Abstract
Background:
Cervical cerclage placement has been shown to benefit women who have cervical insufficiency, however, the best type of suture to use for transvaginal cerclage placement is unknown.
Objective:
To evaluate the association between transvaginal cerclage suture thickness and pregnancy outcomes.
Study Design:
Retrospective cohort study of women with a singleton, non-anomalous gestation who underwent history-, ultrasound- or physical exam-indicated transvaginal cerclage at a single tertiary care center (2013–2016). The primary outcome was gestational age at delivery. Secondary outcomes included preterm birth less than 34 weeks, chorioamnionitis, neonatal intensive care unit admission and composite neonatal morbidity. Baseline characteristics and outcomes were compared by thickness of suture material: thick 5mm braided polyester fiber (Mersilene® tape) versus thin polyester braided thread (Ethibond®) or polypropylene non-braided monofilament (Prolene®) with selection of suture type at the discretion of the provider. The association between thick suture and gestational age at delivery was estimated using Cox proportional hazard regression. Multivariable logistic regression was used to estimate the association between thick suture and the secondary outcomes. Effect modification of cerclage indication was also assessed.
Results:
A total of 203 women met inclusion criteria: 120 (59%) with thick suture and 83 (41%) with thin suture. Of these, 130 women had history-indicated, 35 had ultrasound-indicated, and 38 had exam-indicated cerclages. Compared to women who had thin suture, women with thick suture were more likely to have had a history- or ultrasound-indicated cerclage, rather than exam-indicated cerclage, and more likely to have had a Shirodkar or cervico-isthmic approach, rather than McDonald. Women with thick suture were also more likely to have received progesterone and had placement at earlier gestational age, but there were no differences in cervical exam at placement. After adjusting for confounding factors, thick suture was associated with longer pregnancy duration among women with ultrasound-indicated cerclage (aHR 0.61, 95%CI 0.41–0.91) and exam-indicated cerclage (aHR 0.30, 95%CI 0.15–0.58), but not with history-indicated cerclage (aHR 1.27, 95%CI 0.83–1.94). Thick suture was also associated with lower odds of preterm birth < 34 weeks, chorioamnionitis and neonatal intensive care unit admission, compared to thin suture.
Conclusion:
Thick, compared to thin suture, for transvaginal cervical cerclage was associated with longer duration of pregnancy among women with ultrasound- and exam-indicated cerclages and lower odds of chorioamnionitis and neonatal intensive care unit admission among all women regardless of cerclage indication.
Keywords: cervical cerclage, suture, preterm birth
Condensation:
Use of thicker, compared to thinner, suture for transvaginal cervical cerclage is associated with improved pregnancy outcomes.
INTRODUCTION
Preterm birth complicates approximately 10% of all pregnancies in the United States1 and is the leading cause of neonatal morbidity and mortality among non-anomalous neonates in the United States.2 Spontaneous preterm birth occurs after the idiopathic onset of preterm labor, prelabor rupture of membranes, or asymptomatic cervical dilation due to cervical insufficiency.3 For women with cervical insufficiency, one of the main obstetric interventions to try to prevent preterm birth is cervical cerclage.4 Cervical cerclage placement has been shown to benefit women who have a history of mid-trimester loss due to cervical insufficiency,5 short cervix on ultrasound with a history of preterm birth,6 or a dilated cervix on exam regardless of previous obstetric history.7
While there has been extensive research to identify the population of women who may benefit the most from cerclage placement, the suture type used for cerclage has received less attention. A variety of suture types, each with their own distinct characteristics, are commonly used for transvaginal cerclage including Mersilene® tape, a thick 5mm braided polyester fiber; Ethibond®, a thinner polyester thread; and Prolene®, a polypropylene non-braided monofilament. Though all of these are non-absorbable sutures, whether the specific type of permanent suture used for cerclage affects pregnancy outcomes is unknown. In a survey of consultant members and fellows of the Royal College of Obstetricians and Gynecologists, the majority of respondents used Mersilene® tape, but 75% acknowledged that they were not certain about the best suture material to use.8
Thicker suture has been hypothesized to provide increased strength and spread the tension out across a larger diameter, resulting in improved pregnancy outcomes;8,9 whereas other experts caution the use of braided suture material with the theory that thicker, braided suture may increase the risk of infection and cause shifts in the vaginal microbiome increasing the chance of preterm birth and adverse neonatal outcomes.10 Given that the choice of suture type has been associated with surgical outcomes both in obstetrics and other surgical specialties,11–13 our objective was to evaluate whether pregnancy outcomes vary by the thickness of suture material used for transvaginal cerclage placement.
METHODS
This is a retrospective cohort study of women with transvaginal cervical cerclage placement at a single tertiary care center from 2013 to 2016. Women were identified from a query of the electronic medical record and our prospectively collected perinatal database. Pregnant women with a non-anomalous, singleton gestation and transvaginal cervical cerclage were included regardless of cerclage indication. Women were excluded if information about cerclage placement (suture and indication) or delivery outcomes were unavailable. All records were manually reviewed for eligibility. Baseline demographic characteristics, past obstetrical history as well as obstetric course and complications during the current pregnancy (indication for cerclage placement, timing and route of delivery, and neonatal complications) were manually abstracted.
Operative reports were reviewed and information was collected about the indication for cerclage placement, cervical exam prior to cerclage, and other details of the procedure itself including the type of surgical approach used for cerclage placement. History-indicated cerclage was defined as cerclage placement after 1 or more prior mid-trimester pregnancy losses or early spontaneous preterm birth <28 weeks’ suggestive of cervical insufficiency. Ultrasound-indicated cerclage was defined as cerclage placement in a woman with a history of a prior spontaneous preterm birth and ultrasound finding of short cervical length less than 25mm. Exam-indicated cerclage was defined as cerclage placement after asymptomatic mid-trimester cervical dilation of at least 1 centimeter by digital examination. In addition to the more common McDonald and Shirodkar surgical techniques,14 a cervico-isthmic approach is also used at our institution whereby a transvaginal cerclage is placed at the level of the internal cervical os after anterior and posterior colpotomy. Last, we abstracted details about whether an Obstetrics and Gynecology resident or a Maternal-Fetal Medicine fellow were involved in the procedure based on documentation in the operative report as well as the experience of the attending surgeon, defined as the number of years in practice. We did not exclude subjects if they labored, experienced preterm prelabor rupture of membranes, or were diagnosed with chorioamnionitis in the days following cerclage placement.
The primary outcome was gestational age at delivery. Secondary outcomes were preterm birth < 34 weeks’ gestation, chorioamnionitis, neonatal intensive care unit admission, and composite neonatal morbidity including necrotizing enterocolitis, grade 3 or 4 IVH, bronchopulmonary dysplasia, and death. Study outcomes were assessed by type of suture material used for cerclage: thinner versus thicker suture. Thinner suture materials included polyester thread (Ethibond®) and polypropylene non-braided monofilament (Prolene®). Thicker suture material included 5mm braided polyester fiber (Mersilene®) tape. All operative and pregnancy management decisions, including suture type selection, were at the discretion of the primary obstetrician.
Demographic and obstetric variables were compared by type of cerclage suture material using Chi-square, Mann-Whitney U, and Student’s t-test, as appropriate. Cox proportional hazard regression was used to estimate the association between thick suture and gestational age at delivery. We evaluated for effect modification of cerclage indication (history versus ultrasound versus physical exam) on the relationship between suture type and gestational age delivery and adjusted for confounding factors. Finally, multivariable logistic regression modeling was performed to estimate the association between cerclage suture type and the secondary outcomes, again with assessment for effect modification and adjustment for confounding factors. Demographic and obstetric characteristics previously shown to be associated with cerclage outcomes were considered as potential confounding factors, and the final list of factors included in the multivariable regression models were those with p<0.05 in bivariable analysis. The type of cerclage (McDonald, Shirodkar, or cervicoisthmic) was not able to be included as a confounder due to high degree of correlation with cerclage indication. Hazard ratios and odds ratios with 95% confidence intervals were obtained from the final regression models, respectively. All tests were two-tailed and p < 0.05 was used to define significance. This study was approved by the University of North Carolina-Chapel Hill Institutional Review Board under a waiver of informed consent (#14–2855).
RESULTS
Two-hundred three women met inclusion criteria (Figure 1). One hundred twenty-eight (59.8%) had thicker suture and 83 (41%) had thinner suture used for cervical cerclage. The majority of women had history-indicated cerclage (n=130, 64%) whereas the remaining were evenly distributed between ultrasound-indicated (n=35, 17%) and exam-indicated (n=38, 19%) cerclages. Most cerclages were placed using the McDonald technique (n=147, 72%), followed by Shirodkar (n=48, 24%) and cervico-isthmic (8, 4%) techniques. Demographic and ultrasonographic characteristics were similar between women who had thicker versus thinner suture, with the exception of cerclage indication, surgical approach, gestational age at cerclage placement, and progesterone use (Table 1). Women with thick suture were more likely to have had a history-indicated cerclage (70.8% vs 54.2%) or ultrasound-indicated cerclage (17.5% vs 16.9%) and less likely to have had an exam-indicated cerclage (11.7% vs 28.9%, compared to women with thin suture (p<0.01). Women with thick suture were more likely to have had a Shirodkar approach (38.3% vs 2.4%) or cervico-isthmic approach (6.7% vs 0%), and less likely to have had a McDonald approach (55.0% vs 97.6%), compared to women with thin suture. Women with thick suture were more likely to have received either vaginal or intramuscular progesterone (90.0% vs 78.3%, p=0.02) and have had their cerclage placed at an earlier gestational age (14.3 weeks vs 15.9 weeks, p=0.01), compared to women with thin suture (p<0.001). There were no differences in cervical length or dilation at time of placement by suture thickness (Table 1).
Figure 1.
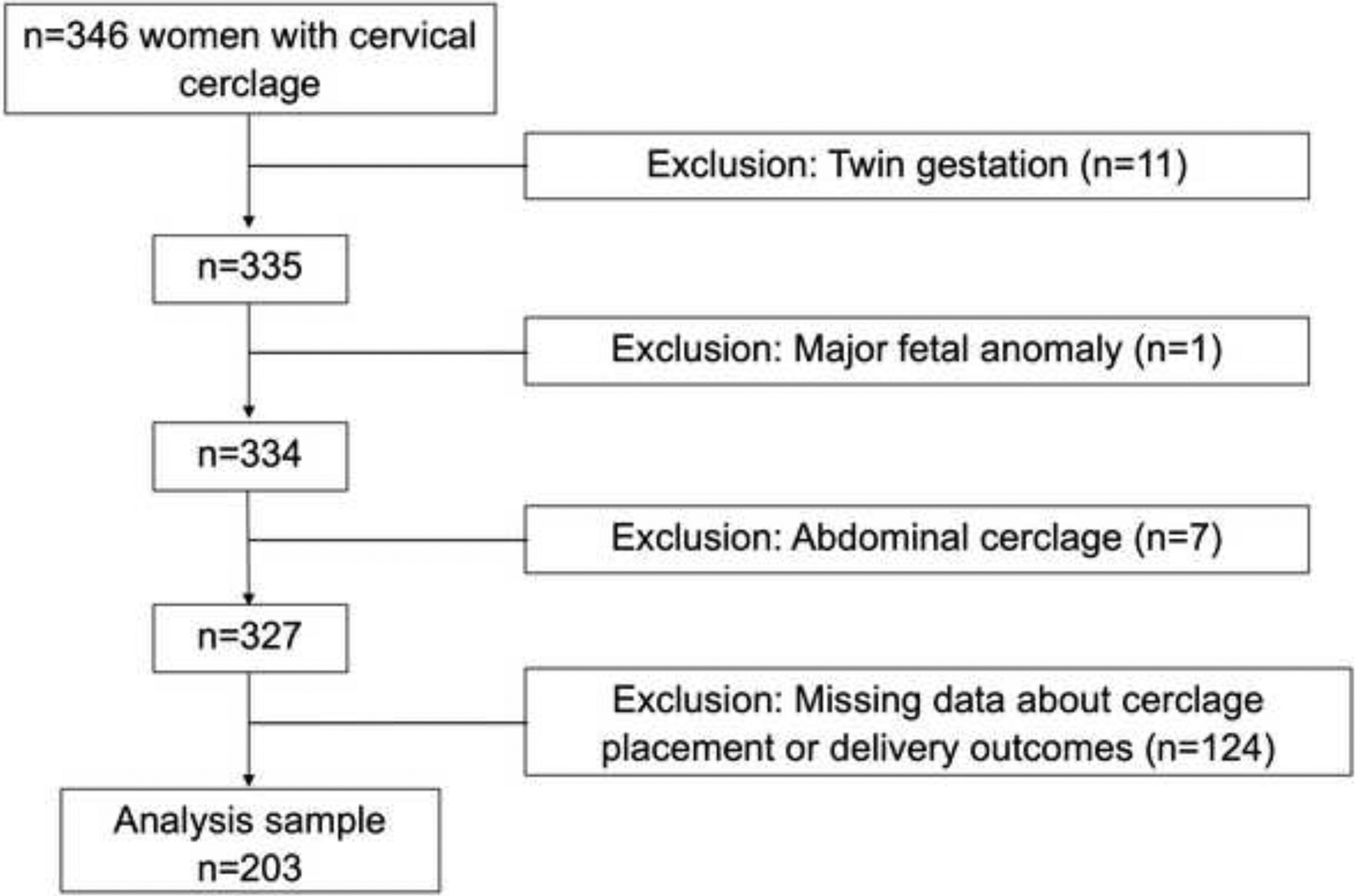
Flow diagram of study cohort
Table 1.
Maternal demographic, cerclage and other pregnancy characteristics compared by cerclage suture type
| Thicker suture (Mersilene tape) n=120 | Thinner suture (Ethibond/Prolene) n=83 | p-value | |
|---|---|---|---|
| Maternal demographic characteristics | |||
| Maternal age (years) | 31.7 +/− 5.2 | 32.3 +/− 5.1 | 0.49 |
| Maternal race | 0.07 | ||
| Non-Hispanic Black | 48 (45.3) | 39 (58.2) | |
| Non-Hispanic White | 40 (37.7) | 14 (20.9) | |
| Hispanic | 15 (14.2) | 9 (13.4) | |
| Other | 3 (2.8) | 5 (7.5) | |
| Pre-pregnancy maternal body mass index (kg/m2) | 27.9 (23.6, 35.3) | 27.5 (24.0, 35.0) | 0.89 |
| Gestational age of earliest prior PTB (weeks)* | 21.4 +/− 4.1 | 21.4 +/− 4.0 | 0.97 |
| Cerclage in one or more previous pregnancies* | 50 (53.8) | 26 (44.1) | 0.24 |
| Cerclage characteristics | |||
| Cerclage indication | 0.01 | ||
| History-indicated | 85 (70.8) | 45 (54.2) | |
| Ultrasound-indicated | 21 (17.5) | 14 (16.9) | |
| Exam-indicated | 14 (11.7) | 24 (28.9) | |
| Gestational age at cerclage placement (weeks) | 14.3 (13.1, 17.7) | 15.9 (13.6, 20.5) | 0.01 |
| Cervical length in mm at cerclage (for ultrasound-indicated cerclage) | 16.0 (14.0, 19.0) | 11.5 (9.0, 16.0) | 0.11 |
| Cervical dilation in cm at cerclage (for exam-indicated cerclage) | 1 (1, 1) | 1.5 (1, 3) | 0.14 |
| Surgical approach to cerclage placement | <0.001 | ||
| McDonald | 66 (55.0) | 81 (97.6) | |
| Shirodkar or modified Shirodkar | 46 (38.3) | 2 (2.4) | |
| Cervicoisthmic | 8 (6.7) | 0 | |
| Resident involved in cerclage placement | 85 (73.9) | 58 (73.4) | 0.94 |
| Maternal-Fetal Medicine fellow involved in cerclage placement | 37 (32.2) | 21 (26.6) | 0.40 |
| Generalist obstetrician as attending provider | 5 (6.3) | 2 (1.7) | 0.10 |
| Attending surgeon number of years of experience | 19.2 +/− 8.4 | 13.2 +/− 8.2 | <0.001 |
| Other pregnancy characteristics | |||
| Progesterone use during pregnancy | 108 (90.0) | 65 (78.3) | 0.02 |
| Vaginal progesterone | 33 (29.2) | 32 (39.5) | |
| Intramuscular 17-alpha hydroxyprogesterone caproate | 87 (72.5) | 50 (61.0) | |
| Gestational or pregestational diabetes | 24 (20.0) | 16 (19.3) | 0.90 |
| Chronic hypertension | 17 (14.2) | 15 (18.1) | 0.45 |
| Gestational hypertension or preeclampsia | 8 (6.7) | 3 (3.6) | 0.35 |
| Asthma | 11 (9.2) | 10 (12.1) | 0.52 |
| Loop electrosurgical excision procedure or cold knife cone | 16 (13.6) | 9 (11.0) | 0.59 |
| Gonorrhea or chlamydia at initial prenatal visit | 3 (2.5) | 0 | 0.15 |
| Illicit drug use during pregnancy | 4 (3.4) | 3 (3.6) | 0.92 |
Among multiparous women
Data are presented as n (%), mean +/− standard deviation, and median (interquartile range)
Overall, the median gestational age at delivery was 37.1 weeks (IQR 33.1, 39.0) and 57 women (28%) delivered < 34 weeks. The median time from cerclage placement to delivery was longer for women with thick suture (21.7 weeks, IQR 17.7, 24.6 weeks) compared to thin suture (17.2 weeks, IQR 11.3, 24.7 weeks; p=0.01). Women with thick suture were more likely to deliver later (37.2 weeks vs 36.0 weeks, p=0.04) and less likely to have preterm birth < 34 weeks (17.5% vs 43.4%, p<0.001), chorioamnionitis (13.3% vs 31.3%, p<0.01), neonatal intensive care unit admission (24.6% vs 47.4%, p<0.01), and composite neonatal morbidity (9.2% vs 20.5%, p<0.01), compared to women with thin suture (Table 2). There was no significant difference in the indication(s) for preterm birth < 34 weeks or neonatal gender.
Table 2.
Obstetric and neonatal outcomes
| Thicker suture (Mersilene tape) n=120 | Thinner suture (Ethibond/Prolene) n=83 | p-value | |
|---|---|---|---|
| Latency between cerclage and delivery (weeks) | 21.7 (17.7, 24.6) | 17.2 (11.3, 24.7) | 0.01 |
| Gestational age at delivery (weeks) | 37.2 (35.1, 39.0) | 36.0 (29.7, 39.0) | 0.04 |
| Delivered < 37 weeks’ gestation | 49 (40.8) | 45 (54.2) | 0.06 |
| Indication for preterm delivery < 37 weeks | 0.60 | ||
| Spontaneous PPROM or PTL | 32 (69.6) | 33 (73.3) | |
| Maternal | 7 (15.2) | 9 (20.0) | |
| Fetal | 5 (10.9) | 2 (4.4) | |
| Elective | 2 (4.4) | 1 (2.2) | |
| Delivered < 34 weeks’ gestation | 21 (17.5) | 36 (43.4) | <0.001 |
| Indication for preterm delivery < 34 weeks | 0.85 | ||
| Spontaneous PPROM or PTL | 17 (85.0) | 30 (83.3) | |
| Maternal | 2 (10.0) | 5 (13.9) | |
| Fetal | 1 (5.0) | 1 (2.8) | |
| Male fetus | 54 (45.4) | 45 (54.2) | 0.22 |
| Birthweight (grams) | 2977 (2485, 3411) | 2510 (1255, 3126) | <0.01 |
| Evidence of chorioamnionitis or funisitis on | 16 (13.3) | 26 (31.3) | <0.01 |
| placental pathology | |||
| Neonatal ICU admission | 28 (24.6) | 37 (47.4) | <0.01 |
| Composite neonatal morbidity* | 11 (9.2) | 17 (20.5) | 0.02 |
Data presented as n (%) or median (IQR)
Composite includes necrotizing enterocolitis, intraventricular hemorrhage, bronchopulmonary dysplasia, and perinatal death
In Cox proportional hazard regression evaluating the association between suture type and gestational age at delivery, there was evidence of effect modification by cerclage indication (p<0.001). Thick suture was associated with longer pregnancy duration among women with ultrasound-indicated cerclage (aHR 0.61, 95% CI 0.41–0.91) and exam-indicated cerclage (aHR 0.30, 95% CI 0.15–0.58), but there was no significant association between suture type and gestational age at delivery among women with history-indicated cerclage (aHR 1.27, 95% CI 0.83–1.94, Figure 2). After adjusting for cerclage indication as an effect modifier and other confounding factors including progesterone use during pregnancy, surgical approach, and attending surgeon years of experience, use of thick suture was associated with a lower odds of PTB < 34 weeks’ among women with ultrasound-indicated cerclage (aOR 0.19, 95% CI 0.07–0.49) and exam-indicated cerclage (aOR 0.06, 95% CI 0.01–0.31), but not among women with history-indicated cerclage (Table 3, Figure 2). Thick suture was also associated with lower adjusted odds of chorioamnionitis (aOR 0.31, 95% CI 0.12–0.77), and neonatal intensive care unit admission (aOR 0.34, 95% CI 0.16–0.75). The association between thick suture and composite neonatal morbidity was in the same direction, but did not reach statistical significance (aOR 0.39, 95% CI 0.13–1.14; Table 3).
Figure 2.
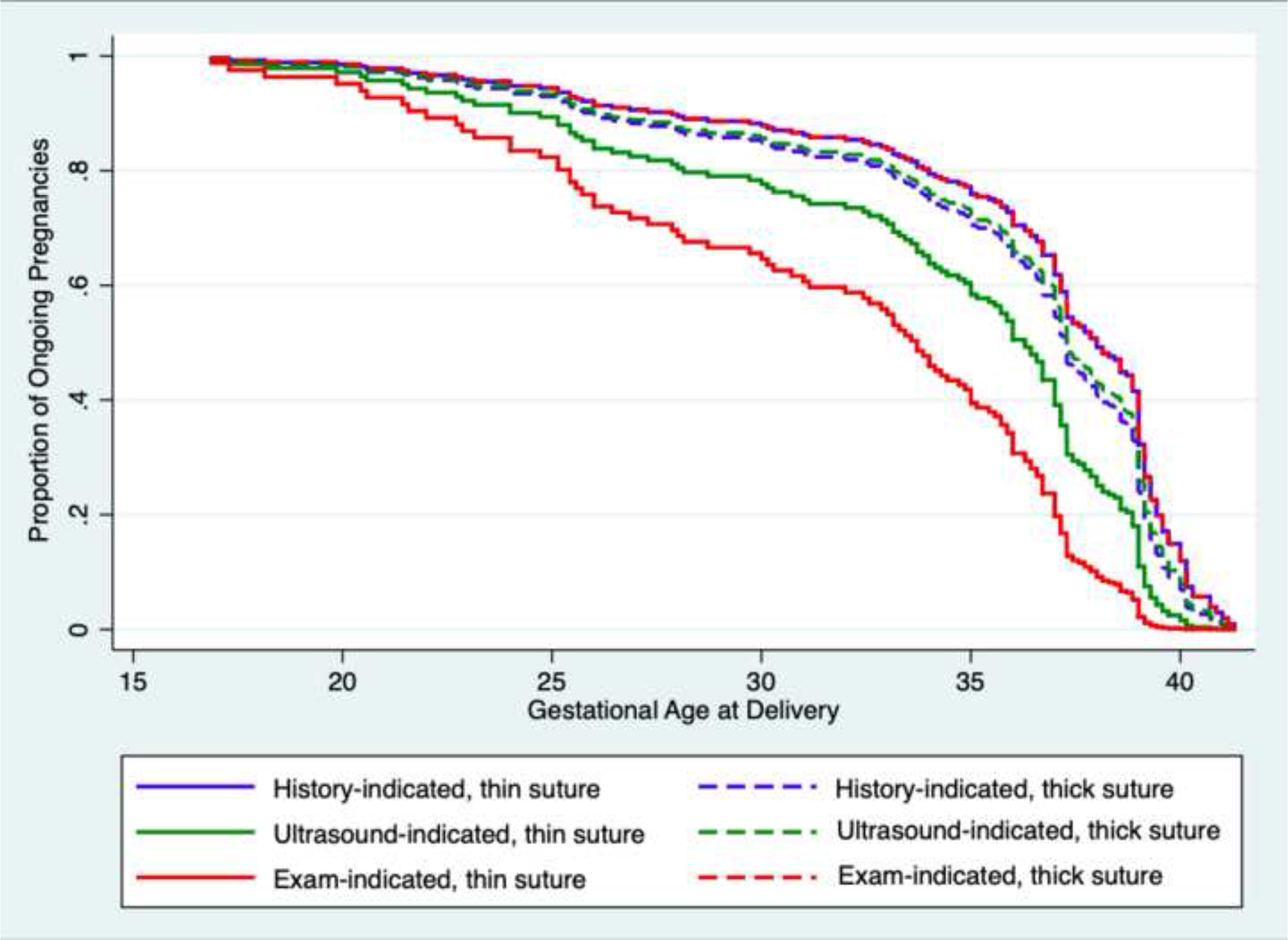
Cox proportional hazard regression of delivery gestational age by thickness of suture type and cerclage indication
Thick cerclage suture is associated with later gestational age at delivery among women with ultrasound- and exam-indicated cerclages, but not for history-indicated cerclages (effect modification p<0.001). Adjusted for progesterone use during pregnancy, cerclage indication, gestational age at cerclage placement, cerclage type, and attending surgeon years of experience.
Table 3.
Multivariable logistic regression of obstetric and neonatal outcomes by thickness of cerclage suture type
| Thick cerclage suture aOR (95% CI)* | |
|---|---|
| Preterm birth < 34 weeks† | |
| History-indicated cerclage | 0.62 (0.22–1.74) |
| Ultrasound-indicated cerclage | 0.19 (0.07–0.49) |
| Exam-indicated cerclage | 0.06 (0.01–0.31) |
| Chorioamnionitis | 0.31 (0.12–0.77) |
| Neonatal ICU admission | 0.34 (0.16–0.75) |
| Composite neonatal morbidity‡ | 0.39 (0.13–1.14) |
Adjusted for any progesterone use during pregnancy, cerclage indication, gestational age at cerclage placement, cerclage type, and attending surgeon years of experience; Referent=thin cerclage suture
Effect modification of cerclage indication p=0.01
Composite includes necrotizing enterocolitis, intraventricular hemorrhage, bronchopulmonary dysplasia, and perinatal death Abbreviations: aOR, adjusted odds ratio; CI, confidence interval
COMMENT
Our results demonstrate that use of thick compared to thin suture for transvaginal cervical cerclage was associated with later gestational age at delivery among women with ultrasound- and exam-indicated cerclages. In addition, thick suture was associated with 83–95% reduced odds of preterm birth less than 34 weeks among women with ultrasound- and exam-indicated cerclages. Among women with history-indicated cerclages, there was no association between suture thickness and gestational age or preterm birth less than 34 weeks’ gestation. Regardless of cerclage indication, use of thick compared to thin suture was associated with lower odds of maternal and neonatal complications including chorioamnionitis and neonatal intensive care unit admission.
These results extend previous literature on the optimal suture type for transvaginal cervical cerclage. In a secondary analysis of 138 women enrolled in a multicenter trial of ultrasound-indicated cerclage for short cervical length, there was no statistically significant difference between the rate of preterm birth less than 35 weeks’ gestation or the mean gestational age at birth among women who had Mersilene tape® compared to those who had Braided polyester suture (Mersilene® or Ethibond®) for cerclage placement.9 This study, however, had limited power to detect a significant difference in pregnancy outcomes. A more recent retrospective cohort study of 108 women also failed to show a difference in pregnancy outcomes based on cerclage suture type, however, it was also limited by small sample size and lack of adjustment for cerclage indication, which may have confounded their results.15
In contrast to the aforementioned studies, Kindinger, et al. demonstrated that braided suture was associated with higher rates of preterm birth and previable delivery, compared to monofilament suture in a retrospective cohort study of 678 women who received ultrasound-indicated cerclages in the United Kingdom.10 The same authors performed a subsequent prospective analysis of 49 women randomized to receive ultrasound-indicated cerclage with either braided or monofilament sutures and demonstrated an association between braided suture and shifts towards vaginal microbiome dysbiosis, compared to monofilament suture.10 They concluded that the differences in pregnancy outcomes may be related to induced changes in the microbiome rather than mechanical properties of the suture material itself. However, minimal clinical data were provided on the larger cohort (e.g., maternal race, prior pregnancy history, concomitant use of progestogens, cerclage criteria), and therefore population differences may account for the differences observed between the study by Kindinger et al as compared to our findings.
Our study has several strengths. We were able to directly compare pregnancy outcomes after cerclage by focusing on cerclage thickness rather than the specific type of filament or whether the suture was braided. Furthermore, inclusion of a diverse cohort of women who had cervical cerclage for a variety of indications made our results more generalizable and also allowed us to evaluate for potential effect modification of cerclage indication on the association between cerclage suture thickness and pregnancy outcomes. The results of our study, however, should be interpreted within the context of the study design. We are unable to discern the reason why thicker suture was associated with improved outcomes in women with unplanned cerclages (ultrasound- and exam-indicated) but not history-indicated cerclages. We theorize that thicker suture is more important when the process of cervical remodeling has already begun; perhaps the thicker suture is superior in these cases because it spreads the tension out across a larger diameter. However, the mechanism of action of cerclage remains unknown, and cannot be directly tested by the current study design. Furthermore, while it is assumed that provider preference primarily affected decisions to choose one particular suture type over another, it is possible that there are additional patient factors that we were unable to measure that may have affected the suture choice and pregnancy outcome (i.e. unmeasured confounding). Additionally, we were unable to evaluate the impact of surgical approach on study outcomes as it was highly correlated with cerclage indication, and we were unable to determine who among the resident, fellow, and attending physician was the primary surgeon who placed the cerclage. Lastly, we were limited by the small sample size of the study, and as with all observational studies, causality cannot be assumed.
While the superiority of a single type of suture has not been definitively established, our findings support the use of thick suture for women with ultrasound- and exam-indicated cerclages, as thick suture was associated with a later gestational age at delivery and lower odds of preterm birth < 34 weeks without any apparent increase in maternal or neonatal morbidity. In fact, thick cerclage suture was associated with lower odds of adverse maternal and neonatal outcomes including chorioamnionitis and neonatal intensive care unit admission compared to thin suture. Randomized controlled trials are needed to evaluate the efficacy of different suture types and determine if outcomes vary by indication for cerclage placement.
Figure 3.
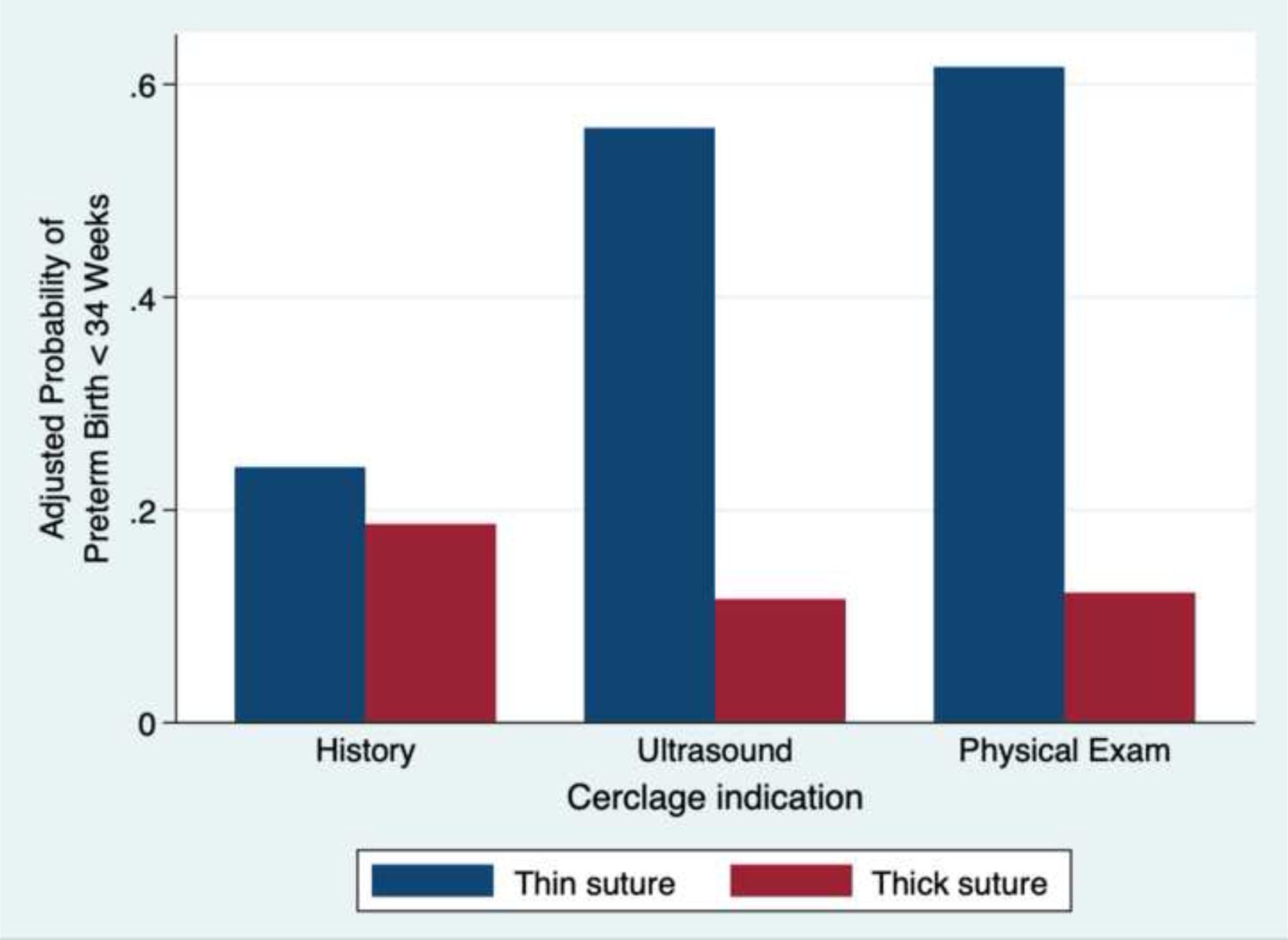
Adjusted probability of preterm birth less than 34 weeks by thickness of suture type and cerclage indication.
Thick cerclage suture is associated with lower probability of preterm birth less than 34 weeks among women with ultrasound- and exam-indicated cerclages, but not for history-indicated cerclages (effect modification p=0.03). Adjusted probabilities were calculated using linear combinations of beta coefficients from the final logistic regression model with cerclage indication as an effect modifier and additional confounders including progesterone use during pregnancy, gestational age at cerclage placement, surgical approach, and attending surgeon years of experience.
AJOG at a Glance:
- Why was this study conducted?
- To evaluate the association between transvaginal cerclage suture thickness and pregnancy outcomes.
- What are the key findings?
- Thick, compared to thin suture, for transvaginal cervical cerclage was associated with longer duration of pregnancy among women with ultrasound- and exam-indicated cerclages.
- Regardless of cerclage indication, thick suture was associated with lower odds of chorioamnionitis and neonatal intensive care unit admission compared to thin suture.
- What does this study add to what is already known?
- Previous studies have evaluated the association between cerclage suture type and perinatal outcomes among women with ultrasound-indicated cerclages, however, there is limited evidence for the optimal type of suture for history- and exam-indicated cerclages. This study was sufficiency powered to evaluate for effect modification by cerclage indication as well as adjust for confounding factors and provides evidence to support the use of thick suture for transvaginal cervical cerclage in order to optimize perinatal outcomes. Specifically, it demonstrates that suture thickness may be most important among women with ultrasound- and exam-indicated cerclages.
Funding:
Funded, in part, by R01-MD011609 (Manuck)
Footnotes
Disclosure statement:
The authors report no conflict of interest.
Presentation: Presented, in part, in poster format at the 38th annual meeting of the Society for Maternal-Fetal Medicine, Dallas, TX, Jan 29 - Feb 3
REFERENCES
- 1.Martin JA, Osterman MJ. Describing the Increase in Preterm Births in the United States, 2014–2016. 2018;2015(312):1–8. https://www.cdc.gov/nchs/data/databriefs/db312_table.pdf#1. [PubMed] [Google Scholar]
- 2.McIntire DD, Leveno KJ. Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol. 2008;111(1):35–41. doi: 10.1097/01.AOG.0000297311.33046.73 [DOI] [PubMed] [Google Scholar]
- 3.Committee on Practice Bulletins-Obstetrics, The American College of Obstetricians and Gynecologists. Practice Bulletin No. 130. Obstet Gynecol. 2012;120(4):964–973. doi: 10.1097/AOG.0b013e3182723b1b [DOI] [PubMed] [Google Scholar]
- 4.American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No.142: Cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014;123(2 Pt 1):372–379. doi: 10.1097/01.AOG.0000443276.68274.cc [DOI] [PubMed] [Google Scholar]
- 5.Final report of the Medical Research Council/Royal College of Obstetricians and Gynaecologists multicentre randomised trial of cervical cerclage. MRC/RCOG Working Party on Cervical Cerclage. Br J Obstet Gynaecol. 1993;100(6):516–523. http://www.ncbi.nlm.nih.gov/pubmed/8334085. [DOI] [PubMed] [Google Scholar]
- 6.Berghella V, Rafael TJ, Szychowski JM, Rust OA, Owen J. Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth: A meta-analysis. Obstet Gynecol. 2011;117(3):663–671. doi: 10.1097/AOG.0b013e31820ca847 [DOI] [PubMed] [Google Scholar]
- 7.Ehsanipoor RM, Seligman NS, Saccone G, et al. Physical Examination-Indicated Cerclage: A Systematic Review and Meta-analysis. Obstet Gynecol. 2015;126(1):125–135. doi: 10.1097/AOG.0000000000000850 [DOI] [PubMed] [Google Scholar]
- 8.Israfil-Bayli F, Toozs-Hobson P, Lees C, et al. Cervical cerclage and type of suture material: a survey of UK consultants’ practice. J Matern Fetal Neonatal Med. 2014;27(15):1584–1588. doi: 10.3109/14767058.2013.870551 [DOI] [PubMed] [Google Scholar]
- 9.Berghella V, Szychowski JM, Owen J, et al. Suture type and ultrasound-indicated cerclage efficacy. J Matern Neonatal Med. 2012;25(11):2287–2290. doi: 10.3109/14767058.2012.688081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kindinger LM, MacIntyre DA, Lee YS, et al. Relationship between vaginal microbial dysbiosis, inflammation, and pregnancy outcomes in cervical cerclage. Sci Transl Med. 2016;8(350):350ra102. doi: 10.1126/scitranslmed.aag1026 [DOI] [PubMed] [Google Scholar]
- 11.Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a metaanalysis. Am J Obstet Gynecol. 2015;212(5):621.e1–621.e10. doi: 10.1016/j.ajog.2014.12.020 [DOI] [PubMed] [Google Scholar]
- 12.Peterson HB, Xia Z, Hughes JM, Wilcox LS, Tylor LR, Trussell J. The Risk of Ectopic Pregnancy after Tubal Sterilization. N Engl J Med. 1997;336(11):762–767. doi: 10.1056/NEJM199703133361104 [DOI] [PubMed] [Google Scholar]
- 13.Patel SV, Paskar DD, Nelson RL, Vedula SS, Steele SR. Closure methods for laparotomy incisions for preventing incisional hernias and other wound complications. Cochrane Database Syst Rev. 2017;11:CD005661. doi: 10.1002/14651858.CD005661.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindsay Wood S, Owen J. Cerclage: Shirodkar, McDonald, and modifications. Clin Obstet Gynecol. 2016;59(2):302–310. doi: 10.1097/GRF.0000000000000190 [DOI] [PubMed] [Google Scholar]
- 15.Stafford IA, Kopkin RH, Berra AL, et al. Efficacy of different cerclage suture materials in reducing preterm birth. J Matern Neonatal Med. 2019;0(0):1–5. doi: 10.1080/14767058.2019.1578744 [DOI] [PubMed] [Google Scholar]


