Abstract
Numerous pathophysiological conditions induce hypoxemia-related cardiopulmonary perturbations, decrements in exercise capacity, and debilitating symptoms. Accordingly, this study investigated the efficacy of an allosteric hemoglobin modulator (voxelotor) to enhance arterial oxygen saturation during low-intensity exercise in hypoxia. Eight normal healthy subjects (36 ± 7 yr; 73.8 ± 9.5 kg; 3 women) completed a submaximal cycling test (60 W) under normoxic (: 0.21; O2 partial pressure: 144 mmHg) and hypoxic (: 0.125; O2 partial pressure: 82 mmHg) conditions before (day 1) and after (day 15) 14 days of oral drug administration. While stationary on a cycle ergometer and during exercise, ratings of perceived exertion (RPE) and dyspnea, oxygen consumption (V̇o2), and cardiac output (Q) were measured noninvasively, while arterial blood pressure (MAP) and blood gases (, , and ) were measured invasively. The 14-day drug administration left shifted the oxygen-hemoglobin dissociation curve (ODC; p50 measured at standard pH and Pco2; day 1: 28.0 ± 2.1 mmHg vs. day 15: 26.1 ± 1.8 mmHg, P < 0.05). RPE, dyspnea, V̇o2, Q, and MAP were not different between day 1 and day 15. was similar during normoxia on day 1 and day 15 while stationary but higher during exercise (day 1: 95.2 ± 0.4% vs. day 15: 96.6 ± 0.3%, P < 0.05). was higher during hypoxia on day 15 while stationary (day 1: 82.9 ± 3.4% vs. day 15: 90.9 ± 1.8%, P < 0.05) and during exercise (day 1: 73.6 ± 2.5% vs. day 15: 84.8 ± 2.7%, P < 0.01). and were systematically higher and lower, respectively, after drug (P < 0.01), while the alveolar-arterial oxygen difference was unchanged suggesting hyperventilation contributed to the rise in . Oral administration of voxelotor left shifted the ODC and stimulated a mild hyperventilation, leading to improved arterial oxygen saturation without altering V̇o2 and central hemodynamics during rest and low-intensity exercise. This effect was more pronounced during submaximal hypoxic exercise, when arterial desaturation was more evident. Additional studies are needed to determine the effects of voxelotor during maximal exercise and under chronic forms of hypoxia.
NEW & NOTEWORTHY In humans, a novel allosteric hemoglobin-oxygen affinity modulator was administered to comprehensively examine the cardiopulmonary consequences of stabilizing a portion of the available hemoglobin in a high-oxygen affinity state during submaximal exercise in normoxia and hypoxia. Oral administration of voxelotor enhanced arterial oxygen saturation during submaximal exercise without altering oxygen consumption and central hemodynamics; however, the partial pressure of arterial carbon dioxide was reduced and the partial pressure of arterial oxygen was increased implying that hyperventilation also contributed to the increase in oxygen saturation. The preservation of arterial oxygen saturation and content was particularly evident during hypoxic submaximal exercise, when arterial desaturation typically occurs, but this did not influence arterial-venous oxygen difference.
Keywords: arterial blood gases, arterial oxygen saturation, GBT440, hematology, hypoxia, oxygen affinity, voxelotor
INTRODUCTION
Arterial hypoxemia occurs in numerous pathophysiological conditions such as during rapid ascent to altitude (18), in numerous cardiopulmonary diseases that cause ventilation-perfusion mismatch (2, 3), and during high-intensity exercise at sea level (7). Under such conditions, hypoxia-related cardiopulmonary and metabolic perturbations lead to decrements in exercise capacity and the development of symptoms such as dyspnea, with the extent of these manifestations often associated with the degree of arterial oxygen desaturation (35). Acute oxygen therapy (i.e., breathing oxygen enriched air) can reverse hypoxia-related perturbations and symptoms in some instances (2); however, logistical impediments (e.g., availability and transport of oxygen tanks) and the deleterious effects of chronic oxygen supplementation (30) limit its widespread application.
Increasing the affinity of hemoglobin (Hb) for oxygen, and thus left shifting the oxygen-hemoglobin dissociation curve (ODC), will increase arterial oxygen saturation for a given alveolar oxygen tension (10, 41) and potentially alleviate hypoxia-induced symptoms. However, increasing the affinity of Hb for oxygen induces an opposing effect at the tissue, such that for a given oxygen delivery, oxygen extraction is reduced. As such, prior attempts to increase or decrease the affinity of Hb for oxygen by modulating its structure and function have met with varying levels of success (16, 25, 31). Indeed, partially modulating the ODC leftward to promote loading of oxygen onto Hb at the lungs (11, 12) or rightward to promote unloading of oxygen at the tissue (37) can both provide beneficial outcomes during periods of extreme hypoxia; however, this has rarely been studied in humans. Of note, hypoxic exposure in humans can acutely induce a rightward ODC shift via increased 2,3-diphosphoglycerate, but this can be offset by a leftward shift under more chronic exposure via respiratory (and to a lesser extent renal) alkalosis (41). Importantly, the physiological mechanisms of oxygen transport are numerous and redundant, such that a mild ODC shift within normal physiological limits may coincide with compensatory changes in other factors (blood flow, ventilation, acid-base status) to preferentially preserve oxygen delivery (40).
Voxelotor, formerly known as GBT440, is an allosteric Hb oxygen affinity modulator that binds with high affinity and specificity to the alpha chain of hemoglobin; stabilizing it in the R-state (Oxy-Hb state) resulting in a left shift of the ODC. This effect is reversible and dose-dependent (29, 33) as measured by the percent occupancy of Hb (22, 27). Interestingly, in experimental models voxelotor-modified Hb retains the Bohr effect (i.e., releases more oxygen with increasing acidity) and responds to allosteric modulators such as 2,3-diphosphoglycerate, albeit with a mildly reduced rate of oxygen unloading (32). In animal studies under hypoxic conditions, ~30% drug occupancy of Hb has been shown to increase the overall affinity for oxygen in the blood, as evidenced by increased arterial oxygen saturation, with associated reduction in tissue hypoxia and improved survival (10). The clinical utility of increasing hemoglobin affinity for oxygen to reduce hemoglobin polymerization is profound for conditions such as sickle cell disease (13, 28) and potentially sickle cell trait during exercise at altitude (38) but may also be beneficial during rapid exposure to high altitude in healthy individuals (12). However, the cardiopulmonary consequences of stabilizing hemoglobin in the R-state during acute hypoxia in humans are not well characterized.
Accordingly, this study investigated the efficacy of voxelotor to preserve arterial oxygen saturation during normoxia and hypoxia in healthy individuals. It was hypothesized that administration of the study drug would improve arterial oxygen saturation and content during submaximal hypoxic exercise without altering oxygen uptake or hemodynamics.
METHODS
Subjects.
Eight recreationally active individuals (3 women, 24–48 yr) were recruited for the study. Participants were considered recreationally active if they attained a peak oxygen uptake above 40 ml·kg−1·min−1 for men or 35 ml·kg−1·min−1 for women during an incremental cycling test and were currently training >5 h/wk. Preparticipation health screening, in accordance with the American College of Sports Medicine, ensured subjects were apparently healthy nonsmokers, had no history of cardiopulmonary, metabolic, or neuromuscular disorders and were not taking any medications. The experimental procedures were registered (NCT03051711) and approved by the Institutional Human Research Ethics Committee in accordance with the Declaration of Helsinki, and all subjects provided written and witnessed informed consent.
Study design.
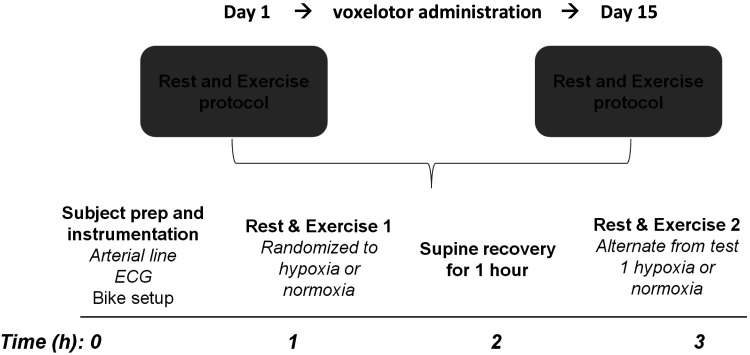
All subjects visited the laboratory on three occasions after abstaining from exercise for a minimum of 24 h. During the first visit, subjects underwent preparticipation health screening and performed an incremental cycling test for the determination of peak exercise values (oxygen uptake and heart rate). The two subsequent visits were undertaken before (day 1) and after (day 15) administration of 900 mg of oral, daily voxelotor for 14 days (Fig. 1). The study drug was provided as single 300-mg dose capsules with subjects taking three capsules daily.
Fig. 1.
Schematic of the study design and experimental procedures.
On day 1 and day 15 subjects underwent resting measures and performed a submaximal exercise test under normoxic and hypoxic conditions. At rest (stationary on the cycle-ergometer) and during submaximal exercise, pulmonary gas exchange, electrocardiography, and cardiac output were measured noninvasively, while hemodynamic variables were measured invasively, and blood samples were drawn for the determination of hematological variables.
Incremental exercise test.
Incremental exercise tests were performed on an upright, electronically-braked cycle ergometer (Lode BV, Groningen, The Netherlands) and comprised 3 min of warm-up at 60 W, before the workload was increased by 20–40 W every 3 min until the subject reached volitional fatigue. The increments were determined by estimating each individual’s peak power output and predicting a time to exhaustion between 15 and 18 min. Peak heart rate and oxygen uptake, measured via 12-lead ECG and indirect calorimetry (Ultima CardiO2, MGC Diagnostics, St Paul, MN), were calculated as the average of the highest two consecutive 30-s bin-averaged values attained during the test.
Submaximal exercise tests.
The submaximal cycling tests were performed on the same cycle ergometer and consisted of cycling at a fixed cadence (60–80 rpm) and work rate (60 W; 25 ± 6% of normoxic maximal exercise capacity) under normoxic (: 0.21; O2 partial pressure: 144 mmHg) and hypoxic (: 0.125; O2 partial pressure: 82 mmHg) conditions. Based on an estimated 25–30% reduction in exercise capacity during hypoxia (i.e., : 0.125), the relative exercise intensity during hypoxia would equate to ~30% of maximal hypoxic exercise capacity (1). Subjects were blinded to the inspired gas mixtures, which were humidified and delivered via a nonrebreathing valve. The order of the exercise tests was balanced on day 1, such that four subjects performed normoxia then hypoxia and four subjects performed hypoxia then normoxia. Subjects were instructed to lay supine for 1 h between the two exercise tests, and each subject’s test order was held constant on day 1 and day 15. Heart rate and cardiac rhythm were measured continuously via 12-lead ECG.
Pulmonary gas exchange and blood flow.
Breath-by-breath pulmonary gas exchange was measured using a pneumotach (Medical Graphics Corporation, St. Paul, MN) and mass spectrometer (MGA 1100, Marquette Electronics, Milwaukee, WI) configured with a commercially available software package (BreezeSuite 6.4.1 SP5, Medical Graphics Corporation, St. Paul, MN). Minute ventilation (V̇e), oxygen uptake (V̇o2), carbon dioxide production (V̇co2), partial pressure of end tidal O2 () and CO2 (), the respiratory exchange ratio (RER), and the ventilatory equivalents for V̇o2 (V̇e/V̇o2) and V̇co2 (V̇e/V̇co2) were quantified breath-by-breath before being averaged for analysis. The last 60 s of gas exchange data while stationary on the cycle ergometer and during exercise were reported for each condition (i.e., during normoxia and hypoxia). The partial pressure of oxygen in the alveoli () was calculated from the alveolar gas equation (39), and the alveolar-to-arterial O2 difference (A-a O2 difference) was quantified (blood gas analysis detailed below).
In addition, pulmonary blood flow as an estimate of cardiac output was measured via the open circuit acetylene ‘wash-in’ technique, as previously described and previously validated against direct Fick cardiac output measurements (4, 23). Briefly, subjects breathed on a nonrebreathing valve that enabled the inspired air to be switched between the normoxic/hypoxic gas mixture (described above) and a mixture of 0.9% He, 0.6% C2H2, with either 21% (normoxia) or 12.5% (hypoxia) O2 and balance N2. Subjects were instructed to breathe at 32 breaths/min, for 12 breaths, and cardiac output was estimated from the rate of disappearance of acetylene (4).
Hemodynamic and hematological measures.
Whole blood, serum, and plasma samples were collected via venipuncture and centrifugation before exercise on day 1 and day 15 for hematological, blood chemistry, and liver function assessments. Hemoglobin concentration was determined from complete blood count (CBC) measurements using fresh whole blood. The oxygen partial pressure at which Hb is 50% saturated (p50) was determined from oxygen association curves using fresh whole blood from an arterial blood sample and reported at standard conditions: 37°C, 40 mmHg carbon dioxide partial pressure, and a pH of 7.40 (Hemox Analyzer, TCS Scientific Corporation, Southampton). In our laboratory, the coefficient of variation for historical data in a large cohort of healthy control subjects was 3.7% with a mean p50 of 28.6 ± 1.05 mmHg. Erythropoietin (EPO) concentration, blood chemistries, and liver function were assessed from serum and plasma samples according to guidelines (26).
An arterial catheter (FA-04020, Arrow International Inc., Reading, PA) was placed under local anesthesia (2% lidocaine) by an experienced anesthesiologist for arterial blood draws and continuous blood pressure recording. At rest and during submaximal exercise, an arterial blood sample was collected for blood gas analysis (IL-1620, Instrumentation Laboratories, Lexington), including arterial oxygen saturation (), partial pressure of arterial oxygen () and carbon dioxide (), pH, Hb, and carboxyhemoglobin (COHb). Arterial oxygen content () was computed as = (1.34 × Hb × ) + ( × 0.0031). Venous oxygen content () and the arterial-venous oxygen content difference (Ca-v O2) were inferred by rearranging the Fick equation, and fractional O2 extraction was calculated by dividing Ca-v O2 difference by . Oxygen delivery (Do2) was calculated as the product of cardiac output and . Estimates of regional tissue oxygenation (r-So2) were continuously recorded from a sensor (SensSmart Model 8004CA, Nonin Medical, Inc., Plymouth, MN) placed on the midline of the Vastus Lateralis via near-infrared spectroscopy (Equanox Model 7600, Nonin Medical Inc, Minnesota).
Statistical analyses.
Normality of the data was determined using the Shapiro-Wilk test, and all significance testing was performed using SPSS software (v21.0, SPSS Inc., Chicago, IL). A paired samples t test was used to determine the effect of drug on clinical and hematological parameters on day 1 and day 15. Two-way ANOVA with repeated measures were performed for the normoxic and hypoxic trials to determine any differences in physiological parameters across condition (stationary on the cycle ergometer vs. submaximal exercise) and over time (day 1 vs. day 15). Where significant main effects were observed, post hoc adjustments were made when interactions were present and an alpha level of 0.05 was used for statistical significance.
RESULTS
Subject characteristics and baseline hematological measures.
Eight subjects (3 women, 24–48 yr) completed the study. Subject demographics and hematological measures at baseline (day 1) and on day 15 are presented in Table 1. Consistent with subject diaries documenting 100% adherence to drug dosing, pharmacokinetic assessment at day 15 confirmed pharmacologically active blood levels at 571 ± 82 µM.
Table 1.
Subject characteristics
| Characteristic | |
| Age, yr | 36 ± 7 |
| Height, cm | 176 ± 8 |
| Weight, kg | 73.8 ± 9.5 |
| Body mass index, kg/m2 | 23.7 ± 2.0 |
| Mean arterial pressure, mmHg | 88 ± 6 |
| Resting heart rate, beats/min | 69 ± 14 |
| Peak heart rate, beats/min | 176 ± 6 |
| Peak oxygen uptake, mL·kg−1·min−1 | 48.8 ± 6.7 |
Data are means ± SD.
Hemoglobin, blood chemistries, and liver function were unchanged on day 1 and day 15 and within the expected normal healthy ranges (Table 2). Laboratory assessments at rest including liver function tests, creatinine, lactate, and creatine kinase were not different on day 1 and day 15, with no adverse findings observed for hematological variables in any subject at any time point. In addition, compared with day 1, Hb at day 15 did not change while erythropoietin levels were increased but remained within the normal range, and p50 decreased by ~2 mmHg (Table 2).
Table 2.
Hematological measures at baseline and after 14 days of voxelotor administration (day 15)
| Hematological Measures | |
| Baseline | |
| Erythropoietin, mU/mL | 9.4 ± 3.8 |
| Hemoglobin, g/dL | 14.2 ± 1.0 |
| p50, mmHg | 28.0 ± 2.1 |
| Creatine kinase, U/L | 173 ± 151 |
| Day 15 | |
| Erythropoietin, mU/mL | 13.8 ± 4.9* |
| Hemoglobin, g/dL | 14.5 ± 1.4 |
| p50, mmHg | 26.1 ± 1.0* |
| Creatine kinase, U/L | 225 ± 262 |
Data are means ± SD. p50, oxygen tension at which hemoglobin is 50% saturated under standard conditions.
Significantly different from baseline.
Submaximal cycling tests.
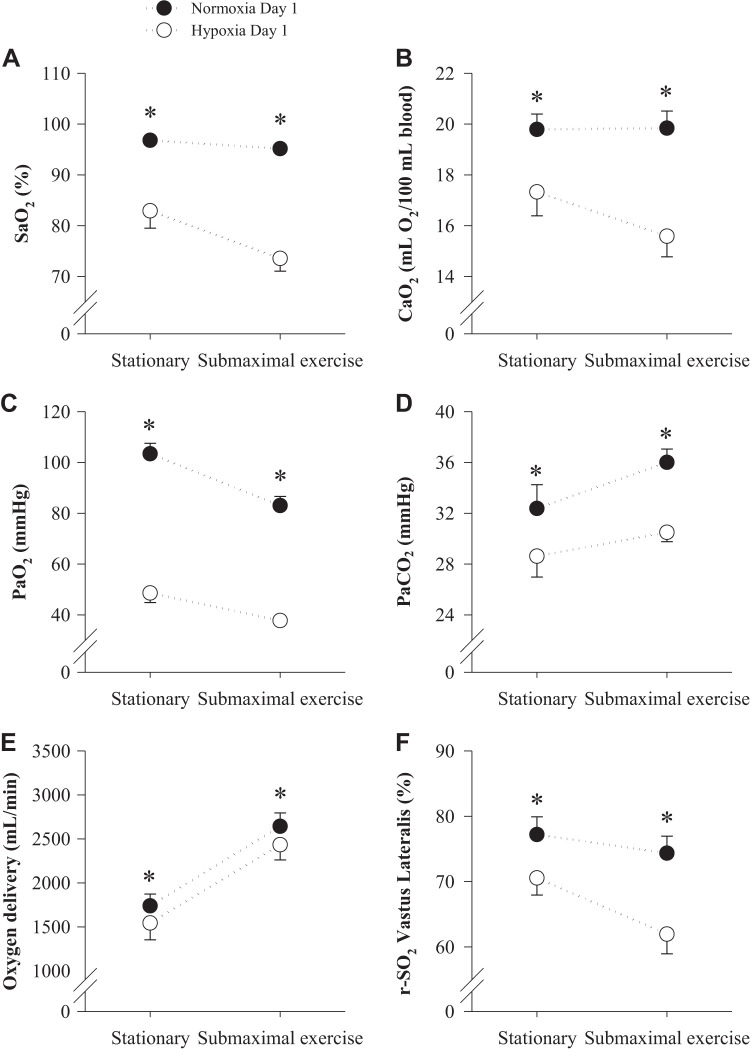
All subject data during the normoxic and hypoxic submaximal cycling tests were as expected, with typical hypoxic perturbations (e.g., increased V̇e, decreased and ) observed (Tables 3 and 4 and Fig. 2). During exercise, ratings of perceived exertion were not altered by hypoxia (7 ± 0 vs. 7 ± 0, P = 0.567) while dyspnea was marginally greater (0.6 ± 0.2 vs. 1.4 ± 0.5, P = 0.024). Ratings of perceived exertion and dyspnea were not different on day 1 and day 15 during both the normoxic (7 ± 0 vs. 7 ± 0, P = 1.00; 0.6 ± 0.2 vs. 0.4 ± 0.2, P = 0.451, respectively) and hypoxic (7 ± 0 vs. 7 ± 0, P = 0.598; 1.4 ± 0.5 vs. 1.0 ± 0.3, P = 0.451, respectively) exercise trials.
Table 3.
Hemodynamic, gas exchange, and blood gas measures while stationary on the cycle ergometer on day 1 and day 15
| Day 1 Normoxia | Day 15 Normoxia | Day 1 Hypoxia | Day 15 Hypoxia | |
|---|---|---|---|---|
| Hemodynamic variables | ||||
| Heart rate, beats/min | 88 ± 5 | 85 ± 6 | 86 ± 6 | 93 ± 4* |
| Mean arterial pressure, mmHg | 95 ± 3 | 95 ± 5 | 95 ± 4 | 95 ± 5 |
| Cardiac output, L/min | 8.7 ± 0.6 | 9.2 ± 0.7 | 8.8 ± 0.8 | 9.7 ± 0.6 |
| Gas exchange variables | ||||
| Oxygen uptake, mL/min | 481 ± 67 | 452 ± 46 | 428 ± 26 | 440 ± 52 |
| Carbon dioxide production, mL/min | 491 ± 68 | 443 ± 50 | 435 ± 37 | 486 ± 88 |
| Ventilation, L/min | 23 ± 4 | 23 ± 4 | 21 ± 2 | 29 ± 9 |
| Respiratory exchange ratio | 1.04 ± 0.07 | 0.98 ± 0.07 | 1.04 ± 0.05 | 1.08 ± 0.08 |
| Ventilatory equivalent for oxygen uptake | 52 ± 7 | 51 ± 5 | 52 ± 3 | 61 ± 10 |
| Ventilatory equivalent for carbon dioxide production | 48 ± 3 | 52 ± 2 | 50 ± 2 | 54 ± 4 |
| Alveolar oxygen partial pressure, mmHg | 112 ± 3 | 113 ± 4 | 57 ± 3 | 60 ± 3 |
| Alveolar-to-arterial oxygen difference, mmHg | 8 ± 2 | 10 ± 2 | 9 ± 1 | 9 ± 1 |
| Blood gas variables | ||||
| Arterial oxygen saturation, % | 96.8 ± 0.2 | 97.2 ± 0.2 | 82.9 ± 3.4 | 90.9 ± 1.8* |
| Arterial oxygen partial pressure, mmHg | 103 ± 4 | 105 ± 5 | 49 ± 4 | 51 ± 3 |
| Arterial carbon dioxide partial pressure, mmHg | 32 ± 2 | 29 ± 2 | 29 ± 2 | 27 ± 2 |
| Arterial oxygen content, mL O2/100 mL | 19.8 ± 0.6 | 19.7 ± 0.5 | 17.3 ± 0.9 | 18.5 ± 0.7 |
| Arterial-venous oxygen difference. mL O2/100 mL | 5.6 ± 0.8 | 5.2 ± 0.8 | 5.2 ± 0.7 | 4.6 ± 0.5 |
| Venous oxygen content, mL O2/100 mL | 14.2 ± 0.8 | 14.8 ± 0.5 | 12.1 ± 1.3 | 13.8 ± 0.6 |
| Fractional oxygen extraction, % | 28 ± 4 | 25 ± 1 | 31 ± 5 | 25 ± 2 |
| Carboxyhemoglobin, %hemoglobin | 1.2 ± 0.1 | 1.6 ± 0.1* | 1.2 ± 0.0 | 1.6 ± 0.1* |
| Bicarbonate, mmol/L | 23 ± 1 | 21 ± 1 | 22 ± 0 | 20 ± 1 |
| pH | 7.46 ± 0.0 | 7.47 ± 0.0 | 7.50 ± 0.0 | 7.49 ± 0.0 |
| Lactate, mmol/L | 2.0 ± 0.3 | 1.9 ± 0.5 | 2.0 ± 0.3 | 2.2 ± 0.4 |
Data are means ± SE. Significance accepted at P < 0.05.
Significantly different from day 1.
Table 4.
Hemodynamic, gas exchange, and blood gas measures during submaximal exercise on day 1 and day 15
| Day 1 Normoxia | Day 15 Normoxia | Day 1 Hypoxia | Day 15 Hypoxia | |
|---|---|---|---|---|
| Hemodynamic variables | ||||
| Heart rate, beats/min | 106 ± 5 | 112 ± 6 | 121 ± 5 | 124 ± 6 |
| Mean arterial pressure, mmHg | 100 ± 3 | 103 ± 5 | 107 ± 4 | 105 ± 6 |
| Cardiac output, L/min | 13.3 ± 0.5 | 13.6 ± 0.9 | 15.6 ± 0.7 | 16.3 ± 1.1 |
| Gas exchange variables | ||||
| Oxygen uptake, mL/min | 1,218 ± 76 | 1,332 ± 90 | 1,263 ± 69 | 1,261 ± 67 |
| Carbon dioxide production, mL/min | 962 ± 133 | 997 ± 104 | 1,097 ± 66 | 1,100 ± 71 |
| Ventilation, L/min | 32 ± 4 | 35 ± 4 | 41 ± 2 | 45 ± 5 |
| Respiratory exchange ratio | 0.78 ± 0.06 | 0.74 ± 0.03 | 0.87 ± 0.02 | 0.88 ± 0.04 |
| Ventilatory equivalent for oxygen uptake | 26 ± 2 | 27 ± 1 | 33 ± 1 | 36 ± 3 |
| Ventilatory equivalent for carbon dioxide production | 34 ± 1 | 36 ± 1 | 38 ± 1 | 41 ± 2 |
| Alveolar oxygen partial pressure, mmHg | 97 ± 3 | 102 ± 3 | 51 ± 1 | 54 ± 2 |
| Alveolar-to-arterial oxygen difference, mmHg | 14 ± 3 | 13 ± 2 | 13 ± 2 | 13 ± 2 |
| Blood gas variables | ||||
| Arterial oxygen saturation, % | 95.2 ± 0.4 | 96.6 ± 0.3* | 73.6 ± 2.5 | 84.8 ± 2.7* |
| Arterial oxygen partial pressure, mmHg | 83 ± 4 | 90 ± 7* | 38 ± 2 | 41 ± 2* |
| Arterial carbon dioxide partial pressure, mmHg | 36 ± 1 | 31 ± 2* | 31 ± 1 | 27 ± 1* |
| Arterial oxygen content, mL O2/100 mL | 19.8 ± 0.7 | 19.6 ± 0.6 | 15.6 ± 0.8 | 17.3 ± 0.7* |
| Arterial-venous oxygen difference, mL O2/100 mL | 9.3 ± 0.7 | 9.6 ± 0.6 | 8.2 ± 0.6 | 7.8 ± 0.3 |
| Venous oxygen content, mL O2/100 mL | 10.6 ± 0.7 | 10.0 ± 0.9 | 7.4 ± 0.9 | 9.5 ± 0.7* |
| Fractional O2 extraction, % | 47 ± 3 | 49 ± 4 | 53 ± 4 | 46 ± 2* |
| Carboxyhemoglobin, %total hemoglobin | 1.1 ± 0.1 | 1.5 ± 0.1* | 1.2 ± 0.0 | 1.7 ± 0.1* |
| Bicarbonate, mmol/L | 24 ± 0 | 21 ± 1 | 23 ± 0 | 20 ± 1 |
| pH | 7.46 ± 0.0 | 7.45 ± 0.0 | 7.49 ± 0.0 | 7.50 ± 0.0 |
Data are means ± SE. Significance accepted at P < 0.05.
Significantly different from day 1.
Fig. 2.
Measures of arterial oxygen saturation (; A), arterial oxygen content (; B), arterial partial pressure of oxygen (; C) and carbon dioxide (; D), and estimates of oxygen delivery (E) and regional tissue saturation (r-So2; F) while stationary on a cycle ergometer and during submaximal exercise under normoxic ( = 0.21, closed circles) and hypoxic ( = 0.125, open circles) conditions. *Significantly different from normoxia.
Pulmonary gas exchange and blood flow.
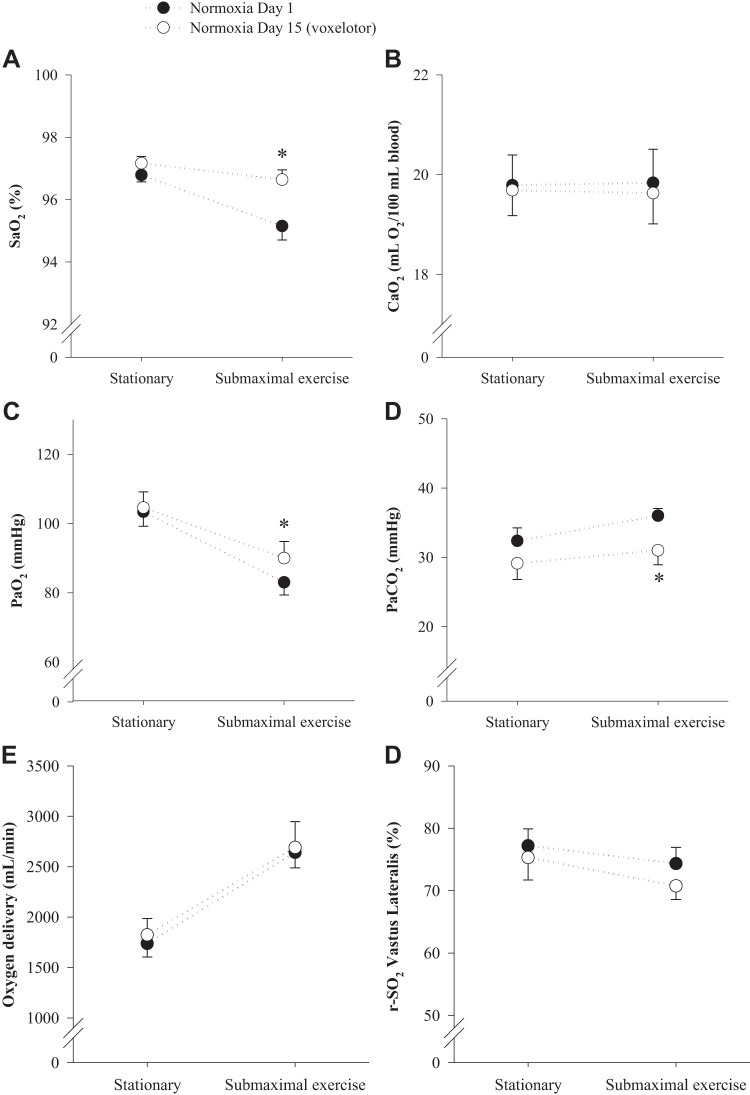
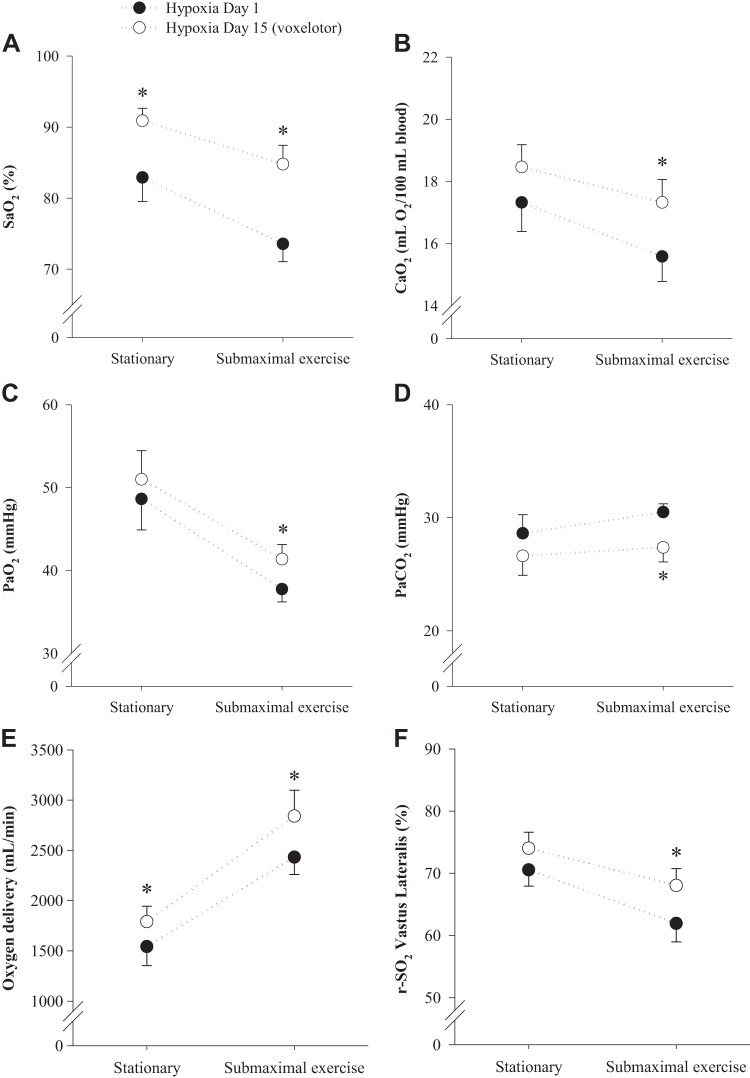
There were no differences in V̇o2, V̇co2, RER, and V̇e (and also respiratory rate and tidal volume) between day 1 and day 15 in both the normoxic and hypoxic trials (Tables 3 and 4). There was, however, a nonsignificant trend toward an increase in V̇e during the normoxic trial on day 15 compared with day 1 that led to a greater V̇e/V̇co2, but V̇e/V̇o2 was not different (Tables 3 and 4). Compared with day 1, was increased on day 15 during hypoxic exercise only, while was decreased during normoxic and hypoxic exercise. There was no difference in or A−a difference between day 1 and day 15 in either the normoxic or hypoxic trials (Tables 3 and 4).
Hemodynamics and hematology.
Heart rate increased slightly on day 15 during exercise in normoxia and at rest during hypoxia, while MAP, Q, and SVR were unchanged from day 1 to day 15 under all conditions (Table 3 and 4). The effects of hypoxia on blood gases at rest and during submaximal exercise are presented in Fig. 2. As expected, the hypoxia challenge reduced , , , , oxygen delivery, and regional tissue saturation (r−So2), when compared with normoxia. The effects of the study drug on blood gases at rest and during submaximal exercise under normoxic and hypoxic conditions are presented in Figs. 3 and 4, respectively. During normoxia, the study drug had no effect on blood gases at rest. However, during normoxic low-intensity exercise and were increased on day 15 compared with day 1, while was reduced (Fig. 3). During hypoxia, and were increased on day 15 at rest, while and were unchanged. During hypoxic low-intensity exercise , and were increased on day 15, compared with day 1, while was reduced (Fig. 4). The was not different on day 15 during normoxia but was higher during hypoxia, while the Ca-vO2 difference was unchanged between day 1 and day 15 under both normoxic and hypoxic conditions. Oxygen delivery and regional tissue saturation were similar during normoxia on day 1 and day 15, but higher during submaximal hypoxic exercise on day 15 compared with day 1 (Fig. 4). The increase in oxygen delivery during hypoxia combined with no change in Ca-vO2 difference during hypoxia, lead to a decrease in fractional O2 extraction during hypoxia (Table 3 and 4). COHb increased slightly on day 15 compared with day 1 but remained within normal range at all time points, while lactate and pH were not different in either trial or at any time points (Table 3 and 4).
Fig. 3.
Measures of arterial oxygen saturation (; A), arterial oxygen content (; B), arterial partial pressure of oxygen (; C) and carbon dioxide (; D), and estimates of oxygen delivery (E) and regional tissue saturation (r-So2; F) while stationary on a cycle ergometer and during submaximal exercise before (closed circles) and after (open circles) 14 days of oral voxelotor administration under normoxic ( = 0.21) conditions. *Significantly different from day 1.
Fig. 4.
Measures of arterial oxygen saturation (; A), arterial oxygen content (; B), arterial partial pressure of oxygen (; C) and carbon dioxide (; D), and estimates of oxygen delivery (E) and regional tissue saturation (r-So2; F) while stationary on a cycle ergometer and during submaximal exercise before (closed circles) and after (open circles) 14 days of oral voxelotor administration under hypoxic (: = 0.125) conditions. *Significantly different from day 1.
The relative contribution of V̇e, A-a O2 difference and drug to the total change in saturation during each condition (i.e., rest and exercise during normoxia and hypoxia) was estimated by partitioning out each component. Briefly, the change in due to V̇e alone was estimated from the alveolar gas equation by imputing the measured and RER, while keeping all other parameters constant. Then, the expected change in from a rise in purely due to V̇e and A-a O2 difference was estimated from the relevant portion of the standard ODC curve. During normoxic exercise (on the flat portion of the ODC), the rise in (~5 mmHg) from increased V̇e would account for an ~0.5% increase in (i.e., ~30% of the observed increase in ), while the change in A-a O2 difference would account for an ~0.1% of the change in . During hypoxic exercise, the rise in (~3 mmHg) from increased V̇e would account for an ~4% increase in (i.e., ~30–50% of the observed increase in ), while changes in A-a O2 were negligible during hypoxia.
DISCUSSION
This study demonstrates that once daily oral administration of voxelotor at 900 mg for 14 days was effective at increasing oxygen saturation under hypoxic conditions in a cohort of young healthy individuals. The affinity of Hb for oxygen was increased, leading to a left shift of the oxy-hemoglobin dissociation curve, resulting in improved arterial oxygen saturation and content, particularly during hypoxia. Oxygen consumption, V̇co2, pH and RER were unaffected by the study drug during normoxic and hypoxic submaximal exercise and the extraction of oxygen at the tissue was preserved (i.e., no change in a-vO2 difference); however, while V̇e was not significantly different, it tended to increase concomitant with reductions in and an increase in , suggesting factors other than the altered p50 (e.g., alveolar ventilation and A-a O2 difference) contributed to the rise in arterial oxygen saturation (detailed below).
Fourteen days of voxelotor administration resulted in a modest left shift, ~2 mmHg at p50, in the ODC. Similar to prior studies partially shifting the ODC left (11, 12) or right (16, 25, 37) during hypoxia, the increased arterial oxygen saturation and content after drug administration accompanied a commensurate change(increase) in venous oxygen content, such that oxygen consumption was not changed and adequate oxygen offloading from Hb was maintained (12). Indeed, exercise-induced reductions in venous oxygen content and widening of the arterial-venous oxygen difference (i.e., increased extraction of oxygen during exercise) were not altered by the drug during submaximal hypoxic exercise, suggesting that oxygen delivery and utilization at the muscle was preserved under these conditions (at rest and during very low intensity exercise). The increased regional tissue saturation may also reflect a preserved or enhanced oxygen delivery; however, this method does not distinguish between arterial/mixed/venous blood and intramuscular oxygen saturations. Of note, however, fractional O2 extraction (a-vO2 difference/) while not different before and after drug during normoxia, was decreased after drug during hypoxia suggesting that pharmacologically increasing oxygen delivery to the tissue does not improve O2 extraction and utilization during submaximal hypoxic exercise. Nonetheless, the comparable V̇o2, V̇co2 and pH before and after 14 days of voxelotor administration lends further support that transport of oxygen across the capillary and into the myocyte sufficiently matched skeletal muscle metabolism during low-intensity exercise (24).
Despite a mildly higher V̇e/V̇co2 and concomitant reduction in during hypoxic submaximal exercise after drug administration, the major determinants of oxygen delivery aside from Hb oxygen affinity (e.g., acid-base balance, ventilation, cardiac output) were predominantly unaltered by a modest left shift of the ODC. It is possible that changes in lung diffusion, alveolar ventilation and the alveolar-arterial O2 difference can also contribute to the increases in . Given that alveolar oxygen tension () and alveolar-arterial O2 difference were similar before and after drug (despite a trend toward a slight increase in on day 15), gross changes in lung diffusion likely did not contribute to the observed changes in arterial oxygen content and saturation (14). However, the higher and lower observed during exercise after voxelotor administration suggest that hyperventilation, in part, contributed to the preserved arterial saturation during hypoxic submaximal exercise (36). Using the alveolar gas equation to estimate the rise in and thus due purely to hyperventilation (i.e., independent from the effect of P50 or A-a O2 difference) suggests that approximately half of the increase in was due to a rise in from hyperventilation. Thus, the observed increase in on day 15 does not solely reflect the impact of drug, per se, but also any potential drug or study effect (e.g., metabolic acidosis, placebo effect) on ventilation and subject responses. Nonetheless, for a given ventilation arterial oxygen saturation remained higher during hypoxia after drug administration (Submaximal /V̇e = 1.83 on day 1 vs. 1.94 on day 15).
In conjunction with the increase in arterial oxygen saturation and perturbations in pulmonary gas exchange/arterial blood gases during low-intensity exercise after drug administration, hemodynamic responses to exercise during normoxia and hypoxia were largely unchanged. With the exception of a slight increase in heart rate at rest during hypoxia while on voxelotor, all other hemodynamic variables, both at rest and during low-intensity exercise, were not altered. The higher arterial oxygen content during hypoxia after administration of the study drug without a change in cardiac output (as well as perfusion pressure) suggests that increasing oxygen delivery to the tissue did not improve or impair steady-state aerobic metabolism. Thus, a modest left shift of the ODC did not alter skeletal muscle metabolism and function during normoxic and hypoxic submaximal exercise, underpinning the notion that the numerous physiological determinants of oxygen transport may compensate for any changes in Hb affinity that are within the normal physiological range (40). Determining the effects of voxelotor under more extreme forms of acute and chronic hypoxia, and during high-intensity exercise, which if sufficiently severe can encroach upon the compensability limits of the physiological determinants of oxygen transport and utilization (34), warrants further study to determine the clinical and physiological utility of left shifting the ODC. Nonetheless, these results are consistent with those in patients with sickle cell disease who underwent maximal exercise testing (cycle ergometry) without evidence of cardiopulmonary or metabolic compromise after 90 days of once daily 900 mg of voxelotor (21).
There are numerous parallels between high-altitude illness due to rapid hypoxic exposure in healthy individuals and the pathophysiological ails observed in chronic hypoxic diseases (18). Notably, hypoxia-related symptoms including dyspnea, malaise/lethargy and nausea are commonly reported in chronic hypoxic diseases and high-altitude sojourners alike (6, 17, 20), with normalization of arterial hypoxemia (either pharmacologically or via supplemental oxygen) the most common therapeutic intervention (18). However, increasing arterial oxygen saturation and content with the study drug did not alter perceptions of effort and dyspnea during hypoxic low intensity exercise, and may relate to mild metabolic acidosis and/or hypocapnea counteracting any beneficial effects from the rise in . The fall in without any change in pH and a trend toward lower bicarbonate suggests a possible metabolic stimulus for hyperventilation alongside bicarbonate buffering. Whether left shifting the ODC alleviates (or exacerbates) hypoxia-related symptoms during more severe and chronic hypoxic stimuli or with other pathological constraints should be explored during hypobaric hypoxia in addition to the acute normobaric hypoxic stimuli from this study.
Interestingly, 14 days of voxelotor supplementation resulted in a small increase in EPO (albeit within the normal range), suggesting a stimulus for EPO production may have been induced by drug. This is not surprising, given that under normoxic conditions with near 100% arterial saturation, left shifting the ODC is not expected to provide benefit and may decrease oxygen extraction fraction, thus stimulating compensatory mechanisms to increase erythropoiesis. While polycythemia was not evident during this 14-day study, increased Hb and hematocrit has been described with naturally occurring high affinity hemoglobin mutations (8, 9). Since whole body metabolic activity and oxygen extraction during low-intensity exercise were not altered by the study drug and were consistent between subjects, there may have been overnight and/or diurnal differences that lead to the variable increase in EPO (5, 15). At present, it cannot be ruled out that regional tissue hypoxia or altered renal O2 transfer did not prelude the observed increase in EPO. Although ambulatory measures of physical exertion and arterial saturation were not performed, the hemodynamic, metabolic and subjective ratings during rest and low-intensity exertion were not altered by the study drug. Nonetheless, higher-intensity exertional efforts and the presence of responders and nonresponders may have contributed to the variable changes in EPO (5, 15). Indeed, the participants each reported a regular exercise training regime that included varying amounts of high-intensity exercise and were asked to maintain their habitual exercise regimes throughout the study. Additional study is required to examine the impact of voxelotor during repeated bouts of high-intensity exercise, where transient tissue hypoxia may occur, and to determine the direct mechanisms by which voxelotor may stimulate EPO production.
Physiological and methodological considerations.
This study aimed to determine the effects of partially left shifting the ODC during submaximal exercise in healthy individuals. The potential benefits and consequences of increasing Hb affinity for oxygen in more chronic forms of hypoxia and during maximal exercise, particularly in clinical populations where exertional dyspnea and arterial desaturation are common, should be explored. To determine the physiological relevance of a small rise in EPO (with no change in Hb concentration) on the oxygen affinity of Hb, the effects of voxelotor on other important regulators of Hb affinity (e.g., 2,3-diphosphoglycerate concentration) should be explored in vivo. In vitro, however, voxelotor does not inhibit the Bohr effect or offloading effects of 2,3-DPG (32). Given the complex biochemical regulation of Hb and the numerous physiological determinants of oxygen transport – which are each both individually and collectively modulated by hypoxia – additional integrative physiology studies are warranted to determine the potential clinical and physiological utility of allosteric Hb modulators. Finally, this study incorporated both male and female participants, whom all stated using a form of contraception during the study timeline which may have altered natural hormonal regulation. As such we cannot exclude hormonal fluctuations as a potential confounding influence on differences ventilatory control on day 1 and day 15.
Conclusions.
This study demonstrates that increasing the oxygen affinity of hemoglobin in healthy individuals improves arterial oxygen saturation and content during hypoxia without altering V̇o2 or hemodynamic responses during submaximal exercise; however, the observed rise in was also caused by a concomitant mild hyperventilatory stimuli and thus a decrease in and increase in . Additional studies should investigate the clinical utility of hemoglobin oxygen affinity modulators in pathological conditions where exertional dyspnea and arterial desaturation are common, and during more severe hypoxia and exertion when the compensability limits of the oxygen transport system are reached.
GRANTS
The study was funded by Global Blood Therapeutics. G. M. Stewart is funded by an American Heart Association Postdoctoral Fellowship (AHA) 19POST34450022).
DISCLOSURES
J. Lehrer-Graiwer, K. Dufu, and N. E. Vlahakis are employees of Global Blood Therapeutics. None of the other authors has any conflicts of interest, financial or otherwise, to disclose.
AUTHOR CONTRIBUTIONS
G.M.S., S.C.C., T.J.C., C.M.W., M.J.J., J.L.-G., K.D., N.E.V., and B.D.J. conceived and designed research; G.M.S., S.C.C., T.J.C., M.J.J., T.B.C., and B.D.J. performed experiments; G.M.S., S.C.C., T.J.C., K.D., N.E.V., and B.D.J. analyzed data; G.M.S., S.C.C., T.J.C., C.M.W., J.L.-G., K.D., N.E.V., and B.D.J. interpreted results of experiments; G.M.S. and B.D.J. prepared figures; G.M.S., T.J.C., C.M.W., M.J.J., T.B.C., J.L.-G., K.D., N.E.V., and B.D.J. drafted manuscript; G.M.S., S.C.C., T.J.C., C.M.W., M.J.J., T.B.C., J.L.-G., K.D., N.E.V., and B.D.J. edited and revised manuscript; G.M.S., S.C.C., T.J.C., C.M.W., M.J.J., T.B.C., J.L.-G., K.D., N.E.V., and B.D.J. approved final version of manuscript.
ACKNOWLEDGMENTS
The authors acknowledge the valuable contributions from Briana Ziegler, Jennifer Isautier, and the Global Blood Therapeutics support team of Bella Oguno, Mary Poppenheimer, and Sandy Dixon.
REFERENCES
- 1.Agostoni P, Cattadori G, Guazzi M, Bussotti M, Conca C, Lomanto M, Marenzi G, Guazzi MD. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am J Med 109: 450–455, 2000. doi: 10.1016/S0002-9343(00)00532-5. [DOI] [PubMed] [Google Scholar]
- 2.Ballester E, Reyes A, Roca J, Guitart R, Wagner PD, Rodriguez-Roisin R. Ventilation-perfusion mismatching in acute severe asthma: effects of salbutamol and 100% oxygen. Thorax 44: 258–267, 1989. doi: 10.1136/thx.44.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barberà JA, Riverola A, Roca J, Ramirez J, Wagner PD, Ros D, Wiggs BR, Rodriguez-Roisin R. Pulmonary vascular abnormalities and ventilation-perfusion relationships in mild chronic obstructive pulmonary disease. Am J Respir Crit Care Med 149: 423–429, 1994. doi: 10.1164/ajrccm.149.2.8306040. [DOI] [PubMed] [Google Scholar]
- 4.Bell C, Monahan KD, Donato AJ, Hunt BE, Seals DR, Beck KC. Use of acetylene breathing to determine cardiac output in young and older adults. Med Sci Sports Exerc 35: 58–64, 2003. doi: 10.1097/00005768-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Chapman RF, Stray-Gundersen J, Levine BD. Individual variation in response to altitude training. J Appl Physiol (1985) 85: 1448–1456, 1998. doi: 10.1152/jappl.1998.85.4.1448. [DOI] [PubMed] [Google Scholar]
- 6.Clark AL, Poole-Wilson PA, Coats AJ. Exercise limitation in chronic heart failure: central role of the periphery. J Am Coll Cardiol 28: 1092–1102, 1996. doi: 10.1016/S0735-1097(96)00323-3. [DOI] [PubMed] [Google Scholar]
- 7.Dempsey JA, Hanson PG, Henderson KS. Exercise-induced arterial hypoxaemia in healthy human subjects at sea level. J Physiol 355: 161–175, 1984. doi: 10.1113/jphysiol.1984.sp015412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dominelli PB, Baker SE, Wiggins CC, Stewart GM, Sajgalik P, Shepherd JR, Roberts SK, Roy TK, Curry TB, Hoyer JD, Oliveira JL, Foster GE, Joyner MJ. Dissociating the effects of oxygen pressure and content on the control of breathing and acute hypoxic response. J Appl Physiol (1985) 127: 1622–1631, 2019. doi: 10.1152/japplphysiol.00569.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dominelli PB, Wiggins CC, Baker SE, Shepherd JR, Roberts SK, Roy TK, Curry TB, Hoyer JD, Oliveira JL, Joyner MJ. Influence of high affinity haemoglobin on the response to normoxic and hypoxic exercise. J Physiol 598: 1475–1490, 2020. doi: 10.1113/JP279161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dufu K, Yalcin O, Ao-Ieong ES, Hutchaleelala A, Xu Q, Li Z, Vlahakis N, Oksenberg D, Lehrer-Graiwer J, Cabrales P. GBT1118, a potent allosteric modifier of hemoglobin O2 affinity, increases tolerance to severe hypoxia in mice. Am J Physiol Heart Circ Physiol 313: H381–H391, 2017. doi: 10.1152/ajpheart.00772.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eaton JW. Oxygen affinity and environmental adaptation. Ann N Y Acad Sci 241: 491–497, 1974. doi: 10.1111/j.1749-6632.1974.tb21905.x. [DOI] [PubMed] [Google Scholar]
- 12.Eaton JW, Skelton TD, Berger E. Survival at extreme altitude: protective effect of increased hemoglobin-oxygen affinity. Science 183: 743–744, 1974. doi: 10.1126/science.183.4126.743. [DOI] [PubMed] [Google Scholar]
- 13.Eaton WA, Bunn HF. Treating sickle cell disease by targeting HbS polymerization. Blood 129: 2719–2726, 2017. doi: 10.1182/blood-2017-02-765891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Filley GF, Gregoire F, Wright GW. Alveolar and arterial oxygen tensions and the significance of the alveolar-arterial oxygen tension difference in normal men. J Clin Invest 33: 517–529, 1954. doi: 10.1172/JCI102922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedmann B, Frese F, Menold E, Kauper F, Jost J, Bärtsch P. Individual variation in the erythropoietic response to altitude training in elite junior swimmers. Br J Sports Med 39: 148–153, 2005. doi: 10.1136/bjsm.2003.011387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gersonde K, Nicolau C. Modification of the oxygen affinity of intracellular haemoglobin by incorporation of polyphosphates into intact red blood cells and enhanced O2 release in the capillary system. Bibl Haematol 46: 81–95, 1980. doi: 10.1159/000430550. [DOI] [PubMed] [Google Scholar]
- 17.Ghofrani HA, Voswinckel R, Reichenberger F, Weissmann N, Schermuly RT, Seeger W, Grimminger F. Hypoxia- and non-hypoxia-related pulmonary hypertension - established and new therapies. Cardiovasc Res 72: 30–40, 2006. doi: 10.1016/j.cardiores.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 18.Hackett PH, Roach RC. High-altitude illness. N Engl J Med 345: 107–114, 2001. doi: 10.1056/NEJM200107123450206. [DOI] [PubMed] [Google Scholar]
- 20.Honigman B, Theis MK, Koziol-McLain J, Roach R, Yip R, Houston C, Moore LG, Pearce P. Acute mountain sickness in a general tourist population at moderate altitudes. Ann Intern Med 118: 587–592, 1993. doi: 10.7326/0003-4819-118-8-199304150-00003. [DOI] [PubMed] [Google Scholar]
- 21.Howard J, Hemmaway CJ, Telfer P, Layton DM, Porter J, Awogbade M, Mant T, Gretler DD, Dufu K, Hutchaleelaha A, Patel M, Siu V, Dixon S, Landsman N, Tonda M, Lehrer-Graiwer J. A phase 1/2 ascending dose study and open-label extension study of voxelotor in patients with sickle cell disease. Blood 133: 1865–1875, 2019. doi: 10.1182/blood-2018-08-868893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hutchaleelaha A, Patel M, Washington C, Siu V, Allen E, Oksenberg D, Gretler DD, Mant T, Lehrer-Graiwer J. Pharmacokinetics and pharmacodynamics of voxelotor (GBT440) in healthy adults and patients with sickle cell disease. Br J Clin Pharmacol 85: 1290–1302, 2019. doi: 10.1111/bcp.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson BD, Beck KC, Proctor DN, Miller J, Dietz NM, Joyner MJ. Cardiac output during exercise by the open circuit acetylene washin method: comparison with direct Fick. J Appl Physiol (1985) 88: 1650–1658, 2000. doi: 10.1152/jappl.2000.88.5.1650. [DOI] [PubMed] [Google Scholar]
- 24.Koike A, Wasserman K, McKenzie DK, Zanconato S, Weiler-Ravell D. Evidence that diffusion limitation determines oxygen uptake kinetics during exercise in humans. J Clin Invest 86: 1698–1706, 1990. doi: 10.1172/JCI114894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kunert MP, Liard JF, Abraham DJ, Lombard JH. Low-affinity hemoglobin increases tissue PO2 and decreases arteriolar diameter and flow in the rat cremaster muscle. Microvasc Res 52: 58–68, 1996. doi: 10.1006/mvre.1996.0043. [DOI] [PubMed] [Google Scholar]
- 26.Kwo PY, Cohen SM, Lim JK. ACG clinical guideline: evaluation of abnormal liver chemistries. Am J Gastroenterol 112: 18–35, 2017. doi: 10.1038/ajg.2016.517. [DOI] [PubMed] [Google Scholar]
- 27.Lehrer-Graiwer J, Howard J, Hemmaway CJ, Awogbade M, Telfer P, Layton M, Mant T, Dufu K, Hutchaleelaha A, Koller T, Oksenberg D, Patel M, Ramos E. GBT440, a potent anti-sickling hemoglobin modifier reduces hemolysis, improves anemia and nearly eliminates sickle cells in peripheral blood of patients with sickle cell disease. Blood 126: 542, 2015. doi: 10.1182/blood.V126.23.542.542. [DOI] [Google Scholar]
- 28.Lehrer-Graiwer J, Howard J, Hemmaway CJ, Awogbade M, Telfer P, Layton M, Porter JB, Mant T, Dufu K, Hutchaleelaha A, Oksenberg D, Patel M, Tonda ME, Bridges K, Ramos E. Long-term dosing in sickle cell disease subjects with GBT440, a novel HbS polymerization inhibitor. Blood 128: 2488, 2016. doi: 10.1182/blood.V128.22.2488.2488. [DOI] [Google Scholar]
- 29.Oksenberg D, Dufu K, Patel MP, Chuang C, Li Z, Xu Q, Silva-Garcia A, Zhou C, Hutchaleelaha A, Patskovska L, Patskovsky Y, Almo SC, Sinha U, Metcalf BW, Archer DR. GBT440 increases haemoglobin oxygen affinity, reduces sickling and prolongs RBC half-life in a murine model of sickle cell disease. Br J Haematol 175: 141–153, 2016. doi: 10.1111/bjh.14214. [DOI] [PubMed] [Google Scholar]
- 30.Oswald-Mammosser M, Weitzenblum E, Quoix E, Moser G, Chaouat A, Charpentier C, Kessler R. Prognostic factors in COPD patients receiving long-term oxygen therapy. Importance of pulmonary artery pressure. Chest 107: 1193–1198, 1995. doi: 10.1378/chest.107.5.1193. [DOI] [PubMed] [Google Scholar]
- 31.Perutz MF, Fermi G, Abraham DJ, Poyart C, Bursaux E. Hemoglobin as a receptor of drugs and peptides–x-ray studies of the stereochemistry of binding. J Am Chem Soc 108: 1064–1078, 1986. doi: 10.1021/ja00265a036. [DOI] [Google Scholar]
- 32.Pochron M, Siu V, Oksenberg D, Dufu K. Central physiologic mechanisms which augment oxygen release (bohr effect and 2,3-dpg binding) are preserved in the presence of voxelotor at the therapeutic target of 30% hb modification: PS1522. HemaSphere 3: 701–702, 2019. doi: 10.1097/01.HS9.0000564348.52740.18. [DOI] [Google Scholar]
- 33.Rademacher P, Hutchaleelaha A, Washington C, Lehrer J, Ramos E. Absorption, metabolism and excretion of GBT440, a novel hemoglobin S (HbS) polymerization inhibitor for the treatment of sickle cell disease (SCD), in healthy male subjects. Blood 128: 2487, 2016. doi: 10.1182/blood.V128.22.2487.2487. [DOI] [Google Scholar]
- 34.Richardson RS, Tagore K, Haseler LJ, Jordan M, Wagner PD. Increased V̇o2max with right-shifted Hb-O2 dissociation curve at a constant O2 delivery in dog muscle in situ. J Appl Physiol (1985) 84: 995–1002, 1998. doi: 10.1152/jappl.1998.84.3.995. [DOI] [PubMed] [Google Scholar]
- 35.Roach RC, Greene ER, Schoene RB, Hackett PH. Arterial oxygen saturation for prediction of acute mountain sickness. Aviat Space Environ Med 69: 1182–1185, 1998. [PubMed] [Google Scholar]
- 36.Rotsztain A, Haddad R, Canter HG. Blood gas changes during voluntary hyperventilation in normal and disease states. Am Rev Respir Dis 102: 205–212, 1970. [DOI] [PubMed] [Google Scholar]
- 37.Wahr JA, Gerber M, Venitz J, Baliga N. Allosteric modification of oxygen delivery by hemoglobin. Anesth Analg 92: 615–620, 2001. doi: 10.1213/00000539-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Weisman IM, Zeballos RJ, Johnson BD. Cardiopulmonary and gas exchange responses to acute strenuous exercise at 1,270 meters in sickle cell trait. Am J Med 84: 377–383, 1988. doi: 10.1016/0002-9343(88)90256-2. [DOI] [PubMed] [Google Scholar]
- 39.Whipp BJ, Wasserman K. Alveolar-arterial gas tension differences during graded exercise. J Appl Physiol 27: 361–365, 1969. doi: 10.1152/jappl.1969.27.3.361. [DOI] [PubMed] [Google Scholar]
- 40.Winslow RM. The role of hemoglobin oxygen affinity in oxygen transport at high altitude. Respir Physiol Neurobiol 158: 121–127, 2007. doi: 10.1016/j.resp.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 41.Winslow RM, Monge CC, Statham NJ, Gibson CG, Charache S, Whittembury J, Moran O, Berger RL. Variability of oxygen affinity of blood: human subjects native to high altitude. J Appl Physiol 51: 1411–1416, 1981. doi: 10.1152/jappl.1981.51.6.1411. [DOI] [PubMed] [Google Scholar]