansen MB, Alexander R, Kostadinov K, et al. Clinical experiences with a new system for automated hand hygiene monitoring: a prospective observational study. Am J Infect Control. 2020;48:527–533. doi: 10.1016/j.ajic.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 16.Caris MG, Labuschagne HA, Dekker M, Kramer MHH, van Agtmael MA, Vandenbroucke-Grauls CMJE. Nudging to improve hand hygiene. J Hosp Infect. 2018;98:352–358. doi: 10.1016/j.jhin.2017.09.023. [DOI] [PubMed] [Google Scholar]
- 17.Yoong SL, Hall A, Stacey F, et al. Nudge strategies to improve healthcare providers’ implementation of evidence-based guidelines, policies and practices: a systematic review of trials included within Cochrane systematic reviews. Implement Sci. 2020;15:50. doi: 10.1186/s13012-020-01011-0. 01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. My 5 moments for hand hygiene. Available at:http://www.who.int/infection-prevention/campaigns/clean-hands/5moments/en/. Assessed September 20, 2020.
- 19.Statens Serum Institut, Central Enhed for Infektionshygiejne. The Danish National Hand Hygiene Guidelines (Nationale Infektionshygiejniske Retningslinjer). Available at: https://hygiejne.ssi.dk/retningslinjer/nir. Assessed November 2, 2020.
- 20.Larson E. Monitoring hand hygiene: meaningless, harmful, or helpful? Am J Infect Control. 2013;41(5 suppl):S42–S45. doi: 10.1016/j.ajic.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 21.Ward MA, Schweizer ML, Polgreen PM, Gupta K, Reisinger HS, Perencevich EN. Automated and electronically assisted hand hygiene monitoring systems: a systematic review. Am J Infect Control. 2014;42:472–478. doi: 10.1016/j.ajic.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 22.Davis C. Infection-free surgery: how to improve hand-hygiene compliance and eradicate methicillin-resistant Staphylococcus aureus from surgical wards. Ann R Coll Surg Engl. 2010;92:316–319. doi: 10.1308/003588410X12628812459931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Armellino D, Hussain E, Schilling ME, et al. Using high-technology to enforce low-technology safety measures: the use of third-party remote video auditing and real-time feedback in healthcare. Clin Infect Dis. 2012;54:1–7. doi: 10.1093/cid/cis201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one's own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999;77:1121–1134. doi: 10.1037//0022-3514.77.6.1121. [DOI] [PubMed] [Google Scholar]
- 25.Sommerstein R, Geser S, Atkinson A, Tschan F, Morgan DJ, Marschall J. Knowledge sharing in infection prevention in routine and outbreak situations: a survey of the society for healthcare epidemiology of America Research Network. Antimicrob Resist Infect Control. 2017;6:79. doi: 10.1186/s13756-017-0237-5. [DOI] [PMC free article] [PubMed] [Google Scholar]