Abstract
BACKGROUND AND PURPOSE:
Identification of spinal drop metastases is important in the staging and management of pediatric patients with primary brain tumors. Our aim was to assess the diagnostic utility of the balanced steady-state free precession (bSSFP) sequence (CISS/FIESTA/3D driven equilibrium radiofrequency reset pulse) for the detection of spinal drop metastases in pediatric patients with primary intracranial tumors.
MATERIALS AND METHODS:
This was a retrospective study of 44 pediatric patients with primary intracranial tumors undergoing MR imaging spine evaluation for drop metastases before radiation treatment. All patients underwent a whole-spine MRI with both bSSFP and postcontrast T1WI sequences. Two neuroradiologists independently reviewed only the bSSFP sequence, then 1 week later only the postcontrast T1WI sequence.
RESULTS:
Patients ranged from 1 to 18 years of age (mean, 7.1 ± 4.2 years) with 27 males and 17 females. The number of lesions per patient ranged from 1 to 13 and from 2 to 11 mm in size. Lesions suspicious for drop metastases were seen in 8 patients on the postcontrast T1WI (18%) compared with 10 patients on the bSSFP sequence (23%). Twenty-two drop metastases seen on the bSSFP sequence were not visible on the postcontrast T1WI, including nonenhancing drop metastases and multiple nodules of <3 mm. Interrater agreement was excellent for the bSSFP sequence (0.91) and the postcontrast T1 sequence (0.90).
CONCLUSIONS:
The bSSFP sequence increased the diagnostic yield for the detection of drop metastases in pediatric patients with primary intracranial tumors and was particularly advantageous for small drop metastases (<3 mm) and nonenhancing metastases, and it decreased the number of false-positives. The bSSFP sequence may be an important adjunct to postcontrast T1WI for the evaluation of drop metastases.
Spinal cord imaging is considered standard of care for the staging and treatment planning of pediatric brain tumors. The inclusion of spinal imaging is particularly important for those tumors with a propensity for drop metastases. Identification of drop metastases can change radiation planning from focal radiation of the primary tumor bed to craniospinal radiation and may mandate the intensification of both radiation and chemotherapy for appropriate treatment.1
A balanced steady-state free precession (bSSFP) scan (CISS/FIESTA/3D driven equilibrium radiofrequency reset pulse) is a heavily fluid-weighted isotropic sequence. The bSSFP sequence is advantageous for spine imaging, given its superior contrast resolution, enabling sharp discrimination of CSF from the spinal cord and adjacent nerve roots, superior spatial resolution, and isotropy allowing triplanar reconstruction. The bSSFP sequence has been previously used, for example, for the evaluation of duplicated spinal nerve roots and a detailed assessment of spinal cord pathology, including diastematomyelia and syringomyelia.2–8 Most commonly, the bSSFP sequence has been used for the evaluation of vestibular schwannomas, given its superb fluid-to–soft tissue contrast and high spatial resolution.9–11
The screening protocol for the detection of drop metastases at many institutions primarily consists of a postcontrast T1WI sequence through the entire spine. The purpose of this study was to evaluate the diagnostic utility of the bSSFP sequence compared with conventional postcontrast T1WI for detection of drop metastases in pediatric patients with primary intracranial tumors.
Materials and Methods
Study Design
This was a retrospective, institutional review board–approved study examining patients undergoing MR imaging of the spine for the surveillance of drop metastases performed between December 2010 and January 2017 at Massachusetts General Hospital. All pediatric patients with a diagnosis of a primary intracranial tumor included in this study were identified through a search of our Radiology Information System. All patients were referred for a routine clinical MRI for the detection of spinal drop metastases before radiation treatment. Inclusion criteria were patients 18 years of age or younger with a history of an intracranial neoplasm requiring screening for spinal drop metastases and a preradiation MRI that included a bSSFP sequence and a sagittal T1 postcontrast sequence of the entire spine. Exclusion criteria were patients with examinations degraded by technical or motion artifacts precluding a diagnostic assessment, patients with MRI examinations performed immediately following a brain operation to minimize the amount of postoperative hemorrhage and debris in the spinal canal, and patients with prior spinal radiation or resection of a spinal metastasis.
Medical Record Review
A search of the electronic medical record was performed on all patients in this study cohort by a second-year neuroradiology fellow. The electronic medical record was reviewed for the following: 1) basic demographic information including age and sex, 2) oncologic data including pathologic diagnosis, and 3) treatment history including prior surgery and chemotherapy.
Scanner Hardware
MRI examinations were performed on either a 1.5T Signa Excite HDx scanner (GE Healthcare, Milwaukee, Wisconsin) with an 8-channel spine coil or a 3T Tim Trio scanner (Siemens, Erlangen, Germany) with a 32-channel spine coil. All patients received the same intravenous gadolinium contrast agent, gadoterate meglumine. Spine imaging was performed immediately following the brain MRI without the administration of an additional dose of contrast.
Sequences reviewed included a bSSFP sequence of the cervicothoracic and thoracolumbar spine and a postcontrast sagittal T1 sequence with a similar FOV. The same imaging protocol was used for all patients regardless of age or histologic tumor type.
bSSFP (CISS) sequence parameters performed on the 3T Tim Trio scanner included TR/TE = 11.69/5.85 ms, NEX = 1, echo train = 1, matrix = 448 × 269, flip angle = 50°, slice thickness = 0.8 mm, slice spacing = 0 mm, cervicothoracic spine FOV = 15 × 3–5 × 199–220 mm (anterior-to-posterior × right-to-left × superior-to-inferior), thoracolumbar spine FOV = 15 × 3–5 × 199–220 mm (anterior-to-posterior × right-to-left × superior-to-inferior), voxel size = 0.55–0.58 mm3, with a scan time of approximately 5 minutes 20 seconds. For smaller children, the bSSFP sequence comprised two, 30-cm, superior-to-inferior segment slabs. With older and taller children, the bSSFP sequence comprised three, 30-cm, superior-to-inferior segment slabs.
Postcontrast T1 sequence parameters performed on the 3T Tim Trio scanner included TR/TE = 603/9.3 ms, NEX = 2, echo train = 3, matrix = 320 × 224, slice thickness = 3 mm, gap = 0 mm, cervicothoracic spine FOV = 4–7 × 3–5 × 220–240 mm (anterior-to-posterior × right-to-left × superior-to-inferior), thoracolumbar spine FOV = 4–7 × 3–5 × 210–240 mm (anterior-to-posterior × right-to-left × superior-to-inferior), with a scan time of approximately 3 minutes 15 seconds.
bSSFP (FIESTA) sequence parameters performed on the 1.5T Signa Horizon scanner included TR/TE = 5.288/2.044–5.948/2.22 ms, NEX = 1.5–4, echo train = 1, matrix = 448 × 256, flip angle = 65°, slice thickness = 0.8 mm, gap = 0.4 mm, cervicothoracic spine FOV = 15 × 3–5 × 220–280 mm (anterior-to-posterior × right-to-left × superior-to-inferior), thoracolumbar spine FOV = 15 × 3–5 × 220–280 mm (anterior-to-posterior × right-to-left × superior-to-inferior), voxel size = 0.55–0.58 mm3, with a scan time of approximately 5 minutes 40 seconds. For smaller children, the bSSFP sequence comprised two, 30-cm, superior-to-inferior segment slabs. With older and taller children, the bSSFP sequence comprised three, 30-cm, superior-to-inferior segment slabs.
Postcontrast T1WI performed on the 1.5T Signa Horizon scanner included TR/TE = 533.3/7.464 ms, NEX = 2, echo train = 3, matrix = 256 × 224, flip angle = 90°, slice thickness = 3 mm, gap = 0 mm, cervicothoracic spine FOV = 4–7 × 3–5 × 220–240 mm (anterior-to-posterior × right-to-left × superior-to-inferior), thoracolumbar spine FOV = 4–7 × 3–5 × 210–240 mm (anterior-to-posterior × right-to-left × superior-to-inferior), with a scan time of approximately 3 minutes 45 seconds.
Sedation for MR Imaging Examination
Patients younger than 6 years of age underwent sedation for the MRI examination to decrease motion artifacts and improve image quality. Sedation was administered by a pediatric anesthesiology team per our institutional protocol. For older children, we used video goggles and the aid of a dedicated child life specialist during the MRI acquisition to help decrease motion during the MRI examination.
Image Analysis
All preradiation spinal MRI studies obtained for treatment planning were reviewed. The bSSFP and sagittal postcontrast T1WI acquired during the examination were reviewed 1 week apart to reduce the risk of observer bias. All images were reviewed by a second-year neuroradiology fellow and a pediatric neuroradiology attending physician with >15 years' experience reading pediatric neuroimaging studies at our institution.
The presence of drop metastases and the number, size, and location, if applicable, were recorded by each of the 2 radiologists. If diffuse leptomeningeal disease was detected, this was recorded and no discrete measurements were performed.
Definitions of Lesions
A lesion was considered suspicious for a drop metastasis on the bSSFP sequence if it met the following criteria:
An extramedullary, intradural nodule measuring ≥1 mm that lay along nerve roots or the spinal cord and demonstrated smooth, round contours without a fluid-fluid level or the appearance of layering to suggest hemorrhage.
If there were small foci of abnormal signal intensity along the surface of the spinal cord and/or nerve roots, which did not meet the criteria of No. 1 above, these lesions were considered indeterminate.
A lesion was considered suspicious for a drop metastasis on the postcontrast T1WI if it met the following criteria:
An enhancing extramedullary, intradural nodule measuring ≥1 mm that lay along nerve roots or the spinal cord and demonstrated smooth, round contours and did not have the appearance of layering, which would suggest hemorrhage.
If there were small foci of enhancement that did not meet the criteria of No. 1 listed above, they were considered indeterminate.
Findings suggestive of diffuse leptomeningeal disease were defined as the following:
For the bSSFP sequence, diffuse nerve root thickening or nodularity and irregular contour of the spinal cord.
For the postcontrast T1WI, diffuse, abnormal enhancement and nodularity along the spinal cord and/or thickening of the nerve roots.
Findings suggestive of hemorrhage/debris, vascular structures, and flow artifacts were defined as the following:
Foci of signal in the thecal sac that either layered or appeared clearly separate from nerve roots were considered to represent hemorrhage/debris.
Tubular or linear structures along the surface of the spinal cord or adjacent to nerve roots were considered vascular structures.
Web-like, nonanatomic structures within the CSF were considered flow artifacts.
Indeterminate findings were those that did not meet the above criteria.
The results of the independently evaluated sequences (bSSFP and postcontrast T1WI) were compared.
A concordant case was defined as the following:
A case with a finding that was positive for drop metastasis on the bSSFP and positive on the postcontrast T1WI.
A case that was negative for the presence of drop metastases on the bSSFP and negative on the postcontrast T1WI.
A discordant case was defined as the following:
A case with a finding that was positive for drop metastasis on the bSSFP with no positive finding on the postcontrast T1WI.
A case with a finding positive for drop metastasis on the postcontrast T1WI, and no positive finding on the bSSFP.
Interrater Assessment and Statistical Analysis
The level of interrater agreement between the 2 radiologists was assessed using a κ score. Discrepancies between the 2 radiologists were also reviewed by a third rater, a pediatric neuroradiology attending with >15 years' experience. Discrepancies between the number and size of drop metastases between the postcontrast T1WI and bSSFP sequence and the number of “missed” drop metastases were recorded. Basic descriptive statistics were used to evaluate significant differences in lesion size and number between the lesions detected on the bSSFP sequence compared with the postcontrast T1WI sequence.
Results
Cohort Description
A total of 44 pediatric patients were included in this cohort, comprising 27 males and 17 females, ranging from 1 to 18 years of age (mean, 7.21 ± 4.24 years). Thirty patients were scanned on a 1.5T scanner, and 14 patients were scanned on a 3T scanner. Two examinations were excluded secondary to severe motion artifacts on the bSSFP sequence.
The most commonly encountered primary brain tumor pathologies were medulloblastoma (n = 15), germinoma (n = 11), and ependymoma (n = 8). A full list of primary intracranial tumor pathologies in this patient cohort is shown in Table 1.
Table 1:
Demographic and clinical information for the 44-patient cohort
| Patient Demographics | |
|---|---|
| Sex | |
| Male | 27 |
| Female | 17 |
| Age (yr) | |
| Mean | 7.21 |
| SD | 4.24 |
| Min | 1 |
| Max | 18 |
| Primary intracranial tumor type | |
| Medulloblastoma | 15 |
| Germinoma | 11 |
| Ependymoma | 8 |
| Astrocytoma | 4 |
| ATRT | 3 |
| Glioblastoma | 2 |
| Pineoblastoma | 1 |
Note:—Min indicates minimum; max, maximum; ATRT, atypical rhabdoid tumor.
bSSFP Evaluation
Lesions suggestive of drop metastases were detected on 10 bSSFP examinations, ranging from 2 to 13 lesions per examination (Table 2). On average, the number of drop metastases seen in an individual patient on the bSSFP sequence was 6.3 ± 3.9. These lesions ranged from 1 to 25 mm (mean, 3.9 ± 4.6 mm) (Fig 1). Of these spinal drop metastases, on average, a mean of 3.9 ± 2.1 lesions measured <3 mm as shown in Table 3. Thirty-six positive nodules were seen on the bSSFP sequence with no evidence of indeterminate or discordant nodules (Figs 1 and 2 and Table 4).
Table 2:
Number of cases with nodules meeting the criteria for drop metastases (positive cases), cases with no evidence of drop metastases (negative cases), and cases with indeterminate findingsa
| Sequence | Positive Cases | Negative Cases | Indeterminate Cases |
|---|---|---|---|
| bSSFP | 10 | 34 | 0 |
| Postcontrast T1WI | 8 | 32 | 4 |
This classification was performed for both the bSSFP and postcontrast T1WI, which were evaluated independently.
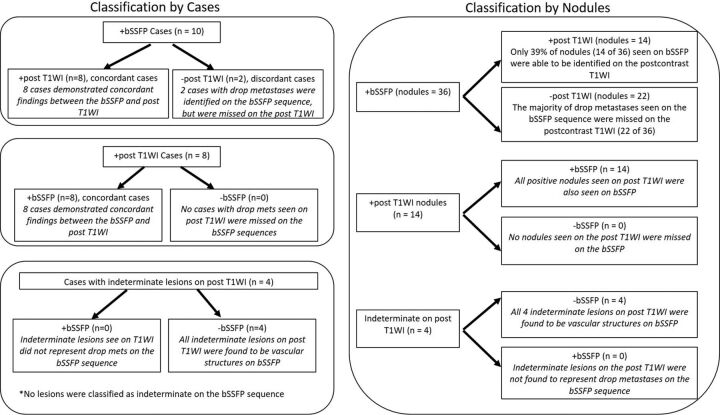
Fig 1.
Classification by cases (left image) with positive, negative, and indeterminate findings on the bSSFP and postcontrast T1WI. Classification by nodules (right image) with positive, negative, and indeterminate findings.
Table 3:
Total number of lesions, lesion size, and number of lesions of ≤3 mm detected on the bSSFP sequence compared with postcontrast T1WI
| bSSFP | Postcontrast T1WI | P Value | |
|---|---|---|---|
| No. of lesions per patient | |||
| Mean | 6.3 | 2.1 | .002 |
| SD | 3.9 | 1.2 | |
| Min | 2 | 1 | |
| Max | 13 | 4 | |
| Lesion size (mm) | |||
| Mean | 3.9 | 4.9 | .43 |
| SD | 4.6 | 6.8 | |
| Min | 1 | 1 | |
| Max | 25 | 24 | |
| Lesions ≤3 mm | |||
| Mean | 3.9 | 1.2 | .03 |
| SD | 2.1 | 1.7 |
Note:—Min indicates minimum; max, maximum.
Fig 2.
A 6-year-old boy with a history of medulloblastoma. Sagittal bSSFP images A and C demonstrate numerous nodular drop metastases (white arrows). B and D, Corresponding enhancing nodules along the cauda equina nerve roots. The axial bSSFP image (E) demonstrates a nodular drop metastasis along the cauda equina nerve roots (white arrow).
Table 4:
Number of nodules seen on the bSSFP and postcontrast T1WI classified as positive nodules, indeterminate nodules, and discordant nodulesa
| Nodule Classification | bSSFP | Postcontrast T1WI |
|---|---|---|
| Positive nodules | 36 | 14 |
| Indeterminate nodules | 0 | 10 |
| Discordant nodules | 0 | 22 |
Discordant or “missed” nodules are nodules not seen on the sequence being evaluated but present on the corresponding sequence. In this case, 22 nodules were not seen on postcontrast T1WI that were seen on the bSSFP sequence. No nodules were seen on the postcontrast T1WI but not the bSSFP sequence.
Sagittal Postcontrast T1WI Evaluation
Lesions suggestive of drop metastases were detected on 8 postcontrast T1WI scans (Figs 1 and 2 and Table 2). On average, the number of drop metastases seen in an individual patient on postcontrast T1WI was 2.1 ± 1.2. These lesions, on average, measured 4.9 ± 6.8 mm as shown in Table 3. Of these lesions, on average, 1.2 ± 1.7 lesions measured <3 mm as shown in Table 3. Fourteen positive nodules were identified on postcontrast T1WI. Ten indeterminate nodules were seen on postcontrast T1WI, for which additional imaging was recommended for further characterization (Fig 1 and Table 4).
Comparison of bSSFP and Postcontrast T1WI
Most drop metastases appeared as discrete, rounded nodules along the surface of the spinal cord and/or along the cauda equina nerve roots; however, in 3 patients, diffuse leptomeningeal disease was noted and was seen on both the postcontrast T1WI and the bSSFP sequence (Fig 3).
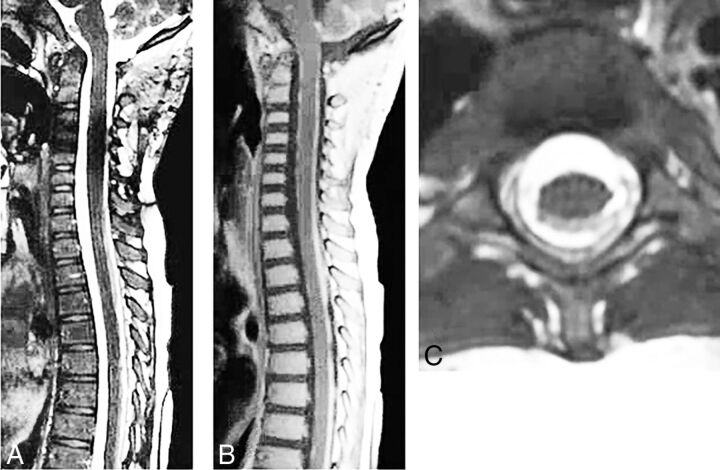
Fig 3.
A 4-year-old boy with a history of medulloblastoma and diffuse leptomeningeal disease. The bSSFP image of the cervical spine (A) demonstrates subtle irregularity of the cervicothoracic spinal cord. Abnormal, confluent enhancement is more pronounced on the sagittal postcontrast T1WI of the cervicothoracic spine (B). The axial bSSFP image (C) demonstrates abnormal, crescentic signal abnormality along the dorsal spinal cord.
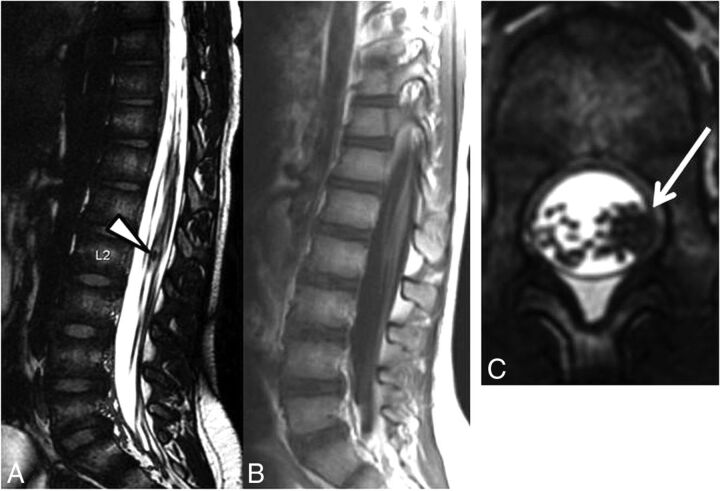
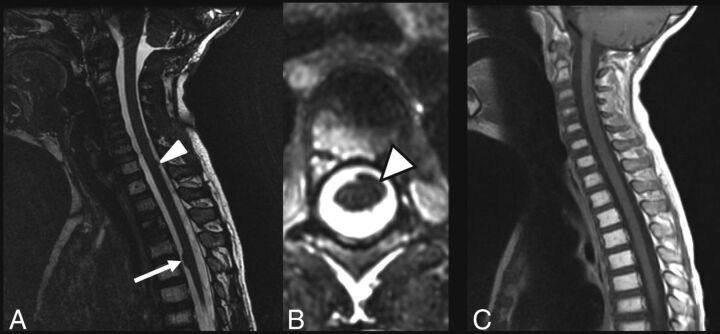
The postcontrast T1WI sequence identified fewer positive lesions (n = 14) suspicious for drop metastases compared with those seen on the bSSFP sequence (n = 36) (Fig 1). Twenty-two positive lesions were seen on the bSSFP sequence, which were not visualized on the postcontrast T1WI. These lesions were found in, among others, a patient with nonenhancing drop metastases related to a nonenhancing primary intracranial tumor (ependymoma) and a patient with multiple, small, <3-mm nodules (Figs 4 and 5).
Fig 4.
An 8-year-old boy with a history of germinoma. Sagittal bSSFP sequence (A) demonstrates a nodular drop metastasis within the cauda equina nerve roots (white arrowhead). No corresponding enhancement is seen on the postcontrast T1WI (B). The axial bSSFP sequence (C) demonstrates a nodular drop metastasis along the cauda equina nerve roots (white arrow) within the left lateral aspect of the thecal sac.
Fig 5.
A 7-year-old boy with a history of ependymoma. A, Sagittal bSSFP sequence demonstrates a dominant, ventral spinal metastasis at the T5 level (white arrow) with multiple, additional, smaller metastases (white arrowhead). B, Axial bSSFP sequence at the T5 level demonstrates a left ventral metastasis (white arrowhead). C, Postcontrast T1WI in the same patient does not demonstrate abnormal enhancement or detectable drop metastases.
In 4 cases, indeterminate lesions were seen on postcontrast T1WI, which warranted additional imaging for classification. Comparison of the postcontrast T1WI with the corresponding bSSFP sequences, revealed these indeterminate lesions were consistent with vascular structures (Fig 1).
Among cases with positive nodules identified on both postcontrast T1WI and bSSFP sequences, there were 2 cases in which only 1 nodule was seen on the postcontrast T1WI, whereas multiple nodules were seen on the bSSFP sequence. This finding is clinically significant because the detection of additional nodules may change treatment from targeted radiation therapy of a single lesion to craniospinal radiation for the treatment of multiple lesions.
Statistically significant differences were seen between the number of drop metastases detected on the bSSFP sequence compared with postcontrast T1WI (P = .03), with a greater number of lesions detected per patient on the bSSFP sequence at 6.3 versus 2.1 detected on postcontrast T1WI.
While, on average, drop metastases measured slightly larger on the postcontrast T1WI (4.9 mm) compared with the bSSFP sequence (3.9 mm), this difference was not statistically significant (P = .43). Lesions measuring ≤3 mm were more frequently seen on the bSSFP sequence, including 27 lesions compared with 17 lesions identified on postcontrast T1WI. This difference was statistically significant (P = .03).
Interrater agreement was excellent for the bSSFP sequence (0.91) and the postcontrast T1WI (0.90).
Discussion
The results of this study demonstrate proof of concept that the bSSFP sequence can enhance the detection of spinal drop metastases in pediatric patients with primary intracranial tumors. The bSSFP sequence is particularly advantageous for small drop metastases and nonenhancing metastases and decreases the number of false-positives.
The bSSFP sequence offers distinct advantages over traditional, standard postcontrast T1WI for drop metastases, including better spatial resolution; better contrast resolution; triplanar reformats, which obviate direct axial images and can thus reduce scan time; and the detection of nonenhancing drop metastases in cases of a nonenhancing or minimally enhancing primary brain tumor. These advantages facilitate the detection of nodular metastases insinuating along spinal nerve roots; decrease the rate of indeterminate lesion classification, which may potentiate additional follow-up imaging; and render the bSSFP sequence superior to the postcontrast T1WI for detection of nonenhancing drop metastases.
The bSSFP sequence demonstrated an improved ability to detect nodular drop metastases measuring <3 mm. In 2 patients, a single drop metastasis was seen on the postcontrast T1WI; however, on the bSSFP sequence, additional smaller drop metastases were identified. This finding is clinically significant because it may change treatment from targeted radiation therapy of a single lesion to craniospinal radiation for these patients.
In 1 patient, nodules were detected on the bSSFP sequence, but not on the postcontrast T1WI. A review of the pretreatment MR imaging showed that the primary brain tumor, an ependymoma, was nonenhancing. This finding exemplifies an advantage of the bSSFP sequence over conventional postcontrast T1WI where primary tumors and their drop metastases may not enhance.
The diagnostic yield of bSSFP was greater than that of the postcontrast T1WI with 6.3 lesions per patient seen on the bSSFP sequence compared with 2.1 lesions per patient on the postcontrast T1WI, and this level reached statistical significance (P = .002).
One important consideration with the bSSFP sequence is awareness of the appearance of leptomeningeal metastases. In 3 of 44 patients, diffuse leptomeningeal disease was detected on postcontrast T1WI as avid enhancement along the surface of the spinal cord. On the bSSFP sequence, this finding appeared as subtle irregularity and distortion of the spinal cord contour. These cases highlight the occasional difficulty of detecting spinal leptomeningeal disease on the bSSFP sequence, which may present as subtle contour distortion and minimal irregularity.
Because of the findings in this study, we continue to advocate the use of postcontrast T1WI of the spine but recommend inclusion of the bSSFP sequence in staging evaluations. The combination of these 2 sequences offers patients the greatest detection of both focal drop metastases and diffuse leptomeningeal disease in the spine.
Although, on average, bSSFP imaging of the entire spine requires an additional 10 minutes of acquisition time, in our experience, this additional scan time is offset by the elimination of axial T1WI because the sagittal, isotropic bSSFP may be reformatted in the axial plane and thus may replace axial postcontrast T1WIs.
We found that the bSSFP sequence, when used as an adjunct to the conventional postcontrast T1WI, decreased the number of prominent vessels misclassified as potential drop metastases, reducing the risk of inaccurate tumor staging and incorrect risk-group assignment.
This study has limitations. The sample size was relatively small. Second, not all imaging was performed on the same MR imaging scanner platform with patients scanned on both 1.5T and 3T scanners. This heterogeneity in the scanning platform is not ideal because 3T imaging may detect a higher number of drop metastases compared with 1.5T imaging. In this study, the bSSFP and postcontrast T1WI of the same patient, which were directly compared with each other, were always performed on the same Tesla-strength scanner. Specifically, there were no instances in which a bSSFP sequence obtained on a 1.5T scanner was directly compared with a postcontrast T1WI performed on a 3T scanner, and vice versa. Last, there is no histopathologic confirmation for the determination of drop metastases. For this study, a constellation of the imaging findings and clinical assessment was used to determine the presence of spinal metastases. We think that this method for determining spinal drop metastases is scientifically sound, and we recognize that obtaining histopathologic confirmation of drop metastases in most cases is not feasible clinically.
Conclusions
The bSSFP sequence is a valuable adjunct for the evaluation of drop metastases in pediatric patients with primary intracranial tumors. As demonstrated in this study, the bSSFP sequence is particularly advantageous over conventional postcontrast T1WI for identifying nonenhancing drop metastases and small metastatic lesions ≤3 mm. In addition, the bSSFP sequence can help decrease the rate of false-positives due to the presence of vascular structures that may be mistaken for drop metastases on the postcontrast T1WI.
ABBREVIATION:
- bSSFP
balanced steady-state free precession
Footnotes
Paper previously presented at: Annual Meeting of the American Society of Neuroradiology and the Foundation of the ASNR Symposium, April 22–27, 2017; Long Beach, California.
References
- 1. Tai P, Dubey A, Salim M, et al. Diagnosis and management of spinal metastasis of glioblastoma. Can J Neurol Sci 2015;42:410–13 10.1017/cjn.2015.285 [DOI] [PubMed] [Google Scholar]
- 2. Ijiri K, Hida K, Yano S, et al. Traumatic spinal-cord herniation associated with pseudomeningocele after lower-thoracic nerve-root avulsion. Spinal Cord 2009;47:829–31 10.1038/sc.2009.38 [DOI] [PubMed] [Google Scholar]
- 3. Nayman A, Ozbek S. Redundant nerve root syndrome of the cauda equina: the benefits of 3D CISS MRI sequence. Spine J 2015;15:e31 10.1016/j.spinee.2015.05.021 [DOI] [PubMed] [Google Scholar]
- 4. Nemoto O, Fujikawa A, Tachibana A. Three-dimensional fast imaging employing steady-state acquisition MRI and its diagnostic value for lumbar foraminal stenosis. Eur J Orthop Surg Traumatol 2014;24(Suppl 1):S209–14 10.1007/s00590-013-1377-9 [DOI] [PubMed] [Google Scholar]
- 5. Ramli N, Cooper A, Jaspan T. High resolution CISS imaging of the spine. Br J Radiol 2001;74:862–73 10.1259/bjr.74.885.740862 [DOI] [PubMed] [Google Scholar]
- 6. Roser F, Ebner FH, Danz S, et al. Three-dimensional constructive interference in steady-state magnetic resonance imaging in syringomyelia: advantages over conventional imaging. J Neurosurg Spine 2008;8:429–35 10.3171/SPI/2008/8/5/429 [DOI] [PubMed] [Google Scholar]
- 7. Hashiguchi K, Morioka T, Yoshida F, et al. Feasibility and limitation of constructive interference in steady-state (CISS) MR imaging in neonates with lumbosacral myeloschisis. Neuroradiology 2007;49:579–85 10.1007/s00234-007-0225-1 [DOI] [PubMed] [Google Scholar]
- 8. McCormack EJ, Egnor MR, Wagshul ME. Improved cerebrospinal fluid flow measurements using phase contrast balanced steady-state free precession. Magn Reson Imaging 2007;25:172–82 10.1016/j.mri.2006.09.023 [DOI] [PubMed] [Google Scholar]
- 9. Abele TA, Besachio DA, Quigley EP, et al. Diagnostic accuracy of screening MR imaging using unenhanced axial CISS and coronal T2WI for detection of small internal auditory canal lesions. AJNR Am J Neuroradiol 2014;35:2366–70 10.3174/ajnr.A4041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ozgen B, Oguz B, Dolgun A. Diagnostic accuracy of the constructive interference in steady state sequence alone for follow-up imaging of vestibular schwannomas. AJNR Am J Neuroradiol 2009;30:985–91 10.3174/ajnr.A1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yoshida T, Sone M, Naganawa S, et al. Accuracy of 3.0 Tesla magnetic resonance imaging in the diagnosis of intracochlear schwannoma. Auris Nasus Larynx 2011;38:551–54 10.1016/j.anl.2010.12.011 [DOI] [PubMed] [Google Scholar]